Executive Summary
In early August 2007, the Medical Advisory Secretariat began work on the Aging in the Community project, an evidence-based review of the literature surrounding healthy aging in the community. The Health System Strategy Division at the Ministry of Health and Long-Term Care subsequently asked the secretariat to provide an evidentiary platform for the ministry’s newly released Aging at Home Strategy.
After a broad literature review and consultation with experts, the secretariat identified 4 key areas that strongly predict an elderly person’s transition from independent community living to a long-term care home. Evidence-based analyses have been prepared for each of these 4 areas: falls and fall-related injuries, urinary incontinence, dementia, and social isolation. For the first area, falls and fall-related injuries, an economic model is described in a separate report.
Please visit the Medical Advisory Secretariat Web site, http://www.health.gov.on.ca/english/providers/program/mas/mas_about.html, to review these titles within the Aging in the Community series.
Aging in the Community: Summary of Evidence-Based Analyses
Prevention of Falls and Fall-Related Injuries in Community-Dwelling Seniors: An Evidence-Based Analysis
Behavioural Interventions for Urinary Incontinence in Community-Dwelling Seniors: An Evidence-Based Analysis
Caregiver- and Patient-Directed Interventions for Dementia: An Evidence-Based Analysis
Social Isolation in Community-Dwelling Seniors: An Evidence-Based Analysis
The Falls/Fractures Economic Model in Ontario Residents Aged 65 Years and Over (FEMOR)
Objective
To identify interventions that may be effective in reducing the probability of an elderly person’s falling and/or sustaining a fall-related injury.
Background
Although estimates of fall rates vary widely based on the location, age, and living arrangements of the elderly population, it is estimated that each year approximately 30% of community-dwelling individuals aged 65 and older, and 50% of those aged 85 and older will fall. Of those individuals who fall, 12% to 42% will have a fall-related injury.
Several meta-analyses and cohort studies have identified falls and fall-related injuries as a strong predictor of admission to a long-term care (LTC) home. It has been shown that the risk of LTC home admission is over 5 times higher in seniors who experienced 2 or more falls without injury, and over 10 times higher in seniors who experienced a fall causing serious injury.
Falls result from the interaction of a variety of risk factors that can be both intrinsic and extrinsic. Intrinsic factors are those that pertain to the physical, demographic, and health status of the individual, while extrinsic factors relate to the physical and socio-economic environment. Intrinsic risk factors can be further grouped into psychosocial/demographic risks, medical risks, risks associated with activity level and dependence, and medication risks. Commonly described extrinsic risks are tripping hazards, balance and slip hazards, and vision hazards.
Note: It is recognized that the terms “senior” and “elderly” carry a range of meanings for different audiences; this report generally uses the former, but the terms are treated here as essentially interchangeable.
Evidence-Based Analysis of Effectiveness
Research Question
Since many risk factors for falls are modifiable, what interventions (devices, systems, programs) exist that reduce the risk of falls and/or fall-related injuries for community-dwelling seniors?
Inclusion and Exclusion Criteria
Inclusion Criteria
English language;
published between January 2000 and September 2007;
population of community-dwelling seniors (majority aged 65+); and
randomized controlled trials (RCTs), quasi-experimental trials, systematic reviews, or meta-analyses.
Exclusion Criteria
special populations (e.g., stroke or osteoporosis; however, studies restricted only to women were included);
studies only reporting surrogate outcomes; or
studies whose outcome cannot be extracted for meta-analysis.
Outcomes of Interest
number of fallers, and
number of falls resulting in injury/fracture.
Search Strategy
A search was performed in OVID MEDLINE, MEDLINE In-Process and Other Non-Indexed Citations, EMBASE, the Cumulative Index to Nursing & Allied Health Literature (CINAHL), The Cochrane Library, and the International Agency for Health Technology Assessment (INAHTA) for studies published between January 2000 and September 2007. Furthermore, all studies included in a 2003 Cochrane review were considered for inclusion in this analysis. Abstracts were reviewed by a single author, and studies meeting the inclusion criteria outlined above were obtained. Studies were grouped based on intervention type, and data on population characteristics, fall outcomes, and study design were extracted. Reference lists were also checked for relevant studies. The quality of the evidence was assessed as high, moderate, low, or very low according to the GRADE methodology.
Summary of Findings
The following 11 interventions were identified in the literature search: exercise programs, vision assessment and referral, cataract surgery, environmental modifications, vitamin D supplementation, vitamin D plus calcium supplementation, hormone replacement therapy (HRT), medication withdrawal, gait-stabilizing devices, hip protectors, and multifactorial interventions.
Exercise programs were stratified into targeted programs where the exercise routine was tailored to the individuals’ needs, and untargeted programs that were identical among subjects. Furthermore, analyses were stratified by exercise program duration (<6 months and ≥6 months) and fall risk of study participants. Similarly, the analyses on the environmental modification studies were stratified by risk. Low-risk study participants had had no fall in the year prior to study entry, while high-risk participants had had at least one fall in the previous year.
A total of 17 studies investigating multifactorial interventions were identified in the literature search. Of these studies, 10 reported results for a high-risk population with previous falls, while 6 reported results for study participants representative of the general population. One study provided stratified results by fall risk, and therefore results from this study were included in each stratified analysis.
Conclusions
High-quality evidence indicates that long-term exercise programs in mobile seniors and environmental modifications in the homes of frail elderly persons will effectively reduce falls and possibly fall-related injuries in Ontario’s elderly population.
A combination of vitamin D and calcium supplementation in elderly women will help reduce the risk of falls by more than 40%.
The use of outdoor gait-stabilizing devices for mobile seniors during the winter in Ontario may reduce falls and fall-related injuries; however, evidence is limited and more research is required in this area.
While psychotropic medication withdrawal may be an effective method for reducing falls, evidence is limited and long-term compliance has been demonstrated to be difficult to achieve.
Multifactorial interventions in high-risk populations may be effective; however, the effect is only marginally significant, and the quality of evidence is low.
In early August 2007, the Medical Advisory Secretariat began work on the Aging in the Community project, an evidence-based review of the literature surrounding healthy aging in the community. The Health System Strategy Division at the Ministry of Health and Long-Term Care subsequently asked the secretariat to provide an evidentiary platform for the ministry’s newly released Aging at Home Strategy.
After a broad literature review and consultation with experts, the secretariat identified 4 key areas that strongly predict an elderly person’s transition from independent community living to a long-term care home. Evidence-based analyses have been prepared for each of these 4 areas: falls and fall-related injuries, urinary incontinence, dementia, and social isolation. For the first area, falls and fall-related injuries, an economic model is described in a separate report.
Please visit the Medical Advisory Secretariat Web site, http://www.health.gov.on.ca/english/providers/program/mas/mas_about.html, to review these titles within the Aging in the Community series.
Aging in the Community: Summary of Evidence-Based Analyses
Prevention of Falls and Fall-Related Injuries in Community-Dwelling Seniors: An Evidence-Based Analysis
Behavioural Interventions for Urinary Incontinence in Community-Dwelling Seniors: An Evidence-Based Analysis
Caregiver- and Patient-Directed Interventions for Dementia: An Evidence-Based Analysis
Social Isolation in Community-Dwelling Seniors: An Evidence-Based Analysis
The Falls/Fractures Economic Model in Ontario Residents Aged 65 Years and Over (FEMOR)
Objective
To identify interventions that may be effective in reducing the probability of an elderly person’s falling and/or sustaining a fall-related injury.
Clinical Need: Target Population and Condition
Definition of a Fall
Several definitions for falls exist in the literature; however, a recently published consensus statement suggested that a fall be defined as “an unexpected event in which the participant comes to rest on the ground, floor, or lower level.” (1)
Target Population and Prevalence of Falls
Although estimates of fall rates vary widely based on the location, age, and living arrangements of the elderly population, it is estimated that approximately 30% of community-dwelling individuals aged 65 and older, and 50% of those aged 85 and older will fall each year. (2-4) Of those individuals who fall, 12% to 42% will have a fall-related injury. (5;6) Elderly women living independently in the community are more likely to experience a fall than men, (6;7) and a study by Campbell et al. (8) found that the risk of falling for women was more than 1.5 times higher than for men, even after controlling for physical and sociological variables associated with increased fall risk.
In 2005, 12.8% of Ontario’s population was aged 65 or older, a figure that is expected to increase by almost 65% by 2031. (9) With more than 1 in 5 Ontarians being 65 or older in 2031, the number of community-dwelling seniors at risk for encountering a fall will dramatically increase, thus increasing the demand for community-based services and the burden on Ontario’s health system.
Note: It is recognized that the terms “senior” and “elderly” carry a range of meanings for different audiences; this report generally uses the former, but the terms are treated here as essentially interchangeable.
Fall Outcomes and Burden
Minor injuries such as bruises, abrasions, lacerations and sprains occur after 44% of falls (10), while major injuries such as hip and wrist fractures occur after approximately 4% to 5% of falls. (11;12) As an individual ages, their ability to use their hands to break a fall and protect their hip is reduced, and therefore wrist fractures are more common than hip fractures between the ages of 65 and 75, while hip fractures become more prevalent after the age of 75. (13)
Injuries due to falls place a significant burden on the Ontario health system and are the leading cause of injury-related hospital visits (1,201/100,000 population) and emergency department visits (4,821/100,000 population) in Ontarians aged 65 and older. (14) Furthermore, once an individual is admitted into an acute hospital following a fall, their average length of stay (ALOS) is approximately 40% longer than that for all-cause hospitalizations. (15) This highlights not only the severity of injuries due to falls, but also the need for community-based services that will allow a more expedient discharge of elderly individuals back to their homes following a fall-related hospitalization.
Difficulties exist in measuring mortality directly associated with falls; however, it is estimated that up to 40% of injury-related deaths, and 1% of total deaths in those aged 65 and over, are due to falls. (16)
Falls as a Predictor of Long-Term Care Home Admission
A prospective cohort study was conducted in 1997 by Tinetti and Williams (17) to assess the risk of admission to a LTC home following falls and fall-related injuries. A cohort of 1,103 community-dwelling seniors aged 71 and older were followed for a median of 12 months. The outcome of interest in this study was the number of days from initial assessment to a first long-term admission to a skilled-nursing facility. The results of this study showed that after adjusting for demographic, psychosocial, cognitive, health-related and functional characteristics, there was a significant increase in the hazard of LTC home admission following falls (Table 1).
Executive Summary Table 1: Summary of Meta-Analyses of Studies Investigating the Effectiveness of Interventions on the Risk of Falls in Community-Dwelling Seniors*.
| Intervention | RR [95% CI] | GRADE |
|---|---|---|
| Exercise programs | ||
| 1. Targeted programs | ||
| General population | 0.81 [0.67–0.98] | Low |
| High-risk population | 0.93 [0.82–1.06] | High |
| Short duration | 0.91 [0.73–1.13] | High |
| Long duration | 0.89 [0.79–1.01] | Moderate |
| 2. Untargeted programs | ||
| General population | 0.78 [0.66–0.91] | Moderate |
| High-risk population | 0.89 [0.72–1.10] | Very low |
| Short duration | 0.85 [0.71–1.01] | Low |
| Long duration | 0.76 [0.64–0.91] | Moderate |
| 3. Combined targeted vs. untargeted programs | ||
| General population | N/A | N/A |
| High-risk population | 0.87 [0.57–1.34] | Moderate |
| Short duration | 1.11 [0.73–1.70] | High |
| Long duration | 0.73 [0.57–0.95] | High |
| Vision intervention | ||
| Assessment/referral | 1.12 [0.82–1.53] | Moderate |
| Cataract surgery | 1.11 [0.92–1.35] | Moderate |
| Environmental modifications | ||
| Low-risk population | 1.03 [0.75–1.41] | High |
| High-risk population | 0.66 [0.54–0.81] | High |
| General population | 0.85 [0.75–0.97] | High |
| Drugs/Nutritional supplements | ||
| Vitamin D (men and women) | 0.94 [0.77–1.14] | High |
| Vitamin D (women only) | 0.55 [0.29–1.08] | Moderate |
| Vitamin D and calcium (men and women) | 0.89 [0.74–1.07] | Moderate |
| Vitamin D and calcium (women only) | 0.83 [0.73–0.95] | Moderate |
| Hormone replacement therapy | 0.98 [0.80–1.20] | Low |
| Medication withdrawal | 0.34 [0.16–0.74]† | Low |
| Gait-stabilizing device | 0.43 [0.29–0.64] | Moderate |
| Multifactorial intervention | ||
| Geriatric screening (general population) | 0.87 [0.69–1.10] | Very low |
| High-risk population | 0.86 [0.75–0.98] | Low |
CI refers to confidence interval; RR, relative risk.
Hazard ratio is reported, because RR was not available.
A meta-analysis published by Gaugler et al. in 2007 (18) investigated predictors of LTC home admission in community-dwelling elderly populations. This analysis was based on two large cohort studies in the United States, and found that the hazard of LTC home admission was approximately 16% higher in seniors with a history of falls than in those without (hazard ratio [HR], 1.16, [95% confidence interval (CI), 1.02–1.30]). The smaller effect size in this study as compared with the Tinetti and Williams study is likely due to the fact that fall status was based on annual recall in the studies included in the Gaugler et al. review, while the Tinetti and Williams study measured falls based on monthly calendars. While evidence regarding the most valid method of falls-outcome collection is limited, the use of monthly falls calendars is generally accepted to be a more rigorous and sensitive method of measuring fall status in elderly individuals. (19)
Table 1: Hazard Ratios for Admission to a Long-term Care Home Following Falls and Fall-related Injuries*.
| Fall Severity | HR [95% CI] | Population Attributable Risk (%) |
|---|---|---|
| 1 fall without serious injury | 3.1 [1.9–4.9] | 13% |
| 2 or more falls without serious injury | 5.5 [2.1–14.2] | 3% |
| At least one fall causing serious injury | 10.2 [5.8–17.9] | 10% |
CI refers to confidence interval; HR, hazard ratio.
Tinetti and Williams (20)
Fall Risks for Community-Dwelling Seniors
Falls result from the interaction of a variety of risk factors that can be both intrinsic and extrinsic. Intrinsic factors are those that pertain to the physical, demographic, and health status of the individual, while extrinsic factors relate to the physical and socio-economic environment. (21;22) Intrinsic risk factors can be further grouped into psychosocial/demographic risks, medical risks, risks associated with activity level and dependence, and medication risks.
Intrinsic Risk Factors
Psychosocial and Demographic Risks
As mentioned earlier in this report, increasing age and gender are both strong risk factors for falls. (6;23;24) Two psychosocial risk factors that have also been studied extensively are previous history of falls and fear of falling. A previous history of falls has been demonstrated as one of the strongest predictors of future falls and injurious falls. (25) This may be due to a loss of mobility and balance, or because of increased fear of falling, which can in turn lead to activity restrictions, loss of strength, and social isolation. (26;27)
Medical Risk Factors
In general, the risk of falling and sustaining a fall-related injury increases with the number of chronic health problems, with individuals having 5 to 7 chronic illnesses having more than 2.5 times the risk of falling and 4.5 times the risk of having an injurious fall as someone without chronic conditions. (28) More specifically, chronic medical problems that have been shown to be associated with an increased risk of falls are a history of stroke, arthritis of the knee, foot problems, low systolic blood pressure, poor vision, cognitive impairment, Parkinson’s disease, poor strength, muscle weakness, decreased reaction time, limited mobility and impaired balance and gait. (6;29-31)
Activity and Dependence
As individuals age, limited mobility, fear of falling, chronic illnesses and various other factors lead to decreased physical activity, which can result in decreased muscle strength and balance. Several studies have indicated that inactivity and decreased physical fitness in seniors are a major risk factor for falls and injurious falls. (32) However, some studies identify high physical activity as a risk factor for falls in older populations, indicating that the risks associated with increased physical activity for some elderly people must also be considered. (6) More research is needed in this area to determine the potential harm and benefit of various types and intensities of physical activity.
Medications
Research surrounding the risks of falls and fall-related injuries following medication use is extensive. Multiple prescriptions can lead to dizziness, and to problems with alertness, coordination, and balance. (33) As a result, studies have found that taking multiple medications leads to a significant increase in the risk of falls and injurious falls. (34-37) Furthermore, several drugs that are frequently prescribed to elderly individuals are independently associated with a high risk of falls. These include sedatives and hypnotics, psychotropic medications, benzodiazepines, and diuretics. (6;38;39) Some studies indicate that antihypertensive medications may also increase the risk of falls and fall-related injuries; however, results in this area are inconsistent. (40)
Extrinsic Risk Factors
There is very little evidence surrounding the level of risk associated with extrinsic risk factors. Commonly described extrinsic risks are tripping hazards, balance and slipping hazards, and vision hazards. (6;41-43)
Tripping hazards
loose rugs,
electrical cords,
pets,
uneven sidewalks, and
inappropriate or ill-fitting footwear.
Balance and slipping hazards
narrow or slippery stairs,
no handrails on stairs,
bathroom hazards (e.g., low toilets, unsafe or slippery bathtubs/showers),
low furniture, and
ice and snow.
Vision hazards
cataracts,
eyeglasses, and
poor lighting.
Evidence-Based Analysis of Effectiveness
Objective
To identify interventions that may be effective in reducing the probability of an elderly person’s falling and/or sustaining a fall-related injury.
Research Questions
Since many risk factors for falls are modifiable, what interventions (devices, systems, programs) exist that reduce the risk of falls and/or fall-related injuries for community-dwelling elderly persons?
Are there differences in the effectiveness of interventions in high-risk groups (e.g., frail, history of falling)?
Methods
Inclusion and Exclusion Criteria
Inclusion Criteria
English language;
published between January 2000 and September 2007;
population of community-dwelling seniors (majority aged 65+); and
randomized controlled trials (RCTs), quasi-experimental trials, systematic reviews, or meta-analyses.
Exclusion Criteria
special populations (e.g., stroke or osteoporosis; however, studies restricted only to women were included);
studies only reporting surrogate outcomes; or
studies whose outcome cannot be extracted for meta-analysis.
Outcomes of Interest
number of fallers, and
number of falls resulting in injury/fracture.
Method of Review
A search was performed in OVID MEDLINE, MEDLINE In-Process and Other Non-Indexed Citations, EMBASE, the Cumulative Index to Nursing & Allied Health Literature (CINAHL), The Cochrane Library, and the International Agency for Health Technology Assessment (INAHTA) for studies published between January 2000 and September 2007. The search strategy is detailed in Appendix 1.
Furthermore, all studies included in a 2003 Cochrane review published by Gillespie et al. (44) were considered for inclusion in this review.
Abstracts were reviewed, and studies meeting the inclusion criteria outlined above were obtained. Studies were grouped based on intervention type, and data on population characteristics, falls outcomes, and study design were extracted. Reference lists were also checked for relevant studies. Results for each outcome from individual studies were meta-analyzed using fixed-effects models.
Assessment of Quality of Evidence
The quality assigned to individual studies was determined using the Medical Advisory Secretariat’s adaptation of the levels-of-evidence hierarchy proposed by Goodman. (45)
The overall quality of the evidence was examined according to the GRADE Working Group criteria (see Appendix 2). (46)
Quality refers to criteria such as the adequacy of allocation concealment, blinding, and follow-up.
Consistency refers to the similarity of estimates of effect across studies. If there is important unexplained inconsistency in the results, our confidence in the estimate of effect for that outcome decreases. Differences in the direction of effect, the size of the differences in effect, and the significance of the differences guide the decision about whether important inconsistency exists.
Directness refers to the extent to which the interventions and outcome measures are similar to those of interest.
