Abstract
The purpose of this study was to evaluate the influence of different implant designs of total lumbar disc replacements on the segmental biomechanics of the lumbar spine. The unconstrained Charité, the semi-constrained Prodisc and a semi-constrained Prototype with more posterior centre of rotation than the Prodisc were tested in vitro using six human, lumbar spines L2–L5. The segmental lordosis was measured on plain radiographs and the range of motion (ROM) for all six degrees of freedom with a previously described spine tester. All prostheses were implanted at level L3–L4. Compared with the intact status all prostheses resulted in a significant increase of segmental lordosis (intact 5.1°; Charité 10.6°, p = 0.028; Prodisc 9.5°, p = 0.027; Prototype 8.9°, p = 0.028), significant increase of flexion/extension (intact 6.4°, Charité 11.3°, Prodisc 12.2°, Prototype 12.2°) and axial rotation (intact 1.3°, Charité 5.4°, Prodisc 3.9°, Prototype 4.2°). Lateral bending increased significantly only for the Charité (intact 7.7°; Charité 11.6°, p = 0.028; Prodisc 9.6°, Prototype 9.8°). The segmental lordosis after Prototype implantation was significantly lower compared with Charité (p = 0.024) and Prodisc (p = 0.044). No significant difference could be observed for segmental lordosis between Charité and Prodisc and for ROM between the two semi-constrained prosthesis Prodisc and Prototype. The axial rotation for the unconstrained Charité was significantly higher than for the semi-constrained prosthesis Prodisc and Prototype, flexion/extension and lateral bending did not differ. Summarizing, the unconstrained prosthesis design increased segmental lordosis and showed a tendency towards higher ROM for axial rotation/lateral bending and lower ROM for flexion/extension than a semi-constrained prosthesis. A more anterior centre of rotation in a semi-constrained prosthesis resulted in a higher increase of segmental lordosis after TDR than a semi-constrained prosthesis with more posterior centre of rotation. The location of the centre of rotation in a semi-constrained prosthesis did not alter the magnitude of ROM. Despite the different alterations of ROM and segmental lordosis due to implant design, these differences were negligible compared with the overall increase of ROM and segmental lordosis by the implantation of a TDR compared with the physiologic state.
Keywords: Lumbar disc replacement, Range of motion, Centre of rotation, Biomechanics
Introduction
In the past few years the number of total lumbar disc replacements (TDR) is rapidly growing. Two main concepts of TDR, unconstrained and semi-constrained, are in use. Although some TDRs are in use for several years and are clinically established, such as the Charité-Prosthesis with its unconstrained and the Prodisc-Prosthesis with its semi-constrained disc kinematic, little is known about the impact of different disc kinematics on biomechanical behaviour of the lumbar spinal unit. Also the variable centre of rotation in case of semi-constrained prosthesis is supposed to be of crucial importance for segmental biomechanics [2, 7]. Further insight into the biomechanical behaviour of TDR could help to assess clinical outcome better. For determination of segmental biomechanics of the spinal unit multiple parameters exist. Clinically mobility and alignment seem to be most relevant when analyzing spinal biomechanics, especially in case of TDR with its concept of motion preservation.
For a refined understanding of the biomechanical properties of TDR the purpose of this in vitro study was to compare the influence of different prostheses kinematic-concepts (semi-constrained vs. unconstrained and anterior vs. posterior centre of rotation in semi-constrained prosthesis) on mobility (range of motion and neutral zone) and alignment of the lumbar spine.
Materials and methods
Specimen preparation
Six fresh-frozen segmental lumbar spines L2–L5 (mean age 38.6 ± 14.9 years) were used for testing. To rule out intervertebral disc or osseous pathology, the specimen and anteroposterior/lateral plain radiographs were inspected. Exclusion criteria were joint space narrowing, anterior/posterior osteophytes and obvious sclerosis. All soft tissue was dissected, keeping the capsules, ligaments and supporting structures intact. For the fixation in the spine tester, the L2 and L5 vertebra were embedded in PMMA (Polymethylmethacrylate, Technovit 3040, Heraeus Kulzer, Wehrheim/Ts, Germany) in such a manner that the L3–L4 disc was in the horizontal plane. The specimens were frozen in triple sealed plastic bags at −20°C and thawed at 6°C before testing.
