Abstract
Background
Despite efforts to disseminate guidelines for managing chronic obstructive pulmonary disease (COPD), adherence to COPD guidelines remains suboptimal. Barriers to adhering to guidelines remain poorly understood.
Methods
Clinicians from two general medicine practices in New York City were surveyed to identify barriers to implementing seven recommendations from the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines. Barriers assessed included unfamiliarity, disagreement, low perceived benefit, low self-efficacy, and time constraints. Exact conditional regression was used to identify barriers independently associated with non-adherence.
Results
The survey was completed by 154 clinicians. Adherence was lowest to referring patients with a forced expiratory volume in one second (FEV1) <80% predicted to pulmonary rehabilitation (5%); using FEV1 to guide management (12%); and ordering pulmonary function tests (PFTs) in smokers (17%). Adherence was intermediate to prescribing inhaled corticosteroids when FEV1 <50% predicted (41%) and long-acting bronchodilators when FEV1 <80% predicted (54%). Adherence was highest for influenza vaccination (90%) and smoking cessation counseling (91%). In unadjusted analyses, low familiarity with the guidelines, low self-efficacy, and time constraints were significantly associated with non-adherence to ≥2 recommendations. In adjusted analyses, low self-efficacy was associated with less adherence to prescribing inhaled corticosteroids (OR: 0.28; 95% CI: 0.10, 0.74) and time constraints were associated with less adherence to ordering PFTs in smokers (OR: 0.31; 95% CI: 0.08, 0.99).
Conclusions
Poor familiarity with recommendations, low self-efficacy, and time constraints are important barriers to adherence to COPD guidelines. This information can be used to develop tailored interventions to improve guideline adherence.
Keywords: COPD, guidelines, adherence, primary care
Background
Chronic obstructive pulmonary disease (COPD) is a highly prevalent disease that is projected to become the third leading cause of mortality worldwide by 20201,2 and that results in considerable health care expenditures with an estimated annual cost of $50 billion in the United States, alone.3 To standardize treatment for COPD, an international group of experts in conjunction with the World Health Organization and the National Heart, Lung and Blood Institute (NHLBI) developed the Global Initiative for Chronic Obstructive Lung Disease (GOLD) in 1997. The main purpose of this project was to create and disseminate guidelines that would help prevent COPD and would establish a standard of care for treating patients with COPD based on the most current medical evidence.4 The GOLD guidelines, last updated in 2010, are widely recognized by professional medical organizations in the US and internationally as the most complete and up-to-date source of information regarding COPD care.5
Even though the GOLD Dissemination Committee has made major efforts to increase awareness of the guidelines, studies suggest that the adoption of the GOLD guidelines has been suboptimal.6–9 For example, in a recent study of 200 individuals treated at a family medicine clinic, only 50% of patients diagnosed as having COPD ever underwent pulmonary function tests (PFT) to confirm the presence of airway obstruction disease and only 40% received stage appropriate medications.8 While several studies have examined rates of non-adherence to the GOLD guidelines, few have examined physician barriers to adherence to the GOLD guidelines. This study was designed to assess the barriers to adherence to the GOLD guidelines for the outpatient management of COPD among primary care providers (PCPs), a group that provides approximately 80% of the care to patients with COPD in the US.
Methods
Our study population consisted of PCPs from hospital-based practices affiliated with Mount Sinai Medical Center, a large academic hospital, and North General Hospital, a community hospital. Both practices are located in East Harlem, New York, a community with a large population of underserved low-income and minority patients. PCPs were eligible for this study if they provided direct care to patients with COPD at either of these practices. Eligible PCPs were identified from clinic rosters; physicians-in-training were eligible once they had completed at least six months of internal medicine residency. No pulmonary specialists were recruited for this study. The study protocol was approved by the Institutional Review Boards of the Mount Sinai School of Medicine and North General Hospital.
