Executive Summary
In July 2009, the Medical Advisory Secretariat (MAS) began work on Non-Invasive Cardiac Imaging Technologies for the Diagnosis of Coronary Artery Disease (CAD), an evidence-based review of the literature surrounding different cardiac imaging modalities to ensure that appropriate technologies are accessed by patients suspected of having CAD. This project came about when the Health Services Branch at the Ministry of Health and Long-Term Care asked MAS to provide an evidentiary platform on effectiveness and cost-effectiveness of non-invasive cardiac imaging modalities.
After an initial review of the strategy and consultation with experts, MAS identified five key non-invasive cardiac imaging technologies for the diagnosis of CAD. Evidence-based analyses have been prepared for each of these five imaging modalities: cardiac magnetic resonance imaging, single photon emission computed tomography, 64-slice computed tomographic angiography, stress echocardiography, and stress echocardiography with contrast. For each technology, an economic analysis was also completed (where appropriate). A summary decision analytic model was then developed to encapsulate the data from each of these reports (available on the OHTAC and MAS website).
The Non-Invasive Cardiac Imaging Technologies for the Diagnosis of Coronary Artery Disease series is made up of the following reports, which can be publicly accessed at the MAS website at: www.health.gov.on.ca/mas or at www.health.gov.on.ca/english/providers/program/mas/mas_about.html
Single Photon Emission Computed Tomography for the Diagnosis of Coronary Artery Disease: An Evidence-Based Analysis
Stress Echocardiography for the Diagnosis of Coronary Artery Disease: An Evidence-Based Analysis
Stress Echocardiography with Contrast for the Diagnosis of Coronary Artery Disease: An Evidence-Based Analysis
64-Slice Computed Tomographic Angiography for the Diagnosis of Coronary Artery Disease: An Evidence-Based Analysis
Cardiac Magnetic Resonance Imaging for the Diagnosis of Coronary Artery Disease: An Evidence-Based Analysis
Pease note that two related evidence-based analyses of non-invasive cardiac imaging technologies for the assessment of myocardial viability are also available on the MAS website:
Positron Emission Tomography for the Assessment of Myocardial Viability: An Evidence-Based Analysis
Magnetic Resonance Imaging for the Assessment of Myocardial Viability: an Evidence-Based Analysis
The Toronto Health Economics and Technology Assessment Collaborative has also produced an associated economic report entitled:
The Relative Cost-effectiveness of Five Non-invasive Cardiac Imaging Technologies for Diagnosing Coronary Artery Disease in Ontario [Internet]. Available from: http://theta.utoronto.ca/reports/?id=7
Objective
The objective of the analysis is to determine the diagnostic accuracy of single photon emission tomography (SPECT) in the diagnosis of coronary artery disease (CAD) compared to the reference standard of coronary angiography (CA). The analysis is primarily meant to allow for indirect comparisons between non-invasive strategies for the diagnosis of CAD, using CA as a reference standard.
SPECT
Cardiac SPECT, or myocardial perfusion scintigraphy (MPS), is a widely used nuclear, non-invasive image acquisition technique for investigating ischemic heart disease. SPECT is currently appropriate for all aspects of detecting and managing ischemic heart disease including diagnosis, risk assessment/stratification, assessment of myocardial viability, and the evaluation of left ventricular function. Myocardial perfusion scintigraphy was originally developed as a two-dimensional planar imaging technique, but SPECT acquisition has since become the clinical standard in current practice. Cardiac SPECT for the diagnosis of CAD uses an intravenously administered radiopharmaceutical tracer to evaluate regional coronary blood flow usually at rest and after stress. The radioactive tracers thallium (201Tl) or technetium-99m (99mTc), or both, may be used to visualize the SPECT acquisition. Exercise or a pharmacologic agent is used to achieve stress. After the administration of the tracer, its distribution within the myocardium (which is dependent on myocardial blood flow) is imaged using a gamma camera. In SPECT imaging, the gamma camera rotates around the patients for 10 to 20 minutes so that multiple two-dimensional projections are acquired from various angles. The raw data are then processed using computational algorithms to obtain three-dimensional tomographic images.
Since its inception, SPECT has evolved and its techniques/applications have become increasingly more complex and numerous. Accordingly, new techniques such as attenuation correction and ECG gating have been developed to correct for attenuation due to motion or soft-tissue artifact and to improve overall image clarity.
Research Questions
What is the diagnostic accuracy of SPECT for the diagnosis of CAD compared to the reference standard of CA?
Is SPECT cost-effective compared to other non-invasive cardiac imaging modalities for the diagnosis of CAD?
What are the major safety concerns with SPECT when used for the diagnosis of CAD?
Methods
A preliminary literature search was performed across OVID MEDLINE, MEDLINE In-Process and Other Non-Indexed Citations, EMBASE, the Cochrane Library, and the International Agency for Health Technology Assessment (INAHTA) for all systematic reviews/meta-analysis published between January 1, 2004 and August 22, 2009. A comprehensive systematic review was identified from this search and used as a basis for an updated search.
A second comprehensive literature search was then performed on October 30, 2009 across the same databases for studies published between January 1, 2002 and October 30, 2009. Abstracts were reviewed by a single reviewer and, for those studies meeting the eligibility criteria, full-text articles were obtained. Reference lists were also hand-searched for any additional studies.
| Inclusion Criteria | Exclusion Criteria |
|---|---|
|
|
Summary of Findings
Eighty-four observational studies, one non-randomized, single arm controlled clinical trial, and one poorly reported trial that appeared to be a randomized controlled trial (RCT) met the inclusion criteria for this review. All studies assessed the diagnostic accuracy of myocardial perfusion SPECT for the diagnosis of CAD using CA as a reference standard. Based on the results of these studies the following conclusions were made:
According to very low quality evidence, the addition of attenuation correction to traditional or ECG-gated SPECT greatly improves the specificity of SPECT for the diagnosis of CAD although this improvement is not statistically significant. A trend towards improvement of specificity was also observed with the addition of ECG gating to traditional SPECT.
According to very low quality evidence, neither the choice of stress agent (exercise or pharmacologic) nor the choice of radioactive tracer (technetium vs. thallium) significantly affect the diagnostic accuracy of SPECT for the diagnosis of CAD although a trend towards accuracy improvement was observed with the use of pharmacologic stress over exercise stress and technetium over thallium.
Considerably heterogeneity was observed both within and between trials. This heterogeneity may explain why some of the differences observed between accuracy estimates for various subgroups were not statistically significant.
More complex analytic techniques such as meta-regression may help to better understand which study characteristics significantly influence the diagnostic accuracy of SPECT.
Background
In July 2009, the Medical Advisory Secretariat (MAS) began work on Non-Invasive Cardiac Imaging Technologies for the Diagnosis of Coronary Artery Disease (CAD), an evidence-based review of the literature surrounding different cardiac imaging modalities to ensure that appropriate technologies are accessed by patients suspected of having CAD. This project came about when the Health Services Branch at the Ministry of Health and Long-Term Care asked MAS to provide an evidentiary platform on effectiveness and cost-effectiveness of non-invasive cardiac imaging modalities.
After an initial review of the strategy and consultation with experts, MAS identified five key non-invasive cardiac imaging technologies for the diagnosis of CAD. Evidence-based analyses have been prepared for each of these five imaging modalities: cardiac magnetic resonance imaging, single photon emission computed tomography, 64-slice computed tomographic angiography, stress echocardiography, and stress echocardiography with contrast. For each technology, an economic analysis was also completed (where appropriate). A summary decision analytic model was then developed to encapsulate the data from each of these reports (available on the OHTAC and MAS website).
The Non-Invasive Cardiac Imaging Technologies for the Diagnosis of Coronary Artery Disease series is made up of the following reports, which can be publicly accessed at the MAS website at: www.health.gov.on.ca/mas or at www.health.gov.on.ca/english/providers/program/mas/mas_about.html
Single Photon Emission Computed Tomography for the Diagnosis of Coronary Artery Disease: An Evidence-Based Analysis
Stress Echocardiography for the Diagnosis of Coronary Artery Disease: An Evidence-Based Analysis
Stress Echocardiography with Contrast for the Diagnosis of Coronary Artery Disease: An Evidence-Based Analysis
64-Slice Computed Tomographic Angiography for the Diagnosis of Coronary Artery Disease: An Evidence-Based Analysis
Cardiac Magnetic Resonance Imaging for the Diagnosis of Coronary Artery Disease: An Evidence-Based Analysis
Pease note that two related evidence-based analyses of non-invasive cardiac imaging technologies for the assessment of myocardial viability are also available on the MAS website:
Positron Emission Tomography for the Assessment of Myocardial Viability: An Evidence-Based Analysis
Magnetic Resonance Imaging for the Assessment of Myocardial Viability: an Evidence-Based Analysis
The Toronto Health Economics and Technology Assessment Collaborative has also produced an associated economic report entitled:
The Relative Cost-effectiveness of Five Non-invasive Cardiac Imaging Technologies for Diagnosing Coronary Artery Disease in Ontario [Internet]. Available from: http://theta.utoronto.ca/reports/?id=7
SPECT
Cardiac SPECT, or myocardial perfusion scintigraphy, is a widely used nuclear, non-invasive image acquisition technique for investigating ischemic heart disease. According to the American College of Cardiology Foundation (ACCF) Appropriate Use Criteria Task Force, SPECT is deemed useful for all aspects of detecting and managing ischemic heart disease including diagnosis, risk assessment/stratification, assessment of myocardial viability and evaluation of left ventricular function. (1) Myocardial perfusion scintigraphy was originally developed as a planar imaging technique, but SPECT has since become the clinical standard in current practice. (2)
Cardiac SPECT for the diagnosis of CAD uses an intravenously administered radiopharmaceutical tracer to evaluate regional coronary blood flow, usually at rest and after stress. After the administration of the tracer, its distribution within the myocardium is imaged using a gamma camera. In SPECT imaging, the gamma camera rotates around the patients for 10 to 20 minutes so that multiple two-dimensional projections are acquired from various angles. The raw data are then processed using computational algorithms to obtain three-dimensional tomographic images. (2)
Perfusion Imaging
For the diagnosis of CAD, SPECT images are taken at stress and at rest (or re-injection) and the resulting images compared. Generally, a patient absent significant infarction or coronary stenosis will show homogenous uptake of the tracer throughout the myocardium. A defect in the ‘tress images’ that is absent or normalized in the ‘rest images’ usually corresponds to a significant coronary stensosis (3); however, the exact interpretation and criteria used to denote CAD positivity will vary according to the SPECT protocol and tracer used. (4)
The total patient contact time for stress induction, injection and image acquisition is approximately one hour. Stress and rest image acquisitions are normally separated by three to four hours, although rest acquisitions may occur on subsequent days depending on the protocol being used. (3)
Exercise and/or pharmacological agents are used to induce stress for all perfusion studies. When patients can exercise to an appropriate level of cardiovascular stress, stress induction via a conventional treadmill or stationary bicycle is preferred to pharmacologic stress. Pharmacological stress testing is particularly useful in patients who cannot exercise, in which case a pharmacologic agent, such as the positive inotrope, dobutamine; or the vasodilators, adenosine and dipyridamole, are used to induce cardiovascular stress. (2)
Radioactive Tracers
Two radioactive tracers are licensed for use by Health Canada and available commercially for use in myocardial perfusion SPECT in Ontario: thallium (201Tl) and two classes of technetium (99mTc): sestamibi (MIBI) and tetrofosmin. Briefly, thallium is a potassium analogue with a long half life of 73 hours. It emits photons with a low energy of about 80 keV. Technetium analogues, on the other hand, have a half life of only six hours but emit photons with a higher energy, in the range of 140 keV. Because of its higher energy, technetium is less subject to attenuation than thallium, and generally leads to better quality images. (4) Technetium analogues have thus become the isotope of choice for the majority of cardiac SPECT tests. A major disruption in the supply of technetium has, however, threatened supplies in Ontario and worldwide.
On May 14, 2009, the National Research Universal (NRU) reactor at Chalk River was shut down as a result of loss of electrical power in eastern Ontario and western Quebec. The facility produces nearly 50% of the world’s molybdenum-99 (Mo-99), a precursor to technetium-99m. During a follow-up inspection, a heavy water leak was detected. The rate of this leak has been slowed and all material has been contained. (5) However, as of December 23, 2009, only 11% of the planned repairs had been completed. A return-to-service date of March 31, 2010 has been targeted by the NRU. (6) The U.S. and Canadian medical communities are most affected by the disruption in molybdenum-99 supply. In lieu of this shortage, the Ontario Ministry of Health and Long-Term Care has issued guidelines for the prioritization of procedures employing technetium. (7)
Attenuation Correction and ECG Gating
A particular problem with SPECT is that of attenuation. Soft-tissue in the breasts, abdomen, and chest wall can degrade SPECT image quality or create artifacts that mimic true perfusion abnormalities thus posing particular problems in obese individuals. The movement of the beating heart may also give way to motion artifacts, impeding image clarity or interpretation. (2) Since the early 1990s, several techniques have been developed to overcome these challenges. These techniques are commonly referred to as attenuation correction (AC) and electrocardiogram (ECG) gating. (8) Both techniques have been shown to improve diagnostic accuracy over traditional SPECT and are even recommended in combination by the American Society of Nuclear Cardiology (ASNC) and the Society of Nuclear Medicine (SNM). (9)
Today, AC has become a catchall phrase to refer to compensation for all phenomena that may affect image acquisition/interpretation. At the very least, this requires measuring errant photon absorption via a transmission scan that employs an external radiation source, such as gadolinium or x-ray (to correct for soft tissue attenuation), as well as correction for Compton scatter and correction for resolution degradation. (10;11)
In ECG-gated SPECT, an ECG guides the SPECT acquisition so the resulting set of images are aggregated and displayed as a continuous cinematic loop resembling a beating heart. By minimizing artifacts caused by cardiac motion, ECG gating generates a clearer image. Gating also provides additional functional information (e.g., wall motion information). (2)
Regulatory Status
SPECT gamma cameras and associated equipment/software are currently licensed by Health Canada as Class II devices.
Evidence-Based Analysis
Objective
The objective of the analysis is to determine the diagnostic accuracy of SPECT in the diagnosis of CAD compared to the reference standard of CA. This analysis is meant to allow for both indirect and direct comparisons with other non-invasive strategies for the diagnosis of CAD, using CA as a reference.
Research Questions
What is the diagnostic accuracy of SPECT for the diagnosis of CAD compared to the reference standard of CA?
Is SPECT cost-effective compared to other non-invasive cardiac imaging modalities for the diagnosis of CAD?
What are the adverse events/safety concerns with SPECT when used for the diagnosis of CAD?
Methods
Literature search
A preliminary literature search was performed across OVID MEDLINE, MEDLINE In-Process and Other Non-Indexed Citations, EMBASE, the Cochrane Library, and the International Agency for Health Technology Assessment (INAHTA) for all systematic reviews/meta-analysis published between January 1, 2004 and August 22, 2009. If identified, any comprehensive systematic-review/meta-analysis would form the basis for an updated search. The preliminary scan identified a comprehensive systematic review of meta-analyses with search dates no sooner than January 1, 2002 (see Literate Search Results below)).
Due to the vast amount of literature on cardiac SPECT, a decision was made to update the literature base of the MAS review starting from January 1, 2002. A second comprehensive literature search was thus performed on October 30, 2009 across the same databases for studies published between January 1, 2002 and October 30, 2009. Abstracts were reviewed by a single reviewer and, for those studies meeting the eligibility criteria, full-text articles were obtained. Reference lists were also hand-searched for any relevant studies not identified through the electronic search (see Appendix 1 for the full search strategy).
| Inclusion Criteria | Exclusion Criteria |
|---|---|
|
|
Outcomes of Interest
TP, FP, FN, TN, sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), positive likelihood ratio (+LR), negative likelihood ratio (-LR), and diagnostic accuracy
Adverse events
Costs
SPECT Techniques
All modern SPECT techniques were investigated:
Attenuation correction SPECT with or without ECG gating (termed “AC SPECT”)
ECG-gated SPECT without AC (termed “gated SPECT”)
SPECT without AC and without ECG gating (termed “traditional SPECT”)
Subgroup Analyses
All subgroup analyses were decided a priori. Multiple univariate analyses were planned for the following subgroups:
Primary analyses:
by SPECT technique (e.g., traditional vs. AC vs. ECG-gated)
by isotope (e.g., thallium vs. technetium vs. dual isotop)
by stress agent [e.g., exercise vs. pharmacologic (any agent) vs. adenosine vs. dobutamine vs. dipyridamole]
Secondary analyses:
by angiographic definition of CAD (≥50% vs. ≥70% stenosis)
by method of SPECT interpretation (qualitative vs. quantitative)
by history of MI (previous MI vs. no previous MI)
Subgroups containing few trials were excluded from subgroup analyses.
Calculations & Statistical Analysis
As indicated in the inclusion/exclusion criteria above, only trials which included enough raw data to derive numbers of TP, FP, FN and TN were included (to allow for meta-analysis of sensitivities and specificities). Wherever possible, accuracy data were calculated to reflect “any CAD” meaning that data reported by disease location (e.g., CAD in the LAD, RCX or circumflex) or by the number of arteries involved (e.g., single vs. multi-vessel CAD) were collapsed if possible to reflect an estimate of “any CAD.” All accuracy estimates reported are by patient, not by segment.
Some trials may have reported multiple sets of accuracy data for the same patient group according to stratified variables. In such cases, only one set of values was chosen for inclusion into meta-analysis to avoid artificially over-inflating sample sizes. An attempt was made to choose a set of values most consistent with current Ontario clinical practice/expectations using advice from an expert panel. Such an approach was taken in part because a meta-regression was not possible due to time and resource constraints.
Due to the nature of patient accrual in cardiac SPECT diagnostic trials, large differences in sample sizes were observed between the sample enrolled and the sample that was actually analyzed. As a result, descriptive variables of Mean Age and % Men were presented for only those trials which provided these data according to the population analyzed for diagnostic accuracy (i.e., in those patients who completed CA).
Pooled estimates of sensitivity, specificity and diagnostic odds ratios (DORs) were calculated using a bivariate, binomial generalized linear mixed model. (12) Statistical significance was defined by P-values less than 0.05, where false discovery rate adjustments were made for multiple hypothesis testing. (13) The bivariate regression analyses were performed using SAS version 9.2 (SAS Institute Inc.; Cary, NC, USA). Summary receiver operating characteristic (sROC) curves weighted by inverse variance were produced using Review Manager 5.0.22 (The Nordiac Cochrane Centre, The Cochrane Collaboration, 2008) and the curves were adjusted by bivariate model parameters. All other statistics were calculated using STATA version 10.1 (StataCorp; Texas, USA).
Unless otherwise stated, all univariate tests were carried out as indirect comparisons, meaning that pooled estimates were formed by combining single patient arms from all available studies. Comparisons stated as “direct” involved summarizing data only from studies which directly compared the subgroups in question within the same trial, using CA as a reference standard. Indirect comparisons were used in order to facilitate comparisons between technologies, particularly to overcome absences in direct comparative data.
Quality of Evidence
The quality of the body of evidence was assessed as high, moderate, low, or very low according to the GRADE Working Group criteria (14) as presented below:
Quality refers to the criteria such as the adequacy of allocation concealment, blinding and follow-up.
Consistency refers to the similarity of estimates of effect across studies. If there are important and unexplained inconsistencies in the results, our confidence in the estimate of effect for that outcome decreases. Differences in the direction of effect, the magnitude of the difference in effect, and the significance of the differences guide the decision about whether important inconsistency exists.
Directness refers to the extent to which the interventions and outcome measures are similar to those of interest.
As stated by the GRADE Working Group, the following definitions of quality were used in grading the quality of the evidence:
| High | Further research is very unlikely to change confidence in the estimate of effect. |
| Moderate | Further research is likely to have an important impact on confidence in the estimate of effect and may change the estimate. |
| Low | Further research is very likely to have an important impact on confidence in the estimate of effect and is likely to change the estimate. |
| Very Low | Any estimate of effect is very uncertain |
Results of Evidence-Based Analysis
Literature Search Results
The preliminary search yielded 624 articles published from January 1, 2004 to August 22, 2009, including a recent, comprehensive systematic review. Published by Heijenbrok-Kal et al. (15), the review compared the diagnostic performance of stress ECHO, SPECT and electron beam computed tomography (EBCT) for CAD using CA as the reference standard. The authors performed a meta-analysis of 351 patient-series including 35,258 patients reported across 11 meta-analyses. Given the vast amount of published literature on cardiac SPECT, it was decided that the studies contained in the Heijenbrok-Kal et al. review would be used as the basis for the MAS evidence-based analysis. Of the 11 meta-analyses it covered, five meta-analyses contained information on 103 studies on SPECT compared to CA for the diagnosis of CAD (see Table 1).
Table 1: Characteristics of meta-analyses included in systematic review by Heijenbrok-Kal, 2007*.
| Study | Search Dates | Type of Stress | No of Studies (Patients) | CAD | Pooled Sensitivity | Pooled Specificity | Other Technologies Evaluated |
|---|---|---|---|---|---|---|---|
| O’Keefe et al., 1995 (16) | Database inception until Dec. 1993 | Ex SPECT Ad SPECT |
12 (2549) 8 (925) |
73% 80% |
90% 89% |
72% 83% |
Ex echo, Dob echo |
| Fleischmann et al., 1998 (17) | Jan 1990 – Oct 1997 | Ex SPECT | 27 (3237) | 78% | 87% | 64% | Ex echo |
| Kim et al., 2001 (18) | Jan 1997 – June 1999 | Ad SPECT Dip SPECT Dob SPECT |
9 (1207) 21 (1464) 14 (1066) |
80% 71% 66% |
90% 89% 82% |
75% 65% 75% |
Ad echo, Dip echo, Dob echo |
| Imran et al., 2003 (19) | Jan 1986 – March 2001 | Mix SPECT | 13 (2922) | 71% | 81% | 65% | Dip echo |
| Mowatt et al., 2004 (2) | Jan 1981 – Dec 2001 | Mix SPECT | 13 (2922) | 71% | 81% | 65% | Ex ECG |
Abbreviations: Ad, adenosine; CAD, coronary artery disease; Dip, dipyridamole; Dob, dobutamine; ECG, electrocardiogram; ECHO, echocardiography; Ex, Exercise; Mix, combination of stressors; NR, not reported.
