Abstract
Chemical burn under pneumatic tourniquet is an iatrogenic preventable injury and is rarely reported in the literature. The two important mechanisms are maceration (friction) and wetness underneath the tourniquent. In this report, our experience with two illustrative patients who presented with iatrogenic tourniquet associated burn is described.
Keywords: Chemical burn, irritation, maceration, tourniquet
INTRODUCTION
Pneumatic tourniquets have been commonly utilized during orthopedic extremity surgeries to attain a bloodless field facilitating operative procedures. Although tourniquet associated complications including postoperative swelling, delay of recovery of muscle power, compression neuropraxia, wound hematoma with the potential for infection, vascular injury, tissue necrosis, compartment syndrome, and systemic complications have been reported in the literature, the iatrogenic chemical burn during pneumatic tourniquet use has been rarely reported.1–4 Here, we report two cases of chemical burn to sensitize the orthopaedic surgeons about its possible occurrence.
CASE REPORTS
Case 1
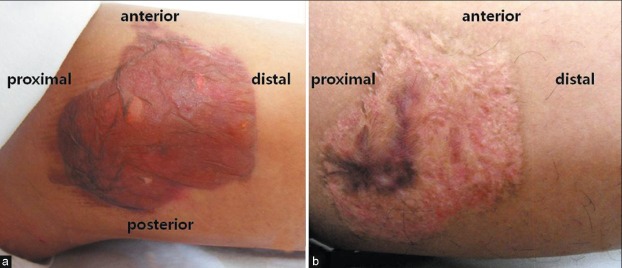
A 24 year old male underwent lateral meniscus allograft transplantation on his left knee. The patient did not have thin skin and any underlying skin disease and allergies. The patient's operation was performed under tourniquet control. The tourniquet cuff used was a standard leg tourniquet (18 cm) and was applied with four layers of adequate wool padding. The skin preparation used was a 10% povidone-iodine (betadine) solution. The set pressure was 250 mmHg which was about 100 mmHg higher than the patient's systolic pressure. The tourniquet compression time was 2 h (total operation time=3 h). When the tourniquet was removed after operation, the burn was seen on the medial aspect of thigh [Figure 1a]. While inspecting the padding where the burn was present, the drape preparation seemed to have run down the patient's thigh during painting and had been left in wet condition underneath the tourniquet. The wound was of intermediate to deep second degree burn with blisters of size about 5 × 6 cm. The patient was treated conservatively with a furazone gauze occlusive dressing and was discharged from orthopedic department without skin grafting. However, he underwent multiple treatments with the dermatologist for complete healing which took almost 12 months [Figure 1b]. Even to this time (2 years postoperation), the patient continuously complains of hypersensitivity on the scar area, which aggravates during normal gait.
Figure 1.
Case 1. Tourniquet-associated chemical burn developed on medial aspect of thigh: (a) immediate postoperative; (b) 1year and 9 months postoperative
Case 2
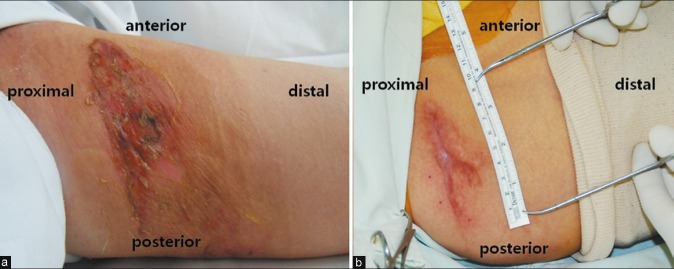
A 65 year old female patient, underwent elective unicompartmental knee arthroplasty for medial compartment osteoarthritis of the knee. The patient was free of chronic underlying diseases and had moderate skin thickness. The tourniquet cuff used was a standard leg tourniquet and was applied with four layers of adequate wool padding. The skin preparation used was a 10% povidone-iodine (betadine) solution. The set pressure was 250 mmHg which was about 100 mmHg higher than the patient's systolic pressure. The tourniquet compression time was 1.5 h (total operation time=2 h). When the tourniquet was removed, the burn was seen on the medial aspect of thigh. The burn was also of intermediate to deep second degree with dermis involvement. Betadine soaked padding was also observed at the site of burn. One week postoperatively, blisters and crusts were found roughly at the proximal margin of tourniquet [Figure 2a]. Local furazone gauze was applied for dressing and complete healing needed almost 1 year after operation. During this followup period, analgesics were continuously prescribed for the irritating, hypersensitive scar. Scar revision excising this hypersensitive, hypertrophic scar was needed after 1 year 4 months postoperatively [Figure 2b].
Figure 2.
