Abstract
Purpose
Adjacent level degeneration that occurs above and/or below long fusion constructs is a documented clinical problem that is widely believed to be associated with the considerable change in stiffness caused by the fusion. Some researchers have suggested that early degeneration at spinal joints adjacent to a fusion could be treated by implanting total disc replacements at these levels. It is thought that further degeneration could be prevented through the disc replacement’s design aims to reproduce normal disc heights, kinematics and tissue loading. For this reason, there is a clinical need to evaluate if a total disc replacement can maintain both the quantity of motion (i.e. range) and the quality of motion (i.e. center of rotation and coupling) at segments adjacent to a long spinal fusion. The purpose of this study was to experimentally evaluate range of motion (ROM—the intervertebral motion measured) and helical axis of motion (HAM) changes due to one- and two-level Maverick total disc replacement (TDR) adjacent to a long spinal fusion.
Methods
Seven spine specimens (T8–S1) were used in this study (66 ± 19 years old, 3F/4 M). A continuous pure moment of ±5.0 Nm was applied to the specimen in flexion–extension (FE), lateral bending (LB) and axial rotation (AR), with a compressive follower preload of 400 N. The 5.0 Nm data were analyzed to evaluate the operated segment biomechanics at the level of the disc replacements. The data were also analyzed at lower moments using a modified version of Panjabi’s proposed “hybrid” method to evaluate adjacent segment kinematics (intervertebral motion at the segments adjacent to the fusion) under identical overall (T8–S1) specimen rotations. The motion of each vertebra was monitored with an optoelectronic camera system. The biomechanical test was completed for (1) the intact condition and repeated after each surgical technique was applied to the specimen, (2) capsulotomy at L4–L5 and L5–S1, (3) T8–L4 fusion and capsulotomy at L4–L5 and L5–S1, (4) Maverick at L4–L5, and (5) Maverick at L5–S1. The capsulotomy was performed to allow measurement of facet joint loads in a companion study. Paired t tests were used to determine if differences in the kinematic parameters measured were significant. Holm–Sidak corrections for multiple comparisons were applied where appropriate.
Results
Under the 5.0 Nm loads, L4–L5 ROMs tended to decrease in all directions following L4–L5 Maverick replacement (mean = 22 %, compared to the fused condition). Two-level Maverick implantation also tended to reduce L4–S1 ROM (mean 18, 7 and 31 % in FE, LB and AR, respectively, compared to the fused condition without TDR). Following TDR replacement, the HAM location tended to shift posteriorly in FE (at L5–S1), anteriorly in AR, and inferiorly in LB. However, although the above-mentioned trends were observed, neither one- nor two-level TDR replacement showed statistically significant ROM or HAM change in any of the three directions. At the identical T8–S1 posture identified by the modified hybrid analysis, the L4–L5 and L5–S1 levels underwent significant larger motions, relative to the overall specimen rotation, after fusion. In the hybrid analysis, there were no significant differences between the ROM after fusion with intact natural discs at L4–L5 and L5–S1 and the motions at those levels with one or two TDRs implanted.
Conclusions
The present results demonstrated that one or two Maverick discs implanted subjacent to a long thoracolumbar fusion preserved considerable and intact-like ranges of motion and maintained motion patterns similar to the intact specimen, in this ex vivo study with applied pure moments and compressive follower preload. The hybrid analysis demonstrated that, after fusion, the TDR-implanted levels are required to undergo large rotations, relative to those necessary before fusion, in order to achieve the same motion between T8 and S1. Additional clinical and biomechanical research is necessary to determine if such a kinematic demand would be made on these levels clinically and the biomechanical performance of these implants if it were.
Keywords: Biomechanics, Total disc replacement, Adjacent level effects, Scoliosis, Instrumentation
Introduction
Degeneration of intervertebral discs adjacent to long fusion constructs occurs frequently in the thoracolumbar spine [3, 6–8, 16, 21, 30, 35]. Long fusion constructs are defined as those joining three or more vertebral levels by surgical means. Clinical and biomechanical studies have identified two main potential adjacent segment degeneration etiologies: genetic- or age-related predisposition [22, 30, 33, 38], and the altered biomechanical environment of the adjacent discs due to fusion [9, 17, 30, 39]. The primary biomechanical characteristics that may be altered at the spinal levels adjacent to the fusion are range and quality (i.e. center of rotation and coupling behavior) of motion, and the related quantities of load-sharing between the various load bearing elements (vertebral body, facet joints, columns, ligaments, implants). Together these changes may subsequently cause degenerative tissue responses [11].
One method for evaluating the quality of spinal motion is the helical axis of motion (HAM) [20]. This is a three-dimensional analog to the two-dimensional center of rotation. It is a three dimensional axis of motion that can be used to describe the motion of any rigid body (such as a vertebra) in space. It is defined as the axis about which the body rotates while the body simultaneously translates along the same axis. The HAM has been used previously to describe natural, injured and surgically treated cadaveric spine motions [19, 24, 37, 44]. The HAM incorporates and quantifies many characteristics of the quality of motion such as the center of rotation, translation of the vertebra during the motion and the coupling of the two bodies. To compare the spinal motion provided by a TDR with the “gold standard” motion, which would be the intact motion of a healthy spinal joint, both the ROM and the HAM can be calculated. If the intact and TDR ROM are the same then the quantity of motion is the same. If the intact and TDR HAM of the joint are the same then the quality of the motion can be said to be replicated. The HAM has previously been used in this fashion in this laboratory to evaluate the quality of motion provided by dynamic posterior instrumentation implants [24] and a facet joint arthroplasty device [44].
The most common clinical treatment for adjacent segment disease that limits mobility or causes pain is subsequent additional fusion of the adjacent degenerated spinal levels. One potential surgical alternative to fusion of the degenerated segments is implantation of a total disc replacement (TDR), such as the Maverick artificial disc (Maverick TDR, Medtronic Inc., Memphis, TN, USA), at these levels [2, 23]. The Maverick disc is used primarily in Europe and it is also in use in several other countries such as Australia, New Zealand, Canada, Korea, South Africa, India and Latin America. The Maverick implantation allows resection of osteophytes, and aims to restore natural disc height and preserve segmental motion [18]. Preservation of the range and quality of motion may lead to replication of the normal loading environment and thereby mitigate deleterious adaptive tissue responses. However, there is a concern that the disc prosthesis, especially by virtue of its proximity to the fusion which is an area of significant change in stiffness within the spine, might allow more motion or more motion may be required of it than would be the case for the natural disc. If this happened, there is a concern that the prosthesis could loosen or sublux in extreme positions. It is also important to consider the range of motion and quality of the motion at the TDR level, because different motion behavior could be a trigger for deleterious tissue responses.
In part to address this question there have been recent biomechanical studies studying adjacent level effects including kinematics and/or disc pressure with TDRs neighboring short [10, 14, 25] and long [34] fusions in the lumbar spine. Stiffness or hybrid protocols, rather than flexibility protocols, must be used to study the effects of surgical interventions on the biomechanics of the adjacent (non-operated) spinal levels [28, 40]. With these methods, segmental kinematics are evaluated for the intact non-fusion, fusion, and TDR situations at an identical spinal posture [14, 26, 27, 29, 36, 40, 41]. However, some of the studies that have been performed to study TDR’s adjacent to fusions [10, 25, 34] did not apply hybrid testing methods [10, 34], or applied bending using an offset shear force that resulted in combined bending and shear loading [25]. The kinematics of isolated or multiple total disc replacements and isolated fusions have also been studied in the past [5, 12, 26, 27, 40]. However, to the authors’ knowledge, there are no biomechanical studies documenting the range of motion and quality of kinematics (i.e. HAM) of TDRs implanted adjacent to long fusion.
Both in vivo [1] and ex vivo (hybrid or stiffness) biomechanical [5, 26, 27, 29, 36, 40, 41] studies have shown that fusion results in a redistribution of motion (i.e. increased motion) to the adjacent segments. It has also been shown in clinical and biomechanical studies that the increased motion that occurs at adjacent levels in response to fusion occurs at multiple adjacent levels [1, 5]. Although surgical decision making must consider a range of clinical factors, these studies would suggest that it may be necessary to implant TDR at multiple levels to treat multiple level disc degeneration. There is, thus, a clinical need to evaluate if one or multiple TDR devices can be used to maintain the range of motion at segments adjacent to long spinal fusions while preserving an intact-like quality of motion.