Testing protocol
Biomechanical testing of the specimen was performed in a spine tester at room temperature [27]. The cranial vertebra (L2) was mounted on a gimbal, which allowed rotation around all three coordinate axes and up-and-down movements in vertical direction. The entire system can move with a traveling gantry and a secondary slide allowing translation in the remaining two planes. The specimens were loaded with pure moments of ±7.5 Nm in all three principal motion planes with alternating sequences (flexion–extension ± My, right/left lateral bending ± Mx, left/right axial rotation ± Mz). No axial preload was applied. The moments were applied continuously with a constant rate of 1.0°/s, except for axial rotation (0.5°/s). The specimen moved unconstrained in the five uncontrolled degrees of freedom. During loading, the motion at the segment L3–L4 was recorded simultaneously with an ultrasound based motion analysis system (Zebris 50/4, Isny, Germany). The spinal testing was performed according to the recommendation for the standardized testing of spinal implants [28].
Description of implant and surgical technique
The Prodisc-L (Synthes, Oberdorf Switzerland), the Charité (DePuy Spine, Inc., Raynham, USA) and a Prototype (Prototype, Ulrich medical, Ulm, Germany) with ball-and socket principle were utilized for further testing (Fig. 1). To allow for comparable results with regard to prosthesis height and prosthesis angulation, prosthesis components were used which assured the lowest possible difference in prosthesis height and angulation between all three prostheses. In case of Charité 5°-angulated upper endplate, in case of Prodisc a 6°-angulated upper endplate and in case of Prototype a 6°-angulated upper endplate was used. The prosthesis height was adopted for each specimen individually. In case of Charité and Prodisc this is accomplished by varying the inlay-height and in case of Prototype by varying the lower endplate height.
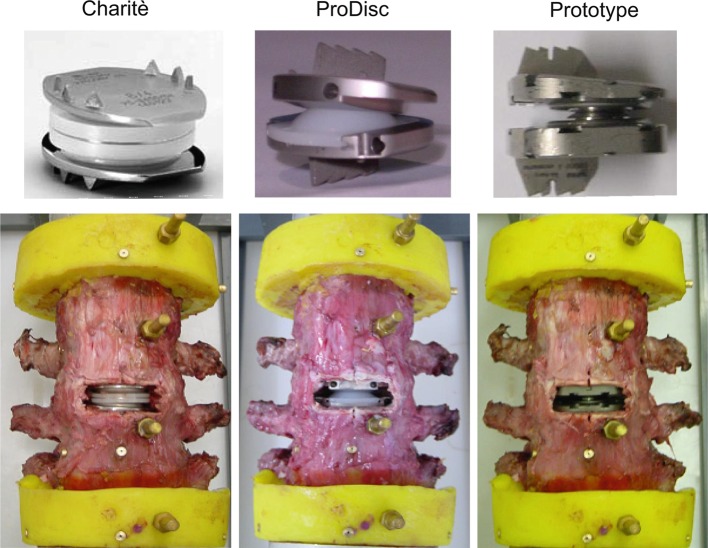
Fig. 1.
Charité, Prodisc-L and Prototype prosthesis types, and after implantation into segment L3–L4
One spine surgeon performed all implantations. For prosthesis implantation anterior anulus fibers were excised while preserving the lateral anulus fibers. Complete discectomy and curettage of the cartilaginous endplates was performed without violating the lateral anulus fibers. The intervertebral space was appropriately mobilized using a distractor. The implantation of the prostheses was carried out as recommended by the manufacturer with special implantation tools. The resection of the posterior anulus fibers and PLL was carried out transforaminally after implantation of the first prosthesis. Final anterior–posterior and lateral fluoroscopic views were taken to confirm correct position of the prostheses.
For all measurements, two precycles were applied to the specimens and the third cycle was used for data analysis to account for viscoelastic creep. All measurements were performed on the same day.
The following sequences were studied:
Intact
Implantation of the first TDR with a proper height and angulation and resection of posterior anulus fibers (PAF) and posterior longitudinal ligament (PLL)
Implantation of the second TDR with a proper height and angulation (PAF and PLL already resected)
Implantation of the third TDR with a proper height and angulation (PAF and PLL already resected)
The three different prostheses (Fig. 1) were tested in alternating sequences.