Table adapted from Heijenbrok-Kal et al. (15)
To further refine the data obtained from the review by Heijenbrok-Kal et al. (15), additional inclusion/exclusion criteria, as outlined in the Methods section above, were applied. Applying these additional criteria yielded 36 observational studies published between January 1, 1995 and December 31, 2001. (20-55)
As indicated in the Methods section above, an updated search was conducted using the most recent search dates from the review by Heijenbrok-Kal et al. (15) The updated secondary search yielded 3,555 articles published from January 1, 2002 to October 30, 2009. Of these, 50 met the inclusion criteria for this review. (56-105) The total number of studies included for review was therefore 86, comprising a total of 10,870 analyzed patients.
Trial Characteristics
All included trials were published between January 1, 1995 and October 30, 2009 and were either prospective or retrospective observational studies except for one non-randomized, single arm clinical trial (59) and one poorly reported trial that appears to be a randomized controlled trial (RCT) (Table 2). (51)
Table 2: Quality of evidence of included studies.
| Study Design | Level of Evidence† | Number of Eligible Studies |
|---|---|---|
| Large RCT, systematic review of RCTs | 1 | |
| Large RCT unpublished but reported to an international scientific meeting | 1(g) | |
| Small RCT | 2 | 1 |
| Small RCT unpublished but reported to an international scientific meeting | 2(g) | |
| Non-RCT with contemporaneous controls | 3a | 85 |
| Non-RCT with historical controls | 3b | |
| Non-RCT presented at international conference | 3(g) | |
| Surveillance (database or register) | 4a | |
| Case series (multisite) | 4b | |
| Case series (single site) | 4c | |
| Retrospective review, modelling | 4d | |
| Case series presented at international conference | 4(g) | |
| Total | 86 |
RCT refers to randomized controlled trial
Table adapted from Goodman, 1996 (106)
Across all studies, the majority of patients were male (64.7% overall, n=56 studies) and the mean age was 60.8 (n=56 studies). The mean prevalence of CAD was 65.9% (n=84 studies) with a range of 19.6% to 94.3%. Appendix 2 contains detailed information on study characteristics and results at the individual trial level.
Diagnostic Accuracy of SPECT
Pooled estimates of sensitivity, specificity and DOR varied across trials (Appendix 2) and subgroups (see Table 3). Despite large differences in pooled accuracy estimates, however, no significant differences were observed between subgroups when the subgroups were submitted to significance testing (Table 4). This phenomenon is likely attributable to the high heterogeneity within and between studies, as well as the indirect nature of the comparisons themselves.
Table 3: Pooled accuracy estimates of included trials stratified by study characteristic.
| Characteristic | # Trials (Patients) | Pooled Sensitivity (95% CI) | Pooled Specificity (95% CI) | DOR (95% CI) |
|---|---|---|---|---|
| SPECT Modality (n=86) | ||||
| Traditional Gated AC |
63 (7,186) 19 (2,710) 12 (1,238) |
0.87 (0.85–0.89) 0.84 (0.79–0.89) 0.87 (0.82–0.92) |
0.70 (0.66–0.75) 0.78 (0.72–0.85) 0.81 (0.73–0.89) |
15.48 (11.43–19.54) 18.88 (10.22–27.53) 27.01 (10.73–43.30) |
| Tracer (n=63)* | ||||
| Technetium Thallium |
39 (3,488) 24 (3,338) |
0.88 (0.85–0.91) 0.84 (0.80–0.88) |
0.70 (0.64–0.76) 0.71 (0.64–0.78) |
16.80 (10.88–22.71) 12.88 (7.58–18.18) |
| Stress agent (n=63)* | ||||
| Pharmacologic (any) Dobutamine alone Adenosine alone Dipyridamole alone Exercise |
33 (3,129) 11 (671) 6 (643) 15 (1,336) 20 (2,688) |
0.86 (0.82–0.89) 0.83 (0.76–0.90) 0.88 (0.81–0.95) 0.88 (0.83–0.92) 0.86 (0.82–0.90) |
0.76 (0.70–0.82) 0.81 (0.73–0.90) 0.84 (0.75–0.94) 0.74 (0.65–0.83) 0.68 (0.59–0.76) |
18.81 (11.72–25.90) 20.79 (7.52–34.06) 41.01 (5.54–76.48) 20.87 (8.93–32.80) 13.26 (6.98–19.55) |
| Method of Interpretation (n=63)* | ||||
| Qualitative Quantitative |
50 (4,730) 7 (813) |
0.88 (0.86–0.90) 0.86 (0.79–0.93) |
0.70 (0.64–0.75) 0.73 (0.60–0.85) |
16.72 (11.84–21.60) 15.81 (4.04–27.59) |
| % Stenosis (n=63)* | ||||
| ≥50 ≥70 |
51 (5,403) 12 (1,415) |
0.87 (0.84–0.89) 0.88 (0.84–0.93) |
0.72 (0.67–0.77) 0.66 (0.55–0.76) |
16.73 (11.92–21.54) 14.66 (6.28–23.05) |
| Previous MI (n=63)* | ||||
| Yes No |
37 (4,074) 23 (1,928) |
0.86 (0.83–0.89) 0.89 (0.86–0.93) |
0.69 (0.63–0.75) 0.75 (0.69–0.82) |
13.39 (8.95–17.83) 25.37 (14.29–36.45) |
Abbreviations: AC, attenuation correction; CI, confidence interval; DOR, diagnostic odds ratio; Ex., exercise; MI, myocardial infarction; Pharma., pharamcologic (any)
For traditional SPECT studies only (subgroups by tracer, stress agent, method of interpretation, % stenosis and previous MI were not investigated for AC or gated SPECT due to the small number of trials).
Note that a trial may appear more than once as a result of multiple subgroup analysis on the same patient population.
Table 4: Tests of significance between SPECT subgroups.
| Subgroup | Unadjusted P-Value Sensitivity | Adjusted P-Value Sensitivity | Unadjusted P-Value Specificity | Adjusted P-Value Specificity | Unadjusted P-Value DOR | Adjusted P-Value DOR |
|---|---|---|---|---|---|---|
| SPECT Modality (n=84) | ||||||
| Gated vs. Traditional | 0.3203 | 0.7687 | 0.0378 | 0.1512 | 0.4245 | 0.5660 |
| AC vs. Traditional | 0.9750 | 0.9750 | 0.0194 | 0.1164 | 0.0809 | 0.3236 |
| AC vs. Gated | 0.4732 | 0.9054 | 0.6311 | 0.7535 | 0.3362 | 0.5043 |
| AC vs. Non AC (Direct) | 0.7089 | 0.9452 | 0.0058 | 0.0696 | 0.0460 | 0.2760 |
| Tracer (n=63)* | ||||||
| Technetium vs. Thallium | 0.1614 | 0.7596 | 0.8263 | 0.8263 | 0.3253 | 0.5043 |
| Stress agent (n=63)* | ||||||
| Pharmacologic (any) vs. Exercise | 0.8200 | 0.9750 | 0.1063 | 0.3156 | 0.2338 | 0.4676 |
| Adenosine vs. Dobutamine | 0.2532 | 0.7596 | 0.6402 | 0.7535 | 0.2162 | 0.4676 |
| Dipyridamole vs. Dobutamine | 0.2276 | 0.7596 | 0.2471 | 0.4236 | 0.9963 | 0.9963 |
| Adenosine vs. Dipyridamole | 0.9040 | 0.9750 | 0.1315 | 0.3156 | 0.2010 | 0.4676 |
| Method of Interpretation (n=63)* | ||||||
| Qualitative vs. Quantitative | 0.5804 | 0.9054 | 0.6907 | 0.7535 | 0.8958 | 0.9772 |
| % Stenosis (n=63)* | ||||||
| ≥50 vs. ≥70 | 0.6036 | 0.9054 | 0.3168 | 0.4752 | 0.6827 | 0.8192 |
| Previous MI (n=63)* | ||||||
| No vs. Yes | 0.1390 | 0.7596 | 0.1589 | 0.3178 | 0.0224 | 0.2688 |
Abbreviations: AC, attenuation correction; DOR, diagnostic odds ratio; MI, myocardial infarction.
Bolding denotes significance difference at a P-value<0.05 in favour of the first listed technology.
Accuracy of SPECT by technique
Of the three SPECT techniques, AC SPECT showed highest pooled sensitivity (87%; range: 73% to 94%) and specificity (81%; range: 57% to 94%). ECG-gated SPECT had a pooled sensitivity of 84% (range: 51% to 97%) and a pooled specificity of 78% (range: 29% to 100%) while traditional SPECT without ECG gating or AC had a pooled sensitivity of 87% (range: 49% to 100%) and the lowest pooled specificity of 70% (range: 29% to 100%).
Figure 1 illustrates SROCs for all included studies stratified by SPECT technique (Forest plots are provided in Appendix 3). As can be seen in the Forest plots in Appendix 3, AC SPET had the narrowest range in both sensitivity and specificity.
Figure 1: SROC comparing SPECT by technique using the bivariate model paramaters.
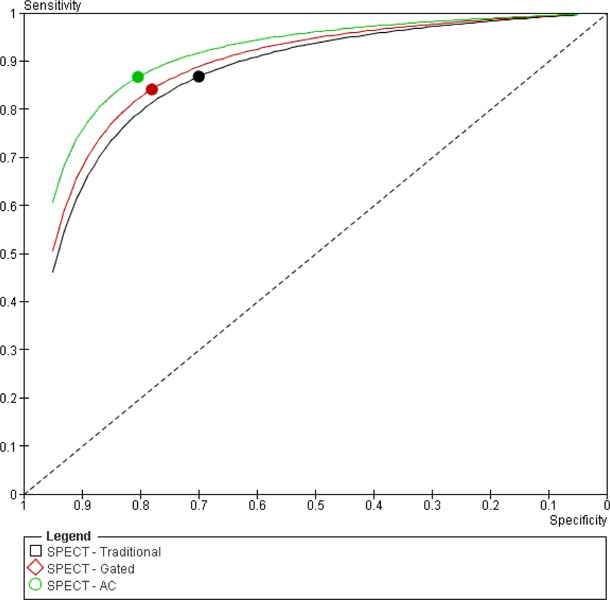
Despite the seemingly large differences observed in pooled estimates of specificity between SPECT techniques, there were no statistically significant differences observed in any of the accuracy estimates when comparing SPECT techniques (Table 2), although, for the comparison of AC versus traditional SPECT, the improvement in specificity with AC bordered significance (adjusted P-value of 0.1164; unadjusted P-value of 0.0194).
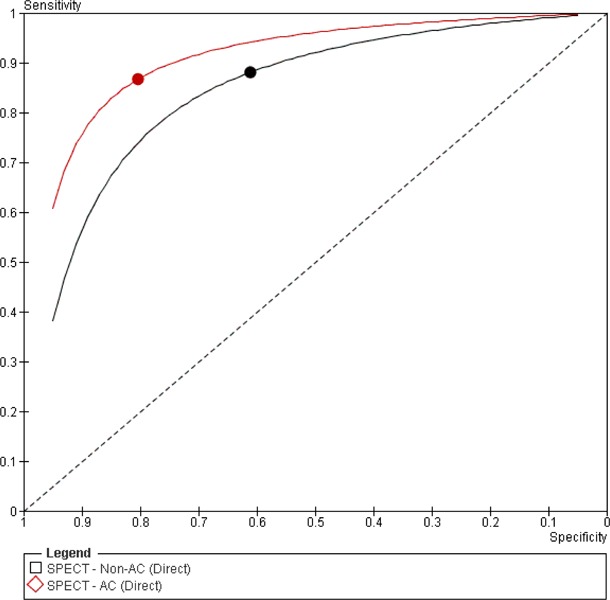
Studies that compared both SPECT with AC to SPECT without AC (non-AC SPECT) within the same trial (i.e., direct comparison), using CA as a reference standard, mirrored the results of the indirect analyses above. SPECT with AC showed a pooled sensitivity and specificity of 87% and 81%, respectively. Meanwhile, SPECT without AC had a pooled sensitivity of 88% and specificity 61%.
Figure 2 illustrates the direct comparison of AC and non-AC (Forest plots are provided in Appendix 3).
Figure 2: SROC of studies directly comparing AC and Non-AC SPECT.
Accuracy of SPECT by stress agent
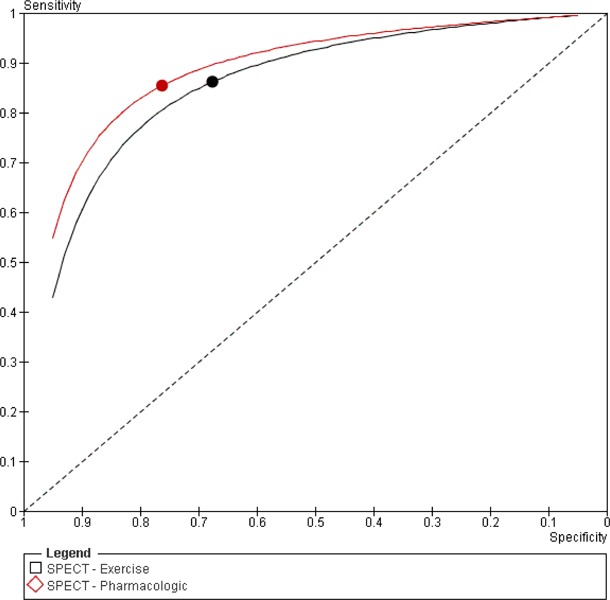
The use of a pharmacologic stress agent seemed to slightly improve accuracy over the use of exercise stress (Table 3) although the observed differences were not significant (Table 4). The pooled sensitivity of studies using pharmacologic stress alone was 86% (range: 49% to 98%) while the pooled specificity was 76% (range: 28% to 100%). Studies using exercise stress alone yielded a pooled sensitivity of 86% (range: 56% to 100%) and specificity of 68% (range: 36% to 100%).
Figure 3 illustrates the SROC for the comparison by stress agent (the associated Forest plots are provided in Appendix 3).
Figure 3: SROC comparing SPECT by stress agent using the bivariate model parameters.
Accuracy of SPECT by radioactive tracer
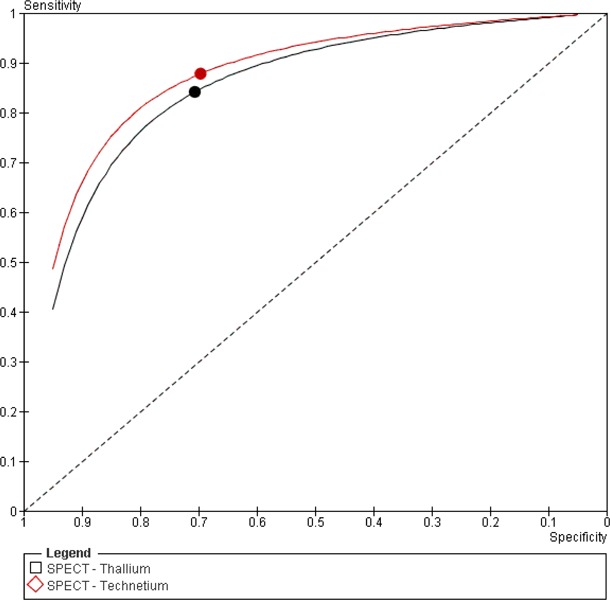
The radioactive tracer used during SPECT analysis also had minimal effect on accuracy estimates (Table 3). Studies using technetium had a pooled sensitivity of 88% (range: 49% to 98%) and specificity 70% (range: 30% to 100%) while studies using thallium had a pooled sensitivity of 84% (range: 56% to 100%) and specificity 71% (range: 44% to 94%). The differences in accuracy estimates between thallium and technetium were not significant (see Table 4).
Figure 4 illustrates the SROC for the comparison by radioactive tracer (the associated Forest plots are provided in Appendix 3)
Figure 4: SROC comparing SPECT by radioactive tracer using the bivariate model parameters.
Accuracy of traditional SPECT compared to stress echocardiography
Fourteen studies directly compared traditional SPECT without AC or ECG gating to stress echocardiography within the same trial (i.e., direct comparison), using CA as a reference standard. Meta-analysis of direct data mirrored the indirect data (see Table 5). No trials were identified that compared ECG-gated or AC SPECT to stress echocardiography.
Table 5: Diagnostic GRADE evaluation of methodological quality of included trials.
| Stress ECHO | SPECT | |||
|---|---|---|---|---|
| Indirect | Direct | Indirect | Direct | |
| Pooled Sensitivity (95% C.I.) | 0.80 (0.77–0.82) | 0.78 (0.72–0.84) | 0.86 (0.84–0.89) | 0.89 (0.85 – 0.93) |
| Pooled Specificity (95% C.I.) | 0.84 (0.82–0.87) | 0.88 (0.83–0.94) | 0.71 (0.67–0.76) | 0.70 (0.59–0.80) |
Abbreviations: CI, confidence interval; ECHO, echocardiography; SPECT, single photon emission computed tomography.
Study Quality
Overall quality of included studies (regardless of subgrouping) was very low according to GRADE criteria (Table 6). Reasons for the downgrading are discussed in the Limitations section below.
Table 6: Diagnostic GRADE evaluation of methodological quality of included trials.
| Factor | Explanation | GRADE |
|---|---|---|
| Risk of Bias | ||
| Study design | Observational / non-randomized clinical trials | High |
| Limitations | Verificiation/referall bias, lack of proper blinding and generally, poor reporting | Reduced by one level → Moderate |
| Indirectness | ||
| Outcomes | Accuracy estimates of sensitivity and specificity serve as indirect patient-important outcomes | Reduced by one level → Low |
| Patient populations, diagnostic test, comparison test, and indirect comparisons | Patient populations under study were mixed with respect to CAD status (trials included both patients with suspected CAD and known CAD) | Reduced by one level → Very Low |
| Prevalence of CAD was likely higher in the populations studied than in the population who would seek testing in a real-world setting | ||
| Technologies/SPECT strategies were indirectly compared using a gold standard and were not generally compared directly in head-to-head trials due to a lack of direct trials | ||
| Important inconsistency in study results | Large heterogeneity in accuracy estimates between studies | Unchanged |
| Imprecise evidence | Due to large number of trials, precision was acceptable | Unchanged |
| Publication bias | None detected | Unchanged |
| Quality of Evidence | Very Low | |
Abbreviations: CAD, coronary artery disease; SPECT, single photon emission computed tomography.
Adverse Events
One of the principal concerns with nuclear/X-ray technologies is the issue of radiation dose. What is termed the ‘effective dose’ is a useful method of comparing risk among different diagnostic tests as it takes into account the risk of absorbed dose to different organs. Currently, the radiation total effective dose of SPECT or CT varies from three to nine times that of the U.S. background effective dose of 3.0 millisieverts (mSv). (107) The U.S. Food and Drug Administration (FDA) has estimated that a technology that exposes a patient to an effective dose of 10 mSv may be associated with an increase in the possibility of fatal cancer at approximately 1 chance in 2000. This probability is in addition to the natural incidence of fatal cancer of 1 chance in 5 in the U.S. (108)
Although the radiation dose of SPECT and CT may be considered low, it is currently hypothesized that there is a linear, no-threshold dose response relationship between the exposure of ionizing radiation and the development of cancer in human beings. Thus, even relatively low doses of radiation increase the risk of a patient developing malignancy over the patient’s lifetime. Accordingly, the lifetime risk of cancer development in a patient becomes an important consideration. (109)
Lifetime radiation risks are of particular concern with respect to children because of a child’s increased sensitivity to radiation and because children have more expected years of life after radiation exposure compared to adults. As cardiac diagnostic procedures are more commonly performed in individuals of advanced age, a risk-benefit scenario comes into effect. Accordingly, for a cardiac diagnostic tests performed in older adults, the risk of serious heart disease (or the risk of missing a diagnosis of serious heart disease) is greater than the theoretical risk of radiation-related cancer over a patient’s lifetime, since they have fewer years to live than children. Because the potential benefits of correctly diagnosing heart disease far outweigh the risk of radiation-associated cancer in older adults, radiation dosage rarely factors into the decision-making process when devising a clinical diagnostic plan. (107)
It should be noted that stress-only SPECT studies and low dose alternative techniques are currently being investigated in effort to lower the total effective dose, particularly for younger patients.
Aside from radiation-related events, the majority of adverse events associated with SPECT may be attributed to the administration of stress, whether by exercise or a pharmacologic agent. Generally, exercise testing is a low-risk investigation even in patients with known CAD, but serious complications can occur in 2–4 per 1000 tests. (110) Although rare, death may occur at a rate of 1–5 per 10,000 tests. Lastly, while severe side effects with pharmacologic agents are rare, mild side effects are commonly reported in 50% to 80% of patients or more, depending on the specific pharmacologic agent. (111)
Table 7: Total effective dose of various cardiac diagnostic procedures.
| Test | Effective Dose (mSv) |
|---|---|
| Average U.S. background rate | 3.0/year |
| Tc-99m tetrofosmin rest-stress (10 mCi + 30 mCi) | 10.6/study |
| Tc-99m sestamibi 1-day rest-stress (10 mCi + 30 mCi) | 12.0 |
| Tc-99m sestamibi 2-day stress-rest (30 mCi + 30 mCi) | 17.5 |
| TI-201 stress and reinjection (3.0 mCi + 1.0 mCi) | 25.1 |
| Dual-isotope (3.0 mCi TI-201 + 30 mCi Tc-99m) | 27.3 |
| Gd-153 transmission for SPECT (AC) | 0.05 |
| 64-Slice MDCT coronary CTA (female) | 13.5–21.4 |
| 64-Slice MDCT coronary CTA (male) | 9.6–15.2 |
| 64-Slice MDCT coronary CTA (female) with ECG pulsing | 6.8–14 |
| 64-Slice MDCT coronary CTA (male) without ECG pulsing | 4.8–10 |
Data from reference (107)
Limitations
There were several limitations inherent within this analysis. First, the body of literature from 1995 to 2002 may not be complete. This evidentiary base was taken from a systematic review of meta-analyses by Heijenbrok-Kal et al. (15) and, while comprehensive, the SPECT portion of this review was based on five meta-analyses, each with differing search strategies and inclusion criteria. There is, therefore, a possibility that some trials may have been missed. The decision to rely on a past systematic review was made to improve feasibility, on account of the breadth of literature published on cardiac SPECT.
