Abstract
Background
Psychiatric disorders are known to be a risk factor for the development of different oral health problems especially for dental caries and periodontal diseases. In spite of this fact, no study has been conducted to reveal its magnitude in Ethiopia. Hence, this study was conducted to determine the oral health status of psychiatric patients at Jimma University Specialized Hospital (JUSH), Psychiatric Clinic.
Methods
A hospital based cross- sectional study was used from January to May 2011. A total of 240 participants were included in the study. Dental examination was done to measure indices of oral health: decayed, missing, and filled teeth (DMFT) index and community periodontal index (CPI). Oral examination was performed using mirror, probe and explorer by experienced dental doctors. A simple random sampling technique was implemented to collect data. ANOVA test, binary logistic and multinomial logistic regression analyses were done using SPSS 16.0 statistical software.
Results
The mean DMFT score among the psychiatric patients was 1.94±2.12 (mean±SD) with 1.28±1.69, 0.51±1.19 and 0.14±0.48 (mean±SD) for decayed, missed and filled teeth respectively. Only about 24% of the psychiatric patients had a healthy CPI score. Incorrect tooth brushing technique was significantly associated with a DMFT score greater than 2 (AOR = 3.58; 95% CI: 1.65, 7.79). The habit of sweet intake was also associated with dental caries (AOR = 2.91; 95% CI: 1.43, 5.95). Similarly, patients with a smoking habit also demonstrated statistically significant association with dental caries (AOR = 18.98; 95% CI: 5.06, 71.24).
Conclusion
The oral health status of the psychiatric patients was poor. Thus, health education about oral hygiene should be given for psychiatric patients so they can avoid the frequent intake of sweets, smoking and learn correct tooth brushing technique.
Introduction
Oral health is fundamental to general health and essential for wellbeing. The psychosocial impact of oral health problem significantly diminishes quality of life [1], [2]. It affects eating, talking and other social and psychological areas of life [3]. Dental caries and periodontal disease are the two most common diseases that affect oral health [4], [5]. Up to 90% of the world population could be affected with periodontal diseases demonstrating the high rates of infection. If left untreated, it can lead to progressive loss of the alveolar bone around the teeth, resulting in loosening and loss of teeth. Psychosocial factors and certain medical conditions such as diabetes and infection with human immunodeficiency virus were identified as risk factors for poor oral hygiene [6]–[8].
On the other hand, mental health is one of the fundamental components of health [9], [10]. Over 450 million people are estimated to be suffering from mental disorders in the world today [11] and it affects people at all socioeconomic levels [12]. According to a cross sectional community based study carried out in Jimma town, the prevalence of mental disorder was 22.7% [13]. Major depressive disorder and schizophrenia were the most common disorders seen in JUSH while bipolar disorder and anxiety occurred at a lesser percentage [14].
People with severe mental illness have a greater risk to oral diseases than those without. This is because of various reasons such as the type and severity of mental illness, lack of personal perception of oral health problems, poor oral hygiene, specific dental phobia, difficulty in accessing health care facilities, the side effects of psychiatric drugs, poor diet, self-neglect and dental professional’s knowledge and attitudes toward people with mental illness. At the same time dental treatment is difficult for these patients because of their lack of motivation and apathy, limited cooperation, low adaptability to new prostheses, mobility difficulties, fear of treatment, poor communication as well as financial considerations [15]–[19].
In the past two decades, it has been reported that the consequence of oral health whether from mental illness or other causes, has an effect on general health. It results in a range of medical conditions including cardiovascular diseases, type 2 diabetes, adverse pregnancy outcome, osteoporosis, aspiration pneumonia and rheumatoid arthritis. Current evidence suggests that improved oral health should be encouraged as part of the healthy lifestyle message to reduce the burden of chronic disease [20]. In Ethiopia, oral health has a low priority in the context of mental illness. To the best of our knowledge, no information is available regarding oral health among patients with mental disorders in Ethiopia. Hence, the purpose of this study was to assess oral health status of psychiatric patients at JUSH.
