Abstract
OBJECTIVE
To determine whether exercise-induced reductions in fall risk are maintained in older women one year following the cessation of three types of interventions – resistance training, agility training, and general stretching.
DESIGN
One-year observational study.
PARTICIPANTS
98 women aged 75–85 years with low bone mass.
MEASUREMENTS
Primary outcome measure was fall risk as measured by the Physiological Profile Assessment tool. Secondary outcome measures were current physical activity level as assessed by the Physical Activity Scale for the Elderly and formal exercise participation as assessed by interview.
RESULTS
At the end of the follow-up, the fall risk among former participants of all three exercise programs was maintained (i.e., still reduced) from trial completion. Mean fall risk value at the end of follow-up was 43.3% reduced compared with the mean baseline value among former participants of the Resistance Training group, 40.1% reduced in the Agility Training group, and 37.4% reduced in the general Stretching group. Physical activity levels were also maintained from trial completion. Specifically, there was a 3.8% increase in physical activity from baseline for the Resistance Training group, a 29.2% increase for the Agility Training group, and 37.7% increase for the general Stretching group.
CONCLUSION
After three types of group-based exercise programs, benefits are sustained for at least 12 months without further formal exercise intervention. Thus, these six-month exercise interventions appeared to act as a catalyst for increasing physical activity with resultant reductions in fall risk profile that were maintained for at least 18 months among older women with low bone mass.
Keywords: Fall Risk, Physical Activity, Detraining, Aged, Low Bone Mass
Falls in older people is a major health care problem 1 and falls prevention is a major health care priority. Falls occur, at least in part, due to physiological impairments of balance, muscle weakness, and reaction time 2,3. Although several randomized controlled trials demonstrated that exercise reduced both fall risk factors and falls in older people by ameliorating physiological impairments, very few have examined whether such benefits persist after formal cessation of the trials 4,5, and none has done so in those at high risk of sustaining fall-related fractures, such as older adults with low bone mass.
Exercise comes in various types including resistance, agility, and stretching training. Whether or not exercise benefits persist or are lost with ‘detraining’ after each of these types of exercise interventions has not been compared within one study. If one type of exercise were to provide more persisting benefits than another it would have implications for exercise prescription to prevent falls.
Although physical activity reduces the risk of falls in those with physiological risk factors 6, physical activity declines progressively with age. Physical inactivity results in functional decline, loss of independence, and increased disease burden 7. While a secondary benefit of exercise interventions is purported to be to an increase in general physical activity participation, only one published randomized controlled trial has examined the level of physical activity among their participants afterwards 8 and none has done so in the context of different types of group-based exercise programs or in frail older adults, such as those with low bone mass. It may be hypothesized that participation in group-based exercise programs would exert a positive change in general physical activity 7.
Recently, it was reported that both group-based resistance and agility training significantly reduced fall risk profile compared with a stretching program in women aged 75 to 85 years with low bone mass (i.e., osteoporosis or osteopenia) 9. In the present paper, these participants were observed during a 12-month period immediately after cessation of the 3 types of exercises to assess: (i) how fall risk profile changed after each was ceased, and (ii) participants’ level of physical activity.
METHODS
Study Design
A 12-month follow-up study immediately following the completion of our 25-week randomized controlled trial of three different types of exercises 9 was conducted. There were two measurement sessions during the 12-month follow-up, at 8 and 12 months post trial completion. Assessors were blinded to the participants’ original exercise group assignments.
Participants
The participants of this 12-month follow-up study were 98 women with low bone mass, aged 75 to 85 years at recruitment, who completed the 25-week randomized controlled trial that has been described previously9. The recruitment process for the randomized controlled trial identified all women aged 75 to 85 years who were residents of Vancouver and in whom osteoporosis or osteopenia had been diagnosed at the BC Women’s Hospital and Health Centre (T-score at the total hip or spine at least 1.0 standard deviations below the young normal sex-matched areal bone mineral density of the Lunar reference database) 10. The number of participants in the treatment arms at each the stage of the 25-week randomized controlled trial have been previously reported 9.
The 98 women who completed the 25-week randomized controlled trial were invited to participate in the one-year follow-up study. As none of the three exercise intervention programs offered during the trial were available at the community level at trial completion, all participants were provided information regarding various group-based exercise programs offered for older adults by local community centres.