A second limitation inherently stems from the trials included in this review. The issue is one of verification bias, also known as referral bias, whereby the results of the diagnostic test being studied may have been used in selecting whether the patient receives confirmatory testing by the gold standard. This form of selection bias will often increase the sensitivity while decreasing the specificity of the diagnostic technology being studied. More recent trials have begun adjusting for verification bias by investigating normalcy rates in place of specificity, although such trials are limited in number and there are too few trials to allow for comparing normalcy rates between cardiac diagnostic technologies. Trials reporting normalcy only were thus excluded from the current analysis and no adjustments were made to control for verification bias as its presence is difficult to deduce without detailed reporting. Verification bias may, therefore, exist as an important confounder.
Third, it should be noted that the gold standard of CA is, in itself, a limited test because its interpretation is often subjective. Differences in how CA was used or interpreted (e.g., qualitatively vs. quantitatively) may have disproportionately influenced the accuracy estimates of the non-invasive tests being studied.
A fourth limitation arises from the indirect nature of subgroup comparisons. By pooling estimates from single arms of trials and comparing arms indirectly, inter-study (i.e., between-study) heterogeneity is substantially increased. This increase in heterogeneity may mask significant differences between trials. Indirect comparisons were used in order to facilitate comparisons between technologies, particularly to overcome absences in direct comparative data. Accordingly, direct comparisons were examined where appropriate and when possible in attempt to confirm the findings of the indirect comparisons.
Lastly, a meta-regression was not possible due to resource constraints. The finding of no significant differences between subgroups may therefore be erroneous if significant differences are being masked by potential confounders. The ability to evaluate important subgroups should be an important consideration for future evidence-based analyses of SPECT considering the complexity of the SPECT technique and its rapid evolution in clinical practice. The need to separately evaluate the transmission source (e.g., external radiation source versus X-ray) used in AC SPECT is one example of a potentially important stratification; however, the current literature base did not permit such stratification due to the small number of studies.
Conclusions
Based on MAS’ systematic review and meta-analysis of 86 studies assessing the accuracy of SPECT for the diagnosis of CAD using CA as a reference standard, the following conclusions were made:
According to very low quality evidence, the addition of attenuation correction to traditional or ECG-gated SPECT greatly improves the specificity of SPECT for the diagnosis of CAD, although this improvement is not statistically significant. A trend towards improvement of specificity was also observed with the addition of ECG gating to traditional SPECT.
According to very low quality evidence, neither the choice of stress agent (exercise vs. pharmacologic) nor the choice of radioactive tracer (technetium vs. thallium) significantly affect the diagnostic accuracy of SPECT for the diagnosis of CAD although a trend towards accuracy improvement was observed with the use of pharmacologic stress over exercise stress and technetium over thallium.
Considerably heterogeneity was observed both within and between trials. This heterogeneity may explain why some of the differences observed between accuracy estimates for various subgroups were not statistically significant.
More complex analytic techniques such as meta-regression may help to better understand which study characteristics significantly influence the diagnostic accuracy of SPECT.
Economic Analysis
Disclaimer: The Medical Advisory Secretariat uses a standardized costing method for its economic analyses of interventions. The main cost categories and the associated methods from the province’s perspective are as follows:
Hospital: Ontario Case Costing Initiative cost data are used for in-hospital stay, emergency visit and day procedure costs for the designated International Classification of Diseases (ICD) diagnosis codes and Canadian Classification of Health Interventions procedure codes. Adjustments may be required to reflect accuracy in estimated costs of the diagnoses and procedures under consideration. Due to the difficulties of estimating indirect costs in hospitals associated with a particular diagnosis or procedure, the secretariat normally defaults to considering direct treatment costs only.
Nonhospital: These include physician services costs obtained from the Ontario Schedule of Benefits, laboratory fees from the Ontario Schedule of Laboratory Fees, drug costs from the Ontario Drug Benefit Formulary, and device costs from the perspective of local health care institutions whenever possible or its manufacturer.
Discounting: For cost-effectiveness analyses, a discount rate of 5% is applied as recommended by economic guidelines.
Downstream costs: All numbers reported are based on assumptions on population trends (i.e. incidence, prevalence and mortality rates), time horizon, resource utilization, patient compliance, healthcare patterns, market trends (i.e. rates of intervention uptake or trends in current programs in place in the Province), and estimates on funding and prices. These may or may not be realized by the system or individual institutions and are often based on evidence from the medical literature, standard listing references and educated hypotheses from expert panels. In cases where a deviation from this standard is used, an explanation is offered as to the reasons, the assumptions, and the revised approach. The economic analysis represents an estimate only, based on the assumptions and costing methods that have been explicitly stated above. These estimates will change if different assumptions and costing methods are applied to the analysis.
Study Question
The objective of this economic analysis is to determine the cost effectiveness of SPECT for the diagnosis of patients with suspected CAD as compared to: stress ECHO, stress contrast ECHO, cardiac MRI, and CT angiography. The relative cost-effectiveness of these five non-invasive cardiac imaging technologies was assessed in two patient populations: a) out-patients presenting with stable chest pain; and b) in-patients presenting with acute, unstable chest pain. Note that the term “contrast ECHO” used in the following sections refers to stress echocardiography performed with the availability of contrast medium if needed, due to poor image quality. Also, attenuation-correction SPECT was found to weakly dominate traditional and gated SPECT in the current analyses, providing better effectiveness at the same price, and so was the SPECT technology adopted for the comparisons below.
Economic Analysis Overview
For the two patient populations decision-analytic cost-effectiveness analyses were conducted to evaluate the relative cost-effectiveness of the five non-invasive cardiac imaging technologies. Two decision analytic models were developed for these patient populations with two reported outcomes: the cost per accurate diagnosis of CAD and the cost per true positive diagnosis of CAD. The physician and hospital costs for the non-invasive imaging tests were taken from 2009 Ontario Health Insurance Plan (OHIP) and the Ontario Case Costing Initiative (OCCI) administrative databases. (112;113) A budget impact analysis (BIA) was then performed to assess the effect of replacing a certain proportion of stress echocardiography (ECHO) tests with other cost-effective, non-invasive modalities. The costs presented in this BIA were estimated from Ontario data sources from 2009; the volumes of tests performed were estimated from data from fiscal years 2002 to 2008.
Economic Literature Review
The purpose of the systematic review of economic literature was to identify, retrieve, and summarize studies evaluating the cost-effectiveness of selected cardiac imaging tests for the diagnosis of CAD. Medline and the National Health Service Economic Evaluation Database (NHSEED) were searched from their inception up to October 2009. Included studies were those full economic evaluations describing both costs and consequences of CT angiography, Cardiac MRI, SPECT, stress ECHO, and stress contrast ECHO in the diagnosis of CAD. Article selection was performed by independent pairs of researchers. Target data for extraction included: study first author and year of publication, imaging tests compared, type of economic analysis, reported costs and outcomes, incremental cost-effectiveness ratio (ICER), currency, and patient characteristics (i.e., known or suspected CAD and risk of CAD). The primary outcome of interest was the ICER of each imaging test in relation to another test of interest.
Search results
A total of 883 non-duplicate citations were from the two electronic databases. Based on the content of their abstracts, 147 full-text articles were retrieved for further assessment of their inclusion/exclusion. Of these, 122 were rejected leaving 25 articles for inclusion. Following the data extraction process, 13 studies were excluded (2;114-124), with 12 studies being ultimately selected for analysis. (2;114-124), with 12 studies being ultimately selected for analysis.(125-136)
Characteristics of included studies
From the 12 included studies, eight assessed the cost-effectiveness of two of the selected imaging tests (128-131;133;135;136), three evaluated three concomitant technologies (125;132;134), and one study evaluated five technologies. (126) Five studies were cost-effectiveness analyses, where the most common outcome was cost per correct/successful CAD diagnosis. (125;126;133;135;136) The other seven studies were cost-utility analyses using cost per quality adjusted life years (QALYs) as their primary outcome. (127-132;134) The time-horizon used across the included studies ranged from 30 days to lifetime, with five studies having 25 years or more of follow-up.(127-129;131;135) The remaining studies used 18 months (134), 3 months (136), and 30 days of analytical time horizon. (130) Four studies did not report the time-horizon used in their analysis.(125;126;132;133)
All studies evaluated at least one form of ECHO against one of the other remaining selected imaging tests.(125-136) The cost-effectiveness of SPECT was studied in nine studies (125;127-129;131;132;134-136), three studies assessed CT angiography in comparison to stress ECHO or MRI (126;130;133), while cardiac MRI was compared to each of the three other selected imaging tests in two studies. (126;134) No full economic analysis between CT angiography and SPECT was found in the published literature.
Literature results for SPECT
SPECT was compared to stress ECHO in nine economic evaluations and was dominated (i.e., had a higher cost and worse outcomes) in three comparisons.(125;128;129) In one study, SPECT was compared to stress ECHO and the authors reported an ICER per correct CAD diagnosis of CDN $5,029 (136). A second economic evaluation reported that SPECT was cost-saving against stress ECHO.(134) In three other comparisons, the base-case ICER per QALY reported for SPECT in comparison to stress ECHO was above the $50,000 threshold.(127;131;135) The last study did not report an ICER, but it was stated that SPECT was cost-effective when the probability of CAD was greater than or equal to 30%.(132)
One study compared the incremental cost-effectiveness of SPECT versus MRI and reported that in the base-case analysis, SPECT was dominant over MRI for producing lower costs and greater number of QALYs. (134)
Table 8: Summary incremental cost-effectiveness ratios across selected studies evaluating SPECT.
| Study | Comparator | Outcome of interest | Reported as cost-effective? | ICER |
|---|---|---|---|---|
| Sharples et al., 2007 | MRI | Cost per QALY | Yes | Dominant |
| Bedetti et al., 2008 | Stress ECHO | Cost per correct diagnosis | No | Dominated |
| Garber et al., 1999 | Stress ECHO | Cost per QALY | No | USD (1996) $78,444 |
| Hayashino et al., 2004 | Stress ECHO | Cost per QALY | No | Dominated |
| Hernandez et al., 2007 | Stress ECHO | Cost per QALY | No | Dominated |
| Kuntz et al., 1999 | Stress ECHO | Cost per QALY | No | USD (1996) $62,800 |
| Lee et al., 2002 | Stress ECHO | Cost per QALY | Yes | Not reported* |
| Sharples et al., 2007 | Stress ECHO | Cost per QALY | Yes | Less costly, same QALYs |
| Shaw et al., 2066 | Stress ECHO | Cost per LYS | No | USD (2003) $72,187 |
Abbreviation: ND = Not defined
SPECT was cost-effective when the probability of CAD was >=30%. Stress ECHO was cost-effective when the probability of CAD was <=20%.
Conclusion
Overall, CT angiography was found to be cost-effective or cost-saving in all four of the comparisons for that technology; stress ECHO was found cost-effective in eight of the 13 comparisons in which it was evaluated; and SPECT was found cost-effective in three of nine comparisons. Cardiac MRI was not found to be cost-effective or cost-saving in any of the four comparisons found.
According to the published economic data, CT angiography is often found to be cost-effective when compared to other technologies. SPECT and stress ECHO were also found to be cost-effective in several of the comparative studies examined, while cardiac MRI was not cost-effective in any study. Limitations to these conclusions apply, such as the analyses found in the literature evaluated other forms of the selected cardiac imaging tests which might change the proposed relative cost-effectiveness.
Decision analytic Cost Effectiveness Analysis
Design
This study was designed as a cost effectiveness analysis, with primary results reported as incremental cost per true positive diagnosis, or incremental cost per accurate diagnosis. Two populations were defined for evaluating the cost-effectiveness of an accurate diagnosis (i.e., true positive and true negative diagnoses) of CAD: a) out-patients presenting with stable chest pain; and b) in-patients presenting with acute, unstable chest pain. The first population was defined as persons presenting with stable chest pain, with an intermediate risk of CAD following physical examination and a graded exercise test, as defined by the American College of Cardiology / American Heart Association 2002 Guideline Update for the Management of Patients with Chronic Stable Angina. (137)The second population was defined as persons presenting to emergency for acute, unstable chest pain, and who are admitted to hospital, as defined by the American College of Cardiology / American Heart Association 2007 Guidelines for the Management of Patients with Unstable Angina/Non-ST-Elevation Myocardial Infarction. (138)
The analytic perspective was that of the Ontario Ministry of Health and Long-Term Care (MOHLTC).
Comparators & Parameter Estimates
The imaging technologies that were compared in the current cost-effectiveness analysis included: CT angiography, stress ECHO (with and without contrast), cardiac perfusion stress MRI, and attenuation-corrected SPECT. Test characteristic estimates (i.e., specificity, sensitivity, accuracy) for each cardiac imaging technology were obtained from the systematic review and meta-analysis conducted by MAS and the MOHLTC. Table 9 shows a list of the parameters with the corresponding 95% confidence intervals used for both the outpatient and inpatient decision-analytic cost-effectiveness models.
Table 9: Parameter estimates for SPECT tests.
| Pooled Diagnostic Accuracy | Point Estimate | 95% Lower | 95% Upper |
| CAD diagnosis: Sensitivity | 0.861 | 0.812 | 0.910 |
| CAD diagnosis: Specificity | 0.821 | 0.748 | 0.895 |
| Additional time for test (compared to GXT) | Average | Low | High |
| Inpatient population: Additional days for test | 1.3 | 1.0 | 2.0 |
| Uninterpretable test result | Average | Low | High |
| Outpatient population: % of tests that are uninterpretable | 6.9% | 0.5% | 10.0% |
| Inpatient population: % of tests that are uninterpretable | 7.0% | 0.5% | 10.0% |
Note: Sensitivity and specificity estimates are taken from the effectiveness literature review of SPECT. Other estimates are based on consultations with experts in cardiology.
The average wait-time for each cardiac imaging test was measured as the additional days needed to wait for a non-invasive test compared to the average wait time for a typical graded exercise stress test (GXT). The proportion of tests deemed uninterpretable by expert opinion is shown in Table 9, with a corresponding range of high and low values. The probability of receiving pharmacological stress versus exercise stress is not listed, but reported here for completeness: approximate values of 30% for the stable, outpatient population and 80% for the unstable, inpatient population.
Time Horizon & Discounting
The time horizon for both decision-analytic models (i.e., for outpatient and inpatient populations) was the time required to determine an accurate, or true positive diagnosis of CAD. As a result, the actual time taken to determine the CAD status of patients may differ across non-invasive test strategies.
Model Structure & Outcomes
Figure 5 provides a simplified illustration of the decision-analytic model structure used for the outpatient and inpatient populations. The following two simplifying assumptions were made for the models:
Figure 5: Decision analytic model used to evaluate the cost-effectiveness of cardiac imaging technologies for the diagnosis of CAD.
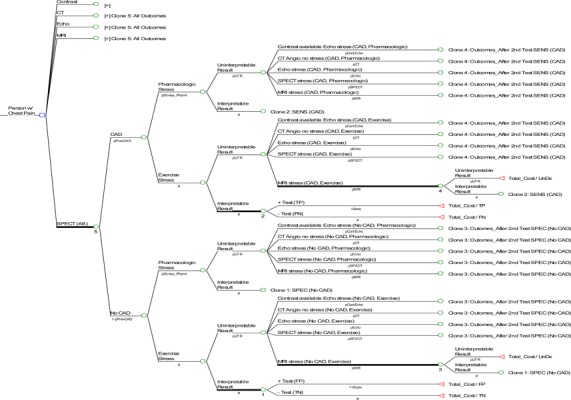
When results of the first cardiac imaging test are un-interpretable, a patient will undergo a second cardiac test. The second test will be one of the four remaining tests that were not used as the first test.
Should a second test be required, the type of stress (pharmacological or exercise) that a patient receives be the same as that used in the first test.
The short-term outcome presented in this report focuses on an accurate diagnosis of CAD (i.e., true positive and true negative test results). A second outcome of true positive diagnosis was examined for the two models, with results reported by THETA. (139;139)
Sensitivity Analyses
Various sensitivity analyses were conducted for the outpatient and inpatient populations. First, the prevalence of CAD was varied from 5% to 95% in 5% increments, while all other model estimates were held constant. Willingness-to-pay (WTP) was also varied and a range of results were presented. Second, one-way sensitivity analyses were conducted in which selected estimates were varied over plausible ranges. The varied parameters which were varied included sensitivity and specificity estimates, wait times for imaging tests performed in hospital, as well as the costs of CT angiography, ECHO tests, and cardiac MRI. A third series of sensitivity analyses was conducted that specifically addressed the possibility unavailable imaging technologies.
Resource Use and Costs
Resource use and costs were derived from Ontario data sources: the OHIP and OCCI administrative databases. (112;113) The cost of conducting each cardiac test was calculated as the sum of the test’s respective professional fees and technical fees, as described in the Ontario Schedule of Benefits (see Table 10). Note that for contrast ECHO tests, the cost for the contrast medium was added for use in the event of uninterpretable ECHO results. The cost of this contrast medium was estimated as $170 per vial (single use) through consultation with industry experts. Only this cost was added to the base test cost of contrast ECHO. In general, where an imaging test result was uninterpretable, an additional cost of follow-up with the patient (physician fee) was incurred, as well as the cost for conducting another cardiac imaging test. For out-patients presenting with stable chest pain, a consultation professional fee of $30.60 (OHIP code A608 for “partial assessment”) was used after an uninterpretable test result (one time cost).
Table 10: List of cardiac imaging tests and associated OHIP 2009 costs.
| Technology | List of professional fees | Subtotal | List of technical fees | Subtotal | Total | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cardiac CT | Fee code | X125 | X417 | Imputed | |||||||||
| Cost | $89.20 | $64.00 | $153.20 | $336.52 | $336.52 | $489.72 | |||||||
| Cardiac MRI (dobutamine stress with gadolinium) | Fee code | X441 | X445 | X487 | G319 | Imputed | G315 | G174 | |||||
| Multiplier | 1.0 | 3.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | ||||||
| Cost | $75.55 | $37.80 | $37.75 | $62.65 | $289.35 | $463.06 | $33.65 | $37.00 | $533.71 | $823.06 | |||
| Cardiac SPECT (exercise stress) | Fee code | J866 | J811 | J807 | G319 | J866 | J811 | J807 | G315 | ||||
| Cost | $28.70 | $55.30 | $47.00 | $62.65 | $193.65 | $44.60 | $97.55 | $223.15 | $33.65 | $398.95 | $592.60 | ||
| Cardiac SPECT (dobutamine stress) | Fee code | J866 | J811 | J807 | G319 | J866 | J811 | J807 | G315 | G174 | |||
| Cost | $28.70 | $55.30 | $47.00 | $62.65 | $193.65 | $44.60 | $97.55 | $223.15 | $33.65 | $37.00 | $435.95 | $629.60 | |
| Cardiac SPECT (dipyramidole stress) | Fee code | J866 | J811 | J807 | G112 | J866 | J811 | J807 | G111 | ||||
| Cost | $28.70 | $55.30 | $47.00 | $75.00 | $206.00 | $44.60 | $97.55 | $223.15 | $41.10 | $406.40 | $612.40 | ||
| ECHO (exercise stress) | Fee code | G571 | G578 | G575 | G319 | G570 | G577 | G574 | G315 | ||||
| Cost | $74.10 | $36.90 | $17.45 | $62.65 | $191.10 | $76.45 | $45.15 | $16.45 | $33.65 | $171.70 | $362.80 | ||
| ECHO (dobutamine stress) | Fee code | G5 71 | G578 | G575 | G319 | G570 | G577 | G574 | G315 | G174 | |||
| Cost | $74.10 | $36.90 | $17.45 | $62.65 | $191.10 | $76.45 | $45.15 | $16.45 | $33.65 | $37.00 | $208.70 | $399.80 | |
| ECHO (dipyramidole stress) | Fee code | G571 | G578 | G575 | G112 | G570 | G577 | G574 | G111 | ||||
| Cost | $74.10 | $36.90 | $17.45 | $75.00 | $203.45 | $76.45 | $45.15 | $16.45 | $41.10 | $179.15 | $382.60 | ||
Notes: Fee codes are taken from the 2009 OHIP fee schedule. (113) Imputed technical fees were based on the proportion of average technical fees associated with above ECHO and SPECT fee code combinations. For cardiac SPECT and ECHO stress tests, an average test cost was calculated using dobutamine and dipyramidole fee codes.
In the case of patients presenting with acute, unstable chest pain, inpatient hospitalization costs were also included in the model. The total cost of hospitalization was calculated based on the average wait time for each cardiac imaging test and a cost per diem for each day spent in hospital (for the SPECT wait time, see Table 9). An additional consultation fee was also used only for the inpatient population: $29.20 (OHIP code C602 for “subsequent visit- first five weeks”) was used for each inpatient day spent in hospital.
Willingness-to-pay
The WTP must be determined by the MOHLTC. As such, all reasonable WTP values are presented in the Results and Discussion section are interpreted at two WTP ‘anchors’, representing the estimated cost of the most expensive non-invasive test considered in our model (cardiac MRI perfusion, $804) and the estimated cost of a coronary angiography ($1,433). These anchors are intended only to guide discussion.
Note that the following points might be useful in determining the WTP:
An ‘accurate diagnosis’ of CAD can be obtained through a coronary angiography for $1,433. It would thus be reasonable to expect the WTP for an accurate diagnosis through a non-invasive test to resemble this amount; however, an accurate diagnosis does not include the value or benefit of providing additional diagnostic or prognostic information from either non-invasive imaging or coronary angiography
The MOHLTC is currently willing to pay up to $804 for a non-invasive test with less-than-perfect diagnostic accuracy. Its willingness to pay for an accurate diagnosis from such a test thus appears to be greater than $804.
While coronary angiography is invasive, the other tests are non-invasive and would presumably be of greater value (i.e., incur a higher premium). These tests do, however, impose risks not applicable to coronary angiography, such as increased radiation exposure and adverse reaction to contrast agents
These tests are not perfectly accurate. An accurate diagnosis from such a test may be valued less than one from a coronary angiography
Results and Discussion
As shown in Tables 11 and 12, in stable outpatients SPECT was dominated by CT angiography – it had higher costs and was less effective. In acute inpatients SPECT reported an ICER of $5,113 per accurate diagnosis versus contrast ECHO. At reasonable WTP values (anchored at approximately $804 or $1,433 per accurate diagnosis) SPECT does not, therefore, appear cost-effective.