The objective was thus to evaluate the range of motion and HAM changes at the operated level due to one- and two-level Maverick total disc replacements adjacent to a long spinal fusion using a three-dimensional flexibility protocol. A related objective was to use a modified hybrid stiffness protocol to evaluate the kinematic effects of implanting TDR at the adjacent segments.
Materials and methods
Specimens
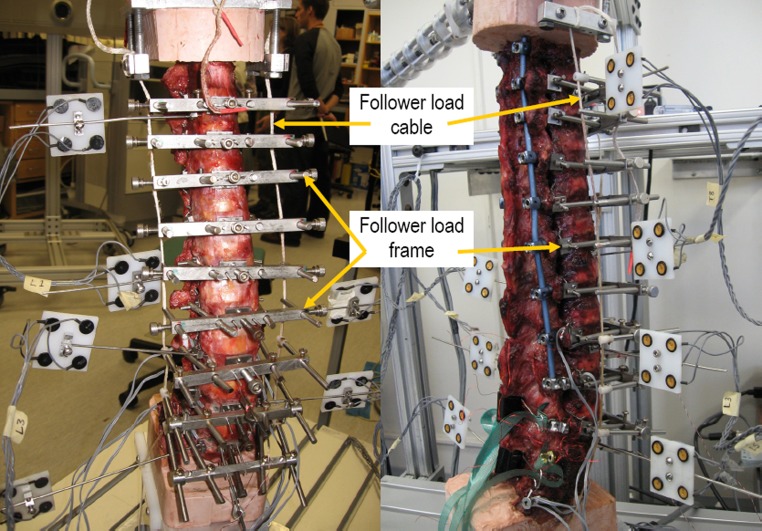
Seven fresh-frozen human cadaveric osteoligamentous thoracolumbar spine segments (T7–S1), mean age 66 (range 40–86 years, SD 19 years, 1 unknown age, 4 M/3F), were used. Due to a technical error, the modified hybrid calculations could not be performed for one of the female specimens, so the modified hybrid calculations are based on six specimens. Prior to preparation, the specimens were screened for age-inappropriate pathologies including excessive facet or disc degeneration. All specimens were fresh-frozen after harvesting and thawed at room temperature prior to preparation and testing for this protocol. The specimens were refrigerated when possible during the preparation and testing schedule. Specimens were hydrated by frequently spraying them with saline solution throughout preparation and testing. All specimens were prepared with standardized techniques. Musculature was carefully dissected while the vertebrae, intervertebral discs, joint capsules, and ligaments were left intact. Following dissection, the T7/8 and sacral vertebrae were potted in Tru-stone (Heraeus Kulzer, Armonk, NY, USA) such that the spine maintained its natural thoracic kyphosis and lumbo-sacral lordosis (Fig. 1). The T8/9 and L5/S1 intervertebral discs remained free.
Fig. 1.
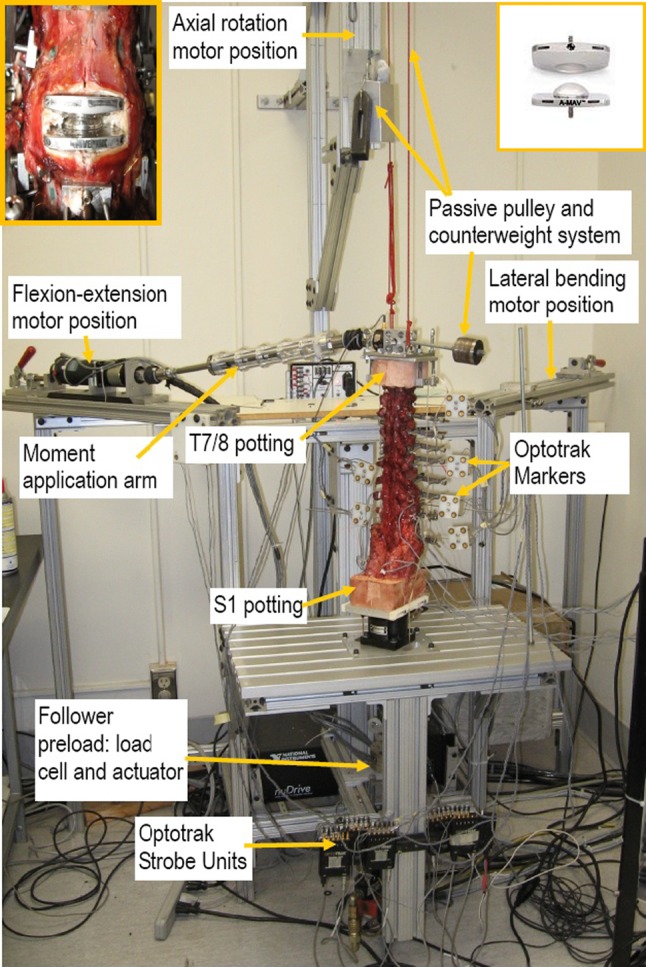
A T8–S1 spine specimen from the current study in the UBC Spine Motion Simulator. The specimen is shown in the flexion–extension configuration. The motor position is shifted to obtain the three spine motions (flexion–extension, lateral bending and axial rotation). An anterior view of the Maverick TDR implanted at level L4–L5 is shown inset at top left and a photograph of a Maverick prior to implantation is shown inset at right
Implants
All implants and associated surgical instrumentation were provided by Medtronic Sofamor Danek Inc. (Memphis, TN, USA). The sizes available for implantation are detailed in Table 1. Experienced fellowship-trained spine surgeons (Lenke and Itshayek) implanted the various spine implant constructs using standard clinical techniques that were modified where appropriate based on Dr. Lenke’s instructions. The technique required dissection of the anterior longitudinal ligament (Fig. 1) but preserved the posterior longitudinal ligament.
Table 1.
Implants provided by Medtronic Inc. for this study
| System | Implant type | Sizes available | Sizes generally used |
|---|---|---|---|
| Maverick TDR | Superior | 3° S 10 (×2), 6° S 12 (×2) | 3° S 10 |
| Inferior | 3° (×2), 6° (×2) | 3° | |
| CD Horizon posterior instrumentation | Pedicle screws and nuts | 4.0 × 30 6.5 × 30, 35, 40, 50, 55 7.5 × 50 |
6.5 × 30, 35, 40, 50 |
| Rod | 5.5 mm dia. | N/A |
Flexibility test protocol
Using the University of British Columbia (UBC) Spine Motion Simulator [13] (Fig. 1), a pure moment of ±5 Nm was applied to the superior-most free vertebra (T8) in flexion/extension (FE), lateral bending (LB), and axial rotation (AR), for each surgical condition. The simulator maintained the inferior vertebra (S1) in a fixed position while the rest of the specimen, including the splined moment application arm, was allowed to move unconstrained in three dimensions in response to the applied moment. The rate of moment application was approximately 0.5°/s in all directions until a load of 5.0 Nm was achieved at which point the load was reversed at the same rate. Three cycles of moment were applied; the first two served to precondition the specimen and the third load cycle was used for the kinematic analysis. Kinematics were measured using an Optotrak 3020 infrared motion analysis system that tracked active infrared light emitting diode markers (Northern Digital, Waterloo, ON, Canada). Four infrared markers were attached to polyethylene marker carriers which were in turn attached to Kirschner wires (sharpened stainless steel wires) inserted into the vertebral bodies of interest (Fig. 1). Markers were attached to vertebrae T8, L1, L2, L3, L4, L5 and S1. The vertebrae between T8 and L4 were stabilized by a posterior instrumentation system and were thus of little relevance to the main research questions. Therefore, no vertebrae in the thoracic spine were tracked other than the cranial most free vertebra (T8).
In total, five conditions were tested, with a 400 N follower preload for all tests:
Intact
Capsulotomy* of facet joints at L4–L5 and L5–S1
Capsulotomy* + posterior Fusion from T8 to L4
Capsulotomy* + Fusion + Maverick TDR at L4–L5
Capsulotomy* + Fusion + Maverick TDR at L4–S1
*Capsulotomy was performed to allow insertion of facet joint load sensors (data not presented here).
Follower load
The UBC follower load frame is a custom guide system that attaches to each vertebra without penetrating or causing defects to the bony anatomy or soft tissues. The rigid frame is wired to the pedicles posteriorly and it is tensioned and held in place using a screw that presses a smooth pad against the anterior aspect of the vertebral body. Using this, approach allows a very stable connection between the follower load frame and the vertebrae. The frame incorporates adjustable guides that align the follower load cables at each level (Fig. 2). After the specimen was placed on the UBC Spine Motion Simulator, the follower load frames were adjusted; so that the loading cable path followed the contour of the spinal column and was close to the expected centre of rotation of the vertebrae [32]. This ensured that the applied 400 N compressive force was nearly pure compression at each level, and hence caused minimal rotation of T8 or any other vertebrae as it was applied. This follower preload was found to function similarly for all test conditions and it was used for all testing conditions. Prior to each treatment condition test, the spine was preconditioned with three cycles of axial compression (0–320 N), via the follower load frame, to minimize viscoelastic effects. The 400 N compressive follower load was applied before the flexibility test moments were applied.