The study was approved by the University Clinical Research Ethics Board and the Research Committee of the Women’s Hospital of British Columbia. All participants gave written informed consent prior to study participation.
Randomization (Original Trial)
After baseline assessment, participants were randomly assigned to one of three groups: Resistance Training, Agility Training, and Stretching (sham exercise). Randomization was stratified by baseline postural sway (cm), bisphosphonate use (yes/no), and baseline total hip area bone mineral density (g/cm2).
Exercise Intervention (Original Trial)
These exercise programs have been detailed elsewhere 9. Participants were required to attend their assigned exercise program twice weekly.
Descriptive Variables
General health was assessed at baseline of the 25-week randomized controlled trial by a questionnaire 11 relating to current medication use, current supplement use, and medical conditions. Cognitive state was assessed at baseline using the Folstein’s Mini-Mental State Examination (MMSE) 12. Falls were also documented by monthly fall calendars during the 12-month follow-up period.
Primary Outcome Measure – Fall Risk
Participant’s fall risk was assessed at the 8- and 12-month follow-up measurement periods using the Physiological Profile Assessment (PPA) © 13 (Prince of Wales Medical Research Institute, Randwick, Sydney, NSW, Australia). The PPA is a valid 14,15 and reliable 16 tool for assessing fall risk in older people. Based on the performance of five physiological domains (vision, proprioception, strength, reaction time and balance), the PPA computes a fall risk score (standardized score) for each individual and this measure has a 75% predictive accuracy for falls in older people over a 12-month period 14,15.
Secondary Outcome Measures – Physical Activity & Formal Exercise Participation
Each participant’s current level of physical activity was ascertained at the 8- and 12-month follow-up measurement periods with the Physical Activities Scale for the Elderly (PASE) questionnaire 17,18. As well, participants were asked if they were participating in any formal exercise classes or programs. Formal exercise programs were defined as those that are supervised, offered by community-centres, organizations, or by individuals, and they could be group-based or individual-based (e.g., personal training).
Statistical Analysis
Data were analysed using SPSS 19 statistical software. Variables that were not normally distributed (sway and hand reaction time) were transformed using natural logarithm before comparisons between the groups were made 9. Comparisons of group characteristics and baseline scores were undertaken using a Chi Square test for differences in proportions and Students t-tests for differences in means. Fall risk (i.e., PPA score), the five components of PPA, physical activity level (i.e., PASE scores) measured at the 8- and 12-month follow-up measurement periods were compared by forced entry multiple linear regression analysis, with trial completion scores and experimental group included as independent variables in the models 9. Multivariate analysis of variance (MANOVA) with repeated measures was used to determine whether there were significant changes in PPA scores, dominant quadriceps strength, postural sway, hand reaction time, joint position sense, and PASE scores at the end of the 12-month follow-up compared with trial completion and 8-month follow-up values within each of the three experimental groups (Resistance Training, Agility Training, and Stretching). Polynomial contrasts were also selected giving measures of linear and quadratic trends in the analyses of fall risk and current physical activity level. Finally, paired t-tests were used to determine within-group differences between baseline and 12-month follow-up values in fall risk scores. The overall alpha level was sets at P ≤ .05.
RESULTS
Descriptive Variables
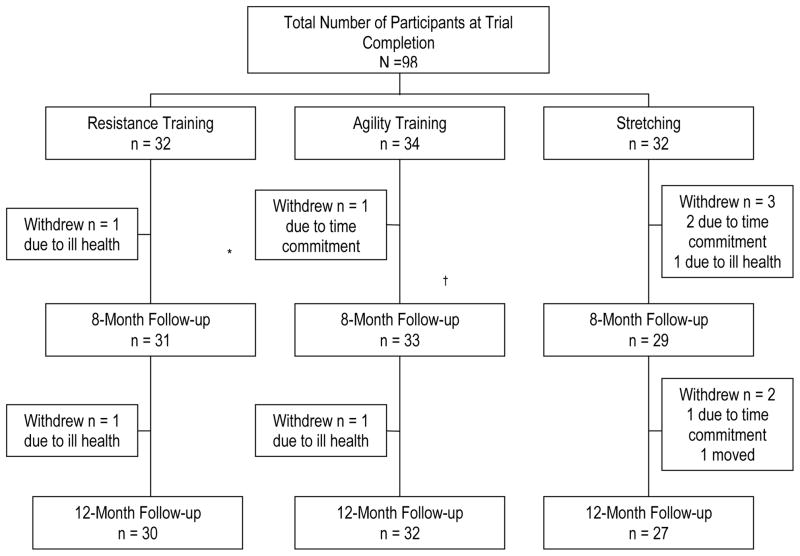
Of the 98 participants who completed the 25-week randomized controlled trial, 93 participants were assessed at the 8-month follow-up measurement period and 89 participants at the 12-month follow-up measurement period (Figure 1).