Measurement of disc height, segmental lordosis and lateral tilt
Before and after implantation the segmental lordosis (SL) and the disc height were measured on lateral fluoroscopic images and the lateral tilt (LT) on anterior-posterior fluoroscopic images (Fig. 2). Disc heights were expressed with the “Dabbs-Ratio” [6], which is (anterior disc height + posterior disc height)/2. For evaluation the radiographs were stored by a video camera-based image capture system (DiagnostiX, Basis 2048, GEMED, Germany) in digital format on a personal computer. All measurements were performed digitally, where the software allows the examiner to draw separate lines through the endplates of the vertebrae and measure distance between two landmarks. The software automatically displays the angle formed by these lines and the distances. For exact distance measurements, the magnification of the fluoroscopic images was adjusted by measuring the known diameter of metallic seeds in the vertebral bodies. The angles and distances were measured twice with at least 8 weeks of time delay between both measurements to allow for calculation of intra-observer measurement error.
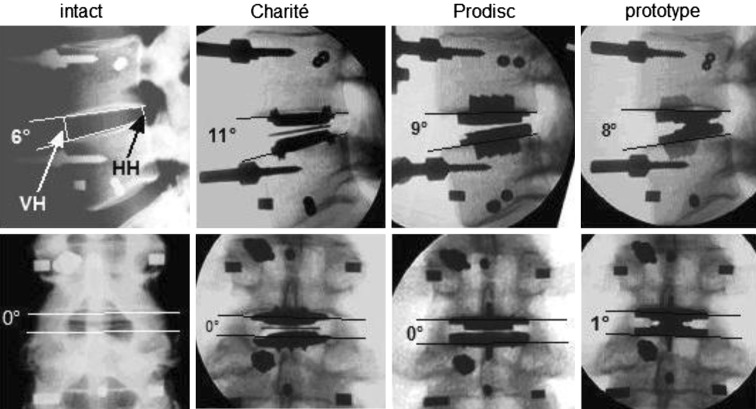
Fig. 2.
Measurement of disc height, segmental lordosis and lateral tilt: (upper line) measurement of segmental lordosis, anterior disc height (VH) and posterior disc height (HH) on lateral fluoroscopic images; (lower line) measurement of lateral tilt on anterior–posterior fluoroscopic images
Statistical analysis
Data were analysed using the SPSS 12.0 statistical software (SPSS Inc., Chicago, IL, USA). Wilcoxon matched-pairs signed rank test were performed to check for significant differences before and after implantation. The significance level was set at p < 0.05.
The measurement error was expressed with the 95% confidence interval as proposed by Bland et al. [1].
Results
The measurement errors for intra-observer reliability with regard to 95% CI was as follows: segmental lordosis ±0.8°; lateral tilt ±1.2°; disc height measurement ±0.9 mm.
No significant differences could be observed for the lateral tilt for all testing sequences (Table 1). A significant increase of segmental lordosis and disc height was observed for all implanted prosthesis compared with the intact specimen (Table 1). No significant differences could be observed with regard to disc height between the different prostheses, whereas the increase in segmental lordosis was significantly higher in the Charité (p = 0.046) and Prodisc (p = 0.042) compared with the Prototype (Table 1). The increase of segmental lordosis was not significantly different between the Charité and Prodisc.
Table 1.