Fig. 2.
Anterior (left) and posterior-lateral (right) view of the follower load frame and the follower load cable attached to a specimen
Kinematic data analysis
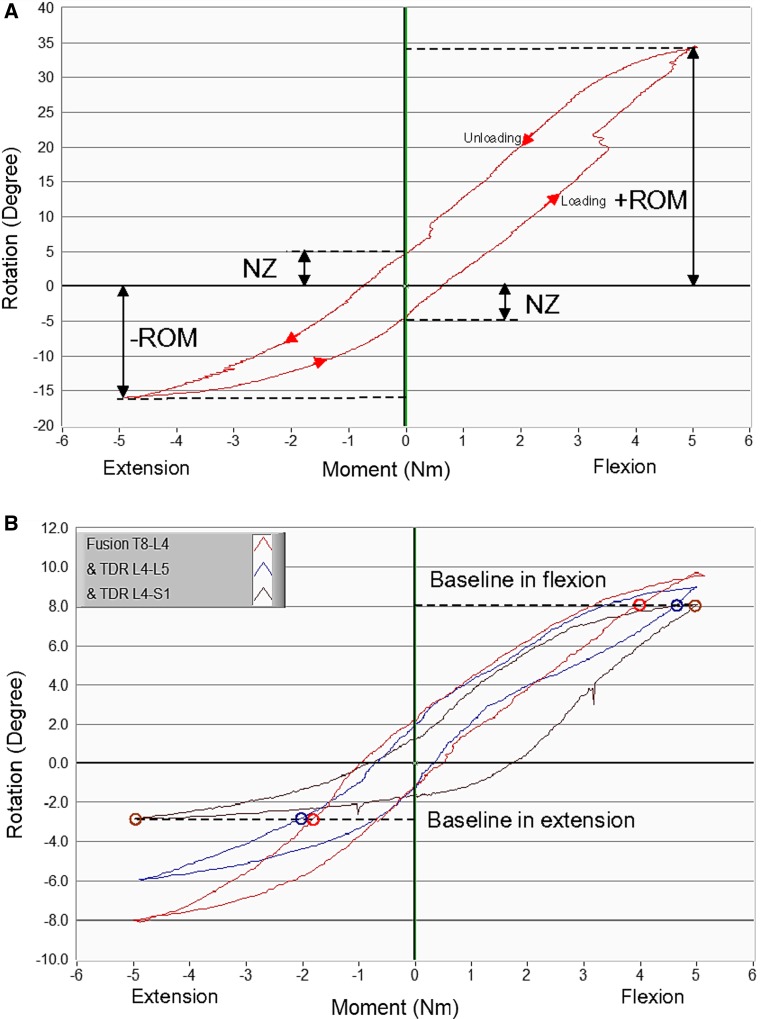
The intervertebral kinematics for each spinal level were determined via the three-dimensional Optotrak marker data. Each vertebra was assumed to be a rigid body and kinematics were calculated and analyzed using a custom Labview (6.1, National Instruments, Austin, TX, USA) program. The ROM was defined as the relative rotation between two vertebral bodies, in the direction of the applied moment, for a given moment (Fig. 3a). The rotation, at the maximum applied moment of 5 Nm shown in Fig. 3a, is the ROM associated with the flexibility analysis. The neutral zone (NZ) was defined, on a specimen by specimen basis, as the width of the hysteresis loop at zero moment from a full continuous loading cycle of rotation versus moment (Fig. 3a). Neutral zone is a widely reported spine kinematics parameter and it is an indicator of joint laxity.
Fig. 3.
a Schematic of the T8–S1 rotation versus applied moment from the continuous flexibility test indicating the definition of Range of Motion and Neutral Zone. Note that in this figure +ROM and −ROM corresponding to the range of motion at the maximum and minimum applied moments.b An example of the modified hybrid flexibility–stiffness protocol analysis demonstrated on the T8–S1 total motion graph for the various surgical conditions. Baselines in flexion and extension are determined by the least motion in all surgical conditions tested at those directions (most leftward and rightward circled data points). The baseline moments corresponding to the baseline motions are determined for each condition (other circled points) and the kinematic parameters are subsequently analyzed at these baseline moments. MAV Maverick
Modified hybrid protocol
Adjacent level effects were analyzed using a modified hybrid flexibility–stiffness protocol [40] which is a modified form of the hybrid protocol promoted by Panjabi and colleagues [12, 26–29]. This analysis technique is graphically illustrated for the flexion–extension response of a typical specimen in Fig. 3b. The baseline ROM was defined as the lowest overall T8–S1 ROM observed under the applied 5 Nm moment. The baseline moment was defined as the moment that was applied to produce the baseline motion and it was different for each surgical condition and specimen. Segmental motion (i.e. L5–S1 etc.) was determined from the overall 5 Nm flexibility test moment rotation curves but at the baseline moment (which was always less than the maximum 5 Nm moment) for each condition. Thus, segmental motions were compared among all conditions with the same overall motions, i.e. the baseline motion, but the applied moments were different. In the adjacent segment kinematics analysis, segmental or ROM data were presented as percentage of the total T8–S1 ROM for the specimen under consideration. This is a modified version of the percentage change proposed by Panjabi [28].
Helical axis of motion
The HAM was calculated for the rotational motion of segments L4/L5 and L5/S1, to allow comparison of the quality (i.e. because the HAM is an analogue for center of rotation and coupling) of the motion of these segments with the natural disc and with the TDRs [20]. For this analysis, a local coordinate system for each vertebra was defined to originate at the anterior, superior corner of the vertebral body and was aligned with the major anatomical axes: transverse, axial and sagittal. The location and orientation of the HAM were described by the intersection or orientation of the helical axis with the planes of the co-ordinate system described above. An unpublished HAM location accuracy study, determined that the location of the HAM would be within 2 mm of the true location for the relative rotations between two vertebrae of more than 1°.
Statistics
Paired t tests were used to determine if differences in the kinematic parameters measured were significant (p < 0.05). Holm–Sidak corrections for multiple comparisons were applied, with results grouped according to motion direction, where multiple comparisons were made. These statistical methods were used to make the following operated level comparisons and adjacent level comparisons:
Compare the ROM, NZ, HAM location and HAM orientation of the Maverick discs with those of the natural discs at L4–L5 (one TDR) and L4–S1 (two TDR). This was an operated level comparison made at the 5 Nm applied moment.
Compare the ROM, NZ, HAM location and HAM orientation of the intact spine with the capsulotomy at L4–L5 and L4–S1. This was an operated level comparison made at the 5 Nm applied moment.
Compare the modified hybrid moments for the fusion condition with those for the one TDR and two TDR conditions. This was an adjacent segment comparison made using the modified hybrid protocol moments.
Compare the modified hybrid ROM for the fusion condition with each of the Maverick at L4–L5 and Maverick at L4–S1 conditions. This was an adjacent segment analysis made at the modified hybrid protocol moments.
Results
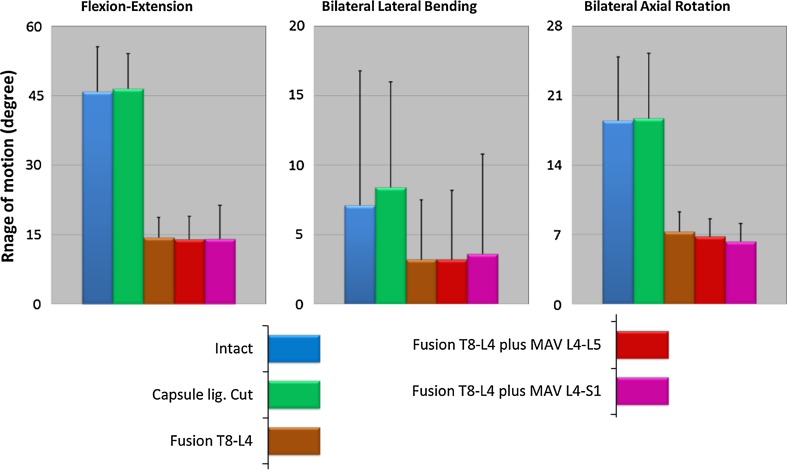
Overall the T8–S1 ROMs decreased considerably after the T8/L4 fusion in all three tested directions under the 5 Nm flexibility protocol (Fig. 4). Therefore, moments to drive the specimen to a certain ROM were greatest with the fusion or fusion plus one or two Maverick TDR and least for the conditions of intact and capsulotomy (Table 2). Specifically, comparing the moments necessary to achieve the baseline ROM for fusion with those for fusion and one TDR or fusion and two TDRs; the two TDR conditions tended to require less moment in lateral bending, but more in extension and axial rotation (Table 2). However, no statistically significant differences were observed for the moment when comparing the fusion and two-TDR conditions.