As stated by the GRADE Working Group, the following definitions were used in grading the quality of the evidence.
| High | Further research is very unlikely to change confidence in the estimate of effect. |
| Moderate | Further research is likely to have an important impact on confidence in the estimate of effect and may change the estimate. |
| Low | Further research is very likely to have an important impact on confidence in the estimate of effect and is likely to change the estimate. |
| Very low | Any estimate of effect is very uncertain. |
Results of Evidence-Based Analysis
The database search identified 507 citations published between January 2000 and September 2007. Of the 155 studies set in the community as opposed to a hospital or LTC home, 43 met the inclusion criteria described above. A further 17 studies were identified in the Cochrane review on falls in the elderly, 15 of which were published before the year 2000. (44) All studies identified were RCTs, and only one was defined as small (total sample size N=28) (Table 2).
Executive Summary Table 2: Summary of Meta-Analyses of Studies Investigating the Effectiveness of Interventions on the Risk of Fall-Related Injuries in Community-Dwelling Seniors*.
| Intervention | RR [95% CI] | GRADE |
|---|---|---|
| Exercise programs | ||
| Targeted programs | 0.67 [0.51–0.89] | Moderate |
| Untargeted programs | 0.57 [0.38–0.86] | Low |
| Combined targeted vs untargeted programs | 0.31 [0.13–0.74] | High |
| Drugs/nutritional supplements | ||
| Vitamin D plus calcium (women only) | 0.77 [0.49–1.21] | Moderate |
| Gait-stabilizing device | 0.10 [0.01–0.74] | Moderate |
| Hip protectors | 3.49 [0.68–17.97]† | Low |
| Multifactorial intervention | ||
| Geriatric screening (general population) | 0.90 [0.53–1.51] | Low |
| High-risk population | 0.86 [0.66–1.11] | Moderate |
CI refers to confidence interval; RR, relative risk.
Odds ratio is reported, because RR was not available.
Table 2: Quality of Evidence of Included Studies*.
| Study Design | Level of Evidence |
Number of Eligible Studies |
|---|---|---|
| Large RCT, systematic review of RCTs | 1 | 59 |
| Large RCT unpublished but reported to an international scientific meeting | 1(g) | 0 |
| Small RCT | 2 | 1 |
| Small RCT unpublished but reported to an international scientific meeting | 2(g) | 0 |
| Non-RCT with contemporaneous controls | 3a | 0 |
| Non-RCT with historical controls | 3b | 0 |
| Non-RCT presented at international conference | 3(g) | 0 |
| Surveillance (database or register) | 4a | 0 |
| Case series (multisite) | 4b | 0 |
| Case series (single site) | 4c | 0 |
| Retrospective review, modeling | 4d | 0 |
| Case series presented at international conference | 4(g) | 0 |
For each included study, levels of evidence were assigned according to a ranking system based on a hierarchy proposed by Goodman. (45) An additional designation “g” was added for preliminary reports of studies that have been presented at international scientific meetings. Non-RCT, clinical trial that is not randomized, e.g., a cohort study; RCT, randomized controlled trial.
Adapted from the Oxford Centre for Evidence (45)
Summary of Existing Evidence
Interventions Identified in Literature
physical exercise
vision assessment and referral
cataract surgery
environmental modifications
vitamin D supplements
vitamin D and calcium supplements
hormone replacement therapy (HRT)
medication withdrawal
gait-stabilizing devices
hip protectors
multifactorial interventions
Detailed study characteristics are provided in Appendix 3.
Exercise
There were 25 studies identified that described the effects of a physical exercise intervention on the proportion of people falling or experiencing a fall-related injury. The types of exercise programs provided to the intervention group varied considerably between trials. Most exercise programs contained a combination of exercises designed to improve balance, endurance, strength, coordination, and flexibility. Although most were conducted in a group setting, several programs incorporated a home-based exercise program to be completed between group sessions.
In general, the exercise interventions described in the literature can be grouped into 2 main categories: targeted and untargeted. Targeted interventions are tailored exercise programs that are based on the individual’s risk factors and needs, while untargeted interventions provide the same exercise program to all individuals enrolled. Eighteen studies investigated the effects of an untargeted intervention, 5 studies investigated the effects of a targeted intervention, and in 2 studies, the authors compared a combination of untargeted and targeted exercises against an untargeted exercise program. The meta-analysis of these studies indicated that there is a moderate reduction in the risk of falling following untargeted interventions (relative risk [RR], 0.82 [95% CI, 0.72–0.93]). Forest plots for all meta-analyses are presented in Appendix 4.
After evaluating the population and program characteristics found in the literature, two important stratifications were identified. The first stratification was by fall risk, where individuals were identified as high-risk if they were extremely frail or had a history of previous falls. Ten studies restricted the population of interest to frail elderly persons at high risk for falls, while the remaining 15 studies did not limit their population based on fall risk. The meta-analysis indicated that there was no statistically significant reduction in the number of high-risk individuals falling following an exercise program (Table 3). However, in studies that did not restrict the study population to those at high risk, both targeted and untargeted exercise programs significantly reduced an individual’s risk of falling and having a fall-related injury (Tables 4 and 5).
Table 3: Summary of Evidence Surrounding the Risk of Falls After an Exercise Program: High-Risk Population*.
| Untargeted Exercise vs. No Exercise |
Targeted Exercise vs. No Exercise |
Combination Exercise vs. Untargeted Exercise |
|
|---|---|---|---|
| Number of studies | 6 | 2 | 2 |
| Total N (case/control) | 372/270 | 329/330 | 77/61 |
| RR (95% CI) | 0.89 (0.72–1.10) | 0.93 (0.82–1.06) | 0.87 (0.57–1.34) |
CI refers to confidence interval; RR, relative risk; combination refers to untargeted and targeted exercise programs.
Table 4: Summary of Evidence Surrounding the Risk of Falls After an Exercise Program: General Population*.
| Untargeted Exercise vs. No Exercise |
Targeted Exercise vs. No Exercise |
Combination Exercise vs. Untargeted Exercise |
|
|---|---|---|---|
| Number of studies | 12 | 3 | 0 |
| Total N (case/control) | 1250/1234 | 282/284 | 0/0 |
| RR (95% CI) | 0.78 (0.66–0.91) | 0.81 (0.67–0.98) | N/A |
CI refers to confidence interval; RR, relative risk; combination refers to untargeted and targeted exercise programs.
Table 5: Summary of Evidence Surrounding the Risk of Fall-Related Injuries After an Exercise Program: General Population*.
| Untargeted Exercise vs. No Exercise |
Targeted Exercise vs. No Exercise |
Combination Exercise vs. Untargeted Exercise |
|
|---|---|---|---|
| Number of studies | 2 | 3 | 0 |
| Total N (case/control) | 239/187 | 269/277 | 0/0 |
| RR (95% CI) | 0.44 (0.27–0.72) | 0.67 (0.51–0.89) | N/A |
CI refers to confidence interval; RR, relative risk; combination refers to untargeted and targeted exercise programs.
The second stratification considered was based on intervention duration. There was inconsistency in results of studies based on the duration of the exercise program, and therefore studies were stratified into those exercise programs lasting for less than 6 months, and those lasting 6 months or more. The results of this meta-analysis indicated that there was no statistically significant reduction in the risk of falling following a short exercise intervention of any kind (Table 6). Conversely, untargeted exercise interventions lasting 6 months or longer showed a statistically significant reduction in the risk of falling (Table 7). Only two studies investigating a short-term exercise intervention reported fall-related injuries as an outcome (47;48), and only one of these studies (49) reported any fall-related injuries during its follow-up period. The authors of this study reported a reduction in the risk of fall-related injuries following an untargeted exercise program; however, this reduction was not significant. A meta-analysis of the effectiveness of long-term exercise interventions on risk of fall-related injury indicated that targeted exercise programs moderately reduce the risk of fall-related injuries (Table 8).
Table 6: Summary of Evidence Surrounding the Risk of Falls After an Exercise Program: Short Intervention (<6 months)*.
| Untargeted | Targeted | Combination* Versus Untargeted |
|
|---|---|---|---|
| Number of studies | 10 | 2 | 1 |
| Total N (case/control) | 1160/1070 | 157/158 | 34/34 |
| RR (95% CI) | 0.85 (0.71–1.01) | 0.91 (0.73–1.13) | 1.11 (0.73–1.70) |
CI refers to confidence interval; RR, relative risk; combination refers to untargeted and targeted exercise programs.
Table 7: Summary of Evidence Surrounding the Risk of Falls After an Exercise Program: Long Intervention (≥6 months)*.
| Untargeted | Targeted | Combination* Versus Untargeted |
|
|---|---|---|---|
| Number of studies | 8 | 3 | 1 |
| Total N (case/control) | 462/434 | 454/456 | 43/27 |
| RR (95% CI) | 0.76 (0.64–0.91) | 0.89 (0.79–1.01) | 0.73 (0.57–0.95) |
CI refers to confidence interval; RR, relative risk; combination refers to untargeted and targeted exercise programs
Table 8: Summary of Evidence Surrounding the Risk of Fall-Related Injuries After an Exercise Program: Long Intervention (≥6 months)*.
| Untargeted | Targeted | Combination* Versus Untargeted |
|
|---|---|---|---|
| Number of studies | 2 | 2 | 1 |
| Total N (case/control) | 171/167 | 224/229 | 43/27 |
| RR (95% CI) | 0.61 (0.33–1.12) | 0.68 (0.51–0.90) | 0.31 (0.13–0.74) |
CI refers to confidence interval; RR, relative risk; combination refers to untargeted and targeted exercise programs
Vision Assessment and Referral
The literature search identified two studies that investigated the effects of vision assessment and referral on fall risk in a population of healthy elderly people aged 70 and over. (50;51) The intervention in the study by Day et al. (52) consisted of a visual acuity test by a trained assessor followed by referrals to an eye care provider, general practitioner, or optometrist where needed. In the study by Cumming et al. (53), the vision assessment was performed by an optometrist, and further referrals to an ophthalmologist or eye clinic were determined by the optometrist. A meta-analysis of these two studies showed that there was no significant reduction in the risk of falls following vision assessment and referral (Table 9).
Table 9: Summary of Evidence Surrounding the Risk of Falls After Vision Interventions*.
| Vision Assessment and Referral |
Cataract Surgery | |
|---|---|---|
| Number of studies | 2 | 2 |
| Total N (case/control) | 448/444 | 274/271 |
| RR (95% CI) | 1.12 (0.82–1.53) | 1.11 (0.92–1.35) |
CI refers to confidence interval; RR, relative risk.
Cataract Surgery
Two studies have investigated the effects of cataract surgery in women aged 70 and over on risk of falling after 12 months of follow-up. (54;55) The intervention in the study by Harwood et al. (56) was small-incision cataract surgery and implantation of a folding silicone intraocular lens in women with cataracts and no previous ocular surgery. The study by Foss et al. (57) was a follow-up to this study and investigated the effects of cataract surgery on the second eye following successful cataract surgery in the study by Harwood et al. The results of a meta-analysis on these studies indicates that there is no reduction in risk of falls following cataract surgery in elderly women eligible for this procedure (Table 9).
Environmental Modifications
Environmental modifications are generally implemented in an elderly person’s home to reduce the risk associated with many of the extrinsic risk factors such as loose rugs, poor lighting, and slippery floors. This literature search identified 4 studies that assessed the effectiveness of a home modification program in community-dwelling seniors. (58-61) The interventions consisted of one assessment visit in the elderly individual’s home, followed by any necessary modifications such as the removal of floor coverings and loose electrical cords, changes to footwear, and the addition of hand rails, contrast edging to stairs, and non-slip bathmats. While the modifications available in each study were similar, the personnel responsible for the assessment and the cost of materials differed between programs. In two studies, an occupational therapist was responsible for the home assessment, (58;62) while in the remaining two studies, the assessment was carried out by a trained assessor (63) and a team consisting of a physical medicine and rehabilitation doctor and ergotherapist. (64) Only 2 studies described the costs associated with the home modifications. In the trial by Cumming et al., (65) modifications were funded through the usual sources available in the Central Sydney Area Health Service, and in the study by Day et al., (66) labour and materials up to a value of $100 (Australian) ($54 US) were provided at no cost to the client.
Several of these studies investigated whether prior fall risk was associated with fall outcomes following an environmental modification program, and therefore the results are stratified by fall risk. High-risk populations are those with one or more falls in the previous year, and low-risk populations are those with no fall in the previous year. Three studies reported results on the risk of falling for high-risk populations, and 1 study reported outcomes for low-risk populations. The results of meta-analyses on these subgroups showed that environmental modifications effectively reduce the risk of falling in high-risk populations (RR, 0.66 [95% CI, 0.54–0.81]) but show no effect for seniors at low risk of falling (RR, 1.03 [95% CI, 0.65–1.41]) (Table 10). Three studies also reported results in a population that contained both high- and low-risk individuals. A meta-analysis of these studies showed that there was a slight reduction in risk of falling following a home modification program if the program was implemented in a population with mixed risk of falling (RR, 0.85 [95% CI, 0.75–0.97]) (Table 10). No studies reported fall-related injuries as an outcome.
Table 10: Summary of Evidence Surrounding the Risk of Falls After Environmental Modifications*.
| High Risk (≥1 fall in previous year) |
Low Risk (no fall in previous year) |
High and Low Risk | |
|---|---|---|---|
| Number of studies | 3 | 1 | 3 |
| Total N (case/control) | 186/188 | 161/163 | 581/582 |
| RR (95% CI) | 0.66 (0.54–0.81) | 1.03 (0.75–1.41) | 0.85 (0.75–0.97) |
CI refers to confidence interval; RR, relative risk.
Vitamin D Supplements
Studies have shown that vitamin D deficiency may play a role in the development of osteoporosis and risk of fractures. (67;68) In 1999, two cross-sectional studies showed that vitamin D levels are associated with reduced muscle function and strength, (69;70) and as a result, several published studies have looked at the relationship between vitamin D supplementation and the risk of falls and fall-related injuries.
Four RCTs meeting the inclusion criteria were identified, one of which restricted the study population to women only. In two studies, a single dose of vitamin D was administered at study entry, after which participant fall outcomes were monitored for 6 months. (71;72) In the third study, participants received 1-μg capsules of alfacalcidol for 36 weeks, (73) and in the last study, participants were randomized to receive for 3 months either a 600-mg calcium carbonate supplement alone, or a combination supplement containing 600 mg calcium carbonate and 400 IU cholecalciferol (74). The results of the meta-analysis indicated that supplementation with vitamin D does not significantly reduce the risk of falling in the community-dwelling elderly population (Table 11). Similarly, in the study restricted to a population of elderly women, there was no evidence that vitamin D supplementation reduced the risk of falls (RR, 0.55 [95% CI, 0.29–1.08]) or fall-related injuries (RR, 0.48 [95% CI, 0.12–1.84]).
Table 11: Summary of Evidence Surrounding the Risk of Falls After Supplementation with Vitamin D*.
| Men and Women | Women | |
|---|---|---|
| Number of studies | 3 | 1 |
| Total N (case/control) | 383/369 | 70/67 |
| RR (95% CI) | 0.94 (0.77–1.14) | 0.55 (0.29–1.08) |
CI refers to confidence interval; RR, relative risk.
Vitamin D and Calcium Supplements
Supplementation with calcium has been shown to be effective in reducing bone loss by approximately 1% per year in post-menopausal women. (75) As a result, it has been hypothesized that the combination of vitamin D and calcium supplementation will reduce bone loss, body sway and loss of muscle strength, thus reducing the risk of falls and fractures in elderly individuals. Two studies were identified which investigated the joint effect of vitamin D and calcium supplementation in an elderly community-dwelling population. Both studies followed patients prospectively for 1 to 3 years; however, there were substantial differences in the intervention between the trials. A 3-year RCT conducted by Bischoff-Ferrari et al. (76) investigated the effects of a combination of 700 IU vitamin D3 and 600 mg calcium citrate malate each day on risk of falling in elderly men and women, while Barr et al. (77) investigated a screening intervention where supplementation with vitamin D and calcium were only suggested for women at increased risk of hip fracture.
The results of the analyses indicated that supplementation with vitamin D and calcium can effectively reduce the risk of falls in women. Although the meta-analysis of two small studies investigating the effect of vitamin D alone on fall risk were not significant, the relative risk was small (RR, 0.55 [95% CI, 0.29–1.08]), and the meta-analysis may not have been adequately powered to detect a significant reduction. Therefore, it is not possible to draw from these analyses any conclusions regarding the individual effectiveness of vitamin D or calcium on fall risk in women. The evidence does not suggest a statistically significant reduction in falls in the study that included both men and women in their study population or in fall-related injuries in women (Tables 12 and 13).
Table 12: Summary of Evidence Surrounding the Risk of Falls After Supplementation with Vitamin D and Calcium.
| Men and Women | Women | |
|---|---|---|
| Number of studies | 1 | 2 |
| Total N (case/control) | 219/226 | 720/1401 |
| RR (95% CI) | 0.89 (0.74–1.07) | 0.83 (0.73–0.95) |
CI refers to confidence interval; RR, relative risk.
Table 13: Summary of Evidence Surrounding the Risk of Fall-Related Fractures After Supplementation with Vitamin D and Calcium*.
| Men and Women | Women | |
|---|---|---|
| Number of studies | 0 | 2 |
| Total N (case/control) | 0/0 | 1313/2667 |
| RR (95% CI) | N/A | 0.77 (0.49–1.21) |
CI refers to confidence interval; RR, relative risk.
Hormone Replacement Therapy
The literature search identified one study that examined the effect of HRT on fall risk in elderly women. (78) In this study, women in the intervention group with a hysterectomy were given conjugated equine estrogen (0.625 mg/day), and women without a hysterectomy were given conjugated equine estrogen (0.625 mg/day) and medroxyprogesterone (2.5 mg/day). All women in the trial were given a calcium and vitamin D supplement. This study found no evidence of a reduction in the risk of falling following HRT (RR, 0.98 [95% CI, 0.80–1.20]).
Medication Withdrawal
As described earlier, the use of medications, particularly psychotropic medications, is frequently identified as a major risk factor for falls in the elderly. The literature search identified one study that investigated the effect of psychotropic medication withdrawal on the risk of falls in a community-dwelling elderly population. (79) Participants in the intervention arm of this study had the amount of active ingredient in their medication gradually reduced over 14 weeks. After 14 weeks, these individuals were taking capsules that contained inert substances only. Individuals in the control arm did not have any change in the active ingredients in their medication. After controlling for fall history and total number of medications taken, the relative hazard of falls was significantly lower in the medication withdrawal group than in the control group (HR, 0.34 [95% CI, 0.16–0.74]). However, a major limitation of this study was that compliance 1 month following study completion was very low, with 47% of the participants in the medication withdrawal group restarting psychotropic medications. Therefore, the acceptability of this intervention as a method of reducing falls in community-dwelling seniors is questionable.
Gait-stabilizing Devices
One study published in 2005 investigated the effects of a gait-stabilizing device on outdoor slips and falls in 109 community-dwelling seniors with a history of falls. (80) Study participants in the intervention arm were provided with a gait-stabilizing device (Yaktrax Walker) for use outdoors during the winter months. The Yaktrax Walker is an injection-molded thermal plastic elastomer netting with high-strength horizontal coils to provide forward and backward stability. (81) This study found that there was a significant reduction in the risks of outdoor falls and of injurious falls when using the gait-stabilizing device as compared with the controls (RR, 0.43 [95% CI, 0.29–0.64]; RR, 0.10 [95% CI, 0.01–0.74], respectively). This results in a number needed to prevent (NNP) of 3 to prevent one fall, and 6 to prevent one injurious fall. Furthermore, the compliance with this intervention was high, with 78% of study participants reporting the Yaktrax Walker as their primary winter footwear during the course of the study.