Figure 1.
Flow Chart Outlining Number of Participants in Each Study Arm during the 12-Month Follow-up
The mean age of women at baseline of the randomized controlled trial was 79 ± 3 years. The three groups did not differ in any of the descriptive variables at baseline and there were no differences in exercise adherence during the 25-week intervention period (Table 1). From baseline to end of the 12-month follow-up, no major changes in general health were observed among the participants except in four individuals (two from Resistance Training, one each from Agility Training and Stretching). Of the two individuals from the Resistance Training group, one suffered a heart attack and the other became unable to live independently and moved in with her daughter. Chronic obstructive pulmonary disease became increasingly symptomatic for the one participant from the Agility Training group. The participant from the general Stretching group fell and fractured her sacrum. These women were unable to participate follow-up measurement sessions as a direct result of their medical conditions.
Table 1.
Descriptive Statistics for Descriptor Variables (N = 98)
| Variable * † | Resistance (n = 32) | Agility (n = 34) | Stretching (n = 32) |
|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | |
| Baseline Age (yr) | 79.6 (2.1) | 78.9 (2.8) | 79.5 (3.2) |
| Baseline Height (cm) | 160.1 (6.0) | 157.0 (6.1) | 158.3 (8.4) |
| Trial Completion Height (cm) | 159.9 (6.0) | 156.8 (6.2) | 158.4 (8.3) |
| Baseline Weight (kg) | 59.9 (9.4) | 62.5 (9.3) | 65.2 (12.6) |
| Trial Completion Weight (kg) | 58.7 (9.2) | 61.5 (8.7) | 64.2 (12.7) |
| Prescribed Medications at Baseline | 2.6 (2.3) | 3.2 (2.1) | 4.1 (3.3) |
| Number of Classes Attended§ | 41.0 (9.4) | 41.9 (6.1) | 37.8 (10.1) |
| Baseline PASE Score|| | 98.0 (51.8) | 83.3 (35.1) | 76.3 (30.0) |
| Baseline MMSE Score (max 30 pts)|| | 28.7 (1.4) | 28.6 (1.4) | 28.3 (1.9) |
| Osteoarthritis¶ | 11 (34.4) | 13 (38.2) | 17 (53.1) |
| Osteoarthritis of the Knee¶ | 5 (15.6) | 6 (17.6) | 6 (18.8) |
| Use of Walking Aid¶ | 4 (12.5) | 2 (5.9) | 5 (15.6) |
| Formal Exercise Participation¶ # | 16 (53.3) | 21 (65.6) | 13 (48.1) |
yr = year; cm = centimetres; kg = kilograms; PASE = Physical Activity Scale for the Elderly; MMSE = Mini-Mental State Examination
SD = standard deviation;
There were no significant differences among the groups for any measure.
During the 25-week intervention period. Maximum number of classes required to be attended was 48.
PASE scores may range from 0 to 400 (or higher), with a higher value indicative of higher levels of physical activity. MMSE scores: Scores of 24 to 30 indicate no cognitive impairment. Scores of 18 to 23 indicate mild cognitive impairment. Scores of 0 to 17 indicate severe cognitive impairment 30.
Count (%). Count=Number of “yes” cases within each group. % =Percent of “yes” cases within each group.
During the 12-month follow-up period. N = 89. Resistance Training = 30, Agility Training = 32, Stretching = 27.
PPA Fall Risk Score & Its Components
Table 2 shows the fall risk (i.e., PPA scores) at baseline, trial completion, 8- and 12-month follow-up for the three experimental groups. The regression analyses revealed no significant between-group differences in fall risk at the 8- and the 12-month follow-up measurement periods (P ≥ .226). Fall risk at the end of the 12-month follow-up period was not significantly different from trial completion and 8-month follow-up values within each of the three experimental groups (P ≥ .229). The paired t-tests indicated a significant difference in fall risk from baseline to the end of the 12-month follow-up period within all three groups (P ≤ .001). There were also no significant between-group differences (P ≥ .383) or within-group differences (P ≥ .108) in any of the PPA components.