Survey Instrument
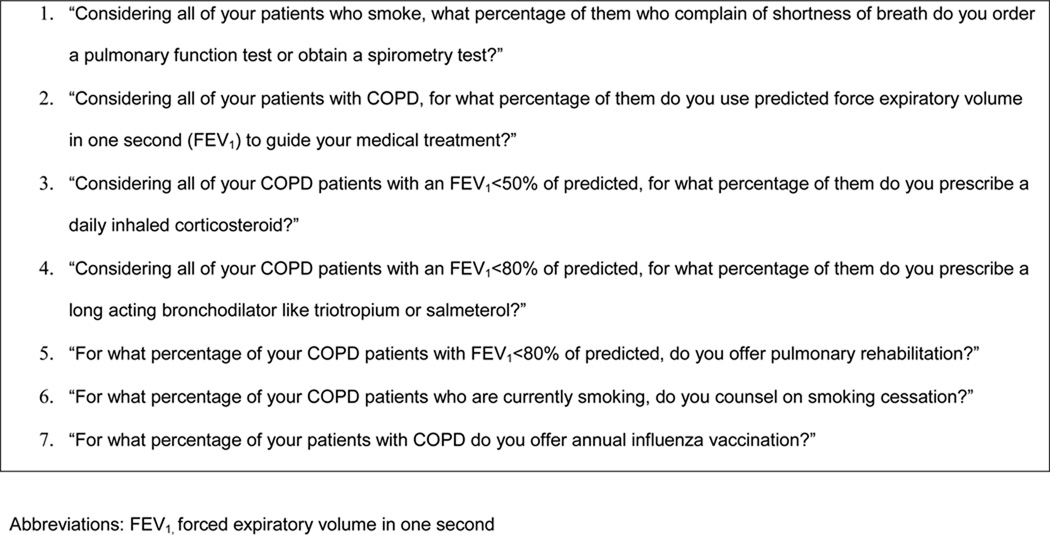
A standardized, self-administered questionnaire was used to collect information about provider sociodemographics, year of graduation, number of COPD patients seen in the outpatient setting in a “typical” month, level of training (faculty vs. trainee), and whether the provider had a family history of COPD. Providers were asked to report their adherence to seven COPD management practices recommended by the GOLD guidelines that are essential to quality outpatient COPD care and are recommended by the GOLD guidelines (Figure 1). Specifically, PCPs were asked whether they ordered PFTs or spirometry to diagnose COPD in smokers; used forced expiratory volume in one second (FEV1) to guide treatment of COPD; prescribed inhaled corticosteroids for COPD patients with an FEV1 <50% predicted; prescribed long-acting bronchodilators for COPD patients with FEV1 <80% predicted; offered pulmonary rehabilitation for COPD patients with FEV1 <80% predicted; counseled on smoking cessation; and offered annual influenza vaccination. Providers reported whether they were adherent to each guideline component 0%, 1% to 25%, 26% to 50%, 51% to 75%, 76% to 99%, or 100% of the time. Providers who reported following a practice >75% of the time were classified as adherent to that recommendation; other providers were classified as non-adherent.10,11
Figure 1.
Survey Items Assessing Adherence to Seven Chronic Obstructive Pulmonary Disease (COPD) Management Practices Recommended by the Global Initiative for Chronic Obstructive Lung Disease (GOLD) Guidelines
Barriers to guideline adherence were assessed using the theoretical model of Knowledge, Attitude, and Behavior.12,13 According to this model, for guidelines to be incorporated into everyday practice, a series of internal barriers (directly related to the provider) and external barriers (outside the provider’s control) need to be overcome. Internal barriers are considered to affect provider adherence through the cognitive and affective components of knowledge and attitudes. To assess knowledge, we asked providers whether they had heard about and/or had read the GOLD guidelines. In addition, irrespective of whether they had heard or read the GOLD guidelines, we asked them to rate their familiarity with each of the seven recommendations listed in the guidelines. Familiarity was assessed with a 4-point Likert Scale ranging from 1 (not familiar) to 4 (very familiar).
According to the model of Knowledge, Attitudes, and Behavior, physicians acquire information about caring for patients with COPD from multiple sources (e.g., supervisors, textbooks, peers) and guidelines represent just one source. Hence, physicians may still hold attitudes about specific COPD management practices even if they lack knowledge that these practices are recommended by specific guidelines. Accordingly, we asked all providers about their attitudes toward practices recommended by the guidelines irrespective of their knowledge about the GOLD guidelines. Specifically, providers were asked to rate 1) their level of agreement with each recommended practice; 2) their perception of the benefit of performing each practice; and 3) their self-efficacy for performing each recommendation. Self-efficacy refers to the belief that one can actually perform a behavior. Providers were asked to rate their responses using 4-point Likert scales for 1) level of agreement (completely disagree to completely agree), 2) perception of benefit (no benefit to large benefit), and 3) self-efficacy (not at all confident to very confident). To assess external workplace-related barriers, we asked providers how much their ability to follow each recommendation was limited by time constraints using a 4-point Likert scale (very limiting to not limiting).
When assessing attitudes and time constraints, providers were given a description of each recommended practice so that they could rate their responses to these items even if they lacked familiarity with the fact that the practice was recommended by the GOLD guidelines. For analytic purposes, responses were dichotomized and, according to convention, 11,14 a barrier was coded as present if a provider answered ≤2 on the corresponding Likert scale.
