Abstract
Background:
The objective of this study was to evaluate of prevalence of co-existing spine and hip disease using initial screening kidney–ureter–bladder (KUB) radiograph in patients over 50 who underwent spinal surgery.
Materials and Methods:
The study subjects were 388 patients (male: female=117:271; mean age 62.0 years) who underwent spinal surgery between 2008 and 2010. We retrospectively reviewed the initial KUB radiographs used to diagnose the spine and hip disease. Depending on the extent of acetabular and hip joint visualization in KUB, we divided the subjects into three groups: Acetabulum, hip joint, and femoral neck visualization. The hip visualization rate was also assessed with respect to patient height. χ2 and logistic regression test were used for statistical analysis.
Results:
126 (32.5%) cases had significant hip pathology including hip osteoarthritis (Kellgren/Lawrence grade 3 in 123 cases, grade 4 in 3 cases) and avascular necrosis (1 case each of Ficat stage IIA and IIB), and 8 cases had other morphologic abnormalities. Regarding acetabulum–hip visualization in KUB, 7 (1.8%) cases had acetabulum visualization only, 16 (4.1%) had hip joint visualization, and 365 (94.1%) had femoral neck including lesser trochanter visualization. Patients were categorized into four groups according to height (less than 150 cm, 150–159 cm, 160–169 cm, greater than 170 cm). The hip visualization rates differed significantly among these four groups (P<0.05).
Conclusions:
The prevalence of discernible hip pathology in patients who underwent spinal surgery was 32.5%. Hip joint visualization was excellent (98.2%) in KUB radiographs. Hence, spinal surgeons should pay attention to hip pathology in surgically indicated spinal patients.
Keywords: Hip pathology, spinal surgery, elderly
INTRODUCTION
The lower back pain, pelvic pain, and leg pain are common occurrence in aging patients and, careful scrutiny to achieve definitive diagnosis of the origin of the pain, such as spondylogenic, coxogenic, or both is mandatory. Comorbidity of spine and hip conditions sometimes results in misdiagnosis or delayed diagnosis.1
The purposes of this study were to assess the prevalence of hip pathology in patients who underwent spinal surgery and to test the diagnostic efficiency of conventional plain radiography of the kidney–ureter–bladder (KUB) to detect hip pathology.
MATERIALS AND METHODS
Between 2008 and 2010, 388 patients who had low back pain with or without pain in the lower extremities were enrolled in this study. This study was approved by the Institutional Review Board (IRB No. 4-2010-0615). All patients underwent spinal surgery for corresponding spinal conditions. After collecting medical history and performing a physical examination, diagnostic image tests such as KUB and lumbosacral lateral radiographs were performed in each supine and lateral decubitus position using a 14 × 17 inch cassette according to Rowe and Yohum's technique.2 Then, in all surgically indicated patients, magnetic resonance imaging (MRI) of the spine was performed. We retrospectively reviewed the corresponding 388 medical records to retrieve basic information of the patients. The rate and extent of visualization of both hip joints was assessed using KUB radiographs. To assess the extent of hip joint visualization, we divided the subjects into three groups depending on the extent of acetabular and hip joint visualization: acetabulum, hip joint, and femoral neck including lesser trochanter visualization [Figure 1a–c]. The hip visualization rate was also assessed with respect to patient's height.
Figure 1.
KUB lumbar spine AP and radiographic grades. (a) Acetabulum visualization: Entire (partial) acetabula are visible. (b) Hip joint visualization: Entire acetabula and femoral head areas are visible. (c) Femoral neck including lesser trochanter visualization: Entire hip joints including femoral necks and lesser trochanter areas are visible
In cases with any hip pathology according to the radiograph, possible diagnoses were made by two separate co-working hip surgeons. In cases of hip osteoarthritis and avascular necrosis of the femoral head, the Kellgren/Lawrence (K/L) scale and Ficat stage were used, respectively.3,4 The inter-observer correlation coefficient (r) was 0.91. Furthermore, based on the hypothesis that patient trunk height might affect the visualization rate or extent of the hip joints because KUB uses a standard sized radiographic cassette (14 × 17 inch), patients were categorized into four groups according to height. The statistical differences among groups were evaluated using the χ2 and logistic regression test, and all P<0.05 were considered significant.