Methods
Ethical Statement
The research protocol conducted by the department of Dentistry in the Psychiatric Clinic of JUSH has been reviewed and approved by the ethical committee of Jimma University. Permission was sought from the psychiatry clinic to conduct the study. The purpose of the study was clearly explained to the participants, their guardians/care-givers and psychiatric clinic staffs. Participants fulfilling the inclusion criteria were included in the study only after obtaining an informed written consent from their guardians/care-givers as they had a reduced capacity to be consented. For literates, they themselves read the consent request. But for those who could not read, the data collectors read for them and obtained their signature or finger print to affirm their consent. To ensure participants confidentiality code numbers replaced names and no personal identifiers were included in the written questionnaires.
Study Design and Area
A hospital based cross-sectional study was conducted in JUSH, Psychiatric Clinic. Jimma town is located south west of Addis Ababa, the capital of Ethiopia. This Psychiatric center was chosen because it is the only psychiatric clinic providing psychiatric service in South West Ethiopia for a population of 2,495,795 in the Zone.
Participants
We included patients who had a primary diagnosis of dementia, schizophrenia, anxiety, depressive and bipolar affective disorders. These same patients whose conditions were deemed very serious thus posing limited ability to cooperate were excluded as were those with alcohol or substance use disorders, brain injury, intellectual disability and aggression tendencies.
The sample size was determined using single population proportion formula by assuming that 50% of the patients will have oral health problem to obtain maximum sample size with 95% confidence level and 5% level of significance. The total sample size was 384. From these eligible study subjects, 91(23.7%) were too ill and aggressive to continue after being engaged for the study and 53(13.8%) flatly refused to participate. As a result, the final study group included 240 (62.5%) participants.
Measurements
Socio-demographic data was collected by a well-trained dental intern using pre-tested and structured questionnaire which had been designed based on the primary objective of the study. The questionnaire was prepared in English, translated into local languages and then re-translated back to English to check for consistency. Dental examination was carried out by two experienced dentists as required by a WHO protocol [21]. The two experienced dentists read, understood and standardized their methods of operation so as to minimize error and have reproducible data. CPI was assessed by using a North Carolina probe (HuFriedy®) calibrated every millimeter. All teeth in a sextant were recorded. Data was collected from six sites on every tooth present and registered on a chart. Mental health diagnosis was determined by mental health professionals. Our information was then obtained from medical histories after the patient diagnosis.
DMFT score and CPI were considered as dependent variables. Socio-demographic variables: age, sex, occupation, marital status, educational level; and factors predisposing for oral health problems including oral hygiene habit, frequency of tooth brushing, smoking habit, type of psychiatric disorder, duration of psychiatric illness, Khat chewing habit, sweet intake habit, medication used for the illness were taken as explanatory variables. ANOVA test, univariate and multivariate logistic regression and multinomial logistic regression analyses were done using SPSS version 16 software. The mean DMFT score of our study was 1.94±2.12, but for the purpose of comparison we rounded off the decimal and used 2 as mean DMFT.
Results
Study Subjects Characteristics
From a total of 240 total participants, one-hundred and sixty eight (70%) were males, psychiatric patients age ranged from15–68 (29.9±9.79; mean age (year) ±SD. One–hundred and fifty six (65.0%) were Muslim in religion, one-hundred and fifty eight (65.8%) were Oromo in ethnicity, ninety six (40.0%) had secondary school education, sixty three (26.2%) were farmers in occupation and one-hundred and fifteen (47.9%) were single in marital status category ( Table 1 ).