Table 11: Cost-effectiveness analysis base case results for stable outpatients.
| Technology | Cost (C) | Δ Cost | Effect (E) | Δ Effect | C/E | ICER |
|---|---|---|---|---|---|---|
| Stress contrast ECHO | $433.49 | 81.83% | $530 | N/A | ||
| CT angiography | $517.73 | $84.24 | 87.35% | 5.52% | $593 | $1,527 |
| Stress ECHO | $551.58 | 81.06% | $680 | (Dominated) | ||
| SPECT | $634.63 | 82.80% | $766 | (Dominated) | ||
| Cardiac MRI | $835.47 | 85.15% | $981 | (Dominated) |
Table 12: Cost-effectiveness analysis base case results for acute inpatients.
| Technology | Cost (C) | Δ Cost | Effect (E) | Δ Effect | C / E | ICER |
|---|---|---|---|---|---|---|
| Stress contrast ECHO | $1,794.58 | 81.94% | $2,190 | N/A | ||
| SPECT | $1,982.91 | $188.32 | 83.92% | 1.99% | $2,363 | $9,489 |
| Stress ECHO | $2,550.87 | 81.53% | $3,129 | (Dominated) | ||
| CT angiography | $3,267.39 | $1,284.48 | 87.49% | 3.56% | $3,735 | $36,055 |
| Cardiac MRI | $4,918.02 | 85.55% | $5,749 | (Dominated) |
For stable outpatients, when both CT angiography and contrast ECHO were removed from the analysis, SPECT appeared cost-effective at the higher WTP anchor ($1,433 per accurate diagnosis) only when the prevalence of CAD was greater than 55%. At the lower WTP anchor ($804 per accurate diagnosis), SPECT did not appear to be cost-effective at any CAD prevalence value. Sensitivity analysis also showed that SPECT could be considered a cost-effective strategy for acute inpatients only under a very high prevalence of CAD and for WTP values much higher than these anchors. When contrast ECHO was removed from the analysis, however, SPECT appeared cost-effective for acute inpatients at all reasonable WTP and prevalence values.
To summarize, attenuated SPECT appeared more cost-effective than both traditional and gated SPECT, although SPECT was not considered a cost-effective strategy compared to either contrast ECHO or CT angiography in the stable chest pain patient population. SPECT appeared cost-effective at the higher WTP anchor only in cases where other, more cost-effective technologies were unavailable and where the prevalence of CAD was greater than 55%.
Budget Impact Analysis
The budget impact analysis (BIA) was performed taking the perspective of the MOHLTC and includes both physician and hospital (clinic) costs of non-invasive cardiac imaging tests. Volumes of cardiac tests in Ontario were taken from administrative databases (OHIP, DAD, NACRS) for fiscal years 2004 to 2008 using methodology summarized in The THETA report (139). The following technologies were considered in the current BIA for the diagnosis of CAD: ECHO (including both stress and stress with contrast agent available), nuclear cardiac imaging (including MPI and SPECT tests), cardiac MRI, and CT angiography.
In the current BIA, the effect of moving a certain proportion of the volume of specific tests to another, substitute technology was assessed for various scenarios. These scenarios are presented irrespective of whether a technology was found to be cost-effective and are reported as general reference tables. These scenarios are presented irrespective of whether a technology was found to be cost-effective and are reported as general reference tables. To summarize briefly, nuclear cardiac tests (MPI and SPECT) were found to be the second most expensive of the compared cardiac imaging modalities. When the volume of nuclear cardiac tests is shifted to other technologies, all scenarios result in lower projected costs, except for cardiac MRI imaging. If 25% of the nuclear cardiac tests are moved to other imaging technologies, ensuing projected costs would be lower (excluding cardiac MRI): from the largest cost avoidance of about $10.8M per year for stress ECHO testing to the smallest cost avoidance of $5.8M for CT angiography. The largest possible cost avoidance corresponds to replacing 50% of nuclear cardiac tests with stress ECHO imaging ($21.7M per year); the smallest cost avoidance occurs by replacing 5% of nuclear cardiac tests with CT angiography imaging ($1.2M per year), excluding cardiac MRI.
Glossary
- Attenuation Correction (AC) SPECT
A SPECT analysis using motion correction, blur correction and/or soft tissue attenuation correction. AC may have been achieved by any one or combination of software, gadolinium line source or CT x-ray radiation methods. Note that trials labelled or analyzed as AC may or may not have also included ECG gating. (Due to the small number of studies, ECG-gated SPECT plus AC was not analyzed as a distinct subgroup.)
- Dual Isotope
Any trial which used a different radioactive tracer at stress than at rest within the same SPECT study (i.e., within the same patient).
- ECG-Gated SPECT
A SPECT acquisition guided by ECG gating. For the purposes of this review, all trials labelled as ECG-gated SPECT did not report attenuation correction.
- Previous myocardial infarction (MI)
Any history of MI or previous MI within the last one month (i.e., “No” signifies that no patient had a previous MI within one month; “Yes” signifies that at least one or more patients had a history of MI or previous MI within the last one month)
- Interpretation
Describes the method of SPECT image interpretation used to define CAD positivity. For the purpose of subgroup analysis, all trials reporting visual, visual and semi-quantitative, or semi-quantitative interpretation were labelled as “Qualitative” while trials reporting quantitative or semi-quantitative + quantitative interpretation were labelled as “Quantitative.”
Appendices
Appendix 1: Literature Search Strategies
Updated Literature Search: January 2, 2002 to October 30, 2009
Search date: October 30, 2009
Databases searched: OVID MEDLINE, MEDLINE In-Process and Other Non-Indexed Citations, OVID EMBASE, Wiley Cochrane, Centre for Reviews and Dissemination/International Agency for Health Technology Assessment
Database: Ovid MEDLINE(R) <1996 to October Week 4 2009>
Search Strategy
exp Myocardial Ischemia/ (135175)
(coronary adj2 arter* disease*).mp. [mp=title, original title, abstract, name of substance word, subject heading word, unique identifier] (38944)
((myocardi* or heart or cardiac or coronary) adj2 (viable or viability or perfusion or function or isch?emi* or atheroscleros* or arterioscleros* or infarct* or occlu* or stenos* or thrombosis)).mp. (125265)
(myocardi* adj2 hibernat*).mp. [mp=title, original title, abstract, name of substance word, subject heading word, unique identifier] (610)
(stenocardia* or angina).mp. [mp=title, original title, abstract, name of substance word, subject heading word, unique identifier] (21606)
heart attack*.mp. (1896)
exp Heart Failure/ (34267)
((myocardi* or heart or cardiac) adj2 (failure or decompensation or insufficiency)).mp. (60297)
exp Ventricular Dysfunction, Left/ (13993)
(left adj2 ventric* adj2 (dysfunction* or failure or insufficienc*)).mp. (17297)
or/1-10 (226980)
exp Tomography, Emission-Computed, Single-Photon/or exp Myocardial Perfusion Imaging/ (15654)
((single photon adj3 tomograph*) or SPECT or SPET or MPS).ti,ab. (15722)
(scinti* adj2 (coronary or heart or myocardi* or cardiac or perfusion or viability or isch?emi* or cad or coronary artery disease or thallium or sestamibi or mibi or technetium)).ti,ab. (3249)
or/12-14 (22579)
11 and 15 (5932)
limit 16 to (english language and humans and yr=“2002 -Current”) (2933)
limit 17 to (case reports or comment or editorial or letter) (479)
17 not 18 (2454)
Database: EMBASE <1980 to 2009 Week 43>
Search Strategy
exp ischemic heart disease/ (241354)
exp coronary artery disease/ (89908)
exp stunned heart muscle/ (1537)
(coronary adj2 arter* disease*).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] (72491)
((myocardi* or heart or cardiac or coronary) adj2 (viable or viability or perfusion or function or ischemi* or atheroscleros* or arterioscleros* or infarct* or occlu* or stenos* or thrombosis)).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] (278988)
(myocardi* adj2 hibernat*).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] (1059)
(stenocardia* or angina).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] (46732)
heart attack*.mp. (2053)
exp heart failure/ (127353)
((myocardi* or heart or cardiac) adj2 (failure or decompensation or insufficiency)).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] (109249)
exp heart left ventricle failure/ (9478)
(left adj2 ventric* adj2 (dysfunction* or failure or insufficienc*)).mp. (16310)
or/1-12 (435714)
exp single photon emission computer tomography/ (26142)
((single photon adj3 tomograph*) or SPECT or SPET or MPS).ti,ab. (22465)
(scinti* adj2 (coronary or heart or myocardi* or cardiac or perfusion or viability or isch?emi* or cad or coronary artery disease or thallium or sestamibi or mibi or technetium)).ti,ab. (6378)
or/14-16 (36626)
17 and 13 (10134)
limit 18 to (human and english language and yr=“2002 -Current”) (3668)
limit 19 to (editorial or letter or note) (366)
case report/ (1060365)
19 not (20 or 21) (2908)
Appendix 2: Included Studies
Table A1: Characteristics of included studies comparing the accuracy of SPECT to CA for the diagnosis of CAD.
| Author | Year | N* | Type of SPECT | Tracer | Stress Agent | % Stenosis | % Men† | Mean Age† | Prior MI | Interp. |
|---|---|---|---|---|---|---|---|---|---|---|
| Aggeli (90) | 2007 | 48 | Traditional | Tl | Ad | 50 | - | - | Yes | V+Q |
| Amanullah (36) | 1997 | 222 | Traditional | Dual | Ad | 50 | 54 | 71 | No | SQ |
| Astarita (53) | 2001 | 53 | Traditional | Tl | Ex | 50 | 55 | 58 | No | V |
| Banzo (91) | 2003 | 99 | Traditional/AC | Tc | Ex+Dip+Ad | 70 | 72 | 59 | Yes | V+SQ |
| Benoit (59) | 1996 | 72 | Traditional | Tc | Ex | 50 | 82 | 58 | Yes | V |
| Berman (82) | 2006 | 785 | Gated | Tc | Ex/Ad | 70 | - | - | No | V+SQ/Q |
| Bokhari (95) | 2008 | 218 | Gated | Tl+Dual | Ex | 50 | 69 | 62 | No | V+Q |
| Chammas (105) | 2002 | 58 | Traditional | Tc | Ex | 60 | 83 | 57 | No | - |
| Cramer (54) | 1996 | 35 | Traditional | Tc | Dip | 50 | 69 | 58 | No | V |
| Daou (20) | 2002 | 338 | Traditional | Tl | Ex | 50 | - | - | Yes | V |
| De (21) | 2002 | 49 | Traditional | Tc | - | 70 | - | - | - | - |
| DiBello (37) | 1996 | 45 | Traditional | Tc | Dob | 50 | 73 | 43 | No | V+SQ |
| Dondi (70) | 2004 | 130 | Traditional/AC | Tc | Ex+Pharma | 50 | - | - | Yes | V |
| Elhendy (38) | 1998 | 70 | Traditional | Tc | Dob | 50 | 0 | 58 | Yes | V+SQ |
| Elhendy (83) | 2006 | 88 | Traditional | Tc | Ex+Dob | 50 | 0 | 100 | No | V+SQ |
| Emmett (61) | 2002 | 100 | Gated | Tc | Ex | 70 | 77 | 60 | Yes | V+SQ |
| Ficaro (56) | 1996 | 60 | Traditional | Dual | Ex+Pharma | 50 | 63 | 63 | Yes | V/Q |
| Fragasso (52) | 1999 | 101 | Traditional | Tc | Ex | 50 | 54 | 61 | No | V |
| Gallowitsch (31) | 1998 | 107 | Traditional/AC | Tl | Ex/Dip | 70 | 64 | 64 | Yes | V |
| Gentile (22) | 2001 | 132 | Traditional | Tl | Ex+Dip | 60 | 68 | 71 | No | V |
| Gonzalez (77) | 2005 | 145 | Traditional | Tl | Ex+Dip | 50 | 68 | 60 | Yes | V+SQ |
| Groutars (67) | 2003 | 123 | Traditional | Dual | Ex+Ad | 50/70 | 72 | 59 | No | V+SQ |
| Grossman (71) | 2004 | 74 | Gated/Gated+AC | Tc | Ex | 50 | - | - | - | Q |
| Hambye (72) | 2004 | 100 | Gated/Gated+AC | Tc | Ex+Ad | 50 | 48 | 64 | Yes | SQ+Q |
| Hannoush (68) | 2003 | 51 | Traditional | Tc | Ex+Dip | 50 | - | - | Yes | V |
| He (62) | 2002 | 51 | Traditional | Tc | Ad | 50 | - | - | No | V |
| He (63) | 2003 | 26 | Traditional | Tc | Ex | 50 | 81 | 58 | - | V |
| Heiba (32) | 1997 | 34 | Traditional | Tc | Ex | 50 | - | - | Yes | SQ |
| Hida (100) | 2009 | 119 | Gated | Tc | Ad | 75 | 66 | 68 | No | V |
| Ho (40) | 1997 | 51 | Traditional | Tl | Ex | 50 | - | - | Yes | V |
| Ho (39) | 1995 | 54 | Traditional | Tl | Dip | 50 | 85 | 58 | Yes | V |
| Huang (41) | 1998 | 110 | Traditional | Tl | Dob | 50 | 74 | 61 | No | V |
| Huang (42) | 1997 | 93 | Traditional | Tl | Dob | 50 | 77 | 61 | Yes | V |
| Hung (84) | 2006 | 126 | Gated | Tl | Dip | 70 | 71 | 66 | Yes | V |
| Iftikhar (57) | 1996 | 38 | Traditional | Tc | Dob | 50 | - | - | Yes | V |
| Jeetley (85) | 2006 | 123 | Traditional | Tc | Dip | 50 | 71 | 62 | Yes | V+SQ |
| Johansen (78) | 2005 | 357 | Gated | Dual | Ex+Pharma | 50 | 54 | 57 | No | V+SQ |
| Kajinami (23) | 1995 | 251 | Traditional | Tl | Ex | 75 | 69 | 56 | - | V |
| Katayama (96) | 2008 | 46 | Traditional | Tl | Ex+Dip | 75 | 74 | 71 | Yes | SQ |
| Khattar (24) | 1998 | 100 | Traditional | Tc | Dob+Ad | 50 | 70 | 62 | Yes | SQ |
| Kisacik (58) | 1996 | 69 | Traditional | Tc | Ex | 50 | - | - | Yes | V |
| Korosoglou (86) | 2006 | 89 | Traditional | Tc | Pharma | 75 | - | - | Yes | V |
| Lima (64) | 2002 | 255 | Gated | Tc | Ex+Pharma | 70 | 65 | 61 | Yes | Q |
| Lin (87) | 2006 | 40 | Traditional | Dual | Dip | 50 | - | - | Yes | V |
| Links (60) | 2000 | 69 | Gated/Gated+AC | Mixed | Ex+Pharma | 50 | - | - | Yes | V |
| Lipiec (97) | 2008 | 103 | Traditional | Tc | Dip | 50 | 63 | 58 | Yes | V+Q |
| Masood (79) | 2005 | 118 | Traditional/AC | Tc | Ex+Pharma | 50 | 67 | 61 | No | V/Q1/Q2 |
| Matsumoto (88) | 2006 | 56 | Gated | Tc | Ex+Pharma | 50 | - | - | Yes | SQ |
| McClellan (25) | 1996 | 303 | Traditional | Tl | Ex | 50 | - | - | Yes | V+Q |
| Michaelides (26) | 1999 | 245 | Traditional | Tl | Ex | 70 | 89 | 52 | No | V+Q |
| Mieres (92) | 2007 | 42 | Gated | Tc/Dual | Ex+Ad | 50 | - | - | No | - |
| Miller (43) | 1997 | 243 | Traditional | Tc | Dip | 50 | - | - | Yes | V |
| Mohiuddin (44) | 1996 | 202 | Traditional | Tl | Ad | 50 | 59 | 58 | Yes | Q |
| Nallamothu (27) | 1995 | 321 | Traditional | Tl | Ex | 50 | 75 | 57 | - | V+Q |
| Ogilby (55) | 1998 | 26 | Traditional | Tc | Dip | 50 | 73 | 57 | Yes | V |
| Palmas (33) | 1995 | 70 | Traditional | Tc | Ex | 50 | 81 | 60 | Yes | V |
| Patsilinakos (73) | 2004 | 75 | Traditional | Tl | Ad | 50 | 68 | 69 | - | V |
| Peltier (74) | 2004 | 35 | Traditional | Tc | Dip | 70 | 71 | 62 | No | V+Q |
| Psirropoulos (28) | 2002 | 301 | Traditional | Tl | Ex | 50 | - | - | Yes | - |
| Rollan (65) | 2002 | 54 | Traditional | Tc | Dob | 50 | - | - | Yes | V |
| Rubello (34) | 1995 | 120 | Traditional | Tc | Ex | 50 | 88 | 51 | Yes | V/Q |
| Sakuma (80) | 2005 | 40 | Traditional | Tl | Ex+Pharma | 70 | 70 | 65 | No | V |
| San Roman (45) | 1998 | 92 | Traditional | Tc | Dob | 50 | - | - | No | V |
| Santana-Boado (30) | 1998 | 163 | Traditional | Tc | Ex+Dip | 50 | 61 | 59 | No | V |
| Santoro (46) | 1998 | 60 | Traditional | Tc | Dip/Dob | 70 | - | - | No | V |
| Schepis (93) | 2007 | 77 | Gated+AC | Tc | Ad | 50 | 62 | 66 | No | V+SQ |
| Schillaci (47) | 1997 | 40 | Traditional | Tc | Dip | 70 | 63 | 55 | No | Q |
| Senior (75) | 2004 | 55 | Traditional | Tc | Dob | 50 | 82 | - | No | V |
| Shelley (69) | 2003 | 108 | Gated | Tc | Ad | 50 | - | - | Yes | Q |
| Shirai (29) | 2002 | 603 | Gated | Tl | Ex | 70 | 76 | 63 | Yes | V |
| Slavich (48) | 1996 | 46 | Traditional | Tc | Dob | 50 | 0 | 59 | No | V |
| Slomka (89) | 2006 | 174 | Gated/Gated+AC | Tc | Ex+Pharma | 50 | 67 | 64 | No | Q |
| Soman (49) | 1997 | 27 | Traditional | Tc | Dip/Arb | 50 | 67 | 58 | Yes | SQ |
| Suzuki (98) | 2008 | 90 | Gated | Dual | Ex+Pharma | 50 | 70 | 63 | No | Q |
| Tadehara (99) | 2008 | 101 | Gated | Tc | Ad | 50 | - | - | Yes | V |
| Taillefer (35) | 1997 | 85 | Traditional | Ti/Tc | Ex/Dip | 50/70 | 0 | 60 | Yes | Q |
| Takeuchi (50) | 1996 | 61 | Traditional | Tl | Ex+Dip | 50 | - | - | No | V+Q |
| Thompson (81) | 2005 | 116 | Gated/Gated+AC | Tc | Ex/Pharma | 70 | 70 | 60 | No | V |
| Tsai (66) | 2002 | 86 | Traditional | Tl | Ex | 50 | - | - | Yes | V |
| Watanabe (51) | 1997 | 140 | Traditional | Tl | Dip/Ad | 50 | 64 | 63 | Yes | V |
| Wolak (103) | 2008a | 114 | Gated/Gated+AC | Tc | Ex+Ad | 70 | 0 | 65 | Yes | Q |
| Wolak (104) | 2008b | 188 | Traditional | Tc | Ex+Pharma | 70 | 69 | 64 | Yes | Q |
| Wu (101) | 2009 | 218 | Traditional | Tc | Dip | 50 | 62 | 64 | Yes | V |
| Yao (76) | 2004 | 73 | Traditional | Tc | Ex | 50 | - | - | No | - |
| Yeih (94) | 2007 | 51 | Traditional | Tl | Dob | 50 | 0 | 63 | Yes | V |
| Yoon (102) | 2009 | 344 | Traditional | Tc | Ad+Dip | 70 | - | - | - | - |
Abbreviations: AC, attenuation correction; Ad, adenosine; Arb, arbutamine; Dip, dipyridamole; Dob, dobutamine; Dual, dual isotope; Ex, exercise; Interp., method of SPECT interpretation; Pharma, pharmacologic (agents not specified); Q, quantitative; Q1, quantitative software 1; Q2, quantitative software 2; SQ, semi-quantitative; Tc, technetium; Tl, thallium; V, visual
Sample analyzed
Reported only for sample analyzed
Describes trials which included patients any previous MI or previous MI within the last one month (i.e., “No” signifies that no patients had a previous MI within one month; “Yes” signifies that the trial included some, not necessarily all, patients with a history of MI or previous MI within the last one month)
signifies that the an unspecified combination of modalities/tracers/agents were used, in “either/or” fashion
signifies that the modalities/tracers/agents were analyzed as distinct subgroups
Abbreviations: AC, attenuation correction; Ad, adenosine; Arb, arbutamine; Dip, dipyridamole; Dob, dobutamine; Dual, dual isotope; Ex, exercise; Interp., method of SPECT interpretation; Pharma, pharmacologic (agents not specified); Q, quantitative; Q1, quantitative software 1; Q2, quantitative software 2; SQ, semi-quantitative; Tc, technetium; Tl, thallium; V, visual
Table A2: Estimates of diagnostic accuracy across included studies.