Statistical Analysis
We used the chi-square or Fisher exact test, when appropriate, to test whether the barriers identified by the conceptual model (lack of familiarity, disagreement with the guidelines, low perceived benefit, low self-efficacy, and time constraints) were individually associated with providers’ self-reported adherence to each guideline component. Exact conditional logistic regression analysis was used to assess whether specific barriers were independently associated with adherence to the guidelines after controlling for other COPD patient volume. In secondary analyses, we adjusted our model for provider type (faculty vs trainee). Multivariable analyses were not conducted to assess barriers to offering influenza vaccination and counseling on smoking cessation as a very small number of providers were non-adherent to these recommendations. Multivariable analyses were also not conducted to assess barriers to offering pulmonary rehabilitation as very few providers were adherent to this recommendation. Analyses were conducted with SAS version 9 statistical software (SAS Institute Inc, Cary, North Carolina).
Results
A total of 162 primary care providers were invited to participate in the study, of which 154 (95%) completed the survey (Table 1). The mean age of providers was 30 years; 57% were White; and 69% were internal medicine residents. There were no significant differences in the proportion of trainees and faculty who were aware of (50% vs 44%, respectively, p=0.57) or who had read these guidelines (39% vs 37%, respectively, p = 0.81).
Table 1.
Characteristics of Providers Caring for Patients with Chronic Obstructive Pulmonary Disease (N=154)*
| Characteristic | |
|---|---|
| Age in years, mean (SD) | 30 (7) |
| Male, No (%) | 78 (53) |
| Race, No (%) | |
| White | 85 (57) |
| Asian | 45 (30) |
| Black | 13 (9) |
| Other | 7 (5) |
| Ethnicity, No (%) | |
| Hispanic | 10 (7) |
| Level of training, No (%) | |
| Resident | 107 (70) |
| Faculty† | 45 (30) |
| Years since completing professional school, mean (SD) | 7 (7) |
| Number of outpatients with COPD seen per month, No (%) | |
| 0–5 | 51 (33) |
| 6–10 | 58 (38) |
| 11–20 | 30 (20) |
| >20 | 14 (9) |
| Family History of COPD, No(%) | 15 (10) |
Denominators for variables vary slightly due to missing responses. Fewer than 5% of responses were missing for these variables. Percentages may not add up to 100% as a result of rounding.
Includes 2 nurse practitioners
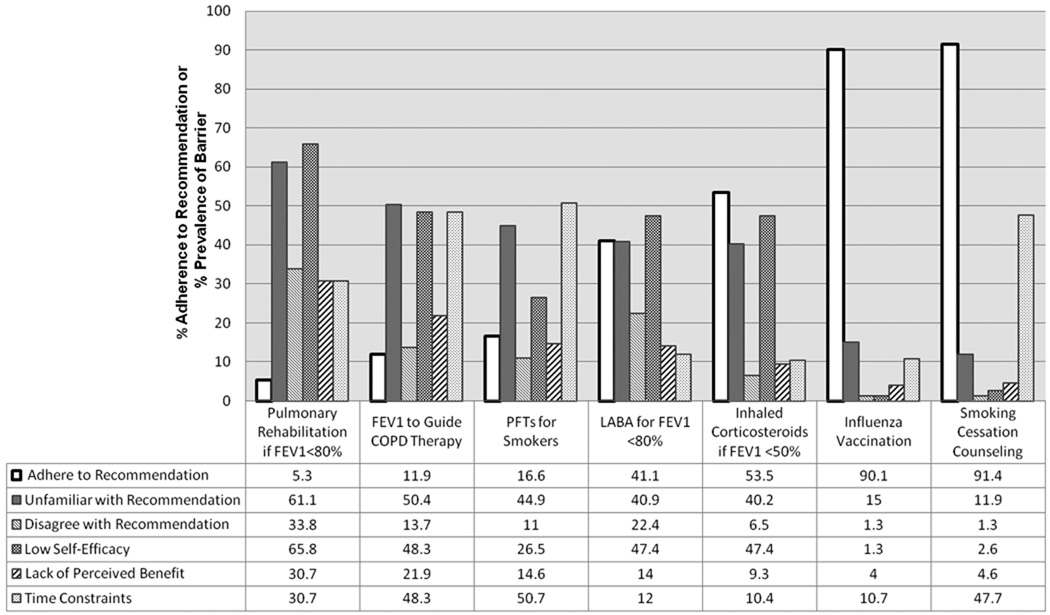
Rates of self-reported adherence to the seven outpatient practice recommendations evaluated in this study are shown in Figure 2. Rates of adherence were relatively low to several practices including: 1) ordering PFTs or spirometry in smokers with shortness of breath (17%); 2) using FEV1 to guide medical treatment in patients with COPD (12%); and 3) referring patients with FEV1 <80% predicted to pulmonary rehabilitation (5%). In contrast, there was high adherence to smoking cessation counseling (91%) and offering influenza vaccination (90%) for patients with COPD. Adherence was intermediate to prescribing inhaled corticosteroids to patients with FEV1 <50% predicted (41%) and long-acting bronchodilators to patients with FEV1 <80% predicted (54%). There were no significant associations between provider type and adherence to any of the specific guideline recommendations.