Table 2.
Mean Values (SDs) for Fall Risk and Current Physical Activity Level – Baseline, Trial Completion, 8-Month Follow-up, and 12-Month Follow-up
| Variable*† | Baseline | Trial Completion | 8-Month F/U | 12-Month F/U |
|---|---|---|---|---|
| Mean (SD) (N = 98) | Mean (SD) (N = 98) | Mean (SD) (N = 93) | Mean (SD) (N = 89) | |
| Resistance | (n = 32) | (n = 32) | (n = 31) | (n = 30) |
| Fall Risk Score | 2.2 (0.7) | 1.0 (1.0)§ | 1.1 (1.1) | 1.3 (1.0)¶ |
| Postural Sway (mm) | 230.1 (93.1) | 159.6 (82.0)|| | 176.30 (86.24) | 188.2 (96.1) |
| Quadriceps Strength (kg) | 17.2 (7.2) | 18.9 (8.6) | 19.2 (7.7) | 18.7 (8.6) |
| Hand Reaction Time (msec) | 328.3 (44.3) | 267.8 (52.3) | 277.0 (55.8) | 283.0 (59.5) |
| Proprioception (deg) | 2.2 (2.1) | 1.5 (1.2) | 1.5 (1.2) | 2.0 (2.1) |
| Edge Contrast (dB) | 17.8 (2.1) | 19.2 (2.2) | 19.5 (1.8) | 19.5 (1.8) |
| PASE Score | 98.0 (51.8) | 100.6 (45.4) | 92.9 (48.5) | 103.6 (49.5) |
| Agility | (n = 34) | (n = 34) | (n = 33) | (n = 32) |
| Fall Risk Score | 2.4 (0.9) | 1.3 (0.9)§ | 1.3 (1.0) | 1.4 (1.1)¶ |
| Postural Sway | 219.2 (80.3) | 155.3 (91.1)|| | 175.7 (87.1) | 175.5 (78.1) |
| Quadriceps Strength | 17.0 (6.5) | 17.2 (7.9) | 18.4 (7.5) | 16.2 (7.2) |
| Hand Reaction Time | 337.8 (61.4) | 294.9 (55.1) | 286.6 (57.9) | 290.8 (63.0) |
| Proprioception | 1.8 (1.2) | 1.5 (1.2) | 1.7 (1.2) | 1.9 (1.5) |
| Edge Contrast | 17.3 (2.3) | 18.7 (2.7) | 19.0 (3.0) | 18.9 (3.5) |
| PASE Score | 83.3 (35.1) | 97.5 (37.0) | 91.1 (45.9) | 108.8 (40.4) |
| Stretching | (n = 32) | (n = 32) | (n = 29) | (n = 27) |
| Fall Risk Score | 1.9 (0.8) | 1.5 (1.2) | 1.3 (1.1) | 1.2 (1.0)¶ |
| Postural Sway | 217.0 (104.7) | 217.4 (148.2) | 207.1 (124.8) | 197.8 (181.1) |
| Quadriceps Strength | 16.1 (7.2) | 17.5 (6.4) | 19.2 (6.8) | 17.5 (9.2) |
| Hand Reaction Time | 307.6 (43.1) | 280.7 (60.2) | 274.2 (53.8) | 271.5 (50.3) |
| Proprioception | 1.7 (0.9) | 1.8 (1.2) | 2.2 (1.1) | 2.0 (1.3) |
| Edge Contrast | 18.0 (1.5) | 18.6 (1.9) | 19.7 (1.6) | 19.6 (2.3) |
| PASE Score | 73.6 (30.0) | 101.8 (42.9) | 94.7 (45.2) | 110.0 (58.1) |
F/U = follow-up
SD = standard deviation
PASE = Physical Activity Scale for the Elderly
mm = millimetres
kg = kilograms
msec = milliseconds
deg = degrees
dB = decibels
High fall risk scores, high sway values, high reaction time values, low quadriceps strength values, and low edge contrast scores indicate impaired performances. PASE scores may range from 0 to 400 (or higher), with a higher value indicative of higher levels of physical activity.
Significantly different from the Stretching group at P < .01 (by forced entry multiple linear regression analysis) 9.