Case 2. Tourniquet-associated chemical burn developed on medial aspect of thigh: (a) 1 week postoperative; (b) 1 year and 4 months postoperative (just prior to scar excision)
DISCUSSION
The chemical burn resulting from tourniquet application cause more in-depth injury to the skin than the abrasion wound because there is greater time exposure and the anesthesia prevents the patient from reacting to the noxious burn stimulus.5 Consequently, multiple debridement, skin graft, and even flap surgeries may be needed in such injuries with prolonged treatment period. Both of our cases had intermediate to deep second degree burn extending into deep dermis. Not only a long duration of healing time (up to 1 year postoperatively) was needed, but also hypersensitive and painful scar remained thereafter. The iatrogenic chemical burn induced by tourniquet application can have an impact on surgeon patient relationship.
Tourniquet associated chemical burns have been reported previously also. Dickinson and Bailey1 reported four burns beneath the cuffs of pneumatic tourniquets. In all cases, the burns were seen when the tourniquet was removed. In two cases, the area of iodine staining corresponded exactly with the area of the burn, while in the other two cases the burns were smaller. All burns were of partial thickness and healed within 4 weeks, leaving minimal scarring. Nahlieli et al.2 reported three adult cases. One of these patients had a partial thickness burn under the tourniquet cuff, after a 2-h surgery on his right palm. Similar experiences were reported by other authors.3,6 The scars described in these reports seem to have healed without much complications. Unlike the previous reported cases, our cases required prolonged healing time and patients continuously complained discomfort in the scar area. The basic mechanism of tourniquet induced chemical burn involves irritation by antiseptics2,4,7,8 coupled with maceration,9–11 compression pressure,12–14 duration of compression,13,14 and wetness underneath the tourniquet.15,16 Polyvinylpyrrolidone-iodine (PI) is a widely used antiseptic which was introduced by Shelanski and Shelanski in 1965.17 It is a water-soluble compound that results from the combination of molecular iodine and polyvinylpyrrolidone. The preparations of commercially available PI are povidone-iodine (betadine) solution, scrub, ointment, tincture, and foam; of these, the solution is the most commonly used. The 10% PI solution generally contains 90% water, 8.5% polyvinylpyrrolidone, and 1% available iodine and iodide (pH 4.5–5.5). Although uncommon, chemical burns have been reported with this solution.2,5,18–21 Alcohol (70%), which is used for draping, may also cause hypersensitivity.2,4,7 By using alcohol, the epidermal lipid barrier acting to the skin may be decreased by de-esterification.
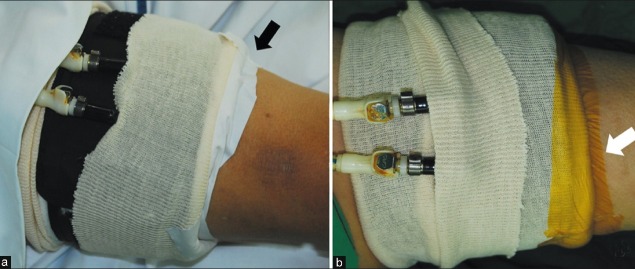
To prevent tourniquet associated chemical burn, two important points should be noted. First, friction between the skin and the tourniquet should be avoided because macerated skin becomes more permeable to PI which may become prone for damage. Movement of tourniquet during draping and compression should also be prevented. An elastic stockinette is known to be effective in preventing the development of maceration induced blisters.22 The shape mismatch between the tourniquet and the thigh should be considered when applying tourniquet to minimize friction. Very muscular or obese patients tend to have conical shaped thigh.14 Even distribution moving the skin and the soft tissues distally underneath the tourniquet may overcome this mismatch. Second, emphasis should be made on some form of barrier occluding the tourniquet, preventing wool soaking from antiseptics.15,16 In addition to a number of commercial covers, a variety of simple, non commercial alternatives have been proposed. Sarkhel and Stride15 suggested using the disposable reservoir bag from a single use anesthetic circuit, while the use of surgical glove was proposed by Tomlinson and Harries.16 Our department has been using adhesive plaster (Sinsin Pharm Co. Ltd., Korea) and antimicrobial incise drape (Ioban™ 2®, 3M Health care, USA) for mechanical barrier [Figure 3a and b]. On taking these precautions, further occurrence of tourniquet associated chemical burns was prevented.
Figure 3.