Hip Protectors
Most studies of the effectiveness of hip protectors on fall-related injury risk in the elderly are conducted in an institutionalized elderly population, and due to different population characteristics and risk factors, the results of these studies are not generalizable to the community-dwelling elderly population. The literature search identified one study that investigated the effects of a hip protector on hip fracture risk in community-dwelling seniors with a previous hip fracture. (82) During a median follow-up of 14 months, 8 hip fractures were reported among the 279 study participants. There was no significant difference in the odds of a second hip fracture between those study participants wearing a hip protector and those in the control group (OR, 3.5 [95% CI, 0.7–18.0]). However, compliance in the intervention group was low (34%), and only one of the 6 individuals in the intervention arm who suffered a hip fracture was wearing the hip protector at the time of the fall. This woman reported falling backwards and not to the side.
Multifactorial Interventions
Several studies have investigated the effect of a combination of interventions whose purpose is to reduce the risk of falls for community-dwelling seniors. In this review, 17 studies provided an initial assessment followed by a multifactorial intervention to reduce falls and fall-related injuries. The components of the multifactorial interventions differed between trials; however, most included a combination of home hazard assessment and environmental modification, an exercise program, and medication review. Other interventions offered in some studies included vision assessment, podiatry, assessment of cognition, provision of assistive devices, and community safety education. In general, services were provided by an occupational therapist, physical therapist, or nurse.
The intervention duration and target population differed among studies. The majority of studies (83-88) had a follow-up of 1 year; however, there was a wide variation, with two studies following participants for only 3 months (89;90), and two studies with a 3-year follow-up period. (91;92) Furthermore, 6 studies restricted their population to the general elderly population (“geriatric screening”), while 10 studies considered a more targeted approach, restricting their inclusion criteria to seniors at high risk of falls. One study performed a stratified analysis, with results provided for both the general elderly population, and that at high risk of falls. (83)
Two studies (93;94) were excluded from the meta-analysis. The mean number of falls in the previous 6 months, and the percentage of recurrent fallers at baseline in the study by Whitehead et al. (93) were significantly higher in the intervention compared with the control group. Since these are important covariates to consider when assessing fall risk, it was not appropriate to include the unadjusted results of this study in the meta-analysis. The adjusted results of this study found no significant change in fall risk following the multifactorial intervention (OR, 1.7; 95% CI, 0.7–4.4). In the study by Mahoney et al. (95) raw data were not presented, and therefore data extraction for meta-analysis was not possible. Similarly, this study did not demonstrate a significant reduction in falls following a multifactorial intervention (RR, 0.81; 95% CI, 0.57–1.17).
The results of the meta-analysis indicated that multifactorial interventions do not significantly reduce the risk of falls among the general elderly population (RR, 0.87 [95% CI, 0.69–1.10]), but there is a marginally significant reduction in the risk of falls in high-risk populations following a multifactorial intervention (RR, 0.86 [95% CI, 0.75-0.98]; Table 14). Only 7 studies reported fall-related injuries as an outcome. The results of the meta-analyses of these trials did not indicate a significant reduction in the risk of fall-related injuries following a multifactorial intervention (Table 15).
Table 14: Summary of Evidence Surrounding the Risk of Falls After a Multifactorial Intervention*.
| Geriatric Screening | High Risk | Total | |
|---|---|---|---|
| Number of studies | 6 | 10 | 16 |
| Total N (case/control) | 1430/1427 | 1301/1309 | 2731/2736 |
| RR (95% CI) | 0.87 (0.69–1.10) | 0.86 (0.75–0.98) | 0.87 (0.78–0.97) |
CI refers to confidence interval; RR, relative risk.
Table 15: Summary of Evidence Surrounding the Risk of Fall-Related Injuries After a Multifactorial Intervention*.
| Geriatric Screening | High Risk | Total | |
|---|---|---|---|
| Number of studies | 2 | 5 | 7 |
| Total N (case/control) | 845/811 | 771/783 | 1616/1594 |
| RR (95% CI) | 0.90 (0.53–1.51) | 0.86 (0.66–1.11) | 0.87 (0.69–1.10) |
CI refers to confidence interval; RR, relative risk.
Despite the lack of a large effect of multifactorial interventions on falls and fall-related injuries, it is important to note that the studies were all quite diverse in the composition of the multifactorial intervention. Furthermore, since studies did not generally describe the uptake of specific interventions within their study population, it is possible that the effects of effective interventions were diluted. Therefore, it is difficult to draw a strong conclusion as to whether appropriate, well-conducted multifactorial interventions would be effective in the population of Ontario’s seniors.
Four study protocols for multifactorial interventions were identified in the literature search. These studies are all investigating the effectiveness of multifactorial interventions in high-risk populations in preventing falls after 12 months of follow-up. (96-99)
Summary of Findings of Literature Review
The results of the meta-analyses for the interventions identified in the literature search are summarized below in Tables 16 and 17.
Table 16: Summary of Meta-Analyses of Studies Investigating the Effectiveness of Interventions on the Risk of Falls in Community-Dwelling Seniors*.
| Intervention | RR [95% CI] | |
|---|---|---|
| Exercise programs | ||
| 1. | Targeted programs | |
| General population | 0.81 [0.67–0.98] | |
| High-risk population | 0.93 [0.82–1.06] | |
| Short duration | 0.91 [0.73–1.13] | |
| Long duration | 0.89 [0.79–1.01] | |
| 2. Untargeted programs | ||
| General population | 0.78 [0.66–0.91] | |
| High risk population | 0.89 [0.72–1.10] | |
| Short duration | 0.85 [0.71–1.01] | |
| long duration | 0.76 [0.64–0.91] | |
| 3. Combined targeted vs. untargeted programs | ||
| General population | N/A | |
| High-risk population | 0.87 [0.57–1.34] | |
| Short duration | 1.11 [0.73–1.70] | |
| Long duration | 0.73 [0.57–0.95] | |
| Vision intervention | ||
| Assessment/referral | 1.12 [0.82–1.53] | |
| Cataract surgery | 1.11 [0.92–1.35] | |
| Environmental modifications | ||
| Low-risk population | 1.03 [0.75–1.41] | |
| High-risk population | 0.66 [0.54–0.81] | |
| General population | 0.85 [0.75–0.97] | |
| Drugs/nutritional supplements | ||
| Vitamin D (men and women) | 0.94 [0.77–1.14] | |
| Vitamin D (women only) | 0.55 [0.29–1.08] | |
| Vitamin D and calcium (men and women) | 0.89 [0.74–1.07] | |
| Vitamin D and calcium (women only) | 0.83 [0.73–0.95] | |
| Medication withdrawal | 0.34 [0.16–0.74]† | |
| Gait-stabilizing device | 0.43 [0.29–0.64] | |
| Multifactorial intervention | ||
| Geriatric screening (general population) | 0.87 [0.69–1.10] | |
| High-risk population | 0.86 [0.75–0.98] | |
CI refers to confidence interval; N/A, not applicable; RR relative risk.
Hazard ratio is presented, because relative risk was not reported
Table 17: Summary of meta-analyses of studies investigating the effectiveness of interventions on the risk of fall-related injuries in community-dwelling seniors*.
| Intervention | RR [95% CI] | |
|---|---|---|
| Exercise programs | ||
| Targeted programs | 0.67 [0.51–0.89] | |
| Untargeted programs | 0.57 [0.38–0.86] | |
| Combined targeted vs untargeted programs | 0.31 [0.13–0.74] | |
| Drugs/nutritional supplements | ||
| Vitamin D plus calcium (Women only) | 0.77 [0.49–1.21] | |
| Gait-stabilizing device | 0.10 [0.01–0.74] | |
| Hip protectors | 3.49 [0.68–17.97]† | |
| Multifactorial intervention | ||
| Geriatric screening (general population) | 0.90 [0.53–1.51] | |
| High-risk population | 0.86 [0.66–1.11] | |
CI refers to confidence interval; RR relative risk
Odds ratio is presented, because relative risk could not be calculated
Quality of the Evidence
Table 18: Summary of GRADE Quality Assessment for Exercise Interventions: Stratified by Intervention Length*.
| Intervention | No. of Studies | Quality Assessment | Summary of Findings | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. of Patients | Effect (RR [95% CI]) | |||||||||
| Design | Quality | Consistency | Directness | Other | Interv | Control | Quality | |||
| Exercise (untargeted, long duration) | 8 | RCT | Serious limitations† | Consistent | Direct | None | 462 | 434 | 0.76 [0.64–0.91] |
Moderate |
| High | Moderate | Moderate | Moderate | Moderate | ||||||
| Long duration: targeted | 3 | RCT | No serious limitations | Consistent | Some uncertainty about directness‡ | None | 454 | 456 | 0.89 [0.79–1.01] |
Moderate |
| High | High | High | Moderate | Moderate | ||||||
| Long duration: Combined | 1 | RCT | No serious limitations | Only 1 study | Direct | None | 43 | 27 | 0.73 [0.57–0.95] |
High |
| High | High | High | High | High | ||||||
| Short duration: Untargeted | 10 | RCT | Serious limitations§ | Slightly inconsistent | Direct | None | 1160 | 1070 | 0.85 [0.71–1.01] |
Low |
| High | Moderate | Low | Low | Low | ||||||
| Short duration: Targeted | 2 | RCT | No serious limitations | Consistent | Direct | None | 157 | 158 | 0.91 [0.73–1.13] |
High |
| High | High | High | High | High | ||||||
| Short duration: Combined | 1 | RCT | No serious limitations | Only 1 study | Direct | None | 34 | 34 | 1.11 [0.73–1.70] |
High |
| High | High | High | High | High | ||||||
RR refers to relative risk; CI, confidence interval; Interv, intervention; RCT, randomized controlled trial;
Several studies (100-103) did not describe randomization process and by this omission might conceal biases in study allocation. Heterogeneity in exercise programs.
Table 19: Summary of GRADE Quality Assessment for Exercise Interventions: Stratified by Target Population*.
| Intervention | No. of Studies | Quality Assessment | Summary of Findings | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. of Patients | Effect (RR [95% CI]) | |||||||||
| Design | Quality | Consistency | Directness | Other | Interv | Control | Quality | |||
| General population: Untargeted | 12 | RCT | Serious limitations† | Consistent | Direct | None | 1250 | 1234 | 0.78 [0.66–0.91] | Moderate |
| High | Moderate | Moderate | Moderate | Moderate | ||||||
| General population: Targeted | 3 | RCT | Serious limitations‡ | Consistent | Some uncertainty about directness§ | None | 282 | 284 | 0.81 [0.66–0.98] | Low |
| High | Moderate | Moderate | Low | Low | ||||||
| High-risk population: Untargeted | 6 | RCT | Serious limitations║ | Some inconsistency | Some uncertainty about directness¶ | None | 372 | 270 | 0.89 [0.72–1.10] | Very low |
| High | Moderate | Low | Very low | Very low | ||||||
| High-risk population: Targeted | 2 | RCT | No serious limitations | Consistent | Direct | None | 329 | 330 | 0.93 [0.82–1.06] | High |
| High | High | High | High | High | ||||||
| High-risk population: Combined | 2 | RCT | No serious limitations | Some inconsistency | Direct | None | 77 | 61 | 0.87 [0.57–1.34] | Moderate |
| High | High | Moderate | Moderate | Moderate | ||||||
RR refers to relative risk; CI, confidence interval; Interv, intervention; RCT, randomized controlled trial;
Three studies (102) (100;113) did not describe randomization process, an omission which could conceal biases in study allocation; Exercise programs differed.
One study (114) only 19% randomized; Exercise programs differed.
One study only on older (80+) women (115)
Table 20: Summary of GRADE Quality Assessment for Nutritional Supplementation*.
| Intervention | No. of Studies | Quality Assessment | Summary of Findings | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. of Patients | Effect (RR [95% CI]) | |||||||||
| Design | Quality | Consistency | Directness | Other | Interv | Control | Quality | |||
| Vitamin D: Men and women | 3 | RCT | No serious limitations | Consistent | Direct | None | 383 | 369 | 0.94 [0.77–1.14] | High |
| High | High | High | High | High | ||||||
| Vitamin D: Women | 1 | RCT | Serious limitations† | Only 1 study | Direct | None | 70 | 67 | 0.55 [0.29–1.08] | Moderate |
| High | Moderate | Moderate | Moderate | Moderate | ||||||
| Vitamin D plus calcium: Men and Women | 1 | RCT | Serious limitations† | Only 1 study | Direct | None | 219 | 226 | 0.89 [0.74–1.07] | Moderate |
| High | Moderate | Moderate | Moderate | Moderate | ||||||
| Vitamin D plus calcium: Women | 2 | RCT | No serious limitations | Consistent | Direct | High probability of reporting bias‡ | 720 | 1401 | 0.83 [0.73–0.95] | Moderate |
| High | High | High | High | Moderate | ||||||
| Vitamin D plus calcium: Women Outcome: injurious Falls | 2 | RCT | No serious limitations | Consistent | Direct | High probability of reporting bias‡ | 1313 | 2667 | 0.77 [0.49–1.21] | Moderate |
| High | High | High | High | Moderate | ||||||
| Hormone replacement therapy | 1 | RCT | Serious limitations§ | Only 1 study | Direct | None | 187 | 186 | 0.09 [0.80–1.20] | Moderate |
| High | Moderate | Moderate | Moderate | Moderate | ||||||
| Medication withdrawal | 1 | RCT | No serious limitations | Only 1 study | Major uncertaintyabout directness§ | Sparse data║ Strong evidence of association | 24 | 24 | 0.34 [0.16–0.74]¶ | Low |
| High | High | High | Low | Low | ||||||
RR refers to relative risk; CI, confidence interval; Interv, intervention; RCT, randomized controlled trial
No description of randomization or blinding (although stated “double-blinded RCT”) (74)
In one study, use of vitamin D and calcium by self-report only over a period of 1 to 3 years, and falls outcome reported as interval recall (falls in past year). (121)
Study relied on long recall times (6 months) for falls outcome. (122)
Hazard Ratio
Table 21: Summary of GRADE Quality Assessment for Environmental Modifications*.
| Intervention | No. of Studies | Quality Assessment | Summary of Findings | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. of Patients | Effect (RR [95% CI]) | |||||||||
| Design | Quality | Consistency | Directness | Other | Interv | Control | Quality | |||
| Environmental modification (low-risk seniors) | 1 | RCT | No serious limitations | Only 1 study | Direct | None | 161 | 163 | 1.03 [0.75–1.41] | High |
| High | High | High | High | High | ||||||
| Environmental modification (high-risk seniors) | 3 | RCT | No serious limitations | Consistent | Direct | None | 186 | 188 | 0.66 [0.54–0.81] | High |
| High | High | High | High | High | ||||||
| Environmental modification (all seniors) | 3 | RCT | No serious limitations | Consistent | Direct | None | 581 | 582 | 0.85 [0.75–0.97] | High |
| High | High | High | High | High | ||||||
RR refers to relative risk; CI, confidence interval; Interv, intervention; RCT, randomized controlled trial
Table 22: Summary of GRADE Quality Assessment for Vision Interventions*.
| Intervention | No. of Studies | Quality Assessment | Summary of Findings | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. of Patients | Effect (RR [95% CI]) | |||||||||
| Design | Quality | Consistency | Directness | Other | Interv | Control | Quality | |||
| Vision assessment and referral | 2 | RCT | No serious limitations | Some inconsistency† | Direct | None | 448 | 444 | 1.12 [0.82–1.53] | Moderate |
| High | High | Moderate | Moderate | Moderate | ||||||
| Cataract surgery | 2 | RCT | No serious limitations | Consistent | Some uncertainty about directness‡ | None | 274 | 271 | 1.11 [0.92–1.35] | Moderate |
| High | High | High | Moderate | Moderate | ||||||
Table 23: Summary of GRADE Quality Assessment for Devices*.
| Intervention | No. of Studies | Quality Assessment | Summary of Findings | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. of Patients | Effect (RR [95% CI]) | |||||||||
| Design | Quality | Consistency | Directness | Other | Interv | Control | Quality | |||
| Hip Protector | 1 | RCT | Serious limitations† | Only 1 study | Some uncertainty about directness‡ | None | 139 | 140 | 3.49 (0.68–17.97) | Low |
| High | Moderate | Moderate | Low | Low | ||||||
| Gait-stabilizing device | 1 | RCT | Serious limitations§ | Only 1 study | Some uncertainty about directness║ | Strong evidence of association | 55 | 54 | 0.43 [0.29–0.64] | Moderate |
| High | Moderate | Moderate | Low | Moderate | ||||||
RR refers to relative risk; CI, confidence interval; Interv, intervention; RCT, randomized controlled trial
High dropout in hip protector group; randomization technique not described. (82)
Study population of people with previous hip fracture, therefore may not be generalizable to all seniors. (82)
No information as to whether groups comparable at study entry. (80)
No information on number of people excluded because they couldn’t put on device. This may affect the generalizability and use in the general ambulatory, elderly population. (82)
Table 24: Summary of GRADE Quality Assessment for Multifactorial Interventions.
| Population and Outcome | No. of Studies | Quality Assessment | Summary of Findings | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. of Patients | Effect (RR [95% CI]) | |||||||||
| Design | Quality | Consistency | Directness | Other | Interv | Control | Quality | |||
| Geriatric screening Falls | 6 | RCT | Very serious limitations† | Some Inconsistency | Direct | None | 1430 | 1427 | 0.87 [0.69–1.10] | Very low |
| High | Low | Very low | Very low | Very low | ||||||
| Geriatric screening Injurious falls | 2 | RCT | Very serious limitations‡ | Some Inconsistency | Direct | None | 845 | 811 | 0.90 [0.53–1.51] | Low |
| High | Moderate | Low | Low | Low | ||||||
| High risk Falls | 10 | RCT | Serious limitations§ | Some inconsistency | Direct | None | 1301 | 1309 | 0.91 [0.75–0.98] | Low |
| High | Moderate | Low | Low | Low | ||||||
| High risk Injurious falls | 4 | RCT | Serious limitations║ | Consistent | Direct | None | 624 | 639 | 0.85 (0.63–1.17) | Moderate |
| High | Moderate | Moderate | Moderate | Moderate | ||||||
RR refers to relative risk; CI, confidence interval; Interv, intervention; RCT, randomized controlled trial.
No blinding of outcome assessors in 4 studies; (130-133) high dropout in 2 studies; (134;135) fall outcome based on recall at end of study for 4 studies; (133;136-138) randomization technique not described in study by Jitapunkul et al. (139)
Recall required for falls outcome and no blinding or intention-to-treat analysis in one study (133)
Feedback from Expert Panel
The systematic review on falls and fall-related injuries was presented at two expert panel meetings (January 23, 2008, and May 16, 2008). The panel contextualized the evidence and identified several important issues to consider. The following is a summary of comments that were made:
Medication Withdrawal
Medication withdrawal involves a fine balance between benefit and risk, and cannot be as accurately implemented as other initiatives.
There are not enough best practice guidelines for medication withdrawal in seniors.
As a general rule, psychotropic medications are not prescribed unless there are specific needs (such as wandering, inability to sleep, hitting, and other abusive behaviour). In these cases, it is difficult (and perhaps inappropriate) to withdraw this medication since doing so can greatly increase caregiver burden.
A discussion followed that indicated that inadequate training of caregivers to deal with behaviours in seniors may increase the reliance on psychotropic medications. Perhaps if proper training were provided, medication withdrawal could be more successful.
In a home setting, individual compliance with taking psychotropic medications can be low and requires caregiver support for reminders.
Causes of Falls and Injury in Seniors
Many injurious falls occur around indoor stairs, and therefore the proper design of stairs and appropriate handrails (shape, diameter, and height) should be investigated.
Injuries following falls from ladders frequently occur in seniors (largely due to cleaning of eavestroughs and windows). Ladders with hoops or services to clean eavestroughs and windows for seniors should be considered.