RESULTS
The 388 patients consisted of 117 males and 271 females with an average age of 62.0 ± 7.9 years, ranging from 50 to 87 years (males 63.0 ± 8.0 years, range 50–87; females 61.5 ± 7.9 years, range 50–86) [Figure 2]. The average patient height was 157.8 ± 8.8 cm, with a range of 120–183 cm (males 166.7 ± 6.9 cm, range 130–183; females 154.0 ± 6.5 cm, range 120–180). Of these, most patients (377 cases, 97.2%) presented with lower back pain and leg pain and the remainder (11 cases, 2.8%) complained of lower back pain only. Distribution of patients according to symptom duration was quite heterogeneous, ranging from 0.1 to 360 months (mean duration 43.4 ± 58.2 months).
Figure 2.
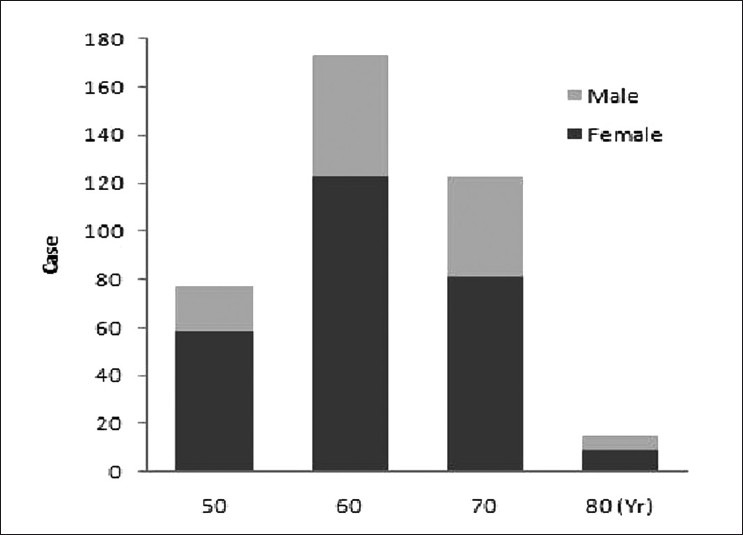
Composition of patient groups according to age and gender
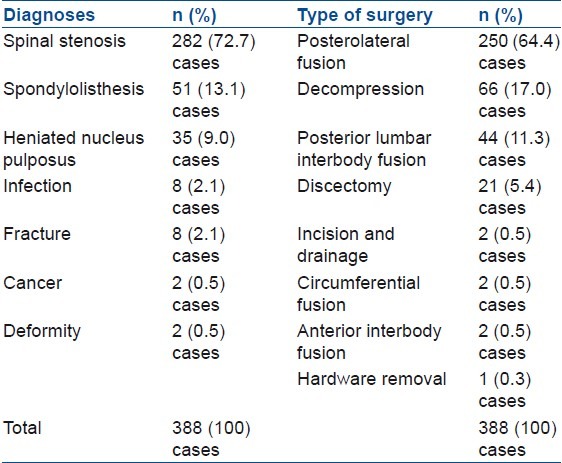
The major diagnoses were spinal stenosis (n=282, 72.7%), spondylolisthesis (n=51, 13.1%), and herniated nucleus pulposus (n=35, 9.0%), although 22 cases (5.6%) had other diagnoses. Twenty-eight patients had undergone previous spinal surgery. Patient treatments included posterolateral fusion (n=250, 64.4%), decompression (n=66, 17.0%), discetomy (n=21, 5.4%), posterolumbar interbody fusion (n=44, 11.3%) and other treatments (n=7, 1.8%) [Table 1].
Table 1.
Diagnoses and type of surgery treatments of enrolled patients
The results of radiologic investigation for hip arthropathy showed that 126 (32.5%) cases had significant hip disease including hip osteoarthritis (123 cases of KL grade 3 and 3 cases of grade 4) and avascular necrosis of the femoral heads (1 case each of Ficat stage IIA and stage IIB). Other morphologic abnormalities were seen in eight cases, including five cases of coxa valga and three cases of other hip dysplasia [Figure 3].
Figure 3.