Suggested method for tourniquet application with elastic stockinette and wool padding. Note the adhesive plaster (black arrow) (a) and antimicrobial incise drape (white arrow) (b) used for mechanical barrier
The chemical burn due to pneumatic tourniquet is a relatively under-reported problem which may be more frequent than believed. The PI related chemical burn in tourniquet use may be prevented by understanding the mechanism of occurrence of this complication to prevent this devastating iatrogenic injury.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Dickinson JC, Bailey BN. Chemical burns beneath tourniquets. Br Med J. 1988;297:1513. doi: 10.1136/bmj.297.6662.1513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nahlieli O, Baruchin AM, Levi D, Shapira Y, Yoffe B. Povidone-iodine related burns. Burns. 2001;27:185–8. doi: 10.1016/s0305-4179(00)00081-4. [DOI] [PubMed] [Google Scholar]
- 3.Handley R. Chemical burns beneath tourniquets. Br Med J. 1989;298:254. [PMC free article] [PubMed] [Google Scholar]
- 4.Chiang YC, Lin TS, Yeh MC. Povidone-iodine-related burn under the tourniquet of a child - a case report and literature review. J Plast Reconstr Aesthet Surg. 2011;64:412–5. doi: 10.1016/j.bjps.2010.04.032. [DOI] [PubMed] [Google Scholar]
- 5.Hodgkinson DJ, Irons GB, Williams TJ. Chemical burns and skin preparation solutions. Surg Gynecol Obstet. 1978;147:534–6. [PubMed] [Google Scholar]
- 6.Madhok R. Chemical burns beneath tourniquets. Br Med J. 1989;298:254. [PMC free article] [PubMed] [Google Scholar]
- 7.Lowe DO, Knowles SR, Weber EA, Railton CJ, Shear NH. Povidone-iodine-induced burn: Case report and review of the literature. Pharmacotherapy. 2006;26:1641–5. doi: 10.1592/phco.26.11.1641. [DOI] [PubMed] [Google Scholar]
- 8.Okano M. Irritant contact dermatitis caused by povidone-iodine. J Am Acad Dermatol. 1989;20:860. doi: 10.1016/s0190-9622(89)80129-x. [DOI] [PubMed] [Google Scholar]
- 9.Bruner JM. Safety factors in the use of the pneumatic tourniquet for hemostasis in surgery of the hand. J Bone Joint Surg Am. 1951;33:221–4. [PubMed] [Google Scholar]
- 10.Kutty S, McElwain JP. Padding under tourniquets in tourniquet controlled surgery: Bruner's ten rules revisited. Injury. 2002;33:75. doi: 10.1016/s0020-1383(01)00072-9. [DOI] [PubMed] [Google Scholar]
- 11.McEwen JA, Kelly DL, Jardanowski T, Inkpen K. Tourniquet safety in lower leg applications. Orthop Nurs. 2002;21:55–62. doi: 10.1097/00006416-200209000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Delgado-Martinez AD. Pneumatic tourniquets in extremity surgery. J Am Acad Orthop Surg. 2002;10:232. doi: 10.5435/00124635-200205000-00010. [DOI] [PubMed] [Google Scholar]
- 13.Noordin S, McEwen JA, Kragh JF, Jr, Eisen A, Masri BA. Surgical tourniquets in orthopaedics. J Bone Joint Surg Am. 2009;91:2958–67. doi: 10.2106/JBJS.I.00634. [DOI] [PubMed] [Google Scholar]
- 14.Wakai A, Winter DC, Street JT, Redmond PH. Pneumatic tourniquets in extremity surgery. J Am Acad Orthop Surg. 2001;9:345–51. doi: 10.5435/00124635-200109000-00008. [DOI] [PubMed] [Google Scholar]
- 15.Sarkhel T, Stride V. The Tourniqu Aid: Prevention of chemical burns. Injury. 2002;33:73–4. doi: 10.1016/s0020-1383(01)00045-6. [DOI] [PubMed] [Google Scholar]
- 16.Tomlinson PJ, Harries WJ. The use of a surgical glove in the prevention of tourniquet-associated chemical burns. Ann R Coll Surg Engl. 2008;90:255. doi: 10.1308/003588408X285720c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shelanski HA, Shelanski MV. PVP-iodine: History, toxicity and therapeutic uses. J Int Coll Surg. 1956;25:727–34. [PubMed] [Google Scholar]
- 18.Bayne D. Prevention of chemical burns. Ann R Coll Surg Engl. 2008;90:715. doi: 10.1308/003588408X321846h. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hubik DJ, Connors A, Cleland H. Iatrogenic chemical burns associated with tourniquet use and prep solution. ANZ J Surg. 2009;79:762. doi: 10.1111/j.1445-2197.2009.05071.x. [DOI] [PubMed] [Google Scholar]
- 20.Liu FC, Liou JT, Hui YL, Hsu JC, Yang CY, Yu HP, et al. Chemical burn caused by povidone-iodine alcohol solution – a case report. Acta Anaesthesiol Sin. 2003;41:93–6. [PubMed] [Google Scholar]
- 21.Nakano S, Uchiyama A, Ueyama H, Nishimura M, Tashiro C, Azuma T. Chemical burn caused by povidone-iodine. Masui. 1991;40:812–5. [PubMed] [Google Scholar]
- 22.Saleh KJ. An elastic stockinette under a pneumatic tourniquet protected against the development of blisters during total knee arthroplasty. J Bone Joint Surg Am. 2007;89:459. doi: 10.2106/JBJS.8902.ebo3. [DOI] [PubMed] [Google Scholar]