Significantly different from the Stretching group at P < .05 (by forced entry multiple linear regression analysis) 9.
Significantly different from baseline value at P ≤ .001 (by paired t-tests).
The Agility and Resistance Training groups both demonstrated a general trend towards an increase in fall risk over the 12-month follow-up period. However, this trend was not significant as the repeated measure MANOVA analysis indicated an insignificant linear contrast (P ≥ .104) and an insignificant quadratic contrast (P ≥ .873) for change in fall risk for both experimental groups.
The Stretching group demonstrated a general trend towards an improvement in fall risk throughout the 12-month follow-up period. However, this trend was not significant as the repeated measure MANOVA analysis indicated an insignificant linear contrast (P = .199) and an insignificant quadratic contrast (P = .817).
Physical Activity Level & Formal Exercise Program Participation
Table 2 shows the current physical activity level at baseline, trial completion, 8- and 12-month follow-up. The regression analyses revealed no significant between-group differences in current physical activity level at the 8- and 12-month follow-up measurement periods (P ≥ .788). Current physical activity level at the end of the 12-month follow-up period was not significantly different from trial completion and 8-month follow-up values within both the Resistance Training and the general Stretching groups (P ≥ .241). However, the repeated measures MANOVA indicated a significant increase in current physical activity during the 12-month follow up within the Agility Training group (P = .023).
All three experimental groups demonstrated a non-linear trend of a decrease in physical activity at the 8-month follow-up period and a subsequent increase in physical activity at the 12-month follow-up period. However, this trend was found to be significant only in the Agility Training group (where P = 0.031 for the quadratic contrast). All linear contrasts were non-significant (P ≥ .104).
Of the 89 participants who completed the follow-up study, 50 participated in formal exercise during the 12-month period. These formal exercise programs included personal training, cardiac rehabilitation, and group-based exercise programs tailored for older adults with low bone mass that include both resistance and balance training. Of the 50 individuals, 16 were former participants of the Resistance Training group, 21 of the Agility Training group, and 13 of the Stretching group (Table 1). Chi Square test indicated no significant differences in these proportions (P = .371).
Falls
Based on the monthly fall calendars, there were four fallers from the Resistance Training group, five from the Agility Training group, and seven from the Stretching group during the 12-month follow-up period. Specifically, there were 5 falls in the Resistance Training group, six in the Agility Training group, and nine in the Stretching group.
DISCUSSION
The risk of falling among former participants of group-based exercise programs remained unchanged (i.e., still reduced fall risk) 12 months after the exercise programs ceased and remained significantly reduced compared with baseline values. Specifically, the mean fall risk at the end of the follow-up period was still 43.3% * reduced from baseline among former participants of the Resistance Training group and 40.1% reduced in the Agility Training group. These novel findings inform the physiology of detraining in the aging population and imply that researchers studying cost-effectiveness of exercise interventions for falls prevention might consider extending the period of analysis beyond the time-frame of the intervention and its immediate follow-up period.
Although the risk of falling at the end of the one-year follow-up was maintained from trial completion, a gradual increase in fall risk was observed in both the Resistance Training and the Agility Training groups over the 12-month period. From trial completion to the end of the follow-up period, the risk of falling increased by 30.6% in the Resistance Training group, and by 15.2% in the Agility Training group. These percentage changes in fall risk are large compared to previous published detraining studies of bone health 20, muscle strength 21, and muscle cross-sectional area 21 and may be attributable, at least in part, to the substantial reductions of PPA scores observed during the intervention period 9.
Aging, withdrawal of a targeted exercise intervention, and physical inactivity could all have contributed to the increase in fall risk after withdrawal of exercise. Based on normative data 13 one would expect a 79 year-old (i.e., mean baseline age of cohort) woman’s fall risk score to increase by 0.09 standard deviations when she reaches 80 years of age. However, as the magnitude of changes in fall risk from trial completion to the end of the follow-up period were greater than 0.09 (range for the three groups, 0.19 to 0.31), aging does not account for all the observed increase in fall risk.
In addition to aging, withdrawing the exercise programs may have contributed to the observed increase in fall risk in both the Resistance and Agility Training groups. Although individuals were free to attend exercise programs during the 12-month observational period, those who had participated in the resistance and agility exercise programs commonly stated that they had difficulty finding exercise programs as challenging as those undertaken during the intervention. Thus, while a high proportion of the former participants of the resistance and agility training programs participated in formal exercise programs during the follow-up period (Table 1), these programs were reported (subjectively) to be of lesser intensity. Thus, a relative reduction in the intensity of exercise programs may have contributed to the increase in fall risk. This study was not designed specifically to quantify such a contribution.