Falls on sidewalks and road crossings are frequent, particularly in the winter. With the deteriorating condition of street clearing, this is becoming a larger issue.
Fear of falling is another important cause of falls since it perpetuates a cycle of immobility, followed by deconditioning and falls.
Falls in the Winter
-
In the winter, several factors reduce the likelihood that an elderly person will go outdoors:
Seniors are most likely to go out during daylight hours, which are fewer.
Fear of slipping on the ice and snow reduces the likelihood of an elderly person choosing to go outdoors unless it is absolutely necessary.
Poorly designed coats and boots make it difficult for seniors with difficulty moving or with lowered flexibility to dress for the outdoors.
These factors can lead to lowered fitness levels, which in turn leads to an increased likelihood of falls both indoors and outdoors.
Furthermore, in the colder months, people tend to walk faster when outdoors, which can increase the likelihood that an individual will fall.
Mobility Aids
At both meetings, the issues of mobility aids was raised by experts on the panel. Regrettably it is very rare to find published trials investigating the effectiveness of mobility aids, and therefore it was not appropriate to include this as a section of this literature review. However, the panel felt that it was important to discuss these aids and their use in reducing falls and fall-related injuries in the elderly population, and that more work should be done to improve existing mobility devices.
-
Mobility aids that were discussed as being effective included
wheeled walkers – while wheeled walkers can decrease the frequency of falls, the panel mentioned that walkers must be properly designed to ensure the best stability and that poorly designed walkers can actually increase the likelihood of falls.
handrails that are at an appropriate height, are cylindrical and are easy to see and grab
raised toilet seats to decrease falls that occur when sitting at and standing up from the toilet
grab bars, particularly in washrooms
While mobility aids are an important tool to reduce falls in community-dwelling seniors, when renovations are not done to an appropriate standard, they can actually increase home hazards and risk of falling. Therefore, it was felt that elderly populations should be provided with access to affordable high-standard renovations.
Emergency buttons that act as a lifeline after a fall were discussed. Because quick access to help can prevent long-term complications and disabilities, it was argued that these emergency buttons are highly effective in elderly populations, although it was suggested that uptake of the technology may be limited, based on reports that many people forget after a fall that they have access to these buttons.
Follow-Up to Comments Made by Expert Panel
Following the expert panel meeting, a literature search was performed to attempt to identify any literature surrounding the effectiveness of mobility devices. It was confirmed that there is very little evidence surrounding mobility devices in the published literature. One recent Canadian study was identified which described current fall-prevention interventions in seniors. (151) This paper described a handrail cueing system, balance-enhancing footwear inserts, and a modified walking aid. The results of these studies indicated that the balance-enhancing footwear inserts improved the ability to stabilize one’s body and may reduce the number of falls, while more research is needed in an elderly population to determine whether an extended arched walker can increase stability in seniors. A study is currently underway to test the effectiveness of handrail cueing systems (both visual and combined visual and verbal cueing) on handrail use and reaching reactions.
In response to the discussion regarding the reasons for falls in the elderly population, the Medical Advisory Secretariat analyzed fall-related data for FY2006/07 on inpatient hospitalization of and emergency department use by elderly Ontarians. Hospitalizations with an external cause recorded as a fall were extracted for Ontarians aged 65 and over between April 1, 2006, and March 31, 2007. The resulting distribution of cause of falls appears in Table 25. This table indicates that mobility devices and furniture are frequently reported as the causes of falls in seniors going to the emergency department, and those admitted to hospital. Additionally, outdoor falls involving ice and snow, falls involving ladders, and falls involving stairs and steps explain 13.0% of hospitalizations for falls and 15.7% of emergency department visits for falls among Ontario’s seniors.
Table 25: Distribution of the Cause of Falls in Hospitalizations for Elderly (Aged 65+) Ontarians (FY2006/2007)*.
| ED Visits | Hospitalizations | |||||
|---|---|---|---|---|---|---|
| Type of Fall | % of all falls |
% of specified falls† |
N‡ | % of all falls |
% of specified falls† |
N‡ |
| Fall involving mobility devices | ||||||
| Fall involving adult walker | 1.55 | 2.13 | 1,410 | 2.10 | 2.88 | 518 |
| Fall involving wheelchair | 1.23 | 1.69 | 1,119 | 1.21 | 1.65 | 298 |
| Fall involving other specified walking devices | 0.09 | 0.12 | 79 | 0.13 | 0.17 | 31 |
| Fall involving unspecified walking devices | 0.01 | 0.02 | 12 | – | – | ≤5 |
| Outdoor Fall | ||||||
| Fall on same level involving ice and snow | 3.69 | 5.08 | 3,359 | 2.72 | 3.73 | 671 |
| Fall from tree | 0.06 | 0.08 | 51 | 0.06 | 0.08 | 15 |
| Fall from scaffolding | 0.04 | 0.05 | 32 | 0.03 | 0.04 | 8 |
| Fall involving playground equipment | 0.01 | 0.01 | 9 | – | – | ≤5 |
| Fall involving furniture | ||||||
| Fall involving bed | 3.87 | 5.32 | 3,520 | 5.00 | 6.85 | 1,233 |
| Fall involving chair | 2.08 | 2.86 | 1,892 | 2.09 | 2.86 | 515 |
| Fall involving other furniture | 0.59 | 0.81 | 537 | 0.52 | 0.71 | 128 |
| Fall involving baby walker | – | – | ≤5 | – | – | ≤5 |
| Other Falls | ||||||
| Fall on the same level from slip, trip, or stumble | 32.44 | 44.66 | 29,540 | 32.72 | 44.81 | 8,070 |
| Unspecified fall | 27.36 | N/A | 24,907 | 26.99 | N/A | 6,658 |
| Other fall on same level | 13.31 | 18.32 | 12,118 | 14.85 | 20.35 | 3,664 |
| Fall on and from stairs and steps | 10.19 | 14.02 | 9,276 | 8.78 | 12.02 | 2,165 |
| Fall on and from ladder | 1.81 | 2.49 | 1,647 | 1.51 | 2.07 | 372 |
| Other fall from one level to another | 1.47 | 2.02 | 1,335 | 0.99 | 1.35 | 244 |
| Fall out of/through building structure | 0.22 | 0.31 | 203 | 0.29 | 0.39 | 71 |
ED indicated emergency department; N, number.
Excludes “Unspecified fall” from denominator
To maintain privacy, all cell sizes of 5 or less are suppressed
Source: The Ministry of Health and Long-Term Care, Provincial Health Planning Database
Conclusions
High-quality evidence indicates that long-term exercise programs in mobile seniors and environmental modifications in the homes of frail elderly persons will effectively reduce falls and possibly fall-related injuries in Ontario’s elderly population.
A combination of vitamin D and calcium supplementation in elderly women will help reduce the risk of falls by more than 40%.
The use of outdoor gait-stabilizing devices for mobile seniors during the winter in Ontario may reduce falls and fall-related injuries; however, evidence is limited and more research is required in this area.
While psychotropic medication withdrawal may be an effective method for reducing falls, evidence is limited and long-term compliance has been demonstrated to be difficult to achieve.
A multifactorial intervention, including a combination of fall prevention interventions such as exercise, medication withdrawal, environmental modifications, vision and hearing interventions may reduce the risk of falls in high-risk populations. However, the quality of the evidence in this area is low, and included interventions are varied. Therefore more research is needed into the most appropriate and effective multifactorial intervention design.
Appendices
Appendix 1: Search Strategies
Search date: October 2, 2007
Databases searched: OVID MEDLINE, MEDLINE In-Process and Other Non-Indexed Citations, EMBASE, CINAHL, Cochrane Library, INAHTA/NHS EED
Database: Ovid MEDLINE(R) <1996 to September Week 3 2007>
Search Strategy:
--------------------------------------------------------------------------------
exp Accidental Falls/pc [Prevention & Control] (2140)
exp Accidental Falls/ (6124)
-
exp Accident Prevention/ or exp Primary Prevention/ or exp risk reduction behavior/ or exp
Preventive Health Services/ or exp Preventive Medicine/ (172856)
2 and 3 (718)
(fall$ adj4 prevent$).mp. [mp=title, original title, abstract, name of substance word, subject heading word] (1416)
1 or 4 or 5 (2961)
limit 6 to (humans and english language and yr=“2000 - 2007”) (1906)
limit 7 to “all aged (65 and over)” (1259)
(elder$ or senior$).mp. [mp=title, original title, abstract, name of substance word, subject heading word] (71440)
7 and (8 or 9) (1292)
limit 10 to (controlled clinical trial or meta analysis or randomized controlled trial) (200)
(meta analy$ or metaanaly$ or pooled analysis or (systematic$ adj2 review$)).mp. or (published studies or published literature or medline or embase or data synthesis or data extraction or cochrane).ab. (54569)
exp Random Allocation/ or random$.mp. [mp=title, original title, abstract, name of substance word, subject heading word] (326025)
exp Double-Blind Method/ (48004)
exp Control Groups/ (493)
exp Placebos/ (8371)
RCT.mp. (1998)
or/11-17 (366985)
10 and 18 (296)
Database: EMBASE <1980 to 2007 Week 39>
Search Strategy:
--------------------------------------------------------------------------------
exp Falling/pc [Prevention] (2)
exp Falling/ (9062)
exp prevention/ or exp Preventive Health Service/ or exp Preventive Medicine/ or exp Risk Reduction/ (456395)
2 and 3 (1568)
(fall$ adj4 prevent$).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] (2198)
1 or 4 or 5 (2963)
limit 6 to (human and english language and yr=“2000 - 2008”) (1351)
limit 7 to aged <65+ years> (661)
(senior$ or elder$).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] (115074)
8 or 9 (115397)
7 and 10 (797)
Randomized Controlled Trial/ (149282)
exp Randomization/ (24000)
exp RANDOM SAMPLE/ (792)
(meta analy$ or metaanaly$ or pooled analysis or (systematic$ adj2 review$)).ti,mp. or (published studies or published literature or medline or embase or data synthesis or data extraction or cochrane).ab. (76601)
Double Blind Procedure/ (66657)
exp Triple Blind Procedure/ (8)
exp Control Group/ (1007)
exp PLACEBO/ (104532)
(random$ or RCT).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] (386635)
or/12-20 (511379)
11 and 21 (238)
Database: CINAHL - Cumulative Index to Nursing & Allied Health Literature <1982 to September Week 4 2007>
Search Strategy:
--------------------------------------------------------------------------------
exp Accidental Falls/pc [Prevention and Control] (2193)
exp Accidental Falls/ (4650)
exp “FALL PREVENTION (IOWA NIC)”/ (1)
exp Preventive Health Care/ (73373)
exp SAFETY/ (37546)
or/3-5 (109313)
2 and 6 (972)
1 or 7 (2510)
(fall$ adj4 prevent$).mp. [mp=title, subject heading word, abstract, instrumentation] (1057)
8 or 9 (2776)
limit 10 to (english and yr=“2000 - 2007”) (1916)
random$.mp. or exp RANDOM ASSIGNMENT/ or exp RANDOM SAMPLE/ (60536)
RCT.mp. (736)
exp Meta Analysis/ (5696)
exp “Systematic Review”/ (3320)
(meta analy$ or metaanaly$ or pooled analysis or (systematic$ adj2 review$) or published studies or medline or embase or data synthesis or data extraction or cochrane).mp. (19960)
exp double-blind studies/ or exp single-blind studies/ or exp triple-blind studies/ (11524)
exp PLACEBOS/ (3799)
or/12-18 (78869)
11 and 19 (222)
Appendix 2: GRADE Score for the Body of Evidence
| Number of Studies | Study Design |
Quality of Studies |
Consistency | Directness | Other Modifying Factors |
|---|---|---|---|---|---|
| N | RCT=High Observational = Low Any other evidence = Very Low |
Serious limitation to study quality (−1) Very serious limitation to study quality (−2) |
Important inconsistency (−1) | Some uncertainty about directness (−1) Major uncertainty about directness (−2) |
Association strong (+1) Association very strong (+2) Dose response gradient (+1) All plausible confounders would have reduced the effect (+1) Imprecise or sparse data (−1) High probability of reporting bias (−1) |
Source: Atkins D et al. Grading quality of evidence and strength of recommendations. BMJ 2004;328(7454):1490. (46)
Appendix 3: Study Characteristics
Exercise Interventions – Summary of Evidence*
| Study | Population | Intervention and Referent Group | Intensity (No. Times/Week) | Targeted or Untargeted | Follow-Up | Outcomes Measured | Results |
|---|---|---|---|---|---|---|---|
| Gillespie: Cochrane Review (2003) (44) |
|
Exercise alone vs. control | Varied |
|
Varied | Number of falls | Meta-analysis results:
|
|
Varied | Number sustaining injury fall | Meta-analysis results:
|
||||
|
Varied | Number sustaining 2 or more falls | Meta-analysis results:
|
||||
| Barnett (2003) (152) |
|
Exercise (balance, coordination, strength, tai chi) vs. control | 37 classes over 1 year 1 h |
Untargeted, Group and Home | 12 months | Falls, fear of falling, fall injuries | No difference in fear of falling at 6 months Falls:
Fall injuries – no difference:
|
| Day (2002)† (153) |
|
Strength and balance (n=135) vs. control (n=137) | 1x/week for 15 weeks 1h Daily home exercises | Untargeted, group and home | 18 months | Number of falls |
|
| Freiberger (2007) (154) |
|
Psychomotor intervention vs. fitness intervention (strength, endurance, flexibility) vs. control | 2x/week for 16 weeks 1h Practice at home daily |
Untargeted, Group and home (unsupervised) | 12 months | Number falls, fallers, multiple fallers | Fitness Intervention:
Psychomotor intervention:
Time to first fall:
|
| Hauer (2001) (155) |
|
Resistance and balance training vs. placebo activity (flexibility, calisthenics, ball games, memory tasks) | 3 days/week for 12 weeks 1.5 h resistance 45 min balance | Untargeted, Group | 6 months | falls |
|
| Helbostad (2004) (156) |
|
Home-based (HT) exercise vs. group exercise (CT) | HT: Daily home exercises + 3 group meetings CT: 2x/wk for 12 weeks (1hr) + same home exercises as HT group daily | Targeted vs. untargeted, Group vs. home | 1 year | Number of falls |
|
| Latham (2003) (157) |
|
Quadriceps exercise program (home) vs. regular home and telephone support | 3/week for 10 weeks | Targeted, Home | 10-week intervention plus 6-month follow-up | Falls, time to first fall | Falls outcome:
|
| Li (2005) (158) |
|
Tai chi intervention vs. stretching control | 3x/week for 6 months (both intervention and control) | Untargeted, Group | After intervention, and 6 months postintervention | Number of falls, injurious falls, fear of falling | After intervention
|
| Luukinen (2006) (159) |
|
Individual exercise plan (could be home or group-based) based on risk factors (low-intensity) vs. control (no exercise plan) | Varied | Targeted, group, and home depending on assessment | Median 16 months’ intervention | Falls | Entire group:
Subgroup: able to move outdoors:
|
| Means (2005) (160) |
|
Balance training (stretching, postural control, endurance) vs. control (attended seminars on non-health-related topics) | 1x/week 6 weeks | Untargeted, Group (6–8 people) | 6 months postintervention | Falls, fall-related injuries |
|
| Robertson (2001)† (161) |
|
Exercise program vs. control | Exercise at least 3x/week, walk 2x/week; 30 min For 1 year | Targeted, home | 1 year | Number of falls, number injuries from falls |
|
| Rubenstein (2000) †(162) |
|
Exercise (strength, endurance and balance) vs. control | 3x/week for 12 weeks 1.5 h | Untargeted, group | 12 weeks | Falls, self-rated health |
|
| Skelton (2005) (163) |
|
Falls management exercise (group and home) vs. regular home exercises | 36 weeks of class Group: 1/week for 1 h Home: 2/week for 30 minutes |
Targeted, Group, and Home (unsupervised) | 36-wk intervention plus mean 49.7-wk follow-up | Falls, injurious falls, died/LTC home/hospital |
|
| Suzuki (2004) (100) |
|
Exercise (tai chi, strength, balance, resistance) vs. control | Group: 1 h every 2 weeks for 6 months Home: 3/wk for ~30 minutes |
Untargeted, Group and Home (unsupervised) | 8 and 20 months | falls |
|
| Voukelatos (2007) (164) |
|
Tai chi vs. control | 1 time/week for 16 weeks 1 hour | Untargeted, Group | 4 and 6 months | Falls, ≥1 fall, ≥2 falls |
|
| Weerdesteyn (2006) (111) |
|
Nijmegen Falls Prevention Program: low-intensity exercise vs. control | 2x/week for 5 weeks 1.5 h | Untargeted, Group | Unclear | Falls |
*note: not completely randomized |
| Woo (2007) (165) |
|
|
3 times/week for 12 months | Untargeted, Group | 6 and 12 months | Falls |
|
HR refers to hazard ratio; IRR, incidence rate ratio; RCT, randomized controlled trial; RR, relative risk.
Also identified in Cochrane review
Vision Interventions – Summary of Evidence*
| Study | Population | Intervention | Follow-Up | Outcomes Measured | Results |
|---|---|---|---|---|---|
| Cumming (2007) (166) |
|
|
12 months | Falls, fallers, multiple fallers, fractures |
not blinded |
| Day (2002) (167) |
|
|
18 months | Number of fallers |
|
| Foss (2006) (168) |
|
|
12 months | Falls, ADLs, QoL, Rate of falling |
|
| Harwood (2005) (169) |
|
|
12 months | Falls, ADLs, QoL, Rate of falling |
|
ADLs refers to activities of daily living; GP, general practitioner; HR, hazard ratio; OT, occupational therapist; QoL, quality of life; RR, relative risk.
Environmental Modifications: Summary of Evidence*
| Study | Population | Intervention and Referent Group (N) | Number of Visits and Description of Intervention | Personnel (e.g., Nurse, OT) | Follow-Up | Outcomes Measured | Results |
|---|---|---|---|---|---|---|---|
| Gillespie: Cochrane Review (2003) (44) |
Fallers in year prior (n=3 studies) No falls in year prior (n=1) Fallers and non-fallers in year prior (n=3) |
Home safety intervention alone vs. control |
|
Varied | Varied | Number of people falling | Results from meta-analysis: Fallers in year prior RR: 0.66 (0.54–0.81) No falls in year prior, RR: 1.03 (0.75–1.41) Fallers and non-fallers in year priorRR: 0.85 (0.74–0.96) |
| Day (2002) †(170) |
|
Home hazard intervention (n=135) vs. no intervention (n=137) |
|
Trained assessor | 18 months | Number of falls, number of home hazards |
|
| Nikolaus (2003)† (58) |
|
Home intervention team (N=140) vs. control (N=139) |
|
Nurse, physiotherapist, occupational therapist, social worker | 1 year | Death or nursing home placement, number of falls |
|
| Pardessus (2002)† (171) |
|
Home visit to assess environmental modifications(N=30) vs. control(N=30) |
|
Physical medicine and rehabilitation doctor, ergotherapist and hospital social worker | Every month for 6 months, and at 12 months | Fall, hospital admission, LTC home admission, death |
|
IRR refers to incidence rate ratio; no., number; OT, occupational therapist; RCT, randomized controlled trial; RR, relative risk;
Also identified in Cochrane review
Nutritional Supplementation: Summary of Evidence*
| Study | Population | Intervention, dose | Follow-Up | Outcomes measured | Results |
|---|---|---|---|---|---|
| Gillespie: Cochrane Review (2003) (44) |
|
Vitamin D vs. control (2 studies) | Varied | Fallers, mean number of falls | Results from meta-analysis
|
| Gillespie (2003): Cochrane Review |
|
Psychotropic medication withdrawal (1 study – Campbell 1999) | 44 weeks | Fallers |
|
| Barr (2005) (172) |
|
|
1 to 3 years (median follow-up 28.9 months) | Fallers, number of people sustaining a fracture |
|
| Bischoff (2006) (76) |
|
|
3 years | Faller (stratified by gender) |
|
| Dhesi (2004) (173) |
|
|
6 months | Fallers, falls |
|
| Dukas (2004) (174) |
|
|
36 weeks | Fallers |
|
| Greenspan (2005) (175) |
|
|
3 years | Falls |
|
| Latham (2003) (176) |
|
|
6 months | Falls, time to first fall | Falls Outcome:
|
| Porthouse (2005) (177) |
|
|
Median follow-up 25 months | All fractures, hip fractures, falls, fear of falling |
|
HR refers to hazard ratio; HRT, hormone replacement therapy; OR, odds ratio; RCT, randomized controlled trial; RR, relative risk.