Fig. 4.
The overall ROM (T8–S1) of 5 testing conditions subjected to 5 Nm moments and 400 N preload compression. The values are mean ± SD. MAV Maverick
Table 2.
Modified hybrid moment data (these are the baseline moments from Fig. 3b) for flexion, extension, lateral bending and axial rotation
| Condition | Flexion | Extension | Lateral bending | Axial rotation |
|---|---|---|---|---|
| Capsulotomy | 1.8 (0.5) | 1.2 (0.3) | 3.4 (0.2) | 1.7 (0.4) |
| Fusion | 4.3 (0.4) | 3.4 (1.5) | 4.6 (0.5) | 4.4 (0.4) |
| Fusion + Maverick L4–L5 | 4.8 (0.3) | 3.1 (1.4) | 4.6 (0.4) | 4.5 (0.5) |
| Fusion + Maverick L4–S1 | 4.3 (0.6) | 4.4 (1.1) | 4.3 (0.4) | 5.0 (0.1) |
All values are Nm. Data are mean (SD)
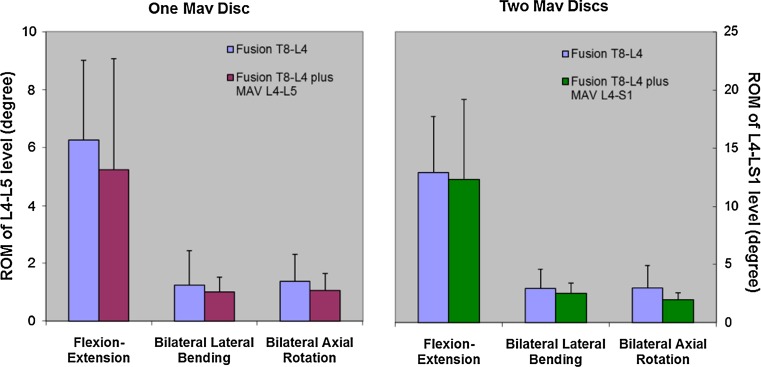
L4–L5 ROMs tended to decrease (on average by approximately 22 %) for all three tested directions following L4–L5 Maverick replacement. Two-level Maverick implantation also tended to reduce L4–S1 ROM (by 18 % in flexion–extension, 7 % in lateral bending and 31 % in axial rotation) compared to the fused condition (Fig. 5). NZs tended to increase after both one- and two-level Maverick implantation in flexion–extension, but tended to decrease in lateral bending and axial rotation (Fig. 6). Although these trends were present consistently, they corresponded to relatively minor differences in ROM and NZ and none of these trends were statistically significant in any of the three directions.
Fig. 5.
Average ROMs at 5.0 Nm applied moment before and after Maverick TDR implantation. Note that ROMs in the L4/L5 and L5/S1 levels are combined in the two-level TDR comparison. MAV Maverick
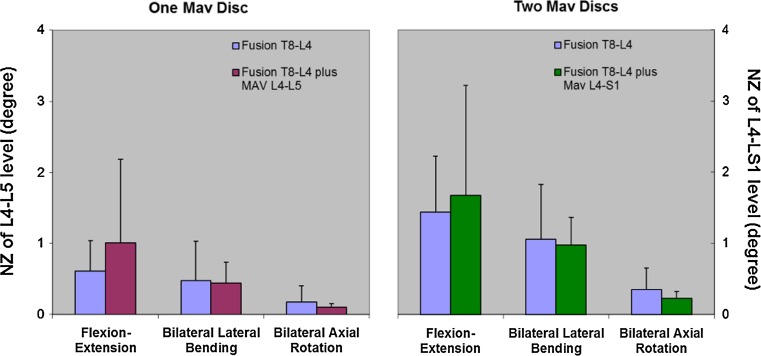
Fig. 6.
Average NZs at 5.0 Nm applied moment before and after Maverick implantation. Note that NZs in the L4/L5 and L5/S1 levels are combined in the two-level TDR comparison. MAV Maverick
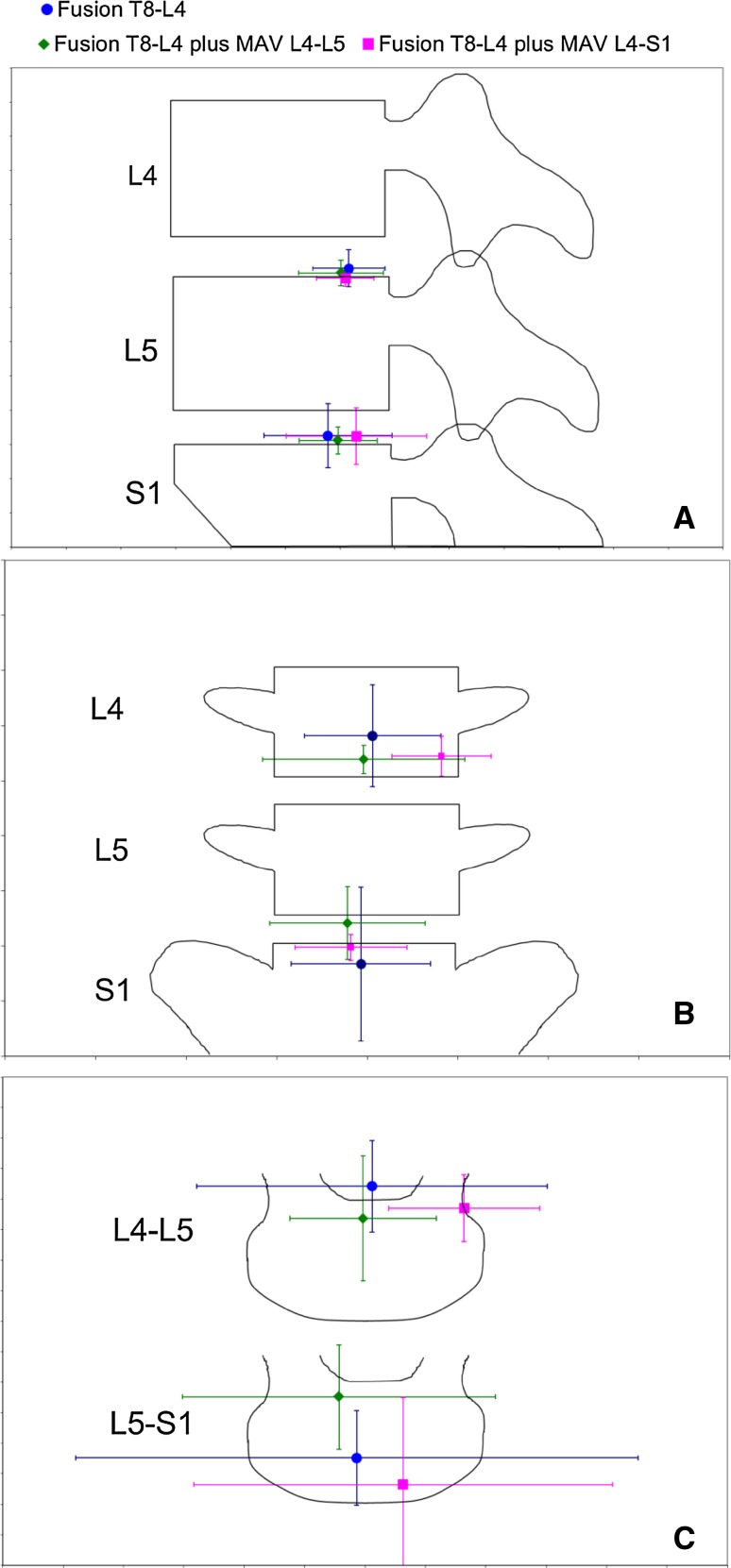
The HAM location at L4–L5 changed slightly and unpredictably in flexion–extension, tended to shift inferiorly in lateral bending, and shifted antero-laterally in axial rotation (Fig. 7). At L5–S1, the HAM location tended to shift posteriorly in flexion–extension, superiorly in lateral bending and antero-laterally in axial rotation following Maverick TDR. However, none of these trends were statistically significant. There were also no significant differences in HAM orientation due to TDR implantation at L4–L5 or L5–S1 (data not shown). The standard deviations for the HAM location were dramatically smaller for flexion–extension than for lateral bending and axial rotation.