Results for segmental lordosis, lateral tilt and disc height measurements for the different testing conditions
| Segmental lordosis in ° Mean (minimum–maximum) |
Lateral tilt in ° Mean (minimum–maximum) |
Disc height in mm Mean (minimum–maximum) |
|
|---|---|---|---|
| Intact | 5.1 (4.0–7.1) | 0.5 (0.2–1.1) | 9.6 (8.6–9.9) |
| Charité | 10.6* (7.3–12.1) | 0.3 (0.3–1.8) | 11.5* (10.4–11.7) |
| Prodisc-L | 9.5* (6.1–12.5) | 0.7 (0.2–2,4) | 10.6* (10.1–12.4) |
| Prototype | 8.9* (4.2–11.5) | 0.9 (0.4–2.5) | 11.1* (10.1–12.5) |
* Significant compared with intact (Wilcoxon matched-pairs signed rank test)
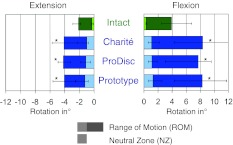
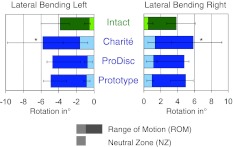
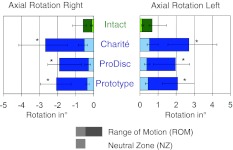
Only the Charité showed a significant increase of ROM and NZ in all motion planes compared with the intact specimen (Figs. 3, 4, 5). The implantation of the semi-constrained Prodisc and Prototype resulted in a significant increase only for flexion/extension and axial rotation, whereas lateral bending did not change significantly compared with the intact specimen. No significant differences could be observed with regard to flexion/extension and lateral bending (ROM and NZ) between the different prosthesis types. The increase in ROM and NZ for axial rotation was significantly higher for the Charité compared with the Prodisc (ROM p = 0.043; NZ p = 0.028), whereas only the increase in NZ for axial rotation was significant for the Charité when compared with the Prototype (p = 0.028). No significant differences in ROM and NZ for all motion planes could be observed between the semi-constrained Prodisc and the Prototype.
Fig. 3.
ROM and NZ in flexion and extension of the segments L3–L4 in the intact state and after implantation of the Charité, Prodisc and Prototype w/o PLL (n = 6). Asterisk ROM significant compared with intact (Wilcoxon matched-pairs signed rank test)
Fig. 4.
ROM and NZ in lateral bending right and left of the segments L3–L4 in the intact state and after implantation of the Charité, Prodisc and Prototype w/o PLL (n = 6). Asterisk ROM significant compared with intact (Wilcoxon matched-pairs signed rank test)
Fig. 5.
ROM and NZ in axial rotation left and right of the segments L3–L4 in the intact state and after implantation of the Charité, Prodisc and Prototype w/o PLL (n = 6). Asterisk ROM significant compared with intact (Wilcoxon matched-pairs signed rank test)
Discussion
One of the proposed fundamental theoretical advantages of TDR over fusion is the preservation of segmental mobility [10, 13]. Beside the preservation of mobility per se, the quantity of postoperative range of motion after TDR seems also to be of notable interest. Huang and co-workers [10] reported about a modest but statistically better outcome according to the ODQ (Oswestry Disability Questionnaire) and a modified Stauffer–Coventry score in patients with segmental mobility >5° on the one hand but already acknowledged that excessive motion after TDR might result in facet joint arthrosis/hypertrophy, stenosis and pain on the other hand. Another proposed advantage of lumbar disc replacement is the physiological realignment of the lumbar spine. With regard to the segmental and global lumbar spine alignment, hypo- and hyperlordosis seem to be more often associated with low back pain than physiological lumbar lordosis [15, 24]. Therefore, another goal of disc replacement is to restore or maintain a physiological alignment of the spine. Having these facts in mind and based on the perception that mobility and alignment of the spine after lumbar total lumbar disc replacement is of special importance for the outcome, it seems more than reasonable to evaluate the impact of implant kinematics on these parameters.
The resulting hypermobility, especially in case of flexion/extension and axial rotation, is most probably explained by the surgical approach, which sacrifices the anterior annulus fibers and anterior longitudinal ligament during implantation while preserving the lateral anulus fibers. This theoretical explanation is supported by the fact that studies on functional biomechanics of spinal ligaments stress the importance of the ALL in providing resistance to motion and stability to the spine [19, 20, 22].
The results for the Charité in the current study are in line with the findings of Lemaire et al. [17], as they also report about a significant increase of flexion/extension and axial rotation, but a non-significant increase for lateral bending after in vitro evaluation of the Charité. Similar results were observed in two other finite-element model studies for the Charité and Prodisc. Zander et al. [29] report about a reduction for flexion but an increase in extension, lateral bending and axial torsion in a validated finite-element model after simulation of prosthesis implantation at level L4–L5 for both prostheses. In a nonlinear three-dimensional finite-element model of L4–L5, Chung et al. [4] observed an increase of ROM in each direction of loading for the Prodisc and Charité. These observations are partially in contrast to the findings of Cunningham et al. [5] who report about a significant increase only for axial rotation (in average 44%) and a non-significant increase for flexion/extension (in average 3%) and lateral bending (in average 16%). The limiting factor for the comparison of the results might be the older age of the specimen (46–63 years) in their study group, which probably does not reflect the intact range of motion of a healthy segment. This theoretical consideration is supported by the fact that Fujiwara et al. [8] reported about an increase of ROM in human lumbar specimen with degeneration.