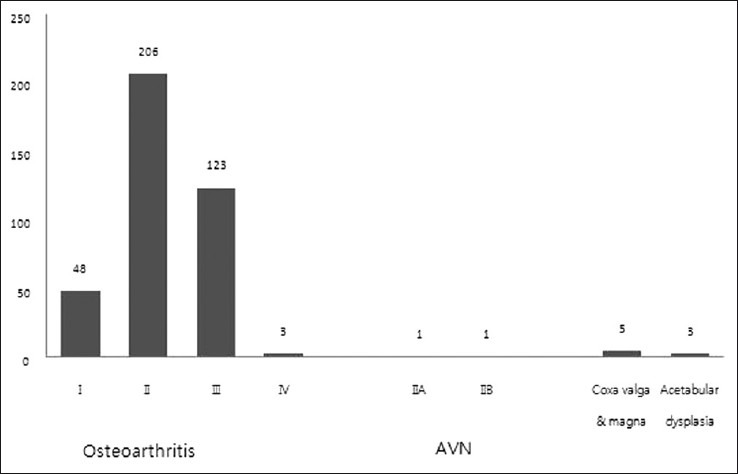
Hip pathologies detected on KUB lumbar anteriorposterior X-rays. In cases of hip osteoarthritis and avascular necrosis of the femoral head, the Kellgren/Lawrence (K/L) scale6 and Ficat stage7 were used. AVN, avascular necrosis
The severity of osteoarthritic hip joints differed significantly depending on age (P=0.05, logistic regression), with older patients exhibiting more advanced osteoarthritis [Figure 4].
Figure 4.
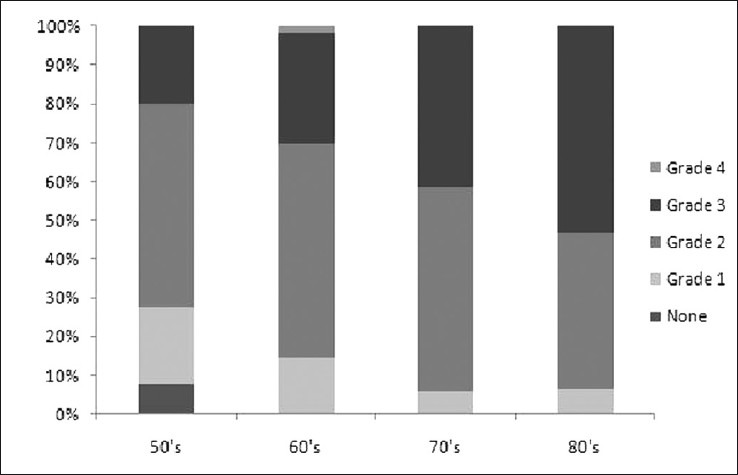
Distribution of hip osteoarthritis according to age. Older patients had greater progression of osteoarthritis (P<0.05, χ2; P=0.05, logistic regression)
Regarding radiographic grade, 7 (1.8%) cases were classified as acetabular visualization, 16 (4.1%) as hip joint visualization, and 365 (94.1%) as femoral neck including lesser trochanter visualization. The extent of hip visualization showed statistically significant differences among the four groups categorized by height according to the χ2 test (P<0.05) and logistic regression tests (P=0.05, logistic regression). In the two tallest groups (160–169 cm and greater than 170 cm), higher percentages of acetabular visualization and hip joint visualization were observed [Table 2, Figure 5].
Table 2.
Comparison of visualization rates among the four height groups
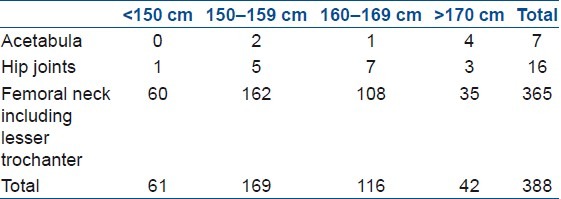
Figure 5.