Devices: Summary of Evidence*
| Study | Device | Population | Intervention | Follow-Up | Outcomes Measured | Results |
|---|---|---|---|---|---|---|
| McKiernan (2005) (80) | Gait-stabilizing device (Yaktrax Walker®) |
|
|
Winter 2003/2004: 10,724 observation-days | Number indoor and outdoor slip falls and injurious falls |
All days:
Days walked on snow/ice:
outdoor fall: NNP, 3 outdoor slip: NNP, 1 |
| Birks (2003) (82) | Hip protector (Safehip®) |
|
|
Median follow-up 14 months | Number of second hip fractures, number falls, fear of falling, compliance |
|
RR refers to relative risk; NNP, number needed to prevent; OR, odds ratio
Multifactorial Interventions: Summary of Evidence*
| Study | Population | Intervention | Follow-Up, Number Contacts During Follow-Up | Outcomes Measured | Results |
|---|---|---|---|---|---|
| Gillespie: Cochrane Review (2003) (44) |
|
|
Varied | Number fallers, number injurious falls, number fractures | All Elderly
High-risk Population
|
| Clemson (2004) (178) |
|
|
|
Falls, falls efficacy scale (fear of falling), worry scale |
|
| Davison (2005) (179) |
|
|
|
Number of falls, number who fell, injury rates, hospital admission, mortality, fear of falling |
|
| Huang (2005) (180) |
|
|
|
Length of initial hospital stay, rate of readmission to hospital, rate of repeat falls, rate of survival, QoL |
|
| Lord (2005) (83) |
|
Extensive Intervention Group (EIG):
Minimal intervention Group (MIG):
Control group (CG):
|
|
Falls, injurious falls |
EIG vs. CG
MIG vs. CG
|
| Mahoney (2007) (181) |
|
Controls:
Intervention
|
|
Accidental fall rate (denominator excluded any days in hospital or LTC home), all-cause hospitalization, LTC home admission, days in LTC home |
Hosp: RR, 1.05, P = .82) LTC: RR, 0.72 (0.38–1.35) Subgroup analyses
|
| Rubenstein (2007) (182) |
|
|
|
Falls, UI, mental health, hospital and nursing home admission |
|
| Tinetti (1994) (183) |
|
|
|
Falls, serious injuries |
|
| Whitehead (2003) (93) |
|
Intervention:
|
|
Falls, uptake of interventions |
|
| Sjosten (2007)(184)In progress |
|
|
12 months | Fall incidence, injurious falls |
|
| Elley (2007) (99) In progress |
|
Control Group:
Intervention Group
|
12 months | Fall incidence, self-efficacy (fear of falling) level of physical activity, ADLs |
|
| Hendriks (2005)(185)In progress |
|
|
Maximum intervention of 3.5 months 1 year follow-up | Falls, recurrent falls (2 or more), injurious falls, QoL |
|
| Peeters (2007)(96)In progress |
|
|
12 months 2 home visits, with measurements taken at 3, 6, 9, and 12 months | Number of falls, time to first fall, QoL, ADLs |
|
ADLs refers to activities of daily living; CG, control group; CI, confidence interval; ED, emergency department; EIG, extensive intervention group; LTC, long-term care; LOS, length of stay; MIG, minimal intervention group; OR, odds ratio; OT, occupational therapist; PT, physical therapist; QoL, quality of life; RCT, randomized controlled trial; RR, relative risk; UI, urinary incontinence.
Appendix 4: Forest Plots
Figure 1: Evidence Surrounding the Risk of Falls After an Exercise Program.
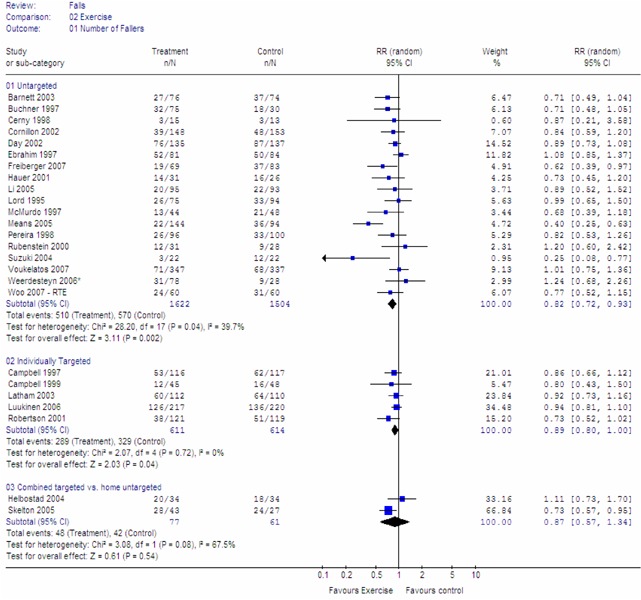
Figure 2: Evidence Surrounding the Risk of Falls After an Exercise Program: High-Risk Population.
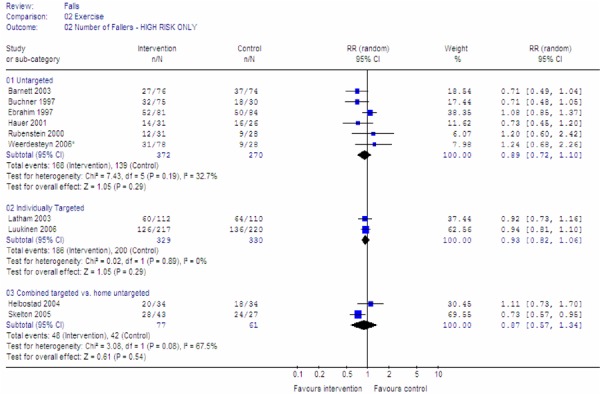
Figure 3: Evidence Surrounding the Risk of Falls After an Exercise Program: General Population.
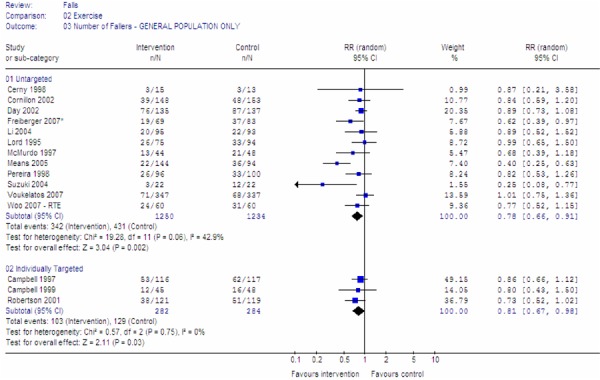
Figure 4: Evidence Surrounding the Risk of Fall-Related Injuries After an Exercise Program: General Population.
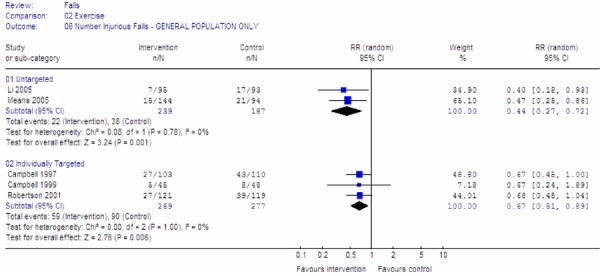
Figure 5: Evidence Surrounding the Risk of Falls After an Exercise Program: Short Intervention (<6 months).
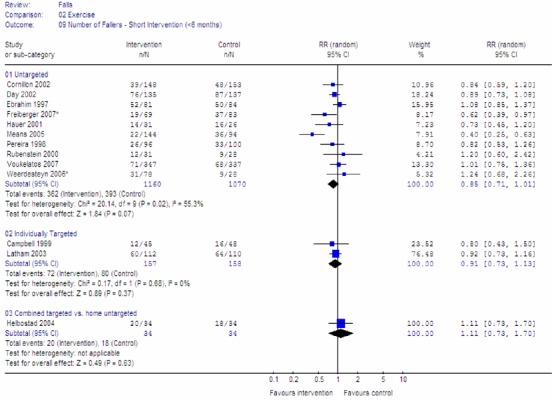
Figure 6: Evidence Surrounding the Risk of Falls After an Exercise Program: Long Intervention (≥6 months).
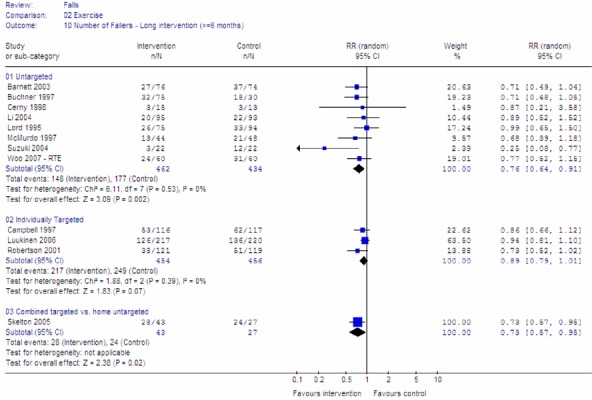
Figure 7: Evidence Surrounding the Risk of Fall-Related Injuries After an Exercise Program: Long Intervention (≥6 months).
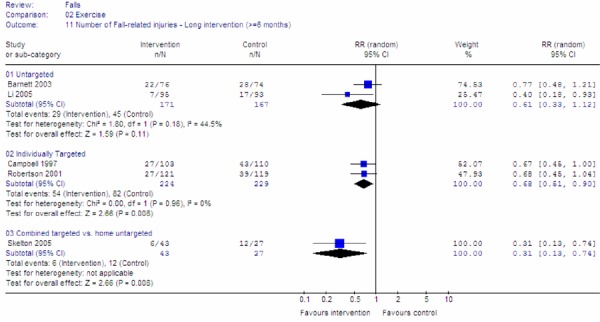
Figure 8: Evidence Surrounding the Risk of Falls After Vision Interventions.
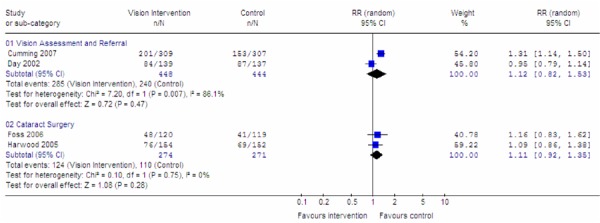
Figure 9: Evidence Surrounding the Risk of Falls After Environmental Modifications.
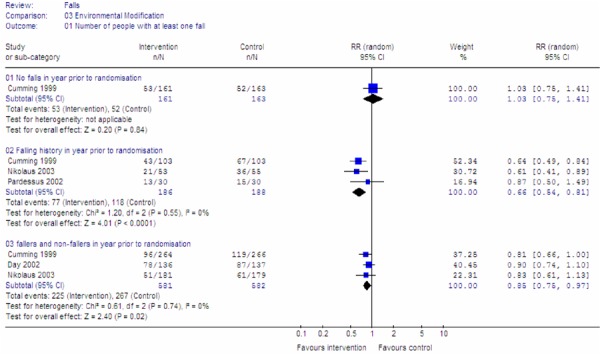
Figure 10: Evidence Surrounding the Risk of Falls After Vitamin D Supplementation.
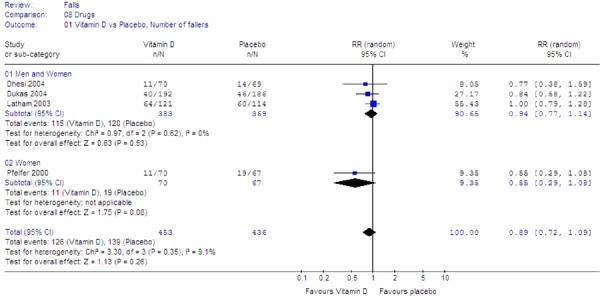
Figure 11: Evidence Surrounding the Risk of Falls After Vitamin D and Calcium Supplementation.
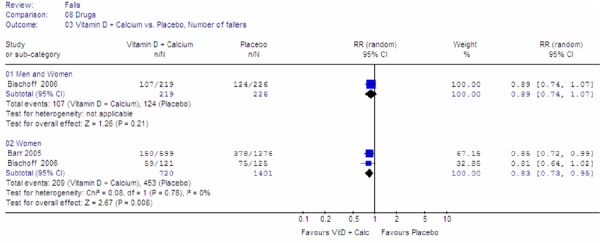
Figure 12: Evidence Surrounding the Risk of Fall-Related Fractures After Vitamin D and Calcium Supplementation.
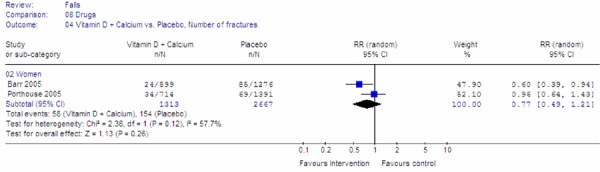
Figure 13: Evidence Surrounding the Risk of Falls After Hormone Replacement Therapy.
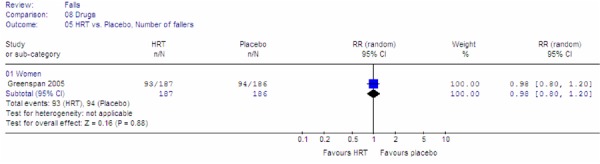
Figure 14: Evidence Surrounding the Risk of Falls After Multifactorial Interventions (Excluding Study by Whitehead et al. (93)).
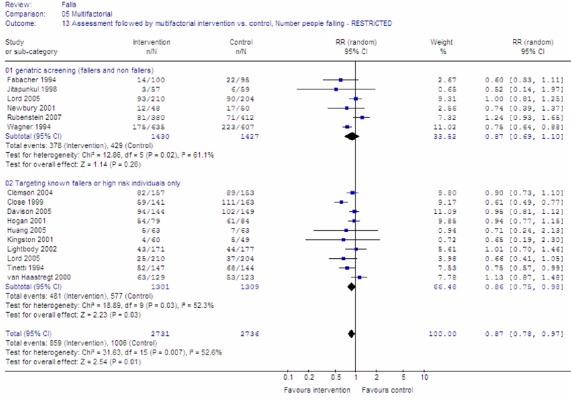
Figure 15: Evidence Surrounding the Risk of Fall-Related Injuries After Multifactorial Interventions.
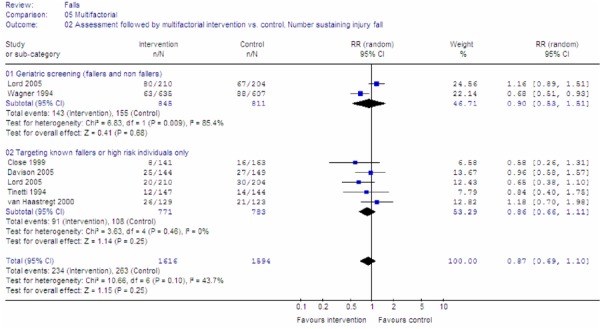
Suggested Citation
This report should be cited as follows:
Medical Advisory Secretariat. Prevention of falls and fall-related injuries in community-dwelling seniors: an evidence-based analysis. Ontario Health Technology Assessment Series 2008;8(2).
Permission Requests
All inquiries regarding permission to reproduce any content in the Ontario Health Technology Assessment Series should be directed to MASinfo.moh@ontario.ca.
How to Obtain Issues in the Ontario Health Technology Assessment Series
All reports in the Ontario Health Technology Assessment Series are freely available in PDF format at the following URL: www.health.gov.on.ca/ohtas.
Print copies can be obtained by contacting MASinfo.moh@ontario.ca.
Conflict of Interest Statement
All analyses in the Ontario Health Technology Assessment Series are impartial and subject to a systematic evidence-based assessment process. There are no competing interests or conflicts of interest to declare.
Peer Review
All Medical Advisory Secretariat analyses are subject to external expert peer review. Additionally, the public consultation process is also available to individuals wishing to comment on an analysis prior to finalization. For more information, please visit http://www.health.gov.on.ca/english/providers/program/ohtac/public_engage_overview.html.
Contact Information
The Medical Advisory Secretariat
Ministry of Health and Long-Term Care
20 Dundas Street West, 10th floor
Toronto, Ontario
CANADA
M5G 2N6
Email: MASinfo.moh@ontario.ca
Telephone: 416-314-1092
ISSN 1915-7398 (Online)
ISBN 978-1-4249-8015-4 (PDF)
About the Medical Advisory Secretariat
The Medical Advisory Secretariat is part of the Ontario Ministry of Health and Long-Term Care. The mandate of the Medical Advisory Secretariat is to provide evidence-based policy advice on the coordinated uptake of health services and new health technologies in Ontario to the Ministry of Health and Long-Term Care and to the healthcare system. The aim is to ensure that residents of Ontario have access to the best available new health technologies that will improve patient outcomes.
The Medical Advisory Secretariat also provides a secretariat function and evidence-based health technology policy analysis for review by the Ontario Health Technology Advisory Committee (OHTAC).
The Medical Advisory Secretariat conducts systematic reviews of scientific evidence and consultations with experts in the health care services community to produce the Ontario Health Technology Assessment Series.
About the Ontario Health Technology Assessment Series
To conduct its comprehensive analyses, the Medical Advisory Secretariat systematically reviews available scientific literature, collaborates with partners across relevant government branches, and consults with clinical and other external experts and manufacturers, and solicits any necessary advice to gather information. The Medical Advisory Secretariat makes every effort to ensure that all relevant research, nationally and internationally, is included in the systematic literature reviews conducted.
The information gathered is the foundation of the evidence to determine if a technology is effective and safe for use in a particular clinical population or setting. Information is collected to understand how a new technology fits within current practice and treatment alternatives. Details of the technology’s diffusion into current practice and input from practicing medical experts and industry add important information to the review of the provision and delivery of the health technology in Ontario. Information concerning the health benefits; economic and human resources; and ethical, regulatory, social and legal issues relating to the technology assist policy makers to make timely and relevant decisions to optimize patient outcomes.
If you are aware of any current additional evidence to inform an existing evidence-based analysis, please contact the Medical Advisory Secretariat: MASinfo.moh@ontario.ca. The public consultation process is also available to individuals wishing to comment on an analysis prior to publication. For more information, please visit http://www.health.gov.on.ca/english/providers/program/ohtac/public_engage_overview.html.
Disclaimer
This evidence-based analysis was prepared by the Medical Advisory Secretariat, Ontario Ministry of Health and Long-Term Care, for the Ontario Health Technology Advisory Committee and developed from analysis, interpretation, and comparison of scientific research and/or technology assessments conducted by other organizations. It also incorporates, when available, Ontario data, and information provided by experts and applicants to the Medical Advisory Secretariat to inform the analysis. While every effort has been made to reflect all scientific research available, this document may not fully do so. Additionally, other relevant scientific findings may have been reported since completion of the review. This evidence-based analysis is current to the date of publication. This analysis may be superseded by an updated publication on the same topic. Please check the Medical Advisory Secretariat Website for a list of all evidence-based analyses: http://www.health.gov.on.ca/ohtas.