| Author | N* | Type of SPECT | Tracer | Stress Agent | % Sten. | MI | Interp. | TP | FP | FN | TN | Sen. | Spe. | PPV | NPV | (+) LR | (-) LR | Ace. |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Aggeli, 2007 (90) | 48 | Traditional | Tl | Ad | 50 | Yes | V+Q | 24 | 1 | 6 | 17 | 0.80 | 0.94 | 0.96 | 0.74 | 14.40 | 0.21 | 0.85 |
| Amanullah, 1997 (36) | 222 | Traditional | Dual | Ad | 50 | No | SQ | 159 | 14 | 12 | 37 | 0.93 | 0.73 | 0.92 | 0.76 | 3.39 | 0.10 | 0.88 |
| Astarita, 2001 (53) | 53 | Traditional | Tl | Ex | 50 | No | V | 23 | 16 | 0 | 14 | 1.00 | 0.47 | 0.59 | 1.00 | 1.88 | 0.00 | 0.70 |
| Banzo, 2003 (91) | 99 | Traditional | Tc | Ex+Dip+Ad | 70 | Yes | V+SQ | 47 | 26 | 4 | 22 | 0.92 | 0.46 | 0.64 | 0.85 | 1.70 | 0.17 | 0.70 |
| 99 | AC | 39 | 14 | 12 | 34 | 0.76 | 0.71 | 0.74 | 0.74 | 2.62 | 0.33 | 0.74 | ||||||
| Benoit, 1996 (59) | 72 | Traditional | Tc | Ex | 50 | Yes | V | 55 | 1 | 8 | 8 | 0.87 | 0.89 | 0.98 | 0.50 | 7.86 | 0.14 | 0.88 |
| Berman, 2006 (82) | 365 | Gated | Tc | Ex | 70 | No | V+SQ | 251 | 40 | 24 | 50 | 0.91 | 0.56 | 0.86 | 0.68 | 2.05 | 0.16 | 0.82 |
| 420 | Ad | V+SQ | 252 | 77 | 28 | 63 | 0.90 | 0.45 | 0.77 | 0.69 | 1.64 | 0.22 | 0.75 | |||||
| 785 | Ex+Ad | V+SQ | 503 | 117 | 52 | 113 | 0.91 | 0.49 | 0.81 | 0.68 | 1.78 | 0.19 | 0.78 | |||||
| 290 | Ex+Ad | Q | 186 | 9 | 39 | 56 | 0.83 | 0.86 | 0.95 | 0.59 | 5.97 | 0.20 | 0.83 | |||||
| Bokhari, 2008 (95) | 218 | Gated | Tl+Dual | Ex | 50 | No | V+Q | 116 | 16 | 27 | 59 | 0.81 | 0.79 | 0.88 | 0.69 | 3.80 | 0.24 | 0.80 |
| Chammas, 2002 (105) | 58 | Traditional | Tc | Ex | 60 | No | - | 30 | 6 | 4 | 18 | 0.88 | 0.75 | 0.83 | 0.82 | 3.53 | 0.16 | 0.83 |
| Cramer, 1996 (54) | 35 | Traditional | Tc | Dip | 50 | No | V | 23 | 1 | 6 | 5 | 0.79 | 0.83 | 0.96 | 0.45 | 4.76 | 0.25 | 0.80 |
| Daou, 2002 (20) | 338 | Traditional | Tl | Ex | 50 | Yes | V | 167 | 17 | 98 | 56 | 0.63 | 0.77 | 0.91 | 0.36 | 2.71 | 0.48 | 0.66 |
| De, 2002 (21) | 49 | Traditional | Tc | - | 70 | - | - | 8 | 26 | 4 | 11 | 0.67 | 0.30 | 0.24 | 0.73 | 0.95 | 1.12 | 0.39 |
| DiBello, 1996 (37) | 45 | Traditional | Tc | Dob | 50 | No | V+SQ | 33 | 1 | 5 | 6 | 0.87 | 0.86 | 0.97 | 0.55 | 6.08 | 0.15 | 0.87 |
| Dondi, 2004 (70) | 130 | Traditional | Tc | Ex+Pharma | 50 | Yes | V | 104 | 6 | 4 | 16 | 0.96 | 0.73 | 0.95 | 0.80 | 3.53 | 0.05 | 0.92 |
| 130 | AC | 100 | 2 | 8 | 20 | 0.93 | 0.91 | 0.98 | 0.71 | 10.19 | 0.08 | 0.92 | ||||||
| Elhendy, 1998 (38) | 88 | Traditional | Tc | Ex+Dob | 50 | No | V+SQ | 29 | 7 | 16 | 18 | 0.64 | 0.72 | 0.81 | 0.53 | 2.30 | 0.49 | 0.67 |
| Elhendy, 2006 (83) | 70 | Traditional | Tc | Dob | 50 | Yes | V+SQ | 44 | 7 | 9 | 28 | 0.83 | 0.80 | 0.86 | 0.76 | 4.15 | 0.21 | 0.82 |
| Emmett, 2002 (61) | 100 | Gated | Tc | Ex | 70 | Yes | V+SQ | 62 | 11 | 8 | 19 | 0.89 | 0.63 | 0.85 | 0.70 | 2.42 | 0.18 | 0.81 |
| Ficaro, 1996 (56) | 60 | Traditional | Dual | Ex+Pharma | 50 | Yes | V | 38 | 6 | 11 | 5 | 0.78 | 0.45 | 0.86 | 0.31 | 1.42 | 0.49 | 0.72 |
| 60 | Q | 41 | 6 | 8 | 5 | 0.84 | 0.45 | 0.87 | 0.38 | 1.53 | 0.36 | 0.77 | ||||||
| Fragasso, 1999 (52) | 101 | Traditional | Tc | Ex | 50 | No | V | 56 | 28 | 1 | 16 | 0.98 | 0.36 | 0.67 | 0.94 | 1.54 | 0.05 | 0.71 |
| Gallowitsch, 1998 (31) | 68 | Traditional | Tl | Ex | 70 | Yes | V | 30 | 10 | 6 | 22 | 0.83 | 0.69 | 0.75 | 0.79 | 2.67 | 0.24 | 0.76 |
| 68 | AC | Ex | 35 | 4 | 1 | 28 | 0.97 | 0.88 | 0.90 | 0.97 | 7.78 | 0.03 | 0.93 | |||||
| 39 | Traditional | Dip | 12 | 1 | 5 | 21 | 0.71 | 0.95 | 0.92 | 0.81 | 15.53 | 0.31 | 0.85 | |||||
| 39 | AC | Dip | 15 | 1 | 2 | 21 | 0.88 | 0.95 | 0.94 | 0.91 | 19.41 | 0.12 | 0.92 | |||||
| 107 | Traditional | Ex/Dip | 42 | 11 | 11 | 43 | 0.79 | 0.80 | 0.79 | 0.80 | 3.89 | 0.26 | 0.79 | |||||
| 107 | AC | Ex/Dip | 50 | 5 | 3 | 49 | 0.94 | 0.91 | 0.91 | 0.94 | 10.19 | 0.06 | 0.93 | |||||
| Gentile, 2001 (22) | 132 | Traditional | Tl | Ex+Dip | 60 | No | V | 101 | 11 | 7 | 13 | 0.94 | 0.54 | 0.90 | 0.65 | 2.04 | 0.12 | 0.86 |
| Gonzalez, 2005 (77) | 145 | Traditional | Tl | Ex+Dip | 50 | Yes | V+SQ | 102 | 12 | 15 | 16 | 0.87 | 0.57 | 0.89 | 0.52 | 2.03 | 0.22 | 0.81 |
| Grossman, 2004 (71) | 74 | Gated | Tc | Ex | 50 | - | Q | 38 | 25 | 1 | 10 | 0.97 | 0.29 | 0.60 | 0.91 | 1.36 | 0.09 | 0.65 |
| 74 | Gated+AC | 35 | 15 | 4 | 20 | 0.90 | 0.57 | 0.70 | 0.83 | 2.09 | 0.18 | 0.74 | ||||||
| 123 | Traditional | Dual | Ex+Ad | 50 | No | V+SQ | 102 | 6 | 6 | 9 | 0.94 | 0.60 | 0.94 | 0.60 | 2.36 | 0.09 | 0.90 | |
| Groutars, 2003 (67) | ||||||||||||||||||
| 123 | 70 | 93 | 11 | 3 | 16 | 0.97 | 0.59 | 0.89 | 0.84 | 2.38 | 0.05 | 0.89 | ||||||
| Ham bye, 2004 (72) | 100 | Gated | Tc | Ex+Ad | 50 | Yes | SQ+Q | 60 | 3 | 26 | 11 | 0.70 | 0.79 | 0.95 | 0.30 | 3.26 | 0.38 | 0.71 |
| 100 | Gated+AC | 63 | 3 | 23 | 11 | 0.73 | 0.79 | 0.95 | 0.32 | 3.42 | 0.34 | 0.74 | ||||||
| Hannoush, 2003 (68) | 51 | Traditional | Tc | Ex+Dip | 50 | Yes | V | 40 | 4 | 1 | 6 | 0.98 | 0.60 | 0.91 | 0.86 | 2.44 | 0.04 | 0.90 |
| He, 2002 (62) | 26 | Traditional | Tc | Ex | 50 | - | V | 33 | 3 | 1 | 14 | 0.97 | 0.82 | 0.92 | 0.93 | 5.50 | 0.04 | 0.92 |
| He, 2003 (63) | 51 | Traditional | Tc | Ad | 50 | No | V | 18 | 0 | 4 | 4 | 0.82 | 1.00 | 1.00 | 0.50 | 81.82 | 0.18 | 0.85 |
| Heiba, 1997 (32) | 34 | Traditional | Tc | Ex | 50 | Yes | SQ | 28 | 1 | 2 | 3 | 0.93 | 0.75 | 0.97 | 0.60 | 3.73 | 0.09 | 0.91 |
| Hida, 2009 (100) | 119 | Gated | Tc | Ad | 75 | No | V | 32 | 7 | 30 | 50 | 0.52 | 0.88 | 0.82 | 0.63 | 4.20 | 0.55 | 0.69 |
| Ho, 1997 (40) | 51 | Traditional | Tl | Ex | 50 | Yes | V | 29 | 3 | 9 | 10 | 0.76 | 0.77 | 0.91 | 0.53 | 3.31 | 0.31 | 0.76 |
| Ho, 1995 (39) | 54 | Traditional | Tl | Dip | 50 | Yes | V | 42 | 3 | 1 | 8 | 0.98 | 0.73 | 0.93 | 0.89 | 3.58 | 0.03 | 0.93 |
| Huang, 1998 (41) | 110 | Traditional | Tl | Dob | 50 | No | V | 53 | 8 | 12 | 37 | 0.82 | 0.82 | 0.87 | 0.76 | 4.59 | 0.22 | 0.82 |
| Huang, 1997 (42) | 93 | Traditional | Tl | Dob | 50 | Yes | V | 60 | 5 | 7 | 21 | 0.90 | 0.81 | 0.92 | 0.75 | 4.66 | 0.13 | 0.87 |
| Hung, 2006 (84) | 126 | Gated | Tl | Dip | 70 | Yes | V | 75 | 16 | 6 | 29 | 0.93 | 0.64 | 0.82 | 0.83 | 2.60 | 0.11 | 0.83 |
| Iftikhar, 1996 (57) | 38 | Traditional | Tc | Dob | 50 | Yes | V | 22 | 1 | 6 | 9 | 0.79 | 0.90 | 0.96 | 0.60 | 7.86 | 0.24 | 0.82 |
| Jeetley, 2006 (85) | 123 | Traditional | Tc | Dip | 50 | Yes | V+SQ | 79 | 13 | 17 | 14 | 0.82 | 0.52 | 0.86 | 0.45 | 1.71 | 0.34 | 0.76 |
| Johansen, 2005 (78) | 357 | Gated | Dual | Ex+Pharma | 50 | No | V+SQ | 94 | 48 | 32 | 183 | 0.75 | 0.79 | 0.66 | 0.85 | 3.59 | 0.32 | 0.78 |
| Kajinami, 1995 (23) | 251 | Traditional | Tl | Ex | 75 | - | V | 110 | 48 | 23 | 70 | 0.83 | 0.59 | 0.70 | 0.75 | 2.03 | 0.29 | 0.72 |
| Katayama, 2008 (96) | 46 | Traditional | Tl | Ex+Dip | 75 | Yes | SQ | 17 | 7 | 5 | 17 | 0.77 | 0.71 | 0.71 | 0.77 | 2.65 | 0.32 | 0.74 |
| Khattar, 1998 (24) | 100 | Traditional | Tc | Dob+Ad | 50 | Yes | SQ | 41 | 11 | 19 | 29 | 0.68 | 0.73 | 0.79 | 0.60 | 2.48 | 0.44 | 0.70 |
| Kisacik, 1996 (58) | 69 | Traditional | Tc | Ex | 50 | Yes | V | 45 | 8 | 2 | 14 | 0.96 | 0.64 | 0.85 | 0.88 | 2.63 | 0.07 | 0.86 |
| Korosoglou, 2006 (86) | 89 | Traditional | Tc | Pharma | 75 | Yes | V | 48 | 13 | 14 | 14 | 0.77 | 0.52 | 0.79 | 0.50 | 1.61 | 0.44 | 0.70 |
| Lima, 2002 (64) | 255 | Gated | Tc | Ex+Pharma | 70 | Yes | Q | 187 | 12 | 25 | 31 | 0.88 | 0.72 | 0.94 | 0.55 | 3.16 | 0.16 | 0.85 |
| Lin, 2006 (87) | 40 | Traditional | Dual | Dip | 50 | Yes | V | 19 | 3 | 6 | 12 | 0.76 | 0.80 | 0.86 | 0.67 | 3.80 | 0.30 | 0.78 |
| Links, 2000 (60) | 69 | Gated | Mixed | Ex+Pharma | 50 | Yes | V | 43 | 8 | 8 | 10 | 0.84 | 0.56 | 0.84 | 0.56 | 1.90 | 0.28 | 0.77 |
| 69 | Gated+AC | 45 | 1 | 6 | 17 | 0.88 | 0.94 | 0.98 | 0.74 | 15.88 | 0.12 | 0.90 | ||||||
| Lipiec, 2008 (97) | 103 | Traditional | Tc | Dip | 50 | Yes | V+Q | 79 | 5 | 10 | 9 | 0.89 | 0.64 | 0.94 | 0.47 | 2.49 | 0.17 | 0.85 |
| Masood, 2005 (79) | 118 | Traditional | Tc | Ex+Pharma | 50 | No | V | 80 | 14 | 6 | 18 | 0.93 | 0.56 | 0.85 | 0.75 | 2.13 | 0.12 | 0.83 |
| 118 | AC | V | 81 | 13 | 5 | 19 | 0.94 | 0.59 | 0.86 | 0.79 | 2.32 | 0.10 | 0.85 | |||||
| 118 | Traditional | Q1 | 60 | 11 | 26 | 21 | 0.70 | 0.66 | 0.85 | 0.45 | 2.03 | 0.46 | 0.69 | |||||
| 118 | AC | Q1 | 67 | 4 | 19 | 28 | 0.78 | 0.88 | 0.94 | 0.60 | 6.23 | 0.25 | 0.81 | |||||
| 118 | Traditional | Q2 | 58 | 7 | 28 | 25 | 0.67 | 0.78 | 0.89 | 0.47 | 3.08 | 0.42 | 0.70 | |||||
| 118 | AC | Q2 | 60 | 7 | 26 | 25 | 0.70 | 0.78 | 0.90 | 0.49 | 3.19 | 0.39 | 0.72 | |||||
| Matsumoto, 2006 (88) | 56 | Gated | Tc | Ex+Pharma | 50 | Yes | SQ | 22 | 1 | 4 | 29 | 0.85 | 0.97 | 0.96 | 0.88 | 25.38 | 0.16 | 0.91 |
| McClellan, 1996 (25) | 303 | Traditional | Tl | Ex | 50 | Yes | V+Q | 193 | 12 | 82 | 16 | 0.70 | 0.57 | 0.94 | 0.16 | 1.64 | 0.52 | 0.69 |
| Michaelides, 1999 | ||||||||||||||||||
| (26) | 245 | Traditional | Tl | Ex | 70 | No | V+Q | 196 | 6 | 15 | 28 | 0.93 | 0.82 | 0.97 | 0.65 | 5.26 | 0.09 | 0.91 |
| Mieres, 2007 (92) | 42 | Gated | Tc/Dual | Ex+Ad | 50 | No | - | 14 | 3 | 2 | 23 | 0.88 | 0.88 | 0.82 | 0.92 | 7.58 | 0.14 | 0.88 |
| Miller, 1997 (43) | 243 | Traditional | Tc | Dip | 50 | Yes | V | 185 | 29 | 18 | 11 | 0.91 | 0.28 | 0.86 | 0.38 | 1.26 | 0.32 | 0.81 |
| Mohiuddin, 1996 (44) | 202 | Traditional | Tl | Ad | 50 | Yes | Q | 144 | 6 | 16 | 36 | 0.90 | 0.86 | 0.96 | 0.69 | 6.30 | 0.12 | 0.89 |
| Nallamothu, 1995 (27) | 321 | Traditional | Tl | Ex | 50 | - | V+Q | 216 | 17 | 51 | 37 | 0.81 | 0.69 | 0.93 | 0.42 | 2.57 | 0.28 | 0.79 |
| Ogilby, 1998 (55) | 26 | Traditional | Tc | Dip | 50 | Yes | V | 18 | 0 | 2 | 6 | 0.90 | 1.00 | 1.00 | 0.75 | 90.00 | 0.10 | 0.92 |
| Palmas, 1995 (33) | 70 | Traditional | Tc | Ex | 50 | Yes | V | 60 | 1 | 6 | 3 | 0.91 | 0.75 | 0.98 | 0.33 | 3.64 | 0.12 | 0.90 |
| Patsilinakos, 2004 (73) | 75 | Traditional | Tl | Ad | 50 | - | V | 31 | 11 | 4 | 29 | 0.89 | 0.73 | 0.74 | 0.88 | 3.22 | 0.16 | 0.80 |
| Peltier, 2004 (74) | 35 | Traditional | Tc | Dip | 70 | No | V+Q | 18 | 2 | 4 | 11 | 0.82 | 0.85 | 0.90 | 0.73 | 5.32 | 0.21 | 0.83 |
| Psirropoulos, 2002 (28) | 301 | Traditional | Tl | Ex | 50 | Yes | - | 33 | 136 | 26 | 106 | 0.56 | 0.44 | 0.20 | 0.80 | 1.00 | 1.01 | 0.46 |
| Rollan, 2002 (65) | 54 | Traditional | Tc | Dob | 50 | Yes | V | 23 | 12 | 3 | 16 | 0.88 | 0.57 | 0.66 | 0.84 | 2.06 | 0.20 | 0.72 |
| Rubello, 1995 (34) | 120 | Traditional | Tc | Ex | 50 | Yes | V | 98 | 5 | 9 | 8 | 0.92 | 0.62 | 0.95 | 0.47 | 2.38 | 0.14 | 0.88 |
| 120 | Q | 100 | 5 | 7 | 8 | 0.93 | 0.62 | 0.95 | 0.53 | 2.43 | 0.11 | 0.90 | ||||||
| Sakuma, 2005 (80) | 40 | Traditional | Tl | Ex+Pharma | 70 | No | V | 17 | 7 | 4 | 12 | 0.81 | 0.63 | 0.71 | 0.75 | 2.20 | 0.30 | 0.73 |
| San Roman, 1998 (45) | 92 | Traditional | Tc | Dob | 50 | No | V | 54 | 9 | 8 | 21 | 0.87 | 0.70 | 0.86 | 0.72 | 2.90 | 0.18 | 0.82 |
| Santana-Boado, 1998 (30) | 163 | Traditional | Tc | Ex+Dip | 50 | No | V | 88 | 7 | 8 | 60 | 0.92 | 0.90 | 0.93 | 0.88 | 8.77 | 0.09 | 0.91 |
| Santoro, 1998 (46) | 60 | Traditional | Tc | Dip | 70 | No | V | 32 | 3 | 1 | 24 | 0.97 | 0.89 | 0.91 | 0.96 | 8.73 | 0.03 | 0.93 |
| 60 | Dob | 30 | 5 | 3 | 22 | 0.91 | 0.81 | 0.86 | 0.88 | 4.91 | 0.11 | 0.87 | ||||||
| Schepis, 2007 (93) | 77 | Gated+AC | Tc | Ad | 50 | No | V+SQ | 32 | 3 | 10 | 32 | 0.76 | 0.91 | 0.91 | 0.76 | 8.89 | 0.26 | 0.83 |
| Schillaci, 1997 (47) | 40 | Traditional | Tc | Dip | 70 | No | Q | 21 | 5 | 1 | 13 | 0.95 | 0.72 | 0.81 | 0.93 | 3.44 | 0.06 | 0.85 |
| Senior, 2004 (75) | 55 | Traditional | Tc | Dob | 50 | No | V | 21 | 1 | 22 | 11 | 0.49 | 0.92 | 0.95 | 0.33 | 5.86 | 0.56 | 0.58 |
| Shelley, 2003 (69) | 108 | Gated | Tc | Ad | 50 | Yes | Q | 64 | 8 | 0 | 36 | 1.00 | 0.82 | 0.89 | 1.00 | 5.50 | 0.00 | 0.93 |
| Shirai, 2002 (29) | 603 | Gated | Tl | Ex | 70 | Yes | V | 106 | 13 | 131 | 353 | 0.45 | 0.96 | 0.89 | 0.73 | 12.59 | 0.57 | 0.76 |
| Slavich, 1996 (48) | 46 | Traditional | Tc | Dob | 50 | No | V | 18 | 4 | 4 | 20 | 0.82 | 0.83 | 0.82 | 0.83 | 4.91 | 0.22 | 0.83 |
| Slomka, 2006 (89) | 174 | Gated | Tc | Ex+Pharma | 50 | No | Q | 115 | 7 | 22 | 30 | 0.84 | 0.81 | 0.94 | 0.58 | 4.44 | 0.20 | 0.83 |
| 174 | Gated+AC | 117 | 10 | 20 | 27 | 0.85 | 0.73 | 0.92 | 0.57 | 3.16 | 0.20 | 0.83 | ||||||
| Soman, 1997 (49) | 27 | Traditional | Tc | Dip | 50 | Yes | SQ | 19 | 2 | 2 | 4 | 0.90 | 0.67 | 0.90 | 0.67 | 2.71 | 0.14 | 0.85 |
| 27 | Arb | 21 | 2 | 0 | 4 | 1.00 | 0.67 | 0.91 | 1.00 | 3.00 | 0.00 | 0.93 | ||||||
| Suzuki, 2008 (98) | 90 | Gated | Dual | Ex+Pharma | 50 | No | Q | 58 | 5 | 5 | 22 | 0.92 | 0.81 | 0.92 | 0.81 | 4.97 | 0.10 | 0.89 |
| Tadehara, 2008 (99) | 101 | Gated | Tc | Ad | 50 | Yes | V | 50 | 14 | 4 | 33 | 0.93 | 0.70 | 0.78 | 0.89 | 3.11 | 0.11 | 0.82 |
| Taillefer, 1997 (35) | 48 | Traditional | Tl | Ex | 50 | Yes | Q | 24 | 8 | 8 | 8 | 0.75 | 0.50 | 0.75 | 0.50 | 1.50 | 0.50 | 0.67 |
| 48 | TC | Ex | 50 | 23 | 3 | 9 | 13 | 0.72 | 0.81 | 0.88 | 0.59 | 3.83 | 0.35 | 0.75 | ||||
| 37 | Tl | Dip | 50 | 24 | 0 | 8 | 5 | 0.75 | 1.00 | 1.00 | 0.38 | 75.00 | 0.25 | 0.78 | ||||
| 37 | TC | Dip | 50 | 23 | 0 | 9 | 5 | 0.72 | 1.00 | 1.00 | 0.36 | 71.87 | 0.28 | 0.76 | ||||
| 48 | Tl | Ex | 70 | 22 | 10 | 6 | 10 | 0.79 | 0.50 | 0.69 | 0.63 | 1.57 | 0.43 | 0.67 | ||||
| 48 | TC | Ex | 70 | 21 | 3 | 7 | 17 | 0.75 | 0.85 | 0.88 | 0.71 | 5.00 | 0.29 | 0.79 | ||||
| 37 | Tl | Dip | 70 | 21 | 4 | 2 | 10 | 0.91 | 0.71 | 0.84 | 0.83 | 3.20 | 0.12 | 0.84 | ||||
| 37 | TC | Dip | 70 | 20 | 3 | 3 | 11 | 0.87 | 0.79 | 0.87 | 0.79 | 4.06 | 0.17 | 0.84 | ||||
| 85 | Tl | Ex/Dip | 50 | 48 | 8 | 16 | 13 | 0.75 | 0.62 | 0.86 | 0.45 | 1.97 | 0.40 | 0.72 | ||||
| 85 | TC | Ex/Dip | 50 | 46 | 3 | 18 | 18 | 0.72 | 0.86 | 0.94 | 0.50 | 5.03 | 0.33 | 0.75 | ||||
| 85 | Tl | Ex/Dip | 70 | 43 | 14 | 8 | 20 | 0.84 | 0.59 | 0.75 | 0.71 | 2.05 | 0.27 | 0.74 | ||||
| 85 | TC | Ex/Dip | 70 | 41 | 6 | 10 | 28 | 0.80 | 0.82 | 0.87 | 0.74 | 4.56 | 0.24 | 0.81 | ||||
| Takeuchi, 1996 (50) | 61 | Traditional | Tl | Ex/Dip | 50 | No | V+Q | 14 | 13 | 4 | 30 | 0.78 | 0.70 | 0.52 | 0.88 | 2.57 | 0.32 | 0.72 |
| Thompson, 2005 (81) | 116 | Gated | Tc | Ex+Pharma | 70 | No | V | 78 | 14 | 10 | 14 | 0.89 | 0.50 | 0.85 | 0.58 | 1.77 | 0.23 | 0.79 |
| 116 | Gated+AC | 76 | 6 | 12 | 22 | 0.86 | 0.79 | 0.93 | 0.65 | 4.03 | 0.17 | 0.84 | ||||||
| Tsai, 2002 (66) | 86 | Traditional | Tl | Ex | 50 | Yes | V | 60 | 11 | 3 | 12 | 0.95 | 0.52 | 0.85 | 0.80 | 1.99 | 0.09 | 0.84 |
| Watanabe, 1997 (51) | 70 | Traditional | Tl | Dip | 50 | Yes | V | 34 | 8 | 7 | 21 | 0.83 | 0.72 | 0.81 | 0.75 | 3.01 | 0.24 | 0.79 |
| 70 | Ad | 40 | 3 | 6 | 21 | 0.87 | 0.88 | 0.93 | 0.78 | 6.96 | 0.15 | 0.87 | ||||||
| 140 | Dip/Ad | 74 | 11 | 13 | 42 | 0.85 | 0.79 | 0.87 | 0.76 | 4.10 | 0.19 | 0.83 | ||||||
| Wolak, 2008a (103) | 114 | Gated | Tc | Ex+Ad | 70 | Yes | Q | 55 | 12 | 14 | 33 | 0.80 | 0.73 | 0.82 | 0.70 | 2.99 | 0.28 | 0.77 |
| 114 | Gated+AC | 56 | 12 | 13 | 33 | 0.81 | 0.73 | 0.82 | 0.72 | 3.04 | 0.26 | 0.78 | ||||||
| Wolak, 2008b (104) | 188 | Traditional | Tc | Ex+Pharma | 70 | Yes | Q | 124 | 13 | 19 | 32 | 0.87 | 0.71 | 0.91 | 0.63 | 3.00 | 0.19 | 0.83 |
| Wu, 2009 (101) | 218 | Traditional | Tc | Dip | 50 | Yes | V | 123 | 33 | 7 | 55 | 0.95 | 0.63 | 0.79 | 0.89 | 2.52 | 0.09 | 0.82 |
| Yao, 2004 (76) | 73 | Traditional | Tc | Ex | 50 | No | - | 28 | 3 | 7 | 35 | 0.80 | 0.92 | 0.90 | 0.83 | 10.13 | 0.22 | 0.86 |
| Yeih, 2007 (94) | 51 | Traditional | Tl | Dob | 50 | Yes | V | 20 | 3 | 8 | 20 | 0.71 | 0.87 | 0.87 | 0.71 | 5.48 | 0.33 | 0.78 |
| Yoon, 2009 (102) | 344 | Traditional | Tc | Ad+Dip | 70 | - | - | 191 | 83 | 28 | 42 | 0.87 | 0.34 | 0.70 | 0.60 | 1.31 | 0.38 | 0.68 |
Sample analyzed
Blank rows below author indicate the presence of subgroups
Abbreviations: AC, attenuation correction; Ad, adenosine; Arb, arbutamine; Dip, dipyridamole; Dob, dobutamine; Dual, dual isotope; Ex, exercise; Interpret., method of SPECT interpretation; LR, likelihood ratio; MI, myocardial infarction; NPV, negative predictive value; Pharma, pharmacologic (agents not specified); PPV, positive predictive value; Q, quantitative; Q1, quantitative software 1; Q2, quantitative software 2; Sen., sensitivity; Spe., specificity; Sten., stenosis; SQ, semi-quantitative; Tc, technetium; Tl, thallium; V, visual
Appendix 3: Forest Plots of Sensitivity and Specificity for Included Studies
Figure A1: Forest plot of sensitivity and specificity for included AC SPECT studies.