Figure 2.
Rates of Adherence and Prevalence of Barriers to Guideline Recommendations
Abbreviations: FEV1, forced expiratory volume in one second; PFTs, pulmonary function tests; LABA, long-acting beta-agonists
The pattern of barriers differed for each of the seven recommendations (Figure 2). For influenza vaccination, none of the barriers was present for more than 15% of clinicians. In contrast, for the recommendation to offer pulmonary rehabilitation to all patients with an FEV1 <80% predicted, each of the barriers was present for at least 30% of providers. Qualitatively, a higher overall prevalence of barriers was associated with lower adherence to guidelines.
Association between Barriers to Adherence and Specific Recommendations
Several internal barriers were associated with non-adherence to specific GOLD guideline recommendations (Table 2). Lack of familiarity with specific recommendations was associated with non-adherence to prescribed inhaled corticosteroids for patients with FEV1 <50% predicted (p=0.01) and to prescribing long-acting bronchodilators for patients with FEV1 <80% predicted (p=0.007). Low self-efficacy was associated with non-adherence to prescribing inhaled corticosteroids for patients with FEV1 <50% predicted, (p<0.001), prescribing long-acting bronchodilators for patients with FEV1 <80% predicted (p=0.04), and offering pulmonary rehabilitation to patients with FEV1 <80% predicted (p=0.01). Lack of perceived benefit was only associated with low adherence to ordering influenza vaccination (p<0.001). Disagreement with the guidelines and not knowing of their existence were not barriers (p>0.05) to adhering to any of the seven guideline components evaluated in this study.
Table 2.
Univariate Associations between Barriers to Adopting Guidelines and Adherence to Practices Recommended by the Global Initiative for Chronic Obstructive Lung Disease Guidelines*
| Practices Recommended the Global Initiative for Chronic Obstructive Lung Disease (GOLD) Guidelines | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Barriers | PFTs or spirometry for smokers |
FEV1 to guide therapy |
Inhaled corticosteroids if FEV1<50% |
LABA if FEV1 <80% |
Pulmonary rehabilitation if FEV1<80% |
Smoking cessation counseling |
Influenza vaccination |
||||||||
| % | P- value |
% | P- value |
% | P-value | % | P- value |
% | P- value |
% | P- value |
% | P- value |
||
| Did not hear about GOLD guidelines† |
|||||||||||||||
| Adherent | 48 | 0.68 | 39 | 0.25 | 46 | 0.18 | 50 | 0.73 | 75 | 0.28 | 51 | 0.47 | 48 | 0.004 | |
| Not adherent | 52 | 53 | 51 | 53 | 50 | 62 | 87 | ||||||||
| Unfamiliar with specific recommendation† |
|||||||||||||||
| Adherent | 43 | 0.84 | 33 | 0.18 | 31 | 0.01 | 26 | 0.007 | 0 | 0.06 | 10 | 0.07 | 15 | 0.53 | |
| Not adherent | 45 | 52 | 53 | 50 | 62 | 30 | 22 | ||||||||