Table 1. Socio-demography of the study participants.
| Socio-demographic data | Frequency (%) |
| Sex | |
| Male | 168(70) |
| Female | 72(30) |
| Age (years) | |
| 15–34 | 164(68.3) |
| 35–54 | 69(28.8) |
| 55–68 | 7(2.9) |
| Ethnicity | |
| Oromo | 158(65.8) |
| Amhara | 58(24.2) |
| Tigrae | 21(8.8) |
| Kefa | 3(1.2) |
| Religion | |
| Muslim | 156(65.0) |
| Orthodox | 61(25.4) |
| Protestant | 21(8.8) |
| Catholic | 2(0.8) |
| Marital status | |
| Single | 115(47.9) |
| Married | 98(40.8) |
| Divorced | 10(4.2) |
| Widowed | 17(7.1) |
| Educational status | |
| Illiterate | 18(7.5) |
| Read and write | 11(4.6) |
| Primary school | 63(26.2) |
| Secondary school | 96(40) |
| Higher education | 52(21.7) |
| Occupation | |
| Daily laborer | 11(4.6) |
| Farmer | 63(26.2) |
| Government employee | 50(20.8) |
| Merchant | 19(7.9) |
| Student | 57(23.8) |
| Others | 40(16.7) |
Mental Health
Amongst two-hundred forty study subjects, about one-hundred fifty eight (65.8%) of patients had a diagnosis of depression, forty two (17.5%) had psychotic disorders (such as schizophrenia), and twenty (8.3%) had anxiety disorder. Five (2.1%) epilepsy, four (1.7%) bipolar disorder and the remainder eleven (4.6%) had others psychiatric disorders (e.g. dementia, somatization disorder and sexual dysfunction).
The majority of patients, one hundred and fifty eight (65.8%) were receiving antidepressant (like amitriptyline, imipramine, fluoxetine). Forty-two (17.5%) and nine (3.8%) were taking antipsychotics (such as haloperidol, thioridazine, fluphenazine decanoate, chlorpromazine) and anti-convulsant drugs (like carbamazepine, phenobarbital) respectively. Only thirty one (12.9%) of subjects were taking other kind of psychiatric medications such as anxiolytics (like diazepam), mood stabilizers (like sodium valproate), and drugs for sexual dysfunction (such as sildenafil citrate).
Oral Health Status
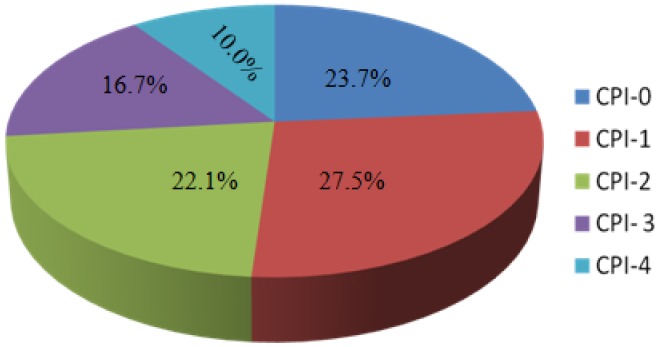
The DMFT score of the study subjects ranged from 0 to 13 (1.94±2.12; mean±SD). The number of decayed teeth ranged from 0 to 11 (1.28±1.69). Most of the subjects had no filled teeth, only five (2.1%) had restorations; the number of filled teeth ranged between 0 and 4 with 0.14±0.48. The number of missing teeth ranged from 0 to 11 (0.51±1.19). The respondent’s CPI score ranged from 0 to 4 (1.6±1.28). Only about one fourth of the study subjects had a healthy CPI score of zero. Sixty six (27.5%) of the patients had bleeding and twenty four (10%) had greater than six mm pocket depth ( Figure 1 ).
Figure 1. CPI score among the study participants.
Risk Factors for Oral Health Problems
ANOVA result for the relationship between type of psychiatric illness diagnosed and DMFT (F5, 234 = 3.48, p = 0.01), filled component scores (F5, 234 = 2.52, p = 0.3), for decayed one (F5, 234 = 2.78, p = 0.02) showed statistically significant association. Whereas, missing component scores (F5, 234 = 0.89, p = 0.49) and CPI ((F5, 234 = 1.82, p = 0.11) did not.