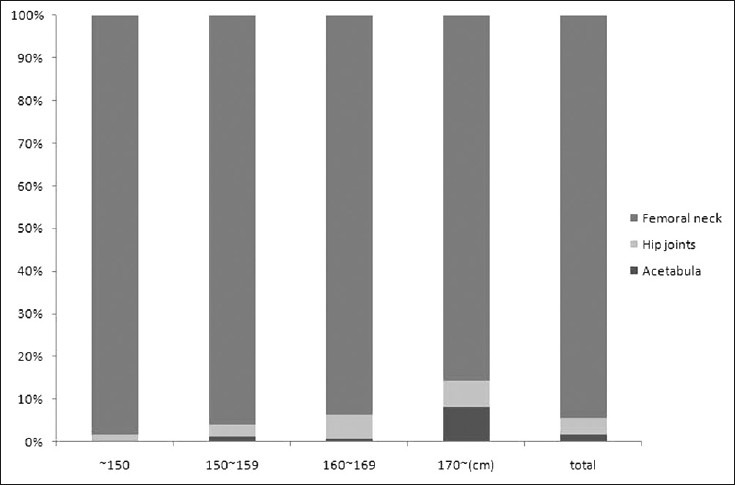
The distribution of the extents of radiographic visualization in the four height groups. The percentages of acetabula visualization and hip joint visualization increased with height (P<0.05, χ2; P=0.05, logistic regression)
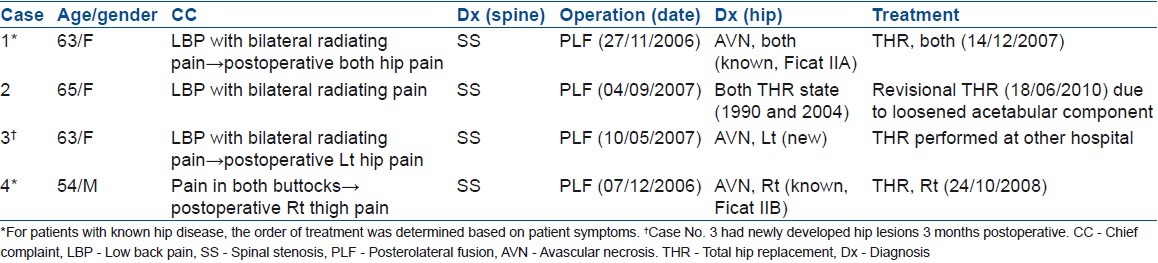
The rate of complete visualization of the lumbar spine and hip joint in single plain KUB was 98.2%, as determined by the sum of hip joint visualization and femoral neck visualizations (381 of 388 cases). Most patients with hip pathology were followed up by a hip reconstructive surgeon. Additionally, the Patrick test was not effective to detect hip pathologic condition [Table 3]. The sensitivity was heterogeneous (0–33.3%) depending on the disease status. Four patients underwent total hip replacement based on the priority to treat hip and spine disease; the others were treated conservatively [Table 4].
Table 3.
The Patrick test results under the hip pathologic condition at spinal operation
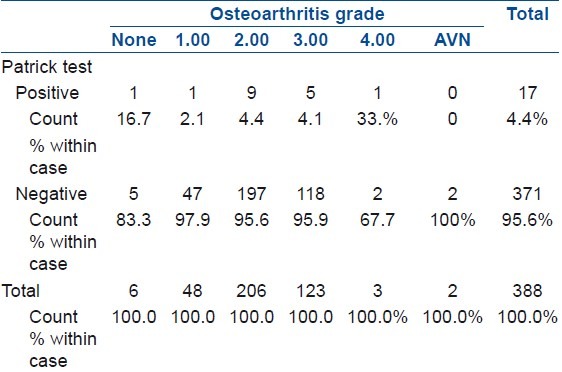
Table 4.
Patients who underwent hip surgery after a spinal operation
DISCUSSION
A recent increase in life expectancy in the general population makes musculoskeletal diseases in elderly people to become major challenges for orthopedic surgeons.5 Hip and spine arthritis in the aged population is part of the same degenerative process and coexist.6 Co-existence of spine and hip pathologies, especially in patients who are indicated for lumbar spinal surgery, prompts spinal surgeons to evaluate the exact source of pain to avoid jeopardizing the surgical outcomes. Therefore, statistics regarding the prevalence of hip pathology in surgically indicated spinal patients are needed.
Furthermore, to rule out spine and hip conditions in the initial screening radiograph, separate lumbar spine and pelvis plain radiographs can be commonly conducted; however, this extra step increases medical costs and radiation exposures of the patients. Evaluation of the diagnostic efficiency of screening spine radiographs for visualization is therefore also needed. Therefore, we tried to assess the prevalence of hip pathology in patients who underwent spinal surgery and to test the diagnostic efficiency of conventional plain radiography of the KUB to visualize hip joints and detect hip pathology.