Contrary to the trend in fall risk observed in the Resistance Training and Agility Training groups, a trend of gradual fall risk reduction was observed among former participants of the Stretching group during the follow-up period. Former participants of the Stretching group demonstrated a 37.4% fall risk reduction from baseline at the end of the follow-up year compared with only a 20.2% 9 risk reduction at trial completion. This trend appears somewhat at odds with the current evidence on the types of exercises that reduce falls and fall risk in older adults 22 (i.e., muscle strengthening and balance retraining 23 and Tai Chi 24). The participants of the general stretching program may have reduced their fall risk by increasing participation in general physical activities (8%; NS), as indicated by the PASE scores, over the one-year follow-up period. Such physical activity may have presented a greater challenge to their physiological systems than that they were encountering in the Stretching classes; these classes were specifically designed to provide core strength and flexibility, but avoided resistance training or balance exercises. Nevertheless, this speculation must remain guarded and future studies may investigate the mechanisms that underpin maintenance, or loss, of exercise-induced reductions in fall risk.
Current physical activity levels at the end of the one-year follow-up period were maintained (i.e., still elevated) from trial completion values. Specifically, at the end of the follow-up period, a 3.8% increase was observed in current physical activity from baseline for the Resistance Training group, a 29.2% increase for the Agility Training group, and 37.7% increase for the general Stretching group. Furthermore, 56.2% of the 89 older women participated in formal exercise programs during the 12-month follow-up. These data reinforce Kriska’s 8 finding that older women who participated in a randomized clinical trial of walking intervention demonstrated higher levels of physical activity compared with controls 10 years after the intervention stopped. One should note the temporary reduction in physical activity at 8-month follow-up (only significant for the Agility Training group) which took place in spring. This was likely related to a seasonal fluctuation in physical activity levels 25, as both trial completion and 12-month follow-up measurement sessions occurred in summer.
The results of this one-year follow-up study indicate that physiological benefits of group-based exercise programs extended at least 12 months beyond the intervention period itself in older women with low bone mass. However, the conclusions that can be drawn about physical activity in this population are limited. Physical activity is a difficult variable to measure and although self-reported measures of current physical activity are commonly used in research studies, they are imperfect 26,27 and are unlikely to be as accurate as direct, objective and prospective measures of physical activity (i.e., pedometers) 28. However, even pedometers cannot measure the different dimensions of an exercise prescription (i.e., intensity, type) that may influence fall risk. Finally, the primary study outcome was fall risk, as opposed to falls. Thus, future research using falls as the primary outcome measure is needed to confirm the persisting beneficial effect of different types of exercises on falls in those with low bone mass.
In conclusion, fall risk profile remained significantly 29 reduced among former participants of three types of group-based exercise programs even one year after the formal cessation of exercise programs. Also, current physical activity levels remained maintained (i.e., still elevated) from trial completion among all three exercise groups. Thus, these six-month intervention exercise programs appeared to act as a catalyst for increasing physical activity with resultant reductions in fall risk that were maintained for at least 18 months among older women with low bone mass. Taken together, these findings support the implementation of all three types of group-based exercise programs in reducing fall risk profile and promoting general physical activity population of older women at high risk of fracture.
Acknowledgments
Funding Source:
This study was supported by a grant from the Vancouver Foundation (BCMSF), salary support to Khan KM from the CIHR (IMA), to Eng JJ from CHIR (MSH-63617), and to Khan KM from the MSFHR, and trainee support to Liu-Ambrose TYL from MSFHR and CIHR Fellowship.
The authors thank the Vancouver Foundation (BCMSF, Operating Grant) and the BC Women’s Hospital Osteoporosis Program, the Vancouver South Slope YMCA management and members who enthusiastically supported the study by allowing free access to participants for the training intervention, and the Osteoporosis Society of Canada, BC Branch, for support with recruitment of participants. The authors are indebted to Ms Connie Waterman, Director of the BC Women’s Hospital Osteofit Program for her help in designing and implementing the training interventions, Dr. Lynda Thayer for the medical assessments, and Ms. Margie Bell for coordinating the measurement sessions. We thank the instructors for their commitment to the participants’ health and safety. Drs. Khan and Eng are Canadian Institutes of Health Research (Institute of Musculoskeletal Health and Arthritis) New Investigators. Drs. McKay and Eng are Michael Smith Foundation for Health Research (MSFHR) Career Scholars. Dr. Liu-Ambrose is a MSFHR, CIHR ICE Grant Post-doctoral Trainee, and CIHR Fellow.