| Disagree with specific recommendation |
|||||||||||||||
| Adherent | 12 | 0.99 | 6 | 0.46 | 4 | 0.18 | 15 | 0.06 | 13 | 0.27 | 1 | 0.99 | 2 | 0.99 | |
| Not adherent | 11 | 14 | 10 | 28 | 35 | 0 | 0 | ||||||||
| Low self-efficacy for perform specific recommendation† |
|||||||||||||||
| Adherent | 16 | 0.21 | 23 | 0.07 | 33 | <0.001 | 37 | 0.04 | 25 | 0.01 | 2 | 0.30 | 1 | 0.17 | |
| Not adherent | 28 | 51 | 64 | 54 | 69 | 8 | 7 | ||||||||
| Low perceived benefit of specific recommendation† |
|||||||||||||||
| Adherent | 24 | 0.15 | 22 | 0.98 | 9 | 0.77 | 12 | 0.46 | 13 | 0.43 | 4 | 0.11 | 9 | <0.001 | |
| Not Adherent | 13 | 22 | 10 | 16 | 31 | 15 | 60 | ||||||||
| Time limits ability to perform specific recommendation† |
|||||||||||||||
| Adherent | 25 | 0.007 | 35 | 0.27 | 9 | 0.60 | 12 | 0.85 | 25 | 0.47 | 44 | 0.46 | 6 | <0.001 | |
| Not adherent | 55 | 50 | 12 | 13 | 45 | 85 | 53 | ||||||||
Abbreviations: GOLD, Global Obstructive Lung Disease; PFT, pulmonary function test; FEV1 forced expiratory volume in one second; LABA, long-acting beta-agonist; p-values compare those with barrier present and adherent to each guideline recommendation to those with barrier present but not adherent to each guideline recommendation
p<0.05 for barrier present for adhering to one or more of the practices recommended by the GOLD guideline
The external barrier of time constraints was associated with non-adherence to ordering PFTs or spirometry on smokers who complain of shortness of breath (p=0.007) and with offering influenza vaccination (p<0.001). There was no association between the volume of COPD patients and any of the barriers or recommendations evaluated.
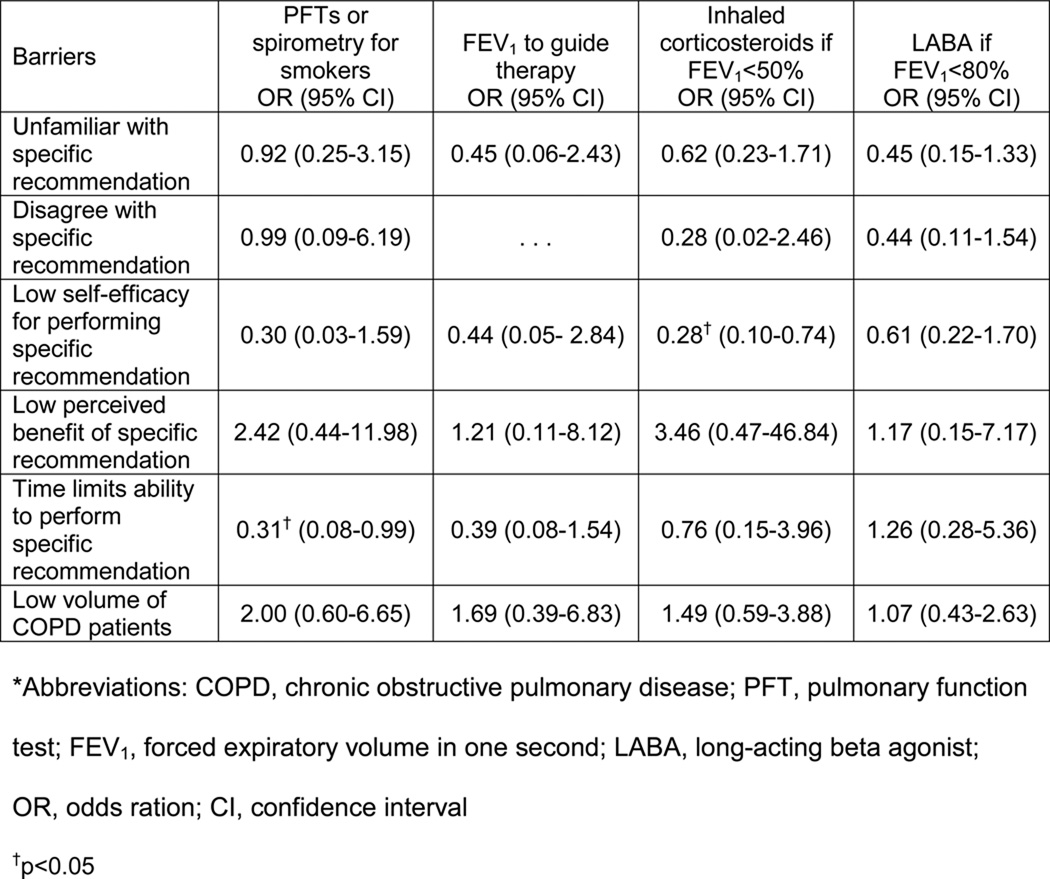
Results of Adjusted Analyses
Adjusted analysis showed that low self-efficacy in prescribing inhaled corticosteroids for COPD patients with FEV1 <50% predicted was a significant barrier in the fully adjusted model; providers who lacked confidence in their ability to perform this task were less adherent to prescribing corticosteroids according to PFT results compared to physicians who did not report this barrier (OR: 0.28; 95% CI: 0.10, 0.74). In addition, time constraints remained a significant barrier to performing PFTs to guide COPD treatment in smokers. Providers who reported time constraints as a barrier were less likely to adhere to PFTs than those who did not have this barrier (OR: 0.31; 95% CI: 0.08, 0.99). None of the other barriers including volume of COPD patients remained significant after testing them in the fully adjusted models.(Figure 3). Additional analyses (data not shown) that substituted volume of COPD patients with provider type (faculty vs trainee) did not significant alter any of the associations between barriers and adherence to selected COPD practices.