Assuming that the observed hypermobility is based on a “segmental ligamentous weakening”, a distraction of the remaining segmental ligamentous elements might result in a relief of this phenomenon, as proposed by Weisskopf et al. [26]. However, one should also keep in mind that the possible distraction of a disc space is limited for several reasons. Liu et al. [18] reported about a significant decrease of the facet joint articulation overlap in sagittal plane following an increase in the lumbar disc space and mentioned that an inappropriate distraction will result in facet joint subluxation. Another consideration prohibiting excessive segmental distraction during implantation of a TDR is ligamentous failure. Panjabi et al. [20] already demonstrated that ligaments have a characteristic nonlinear load–displacement behaviour, which implies a violation of these structures in the so-called plastic zone.
The results of the current study clearly demonstrate the biomechanical impact of anterior longitudinal ligament/anterior anulus fiber complex resection on segmental alignment after TDR implantation by means of an increase of segmental lordosis. Only a few in vivo studies already described an increase of segmental lordosis after implantation of TDR. An increase was observed after implantation of the Prodisc [2, 12], the Charité [9] and the semi-constrained Maverick-prosthesis, which has a more posterior and cranial centre of rotation, compared with the Prodisc [16]. But there is still no agreement if this increase can be considered as a segmental realignment to physiologic values, as proposed by Hopf et al. [9] or as an unphysiological increase towards hyperlordosis, as proposed by Cakir et al. [2]. With an in vivo test this pending question can hardly be answered, as X-rays of patients operated on for disc degeneration with prosthesis would (in most of the cases) not be available showing the not degenerated state of the lumbar spine. Therefore, a reliable reference value is usually missing in the clinical setting. In contrast, in this study, the specimen utilized showed no signs of gross degeneration and the values of the intact specimen can therefore be considered as individual physiological lordosis and taken as reference values. Based on these considerations an anterior implantation of total lumbar disc prosthesis, regardless of the type of prosthesis, results in an increase of segmental lordosis towards hyperlordosis. Possible consequences of this segmental hyperlordosis can be a compensatory loss of segmental lordosis at adjacent levels, as proposed by Cakir et al. [3] or an impingement of prosthesis endplates even in neutral position, as proposed by Rohlmann et al. [21]. The proposed impingement of prosthesis endplates by Rohlmann et al. [21], which is based on finite-element model analysis of the Prodisc, has been confirmed by the in vivo study of Käfer et al. [14] with a posterior endplate impingement in up to 11% of the patients operated on with a Prodisc. There is no doubt that alignment measurements in vitro have limited significance and the most relevant parameter responsible for the sagittal balance of the trunk (e.g. pelvic tilt, sacral slope) is not considered. Moreover, differences of segmental lordosis may also have other reasons, e.g. position, angle and height of the implant. Nevertheless, in vitro measurements may help to identify potential factors, which might have an effect on segmental alignment and has to be confirmed by clinical studies before final conclusion can be drawn with regard to their clinical relevance.
The second major observation of the current study is that alteration of ROM and segmental lordosis due to an artificial disc compared with the intact/physiological state exceeds by far the differences due to implant variability. Although a significant difference could be observed between the unconstrained Charité and the semi-constrained prostheses (Prodisc and Prototype) with regard to the segmental lordosis and between the Charité and Prodisc with regard to axial rotation, these differences are small when compared with the overall increase of segmental lordosis and axial rotation compared with intact status for all evaluated prostheses types.