The differentiation of signs and symptoms suggestive of hip disorder versus spine disorder is important in order to provide proper treatment, especially when the patient has pain associated with both hip and spine disorders. Patients with osteoarthrosis of the hip may present with radiating pain below the knee, back pain, and limited internal rotation of the hip, creating difficulty in the determination of spine versus hip etiology.7 Various physical examination maneuvers have been described to localize the pain source, but most of these have been shown to have either poor inter-observer reproducibility or validity.8 Also, patients in severe or chronic pain may report pain aggravation with almost any maneuver, thus decreasing the specificity of the test.9
Several studies have shown that decompression in patients with spine disorders does not alleviate pain if hip arthrosis is also present.10 In some patients, treatment of one disorder has led to the development of another disorder, for example, development of foot drop secondary to spinal pathology after hip arthroplasty.11 Thus necessitating lumbar decompression. A study by McNamara et al. reported patients with concurrent hip disease and spinal stenosis who initially underwent hip arthroplasty, followed by decompression of spinal stenosis.12 The results showed that eight of nine patients who had decompression reported good or excellent subjective relief of symptoms at their final followup visit.12 The order of treatment for pain depends on the presence of neurologic symptoms and sequelae or the presence of a fixed flexion contracture and absence of neurologic deficits.13 In our series, two patients were diagnosed with simultaneous spinal stenosis and avascular necrosis of the femoral heads. Both underwent spinal surgery first because of spine-originated neurologic symptoms and then underwent total hip arthroplasties as the avascular necrosis progressed. They had favorable outcomes at their final followups in July 2010 and December 2008.
Thus, it should be emphasized that a definitive differential diagnosis and identification of the anatomic source of pain is most important for selecting the proper therapeutic modality. Nevertheless, correct diagnosis based on patient history, physical examination, and simple radiography is sometimes difficult, particularly in the presence of a significant spinal disorder. Several signs and symptoms such as limp, groin pain, limited internal rotation, and reduced spinal range of motion (ROM) have been associated with low back and leg pain.13,14 Other possible, but presumably less common, origins of pain are the retroperitoneal structures within the abdominal and pelvic cavities. Antolak et al. reported that ureter stones could chronically compress and irritate the L2–4 sensory fibers, either part of the obturator or femoral nerve, around the psoas muscle and cause medical thigh pains.15 Pain may also arise from the sacroiliac joint.16–18
Consequently, all small clues should receive attention in order to avoid missing or overlooking important signs that differentiate the most common co-existing diseases. It is useful to take plain radiographs for initial screening of hip and spine disease and to detect the additional rare possibility of urolithiasis. However, plain radiographs may be unable to detect early stages of disease or other intra-articular pathologies such as a labral tear or chondral lesions. In the absence of arthritic changes in the setting of positive physical examination findings, patients could undergo assessment of intra-articular pathologies such as a labral tear.19 One of our cases had collection of hip joint fluid that could not be detected via plain radiographs and lumbar spine MRI. She had aggravating pain for 10 years in both buttocks and radiculopathy in the left lower extremity. The diagnosis was degenerative spondylolisthesis L3 on L4. After decompression and fusion at the L3–4 area, she experienced some improvement in her symptoms (preoperative Oswestry Disability Index score 22 decreased to 13 postoperatively) but complained of continued left hip pain. The MRI of left hip showed hip effusion and she responded to the additional medical treatment.
Since 1983, when Offierski and MacNab discussed the significance of the relationship between the spine and hip joints, described as hip spine syndrome,20 many authors have studied their inter-related pathologies.21–24 Therefore, the inextricable connection between the hip and spine should be considered in relevant cases. One of the purposes of this study was to increase surgeons’ levels of awareness of the co-existence of spine hip diseases and the importance of order of treatment for these two conditions. Therefore, we chose a group of patients who had undergone surgery for spinal disease to determine whether there were any cases that inevitably required another operation on their hip and/or other pain source due to the incorrect initial diagnosis or order of treatment. Fortunately, our study population contained no such cases because of easiness in patients’ referral between the hip and spine department in our clinic.
Another purpose of the study was to increase diagnostic convenience for both physicians and patients. So far, we have taken both KUB and pelvis anteroposterior radiographs at once for initial imaging study. But in the aspect of saving medical expenses and avoiding additional radiation exposure, although KUB X-rays may not be valuable as confirmatory diagnostic tools for hip diseases, we hypothesized that they are sufficiently useful to visualize and diagnose hip joint problems. In our study, visualization of the hip joint was sufficient to evaluate hip pathology in 381 (98.2%) cases. During the followup period, the patients who were classified as acetabula visualization on their first screening KUB could be classified as hip joint or femoral neck including lesser trochanter visualization on their followup films. Among 11 cases of acetabula visualization, 5 cases could be classified as hip joint and femoral neck including lesser trochanter visualization. This indicated that a standardized methodology of KUB X-rays might increase the effectiveness of KUB as a screening test, especially as there are variations in the procedure depending on the radiographer.
