Abstract
Closed traumatic flexor injuries of the hand involving the pulley mechanism are a relatively common injury seen in rock climbers but are very rare in nonclimbers, including bowlers. The injury was first described in 1990. Since then, several studies have shed more light on the diagnostic and therapeutic considerations. Early diagnosis of pulley injuries is crucial since delayed diagnosis can lead to limited range of motion, particularly at the proximal interphalangeal joint. Flexion contractures at the proximal interphalangeal joint have also been cited in the literature. We discuss a case of pulley injury in a bowler and briefly review the anatomy of the pulley architecture, mechanism of injury, imaging manifestations, and clinical management of this injury.
CASE REPORT
A 34-year-old man visited an orthopedist 3 weeks after sustaining an injury to the right long finger. The patient mentioned that his right long finger got stuck in a bowling ball at the time of throwing the ball. He had initially gone to the local emergency room, where radiographs were taken and did not show any evidence of fracture. Finger strain was suspected, and the patient was discharged. Later, at an orthopedist's office, his right long finger was noted to be tender. He had pain directly over the A2 pulley. His proximal phalanx at its palmar aspect was somewhat swollen. The range of motion in this finger was intact. No neurologic or vascular deficits were noted. A strain or A2 pulley rupture of the right long finger was clinically suspected. Magnetic resonance imaging (MRI) was ordered for further clarification.
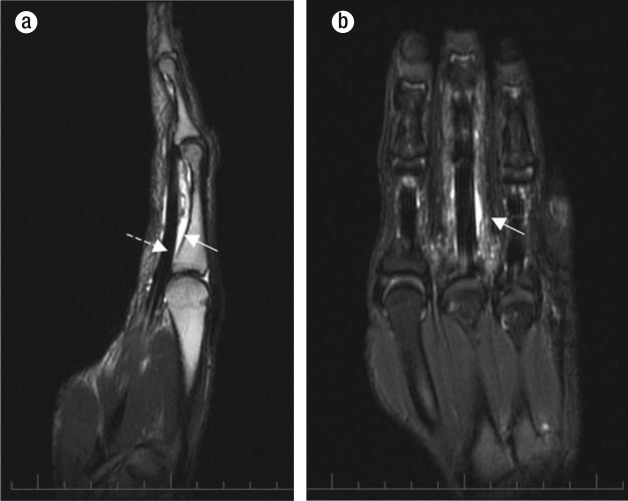
MRI of the right hand revealed prominent edema between the flexor tendons and proximal phalanx of the long finger, with abnormal separation of the flexor tendons from the proximal phalanx (Figures 1 and 2a). The A2 pulley appeared discontiguous, consistent with rupture (Figure 1). The metacarpophalangeal and interphalangeal collateral ligaments were intact. Mild to moderate tenosynovitis of the long finger flexor tendon was noted (Figure 2). No bony injury was identified.
Figure 1.
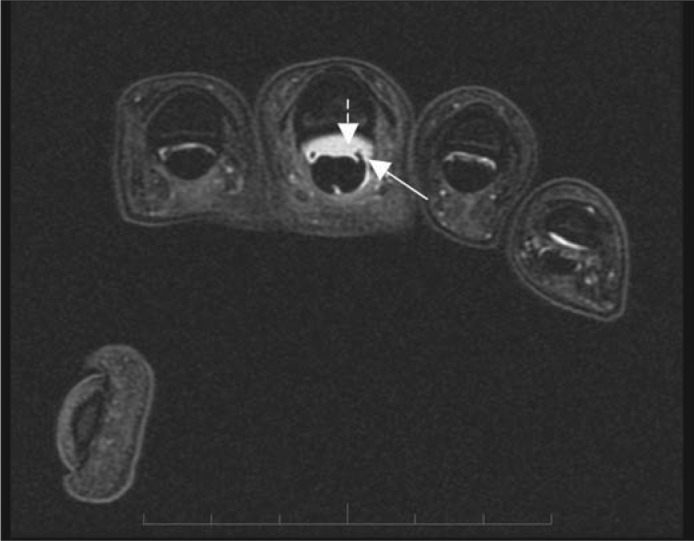
Axial short T1 inversion recovery (STIR) image demonstrates prominent edema (dashed arrow) between the flexor tendons and proximal phalanx of the long finger with abnormal separation of the flexor tendon from the proximal phalanx. Rupture of the A2 pulley was also noted (arrow).
Figure 2.
Additional STIR images. (a) Sagittal STIR image demonstrates prominent edema between the flexor tendons and the proximal phalanx with abnormal separation of the flexor tendons from the proximal phalanx (arrow). Tenosynovitis of the long flexor tendon is also present (dashed arrow). (b) Coronal STIR image demonstrates moderate tenosynovitis of the long flexor tendon (arrow).