Fig. 7.
a HAM location (mean ± SD) of flexion–extension motion in the sagittal plane. b HAM location of left–right lateral bending motion in the coronal plane. c HAM location of left–right axial rotation motion in the transverse plane (MAV Maverick). The HAM locations were calculated between the neutral position and the full 5 Nm flexibility moment
Compared to the intact condition, ROMs changed slightly and unpredictably following the bilateral capsule ligament section at L4/L5 and L5/S1 levels (not shown). NZs tended to increase slightly in all tested directions except lateral bending with two TDRs where NZ decreased slightly (not shown). No statistically significant differences were observed for the ROM or NZ when comparing the capsulotomy condition to the intact condition at the levels where capsulotomy was performed.
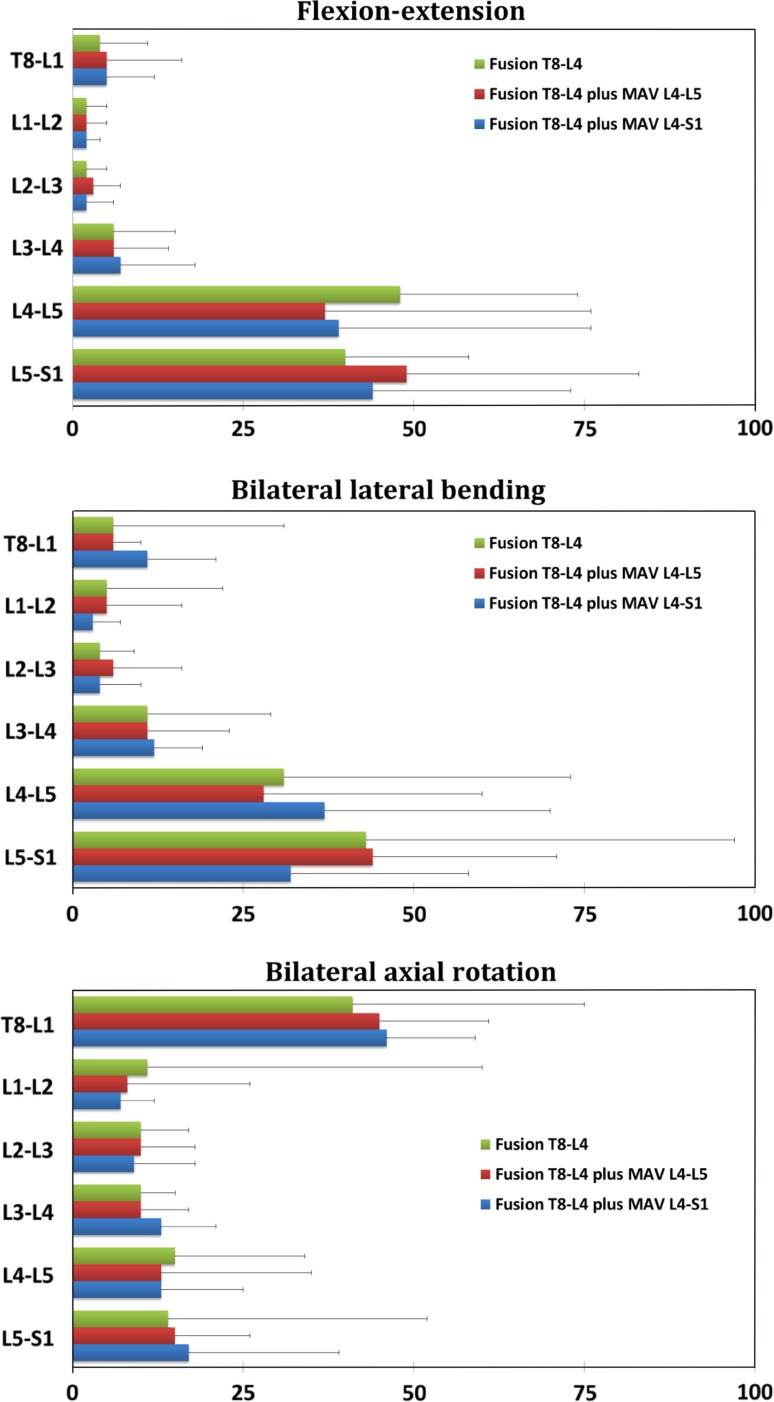
The ROM at each level in the lumbar spine and between T8 and S1 were normalized by the total T8–S1 ROM and they are presented at the modified hybrid protocol moments for capsulotomy, fusion and one- and two-level Maverick conditions in Fig. 8. The corresponding angular ROMs are presented in Table 3. In Fig. 8, the overall T8–S1 motion is the same for fusion Maverick L4–L5 and Maverick L4–S1 conditions. As expected, and as illustrated clearly in Fig. 4, the fusion dramatically decreased segmental motion within the fusion. It can be seen that the effect of the fusion, in all loading directions, was to redistribute the motion that was originally occurring throughout the thoracic and lumbar spine, so that it was primarily occurring at the L4–L5 and L5–S1 levels after fusion. This effect was similar whether the natural disc or the Maverick TDRs were present at the L4–L5 or L4–S1 segments. For all loading directions, similar motion was maintained at the L4–L5 and L5–S1 segments for the fusion (i.e. natural discs at L4–L5 and L5–S1), Maverick L4–L5 (i.e. TDR at L4–L5 only) and Maverick L4–S1 (i.e. TDR at L4–L5 and L5–S1). The fusion condition was statistically compared to Maverick L4–L5 and Maverick L4–S1 conditions at both L4–L5 and L4–S1 levels. There were no significant differences in ROM at the modified hybrid protocol moments between fusion (natural discs) and Maverick (one or two TDR discs) conditions at any level.
Fig. 8.
Modified hybrid analysis. The segmental ROMs are presented (at the baseline moments in Table 1) as a percentage of the total specimen (T8–S1) ROM for each surgical condition. The T8–S1 ROM is considerably lower after fusion. MAV Maverick
Table 3.