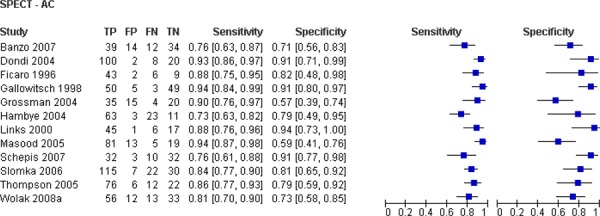
Figure A2: Forest plot of sensitivity and specificity for included ECG-gated SPECT studies.
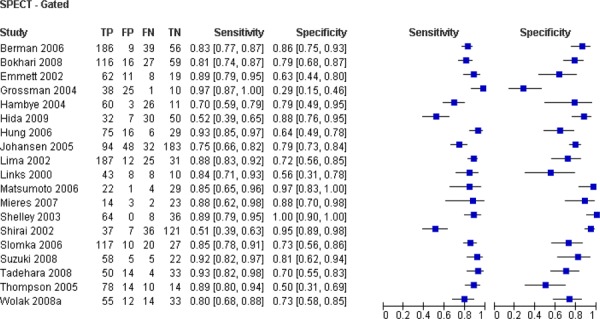
Figure A3: Forest plot of sensitivity and specificity for included traditional SPECT studies.
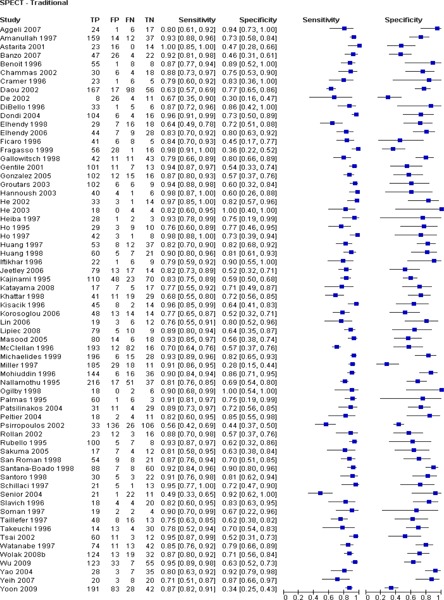
Figure A4: Forest plot of sensitivity and specificity of AC vs .non-AC SPECT trials.
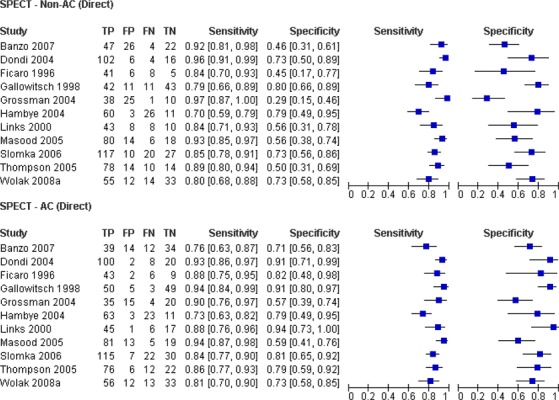
Figure A5: Forest plot of sensitivity and specificity of SPECT by stress agent.
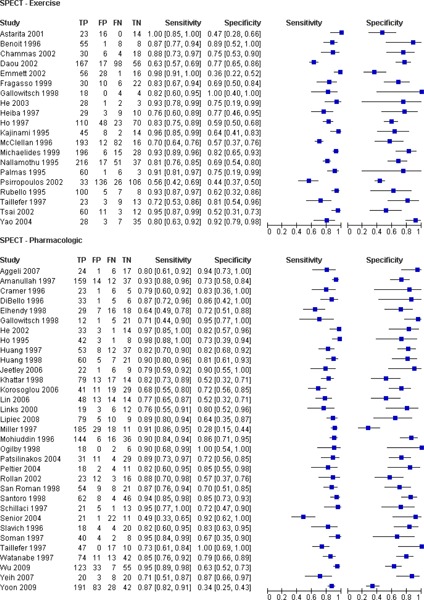
Figure A6: Forest plot of sensitivity and specificity of SPECT radioactive tracer.
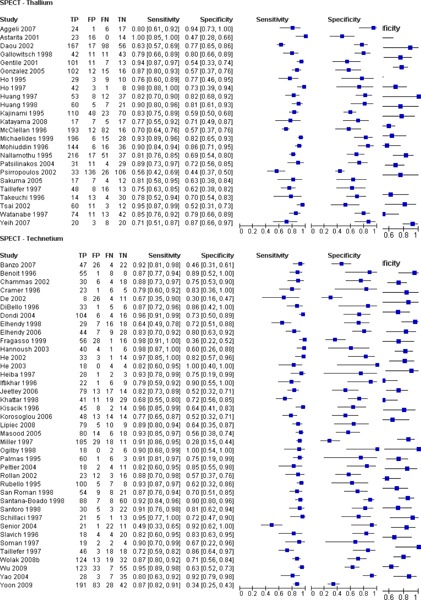
Suggested Citation
This report should be cited as follows:
Medical Advisory Secretariat. Single photon emission computed tomography for the diagnosis of coronary artery disease: an evidence-based analysis. Ont Health Technol Assess Ser [Internet]. 2010 June [cited YYYY MM DD]; 10(8) 1-64. http://www.health.gov.on.ca/english/providers/program/mas/tech/reviews/pdf/cardiac_spect_20100528.pdf
Permission Requests
All inquiries regarding permission to reproduce any content in the Ontario Health Technology Assessment Series should be directed to MASinfo.moh@ontario.ca.
How to Obtain Issues in the Ontario Health Technology Assessment Series
All reports in the Ontario Health Technology Assessment Series are freely available in PDF format at the following URL: www.health.gov.on.ca/ohtas.
Print copies can be obtained by contacting MASinfo.moh@ontario.ca.
Conflict of Interest Statement
All analyses in the Ontario Health Technology Assessment Series are impartial and subject to a systematic evidence-based assessment process. There are no competing interests or conflicts of interest to declare.
Peer Review
All Medical Advisory Secretariat analyses are subject to external expert peer review. Additionally, the public consultation process is also available to individuals wishing to comment on an analysis prior to finalization. For more information, please visit http://www.health.gov.on.ca/english/providers/program/ohtac/public_engage_overview.html.
Contact Information
The Medical Advisory Secretariat
Ministry of Health and Long-Term Care
20 Dundas Street West, 10th floor
Toronto, Ontario
CANADA
M5G 2C2
Email: MASinfo.moh@ontario.ca
Telephone: 416-314-1092
ISSN 1915-7398 (Online)
ISBN 978-1-4435-1962-5 (PDF)
About the Medical Advisory Secretariat
The Medical Advisory Secretariat is part of the Ontario Ministry of Health and Long-Term Care. The mandate of the Medical Advisory Secretariat is to provide evidence-based policy advice on the coordinated uptake of health services and new health technologies in Ontario to the Ministry of Health and Long-Term Care and to the healthcare system. The aim is to ensure that residents of Ontario have access to the best available new health technologies that will improve patient outcomes.
The Medical Advisory Secretariat also provides a secretariat function and evidence-based health technology policy analysis for review by the Ontario Health Technology Advisory Committee (OHTAC).
The Medical Advisory Secretariat conducts systematic reviews of scientific evidence and consultations with experts in the health care services community to produce the Ontario Health Technology Assessment Series.
About the Ontario Health Technology Assessment Series
To conduct its comprehensive analyses, the Medical Advisory Secretariat systematically reviews available scientific literature, collaborates with partners across relevant government branches, and consults with clinical and other external experts and manufacturers, and solicits any necessary advice to gather information. The Medical Advisory Secretariat makes every effort to ensure that all relevant research, nationally and internationally, is included in the systematic literature reviews conducted.
The information gathered is the foundation of the evidence to determine if a technology is effective and safe for use in a particular clinical population or setting. Information is collected to understand how a new technology fits within current practice and treatment alternatives. Details of the technology’s diffusion into current practice and input from practising medical experts and industry add important information to the review of the provision and delivery of the health technology in Ontario. Information concerning the health benefits; economic and human resources; and ethical, regulatory, social and legal issues relating to the technology assist policy makers to make timely and relevant decisions to optimize patient outcomes.
If you are aware of any current additional evidence to inform an existing evidence-based analysis, please contact the Medical Advisory Secretariat: MASinfo.moh@ontario.ca. The public consultation process is also available to individuals wishing to comment on an analysis prior to publication. For more information, please visit http://www.health.gov.on.ca/english/providers/program/ohtac/public_engage_overview.html.
Disclaimer
This evidence-based analysis was prepared by the Medical Advisory Secretariat, Ontario Ministry of Health and Long-Term Care, for the Ontario Health Technology Advisory Committee and developed from analysis, interpretation, and comparison of scientific research and/or technology assessments conducted by other organizations. It also incorporates, when available, Ontario data, and information provided by experts and applicants to the Medical Advisory Secretariat to inform the analysis. While every effort has been made to reflect all scientific research available, this document may not fully do so. Additionally, other relevant scientific findings may have been reported since completion of the review. This evidence-based analysis is current to the date of the literature review specified in the methods section. This analysis may be superseded by an updated publication on the same topic. Please check the Medical Advisory Secretariat Website for a list of all evidence-based analyses: http://www.health.gov.on.ca/ohtas.
List of Tables
| Table 1: Characteristics of meta-analyses included in systematic review by Heijenbrok-Kal, 2007* |
| Table 2: Quality of evidence of included studies |
| Table 3: Pooled accuracy estimates of included trials stratified by study characteristic |
| Table 4: Tests of significance between SPECT subgroups |
| Table 5 Diagnostic GRADE evaluation of methodological quality of included trials |
| Table 6 Diagnostic GRADE evaluation of methodological quality of included trials |
| Table 7: Total effective dose of various cardiac diagnostic procedures |
| Table 8: Summary incremental cost-effectiveness ratios across selected studies evaluating SPECT |
| Table 9: Parameter estimates for SPECT tests: sensitivity, specificity; additional days needed to wait for cardiac tests; proportion of non-invasive tests considered uninterpretable |
| Table 10: List of cardiac imaging tests and associated OHIP 2009 costs |
| Table 11: Cost-effectiveness analysis base case results for stable outpatients |
| Table 12: Cost-effectiveness analysis base case results for acute inpatients |
| Table A1: Characteristics of included studies comparing the accuracy of SPECT to CA for the diagnosis of CAD |
List of Abbreviations
- AC
Attenuation correction
- AUC
Area under the curve
- BIA
Budget impact analysis
- CA
Coronary angiography
- CAD
Coronary artery disease
- CDN
Canadian dollars
- CI
Confidence interval(s)
- DOR
Diagnostic odds ratio
- ECG
Electrocardiogram
- GXT
Graded exercise test
- ICER
Incremental cost-effectiveness ratio
- LR
Likelihood ratio
- LVF
Left ventricular function
- LYS
Life-years saved
- MAS
Medical Advisory Secretariat
- MOHLTC
Ministry of Health and Long-Term Care
- MPA
Myocardial perfusion analysis
- MPI
Myocardial perfusion imaging
- MPS
Myocardial perfusion scintigraphy
- OCCI
Ontario Case Costing Initiative
- OR
Odds ratio
- OHIP
Ontario Health Insurance
- OHTAC
Ontario Health Technology Advisory Committee
- QALY
Quality adjusted life year
- RCT
Randomized controlled trial
- RR
Relative risk
- SD
Standard deviation
- PECT
Single photon emission computed tomography
- SROC
Summary receiver operating characteristic
- WMA
Wall motion analysis
- WTP
Willingness to pay
References
- 1.Hendel RC, Berman DS, Di Carli MF, Heidenreich PA, Henkin RE, Pellikka PA, et al. ACCF/ASNC/ACR/AHA/ASE/SCCT/SCMR/SNM 2009 Appropriate Use Criteria for Cardiac Radionuclide Imaging: A Report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the American Society of Nuclear Cardiology, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the Society of Cardiovascular Computed Tomography, the Society for Cardiovascular Magnetic Resonance, and the Society of Nuclear Medicine. J Am Coll Cardiol. 2009;53(23):2201–29. doi: 10.1016/j.jacc.2009.02.013. Endorsed by the American College of Emergency Physicians. [DOI] [PubMed] [Google Scholar]
- 2.Mowatt G, Vale L, Brazzelli M, Hernandez R, Murray A, Scott N, et al. Systematic review of the effectiveness and cost-effectiveness, and economic evaluation, of myocardial perfusion scintigraphy for the diagnosis and management of angina and myocardial infarction. Health Technol Assess. 2004;8(30):1–223. doi: 10.3310/hta8300. [DOI] [PubMed] [Google Scholar]
- 3.National Health Service. Myocardial perfusion scintigraphy for the diagnosis and management of angina and myocardial infarction. [Internet] [updated 2003; cited 2009 Oct 29] Available from: http://www.nice.org.uk/TA73 .
- 4.Gibbons RJ. Myocardial perfusion imaging. Heart. 2000;83(3):355–60. doi: 10.1136/heart.83.3.355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Canadian Cancer Society. Medical isotopes shortage. [Internet] [updated 2009 Dec 13; cited 2009 Dec 14] Available from: http://www.cancer.ca/Canada-wide/About%20us/Media%20centre/Issues%20watch/Medical%20isotope%20shortage.aspx?sc_lang=en .
- 6.Atomic Energy of Canada Limited. NRU Status Report #35 - AECL provides update on NRU activities. [Internet] [updated 2009 Dec 23; cited 2009 Dec 18] Available from: http://www.aecl.ca/NewsRoom/Community_Bulletins/091223.htm .
- 7.Ministry of Health and Long-Term Care. Guidelines for the prioritization of procedures employing Tc-99m. [Internet] [updated 2009 May; cited 2009 Dec 18] Available from: http://www.health.gov.on.ca/english/providers/program/emu/health_notices/ihn_guidelines_20090520.pdf .