Hip arthritis is a much lesser common condition in comparison to low back pain, afflicting only 3.2% of the population older than 55 years, which is disabling enough to warrant joint arthroplasty in some patients.25 The results of the current study demonstrated that the prevalence of comorbid hip pathology in patients with spine conditions who underwent spinal surgery was 32.5%. All of them were not severe enough to undergo total hip arthroplasty. Also, not all patients were symptomatic on their hip, as the Patrick tests were positive only for 4.4% of pathologic hip conditions. But we archived some useful information of hip pathology rate in patients who underwent lumbar spine surgery.
Furthermore, we showed that a simple KUB radiograph can provide visualization of the hip joint at a rate of 98.2%, sufficiently high to rule out hip pathology, although in rare cases (1.8%), the hip joint was not included in the simple KUB radiograph. Nonvisualization of the hip joint in the KUB radiograph mandates an additional radiographic examination of the hip joint due to the high prevalence of hip pathology in patients with spinal conditions. The limitation of the present study is that we have focused on the radiographic evaluation of hip pathology using single radiograph without correlating the pathologic condition with the surgical outcome of the patients. In future, we will try to investigate the clinical correlation of hip pathologic condition with the surgical outcome.
In conclusion, we found discernible hip pathology on KUB in 32.5% of the patients who underwent spinal surgery. The diagnostic efficiency of conventional plain radiograph of KUB in the detection of hip pathology was sufficient (98.2%) for it to be used as an initial screening test for diseases of the spine and hip, as well as other possible diseases.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Swezey RL. Overdiagnosed sciatica and stenosis, underdiagnosed hip arthritis. Orthopedics. 2003;26:173–4. doi: 10.3928/0147-7447-20030201-20. [DOI] [PubMed] [Google Scholar]
- 2.Rowe LJ, Yochum TR. Radiographic positioning and normal anatomy. In: Yochum TR, Rowe LJ, editors. Essentials of skeletal radiology. 2nd ed. Baltimore: Williams and Wilkins; 1996. pp. 1–138. [Google Scholar]
- 3.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ficat RP. Idiopathic bone necrosis of the femoral head.Early diagnosis and treatment. J Bone Joint Surg Br. 1985;67:3–9. doi: 10.1302/0301-620X.67B1.3155745. [DOI] [PubMed] [Google Scholar]
- 5.Baek GH. Are we prepared for geriatric orthopedics? Clin Orthop Surg. 2010;2:129. doi: 10.4055/cios.2010.2.3.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Parvizi J, Pour AE, Hillibrand A, Goldeberg G, Sharkey PF, Rothman RH. Back pain and total hip arthroplasty: A prospective natural history study. Clin Orthop Relat Res. 2010;468:1325–30. doi: 10.1007/s11999-010-1236-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wolfe F. Determinants of WOMAC function, pain and stiffness scores: Evidence for the role of low back pain, symptom counts, fatigue and depression in osteoarthritis, rheumatoid arthritis and fibromyalgia. Rheumatology. 1999;38:355–61. doi: 10.1093/rheumatology/38.4.355. [DOI] [PubMed] [Google Scholar]
- 8.Stuber KJ. Specificity, sensitivity, and predictive values of clinical tests of the sacroiliac joint: A systematic review of the literature. J Can Chiropr Assoc. 2007;51:30–41. [PMC free article] [PubMed] [Google Scholar]