DISCUSSION
The flexor pulley system is composed of focal thickened areas of the flexor tendon sheath (1). It consists of five annular pulleys (A1–A5) and three cruciate pulleys (C1–C3), which reinforce the structure of the flexor tendon sheaths (Figure 3). These pulleys also provide a fulcrum to elicit flexion and extension. Variations in the pulley anatomy have been reported; however, the A2, A3, and A4 pulleys are relatively constant in their anatomic locations (2). A2 and A4 pulleys are most important biomechanically, since the compromise of one or both of them can lead to significant loss of power and “bowstringing” of the flexor tendon in relation to the bone (3).
Figure 3.
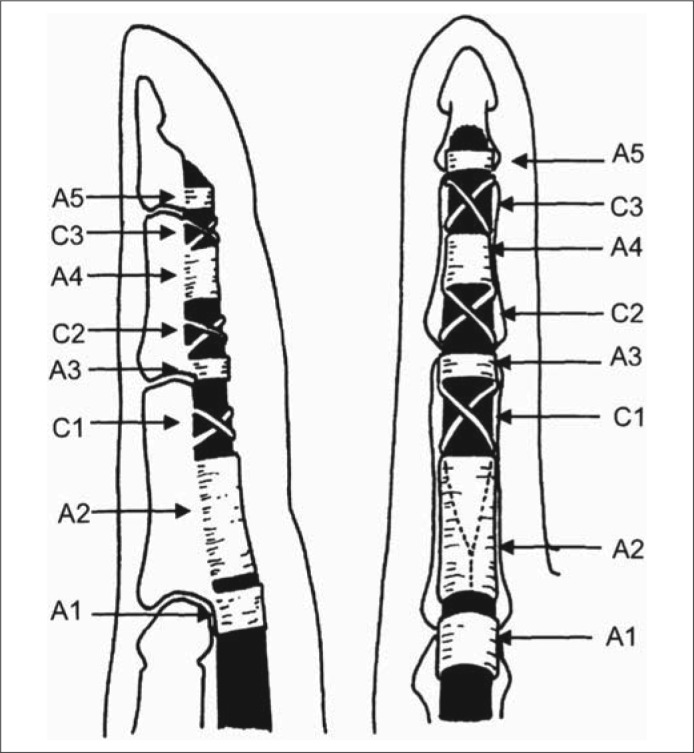
Sagittal (left) and coronal (right) depictions of the pulley system of a typical flexor tendon (black areas) of the finger: fibro-osseous annular pulleys (A2, A4), palmar plate annular pulleys (A1, A3, and A5), and cruciate pulleys (C1, C2, and C3). Reprinted from Hauger et al, 2000 (1) with permission of the Radiological Society of North America.
Bollen and Gunson first described injury to the pulley mechanism in 1990 after examining 67 rock climbers in Britain. Pulley rupture is relatively unique to the rock climbing population, mostly because of the stress involved. One of the two key positions in rock climbing is the crimp position. In this position, the distal interphalangeal joints are extended, the proximal interphalangeal joints are flexed, and the metacarpal joints are extended. The carpal bones are rotated, which puts increased stress on the ring finger, which along with the long finger is most often involved in injury. Imaging plays a crucial role in diagnosing injury to the pulley mechanism because the clinical exam is often limited by pain and soft tissue swelling of the involved finger (2, 4, 5). Evaluation of the injury by ultrasound, computed tomography (CT), and MRI has been described.
Klauser et al designed a study using 64 extreme rock climbers with finger injuries and evaluated the distance between the flexor digitorum profundus (FDP) tendon and the adjacent phalanx (TP distance) using ultrasound to indicate the presence of bowstringing. The symptomatic fingers with evidence of bowstringing on ultrasound were confirmed with MRI. The pulley thickness was <0.3 mm in nonruptured pulleys in asymptomatic fingers. Incomplete rupture, complete rupture (A2 or A4), or complete combined rupture (A2 and A3) demonstrated a TP distance of at least 0.9 mm. Ultrasound was 98% sensitive and 100% specific for depicting finger pulley injuries. One of the biggest drawbacks of ultrasound is interoperator variability (3, 5). However, its low cost and real-time imaging of anatomic structures make it an attractive option.
Similarly, Le Viet et al used CT scans performed at 1.5 mm slice thickness to image the involved fingers as well as the contralateral asymptomatic fingers. Imaging was performed in both passive and active/dynamic positioning. The dynamic images were found to be superior for diagnostic purposes. Although the sample size in the study was small (7 patients), the study successfully identified pulley injuries in all cases. They noted lack of adherence of the FDP tendon to the adjacent bone (bowstringing) in the symptomatic digits and an absence of bowstringing in the contralateral digits. Additionally, fibrous tissue was noted to be interposed between the phalanx and the FDP tendon. Several advantages of CT scans were noted over MRI, including lower cost with CT, better resolution (although this is debatable since MR technology has advanced since the original paper was published), and dynamic imaging (3, 6).