Footnotes
Competing Interests: None.
Contributions & Sponsor’s Role: TLA, KMK, and HAM were responsible for study concept and design. SRL and JJE significantly contributed to study design. TLA and GLG were responsible for data acquisition. TLA, SRL and GLG were responsible for data analyses. TLA, KMK, and SRL were responsible for the interpretation of the results. All authors were responsible for writing and editing of this manuscript. KMK and HAM were co-sponsors and principal investigators of this study.
Percent changes were calculated based on the scores of the 89 individuals who completed the 12-month follow-up study.
References
- 1.Tinetti ME. Clinical practice. Preventing falls in elderly persons. N Engl J Med. 2003;348:42–49. doi: 10.1056/NEJMcp020719. [DOI] [PubMed] [Google Scholar]
- 2.Grimely-Evans J. Fallers, non-fallers and Poisson. Age Ageing. 1990;19:268–269. doi: 10.1093/ageing/19.4.268. [DOI] [PubMed] [Google Scholar]
- 3.Carter ND, Kannus P, Khan KM. Exercise in the prevention of falls in older people: A systematic literature review examining the rationale and the evidence. Sports Med. 2001;31:427–438. doi: 10.2165/00007256-200131060-00003. [DOI] [PubMed] [Google Scholar]
- 4.Campbell A, Robertson M, Gardner M, et al. Falls prevention over 2 years: a randomized controlled trial in women 80 years and older. Age Ageing. 1999;28:513–518. doi: 10.1093/ageing/28.6.513. [DOI] [PubMed] [Google Scholar]
- 5.Hauer K, Rost B, Rutschle K, et al. Exercise training for rehabilitation and secondary prevention of falls in geriatric patients with a history of injurious falls. J Am Geriatr Soc. 2001;49:10–20. doi: 10.1046/j.1532-5415.2001.49004.x. [DOI] [PubMed] [Google Scholar]
- 6.Sherrington C, Lord SR, Finch CF. Physical activity interventions to prevent falls among older people: update of the evidence. J Sci Med Sport. 2004;7:43–51. doi: 10.1016/s1440-2440(04)80277-9. [DOI] [PubMed] [Google Scholar]
- 7.Phillips E, Schneider J, Mercer G. Motivating elders to initiate and maintain exercise. Arch Phys Med Rehabil. 2004;85:S52–S57. doi: 10.1016/j.apmr.2004.03.012. [DOI] [PubMed] [Google Scholar]
- 8.Pereira M, Kriska A, Day R, et al. A randomized walking trial in postmenopausal women: Effects on physical activity and health 10 years later. Arch Intern Med. 1998;158:1695–1701. doi: 10.1001/archinte.158.15.1695. [DOI] [PubMed] [Google Scholar]
- 9.Liu-Ambrose T, Khan K, Eng J, et al. Both resistance and agility training reduce fall risk in 75–85 year old women with low bone mass: A six-month randomized controlled trial. J Am Geriatr Soc. 2004;52:657–665. doi: 10.1111/j.1532-5415.2004.52200.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.WHO Study Group. WHO Technical Report Series. Geneva: World Health Organization; 1994. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. [PubMed] [Google Scholar]
- 11.Krieger N, Tenenhouse A, Joseph L, et al. The Canadian Multicentre Osteoporosis Study. Can J Aging. 1999;18:376–387. [Google Scholar]
- 12.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 13.Lord S, Sherrington C, Menz H. Risk factors and strategies for prevention. Cambridge: Cambridge University Press; 2001. A physiological profile approach for falls prevention. Falls in older people; pp. 221–238. [Google Scholar]
- 14.Lord S, Clark R, Webster I. Physiological factors associated with falls in an elderly population. J Am Geriatr Soc. 1991;39:1194–1200. doi: 10.1111/j.1532-5415.1991.tb03574.x. [DOI] [PubMed] [Google Scholar]