Figure 3.
Exact Conditional Logistic Regression Models of Primary Care Physician Adherence to 4 COPD Guideline Components*
Discussion
In this study, we found that PCPs’ adherence to GOLD guidelines was relatively poor, with <60% of providers being adherent to five of the seven assessed outpatient guideline recommendations. One important barrier identified in this study was low familiarity with specific recommendations of the GOLD guidelines. Low familiarity was associated with lower adherence to three of the guideline components on univariate analyses. Lack of adequate training in COPD management likely contributes to low familiarity. In a study of PCPs attending a respiratory conference, one in four respondents reported inadequate training in the management of COPD.6 Other studies have shown that medical students do not receive sufficient training in the interpretation of PFTs or in the diagnosis of COPD.15–17 In our study, even though the GOLD guidelines were first published more than a decade ago, less than half of respondents were aware of their existence and even fewer had read them. Hence, there may need to be greater resources dedicated to increasing awareness of the GOLD guidelines.
Another important barrier to the implementation of the GOLD guidelines among the PCPs surveyed in this study was low self-efficacy. This barrier remained present even after adjusting for low familiarity in one of the multivariable models. Low self-efficacy has previously been identified as an important barrier to implementing guidelines for the treatment of asthma.11 Each of the recommended practices for which low self-efficacy was associated with low adherence required interpreting PFTs and then recommending treatments based on these interpretations. Hence, low self-efficacy may reflect providers’ lack of confidence in their ability to interpret PFTs and/or to evaluate and counsel patients about the potential benefits, side-effects and adverse consequences of treatments to be recommended on the basis of PFTs. Interventions that aim to improve self-efficacy, such as the Institute for Healthcare Improvement’s Breakthrough Series (BTS), might be appropriate to improve adherence to the GOLD guidelines.18 BTS models are short-term (6- to 15-month) learning systems that bring together a large number of teams from hospitals or clinics with the intention to educate providers, and allow clinicians to implement and sustain practice changes. In one study of 18 practices that utilized the BTS model, rates of adherence to several of the GOLD guideline recommendations increased during a three year period.19
Providers who felt limited by time were less likely to order PFTs or spirometry to diagnose COPD in smokers. Studies evaluating possible causes of underuse of PFTs have found that lack of availability was a key issue,20,21 Yet, in this study, all clinicians had access to PFTs through their hospitals. Hence, it appears that just having access to PFT testing is insufficient for overcoming this barrier. It is possible that clinicians felt constrained by the amount of time it would take to interpret PFT results or to explain the rationale and results of PFTs to smokers. Alternatively, even though these tests were available at each practice, it is possible that there were barriers to ordering the test or obtaining results. Facilitating the delivery of PFT results with clear interpretation from pulmonary specialists may improve adherence to this guideline by PCPs. Time constraints were also associated with less adherence to offering influenza vaccination. To maximize adherence to this guideline, primary care practices might consider enlisting nurses or other members of the health care team to ensure this practice is universally implemented.
Pulmonary rehabilitation is a non-pharmacological intervention that has been consistently shown to decrease dyspnea and improve quality of life in patients with COPD.22,23 Adherence to this recommendation was very low (5%) among providers in this study and low self-efficacy was significantly associated with non-adherence to this guideline. In prior studies, low rate of referral to pulmonary rehabilitation was attributed to lack of availability of this service.6,20,24 It is possible that physicians in this study reported low confidence in being able to carry out this recommendation because they did not know how to refer patients to pulmonary rehabilitation, either because it was not available at their institutions or they were unpracticed at knowing how to access it.