List of Tables
| Executive Summary Table 1: Summary of Meta-Analyses of Studies Investigating the Effectiveness of Interventions on the Risk of Falls in Community-Dwelling Seniors* |
| Executive Summary Table 2: Summary of Meta-Analyses of Studies Investigating the Effectiveness of Interventions on the Risk of Fall-Related Injuries in Community-Dwelling Seniors* |
| Table 1: Hazard Ratios for Admission to a Long-term Care Home Following Falls and Fall-related Injuries* |
| Table 2: Quality of Evidence of Included Studies* |
| Table 3: Summary of Evidence Surrounding the Risk of Falls After an Exercise Program: High-Risk Population* |
| Table 4: Summary of Evidence Surrounding the Risk of Falls After an Exercise Program: General Population* |
| Table 5: Summary of Evidence Surrounding the Risk of Fall-Related Injuries After an Exercise Program: General Population* |
| Table 6: Summary of Evidence Surrounding the Risk of Falls After an Exercise Program: Short Intervention (<6 months)* |
| Table 7: Summary of Evidence Surrounding the Risk of Falls After an Exercise Program: Long Intervention (≥6 months)* |
| Table 8: Summary of Evidence Surrounding the Risk of Fall-Related Injuries After an Exercise Program: Long Intervention (≥6 months)* |
| Table 9: Summary of Evidence Surrounding the Risk of Falls After Vision Interventions* |
| Table 10: Summary of Evidence Surrounding the Risk of Falls After Environmental Modifications* |
| Table 11: Summary of Evidence Surrounding the Risk of Falls After Supplementation with Vitamin D* |
| Table 12: Summary of Evidence Surrounding the Risk of Falls After Supplementation with Vitamin D and Calcium |
| Table 13: Summary of Evidence Surrounding the Risk of Fall-Related Fractures After Supplementation with Vitamin D and Calcium* |
| Table 14: Summary of Evidence Surrounding the Risk of Falls After a Multifactorial Intervention* |
| Table 15: Summary of Evidence Surrounding the Risk of Fall-Related Injuries After a Multifactorial Intervention* |
| Table 16: Summary of Meta-Analyses of Studies Investigating the Effectiveness of Interventions on the Risk of Falls in Community-Dwelling Seniors* |
| Table 17: Summary of meta-analyses of studies investigating the effectiveness of interventions on the risk of fall-related injuries in community-dwelling seniors* |
| Table 18: Summary of GRADE Quality Assessment for Exercise Interventions: Stratified by Intervention Length* |
| Table 19: Summary of GRADE Quality Assessment for Exercise Interventions: Stratified by Target Population* |
| Table 20: Summary of GRADE Quality Assessment for Nutritional Supplementation* |
| Table 21: Summary of GRADE Quality Assessment for Environmental Modifications* |
| Table 22: Summary of GRADE Quality Assessment for Vision Interventions* |
| Table 23: Summary of GRADE Quality Assessment for Devices* |
| Table 24: Summary of GRADE Quality Assessment for Multifactorial Interventions |
| Table 25: Distribution of the Cause of Falls in Hospitalizations for Elderly (Aged 65+) Ontarians (FY2006/2007)* |
Abbreviations
- ADL
Activity of daily living
- ALOS
Average length of stay
- CI
Confidence interval
- ED
Emergency department
- FY
Fiscal year
- HR
Hazard ratio
- ICES
Institute of Clinical Evaluative Science
- IRR
Incidence rate ratio
- IU
International units
- LOS
Length of stay
- LTC
Long-term care
- NNP
Number needed to prevent
- OR
Odds ratio
- OT
Occupational therapist
- PT
Physical therapist
- QoL
Quality of life
- OR
Odds ratio
- RCT
Randomized controlled trial
- RR
Relative risk
- UI
Urinary incontinence
References
- 1.Lamb SE, Jorstad-Stein EC, Hauer K, Becker C. Development of a common outcome data set for fall injury prevention trials: the Prevention of Falls Network Europe consensus. J Am Geriatr Soc. 2005;53(9):1618–22. doi: 10.1111/j.1532-5415.2005.53455.x. [DOI] [PubMed] [Google Scholar]
- 2.Close JC, Lord SL, Menz HB, Sherrington C. What is the role of falls? Best Pract Res Clin Rheumatol. 2005;19(6):913–35. doi: 10.1016/j.berh.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 3.Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319(26):1701–7. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]
- 4.O’Loughlin JL, Robitaille Y, Boivin JF, Suissa S. Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am J Epidemiol. 1993;137(3):342–54. doi: 10.1093/oxfordjournals.aje.a116681. [DOI] [PubMed] [Google Scholar]
- 5.Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35 Suppl(2):ii37–ii41. doi: 10.1093/ageing/afl084. [DOI] [PubMed] [Google Scholar]
- 6.Stalenhoef PA, Crebolder H, Knottnerus JA, van der Horst F. Incidence, risk factors and consequences of falls among elderly subjects living in the community. Eur J Public Health. 1997;7(3):328–34. [Google Scholar]
- 7.Yasumura S, Haga H, Niino N. Circumstances of injurious falls leading to medical care among elderly people living in a rural community. Arch Gerontol Geriatr. 1996;23(2):95–109. doi: 10.1016/0167-4943(96)00711-x. [DOI] [PubMed] [Google Scholar]
- 8.Campbell AJ, Spears GF, Borrie MJ. Examination by logistic regression modelling of the variables which increase the relative risk of elderly women falling compared to elderly men. J Clin Epidemiol. 1990;43(12):1415–20. doi: 10.1016/0895-4356(90)90110-b. [DOI] [PubMed] [Google Scholar]
- 9.Bélanger A, Martel L, Malenfant C. Population projections for Canada, provinces, and territories [Internet] [[updated 2005; cited 2008 Aug 1]];Ottawa: Statistics Canada. Available from: www.statcan.ca/english/freepub/91-520-XIE/0010591-520-XIE.pdf .
- 10.O’Loughlin JL, Robitaille Y, Boivin JF, Suissa S. Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am J Epidemiol. 1993;137(3):342–54. doi: 10.1093/oxfordjournals.aje.a116681. [DOI] [PubMed] [Google Scholar]
- 11.O’Loughlin JL, Robitaille Y, Boivin JF, Suissa S. Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am J Epidemiol. 1993;137(3):342–54. doi: 10.1093/oxfordjournals.aje.a116681. [DOI] [PubMed] [Google Scholar]
- 12.Close JC, Lord SL, Menz HB, Sherrington C. What is the role of falls? Best Pract Res Clin Rheumatol. 2005;19(6):913–35. doi: 10.1016/j.berh.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 13.Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. 2006;35 Suppl(2):ii37–ii41. doi: 10.1093/ageing/afl084. Age Ageing. [DOI] [PubMed] [Google Scholar]
- 14.Macpherson AK, Schull M, Cernat G, Redelmeier DA, Laupacis A. Injuries in Ontario. ICES atlas [Internet] [[updated 2005; cited];Toronto: Institute for Clinical Evaluative Sciences. Available from: www.ices.on.ca/webpage.cfm?site_id=1&org_id=31&morg_id=0&gsec_id=0&item_id=3053 .
- 15.Report on seniors’ falls in Canada. [[updated 2005; cited 2008 Nov 1]];Ottawa: Public Health Agency of Canada. Available from: www.phac-aspc.gc.ca/seniors-aines/pubs/seniors_falls/pdf/seniors-falls_e.pdf .
- 16.Close JC, Lord SL, Menz HB, Sherrington C. What is the role of falls? Best Pract Res Clin Rheumatol. 2005;19(6):913–35. doi: 10.1016/j.berh.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 17.Tinetti ME, Williams CS. Falls, injuries due to falls, and the risk of admission to a nursing home. N Engl J Med. 1997;337(18):1279–84. doi: 10.1056/NEJM199710303371806. [DOI] [PubMed] [Google Scholar]
- 18.Gaugler JE, Duval S, Anderson KA, Kane RL. Predicting nursing home admission in the U.S: a meta-analysis. BMC Geriatr. 2007;7(13) doi: 10.1186/1471-2318-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hauer K, Lamb SE, Jorstad EC, Todd C, Becker C. Systematic review of definitions and methods of measuring falls in randomised controlled fall prevention trials. Age Ageing. 2006;35(1):5–10. doi: 10.1093/ageing/afi218. [DOI] [PubMed] [Google Scholar]
- 20.Tinetti ME, Williams CS. Falls, injuries due to falls, and the risk of admission to a nursing home. N Engl J Med. 1997;337(18):1279–84. doi: 10.1056/NEJM199710303371806. [DOI] [PubMed] [Google Scholar]
- 21.Close JC, Lord SL, Menz HB, Sherrington C. What is the role of falls? Best Pract Res Clin Rheumatol. 2005;19(6):913–35. doi: 10.1016/j.berh.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 22.Report on seniors’ falls in Canada. [[updated 2005; cited 2008 Nov 1]];Ottawa: Public Health Agency of Canada. Available from: www.phac-aspc.gc.ca/seniors-aines/pubs/seniors_falls/pdf/seniors-falls_e.pdf .
- 23.Report on seniors’ falls in Canada. [[updated 2005; cited 2008 Nov 1]];Ottawa: Public Health Agency of Canada. Available from: www.phac-aspc.gc.ca/seniors-aines/pubs/seniors_falls/pdf/seniors-falls_e.pdf .
- 24.Close JC, Lord SL, Menz HB, Sherrington C. What is the role of falls? Best Pract Res Clin Rheumatol. 2005;19(6):913–35. doi: 10.1016/j.berh.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 25.O’Loughlin JL, Robitaille Y, Boivin JF, Suissa S. Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am J Epidemiol. 1993;137(3):342–54. doi: 10.1093/oxfordjournals.aje.a116681. [DOI] [PubMed] [Google Scholar]
- 26.Report on seniors’ falls in Canada. [[updated 2005; cited 2008 Nov 1]];Ottawa: Public Health Agency of Canada. Available from: www.phac-aspc.gc.ca/seniors-aines/pubs/seniors_falls/pdf/seniors-falls_e.pdf .
- 27.O’Loughlin JL, Robitaille Y, Boivin JF, Suissa S. Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am J Epidemiol. 1993;137(3):342–54. doi: 10.1093/oxfordjournals.aje.a116681. [DOI] [PubMed] [Google Scholar]
- 28.O’Loughlin JL, Robitaille Y, Boivin JF, Suissa S. Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. 1993;137(3):342–54. doi: 10.1093/oxfordjournals.aje.a116681. Am J Epidemiol. [DOI] [PubMed] [Google Scholar]
- 29.Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35(Suppl 2):ii37–ii41. doi: 10.1093/ageing/afl084. [DOI] [PubMed] [Google Scholar]
- 30.Close JC, Lord SL, Menz HB, Sherrington C. What is the role of falls? Best Pract Res Clin Rheumatol. 2005;19(6):913–35. doi: 10.1016/j.berh.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 31.Report on seniors’ falls in Canada. [[updated 2005; cited 2008 Nov 1]];Ottawa: Public Health Agency of Canada; Available from: www.phac-aspc.gc.ca/seniors-aines/pubs/seniors_falls/pdf/seniors-falls_e.pdf .
- 32.Report on seniors’ falls in Canada. [[updated 2005; cited 2008 Nov 1]];Ottawa: Public Health Agency of Canada. Available from: www.phac-aspc.gc.ca/seniors-aines/pubs/seniors_falls/pdf/seniors-falls_e.pdf .
- 33.Report on seniors’ falls in Canada. [[updated 2005; cited 2008 Nov 1]];Ottawa: Public Health Agency of Canada. Available from: www.phac-aspc.gc.ca/seniors-aines/pubs/seniors_falls/pdf/seniors-falls_e.pdf .
- 34.Report on seniors’ falls in Canada. [[updated 2005; cited 2008 Nov 1]];Ottawa: Public Health Agency of Canada. Available from: www.phac-aspc.gc.ca/seniors-aines/pubs/seniors_falls/pdf/seniors-falls_e.pdf . [Google Scholar]
- 35.O’Loughlin JL, Robitaille Y, Boivin JF, Suissa S. Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am J Epidemiol. 1993;137(3):342–54. doi: 10.1093/oxfordjournals.aje.a116681. [DOI] [PubMed] [Google Scholar]
- 36.Close JC, Lord SL, Menz HB, Sherrington C. What is the role of falls? Best Pract Res Clin Rheumatol. 2005;19(6):913–35. doi: 10.1016/j.berh.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 37.Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35(Suppl 2):ii37–ii41. doi: 10.1093/ageing/afl084. [DOI] [PubMed] [Google Scholar]
- 38.Report on seniors’ falls in Canada. [[updated 2005; cited 2008 Nov 1]];Ottawa: Public Health Agency of Canada. Available from: www.phac-aspc.gc.ca/seniors-aines/pubs/seniors_falls/pdf/seniors-falls_e.pdf .
- 39.Close JC, Lord SL, Menz HB, Sherrington C. What is the role of falls? Best Pract Res Clin Rheumatol. 2005;19(6):913–35. doi: 10.1016/j.berh.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 40.Leipzig RM, Cumming RG, Tinetti ME. Drugs and falls in older people: a systematic review and meta-analysis: II. Cardiac and analgesic drugs. J Am Geriatr Soc. 1999;47(1):40–50. doi: 10.1111/j.1532-5415.1999.tb01899.x. [DOI] [PubMed] [Google Scholar]
- 41.Close JC, Lord SL, Menz HB, Sherrington C. What is the role of falls? Best Pract Res Clin Rheumatol. 2005;19(6):913–35. doi: 10.1016/j.berh.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 42.Tinetti ME, Speechley M. Prevention of falls among the elderly. N Engl J Med. 1989;320(16):1055–9. doi: 10.1056/NEJM198904203201606. [DOI] [PubMed] [Google Scholar]
- 43.Report on seniors’ falls in Canada. [[updated 2005; cited 2008 Nov 1]];Ottawa: Public Health Agency of Canada. Available from: www.phac-aspc.gc.ca/seniors-aines/pubs/seniors_falls/pdf/seniors-falls_e.pdf .