Logistic regression analysis to determine the relationship between the dental carries status and socio-demographic characteristics is presented in Table 2. The relationship between mean DMFT score had statistically significant relation with sex and age while ethnicity, marital status, and educational level were not statistically significant (p>0.05). Males are more likely to have dental caries with DMFT greater than 2 than females [Adjusted OR = 3.23, (95% CI: 1.31, 7.98)] and as age goes up DMFT score also increases. Considering the age group 15–34 years as a reference, study subjects in the 35–54 years age group and in the 55–68 years age group were observed to have a statistically significant more likely- hood to have a DMFT score greater than 2 indicating a higher level of dental caries [AOR = 2.74; (95% CI = 1.3, 5.7) and (AOR = 20.14; (95% CI = 2.51, 161.69 respectively)] ( Table 2 ).
Table 2. Association of mean DMFT index and socio-demographic characteristics.
| DMFT index >2 | ||||
| Variables | P –value | Crude OR(95% CI) | P –value | Adjusted OR(95% CI) |
| Sex | ||||
| Female | 1 | 1 | 1 | 1 |
| Male | 0.001 | 3.79(1.76,8.16) | 0.11 | 3.23(1.31,7.98) |
| Age (years) | ||||
| 15–34 | 1 | 1 | 1 | 1 |
| 35–54 | 0.042 | 1.88(1.02, 3.47) | 0.008 | 2.74(1.3,5.74) |
| 55–68 | 0.014 | 8.29(1.55, 44.45) | 0.005 | 20.14(2.51,161.69) |
| Ethnicity | ||||
| Amhara | 1 | 1 | 1 | 1 |
| Oromo | 0.374 | 1.38(0.68,2.79) | 0.191 | 1.87(0.73,4.79) |
| Gurage | 0.126 | 6.92(0.58,82.55) | 0.277 | 4.16(0.32,54.42) |
| Tigrae | 0.168 | 2.13(0.73,6.24) | 0.572 | 1.419(0.42,4.78) |
| Marital status | ||||
| Divorced | 1 | 1 | 1 | 1 |
| Married | 0.357 | 2.13(0.43,10.57) | 0.56 | 1.93(0.21,17.68) |
| Single | 0.634 | 1.48(0.29,7.34) | 0.66 | 1.66(0.17,16.13) |
| Widowed | 0.286 | 0.25(0.2,3.19) | 0.54 | 0.38(0.18, 8.3) |
| Educational status | ||||
| Illiterate | 1 | 1 | 1 | 1 |
| Read and write | 0.99 | N/A | 0.999 | 0.0(N/A) |
| Primary school | 0.22 | 2.33(0.6,8.96) | 0.22 | 2.92(0.52,16.36) |
| Secondary school | 0.318 | 1.96(0.52,7.3) | 0.46 | 1.95(0.33,11.3) |
| Higher education | 0.162 | 2.65(0.68,10.36) | 0.29 | 2.74(0.41,18.28) |
NB: N/A = Not Applicable.
Tooth brushing technique was also found to be associated with dental caries status. Psychiatric patients who were brushing their teeth incorrectly were statistically significantly more likely to have a DMFT score greater than 2 than those who brushed their teeth correctly (AOR = 3.58; 95% CI: 1.65, 7.79). Habit of sweet intake was also statistically significantly associated with dental caries. Participants with a habit of sweet intake were statistically significantly more likely to have a higher dental caries than those who had no habit of taking sweet (AOR = 2.91; 95% CI: 1.43, 5.95). Patients with smoking habit demonstrated statistical significant association with dental caries. Smokers are highly likely to have a greater DMFT score compared to non-smokers (AOR = 18.98; 95% CI: 5.06, 71.24). Likewise, type of treatment given for mental illness was also statistically significantly associated with dental caries. Psychiatric patients taking anti-depressants and anti-psychotics are statistically significantly more likely to have a bad dental hygiene (AOR = 3.73; 95% CI: 0.99, 13.93, AOR = 20.0; 95% CI: 4.66, 86.04) respectively compared to subjects with other types of treatments ( Table 3 ).