Although there is no evidence available at the moment that an unconstrained prosthesis like the Charité has a greater amount of ROM compared with prosthesis with a semi-constrained design, Huang et al. [11] postulated that an unconstrained prosthesis might have a greater amount of flexion/extension ability. These considerations are neither supported by the results of a finite-element study [4] nor by the results of an in vivo study [25]. In a finite-element model of L4–L5 (with Prodisc and Charité) Chung et al. [4] reported about a larger range of motion in case of the Charité compared with the Prodisc, especially for lateral bending axial rotation, but not for flexion/extension. The observed values for the Prodisc, especially Charité, was 133% resp. 140% for flexion/extension, 137% resp. 170% for lateral bending and 138% resp. 200% for axial rotation, compared with the intact specimen. The results of an in vivo study of Tournier et al. [25] came to the same conclusion as no difference in flexion/extension ability could be observed for three different disc prostheses (Maverick, Charité and Prodisc). The results of the two aforementioned studies are in line with the results of the current study, as the only significant difference with regard to ROM could be observed for axial rotation between the Prodisc and Charité.
At the moment, the influence of the localization of the centre of rotation (anterior vs. posterior) on the resulting ROM has not been addressed in any in vitro or in vivo study. However, there are several finite-element studies, which have already addressed similar problems and which came to the conclusion that an anterior centre of rotation, in case of semi-constrained prosthesis, would result in a decrease of the flexion ability [7, 21, 23, 29]. The limited value of this study is based on the fact that only the flexion ability (and not flexion/extension) was analysed and that the difference between the centre of rotation (anterior vs. posterior) averaged 8 mm. In contrast, in the current study the difference of the centre of rotation between the Prodisc and Prototype was 4 mm. The results of the current study (no difference in ROM for all degrees of freedom between both semi-constrained prosthesis) are in line with the aforementioned results of Tournier et al. [25] which could not demonstrate a difference in flexion/extension ability for two different semi-constrained prostheses (Maverick and Prodisc).
Although there is some evidence in the literature that anterior implantation of total lumbar disc replacement, regardless of the type of prosthesis, results in an increase of segmental lordosis, which is supported by the current study, at the moment no study addressed the impact of different disc kinematics on segmental lordosis. Based on the results of the current study a possible impact of disc kinematics on resulting segmental lordosis can be assumed. The lowest increase of segmental lordosis was achieved with the Prototype, which has a more posterior centre of rotation, compared with the Prodisc. As no significant difference could be observed between the unconstrained Charité and semi-constrained Prodisc, the centre of rotation seems to have more impact on the resulting segmental lordosis than the disc kinematic. This observation is partially supported by the fact that the reported increases of segmental lordosis vary between different implant types. Hopf et al. [9] reported about an average increase of 10° after implantation of the Charité, whereas Cakir et al. [2] reported about an average increase of 8° after implantation of the Prodisc. In contrast, LeHuec et al. [16] noticed a marked lower increase of segmental lordosis (approximately 5°) after implantation of the Maverick, which has, like the Prototype, a posterior centre of rotation compared with the Prodisc. The results of this study are in line with the statement of Zander et al. [29], that the importance of implant kinematics is often overestimated and that the overall spinal kinematic alterations due to an artificial disc exceed by far the inter-implant differences. Although the difference in segmental lordosis between the Charité and Prototype and the Prodisc and Prototype was significant with regard to statistical analysis, it should be recognized that the error regarding this measurement in the current study was ±0.8°. Therefore, a final conclusion that a more posterior centre of rotation in case of a semi-constrained prosthesis results in a less increase of segmental lordosis cannot be drawn with certainty.
Summarizing, the implantation of a TDR leads to an increase of ROM and segmental lordosis compared with the intact/physiological state in this in vitro study. Although some of the increase can be attributed to different implant designs and kinematics of the TDR, the major part comes from the implantation technique and general kinematic behaviour of TDR. This study deepens our understanding of the biomechanical behaviour of different TDR’s. As some studies showed a possible effect of the alteration of ROM and segmental lordosis on clinical outcome, future in vitro and clinical studies should be performed to further clarify the interaction between biomechanical behaviour of TDR and clinical outcome, so that more specific recommendations for the use of TDR are possible.
Acknowledgments
The study was supported by Ulrich medical, Ulm, Germany. This work was approved by the Research Ethics Committee.
Conflict of interest
None.