Finally, MRI has been regarded as the gold standard by several authors (3, 7). Haugher et al simulated pulley injuries on cadavers and compared MRI, ultrasound, and CT techniques by their ability to directly visualize partial and complete rupture of the pulleys and also their ability to detect the indirect sign of pulley system lesions. The indirect sign consisted of measuring the distance between the bone and the FDP tendon in extension, flexion, and forced flexion. They found MRI to be the most accurate in directly visualizing pulley abnormality, especially the A4 pulley, whereas CT was the least accurate in visualizing direct rupture of the pulleys. All three modalities were deemed similar in detecting an indirect sign of pulley injury. Additionally, MRI can help distinguish between tendonitis, peritendon inflammation, and partial ruptures (2). One of the major limitations with MRI is the motion artifact related to forced flexion. Use of dedicated surface receiver coils can reduce this motion and yield better imaging of the pulleys. MRI has also been used in determining adequate treatment of pulley lesions (7–9).
The therapeutic management of pulley injuries has not yet been clearly defined (3). Schoffl et al proposed a grading scheme for closed pulley injuries based on prospective evaluation of 604 climbers, and that has served as a therapeutic guideline. Grade I injuries consist of pulley strains with no increased dehiscence between the bone and FDP tendon. Grade II injuries consist of complete rupture of the A4 tendon or partial rupture of the A2 or A3 tendon. Grade III injuries consist of complete rupture of A2 or A3. Grade IV injuries consist of multiple ruptures (as A2/A3, A2/A3/A4) or single rupture (as A2 or A3) combined with lumbrical muscle or collateral ligament trauma. Schoffl et al treated the Grades I to III injuries conservatively with immobilization of the affected fingers with a splint for 2 weeks and then treatment consisting of early functional therapy with pulley protection. Grade IV injury was managed with surgical repair. The surgical technique proposed by Widstrom et al, which consists of free transplant of the palmaris longus tendon, was favored over other techniques (2, 7).
References
- 1.Hauger O, Chung CB, Lektrakul N, Botte MJ, Trudell D, Boutin RD, Resnick D. Pulley system in the fingers: normal anatomy and simulated lesions in cadavers at MR imaging, CT, and US with and without contrast material distention of the tendon sheath. Radiology. 2000;217(1):201–212. doi: 10.1148/radiology.217.1.r00oc40201. [DOI] [PubMed] [Google Scholar]
- 2.Schöffl VR, Schöffl I. Injuries to the finger flexor pulley system in rock climbers: current concepts. J Hand Surg Am. 2006;31(4):647–654. doi: 10.1016/j.jhsa.2006.02.011. [DOI] [PubMed] [Google Scholar]
- 3.Kubiak EN, Klugman JA, Bosco JA. Hand injuries in rock climbers. Bull NYU Hosp Jt Dis. 2006;64(3–4):172–177. [PubMed] [Google Scholar]
- 4.Bollen SR, Gunson CK. Hand injuries in competition climbers. Br J Sports Med. 1990;24(1):16–18. doi: 10.1136/bjsm.24.1.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Klauser A, Frauscher F, Bodner G, Halpern EJ, Schocke MF, Springer P, Gabl M, Judmaier W, zur Nedden D. Finger pulley injuries in extreme rock climbers: depiction with dynamic US. Radiology. 2002;222(3):755–761. doi: 10.1148/radiol.2223010752. [DOI] [PubMed] [Google Scholar]
- 6.Le Viet D, Rousselin B, Roulot E, Lantieri L, Godefroy D. Diagnosis of digital pulley rupture by computed tomography. J Hand Surg Am. 1996;21(2):245–248. doi: 10.1016/S0363-5023(96)80108-0. [DOI] [PubMed] [Google Scholar]
- 7.Schöffl V, Hochholzer T, Winkelmann HP, Strecker W. Pulley injuries in rock climbers. Wilderness Environ Med. 2003;14(2):94–100. doi: 10.1580/1080-6032(2003)014[0094:piirc]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 8.Clavero JA, Alomar X, Monill JM, Esplugas M, Golanó P, Mendoza M, Salvador A. MR imaging of ligament and tendon injuries of the fingers. Radiographics. 2002;22(2):237–256. doi: 10.1148/radiographics.22.2.g02mr11237. [DOI] [PubMed] [Google Scholar]
- 9.Gabl M, Rangger C, Lutz M, Fink C, Rudisch A, Pechlaner S. Disruption of the finger flexor pulley system in elite rock climbers. Am J Sports Med. 1998;26(5):651–655. doi: 10.1177/03635465980260050901. [DOI] [PubMed] [Google Scholar]