Table 3. Factors associated with mean DMFT index for periodontal disease.
| DMFT index >2 | |||||
| Variables | Frequency (%) | P –value | Crude OR(95% CI) | P-value | Adjusted OR(95% CI) |
| Tooth brushing technique | |||||
| Incorrect | 127(52.9) | 0.01 | 2.15(1.19,3.85) | 0.001 | 3.58(1.65,7.79) |
| Correct | 113(47.1) | 1 | 1 | 1 | 1 |
| Do you take sweet? | |||||
| Yes | 117(48.8) | 0.00 | 2.97(1.65,5.38) | 0.003 | 2.91(1.43,5.95) |
| No | 123(51.2) | 1 | |||
| How often do you brush your tooth? | |||||
| Once a day | 17(7.1) | 0.99 | NA | 0.99 | NA |
| > one times a day | 9(3.8) | 0.99 | NA | 0.99 | NA |
| Irregularly | 210(87.5) | 0.99 | NA | 0.99 | NA |
| Don’t clean | 4(1.7) | 1 | 1 | ||
| Do you smoke? | |||||
| Yes | 28(11.7) | 0.00 | 2.15(1.19,3.85) | 0.00 | 18.98(5.06,71.24) |
| No | 212(88.3) | 1 | 1 | ||
| Do you chew Khat? | |||||
| Yes | 56(23.3) | 0.001 | 8.54(3.54,20.61) | 0.77 | 1.15(0.45,2.96) |
| No | 184(76.7) | 1 | 1 | ||
| Psychiatric treatment | |||||
| Antidepressant | 158(65.8) | 0.16 | 2.21(0.73,6.72) | 0.05 | 3.73(0.99,13.93) |
| Anti-conversant | 9(3.8) | 0.49 | 2.91(0.29,12.77) | 0.23 | 4.58(0.39,53.66) |
| Anti-psychosis | 42(17.5) | 0.001 | 8.17(2.43,27.49) | 0.00 | 20.0(4.66, 86.04) |
| Others | 31(12.9) | 1 | 1 | ||
| Duration of psychiatric illness (months, mean) | |||||
| >45.9 | 85(35.4) | 0.533 | 0.83(0.46,1.5) | 0.057 | 0.46(0.21,1.02) |
| ≤45.9 | 155(64.6) | 1 | 1 | ||
NB: N/A = Not Applicable.
For CPI score, a multiple logistic regression analysis model was employed for socio-demographic characteristics and risk factors. There was a significant association of sex, marital status and educational level with CPI ( Table 4 ). Habit of sweet intake, type of psychiatric medication, illness duration and tooth brushing technique had also significant association with CPI ( Table 5 ).
Table 4. Multiple logistic regression analysis model for socio-demographic characteristics against CPI score.
| Variables | 2 Log likelihood ofreduced model | Chi-Square | Degree of freedom | Significance |
| Age | 359.41 | 9.36 | 4 | 0.053 |
| Sex | 368.26 | 18.21 | 4 | 0.001 |
| Marital status | 374.95 | 24.91 | 12 | 0.015 |
| Educational status | 385.66 | 35.61 | 16 | 0.003 |
| Ethnicity | 369.75 | 19.69 | 12 | 0.073 |
Table 5. Multiple logistic regression analysis model for risk factors against CPI score.
| Variables | 2 Log likelihood of reducedmodel | Chi- Square | Degree of freedom | Significance |
| Smoking | 351.250 | 1.912 | 4 | 0.752 |
| Time of tooth cleaning | 374.881 | 25.543 | 16 | 0.061 |
| Tooth brushing technique | 365.423 | 16.085 | 8 | 0.041 |
| Chewing Khat | 355.314 | 5.976 | 4 | 0.201 |
| Habit of sweet intake | 384.205 | 34.867 | 4 | 0.000 |
| Type of medication | 402.181 | 52.843 | 16 | 0.000 |
| Illness duration | 374.021 | 24.683 | 4 | 0.000 |
Discussion
In this study, attempts have been made to assess oral health status of psychiatric patients and factors related to dental caries and periodontal status in JUSH. The study had two limitations. First, despite its higher chance of detecting dental caries and the need for treatment, we could not use X-ray imaging; rather we used physical (dental) examination for assessing dental caries. The second was lack of literatures on the subject at a country level for comparison and discussion purposes.