- 9.Waddell G, McCulloch JA, Kummel E, Venner RM. Nonorganic physical signs in low-back pain. Spine. 1980;5:117–25. doi: 10.1097/00007632-198003000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Airaksinen O, Herno A, Turunen V, Saari T, Suomlainen O. Surgical outcome of 438 patients treated surgically for lumbar spinal stenosis. Spine. 1997;22:2278–82. doi: 10.1097/00007632-199710010-00016. [DOI] [PubMed] [Google Scholar]
- 11.Pritchett JW. Lumbar decompression to treat foot drop after hip arthroplasty. Clin Orthop Relat Res. 1994:173–7. [PubMed] [Google Scholar]
- 12.McNamara MJ, Barrett KG, Christie MJ, Spengler DM. Lumbar spinal stenosis and lower extremity arthroplasty. J Arthroplasty. 1993;8:273–7. doi: 10.1016/s0883-5403(06)80089-6. [DOI] [PubMed] [Google Scholar]
- 13.Brown MD, Gomez-Marin O, Brookfield KF, Li PS. Differential diagnosis of hip disease versus spine disease. Clin Orthop Relat Res. 2004:280–4. doi: 10.1097/00003086-200402000-00044. [DOI] [PubMed] [Google Scholar]
- 14.Steultjens MP, Dekker J, van Baar ME, Oostendorp RA, Bijlsma JW. Range of joint motion and disability in patients with osteoarthritis of the knee or hip. Rheumatology. 2000;39:955–61. doi: 10.1093/rheumatology/39.9.955. [DOI] [PubMed] [Google Scholar]
- 15.Antolak C, Canales B, Monga M. Medial thigh pain: Neurology or urology? Urology. 2005;65:799. doi: 10.1016/j.urology.2004.10.056. [DOI] [PubMed] [Google Scholar]
- 16.Sembrano JN, Polly DW., Jr How often is low back pain not coming from the back? Spine. 2009;34:E27–32. doi: 10.1097/BRS.0b013e31818b8882. [DOI] [PubMed] [Google Scholar]
- 17.Fortin JD, Aprill CN, Ponthieux B, Pier J. Sacroiliac joint: Pain referral maps upon applying a new injection/arthrography technique. Part II: Clinical evaluation. Spine. 1994;19:1483–9. [PubMed] [Google Scholar]
- 18.Dreyfuss P, Michaelsen M, Pauza K, McLarty J, Boqdok N. The value of medical history and physical examination in diagnosing sacroiliac joint pain. Spine (Phila Pa 1976) 1996;21:2594–602. doi: 10.1097/00007632-199611150-00009. [DOI] [PubMed] [Google Scholar]
- 19.Toomayan GA, Holman WR, Major NM, Kozlowicz SM, Vali TP. Sensitivity of MR arthrography in the evaluation of acetabular labral tears. AJR Am J Roentgenol. 2006;86:449–53. doi: 10.2214/AJR.04.1809. [DOI] [PubMed] [Google Scholar]
- 20.Offierski CM, MacNab I. Hip-spine syndrome. Spine (Phila Pa 1976) 1983;8:316–21. doi: 10.1097/00007632-198304000-00014. [DOI] [PubMed] [Google Scholar]
- 21.Yoshimoto H, Sato S, Masuda T, Kanno T, Shundo M, Hyakumachi T, et al. Spinopelvic alignment in patients with osteoarthrosis of the hip: A radiographic comparison to patients with low back pain. Spine(Phila Pa 1976) 2005;30:1650–7. doi: 10.1097/01.brs.0000169446.69758.fa. [DOI] [PubMed] [Google Scholar]
- 22.Itoi E. Roentgenographic analysis of posture in spinal osteoporotics. Spine (Phila Pa 1976) 1991;16:750–6. doi: 10.1097/00007632-199107000-00011. [DOI] [PubMed] [Google Scholar]
- 23.Matsuyama Y, Hasegawa Y, Yoshihara H, Tsuji T, Sakai Y, Nakamura H, et al. Hip-spine syndrome: Total sagittal alignment of the spine and clinical symptoms in patients with bilateral congenital hip dislocation. Spine (Phila Pa 1976) 2004;29:2432–7. doi: 10.1097/01.brs.0000143671.67779.14. [DOI] [PubMed] [Google Scholar]
- 24.Ben-Galim P, Ben-Galim T, Rand N, Haim A, Hipp J, Dekel S, et al. Hip-spine syndrome: The effect of total hip replacement surgery on low back pain in severe osteoarthritis of the hip. Spine (Phila Pa 1976) 2007;32:2099–102. doi: 10.1097/BRS.0b013e318145a3c5. [DOI] [PubMed] [Google Scholar]
- 25.Fear J, Hillman M, Chamberlain MA, Tennant A. Prevalence of hip problems in the population aged 55 years and over: Access to specialist care and future demand for hip arthroplasty. Br J Rheumatol. 1997;36:74–6. doi: 10.1093/rheumatology/36.1.74. [DOI] [PubMed] [Google Scholar]