- 8.Baghdasarian SB, Heller GV. The role of myocardial perfusion imaging in the diagnosis of patients with coronary artery disease: developments over the past year. Curr Opin Cardiol. 2005;20(5):369–74. doi: 10.1097/01.hco.0000174211.16257.31. [DOI] [PubMed] [Google Scholar]
- 9.Heller GV, Links J, Bateman TM, Ziffer JA, Ficaro E, Cohen MC, et al. American Society of Nuclear Cardiology and Society of Nuclear Medicine joint position statement: Attenuation correction of myocardial perfusion SPECT scintigraphy. J Nucl Cardiol. 2004;11(2):229–30. doi: 10.1016/j.nuclcard.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 10.Garcia EV. SPECT attenuation correction: an essential tool to realize nuclear cardiology’s manifest destiny. J Nucl Cardiol. 2007;14(1):16–24. doi: 10.1016/j.nuclcard.2006.12.144. [DOI] [PubMed] [Google Scholar]
- 11.Garcia EV. Quantitative myocardial perfusion single-photon emission computed tomographic imaging: quo vadis? (Where do we go from here?) J Nucl Cardiol. 1994;1(1):83–93. doi: 10.1007/BF02940015. [DOI] [PubMed] [Google Scholar]
- 12.Chu H, Cole SR. Bivariate meta-analysis of sensitivity and specificity with sparse data: a generalized linear mixed model approach. J Clin Epidemiol. 2006;59(12):1331–2. doi: 10.1016/j.jclinepi.2006.06.011. [DOI] [PubMed] [Google Scholar]
- 13.Benjamini Y, Hochburg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Series B Stat Methodol. 1995;57(1):289–300. [Google Scholar]
- 14.Schunemann HJ, Oxman AD, Brozek J, Glasziou P, Jaeschke R, Vist GE, et al. Grading quality of evidence and strength of recommendations for diagnostic tests and strategies. BMJ. 2008;336(7653):1106–10. doi: 10.1136/bmj.39500.677199.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heijenbrok-Kal MH, Fleischmann KE, Hunink MG. Stress echocardiography, stress single-photon-emission computed tomography and electron beam computed tomography for the assessment of coronary artery disease: a meta-analysis of diagnostic performance. Am Heart J. 2007;154(3):415–23. doi: 10.1016/j.ahj.2007.04.061. [DOI] [PubMed] [Google Scholar]
- 16.O’Keefe JH Jr, Barnhart CS, Bateman TM. Comparison of stress echocardiography and stress myocardial perfusion scintigraphy for diagnosing coronary artery disease and assessing its severity. Am J Cardiol. 1995;75(11):25D–34D. [PubMed] [Google Scholar]
- 17.Fleischmann KE, Hunink MG, Kuntz KM, Douglas PS. Exercise echocardiography or exercise SPECT imaging? A meta-analysis of diagnostic test performance. JAMA. 1998;280(10):913–20. doi: 10.1001/jama.280.10.913. [DOI] [PubMed] [Google Scholar]
- 18.Kim C, Kwok YS, Heagerty P, Redberg R. Pharmacologic stress testing for coronary disease diagnosis: A meta-analysis. Am Heart J. 2001;142(6):934–44. doi: 10.1067/mhj.2001.119761. [DOI] [PubMed] [Google Scholar]
- 19.Imran MB, Palinkas A, Picano E. Head-to-head comparison of dipyridamole echocardiography and stress perfusion scintigraphy for the detection of coronary artery disease: a meta-analysis. The International Journal of Cardiovascular Imaging. 2003;19(1):23–8. doi: 10.1023/a:1021746515555. Comparison between stress echo and scintigraphy. [DOI] [PubMed] [Google Scholar]
- 20.Daou D, Delahaye N, Vilain D, Lebtahi R, Faraggi M, Le GD. Identification of extensive coronary artery disease: incremental value of exercise Tl-201 SPECT to clinical and stress test variables. J Nucl Cardiol. 2002;9(2):161–8. doi: 10.1067/mnc.2002.119974. [DOI] [PubMed] [Google Scholar]
- 21.De S, Searles G, Haddad H. The prevalence of cardiac risk factors in women 45 years of age or younger undergoing angiography for evaluation of undiagnosed chest pain. Can J Cardiol. 2002;18(9):945–8. [PubMed] [Google Scholar]
- 22.Gentile R, Vitarelli A, Schillaci O, Lagana B, Gianni C, Rossi-Fanelli F, et al. Diagnostic accuracy and prognostic implications of stress testing for coronary artery disease in the elderly. Ital Heart J. 2001;2(7):539–45. [PubMed] [Google Scholar]
- 23.Kajinami K, Seki H, Takekoshi N, Mabuchi H. Noninvasive prediction of coronary atherosclerosis by quantification of coronary artery calcification using electron beam computed tomography: comparison with electrocardiographic and thallium exercise stress test results. J Am Coll Cardiol. 1995;26(5):1209–21. doi: 10.1016/0735-1097(95)00314-2. [DOI] [PubMed] [Google Scholar]
- 24.Khattar RS, Senior R, Lahiri A. Assessment of myocardial perfusion and contractile function by inotropic stress Tc-99m sestamibi SPECT imaging and echocardiography for optimal detection of multivessel coronary artery disease. Heart. 1998;79(3):274–80. doi: 10.1136/hrt.79.3.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McClellan JR, Dugan TM, Heller GV. Patterns of use and clinical utility of exercise thallium-201 single photon emission-computed tomography in a community hospital. Cardiology. 1996;87(2):134–40. doi: 10.1159/000177076. [DOI] [PubMed] [Google Scholar]
- 26.Michaelides AP, Psomadaki ZD, Dilaveris PE, Richter DJ, Andrikopoulos GK, Aggeli KD, et al. Improved detection of coronary artery disease by exercise electrocardiography with the use of right precordial leads. N Engl J Med. 1999;340(5):340–5. doi: 10.1056/NEJM199902043400502. [DOI] [PubMed] [Google Scholar]
- 27.Nallamothu N, Ghods M, Heo J, Iskandrian AS. Comparison of thallium-201 single-photon emission computed tomography and electrocardiographic response during exercise in patients with normal rest electrocardiographic results. J Am Coll Cardiol. 1995;25(4):830–6. doi: 10.1016/0735-1097(94)00471-2. [DOI] [PubMed] [Google Scholar]
- 28.Psirropoulos D, Efthimiadis A, Boudonas G, Papadopoulos I, Papadopoulos G, Ekklisiarchos D, et al. Detection of myocardial ischemia in the elderly versus the young by stress thallium-201 scintigraphy and its relation to important coronary artery disease. Heart Vessels. 2002;16(4):131–6. doi: 10.1007/s003800200009. [DOI] [PubMed] [Google Scholar]
- 29.Shirai N, Yamagishi H, Yoshiyama M, Teragaki M, Akioka K, Takeuchi K, et al. Incremental value of assessment of regional wall motion for detection of multivessel coronary artery disease in exercise (201)Tl gated myocardial perfusion imaging. J Nucl Med. 2002;43(4):443–50. [PubMed] [Google Scholar]
- 30.Santana-Boado C, Candell-Riera J, Castell-Conesa J, guade-Bruix S, Garcia-Burillo A, Canela T, et al. Diagnostic accuracy of technetium-99m-MIBI myocardial SPECT in women and men. J Nucl Med. 1998;39(5):751–5. [PubMed] [Google Scholar]
- 31.Gallowitsch HJ, Sykora J, Mikosch P, Kresnik E, Unterweger O, Molnar M, et al. Attenuation-corrected thallium-201 single-photon emission tomography using a gadolinium-153 moving line source: clinical value and the impact of attenuation correction on the extent and severity of perfusion abnormalities. Eur J Nucl Med. 1998;25(3):220–8. doi: 10.1007/s002590050220. [DOI] [PubMed] [Google Scholar]
- 32.Heiba SI, Hayat NJ, Salman HS, Higazy E, Sayed ME, Saleh Z, et al. Technetium-99m-MIBI myocardial SPECT: supine versus right lateral imaging and comparison with coronary arteriography. J Nucl Med. 1997;38(10):1510–4. [PubMed] [Google Scholar]
- 33.Palmas W, Friedman JD, Diamond GA, Silber H, Kiat H, Berman DS. Incremental value of simultaneous assessment of myocardial function and perfusion with technetium-99m sestamibi for prediction of extent of coronary artery disease. J Am Coll Cardiol. 1995;25(5):1024–31. doi: 10.1016/0735-1097(94)00523-s. [DOI] [PubMed] [Google Scholar]
- 34.Rubello D, Zanco P, Candelpergher G, Borsato N, Chierichetti F, Saitta B, et al. Usefulness of 99mTc-MIBI stress myocardial SPECT bull’s-eye quantification in coronary artery disease. Q J Nucl Med. 1995;39(2):111–5. [PubMed] [Google Scholar]
- 35.Taillefer R, Depuey EG, Udelson JE, Beller GA, Latour Y, Reeves F. Comparative diagnostic accuracy of Tl-201 and Tc-99m sestamibi SPECT imaging (perfusion and ECG-gated SPECT) in detecting coronary artery disease in women. J Am Coll Cardiol. 1997;29(1):69–77. doi: 10.1016/s0735-1097(96)00435-4. [DOI] [PubMed] [Google Scholar]
- 36.Amanullah AM, Berman DS, Kiat H, Friedman JD. Usefulness of hemodynamic changes during adenosine infusion in predicting the diagnostic accuracy of adenosine technetium-99m sestamibi single-photon emission computed tomography (SPECT) Am J Cardiol. 1997;79(10):1319–22. doi: 10.1016/s0002-9149(97)00132-x. [DOI] [PubMed] [Google Scholar]
- 37.Di B V, Bellina CR, Gori E, Molea N, Talarico L, Boni G, et al. Incremental diagnostic value of dobutamine stress echocardiography and dobutamine scintigraphy (technetium 99m-labeled sestamibi single-photon emission computed tomography) for assessment of presence and extent of coronary artery disease. J Nucl Cardiol. 1996;3(3):212–20. doi: 10.1016/s1071-3581(96)90035-5. [DOI] [PubMed] [Google Scholar]
- 38.Elhendy A, Van Domburg RT, Bax JJ, Nierop PR, Geleijnse ML, Ibrahim MM, et al. Noninvasive diagnosis of coronary artery stenosis in women with limited exercise capacity: comparison of dobutamine stress echocardiography and 99mTc sestamibi single-photon emission CT. Chest. 1998;114(4):1097–104. doi: 10.1378/chest.114.4.1097. [DOI] [PubMed] [Google Scholar]
- 39.Ho FM, Huang PJ, Liau CS, Lee FK, Chieng PU, Su CT, et al. Dobutamine stress echocardiography compared with dipyridamole thallium-201 single-photon emission computed tomography in detecting coronary artery disease. Eur Heart J. 1995;16(4):570–5. doi: 10.1093/oxfordjournals.eurheartj.a060952. [DOI] [PubMed] [Google Scholar]
- 40.Ho YL, Wu CC, Huang PJ, Tseng WK, Lin LC, Chieng PU, et al. Dobutamine stress echocardiography compared with exercise thallium-201 single-photon emission computed tomography in detecting coronary artery disease-effect of exercise level on accuracy. Cardiology. 1997;88(4):379–85. doi: 10.1159/000177363. [DOI] [PubMed] [Google Scholar]
- 41.Huang PJ, Yen RF, Chieng PU, Chen ML, Su CT. Do beta-blockers affect the diagnostic sensitivity of dobutamine stress thallium-201 single photon emission computed tomographic imaging? J Nucl Cardiol. 1998;5(1):34–9. doi: 10.1016/s1071-3581(98)80008-1. [DOI] [PubMed] [Google Scholar]
- 42.Huang PJ, Ho YL, Wu CC, Chao CL, Chen MF, Chieng PU, et al. Simultaneous dobutamine stress echocardiography and thallium-201 perfusion imaging for the detection of coronary artery disease. Cardiology. 1997;88(6):556–62. doi: 10.1159/000177419. [DOI] [PubMed] [Google Scholar]
- 43.Miller DD, Younis LT, Chaitman BR, Stratmann H. Diagnostic accuracy of dipyridamole technetium 99m-labeled sestamibi myocardial tomography for detection of coronary artery disease. J Nucl Cardiol. 1997;4(1 Pt 1):18–24. doi: 10.1016/s1071-3581(97)90045-3. [DOI] [PubMed] [Google Scholar]
- 44.Mohiuddin SM, Ravage CK, Esterbrooks DJ, Lucas BD Jr, Hilleman DE. The comparative safety and diagnostic accuracy of adenosine myocardial perfusion imaging in women versus men. Pharmacotherapy. 1996;16(4):646–51. [PubMed] [Google Scholar]
- 45.San Roman JA, Vilacosta I, Castillo JA, Rollan MJ, Hernandez M, Peral V, et al. Selection of the optimal stress test for the diagnosis of coronary artery disease. Heart. 1998;80(4):370–6. doi: 10.1136/hrt.80.4.370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Santoro GM, Sciagra R, Buonamici P, Consoli N, Mazzoni V, Zerauschek F, et al. Head-to-head comparison of exercise stress testing, pharmacologic stress echocardiography, and perfusion tomography as first-line examination for chest pain in patients without history of coronary artery disease. J Nucl Cardiol. 1998;5(1):19–27. doi: 10.1016/s1071-3581(98)80006-8. [DOI] [PubMed] [Google Scholar]
- 47.Schillaci O, Moroni C, Scopinaro F, Tavolaro R, Danieli R, Bossini A, et al. Technetium-99m sestamibi myocardial tomography based on dipyridamole echocardiography testing in hypertensive patients with chest pain. Eur J Nucl Med. 1997;24(7):774–8. doi: 10.1007/BF00879666. [DOI] [PubMed] [Google Scholar]
- 48.Slavich GA, Guerra UP, Morocutti G, Fioretti PM, Fresco C, Orlandi C, et al. Feasibility of simultaneous Tc99m sestamibi and 2D-echo cardiac imaging during dobutamine pharmacologic stress Preliminary results in a female population. Int J Card Imaging. 1996;12(2):113–8. doi: 10.1007/BF01880742. [DOI] [PubMed] [Google Scholar]
- 49.Soman P, Khattar R, Senior R, Lahiri A. Inotropic stress with arbutamine is superior to vasodilator stress with dipyridamole for the detection of reversible ischemia with Tc-99m sestamibi single-photon emission computed tomography. J Nucl Cardiol. 1997;4(5):364–71. doi: 10.1016/s1071-3581(97)90027-1. [DOI] [PubMed] [Google Scholar]
- 50.Takeuchi M, Sonoda S, Miura Y, Kuroiwa A. Comparative diagnostic value of dobutamine stress echocardiography and stress thallium-201 single-photon-emission computed tomography for detecting coronary artery disease in women. Coron Artery Dis. 1996;7(11):831–5. doi: 10.1097/00019501-199611000-00007. [DOI] [PubMed] [Google Scholar]
- 51.Watanabe K, Sekiya M, Ikeda S, Miyagawa M, Kinoshita M, Kumano S. Comparison of adenosine triphosphate and dipyridamole in diagnosis by thallium-201 myocardial scintigraphy. J Nucl Med. 1997;38(4):577–81. [PubMed] [Google Scholar]
- 52.Fragasso G, Lu C, Dabrowski P, Pagnotta P, Sheiban I, Chierchia SL. Comparison of stress/rest myocardial perfusion tomography, dipyridamole and dobutamine stress echocardiography for the detection of coronary disease in hypertensive patients with chest pain and positive exercise test. J Am Coll Cardiol. 1999;34(2):441–7. doi: 10.1016/s0735-1097(99)00231-4. [DOI] [PubMed] [Google Scholar]
- 53.Astarita C, Palinkas A, Nicolai E, Maresca FS, Varga A, Picano E. Dipyridamole-atropine stress echocardiography versus exercise SPECT scintigraphy for detection of coronary artery disease in hypertensives with positive exercise test. J Hypertens. 2001;19(3):495–502. doi: 10.1097/00004872-200103000-00018. [DOI] [PubMed] [Google Scholar]
- 54.Cramer MJ, van der Wall EE, Jaarsma W, Verzijlbergen JF, Niemeyer MG, Zwinderman AH, et al. Detection of coronary artery disease: comparison between technetium 99m-labeled sestamibi single-photon emission computed tomography and two-dimensional echocardiography with dipyridamole low-level exercise-stress. J Nucl Cardiol. 1996;3(5):389–94. doi: 10.1016/s1071-3581(96)90073-2. [DOI] [PubMed] [Google Scholar]
- 55.Ogilby JD, Kegel JG, Heo J, Iskandrian AE. Correlation between hemodynamic changes and tomographic sestamibi imaging during dipyridamole-induced coronary hyperemia. J Am Coll Cardiol. 1998;31(1):75–82. doi: 10.1016/s0735-1097(97)00448-8. [DOI] [PubMed] [Google Scholar]
- 56.Ficaro EP, Fessler JA, Shreve PD, Kritzman JN, Rose PA, Corbett JR. Simultaneous transmission/emission myocardial perfusion tomography. Circulation. 1996;93(3):463–73. doi: 10.1161/01.cir.93.3.463. Diagnostic accuracy of attenuation-corrected 99mTc-sestamibi single-photon emission computed tomography. [DOI] [PubMed] [Google Scholar]
- 57.Iftikhar I, Koutelou M, Mahmarian JJ, Verani MS. Simultaneous perfusion tomography and radionuclide angiography during dobutamine stress. J Nucl Med. 1996;37(8):1306–10. [PubMed] [Google Scholar]
- 58.Kisacik HL, Ozdemir K, Altinyay E, Oguzhan A, Kural T, Kir M, et al. Comparison of exercise stress testing with simultaneous dobutamine stress echocardiography and technetium-99m isonitrile single-photon emission computerized tomography for diagnosis of coronary artery disease. Eur Heart J. 1996;17(1):113–9. doi: 10.1093/oxfordjournals.eurheartj.a014669. [DOI] [PubMed] [Google Scholar]
- 59.Benoit T, Vivegnis D, Lahiri A, Itti R, Braat S, Rigo P. Tomographic myocardial imaging with technetium-99m tetrofosmin. Comparison with tetrofosmin and thallium planar imaging and with angiography. Eur Heart J. 1996;17(4):635–42. doi: 10.1093/oxfordjournals.eurheartj.a014919. [DOI] [PubMed] [Google Scholar]
- 60.Links JM, Becker LC, Rigo P, Taillefer R, Hanelin L, Anstett F, et al. Combined corrections for attenuation, depth-dependent blur, and motion in cardiac SPECT: a multicenter trial. J Nucl Cardiol. 2000;7(5):414–25. doi: 10.1067/mnc.2000.108350. [DOI] [PubMed] [Google Scholar]
- 61.Emmett L, Iwanochko RM, Freeman MR, Barolet A, Lee DS, Husain M. Reversible regional wall motion abnormalities on exercise technetium-99m-gated cardiac single photon emission computed tomography predict high-grade angiographic stenoses. J Am Coll Cardiol. 2002;39(6):991–8. doi: 10.1016/s0735-1097(02)01707-2. [DOI] [PubMed] [Google Scholar]
- 62.He Q, Yao Z, Yu X, Qu W, Sun F, Ji F, et al. Evaluation of 99mTc-MIBI myocardial perfusion imaging with intravenous infusion of adenosine triphosphate in diagnosis of coronary artery disease. Chin Med J (Engl) 2002;115(11):1603–7. [PubMed] [Google Scholar]
- 63.He ZX, Shi RF, Wu YJ, Tian YQ, Liu XJ, Wang SW, et al. Direct imaging of exercise-induced myocardial ischemia with fluorine-18-labeled deoxyglucose and Tc-99m-sestamibi in coronary artery disease. Circulation. 2003;108(10):1208–13. doi: 10.1161/01.CIR.0000088784.25089.D9. [see comment] [DOI] [PubMed] [Google Scholar]
- 64.Lima RS, Watson DD, Goode AR, Siadaty MS, Ragosta M, Beller GA, et al. Incremental value of combined perfusion and function over perfusion alone by gated SPECT myocardial perfusion imaging for detection of severe three-vessel coronary artery disease. J Am Coll Cardiol. 2003;42(1):64–70. doi: 10.1016/s0735-1097(03)00562-x. [DOI] [PubMed] [Google Scholar]
- 65.Rollan MJ, San Roman JA, Vilacosta I, Ramon OJ, Bratos JL. Dobutamine stress echocardiography in the diagnosis of coronary artery disease in women with chest pain: Comparison with different noninvasive tests. Clin Cardiol. 2002;25(12):559–64. doi: 10.1002/clc.4950251205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tsai M-F, Kao P-F, Tzen K-Y. Improved diagnostic performance of thallium-201 myocardial perfusion scintigraphy in coronary artery disease: From planar to single photon emission computed tomography imaging. Chang Gung Medical Journal. 2002;25(8):522–30. [PubMed] [Google Scholar]
- 67.Groutars RGEJ, Verzijlbergen JF, Tiel-Van Buul MMC, Zwinderman AH, Ascoop CAPL, van Hemel NM, et al. The accuracy of 1-day dual-isotope myocardial SPECT in a population with high prevalence of coronary artery disease. Int J Cardiovasc Imaging. 2003;19(3):229–38. doi: 10.1023/a:1023637804898. [DOI] [PubMed] [Google Scholar]
- 68.Hannoush H, Shaar K, Alam S, Nasrallah A, Sawaya J, Dakik HA. Analysis of referral patterns, predictive accuracy, and impact on patient management of myocardial perfusion imaging in a new nuclear cardiology laboratory. J Nucl Cardiol. 2003;10(2):148–53. doi: 10.1067/mnc.2003.397. [DOI] [PubMed] [Google Scholar]
- 69.Shelley S, Sathyamurthy I, Madhavan, Subramanyan K, Najeeb OM, Ramachandran P. Adenosine myocardial SPECT--its efficacy and safety and correlation with coronary angiogram. J Assoc Physicians India. 2003;51:557–60. [PubMed] [Google Scholar]
- 70.Dondi M, Fagioli G, Salgarello M, Zoboli S, Nanni C, Cidda C. Myocardial SPECT: what do we gain from attenuation correction (and when)? Q J Nucl Med Mol Imaging. 2004;48(3):181–7. [PubMed] [Google Scholar]
- 71.Grossman GB, Garcia EV, Bateman TM, Heller GV, Johnson LL, Folks RD, et al. Quantitative Tc-99m sestamibi attenuation-corrected SPECT: development and multicenter trial validation of myocardial perfusion stress gender-independent normal database in an obese population. J Nucl Cardiol. 2004;11(3):263–72. doi: 10.1016/j.nuclcard.2004.02.007. [DOI] [PubMed] [Google Scholar]
- 72.Hambye AS, Vervaet AM, Dobbeleir AA. Head-to-head comparison of uncorrected and scatter corrected, summed and end diastolic myocardial perfusion SPECT in coronary artery disease. Nucl Med Commun. 2004;25(4):347–53. doi: 10.1097/00006231-200404000-00006. [DOI] [PubMed] [Google Scholar]
- 73.Patsilinakos SP, Spanodimos S, Rontoyanni F, Kranidis A, Antonelis IP, Sotirellos K, et al. Adenosine stress myocardial perfusion tomographic imaging in patients with significant aortic stenosis. J Nucl Cardiol. 2004;11(1):20–5. doi: 10.1016/j.nuclcard.2003.10.003. [DOI] [PubMed] [Google Scholar]
- 74.Peltier M, Vancraeynest D, Pasquet A, Ay T, Roelants V, D’Hondt AM, et al. Assessment of the physiologic significance of coronary disease with dipyridamole real-time myocardial contrast echocardiography. J Am Coll Cardiol. 2004;43(2):257–64. doi: 10.1016/j.jacc.2003.07.040. Comparison with technetium-99m sestamibi single-photon emission computed tomography and quantitative coronary angiography. [DOI] [PubMed] [Google Scholar]