In contrast with pulmonary rehabilitation, rates of adherence to smoking cessation counseling and influenza vaccination were high (≥ 90%). Both of these recommendations have been part of quality improvement interventions and broad public health campaigns independent of their relationship to COPD. Although 90% adherence is high, some might argue that this is still suboptimal. A larger sample size would be needed to assess whether any of the barriers in the Knowledge, Attitudes, Behavior model are related to suboptimal adherence to these recommendations.
There are several limitations to the interpretation of our findings. Providers were enrolled from two practices in New York City and, hence, providers may not be representative of other settings. Additionally, a large percentage of providers were internal medicine residents which limits the generalizability of the results. Yet, there were no significant differences in the proportion of trainees who were aware of GOLD guidelines or who adhered to the specific guideline recommendations compared to faculty. Further, most inner-city patients with COPD receive care in hospital-based clinics that are routinely staffed by residents. Also, adherence was based on self-report, and may represent an overestimate as a result of social desirability bias. Nevertheless, participants were instructed that their responses would be kept confidential and commonly reported non-adherence to many recommendations. Furthermore, self-reported rates of adherence to some recommendations such as use of long-acting bronchodilators and inhaled corticosteroids are comparable to those reported in other national surveys.8,25–27 The choice of cutpoint to determine adherence was somewhat arbitrary and the selection of a different cutpoint may have resulted in different estimates of guideline adherence.
Increasing adherence to GOLD guidelines has the potential to improve the outcomes of the large number of COPD patients. Our findings demonstrate that disagreement with the guidelines and lack of perceived benefit are not major barriers. Instead, our data suggest that educational interventions targeted at decreasing unfamiliarity and increasing self-efficacy for implementing the guidelines can improve COPD management. Efforts directed at improving knowledge of PFTs in COPD management and at facilitating the ordering and interpretation of PFTs have potential for the greatest impact. Special attention should also be paid to decreasing barriers to referring appropriate patients to pulmonary rehabilitation.
Acknowledgements
We wish to thank Luis Dominguez, MD, for his generous assistance with conducting this study at North General Hospital.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Murray CJ, Lopez AD. Global mortality, disability, and the contribution of risk factors: Global Burden of Disease Study. Lancet. 1997;349:1436–1442. doi: 10.1016/S0140-6736(96)07495-8. [DOI] [PubMed] [Google Scholar]
- 2.Halbert RJ, Natoli JL, Gano A, Badamgarav E, Buist AS, Mannino DM. Global burden of COPD: systematic review and meta-analysis. Eur Respir J. 2006;28:523–532. doi: 10.1183/09031936.06.00124605. [DOI] [PubMed] [Google Scholar]
- 3.Lin PJ, Shaya FT, Scharf SM. Economic implications of comorbid conditions among Medicaid beneficiaries with COPD. Respir Med. 2010;104:697–704. doi: 10.1016/j.rmed.2009.11.009. [DOI] [PubMed] [Google Scholar]
- 4.Global Initiative for Chronic Obstructive Lung Disease. [accessed September 12, 2010];Global strategy for diagnosis, management, and prevention of COPD [Internet] [updated 2009] Available from: http://www.goldcopd.org.
- 5.Rabe KF, Hurd S, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007;176:532–555. doi: 10.1164/rccm.200703-456SO. [DOI] [PubMed] [Google Scholar]
- 6.Yawn BP, Wollan PC. Knowledge and attitudes of family physicians coming to COPD continuing medical education. Int J Chron Obstruct Pulmon Dis. 2008;3:311–317. doi: 10.2147/copd.s2486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harvey PA, Murphy MC, Dornom E, Berlowitz DJ, Lim WK, Jackson B. Implementing evidence-based guidelines:inpatient management of chronic obstructive pulmonary disease. Intern Med J. 2005;35:151–155. doi: 10.1111/j.1445-5994.2004.00754.x. [DOI] [PubMed] [Google Scholar]