- 44.Gillespie LD, Gillespie WJ, Robertson MC, Lamb SE, Cumming RG, Rowe BH. Interventions for preventing falls in elderly people. Cochrane Database of Systematic Reviews. 2003;(4) doi: 10.1002/14651858.CD000340. Art. No.: CD000340. DOI: 10.1002/14651858.CD000340. [DOI] [PubMed] [Google Scholar]
- 45.Goodman C. Literature searching and evidence interpretation for assessing health care practices. Stockholm, Sweden: The Swedish Council on Technology Assessment in Health Care. 1993 doi: 10.1017/s0266462300008321. [DOI] [PubMed] [Google Scholar]
- 46.Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, et al. Grading quality of evidence and strength of recommendations. BMJ. 2004;328(7454) doi: 10.1136/bmj.328.7454.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Means KM, Rodell DE, O’Sullivan PS. Balance, mobility, and falls among community-dwelling elderly persons: effects of a rehabilitation exercise program. Am J Phys Med Rehabil. 2005;84(4):238–50. doi: 10.1097/01.phm.0000151944.22116.5a. [DOI] [PubMed] [Google Scholar]
- 48.Rubenstein LZ, Josephson KR, Trueblood PR, Loy S, Harker JO, Pietruszka FM, et al. Effects of a group exercise program on strength, mobility, and falls among fall-prone elderly men. J Gerontol A Biol Sci Med Sci. 2000;55(6):M317–M321. doi: 10.1093/gerona/55.6.m317. [DOI] [PubMed] [Google Scholar]
- 49.Means KM, Rodell DE, O’Sullivan PS. Balance, mobility, and falls among community-dwelling elderly persons: effects of a rehabilitation exercise program. Am J Phys Med Rehabil. 2005;84(4):238–50. doi: 10.1097/01.phm.0000151944.22116.5a. [DOI] [PubMed] [Google Scholar]
- 50.Day L, Fildes B, Gordon I, Fitzharris M, Flamer H, Lord S. Randomised factorial trial of falls prevention among older people living in their own homes. BMJ. 2002;325(7356):128–31. doi: 10.1136/bmj.325.7356.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cumming RG, Ivers R, Clemson L, Cullen J, Hayes MF, Tanzer M, et al. Improving vision to prevent falls in frail older people: a randomized trial. J Am Geriatr Soc. 2007;55(2):175–81. doi: 10.1111/j.1532-5415.2007.01046.x. [DOI] [PubMed] [Google Scholar]
- 52.Day L, Fildes B, Gordon I, Fitzharris M, Flamer H, Lord S. Randomised factorial trial of falls prevention among older people living in their own homes. BMJ. 2002;325(7356):128–31. doi: 10.1136/bmj.325.7356.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cumming RG, Ivers R, Clemson L, Cullen J, Hayes MF, Tanzer M, et al. Improving vision to prevent falls in frail older people: a randomized trial. J Am Geriatr Soc. 2007;55(2):175–81. doi: 10.1111/j.1532-5415.2007.01046.x. [DOI] [PubMed] [Google Scholar]
- 54.Foss AJ, Harwood RH, Osborn F, Gregson RM, Zaman A, Masud T. Falls and health status in elderly women following second eye cataract surgery: a randomised controlled trial. Age Ageing. 2006;35(1):66–71. doi: 10.1093/ageing/afj005. [DOI] [PubMed] [Google Scholar]
- 55.Harwood RH, Foss AJ, Osborn F, Gregson RM, Zaman A, Masud T. Falls and health status in elderly women following first eye cataract surgery: a randomised controlled trial. Br J Opthalmol. 2005;89(1):53–9. doi: 10.1136/bjo.2004.049478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Harwood RH, Foss AJ, Osborn F, Gregson RM, Zaman A, Masud T. Falls and health status in elderly women following first eye cataract surgery: a randomised controlled trial. Br J Opthalmol. 2005;89(1):53–9. doi: 10.1136/bjo.2004.049478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Foss AJ, Harwood RH, Osborn F, Gregson RM, Zaman A, Masud T. Falls and health status in elderly women following second eye cataract surgery: a randomised controlled trial. 2006;35(1):66–71. doi: 10.1093/ageing/afj005. Age Ageing. [DOI] [PubMed] [Google Scholar]
- 58.Nikolaus T, Bach M. Preventing falls in community-dwelling frail older people using a home intervention team (HIT): results from the randomized Falls-HIT trial. J Am Geriatr Soc. 2003;51(3):300–5. doi: 10.1046/j.1532-5415.2003.51102.x. [DOI] [PubMed] [Google Scholar]
- 59.Pardessus V, Puisieux F, Di Pompeo C, Gaudefroy C, Thevenon A, Dewailly P. Benefits of home visits for falls and autonomy in the elderly: a randomized trial study. Am J Phys Med Rehabil. 2002;81(4):247–52. doi: 10.1097/00002060-200204000-00002. [DOI] [PubMed] [Google Scholar]
- 60.Day L, Fildes B, Gordon I, Fitzharris M, Flamer H, Lord S. Randomised factorial trial of falls prevention among older people living in their own homes. BMJ. 2002;325(7356):128–31. doi: 10.1136/bmj.325.7356.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Cumming RG, Thomas M, Szonyi G, Salkeld G, O’Neill E, Westbury C, et al. Home visits by an occupational therapist for assessment and modification of environmental hazards: a randomized trial of falls prevention. J Am Geriatr Soc. 1999;47(12):1397–402. doi: 10.1111/j.1532-5415.1999.tb01556.x. [DOI] [PubMed] [Google Scholar]
- 62.Cumming RG, Thomas M, Szonyi G, Salkeld G, O’Neill E, Westbury C, et al. Home visits by an occupational therapist for assessment and modification of environmental hazards: a randomized trial of falls prevention. J Am Geriatr Soc. 1999;47(12):1397–402. doi: 10.1111/j.1532-5415.1999.tb01556.x. [DOI] [PubMed] [Google Scholar]
- 63.Day L, Fildes B, Gordon I, Fitzharris M, Flamer H, Lord S. Randomised factorial trial of falls prevention among older people living in their own homes. BMJ. 2002;325(7356):128–31. doi: 10.1136/bmj.325.7356.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pardessus V, Puisieux F, Di Pompeo C, Gaudefroy C, Thevenon A, Dewailly P. Benefits of home visits for falls and autonomy in the elderly: a randomized trial study. Am J Phys Med Rehabil. 2002;81(4):247–52. doi: 10.1097/00002060-200204000-00002. [DOI] [PubMed] [Google Scholar]
- 65.Cumming RG, Thomas M, Szonyi G, Salkeld G, O’Neill E, Westbury C, et al. Home visits by an occupational therapist for assessment and modification of environmental hazards: a randomized trial of falls prevention. J Am Geriatr Soc. 1999;47(12):1397–402. doi: 10.1111/j.1532-5415.1999.tb01556.x. [DOI] [PubMed] [Google Scholar]
- 66.Day L, Fildes B, Gordon I, Fitzharris M, Flamer H, Lord S. Randomised factorial trial of falls prevention among older people living in their own homes. BMJ. 2002;325(7356):128–31. doi: 10.1136/bmj.325.7356.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Trivedi DP, Doll R, Khaw KT. Effect of four monthly oral vitamin D3 (cholecalciferol) supplementation on fractures and mortality in men and women living in the community: randomised double blind controlled trial. 2003;326(7387):469. doi: 10.1136/bmj.326.7387.469. BMJ. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Reid IR. Therapy of osteoporosis: calcium, vitamin D, and exercise. Am J Med Sci. 1996;312(6):278–86. doi: 10.1097/00000441-199612000-00006. [DOI] [PubMed] [Google Scholar]
- 69.Mowe M, Haug E, Bohmer T. Low serum calcidiol concentration in older adults with reduced muscular function. J Am Geriatr Soc. 1999;47(2):220–6. doi: 10.1111/j.1532-5415.1999.tb04581.x. [DOI] [PubMed] [Google Scholar]
- 70.Bischoff HA, Stahelin HB, Urscheler N, Ehrsam R, Vonthein R, Perrig-Chiello P, et al. Muscle strength in the elderly: its relation to vitamin D metabolites. Arch Phys Med Rehabil. 1999;80(1):54–8. doi: 10.1016/s0003-9993(99)90307-6. [DOI] [PubMed] [Google Scholar]
- 71.Dhesi JK, Jackson SH, Bearne LM, Moniz C, Hurley MV, Swift CG, et al. Vitamin D supplementation improves neuromuscular function in older people who fall. 2004;33(6):589–95. doi: 10.1093/ageing/afh209. Age Ageing. [DOI] [PubMed] [Google Scholar]
- 72.Latham NK, Anderson CS, Lee A, Bennett DA, Moseley A, Cameron ID, et al. A randomized, controlled trial of quadriceps resistance exercise and vitamin D in frail older people: the Frailty Interventions Trial in Elderly Subjects (FITNESS). J Am Geriatr Soc. 2003;51(3):291–9. doi: 10.1046/j.1532-5415.2003.51101.x. [DOI] [PubMed] [Google Scholar]
- 73.Dukas L, Bischoff HA, Lindpaintner LS, Schacht E, Birkner-Binder D, Damm TN, et al. Alfacalcidol reduces the number of fallers in a community-dwelling elderly population with a minimum calcium intake of more than 500 mg daily. J Am Geriatr Soc. 2004;52(2):230–6. doi: 10.1111/j.1532-5415.2004.52060.x. [DOI] [PubMed] [Google Scholar]
- 74.Pfeifer M, Begerow B, Minne HW, Abrams C, Nachtigall D, Hansen C. Effects of a short-term vitamin D and calcium supplementation on body sway and secondary hyperparathyroidism in elderly women. J Bone Miner Res. 2000;15(6):1113–8. doi: 10.1359/jbmr.2000.15.6.1113. [DOI] [PubMed] [Google Scholar]
- 75.Lanham-New SA. Importance of calcium, vitamin D and vitamin K for osteoporosis prevention and treatment. Proc Nutr Soc. 2008;67(2):163–76. doi: 10.1017/S0029665108007003. [DOI] [PubMed] [Google Scholar]
- 76.Bischoff-Ferrari HA, Orav EJ, Dawson-Hughes B. Effect of cholecalciferol plus calcium on falling in ambulatory older men and women: a 3-year randomized controlled trial. Arch Intern Med. 2006;166(4):424–30. doi: 10.1001/archinte.166.4.424. [DOI] [PubMed] [Google Scholar]
- 77.Barr RJ, Stewart A, Torgerson DJ, Seymour DG, Reid DM. Screening elderly women for risk of future fractures--participation rates and impact on incidence of falls and fractures. Calcif Tissue Int. 2005;76(4):243–8. doi: 10.1007/s00223-004-0101-5. [DOI] [PubMed] [Google Scholar]
- 78.Greenspan SL, Resnick NM, Parker RA. The effect of hormone replacement on physical performance in community-dwelling elderly women. Am J Med. 2005;118(11):1232–9. doi: 10.1016/j.amjmed.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 79.Campbell AJ, Robertson MC, Gardner MM, Norton RN, Buchner DM. Psychotropic medication withdrawal and a home-based exercise program to prevent falls: a randomized, controlled trial. J Am Geriatr Soc. 1999;47(7):850–3. doi: 10.1111/j.1532-5415.1999.tb03843.x. [DOI] [PubMed] [Google Scholar]
- 80.McKiernan FE. A simple gait-stabilizing device reduces outdoor falls and nonserious injurious falls in fall-prone older people during the winter. J Am Geriatr Soc. 2005;53(6):943–7. doi: 10.1111/j.1532-5415.2005.53302.x. [DOI] [PubMed] [Google Scholar]
- 81.Yaktrax [Internet] [[cited 2008 May 12]];2006 Available from: www.yaktrax.com .
- 82.Birks YF, Hildreth R, Campbell P, Sharpe C, Torgerson DJ, Watt I. Randomised controlled trial of hip protectors for the prevention of second hip fractures. Age Ageing. 2003;32(4):442–4. doi: 10.1093/ageing/32.4.442. [DOI] [PubMed] [Google Scholar]
- 83.Lord SR, Tiedemann A, Chapman K, Munro B, Murray SM, Gerontology M, et al. The effect of an individualized fall prevention program on fall risk and falls in older people: a randomized, controlled trial. J Am Geriatr Soc. 2005;53(8):1296–304. doi: 10.1111/j.1532-5415.2005.53425.x. [DOI] [PubMed] [Google Scholar]
- 84.Davison J, Bond J, Dawson P, Steen IN, Kenny RA. Patients with recurrent falls attending Accident & Emergency benefit from multifactorial intervention--a randomised controlled trial. Age Ageing. 2005;34(2):162–8. doi: 10.1093/ageing/afi053. [DOI] [PubMed] [Google Scholar]
- 85.Fabacher D, Josephson K, Pietruszka F, Linderborn K, Morley JE, Rubenstein LZ. An in-home preventive assessment program for independent older adults: a randomized controlled trial. 1994;(6):630–8. doi: 10.1111/j.1532-5415.1994.tb06862.x. J Am Geriatr Soc. 42. [DOI] [PubMed] [Google Scholar]
- 86.Newbury J, Marley J. Preventive home visits to elderly people in the community. BMJ. 2000;321(7259):512. Visits are most useful for people aged >/= 75. [PMC free article] [PubMed] [Google Scholar]
- 87.Close J, Ellis M, Hooper R, Glucksman E, Jackson S, Swift C. Prevention of falls in the elderly trial (PROFET): a randomised controlled trial. Lancet. 1999;353(9147):93–7. doi: 10.1016/S0140-6736(98)06119-4. [DOI] [PubMed] [Google Scholar]
- 88.Hogan DB, MacDonald FA, Betts J, Bricker S, Ebly EM, Delarue B, et al. A randomized controlled trial of a community-based consultation service to prevent falls. CMAJ. 2001;165(5):537–43. [PMC free article] [PubMed] [Google Scholar]
- 89.Huang T, Liang S. A randomized clinical trial of the effectiveness of a discharge planning intervention in hospitalized elders with hip fracture due to falling. J Clin Nurs. 2005;14(10):1193–201. doi: 10.1111/j.1365-2702.2005.01260.x. [DOI] [PubMed] [Google Scholar]
- 90.Kingston P, Jones M, Lally F, Crome P. Older people and falls: a randomized controlled trial of a health visitor (HV) intervention. Rev Clin Gerontol. 2001;11(3):209–14. [Google Scholar]
- 91.Jitapunkul S. A randomised controlled trial of regular surveillance in Thai elderly using a simple questionnaire administered by non-professional personnel. J Med Assoc Thai. 1998;81(5):352–6. [PubMed] [Google Scholar]
- 92.Rubenstein LZ, Alessi CA, Josephson KR, Trinidad HM, Harker JO, Pietruszka FM. A randomized trial of a screening, case finding, and referral system for older veterans in primary care. J Am Geriatr Soc. 2007;55(2):166–74. doi: 10.1111/j.1532-5415.2007.01044.x. [DOI] [PubMed] [Google Scholar]
- 93.Whitehead C, Wundke R, Crotty M, Finucane P. Evidence-based clinical practice in falls prevention: a randomised controlled trial of a falls prevention service. Aust Health Rev. 2003;26(3):88–97. doi: 10.1071/ah030088. [DOI] [PubMed] [Google Scholar]
- 94.Mahoney JE, Shea TA, Przybelski R, Jaros L, Gangnon R, Cech S, et al. Kenosha County falls prevention study: a randomized, controlled trial of an intermediate-intensity, community-based multifactorial falls intervention. J Am Geriatr Soc. 2007;55(4):489–98. doi: 10.1111/j.1532-5415.2007.01144.x. [DOI] [PubMed] [Google Scholar]
- 95.Mahoney JE, Shea TA, Przybelski R, Jaros L, Gangnon R, Cech S, et al. Kenosha County falls prevention study: a randomized, controlled trial of an intermediate-intensity, community-based multifactorial falls intervention. J Am Geriatr Soc. 2007;55(4):489–98. doi: 10.1111/j.1532-5415.2007.01144.x. [DOI] [PubMed] [Google Scholar]
- 96.Peeters GM, de Vries OJ, Elders PJ, Pluijm SM, Bouter LM, Lips P. Prevention of fall incidents in patients with a high risk of falling: design of a randomised controlled trial with an economic evaluation of the effect of multidisciplinary transmural care. BMC Geriatr. 2007;7 doi: 10.1186/1471-2318-7-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Sjosten NM, Salonoja M, Piirtola M, Vahlberg T, Isoaho R, Hyttinen H, et al. A multifactorial fall prevention programme in home-dwelling elderly people: a randomized-controlled trial. Public Health. 2007;121(4):308–18. doi: 10.1016/j.puhe.2006.09.018. [DOI] [PubMed] [Google Scholar]
- 98.Hendriks MR, van Haastregt JC, Diederiks JP, Evers SM, Crebolder HF, van Eijk JT. Effectiveness and cost-effectiveness of a multidisciplinary intervention programme to prevent new falls and functional decline among elderly persons at risk: design of a replicated randomised controlled trial [ISRCTN64716113] BMC Public Health. 2005;5 doi: 10.1186/1471-2458-5-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Elley CR, Robertson MC, Kerse NM, Garrett S, McKinlay E, Lawton B, et al. Falls Assessment Clinical Trial (FACT): design, interventions, recruitment strategies and participant characteristics. 2007;7(147) doi: 10.1186/1471-2458-7-185. BMC Public Health. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Suzuki T, Kim H, Yoshida H, Ishizaki T. Randomized controlled trial of exercise intervention for the prevention of falls in community-dwelling elderly Japanese women. J Bone Miner Metab. 2004;22(6):602–11. doi: 10.1007/s00774-004-0530-2. [DOI] [PubMed] [Google Scholar]
- 101.Buchner DM, Cress ME, de Lateur BJ, Esselman PC, Margherita AJ, Price R, et al. The effect of strength and endurance training on gait, balance, fall risk, and health services use in community-living older adults. J Gerontol A Biol Sci Med Sci. 1997;52(4):M218–M224. doi: 10.1093/gerona/52a.4.m218. [DOI] [PubMed] [Google Scholar]
- 102.Cerny K, Blanks R, Mohamed O, Schwab D, Robinson B, Russo A, et al. The effect of a multidimensional exercise program on strength, range of motion, balance and gait in the well elderly. Gait Posture. 1998;7(2):185–6. [Google Scholar]
- 103.McMurdo ME, Mole PA, Paterson CR. Controlled trial of weight bearing exercise in older women in relation to bone density and falls. 1997;314(7080):569. doi: 10.1136/bmj.314.7080.569. BMJ. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Luukinen H, Lehtola S, Jokelainen J, Vaananen-Sainio R, Lotvonen S, Koistinen P. Pragmatic exercise-oriented prevention of falls among the elderly: a population-based, randomized, controlled trial. Prev Med. 2007;44(3):265–71. doi: 10.1016/j.ypmed.2006.09.011. [DOI] [PubMed] [Google Scholar]
- 105.Campbell AJ, Robertson MC, Gardner MM, Norton RN, Tilyard MW, Buchner DM. Randomised controlled trial of a general practice programme of home based exercise to prevent falls in elderly women. BMJ. 1997;315(7115):1065–9. doi: 10.1136/bmj.315.7115.1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Campbell AJ, Robertson MC, Gardner MM, Norton RN, Tilyard MW, Buchner DM. Randomised controlled trial of a general practice programme of home based exercise to prevent falls in elderly women. BMJ. 1997;315(7115):1065–9. doi: 10.1136/bmj.315.7115.1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Cornillon E, Blanchon MA, Ramboatsisetraina P, Braize C, Beauchet O, Dubost V, et al. Ann Readapt Med Phys. 2002;45(9):493–504. doi: 10.1016/s0168-6054(02)00302-1. [Effectiveness of falls prevention strategies for elderly subjects who live in the community with performance assessment of physical activities (before-after)] [DOI] [PubMed] [Google Scholar]
- 108.Day L, Fildes B, Gordon I, Fitzharris M, Flamer H, Lord S. Randomised factorial trial of falls prevention among older people living in their own homes. BMJ. 2002;325(7356):128–31. doi: 10.1136/bmj.325.7356.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Ebrahim S, Thompson PW, Baskaran V, Evans K. Randomized placebo-controlled trial of brisk walking in the prevention of postmenopausal osteoporosis. Age Ageing. 1997;26(4):253–60. doi: 10.1093/ageing/26.4.253. [DOI] [PubMed] [Google Scholar]
- 110.Rubenstein LZ, Josephson KR, Trueblood PR, Loy S, Harker JO, Pietruszka FM, et al. Effects of a group exercise program on strength, mobility, and falls among fall-prone elderly men. J Gerontol A Biol Sci Med Sci. 2000;55(6):M317–M321. doi: 10.1093/gerona/55.6.m317. [DOI] [PubMed] [Google Scholar]
- 111.Weerdesteyn V, Rijken H, Geurts AC, Smits-Engelsman BC, Mulder T, Duysens J. A five-week exercise program can reduce falls and improve obstacle avoidance in the elderly. Gerontology. 2006;52(3):131–41. doi: 10.1159/000091822. [DOI] [PubMed] [Google Scholar]
- 112.Means KM, Rodell DE, O’Sullivan PS. Balance, mobility, and falls among community-dwelling elderly persons: effects of a rehabilitation exercise program. 2005;84(4):238–50. doi: 10.1097/01.phm.0000151944.22116.5a. Am J Phys Med Rehabil. [DOI] [PubMed] [Google Scholar]
- 113.Cornillon E, Blanchon MA, Ramboatsisetraina P, Braize C, Beauchet O, Dubost V, et al. Ann Readapt Med Phys. 2002;45(9):493–504. doi: 10.1016/s0168-6054(02)00302-1. [Effectiveness of falls prevention strategies for elderly subjects who live in the community with performance assessment of physical activities (before-after)] [DOI] [PubMed] [Google Scholar]
- 114.Campbell AJ, Robertson MC, Gardner MM, Norton RN, Buchner DM. Psychotropic medication withdrawal and a home-based exercise program to prevent falls: a randomized, controlled trial. J Am Geriatr Soc. 1999;47(7):850–3. doi: 10.1111/j.1532-5415.1999.tb03843.x. [DOI] [PubMed] [Google Scholar]