- 75.Senior R, Lepper W, Pasquet A, Chung G, Hoffman R, Vanoverschelde JL, et al. Myocardial perfusion assessment in patients with medium probability of coronary artery disease and no prior myocardial infarction: comparison of myocardial contrast echocardiography with 99mTc single-photon emission computed tomography. Am Heart J. 2004;147(6):1100–5. doi: 10.1016/j.ahj.2003.12.030. [DOI] [PubMed] [Google Scholar]
- 76.Yao ZM, Li W, Qu WY, Zhou C, He Q, Ji FS. Comparison of (99)mTc-methoxyisobutylisonitrile myocardial single-photon emission computed tomography and electron beam computed tomography for detecting coronary artery disease in patients with no myocardial infarction. Chin Med J (Engl) 2004;117(5):700–5. [PubMed] [Google Scholar]
- 77.Gonzalez P, Massardo T, Jofre MJ, Yovanovich J, Prat H, Munoz A, et al. 201Tl myocardial SPECT detects significant coronary artery disease between 50% and 75% angiogram stenosis. Rev Esp Med Nucl. 2005;24(5):305–11. doi: 10.1157/13079281. [DOI] [PubMed] [Google Scholar]
- 78.Johansen A, Hoilund-Carlsen PF, Christensen HW, Vach W, Jorgensen HB, Veje A, et al. Diagnostic accuracy of myocardial perfusion imaging in a study population without post-test referral bias. J Nucl Cardiol. 2005;12(5):530–7. doi: 10.1016/j.nuclcard.2005.04.012. [DOI] [PubMed] [Google Scholar]
- 79.Masood Y, Liu YH, DePuey G, Taillefer R, Araujo LI, Allen S, et al. Clinical validation of SPECT attenuation correction using x-ray computed tomography-derived attenuation maps: multicenter clinical trial with angiographic correlation. J Nucl Cardiol. 2005;12(6):676–86. doi: 10.1016/j.nuclcard.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 80.Sakuma H, Suzawa N, Ichikawa Y, Makino K, Hirano T, Kitagawa K, et al. Diagnostic accuracy of stress first-pass contrast-enhanced myocardial perfusion MRI compared with stress myocardial perfusion scintigraphy. AJR Am J Roentgenol. 2005;185(1):95–102. doi: 10.2214/ajr.185.1.01850095. [DOI] [PubMed] [Google Scholar]
- 81.Thompson RC, Heller GV, Johnson LL, Case JA, Cullom SJ, Garcia EV, et al. Value of attenuation correction on ECG-gated SPECT myocardial perfusion imaging related to body mass index. J Nucl Cardiol. 2005;12(2):195–202. doi: 10.1016/j.nuclcard.2004.12.298. [DOI] [PubMed] [Google Scholar]
- 82.Berman DS, Kang X, Nishina H, Slomka PJ, Shaw LJ, Hayes SW, et al. Diagnostic accuracy of gated Tc-99m sestamibi stress myocardial perfusion SPECT with combined supine and prone acquisitions to detect coronary artery disease in obese and nonobese patients. J Nucl Cardiol. 2006;13(2):191–201. doi: 10.1007/BF02971243. [DOI] [PubMed] [Google Scholar]
- 83.Elhendy A, Schinkel AFL, Bax JJ, Van Domburg RT, Valkema R, Biagini E, et al. Accuracy of stress Tc-99m tetrofosmin myocardial perfusion tomography for the diagnosis and localization of coronary artery disease in women. J Nucl Cardiol. 2006;13(5):629–34. doi: 10.1016/j.nuclcard.2006.06.128. [DOI] [PubMed] [Google Scholar]
- 84.Hung GU, Lee KW, Chen CP, Yang KT, Lin WY. Worsening of left ventricular ejection fraction induced by dipyridamole on Tl-201 gated myocardial perfusion imaging predicts significant coronary artery disease. J Nucl Cardiol. 2006;13(2):225–32. doi: 10.1007/BF02971247. [DOI] [PubMed] [Google Scholar]
- 85.Jeetley P, Hickman M, Kamp O, Lang RM, Thomas JD, Vannan MA, et al. Myocardial contrast echocardiography for the detection of coronary artery stenosis: a prospective multicenter study in comparison with single-photon emission computed tomography. J Am Coll Cardiol. 2006;47(1):141–5. doi: 10.1016/j.jacc.2005.08.054. [DOI] [PubMed] [Google Scholar]
- 86.Korosoglou G, Dubart AE, DaSilva KG Jr, Labadze N, Hardt S, Hansen A, et al. Real-time myocardial perfusion imaging for pharmacologic stress testing: added value to single photon emission computed tomography. Am Heart J. 2006;151(1):131–8. doi: 10.1016/j.ahj.2005.02.046. [DOI] [PubMed] [Google Scholar]
- 87.Lin SL, Chiou KR, Huang WC, Peng NJ, Tsay DG, Liu CP. Detection of coronary artery disease using real-time myocardial contrast echocardiography: a comparison with dual-isotope resting thallium-201/stress technectium-99m sestamibi single-photon emission computed tomography. Heart and Vessels. 2006;21(4):226–35. doi: 10.1007/s00380-005-0890-0. [DOI] [PubMed] [Google Scholar]
- 88.Matsumoto N, Sato Y, Suzuki Y, Yoda S, Kunimasa T, Kato M, et al. Usefulness of rapid low-dose/high-dose 1-day 99mTc-sestamibi ECG-gated myocardial perfusion single-photon emission computed tomography. Circ J. 2006;70(12):1585–9. doi: 10.1253/circj.70.1585. [DOI] [PubMed] [Google Scholar]
- 89.Slomka PJ, Fish MB, Lorenzo S, Nishina H, Gerlach J, Berman DS, et al. Simplified normal limits and automated quantitative assessment for attenuation-corrected myocardial perfusion SPECT. J Nucl Cardiol. 2006;13(5):642–51. doi: 10.1016/j.nuclcard.2006.06.131. [DOI] [PubMed] [Google Scholar]
- 90.Aggeli C, Christoforatou E, Giannopoulos G, Roussakis G, Kokkinakis C, Barbetseas J, et al. The diagnostic value of adenosine stress-contrast echocardiography for diagnosis of coronary artery disease in hypertensive patients: comparison to Tl-201 single-photon emission computed tomography. Am J Hypertens. 2007;20(5):533–8. doi: 10.1016/j.amjhyper.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 91.Banzo I, Pena FJ, Allende RH, Quirce R, Carril JM. Prospective clinical comparison of non-corrected and attenuation- and scatter-corrected myocardial perfusion SPECT in patients with suspicion of coronary artery disease. Nucl Med Commun. 2003;24(9):995–1002. doi: 10.1097/00006231-200309000-00008. [DOI] [PubMed] [Google Scholar]
- 92.Mieres JH, Makaryus AN, Cacciabaudo JM, Donaldson D, Green SJ, Heller GV, et al. Value of electrocardiographically gated single-photon emission computed tomographic myocardial perfusion scintigraphy in a cohort of symptomatic postmenopausal women. Am J Cardiol. 2007;99(8):1096–9. doi: 10.1016/j.amjcard.2006.12.024. [DOI] [PubMed] [Google Scholar]
- 93.Schepis T, Gaemperli O, Koepfli P, Namdar M, Valenta I, Scheffel H, et al. Added value of coronary artery calcium score as an adjunct to gated SPECT for the evaluation of coronary artery disease in an intermediate-risk population. J Nucl Med. 2007;48(9):1424–30. doi: 10.2967/jnumed.107.040758. [DOI] [PubMed] [Google Scholar]
- 94.Yeih DF, Huang PJ, Ho YL. Enhanced diagnosis of coronary artery disease in women by dobutamine thallium-201 ST-segment/heart rate slope and thallium-201 myocardial SPECT. J Formos Med Assoc. 2007;106(10):832–9. doi: 10.1016/S0929-6646(08)60048-0. [DOI] [PubMed] [Google Scholar]
- 95.Bokhari S, Shahzad A, Bergmann SR. Superiority of exercise myocardial perfusion imaging compared with the exercise ECG in the diagnosis of coronary artery disease. Coron Artery Dis. 2008;19(6):399–404. doi: 10.1097/MCA.0b013e3283021ab4. [DOI] [PubMed] [Google Scholar]
- 96.Katayama T, Ogata N, Tsuruya Y. Diagnostic accuracy of supine and prone thallium-201 stress myocardial perfusion single-photon emission computed tomography to detect coronary artery disease in inferior wall of left ventricle. Ann Nucl Med. 2008;22(4):317–21. doi: 10.1007/s12149-008-0118-3. [DOI] [PubMed] [Google Scholar]
- 97.Lipiec P, Wejner-mik P, Krzeminska-pakula M, Kusmierek J, Plachcinska A, Szuminski R, et al. Accelerated stress real-time myocardial contrast echocardiography for the detection of coronary artery disease: comparison with 99mTc single photon emission computed tomography. J Am Soc Echocardiogr. 2008;21(8):941–7. doi: 10.1016/j.echo.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 98.Suzuki Y, Slomka PJ, Wolak A, Ohba M, Suzuki S, De YL, et al. Motion-frozen myocardial perfusion SPECT improves detection of coronary artery disease in obese patients. J Nucl Med. 2008;49(7):1075–9. doi: 10.2967/jnumed.108.050997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Tadehara F, Yamamoto H, Tsujiyama S, Hinoi T, Matsuo S, Matsumoto N, et al. Feasibility of a rapid protocol of 1-day single-isotope rest/adenosine stress Tc-99m sestamibi ECG-gated myocardial perfusion imaging. J Nucl Cardiol. 2008;15(1):35–41. doi: 10.1016/j.nuclcard.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 100.Hida S, Chikamori T, Tanaka H, Igarashi Y, Hatano T, Usui Y, et al. Diagnostic value of left ventricular function after adenosine triphosphate loading and at rest in the detection of multi-vessel coronary artery disease using myocardial perfusion imaging. J Nucl Cardiol. 2009;16(1):20–7. doi: 10.1007/s12350-008-9003-7. [DOI] [PubMed] [Google Scholar]
- 101.Wu MC, Chin KC, Lin KH, Chiu NT. Diagnostic efficacy of a low-dose 32-projection SPECT 99mTc-sestamibi myocardial perfusion imaging protocol in routine practice. Nucl Med Commun. 2009;30(2):140–7. doi: 10.1097/MNM.0b013e328319e65f. [DOI] [PubMed] [Google Scholar]
- 102.Yoon AJ, Melduni RM, Duncan SA, Ostfeld RJ, Travin MI. The effect of beta-blockers on the diagnostic accuracy of vasodilator pharmacologic SPECT myocardial perfusion imaging. J Nucl Cardiol. 2009;16(3):358–67. doi: 10.1007/s12350-009-9066-0. [DOI] [PubMed] [Google Scholar]
- 103.Wolak A, Slomka PJ, Fish MB, Lorenzo S, Berman DS, Germano G. Quantitative diagnostic performance of myocardial perfusion SPECT with attenuation correction in women. J Nucl Med. 2008;49(6):915–22. doi: 10.2967/jnumed.107.049387. [DOI] [PubMed] [Google Scholar]
- 104.Wolak A, Slomka PJ, Fish MB, Lorenzo S, Acampa W, Berman DS, et al. Quantitative myocardial-perfusion SPECT: comparison of three state-of-the-art software packages. J Nucl Cardiol. 2008;15(1):27–34. doi: 10.1016/j.nuclcard.2007.09.020. [DOI] [PubMed] [Google Scholar]
- 105.Chammas E, Yatim A, Hage C, Sokhn K, Tarcha W, Ghanem G. Evaluation of Tc-99m tetrofosmin scan for coronary artery disease diagnosis. Asian Cardiovasc Thorac Ann. 2002;10(3):244–7. doi: 10.1177/021849230201000312. [DOI] [PubMed] [Google Scholar]
- 106.Goodman C. Literature searching and evidence interpretation for assessing health care practices. Stockholm Sweden: Swedish Council on Technology Assessment in Health Care. 1996 doi: 10.1017/s0266462300008321. SBU Report No. 119E. [DOI] [PubMed] [Google Scholar]
- 107.Thompson RC, Cullom SJ. Issues regarding radiation dosage of cardiac nuclear and radiography procedures. J Nucl Cardiol. 2006;13(1):19–23. doi: 10.1016/j.nuclcard.2005.11.004. [DOI] [PubMed] [Google Scholar]
- 108.U.S. Food and Drug Administration. What are the radiation risks from CT? [Internet] [updated 2009 Jun 8; cited 2009 Dec 14] Available from: http://www.fda.gov/Radiation-EmittingProducts/RadiationEmittingProductsandProcedures/MedicalImaging/MedicalX-Rays/ucm115329.htm .
- 109.National Research Council. Health risks from exposure to low levels of ionizing radiation: Beir VII phase 2. Washington, D.C.: The National Academies Press. 2006 [PubMed] [Google Scholar]
- 110.Scottish Intercollegiate Guidelines Network. Management of stable angina. A national clinical guideline. [Internet] [updated 2007; cited 2009 Oct 28] Available from: http://www.guideline.gov/summary/summary.aspx?ss=15&doc_id=10584 .
- 111.Fraker TD Jr, Fihn SD, Gibbons RJ, Abrams J, Chatterjee K, Daley J, et al. 2007 chronic angina focused update of the ACC/AHA 2002 guidelines for the management of patients with chronic stable angina: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines Writing Group to develop the focused update of the 2002 guidelines for the management of patients with chronic stable angina. J Am Coll Cardiol. 2007;50(23):2264–74. doi: 10.1016/j.jacc.2007.08.002. [DOI] [PubMed] [Google Scholar]
- 112.Ontario Case Costing Initiative. Costing analysis tool (CAT) [Internet] [updated 2009; cited 2009 Nov 18] Available from: http://www.occp.com/
- 113.Ontario Ministry of Health and Long-Term Care. Ontario health insurance schedule of benefits and fees. [Internet] [updated 2009; cited 2009 Nov 24] Available from: http://www.health.gov.on.ca/english/providers/program/ohip/sob/sob_mn.html .
- 114.Hayashino Y, Shimbo T, Tsujii S, Ishii H, Kondo H, Nakamura T, et al. Cost-effectiveness of coronary artery disease screening in asymptomatic patients with type 2 diabetes and other atherogenic risk factors in Japan: factors influencing on international application of evidence-based guidelines. Int J Cardiol. 2007;118(1):88–96. doi: 10.1016/j.ijcard.2006.03.086. [DOI] [PubMed] [Google Scholar]
- 115.Kreisz FP, Merlin T, Moss J, Atherton J, Hiller JE, Gericke CA. The pre-test risk stratified cost-effectiveness of 64-slice computed tomography coronary angiography in the detection of significant obstructive coronary artery disease in patients otherwise referred to invasive coronary angiography. Heart, Lung & Circulation. 2009;18(3):200–7. doi: 10.1016/j.hlc.2008.10.013. [DOI] [PubMed] [Google Scholar]
- 116.Ladapo JA, Hoffmann U, Bamberg F, Nagurney JT, Cutler DM, Weinstein MC, et al. Cost-effectiveness of coronary MDCT in the triage of patients with acute chest pain. AJR American journal of roentgenology. 2008;191(2):455–63. doi: 10.2214/AJR.07.3611. [DOI] [PubMed] [Google Scholar]
- 117.Lorenzoni R, Cortigiani L, Magnani M, Desideri A, Bigi R, Manes C, et al. Cost-effectiveness analysis of noninvasive strategies to evaluate patients with chest pain. J Am Soc Echocardiogr. 2003;16(12):1287–91. doi: 10.1067/j.echo.2003.07.007. [DOI] [PubMed] [Google Scholar]
- 118.Maddahi J, Gambhir SS. Cost-effective selection of patients for coronary angiography. J Nucl Cardiol. 1997;4(2):S141–S151. doi: 10.1016/s1071-3581(97)90093-3. [DOI] [PubMed] [Google Scholar]
- 119.Medical, Advisory Secretariat. Positron emission tomography for the assessment of myocardial viability. Toronto: Ontario Ministry of Health and Long-Term Care. 2005 [Google Scholar]
- 120.Moir S, Shaw L, Haluska B, Jenkins C, Marwick TH. Left ventricular opacification for the diagnosis of coronary artery disease with stress echocardiography: an angiographic study of incremental benefit and cost-effectiveness. Am Heart J. 2007;154(3):510–8. doi: 10.1016/j.ahj.2007.04.046. [DOI] [PubMed] [Google Scholar]
- 121.Paterson DI, Schwartzman K. Strategies incorporating spiral CT for the diagnosis of acute pulmonary embolism: a cost-effectiveness analysis. Chest. 2001;119(6):1791–800. doi: 10.1378/chest.119.6.1791. [DOI] [PubMed] [Google Scholar]
- 122.Shaw LJ, Monaghan MJ, Nihoyannopolous P. Clinical and economic outcomes assessment with myocardial contrast echocardiography. Heart. 1999;3(82 Suppl):III16–III21. doi: 10.1136/hrt.82.2008.iii16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Wyrick JJ, Kalvaitis S, McConnell KJ, Rinkevich D, Kaul S, Wei K. Cost-efficiency of myocardial contrast echocardiography in patients presenting to the emergency department with chest pain of suspected cardiac origin and a nondiagnostic electrocardiogram. Am J Cardiol. 2008;102(6):649–52. doi: 10.1016/j.amjcard.2008.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Yong Y, Wu D, Fernandes V, Kopelen HA, Shimoni S, Nagueh SF, et al. Diagnostic accuracy and cost-effectiveness of contrast echocardiography on evaluation of cardiac function in technically very difficult patients in the intensive care unit. Am J Cardiol. 2002;89(6):711–8. doi: 10.1016/s0002-9149(01)02344-x. [DOI] [PubMed] [Google Scholar]
- 125.Bedetti G, Pasanisi EM, Pizzi C, Turchetti G, Lore C. Economic analysis including long-term risks and costs of alternative diagnostic strategies to evaluate patients with chest pain. Cardiovasc Ultrasound. 2008:6–21. doi: 10.1186/1476-7120-6-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Dewey M, Hamm B. Cost effectiveness of coronary angiography and calcium scoring using CT and stress MRI for diagnosis of coronary artery disease. Eur Radiol. 2007;17(5):1301–9. doi: 10.1007/s00330-006-0439-3. [DOI] [PubMed] [Google Scholar]
- 127.Garber AM, Solomon NA. Cost-effectiveness of alternative test strategies for the diagnosis of coronary artery disease. Ann Intern Med. 1999;130(9):719–28. doi: 10.7326/0003-4819-130-9-199905040-00003. [DOI] [PubMed] [Google Scholar]
- 128.Hayashino Y, Nagata-Kobayashi S, Morimoto T, Maeda K, Shimbo T, Fukui T. Cost-effectiveness of screening for coronary artery disease in asymptomatic patients with Type 2 diabetes and additional atherogenic risk factors. J Gen Intern Med. 2004;19(12):1181–91. doi: 10.1111/j.1525-1497.2004.40012.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Hernandez R, Vale L. The value of myocardial perfusion scintigraphy in the diagnosis and management of angina and myocardial infarction: a probabilistic economic analysis. Med Decis Making. 2007;27(6):772–88. doi: 10.1177/0272989X07306111. [DOI] [PubMed] [Google Scholar]
- 130.Khare RK, Courtney DM, Powell ES, Venkatesh AK, Lee TA. Sixty-four-slice computed tomography of the coronary arteries: cost-effectiveness analysis of patients presenting to the emergency department with low-risk chest pain. Acad Emerg Med. 2008;15(7):623–32. doi: 10.1111/j.1553-2712.2008.00161.x. [DOI] [PubMed] [Google Scholar]
- 131.Kuntz KM, Fleischmann KE, Hunink MG, Douglas PS. Cost-effectiveness of diagnostic strategies for patients with chest pain. Ann Intern Med. 1999;130(9):709–18. doi: 10.7326/0003-4819-130-9-199905040-00002. [DOI] [PubMed] [Google Scholar]
- 132.Lee DS, Jang MJ, Cheon GJ, Chung JK, Lee MC. Comparison of the cost-effectiveness of stress myocardial SPECT and stress echocardiography in suspected coronary artery disease considering the prognostic value of false-negative results. J Nucl Cardiol. 2002;9(5):515–22. doi: 10.1067/mnc.2002.125217. [DOI] [PubMed] [Google Scholar]
- 133.Rumberger JA, Behrenbeck T, Breen JF, Sheedy PF. Coronary calcification by electron beam computed tomography and obstructive coronary artery disease: a model for costs and effectiveness of diagnosis as compared with conventional cardiac testing methods. J Am Coll Cardiol. 1999;33(2):453–62. doi: 10.1016/s0735-1097(98)00583-x. [DOI] [PubMed] [Google Scholar]
- 134.Sharples L, Hughes V, Crean A, Dyer M, Buxton M, Goldsmith K, et al. Cost-effectiveness of functional cardiac testing in the diagnosis and management of coronary artery disease: a randomised controlled trial. Health Technology Assessment (Winchester, England) 2007;11(49):iii-iv–ix-115. doi: 10.3310/hta11490. The CECaT trial. [DOI] [PubMed] [Google Scholar]
- 135.Shaw LJ, Marwick TH, Berman DS, Sawada S, Heller GV, Vasey C, et al. Incremental cost-effectiveness of exercise echocardiography vs SPECT imaging for the evaluation of stable chest pain. Eur Heart J. 2006;27(20):2448–58. doi: 10.1093/eurheartj/ehl204. [DOI] [PubMed] [Google Scholar]
- 136.Tardif JC, Dore A, Chan KL, Fagan S, Honos G, Marcotte F, et al. Economic impact of contrast stress echocardiography on the diagnosis and initial treatment of patients with suspected coronary artery disease. J Am Soc Echocardiogr. 2002;15(11):1335–45. doi: 10.1067/mje.2002.125287. [DOI] [PubMed] [Google Scholar]
- 137.Gibbons RJ, Abrams J, Chatterjee K, Daley J, Deedwania PC, Douglas JS, et al. ACC/AHA 2002 guideline update for the management of patients with chronic stable angina--summary article: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines (Committee on the Management of Patients With Chronic Stable Angina) J Am Coll Cardiol. 2003;41(1):159–68. doi: 10.1016/s0735-1097(02)02848-6. [DOI] [PubMed] [Google Scholar]
- 138.Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE Jr, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non ST-Elevation Myocardial Infarction): developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons: endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. Circulation. 2007;116(7):e148–e304. doi: 10.1161/CIRCULATIONAHA.107.181940. [DOI] [PubMed] [Google Scholar]
- 139.Toronto Health Economics and Technology Assessment Collaborative. The relative cost-effectiveness of five non-invasive cardiac imaging technologies for diagnosing coronary artery disease in Ontario. Toronto: THETA. 2010. p. 61 p. [cited: 2010 Mar 9] Available from: http://theta.utoronto.ca/reports/?id=7 .