Oral health status was assessed by DMFT score which is a measure of dental caries and CPI as periodontal status indicator. The mean DMFT score in our study was 1.94±2.12 (mean±SD), which was greater than general population of Ethiopian immigrants to Israel with mean DMFT of 1.48±3.16 [22]. In contrast, the findings of Jovanović et al [23], Zusman et al [16], Lewis et al [19], Ramon et al [24], Chu et al [25], Rekha et al [26] and Adeniyi et al [12] demonstrated mean DMFT score of 24.4, 23.8, 19.1, 17.5, 13.9, 6.1 and 2.3 respectively, which were higher than this study. The lower DMFT index in this study might be due to difference in age ranges, type of medication taken by psychiatric patients and duration of illness among study subjects. The mean number of decayed teeth in this study was 1.28. This finding was consistent with a study conducted by Kumar et al [27]. In contrast, it was lower than studies reported by Jovanović et al [23], Zusman et al [16] and Ramon et al [24]. A 0.51 mean of number of missed teeth was also reported in this study and it was lower than studies conducted in Israel [16], Serbia [23] and South Wales [19]. The mean number of filled teeth was 0.14. This finding was similar to a study conducted by Adeniyi et al [12] and lower than studies by Lewis et al [19] and Zusman et al [16]. This is possibly suggestive of reduced access to dental service and care of the study psychiatric patients than for those in developed countries.
Results of multiple logistic regression showed that mean DMFT was associated with sex of study subjects. Being male is a risk factor for development of dental caries. This finding is supported by the result of Jovanović et al [23] and male subjects might, due to culture, have a higher probability of chewing khat and smoking compared to females who generally do not indulge in these habits. At the same time, age has been associated with DMFT. An increase in age raised the mean DMFT score in the study; this was consistent with previous findings [12], [24], [27]. Marital status, ethnicity and educational level had no significant association with dental caries. Absence of association between dental caries and educational level was also reported in studies conducted by Adeniyi et al and Chu et al [12], [25].
Mean DMFT score also increased with the duration of mental illness, tooth brushing technique and sweet intake. Kumar et al [27] and Jovanović et al [23] also reported the association of DMFT scores with duration of mental illness. This study demonstrated statistical association between taking anti-psychotic and anti-depressant treatments and dental caries. The relation of anti-depressant treatment is in accordance with a study done in Serbia [23]. This could probably be because of anti-psychotropic and anti-depressant medications which result in reduced saliva thus causing mouth dryness and exposing study subjects for dental caries [26]. The association of smoking with dental caries was also observed in this study and the results are similar to studies by Millar et al and Ravald et al [28], [29]. We further found DMFT index association with chewing khat in univariate analysis. This finding may provide a new risk factor, which has not yet been reported for dental caries.
In this study, about 27% of psychiatric patients demonstrated periodontal pockets (shallow or deep pockets), whereas it was 5.3% [22] in a study conducted among the general population of Ethiopian immigrants to Israel. This clearly shows a higher degree of periodontal disease in psychiatric patients than the general population of Ethiopia.
Multinomial logistic regression analysis showed sex, marital status and educational level to be associated with periodontal status. In contrast, the finding of Jovanović et al [23] demonstrated its association with sex and absence of association with marital status. Females showed better periodontal conditions in this study possibly due to the culture and norm that prevents female subjects from chewing khat and smoking practices. Likewise, we found that tooth brushing technique, sweet intake habit, medication type and illness duration being statistically associated with periodontal disease predicted with CPI values. This could be explained by the fact that all of the patients already had very high CPI scores and hence there was almost no variation in this value.