- 15.Lord S, Ward J, Williams P, et al. Physiological factors associated with falls in older community-dwelling women. J Am Geriatr Soc. 1994;42:1110–1117. doi: 10.1111/j.1532-5415.1994.tb06218.x. [DOI] [PubMed] [Google Scholar]
- 16.Lord S, Castell S. Physical activity program for older people: Effect on balance, strength, neuromuscular control, and reaction time. Arch Phys Med Rehabil. 1994;75:648–652. doi: 10.1016/0003-9993(94)90187-2. [DOI] [PubMed] [Google Scholar]
- 17.Washburn RA, Smith KW, Jette AM, et al. The Physical Activity Scale for the Elderly (PASE): Development and evaluation. J Clin Epidemiol. 1993;46:153–162. doi: 10.1016/0895-4356(93)90053-4. [DOI] [PubMed] [Google Scholar]
- 18.Washburn RA, McAuley E, Katula J, et al. The physical activity scale for the elderly (PASE): Evidence for validity. J Clin Epidemiol. 1999;52:643–651. doi: 10.1016/s0895-4356(99)00049-9. [DOI] [PubMed] [Google Scholar]
- 19.SPSS. SPSS Base 8.0, Applications Guide. Chicago: SPSS Inc; 1992. [Google Scholar]
- 20.Dalsky G, Stocke K, Ehsani A, et al. Weight-bearing exercise training and lumbar bone mineral content in postmenopausal women. Ann Intern Med. 1988;108:824–828. doi: 10.7326/0003-4819-108-6-824. [DOI] [PubMed] [Google Scholar]
- 21.Trappe S, Williamson D, Godard M. Maintenance of whole muscle strength and size following resistance training in older men. J Gerontol A Biol Sci Med Sci. 2002;57:B138–143. doi: 10.1093/gerona/57.4.b138. [DOI] [PubMed] [Google Scholar]
- 22.Gillespie L, Gillespie W, Robertson M, et al. The Cochrane Database of Systematic Reviews. 2002. Interventions for preventing falls in elderly people; p. 3. [DOI] [PubMed] [Google Scholar]
- 23.Campbell J, Robertson M, Gardner M, et al. Randomised controlled trial of a general practice programme of home based exercise to prevent falls in elderly women. BMJ. 1997;315:1065–1069. doi: 10.1136/bmj.315.7115.1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wolf SL, Barnhart HX, Kutner NG, et al. Reducing frailty and falls in older persons: an investigation of Tai Chi and computerized balance training. Atlanta FICSIT Group. Frailty and Injuries: Cooperative Studies of Intervention Techniques. J Am Geriatr Soc. 1996;44:489–497. doi: 10.1111/j.1532-5415.1996.tb01432.x. [DOI] [PubMed] [Google Scholar]
- 25.Tudor-Locke C, Bassett DR, Swartz AM, et al. A preliminary study of one year of pedometer self-monitoring. Ann Behav Med. 2004;28:158–162. doi: 10.1207/s15324796abm2803_3. [DOI] [PubMed] [Google Scholar]
- 26.Matt G, Garcia M, Primicias W, et al. Exploring biases in self-reported exercising behavior heuristics based on recency, frequency, and preference. Percept Mot Skills. 1999;88:126–128. doi: 10.2466/pms.1999.88.1.126. [DOI] [PubMed] [Google Scholar]
- 27.Klesges R, Eck L, Mellon M, et al. The accuracy of self-reports of physical activity. Med Sci Sports Exerc. 1990;22:690–697. doi: 10.1249/00005768-199010000-00022. [DOI] [PubMed] [Google Scholar]
- 28.Tudor-Locke C, Williams JE, Reis JP, et al. Utility of pedometers for assessing physical activity: construct validity. Sports Med. 2004;34:281–291. doi: 10.2165/00007256-200434050-00001. [DOI] [PubMed] [Google Scholar]
- 29.Campbell A, Borrie M, Spears G. Risk factors for falls in a community-based prospective study of people 70 years and older. J Gerontol. 1989;44:M112–117. doi: 10.1093/geronj/44.4.m112. [DOI] [PubMed] [Google Scholar]
- 30.Tombaugh TN, McIntyre NJ. The mini-mental state examination: a comprehensive review. J Am Geriatr Soc. 1992;40:922–935. doi: 10.1111/j.1532-5415.1992.tb01992.x. [DOI] [PubMed] [Google Scholar]