- 115.Campbell AJ, Robertson MC, Gardner MM, Norton RN, Tilyard MW, Buchner DM. Randomised controlled trial of a general practice programme of home based exercise to prevent falls in elderly women. BMJ. 1997;315(7115):1065–9. doi: 10.1136/bmj.315.7115.1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Buchner DM, Cress ME, de Lateur BJ, Esselman PC, Margherita AJ, Price R, et al. The effect of strength and endurance training on gait, balance, fall risk, and health services use in community-living older adults. J Gerontol A Biol Sci Med Sci. 1997;52(4):M218–M224. doi: 10.1093/gerona/52a.4.m218. [DOI] [PubMed] [Google Scholar]
- 117.Ebrahim S, Thompson PW, Baskaran V, Evans K. Randomized placebo-controlled trial of brisk walking in the prevention of postmenopausal osteoporosis. Age Ageing. 1997;26(4):253–60. doi: 10.1093/ageing/26.4.253. [DOI] [PubMed] [Google Scholar]
- 118.Rubenstein LZ, Josephson KR, Trueblood PR, Loy S, Harker JO, Pietruszka FM, et al. Effects of a group exercise program on strength, mobility, and falls among fall-prone elderly men. J Gerontol A Biol Sci Med Sci. 2000;55(6):MS317–M321. doi: 10.1093/gerona/55.6.m317. [DOI] [PubMed] [Google Scholar]
- 119.Hauer K, Rost B, Rutschle K, Opitz H, Specht N, Bartsch P, et al. Exercise training for rehabilitation and secondary prevention of falls in geriatric patients with a history of injurious falls. J Am Geriatr Soc. 2001;49(1):10–20. doi: 10.1046/j.1532-5415.2001.49004.x. [DOI] [PubMed] [Google Scholar]
- 120.Rubenstein LZ, Josephson KR, Trueblood PR, Loy S, Harker JO, Pietruszka FM, et al. Effects of a group exercise program on strength, mobility, and falls among fall-prone elderly men. J Gerontol A Biol Sci Med Sci. 2000;55(6):M317–M321. doi: 10.1093/gerona/55.6.m317. [DOI] [PubMed] [Google Scholar]
- 121.Barr RJ, Stewart A, Torgerson DJ, Seymour DG, Reid DM. Screening elderly women for risk of future fractures--participation rates and impact on incidence of falls and fractures. Calcif Tissue Int. 2005;76(4):243–8. doi: 10.1007/s00223-004-0101-5. [DOI] [PubMed] [Google Scholar]
- 122.Greenspan SL, Resnick NM, Parker RA. The effect of hormone replacement on physical performance in community-dwelling elderly women. Am J Med. 2005;118(11):1232–9. doi: 10.1016/j.amjmed.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 123.Campbell AJ, Robertson MC, Gardner MM, Norton RN, Buchner DM. Psychotropic medication withdrawal and a home-based exercise program to prevent falls: a randomized, controlled trial. J Am Geriatr Soc. 1999;47(7):850–3. doi: 10.1111/j.1532-5415.1999.tb03843.x. [DOI] [PubMed] [Google Scholar]
- 124.Campbell AJ, Robertson MC, Gardner MM, Norton RN, Buchner DM. Psychotropic medication withdrawal and a home-based exercise program to prevent falls: a randomized, controlled trial. J Am Geriatr Soc. 1999;47(7):850–3. doi: 10.1111/j.1532-5415.1999.tb03843.x. [DOI] [PubMed] [Google Scholar]
- 125.Campbell AJ, Robertson MC, Gardner MM, Norton RN, Buchner DM. Psychotropic medication withdrawal and a home-based exercise program to prevent falls: a randomized, controlled trial. 1999;47(7):850–3. doi: 10.1111/j.1532-5415.1999.tb03843.x. J Am Geriatr Soc. [DOI] [PubMed] [Google Scholar]
- 126.Day L, Fildes B, Gordon I, Fitzharris M, Flamer H, Lord S. Randomised factorial trial of falls prevention among older people living in their own homes. BMJ. 2002;325(7356):128–31. doi: 10.1136/bmj.325.7356.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Cumming RG, Ivers R, Clemson L, Cullen J, Hayes MF, Tanzer M, et al. Improving vision to prevent falls in frail older people: a randomized trial. J Am Geriatr Soc. 2007;55(2):175–81. doi: 10.1111/j.1532-5415.2007.01046.x. [DOI] [PubMed] [Google Scholar]
- 128.Harwood RH, Foss AJ, Osborn F, Gregson RM, Zaman A, Masud T. Falls and health status in elderly women following first eye cataract surgery: a randomised controlled trial. Br J Opthalmol. 2005;89(1):53–9. doi: 10.1136/bjo.2004.049478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Foss AJ, Harwood RH, Osborn F, Gregson RM, Zaman A, Masud T. Falls and health status in elderly women following second eye cataract surgery: a randomised controlled trial. Age Ageing. 2006;35(1):66–71. doi: 10.1093/ageing/afj005. [DOI] [PubMed] [Google Scholar]
- 130.Fabacher D, Josephson K, Pietruszka F, Linderborn K, Morley JE, Rubenstein LZ. An in-home preventive assessment program for independent older adults: a randomized controlled trial. J Am Geriatr Soc. 1994;42(6):630–8. doi: 10.1111/j.1532-5415.1994.tb06862.x. [DOI] [PubMed] [Google Scholar]
- 131.Newbury J, Marley J. Preventive home visits to elderly people in the community. BMJ. 2000;321(7259):512. Visits are most useful for people aged >/= 75. [PMC free article] [PubMed] [Google Scholar]
- 132.Rubenstein LZ, Alessi CA, Josephson KR, Trinidad HM, Harker JO, Pietruszka FM. A randomized trial of a screening, case finding, and referral system for older veterans in primary care. J Am Geriatr Soc. 2007;55(2):166–74. doi: 10.1111/j.1532-5415.2007.01044.x. [DOI] [PubMed] [Google Scholar]
- 133.Wagner EH, LaCroix AZ, Grothaus L, Leveille SG, Hecht JA, Artz K, et al. Preventing disability and falls in older adults: a population-based randomized trial. Am J Public Health. 1994;84(11):1800–6. doi: 10.2105/ajph.84.11.1800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Fabacher D, Josephson K, Pietruszka F, Linderborn K, Morley JE, Rubenstein LZ. An in-home preventive assessment program for independent older adults: a randomized controlled trial. J Am Geriatr Soc. 1994;42(6):630–8. doi: 10.1111/j.1532-5415.1994.tb06862.x. [DOI] [PubMed] [Google Scholar]
- 135.Jitapunkul S. A randomised controlled trial of regular surveillance in Thai elderly using a simple questionnaire administered by non-professional personnel. J Med Assoc Thai. 1998;81(5):352–6. [PubMed] [Google Scholar]
- 136.Fabacher D, Josephson K, Pietruszka F, Linderborn K, Morley JE, Rubenstein LZ. An in-home preventive assessment program for independent older adults: a randomized controlled trial. J Am Geriatr Soc. 1994;42(6):630–8. doi: 10.1111/j.1532-5415.1994.tb06862.x. [DOI] [PubMed] [Google Scholar]
- 137.Newbury J, Marley J. Preventive home visits to elderly people in the community. BMJ. 2000;321(7259):512. Visits are most useful for people aged >/= 75. [PMC free article] [PubMed] [Google Scholar]
- 138.Rubenstein LZ, Alessi CA, Josephson KR, Trinidad HM, Harker JO, Pietruszka FM. A randomized trial of a screening, case finding, and referral system for older veterans in primary care. 2007;55(2):166–74. doi: 10.1111/j.1532-5415.2007.01044.x. J Am Geriatr Soc. [DOI] [PubMed] [Google Scholar]
- 139.Jitapunkul S. A randomised controlled trial of regular surveillance in Thai elderly using a simple questionnaire administered by non-professional personnel. J Med Assoc Thai. 1998;81(5):352–6. [PubMed] [Google Scholar]
- 140.Close J, Ellis M, Hooper R, Glucksman E, Jackson S, Swift C. Prevention of falls in the elderly trial (PROFET): a randomised controlled trial. Lancet. 1999;353(9147):93–7. doi: 10.1016/S0140-6736(98)06119-4. [DOI] [PubMed] [Google Scholar]
- 141.Huang T, Liang S. A randomized clinical trial of the effectiveness of a discharge planning intervention in hospitalized elders with hip fracture due to falling. J Clin Nurs. 2005;14(10):1193–201. doi: 10.1111/j.1365-2702.2005.01260.x. [DOI] [PubMed] [Google Scholar]
- 142.Kingston P, Jones M, Lally F, Crome P. Older people and falls: a randomized controlled trial of a health visitor (HV) intervention. Rev Clin Gerontol. 2001;11(3):209–14. [Google Scholar]
- 143.Lightbody E, Watkins C, Leathley M, Sharma A, Lye M. Evaluation of a nurse-led falls prevention programme versus usual care: a randomized controlled trial. Age Ageing. 2002;31(3):203–10. doi: 10.1093/ageing/31.3.203. [DOI] [PubMed] [Google Scholar]
- 144.van Haastregt JC, Diederiks JP, van RE, de Witte LP, Voorhoeve PM, Crebolder HF. Effects of a programme of multifactorial home visits on falls and mobility impairments in elderly people at risk: randomised controlled trial. BMJ. 2000;321(7267):994–8. doi: 10.1136/bmj.321.7267.994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Close J, Ellis M, Hooper R, Glucksman E, Jackson S, Swift C. Prevention of falls in the elderly trial (PROFET): a randomised controlled trial. Lancet. 1999;353(9147):93–7. doi: 10.1016/S0140-6736(98)06119-4. [DOI] [PubMed] [Google Scholar]
- 146.van Haastregt JC, Diederiks JP, van RE, de Witte LP, Voorhoeve PM, Crebolder HF. Effects of a programme of multifactorial home visits on falls and mobility impairments in elderly people at risk: randomised controlled trial. BMJ. 2000;321(7267):994–8. doi: 10.1136/bmj.321.7267.994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Close J, Ellis M, Hooper R, Glucksman E, Jackson S, Swift C. Prevention of falls in the elderly trial (PROFET): a randomised controlled trial. Lancet. 1999;353(9147):93–7. doi: 10.1016/S0140-6736(98)06119-4. [DOI] [PubMed] [Google Scholar]
- 148.van Haastregt JC, Diederiks JP, van RE, de Witte LP, Voorhoeve PM, Crebolder HF. Effects of a programme of multifactorial home visits on falls and mobility impairments in elderly people at risk: randomised controlled trial. BMJ. 2000;321(7267):994–8. doi: 10.1136/bmj.321.7267.994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Close J, Ellis M, Hooper R, Glucksman E, Jackson S, Swift C. Prevention of falls in the elderly trial (PROFET): a randomised controlled trial. Lancet. 1999;353(9147):93–7. doi: 10.1016/S0140-6736(98)06119-4. [DOI] [PubMed] [Google Scholar]
- 150.van Haastregt JC, Diederiks JP, van RE, de Witte LP, Voorhoeve PM, Crebolder HF. Effects of a programme of multifactorial home visits on falls and mobility impairments in elderly people at risk: randomised controlled trial. BMJ. 2000;321(7267):994–8. doi: 10.1136/bmj.321.7267.994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Maki BE, Cheng KC, Mansfield A, Scovil CY, Perry SD, Peters AL, et al. Preventing falls in older adults: new interventions to promote more effective change-in-support balance reactions. J Electromyogr Kinesiol. 2008;18(2):243–54. doi: 10.1016/j.jelekin.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 152.Barnett A, Smith B, Lord SR, Williams M, Baumand A. Community-based group exercise improves balance and reduces falls in at-risk older people: a randomised controlled trial. Age Ageing. 2003;32(4):407–14. doi: 10.1093/ageing/32.4.407. [DOI] [PubMed] [Google Scholar]
- 153.Day L, Fildes B, Gordon I, Fitzharris M, Flamer H, Lord S. Randomised factorial trial of falls prevention among older people living in their own homes. 2002;325(7356):128–31. doi: 10.1136/bmj.325.7356.128. BMJ. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Freiberger E, Menz HB, Abu-Omar K, Rutten A. Preventing falls in physically active community-dwelling older people: A comparison of two intervention techniques. Gerontology. 2007;53(5):298–305. doi: 10.1159/000103256. [DOI] [PubMed] [Google Scholar]
- 155.Hauer K, Rost B, Rutschle K, Opitz H, Specht N, Bartsch P, et al. Exercise training for rehabilitation and secondary prevention of falls in geriatric patients with a history of injurious falls. J Am Geriatr Soc. 2001;49(1):10–20. doi: 10.1046/j.1532-5415.2001.49004.x. [DOI] [PubMed] [Google Scholar]
- 156.Helbostad JL, Sletvold O, Moe-Nilssen R. Effects of home exercises and group training on functional abilities in home-dwelling older persons with mobility and balance problems. Aging Clin Exp Res. 2004;16(2):113–21. doi: 10.1007/BF03324539. A randomized study. [DOI] [PubMed] [Google Scholar]
- 157.Latham NK, Anderson CS, Lee A, Bennett DA, Moseley A, Cameron ID, et al. A randomized, controlled trial of quadriceps resistance exercise and vitamin D in frail older people: the Frailty Interventions Trial in Elderly Subjects (FITNESS) J Am Geriatr Soc. 2003;51(3):291–9. doi: 10.1046/j.1532-5415.2003.51101.x. [DOI] [PubMed] [Google Scholar]
- 158.Li F, Harmer P, Fisher KJ, McAuley E, Chaumeton N, Eckstrom E, et al. Tai Chi and fall reductions in older adults: a randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2005;60(2):187–94. doi: 10.1093/gerona/60.2.187. [DOI] [PubMed] [Google Scholar]
- 159.Luukinen H, Lehtola S, Jokelainen J, Vaananen-Sainio R, Lotvonen S, Koistinen P. Prevention of disability by exercise among the elderly: A population-based, randomized, controlled trial. Scand J Prim Health Care. 2006;24(4):199–205. doi: 10.1080/02813430600958476. [DOI] [PubMed] [Google Scholar]
- 160.Means KM, Rodell DE, O’Sullivan PS. Balance, mobility, and falls among community-dwelling elderly persons: effects of a rehabilitation exercise program. Am J Phys Med Rehabil. 2005;84(4):238–50. doi: 10.1097/01.phm.0000151944.22116.5a. [DOI] [PubMed] [Google Scholar]
- 161.Robertson MC, Devlin N, Gardner MM, Campbell AJ. Effectiveness and economic evaluation of a nurse delivered home exercise programme to prevent falls. 1: Randomised controlled trial. BMJ. 2001;322(7288):697–701. doi: 10.1136/bmj.322.7288.697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Rubenstein LZ, Josephson KR, Trueblood PR, Loy S, Harker JO, Pietruszka FM, et al. Effects of a group exercise program on strength, mobility, and falls among fall-prone elderly men. J Gerontol A Biol Sci Med Sci. 2000;55(6):M317–M321. doi: 10.1093/gerona/55.6.m317. [DOI] [PubMed] [Google Scholar]
- 163.Skelton D, Dinan S, Campbell M, Rutherford O. Tailored group exercise (Falls Management Exercise--FaME) reduces falls in community-dwelling older frequent fallers (an RCT) Age Ageing. 2005;34(6):636–9. doi: 10.1093/ageing/afi174. [DOI] [PubMed] [Google Scholar]
- 164.Voukelatos A, Cumming RG, Lord SR, Rissel C. A randomized, controlled trial of tai chi for the prevention of falls: the Central Sydney tai chi trial. J Am Geriatr Soc. 2007;55(8):1185–91. doi: 10.1111/j.1532-5415.2007.01244.x. [DOI] [PubMed] [Google Scholar]
- 165.Woo J, Hong A, Lau E, Lynn H. A randomised controlled trial of Tai Chi and resistance exercise on bone health, muscle strength and balance in community-living elderly people. Age Ageing. 2007;36(3):262–8. doi: 10.1093/ageing/afm005. [DOI] [PubMed] [Google Scholar]
- 166.Cumming RG, Ivers R, Clemson L, Cullen J, Hayes MF, Tanzer M, et al. Improving vision to prevent falls in frail older people: a randomized trial. 2007;55(2):175–81. doi: 10.1111/j.1532-5415.2007.01046.x. J Am Geriatr Soc. [DOI] [PubMed] [Google Scholar]
- 167.Day L, Fildes B, Gordon I, Fitzharris M, Flamer H, Lord S. Randomised factorial trial of falls prevention among older people living in their own homes. BMJ. 2002;325(7356):128–31. doi: 10.1136/bmj.325.7356.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Foss AJ, Harwood RH, Osborn F, Gregson RM, Zaman A, Masud T. Falls and health status in elderly women following second eye cataract surgery: a randomised controlled trial. Age Ageing. 2006;35(1):66–71. doi: 10.1093/ageing/afj005. [DOI] [PubMed] [Google Scholar]
- 169.Harwood RH, Foss AJ, Osborn F, Gregson RM, Zaman A, Masud T. Falls and health status in elderly women following first eye cataract surgery: a randomised controlled trial. Br J Opthalmol. 2005;89(1):53–9. doi: 10.1136/bjo.2004.049478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Day L, Fildes B, Gordon I, Fitzharris M, Flamer H, Lord S. Randomised factorial trial of falls prevention among older people living in their own homes. BMJ. 2002;325(7356):128–31. doi: 10.1136/bmj.325.7356.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Pardessus V, Puisieux F, Di Pompeo C, Gaudefroy C, Thevenon A, Dewailly P. Benefits of home visits for falls and autonomy in the elderly: a randomized trial study. Am J Phys Med Rehabil. 2002;81(4):247–52. doi: 10.1097/00002060-200204000-00002. [DOI] [PubMed] [Google Scholar]
- 172.Barr RJ, Stewart A, Torgerson DJ, Seymour DG, Reid DM. Screening elderly women for risk of future fractures--participation rates and impact on incidence of falls and fractures. Calcif Tissue Int. 2005;76(4):243–8. doi: 10.1007/s00223-004-0101-5. [DOI] [PubMed] [Google Scholar]
- 173.Dhesi JK, Jackson SH, Bearne LM, Moniz C, Hurley MV, Swift CG, et al. Vitamin D supplementation improves neuromuscular function in older people who fall. Age Ageing. 2004;33(6):589–95. doi: 10.1093/ageing/afh209. [DOI] [PubMed] [Google Scholar]
- 174.Dukas L, Bischoff HA, Lindpaintner LS, Schacht E, Birkner-Binder D, Damm TN, et al. Alfacalcidol reduces the number of fallers in a community-dwelling elderly population with a minimum calcium intake of more than 500 mg daily. J Am Geriatr Soc. 2004;52(2):230–6. doi: 10.1111/j.1532-5415.2004.52060.x. [DOI] [PubMed] [Google Scholar]
- 175.Greenspan SL, Resnick NM, Parker RA. The effect of hormone replacement on physical performance in community-dwelling elderly women. Am J Med. 2005;118(11):1232–9. doi: 10.1016/j.amjmed.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 176.Latham NK, Anderson CS, Lee A, Bennett DA, Moseley A, Cameron ID, et al. A randomized, controlled trial of quadriceps resistance exercise and vitamin D in frail older people: the Frailty Interventions Trial in Elderly Subjects (FITNESS) J Am Geriatr Soc. 2003;51(3):291–9. doi: 10.1046/j.1532-5415.2003.51101.x. [DOI] [PubMed] [Google Scholar]
- 177.Porthouse J, Cockayne S, King C, Saxon L, Steele E, Aspray T, et al. Randomised controlled trial of calcium and supplementation with cholecalciferol (vitamin D3) for prevention of fractures in primary care. BMJ. 2005;330(7498):1003–6. doi: 10.1136/bmj.330.7498.1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Clemson L, Cumming RG, Kendig H, Swann M, Heard R, Taylor K. The effectiveness of a community-based program for reducing the incidence of falls in the elderly: a randomized trial. J Am Geriatr Soc. 2004;52(9):1487–94. doi: 10.1111/j.1532-5415.2004.52411.x. [DOI] [PubMed] [Google Scholar]
- 179.Davison J, Bond J, Dawson P, Steen IN, Kenny RA. Patients with recurrent falls attending Accident & Emergency benefit from multifactorial intervention--a randomised controlled trial. Age Ageing. 2005;34(2):162–8. doi: 10.1093/ageing/afi053. [DOI] [PubMed] [Google Scholar]
- 180.Huang T, Liang S. A randomized clinical trial of the effectiveness of a discharge planning intervention in hospitalized elders with hip fracture due to falling. 2005;14(10):1193–201. doi: 10.1111/j.1365-2702.2005.01260.x. J Clin Nurs. [DOI] [PubMed] [Google Scholar]
- 181.Mahoney JE, Shea TA, Przybelski R, Jaros L, Gangnon R, Cech S, et al. Kenosha County falls prevention study: a randomized, controlled trial of an intermediate-intensity, community-based multifactorial falls intervention. J Am Geriatr Soc. 2007;55(4):489–98. doi: 10.1111/j.1532-5415.2007.01144.x. [DOI] [PubMed] [Google Scholar]
- 182.Rubenstein LZ, Alessi CA, Josephson KR, Trinidad HM, Harker JO, Pietruszka FM. A randomized trial of a screening, case finding, and referral system for older veterans in primary care. J Am Geriatr Soc. 2007;55(2):166–74. doi: 10.1111/j.1532-5415.2007.01044.x. [DOI] [PubMed] [Google Scholar]
- 183.Tinetti ME, Baker DI, McAvay G, Claus EB, Garrett P, Gottschalk M, et al. A multifactorial intervention to reduce the risk of falling among elderly people living in the community. N Engl J Med. 1994;331(13):821–7. doi: 10.1056/NEJM199409293311301. [DOI] [PubMed] [Google Scholar]
- 184.Sjosten NM, Salonoja M, Piirtola M, Vahlberg T, Isoaho R, Hyttinen H, et al. A multifactorial fall prevention programme in home-dwelling elderly people: a randomized-controlled trial. Public Health. 2007;121(4):308–18. doi: 10.1016/j.puhe.2006.09.018. [DOI] [PubMed] [Google Scholar]
- 185.Hendriks MR, van Haastregt JC, Diederiks JP, Evers SM, Crebolder HF, van Eijk JT. Effectiveness and cost-effectiveness of a multidisciplinary intervention programme to prevent new falls and functional decline among elderly persons at risk: design of a replicated randomised controlled trial [ISRCTN64716113] BMC Public Health. 2005;5(6) doi: 10.1186/1471-2458-5-6. [DOI] [PMC free article] [PubMed] [Google Scholar]