- 8.Chavez PC, Shokar NK. Diagnosis and management of chronic obstructive pulmonary disease (COPD) in a primary care clinic. COPD. 2009;6:446–451. doi: 10.3109/15412550903341455. [DOI] [PubMed] [Google Scholar]
- 9.Bourbeau J, Sebaldt RJ, Day A, et al. Practice patterns in the management of chronic obstructive pulmonary disease in primary practice: the CAGE study. Can Respir J. 2008;15:13–19. doi: 10.1155/2008/173904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garber E, Desai M, Zhou J, et al. Barriers to adherence to cystic fibrosis infection control guidelines. Pediatr Pulmonol. 2008;43:900–907. doi: 10.1002/ppul.20876. [DOI] [PubMed] [Google Scholar]
- 11.Wisnivesky JP, Lorenzo J, Lyn-Cook R, et al. Barriers to adherence to asthma management guidelines among inner-city primary care providers. Ann Allergy Asthma Immunol. 2008;101:264–270. doi: 10.1016/S1081-1206(10)60491-7. [DOI] [PubMed] [Google Scholar]
- 12.Woolf SH. Practice guidelines: a new reality in medicine. III. Impact on patient care. Arch Intern Med. 1993;153:2646–2655. [PubMed] [Google Scholar]
- 13.Cabana MD, Rand CS, Powe NR, et al. Why don't physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282:1458–1465. doi: 10.1001/jama.282.15.1458. [DOI] [PubMed] [Google Scholar]
- 14.Cabana MD, Rand CS, Becher OJ, Rubin HR. Reasons for pediatrician nonadherence to asthma guidelines. Arch Pediatr Adolesc Med. 2001;155:1057–1062. doi: 10.1001/archpedi.155.9.1057. [DOI] [PubMed] [Google Scholar]
- 15.Bolton CE, Ionescu AA, Edwards PH, Faulkner TA, Edwards SM, Shale DJ. Attaining a correct diagnosis of COPD in general practice. Respir Med. 2005;99:493–500. doi: 10.1016/j.rmed.2004.09.015. [DOI] [PubMed] [Google Scholar]
- 16.Tinkelman DG, Price D, Nordyke RJ, Halbert RJ. COPD screening efforts in primary care: what is the yield? Prim Care Respir J. 2007;16:41–48. doi: 10.3132/pcrj.2007.00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yawn BP, Yawn RA. Spirometry testing education in medical schools: a missed opportunity? Prim Care Respir J. 2005;14:21–24. doi: 10.1016/j.pcrj.2004.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.The Breakthrough Series: IHI’s Collaborative Model for Achieving Breakthrough Improvement. IHI Innovation Series white paper. 2003 (Accessed at (Available on www.IHI.org).)
- 19.Deprez R, Kinner A, Millard P, Baggott L, Mellett J, Loo JL. Improving quality of care for patients with chronic obstructive pulmonary disease. Popul Health Manag. 2009;12:209–215. doi: 10.1089/pop.2008.0043. [DOI] [PubMed] [Google Scholar]
- 20.Barr RG, Celli BR, Martinez FJ, et al. Physician and patient perceptions in COPD: the COPD Resource Network Needs Assessment Survey. Am J Med. 2005;118:1415. doi: 10.1016/j.amjmed.2005.07.059. [DOI] [PubMed] [Google Scholar]
- 21.Iqbal A, Schloss S, George D, Isonaka S. Worldwide guidelines for chronic obstructive pulmonary disease: a comparison of diagnosis and treatment recommendations. Respirology. 2002;7:233–239. doi: 10.1046/j.1440-1843.2002.00399.x. [DOI] [PubMed] [Google Scholar]
- 22.Wijkstra PJ, Ten Vergert EM, van Altena R, et al. Long term benefits of rehabilitation at home on quality of life and exercise tolerance in patients with chronic obstructive pulmonary disease. Thorax. 1995;50:824–828. doi: 10.1136/thx.50.8.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Berry MJ, Rejeski WJ, Adair NE, Zaccaro D. Exercise rehabilitation and chronic obstructive pulmonary disease stage. Am J Respir Crit Care Med. 1999;160:1248–1253. doi: 10.1164/ajrccm.160.4.9901014. [DOI] [PubMed] [Google Scholar]
- 24.Rutschmann OT, Janssens JP, Vermeulen B, Sarasin FP. Knowledge of guidelines for the management of COPD: a survey of primary care physicians. Respir Med. 2004;98:932–937. doi: 10.1016/j.rmed.2004.03.018. [DOI] [PubMed] [Google Scholar]
- 25.Yip NH, Yuen G, Lazar EJ, et al. Analysis of hospitalizations for COPD exacerbation: opportunities for improving care. COPD. 2010;7:85–92. doi: 10.3109/15412551003631683. [DOI] [PubMed] [Google Scholar]
- 26.Asche C, Said Q, Joish V, Hall CO, Brixner D. Assessment of COPD-related outcomes via a national electronic medical record database. Int J Chron Obstruct Pulmon Dis. 2008;3:323–326. doi: 10.2147/copd.s1857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Foster JA, Yawn BP, Maziar A, Jenkins T, Rennard SI, Casebeer L. Enhancing COPD management in primary care settings. MedGenMed. 2007;9:24. [PMC free article] [PubMed] [Google Scholar]