Segmental ROMs under the modified hybrid moments in Table 2
| Direction | Condition | L5–S1 | L4–L5 | L3–L4 | L2–L3 | L1–L2 | T8–L1 |
|---|---|---|---|---|---|---|---|
| Flexion–extension | Cap cut | 2.5 ± 1.8 | 0.9 ± 0.9 | 0.9 ± 1.1 | 1.3 ± 1.3 | 1.3 ± 0.9 | 3.8 ± 1.0 |
| Fusion | 4.2 ± 1.5 | 5.2 ± 2.7 | 0.6 ± 0.4 | 0.2 ± 0.2 | 0.3 ± 0.2 | 0.3 ± 0.2 | |
| Mav L4–L5 | 5.1 ± 2.3 | 4.3 ± 3.3 | 0.6 ± 0.3 | 0.3 ± 0.3 | 0.3 ± 0.2 | 0.5 ± 0.4 | |
| Mav L4–S1 | 5.0 ± 2.7 | 4.4 ± 3.0 | 0.8 ± 0.5 | 0.2 ± 0.2 | 0.2 ± 0.1 | 0.5 ± 0.3 | |
| Left–right lateral bending | Cap cut | 0.6 ± 0.4 | 0.5 ± 0.3 | 0.5 ± 0.4 | 0.3 ± 0.3 | 0.4 ± 0.2 | 0.6 ± 0.6 |
| Fusion | 1.4 ± 1.1 | 0.9 ± 0.7 | 0.4 ± 0.2 | 0.2 ± 0.0 | 0.2 ± 0.3 | 0.3 ± 0.4 | |
| Mav L4–L5 | 1.2 ± 0.6 | 0.7 ± 0.4 | 0.2 ± 0.2 | 0.2 ± 0.1 | 0.2 ± 0.2 | 0.2 ± 0.0 | |
| Mav L4–S1 | 0.8 ± 0.2 | 1.0 ± 0.6 | 0.4 ± 0.2 | 0.1 ± 0.0 | 0.0 ± 0.0 | 0.2 ± 0.2 | |
| Left–right axial rotation | Cap cut | 0.3 ± 0.2 | 0.5 ± 0.5 | 0.4 ± 0.2 | 0.4 ± 0.4 | 0.3 ± 0.2 | 4.8 ± 1.8 |
| Fusion | 1.3 ± 1.4 | 1.3 ± 1.0 | 0.7 ± 0.2 | 0.7 ± 0.3 | 1.2 ± 1.2 | 3.2 ± 1.5 | |
| Mav L4–L5 | 1.0 ± 0.4 | 1.0 ± 0.5 | 0.5 ± 0.2 | 0.7 ± 0.2 | 0.6 ± 0.4 | 3.0 ± 1.3 | |
| Mav L4–S1 | 1.0 ± 0.6 | 0.8 ± 0.4 | 0.8 ± 0.2 | 0.6 ± 0.3 | 0.5 ± 0.2 | 3.0 ± 1.1 |
All values are in degrees. Data are mean ± SD. Four conditions were cumulative to each specimen
Cap cut facet capsule cut bilaterally at L4–L5 and L5–S1, Fusion Medtronic posterior pedicle screw fixation between T8 and L4, Mav L4–L5 total disc replacement at L4–L5, Mav L4–S1 total disc replacement at L4–L5 and L5–S1
Discussion
A combined flexibility and modified hybrid protocol evaluation of the kinematic behavior of one- and two-level Maverick total disc replacements adjacent to a long spinal fusion was performed. This allowed the biomechanical simulation and investigation the performance of these implants adjacent to a fusion situation of considerable clinical interest [3, 6–8, 16, 21, 30, 35]. The study design differed from many TDR biomechanics studies. TDRs have generally been studied in their most common role as an alternative to fusion [5, 12, 26, 27, 29]. In that context, studies focus on the situation where the surgeon applies a TDR to maintain motion, disc space and load-sharing at a degenerated segment instead of fusing the degenerated segment. In these cases, the adjacent level effects that are discussed are the kinematic or load-sharing effects adjacent to the TDR. The present experiment focused on a situation where the fusion must be performed to correct scoliosis, and the TDRs were placed within the discs at the segments adjacent to the long fusion. The clinical rationale was as a pre-emptive solution to potential adjacent level degeneration, although this is done at the potential cost of excessive segmental motion adjacent to the long fusion (if the patient, post-scoliosis-surgery, attempted to use the same overall spine range of motion that they had pre-surgery). The analysis did not allow evaluation of the combined long fusion TDR constructs at these high motions; however, with the modified hybrid approach, it was established that the TDR levels would be responsible for providing the bulk of the flexion–extension and lateral bending motion after the fusion. To characterize this unusual and novel application for TDRs, the study was designed to evaluate the TDR kinematics in two very different biomechanical scenarios. The kinematics were characterized at both equal loads (flexibility protocol) and at equal T8–S1 postures (hybrid protocol). In all flexibility and hybrid load cases studied, the Maverick kinematic performance, in terms of ROM, NZ and HAM parameters, was comparable to the intact disc motion. Intact disc motion represented the “gold standard” kinematic behavior in these comparisons. This is appropriate since two design goals of TDRs are to prevent facet degeneration and to maintain enough motion to prevent adjacent segment degeneration at segments adjacent to the TDR [18] and healthy intact discs avoid these pathologies.
To the authors’ knowledge there have been no biomechanical studies published to date that characterize the kinematics of TDR adjacent to long scoliosis fusions in terms of both quantity (ROM) and quality (HAM). Kinematics (in terms of ROM only) have been studied for TDRs adjacent to short [10, 14, 25] and long [34] fusions in the lumbar spine. However, some of the studies that have been performed to study TDR’s adjacent to fusions [10, 25, 34] did not apply hybrid testing methods [10, 34], or applied bending using an offset shear [25] or compression [34] force that resulted in combined bending and shear loading. Two previous studies [5, 10] that have evaluated the Maverick TDR in flexibility protocols have reported small but statistically significant decreases in ROM after implantation of the Maverick disc. This finding is consistent with the non-significant but consistent trend of slightly decreasing ROM after Maverick implantation under the 5 Nm flexibility loads in the present study.
The modified hybrid stiffness results illustrated that the spinal motion, which was distributed throughout the spine before fusion, dramatically shifted to the mobile segments subjacent to the fusion after fusion. This was expected and consistent with the hybrid protocol results of many other investigators [5, 12, 14, 26, 28, 29]. However, this was the first hybrid protocol study, to the authors’ knowledge, where a TDR could be compared to a natural disc in a segment subjacent to a fusion. In the hybrid analysis, at a consistent T8–S1 posture and when comparing natural and TDR fusion conditions, the Maverick TDRs allowed similar motion to the intact discs. This is consistent with the ROM and NZ flexibility results which suggest that the implanted Maverick disc has similar bending resistance to the intact disc. This result may indicate that the extensive annulus tissue that is spared during Maverick implantation may help to maintain the biomechanics of the operated segment at that of the intact state.
HAM has previously been used to characterize the quality of the motion provided by motion-preserving spinal implants. In this laboratory HAM has been used to characterize the motion provided after implantation of dynamic instrumentation systems [24] and to characterize the motion in a total facet arthroplasty system [45]. Other investigators have experimentally characterized nucleus replacements with HAM [19]. HAM has also been used recently to characterize TDR designs with finite element methods [43]. The results of the present study showed no significant differences between the HAM with the Maverick and the intact discs. In the previous publications, the facet arthroplasty system has similarly reproduced intact-like kinematics [44], while dynamic instrumentation systems and nucleus replacements exhibited some differences in HAM compared to intact discs [19, 24]. Using FEA methods, three different TDRs designs (none the Maverick disc evaluated in the present study) were shown to exhibit different HAMs than the intact disc [43]. In the present study, there was considerably more variation in the HAM data for lateral bending and axial rotation and this is consistent with the much smaller ranges of motion present for those loading directions. Small ranges of motion decrease the stability of the mathematics used to calculate the HAM [15, 20, 42]. This may have negatively affected the ability to identify statistically significant differences in this study. The HAM location in the sagittal, transverse and coronal plane is analogous to the center of rotation for flexion–extension, axial rotation and lateral bending, respectively. The good concordance in HAM location in flexion–extension is especially noteworthy since this is the loading direction that allows the greatest ROM, this is the loading direction for which the follower preload is optimized [4, 31, 32] and flexion–extension is likely the most common physiologic activity that people undergo on a daily basis.
The capsulotomy at the L4–L5 and L5–S1 facet joints was necessary to utilize Tekscan sensors to characterise facet joint loading. The resulting facet joint and other tissue load results will be published in a future manuscript. Therefore, the intact condition could not be used as a baseline condition. Most comparisons made in the preceding objectives used the fused condition (with capsulotomy), as the baseline condition for motion of L4/L5 and L5/S1. As expected, the capsulotomy had negligible effects on the motion parameters of the spine; therefore, this condition is thought to provide an adequate representation of completely intact facet joints below a long fusion.
The strengths of this study are that it is the first study, of which the authors are aware, to evaluate the TDR kinematics adjacent to a long fusion. A three-dimensional flexibility protocol with superimposed axial follower load was applied to one of the longest ex vivo spine specimens that has been tested in this manner. The subsequent modified hybrid analysis allowed the evaluation of the TDR kinematics at a consistent global spine posture without applying higher moments than the flexibility tests as is required by the hybrid protocol [5, 14]. Due to inclusion of the relatively small mid-thoracic vertebrae such an increase in moment could have resulted in specimen damage. Both ROM and HAM were used to characterize both the quantity and quality of the TDR motion. HAM is an emerging tool to characterize motion quality and, to the authors’ knowledge, this is the first time that it has been used to characterize the motion of a TDR in an experimental protocol.
As with all biomechanical studies utilizing cadaveric specimens, there are several inherent limitations. First, the results from an ex vivo test are most relevant to the immediate post-surgical period in patients, and do not indicate behaviour that may be seen as a result of osseointegration or other physiological or systemic responses to the implant. In addition, the study is limited to six specimens (or seven in some aspects), and due to the natural variability of the human spine, large variation in results was observed. Such variation can potentially mask differences between test conditions. Only certain screw (CD Horizon) and disc (Maverick) sizes were available at the time of testing, meaning that the sizes selected may not have precisely suited each specimen. With a slightly superiorly placed TDR, the relative motion between the disc bearing surfaces appeared to be restricted. With the modified hybrid protocol, it was not possible to evaluate the TDR devices under the relatively higher rotations that may have occurred under the standard hybrid protocol proposed by Panjabi [28]. However, to the authors’ knowledge, there are no clinical studies that definitively show that patients attempt to recreate their pre-surgery total spine ROM after surgery [28] and it may thus be inappropriate to force the surgically treated cadaver specimen through such large motions. Also, if the spine had been constrained to undergo the large pre-surgery rotations, after fusion of the large T8–L4 segment, the ligaments, annulus or mobile joints may have been damaged. The relatively smaller rotations may have had a deleterious effect on the variation in the HAM calculations, since HAM parameters become ill defined at small angles [20]. Finally, the pure moment and follower preload loading used is a simplification of in vivo spinal loading, but is in accordance with accepted contemporary methods for testing of spinal implants [12, 19, 24, 26–29, 40, 44].