In conclusion, our psychiatric patients have a poor oral health status. Therefore, health education about oral hygiene to avoid high and frequent intake of sweets, smoking and horizontal tooth brushing should be given for psychiatric patients. When psychiatric patients are prescribed for anti-depressants, the effect of the treatment should be taken into consideration and psychiatric patients could be referred to dental clinic for preventative measures.
Acknowledgments
We are grateful to the study participants and their guardians/care-givers for their participation in the study and provision of necessary information. We also acknowledge JU for the grant.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: The authors acknowledge Jimma University (JU) for the grant. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.WHO. The World Oral Health Report 2003: Continuous improvement of oral health in the 21st century –the approach of the WHO Global Oral Health Programme (publication number WHO/NMH/NPH/ORH/03.2) Geneva. 2003.
- 2.Terezakis E, Needleman I, Kumar N, Moles D, Agudo E. The impact of hospitalization on oral health: A systematic review. J Clin Periodontol. 2011;38:628–636. doi: 10.1111/j.1600-051X.2011.01727.x. [DOI] [PubMed] [Google Scholar]
- 3.Mirza I, Day R, Wulff-Cochrane V, Phelan M. Oral health of psychiatric in-patients. A point prevalence survey of an inner-city hospital. Psychiatr Bull. 2001;25:143–145. [Google Scholar]
- 4.Selwitz RH, Ismail AI, Pitts NB. Dental caries. Lancet. 2007;369:51–59. doi: 10.1016/S0140-6736(07)60031-2. [DOI] [PubMed] [Google Scholar]
- 5.Petersen PE. Priorities for research for oral health in the 21st Century- the approach of the WHO Global Oral Health Programme. Community Dent Health. 2005;22:71–74. [PubMed] [Google Scholar]
- 6.Pihlstrom BL, Bryan S Michalowicz BS, Johnson NW. Periodontal diseases. Lancet. 2005;366:1809–1820. doi: 10.1016/S0140-6736(05)67728-8. [DOI] [PubMed] [Google Scholar]
- 7.WHO. Oral Health in aging societies: Integration of oral health and General Health. Geneva: World Health Organization. 2006.
- 8.Jared H, Boggess KA. Periodontal diseases and adverse pregnancy outcomes: A review of the evidence and implications for clinical practice. J Dent Hyg. 2008;82:3–21. [Google Scholar]
- 9.WHO. mhGAP Mental Health Gap Action Programme: Scaling up care for mental, neurological and substance use disorders. Geneva: World Health Organization. 2008. [PubMed]
- 10.WHO. Integrating mental health into primary care: A global perspective. ISBN 978 92 4 156368 0. 2008.
- 11.WHO. Investing in mental health. ISBN 92 4 156257 9. 2003.
- 12.Adeniyi AA, Ola BA, Edeh CE, Ogunbanjo BO, Adewuya AO. Dental status of patients with mental disorders in a Nigerian teaching hospital: A preliminary survey. Spec Care Dentist. 2011;31:134–137. doi: 10.1111/j.1754-4505.2011.00193.x. [DOI] [PubMed] [Google Scholar]
- 13.Mekonnen E, Esayas S. Correlates of Mental Distress in Jimma Town, Ethiopia. Ethiop J Health Sci. 2003;13:39–49. [Google Scholar]
- 14.Girma E, Tesfaye M. Patterns of treatment seeking behavior for mental illnesses in Southwest Ethiopia: A hospital based study. BMC Psychiatry. 2011;11:138. doi: 10.1186/1471-244X-11-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Clifton A, Tosh G, Khokhar W, Jones H, Nicola Wells N. Oral Health Advice for People with Serious Mental Illness. Schizoph Bul. 2011;37:464–465. doi: 10.1093/schbul/sbq169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zusman SP, Ponizovsky AM, Dekel D, Masarwa A, Ramon T, et al. An assessment of the dental health of chronic institutionalized patients with psychiatric disease in Israel. Spec Care Dentist. 2010;30:18–22. doi: 10.1111/j.1754-4505.2009.00118.x. [DOI] [PubMed] [Google Scholar]
- 17.Stevens T, Spoors J, Hale R, Bembridge H. Perceived oral health needs in psychiatric in-patients: impact of a dedicated dental clinic. The Psychiatrist. 2010;34:518–521. [Google Scholar]
- 18.Bardow A, Nyvad B, Nauntofte B. Relationships between medication intake, complaints of dry mouth, salivary flow rate and composition, and the rate of tooth demineralization in situ. Arch Oral Biol. 2001;46:413–23. doi: 10.1016/s0003-9969(01)00003-6. [DOI] [PubMed] [Google Scholar]
- 19.Lewis S, Jagger RG, Treasure E. The oral health of psychiatric in-patients in South Wales. Spec Care Dentist. 2001;21:182–186. doi: 10.1111/j.1754-4505.2001.tb00252.x. [DOI] [PubMed] [Google Scholar]
- 20.Cullinan MP, Ford PJ, Seymour GJ. Periodontal disease and systemic health: current status. Aust Dent J 2009; 54 : doi. 2009;10(1111/j.1834-7819.2009.01144):x. doi: 10.1111/j.1834-7819.2009.01144.x. [DOI] [PubMed] [Google Scholar]
- 21.WHO. Oral health surveys. 1997. Basic methods, 4th ed. Washington: DC.
- 22.Vered Y, Zini A, Livny A, Mann J, Sgan- Cohen HD. Changing dental caries and periodontal disease patterns among a cohort of Ethiopian immigrants to Israel: 1999–2005. BMC Public Health 8:345 doi. 2008. pp. 10.1186/1471–2458–8-345. [DOI] [PMC free article] [PubMed]
- 23.Jovanović S, Milovanović SD, Gajić I, Mandić J, Latas M, et al. Oral Health Status of Psychiatric in-patients in Serbia and implications for their dental care. Croat Med J. 2010;51:443–450. doi: 10.3325/cmj.2010.51.443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ramon T, Grinshpoon A, Zusman SP, Weizman A. Oral health and treatment needs of institutionalized chronic psychiatric patients in Israel. Eur Psychiatry. 2003;18:101–105. doi: 10.1016/s0924-9338(03)00023-3. [DOI] [PubMed] [Google Scholar]
- 25.Chu KU, Yang NP, Chou P, Chiu HJ, Chi LY. Factors associated with dental caries among institutionalized residents with schizophrenia in Taiwan: A cross-sectional study. BMC Public Health. 2010;10:482. doi: 10.1186/1471-2458-10-482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rekha R, Hiremath SS, Bharath S. Oral health status and treatment requirements of hospitalized psychiatric patients in Bangalore city: a comparative study. J Indian Soc Pedod Prev Dent. 2002;20:63–67. [PubMed] [Google Scholar]
- 27.Kumar M, Chandu GN, Shafiulla MD. Oral health status and treatment needs in institutionalized psychiatric patients: One year descriptive cross sectional study. Indian J Dent Res. 2006;17:171–177. doi: 10.4103/0970-9290.29868. [DOI] [PubMed] [Google Scholar]
- 28.Millar WJ, Locker D. Smoking and oral health status. J Can Dent Assoc. 2007;73:2. www.cda-adc.ca/jcda/vol-73/issue-2/155.html. [PubMed] [Google Scholar]
- 29.Ravald N, Starkhammar Johansson C. Tooth loss in periodontally treated patients. Along-term study of periodontal disease and root caries. J Clin Periodontol, doi. 2011;10(1111/j.1600-051X.2011.01811):x. doi: 10.1111/j.1600-051X.2011.01811.x. [DOI] [PubMed] [Google Scholar]