The present results demonstrated that one or two Maverick discs implanted subjacent to a long thoracolumbar fusion preserved considerable and intact-like ranges of motion (Figs. 5, 6, 8) and maintained motion patterns similar to the intact specimen (Fig. 7). The Maverick-treated levels maintained between 25 and 50 % (of the total T8–S1 motion before fusion) motion and this extent (or range) of motion is similar to the natural joint motion. It is well within one standard deviation, on average within 10 % of the natural joint motion and not statistically significantly different from natural joint motion. The quality of the motion is also similar as demonstrated by the HAM positions in Fig. 7. The hybrid analysis demonstrated that after fusion, the TDR-implanted levels are required to undergo large rotations relative to those necessary before fusion, in order to achieve the same motion between T8 and S1. The Maverick-implanted levels exhibited similar ROM after fusion as the intact discs. The concern that larger ROM would be allowed by the TDR design at this location in the spine appears unfounded for the Maverick discs. One important clinical implication of this work is that Maverick implantation into degenerated natural discs subjacent to a long fusion would be expected to restore segmental ROM and motion patterns back to those of the intact disc. In this case, TDR implantation could preserve the mobility at the spine and thereby prevent deleterious effects that pathological spinal biomechanics can have on other joints and tissues of the body. Additional clinical and biomechanical research is necessary to determine if such a kinematic demand would be made on these levels clinically and the biomechanical performance of these implants if it were.
Acknowledgments
The authors thank Medtronic Inc., Memphis, TN, USA for funding this study.
Conflict of interest
None.
Contributor Information
Qingan Zhu, Phone: +1-604-6758845, FAX: +1-604-8222403, Email: qinganzhu@gmail.com.
Claire F. Jones, Phone: +1-604-6758845, FAX: +1-604-8222403
Timothy Schwab, Phone: +1-604-6758845, FAX: +1-604-8222403.
Chadwick R. Larson, Phone: +1-604-6758845, FAX: +1-604-8222403
Peter A. Cripton, Phone: +1-604-6758835, FAX: +1-604-8222403, Email: cripton@mech.ubc.ca
References
- 1.Auerbach JD, Jones KJ, Milby AH, Anakwenze OA, Balderston RA. Segmental contribution toward total lumbar range of motion in disc replacement and fusions: a comparison of operative and adjacent levels. Spine (Phila Pa 1976) 2009;34:2510–2517. doi: 10.1097/BRS.0b013e3181af2622. [DOI] [PubMed] [Google Scholar]
- 2.Bertagnoli R, Yue JJ, Fenk-Mayer A, Eerulkar J, Emerson JW. Treatment of symptomatic adjacent-segment degeneration after lumbar fusion with total disc arthroplasty by using the prodisc prosthesis: a prospective study with 2-year minimum follow up. J Neurosurg Spine. 2006;4:91–97. doi: 10.3171/spi.2006.4.2.91. [DOI] [PubMed] [Google Scholar]
- 3.Cho KJ, Suk SI, Park SR, Kim JH, Choi SW, Yoon YH, Won MH. Arthrodesis to L5 versus S1 in long instrumentation and fusion for degenerative lumbar scoliosis. Eur Spine J. 2009;18:531–537. doi: 10.1007/s00586-009-0883-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cripton PA, Bruehlmann SB, Orr TE, Oxland TR, Nolte LP. In vitro axial preload application during spine flexibility testing: towards reduced apparatus-related artefacts. J Biomech. 2000;33:1559–1568. doi: 10.1016/S0021-9290(00)00145-7. [DOI] [PubMed] [Google Scholar]
- 5.Dmitriev AE, Gill NW, Kuklo TR, Rosner MK. Effect of multilevel lumbar disc arthroplasty on the operative- and adjacent-level kinematics and intradiscal pressures: an in vitro human cadaveric assessment. Spine J. 2008;8:918–925. doi: 10.1016/j.spinee.2007.10.034. [DOI] [PubMed] [Google Scholar]
- 6.Eck KR, Bridwell KH, Ungacta FF, Riew KD, Lapp MA, Lenke LG, Baldus C, Blanke K (2001) Complications and results of long adult deformity fusions down to l4, l5, and the sacrum. Spine (Phila Pa 1976) 26:E182–192 [DOI] [PubMed]
- 7.Edwards CC, II, Bridwell KH, Patel A, Rinella AS, Berra A, Lenke LG. Long adult deformity fusions to L5 and the sacrum. A matched cohort analysis. Spine. 2004;29:1996–2005. doi: 10.1097/01.brs.0000138272.54896.33. [DOI] [PubMed] [Google Scholar]
- 8.Edwards CC, 2nd, Bridwell KH, Patel A, Rinella AS, Jung Kim Y, Berra AB, Della Rocca GJ, Lenke LG. Thoracolumbar deformity arthrodesis to L5 in adults: the fate of the L5–S1 disc. Spine (Phila Pa 1976) 2003 doi: 10.1097/01.BRS.0000084266.37210.85. [DOI] [PubMed] [Google Scholar]
- 9.Ekman P, Moller H, Shalabi A, Yu YX, Hedlund R. A prospective randomised study on the long-term effect of lumbar fusion on adjacent disc degeneration. Eur Spine J. 2009;18:1175–1186. doi: 10.1007/s00586-009-0947-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Erkan S, Rivera Y, Wu C, Mehbod AA, Transfeldt EE. Biomechanical comparison of two-level Maverick disc replacement and a hybrid one-level disc replacement and one-level anterior lumbar interbody fusion. Spine J. 2009 doi: 10.1016/j.spinee.2009.04.014. [DOI] [PubMed] [Google Scholar]
- 11.Gillet P. The fate of the adjacent motion segments after lumbar fusion. J Spinal Disord Tech. 2003;16:338–345. doi: 10.1097/00024720-200308000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Goel VK, Grauer JN, Patel T, Biyani A, Sairyo K, Vishnubhotla S, Matyas A, Cowgill I, Shaw M, Long R, Dick D, Panjabi MM, Serhan H. Effects of charite artificial disc on the implanted and adjacent spinal segments mechanics using a hybrid testing protocol. Spine. 2005;30:2755–2764. doi: 10.1097/01.brs.0000195897.17277.67. [DOI] [PubMed] [Google Scholar]
- 13.Goertzen DJ, Lane C, Oxland TR. Neutral zone and range of motion in the spine are greater with stepwise loading than with a continuous loading protocol. An in vitro porcine investigation. J Biomech. 2004;37:257–261. doi: 10.1016/S0021-9290(03)00307-5. [DOI] [PubMed] [Google Scholar]
- 14.Grauer JN, Biyani A, Faizan A, Kiapour A, Sairyo K, Ivanov A, Ebraheim NA, Patel T, Goel VK. Biomechanics of two-level Charite artificial disc placement in comparison to fusion plus single-level disc placement combination. Spine J. 2006;6:659–666. doi: 10.1016/j.spinee.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 15.Haberl H, Cripton PA, Orr TE, Beutler T, Frei H, Lanksch WR, Nolte LP. Kinematic response of lumbar functional spinal units to axial torsion with and without superimposed compression and flexion/extension. Eur Spine J. 2004;13:560–566. doi: 10.1007/s00586-004-0720-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harding IJ, Charosky S, Vialle R, Chopin DH. Lumbar disc degeneration below a long arthrodesis (performed for scoliosis in adults) to L4 or L5. Eur Spine J. 2008;17:250–254. doi: 10.1007/s00586-007-0539-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hilibrand AS, Robbins M. Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J. 2004;4:190S–194S. doi: 10.1016/j.spinee.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 18.Huang RC, Wright TM, Panjabi MM, Lipman JD. Biomechanics of nonfusion implants. Orthop Clin North Am. 2005;36:271–280. doi: 10.1016/j.ocl.2005.02.010. [DOI] [PubMed] [Google Scholar]
- 19.Kettler A, Marin F, Sattelmayer G, Mohr M, Mannel H, Durselen L, Claes L, Wilke HJ. Finite helical axes of motion are a useful tool to describe the three-dimensional in vitro kinematics of the intact, injured and stabilised spine. Eur Spine J. 2004;13:553–559. doi: 10.1007/s00586-004-0710-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kinzel GL, Hall AS, Hillberry BM (1972) Measurement of the total motion between two body segments-I. Analytical development. J Biomech 5:93–105 [DOI] [PubMed]
- 21.Kuhns CA, Bridwell KH, Lenke LG, Amor C, Lehman RA, Buchowski JM, Edwards C, 2nd, Christine B. Thoracolumbar deformity arthrodesis stopping at L5: fate of the L5–S1 disc, minimum 5-year follow-up. Spine (Phila Pa 1976) 2007;32:2771–2776. doi: 10.1097/BRS.0b013e31815a7ece. [DOI] [PubMed] [Google Scholar]
- 22.Kumar A, Beastall J, Hughes J, Karadimas EJ, Nicol M, Smith F, Wardlaw D. Disc changes in the bridged and adjacent segments after Dynesys dynamic stabilization system after two years. Spine (Phila Pa 1976) 2008;33:2909–2914. doi: 10.1097/BRS.0b013e31818bdca7. [DOI] [PubMed] [Google Scholar]
- 23.Lehman RA, Jr, Lenke LG. Long-segment fusion of the thoracolumbar spine in conjunction with a motion-preserving artificial disc replacement: case report and review of the literature. Spine (Phila Pa 1976) 2007;32:E240–E245. doi: 10.1097/01.brs.0000259211.22036.2a. [DOI] [PubMed] [Google Scholar]
- 24.Niosi CA, Zhu QA, Wilson DC, Keynan O, Wilson DR, Oxland TR. Biomechanical characterization of the three-dimensional kinematic behaviour of the Dynesys dynamic stabilization system: an in vitro study. Eur Spine J. 2006;15:913–922. doi: 10.1007/s00586-005-0948-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nunley PD, Jawahar A, Mukherjee DP, Ogden A, Khan Z, Kerr EJ III, Cavanaugh DA (2008) Comparison of pressure effects on adjacent disk levels after 2-level lumbar constructs: fusion, hybrid, and total disk replacement. Surg Neurol 70:247–251 (discussion 251). doi:10.1016/j.surneu.2008.04.011 [DOI] [PubMed]
- 26.Panjabi M, Henderson G, Abjornson C, Yue J. Multidirectional testing of one- and two-level ProDisc-L versus simulated fusions. Spine (Phila Pa 1976) 2007;32:1311–1319. doi: 10.1097/BRS.0b013e318059af6f. [DOI] [PubMed] [Google Scholar]
- 27.Panjabi M, Malcolmson G, Teng E, Tominaga Y, Henderson G, Serhan H (2007) Hybrid testing of lumbar CHARITE discs versus fusions. Spine (Phila Pa 1976) 32:959–966 (discussion 967). doi:10.1097/01.brs.0000260792.13893.88 [DOI] [PubMed]
- 28.Panjabi MM (2007) Hybrid multidirectional test method to evaluate spinal adjacent-level effects. Clin Biomech (Bristol, Avon) 22:257–265. doi:10.1016/j.clinbiomech.2006.08.006 [DOI] [PubMed]
- 29.Panjabi MM, Henderson G, James Y, Timm JP. Stabilimax (NZ) versus simulated fusion: evaluation of adjacent-level effects. Eur Spine J. 2007;16:2159–2165. doi: 10.1007/s00586-007-0444-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE (2004) Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine (Phila Pa 1976) 29:1938–1944. pii:00007632-200409010-00019 [DOI] [PubMed]
- 31.Patwardhan AG, Havey RM, Carandang G, Simonds J, Voronov LI, Ghanayem AJ, Meade KP, Gavin TM, Paxinos O. Effect of compressive follower preload on the flexion–extension response of the human lumbar spine. J Orthop Res. 2003;21:540–546. doi: 10.1016/S0736-0266(02)00202-4. [DOI] [PubMed] [Google Scholar]
- 32.Patwardhan AG, Havey RM, Meade KP, Lee B, Dunlap B. A follower load increases the load-carrying capacity of the lumbar spine in compression. Spine. 1999;24:1003–1009. doi: 10.1097/00007632-199905150-00014. [DOI] [PubMed] [Google Scholar]
- 33.Penta M, Sandhu A, Fraser RD (1995) Magnetic resonance imaging assessment of disc degeneration 10 years after anterior lumbar interbody fusion. Spine (Phila Pa 1976) 20:743–747 [DOI] [PubMed]
- 34.Quirno M, Kamerlink JR, Valdevit A, Kang M, Yaszay B, Duncan N, Boachie-Adjei O, Lonner BS, Errico TJ. Biomechanical analysis of a disc prosthesis distal to a scoliosis model. Spine (Phila Pa 1976) 2009;34:1470–1475. doi: 10.1097/BRS.0b013e3181a8e418. [DOI] [PubMed] [Google Scholar]
- 35.Rinella A, Bridwell K, Kim Y, Rudzki J, Edwards C, Roh M, Lenke L, Berra A (2004) Late complications of adult idiopathic scoliosis primary fusions to L4 and above: the effect of age and distal fusion level. Spine (Phila Pa 1976) 29:318–325. pii:00007632-200402010-00015 [DOI] [PubMed]
- 36.Rohlmann A, Burra NK, Zander T, Bergmann G. Comparison of the effects of bilateral posterior dynamic and rigid fixation devices on the loads in the lumbar spine: a finite element analysis. Eur Spine J. 2007;16:1223–1231. doi: 10.1007/s00586-006-0292-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schmidt H, Heuer F, Wilke HJ. Interaction between finite helical axes and facet joint forces under combined loading. Spine (Phila Pa 1976) 2008;33:2741–2748. doi: 10.1097/BRS.0b013e31817c4319. [DOI] [PubMed] [Google Scholar]
- 38.Seitsalo S, Schlenzka D, Poussa M, Osterman K. Disc degeneration in young patients with isthmic spondylolisthesis treated operatively or conservatively: a long-term follow-up. Eur Spine J. 1997;6:393–397. doi: 10.1007/BF01834066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Seo M, Choi D. Adjacent segment disease after fusion for cervical spondylosis; myth or reality? Br J Neurosurg. 2008;22:195–199. doi: 10.1080/02688690701790605. [DOI] [PubMed] [Google Scholar]
- 40.Tan JS, Singh S, Zhu QA, Dvorak MF, Fisher CG, Oxland TR. The effect of cement augmentation and extension of posterior instrumentation on stabilization and adjacent level effects in the elderly spine. Spine (Phila Pa 1976) 2008;33:2728–2740. doi: 10.1097/BRS.0b013e318188b2e4. [DOI] [PubMed] [Google Scholar]
- 41.Weinhoffer SL, Guyer RD, Herbert M, Griffith SL (1995) Intradiscal pressure measurements above an instrumented fusion. A cadaveric study. Spine (Phila Pa 1976) 20:526–531 [DOI] [PubMed]
- 42.Woltring HJ, Huiskes R, Lange A, Veldpaus FE. Finite centroid and helical axis estimation from noisy landmark measurements in the study of human joint kinematics. J Biomech. 1985;18:379–389. doi: 10.1016/0021-9290(85)90293-3. [DOI] [PubMed] [Google Scholar]
- 43.Zander T, Rohlmann A, Bergmann G (2009) Influence of different artificial disc kinematics on spine biomechanics. Clin Biomech (Bristol, Avon) 24:135–142. doi:10.1016/j.clinbiomech.2008.11.008 [DOI] [PubMed]
- 44.Zhu Q, Larson CR, Sjovold SG, Rosler DM, Keynan O, Wilson DR, Cripton PA, Oxland TR. Biomechanical evaluation of the total facet arthroplasty system: 3-dimensional kinematics. Spine. 2007;32:55–62. doi: 10.1097/01.brs.0000250983.91339.9f. [DOI] [PubMed] [Google Scholar]
- 45.Zhu QA, Park YB, Sjovold SG, Niosi CA, Wilson DC, Cripton PA, Oxland TR. Can extra-articular strains be used to measure facet contact forces in the lumbar spine? An in vitro biomechanical study. Proc Inst Mech Eng H. 2008;222:171–184. doi: 10.1243/09544119JEIM290. [DOI] [PubMed] [Google Scholar]