References
- 1.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. doi: 10.1016/S0140-6736(86)90837-8. [DOI] [PubMed] [Google Scholar]
- 2.Cakir B, Richter M, Kafer W, Puhl W, Schmidt R. The impact of total lumbar disc replacement on segmental and total lumbar lordosis. Clin Biomech (Bristol, Avon) 2005;20:357–364. doi: 10.1016/j.clinbiomech.2004.11.019. [DOI] [PubMed] [Google Scholar]
- 3.Cakir B, Schmidt R, Huch K, Puhl W, Richter M. Sagittal alignment and segmental range of motion after total disc replacement of the lumbar spine. Z Orthop Ihre Grenzgeb. 2004;142:159–165. doi: 10.1055/s-2004-816275. [DOI] [PubMed] [Google Scholar]
- 4.Chung SK, Kim YE, Wang KC. Biomechanical effect of constraint in lumbar total disc replacement: a study with finite element analysis. Spine. 2009;34:1281–1286. doi: 10.1097/BRS.0b013e3181a4ec2d. [DOI] [PubMed] [Google Scholar]
- 5.Cunningham BW, Gordon JD, Dmitriev AE, Hu N, McAfee PC. Biomechanical evaluation of total disc replacement arthroplasty: an in vitro human cadaveric model. Spine. 2003;28:S110–S117. doi: 10.1097/01.BRS.0000092209.27573.90. [DOI] [PubMed] [Google Scholar]
- 6.Dabbs VM, Dabbs LG. Correlation between disc height narrowing and low-back pain. Spine. 1990;15:1366–1369. doi: 10.1097/00007632-199012000-00026. [DOI] [PubMed] [Google Scholar]
- 7.Dooris AP, Goel VK, Grosland NM, Gilbertson LG, Wilder DG. Load-sharing between anterior and posterior elements in a lumbar motion segment implanted with an artificial disc. Spine. 2001;26:E122–E129. doi: 10.1097/00007632-200103150-00004. [DOI] [PubMed] [Google Scholar]
- 8.Fujiwara A, Lim TH, An HS, Tanaka N, Jeon CH, Andersson GB, Haughton VM. The effect of disc degeneration and facet joint osteoarthritis on the segmental flexibility of the lumbar spine. Spine. 2000;25:3036–3044. doi: 10.1097/00007632-200012010-00011. [DOI] [PubMed] [Google Scholar]
- 9.Hopf C, Heeckt H, Beske C. Disc replacement with the SB Charite endoposthesis—experience, preliminary results and comments after 35 prospectively performed operations. Z Orthop Ihre Grenzgeb. 2002;140:485–491. doi: 10.1055/s-2002-34000. [DOI] [PubMed] [Google Scholar]
- 10.Huang RC, Girardi FP, Cammisa FP, Jr, Lim MR, Tropiano P, Marnay T. Correlation between range of motion and outcome after lumbar total disc replacement: 8.6-year follow-up. Spine. 2005;30:1407–1411. doi: 10.1097/01.brs.0000166528.67425.0e. [DOI] [PubMed] [Google Scholar]
- 11.Huang RC, Girardi FP, Cammisa FP, Jr, Wright TM. The implications of constraint in lumbar total disc replacement. J Spinal Disord Tech. 2003;16:412–417. doi: 10.1097/00024720-200308000-00014. [DOI] [PubMed] [Google Scholar]
- 12.Huang RC, Girardi FP, Cammisa FP, Jr, Tropiano P, Marnay T. Long-term flexion–extension range of motion of the prodisc total disc replacement. J Spinal Disord Tech. 2003;16:435–440. doi: 10.1097/00024720-200310000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Huang RC, Tropiano P, Marnay T, Girardi FP, Lim MR, Cammisa FP., Jr Range of motion and adjacent level degeneration after lumbar total disc replacement. Spine J. 2006;6:242–247. doi: 10.1016/j.spinee.2005.04.013. [DOI] [PubMed] [Google Scholar]
- 14.Kafer W, Clessienne CB, Daxle M, Kocak T, Reichel H, Cakir B. Posterior component impingement after lumbar total disc replacement: a radiographic analysis of 66 ProDisc-L prostheses in 56 patients. Spine. 2008;33:2444–2449. doi: 10.1097/BRS.0b013e318182c37b. [DOI] [PubMed] [Google Scholar]
- 15.La Grone MO. Loss of lumbar lordosis. A complication of spinal fusion for scoliosis. Orthop Clin North Am. 1988;19:383–393. [PubMed] [Google Scholar]
- 16.Le Huec J, Basso Y, Mathews H, Mehbod A, Aunoble S, Friesem T, Zdeblick T. The effect of single-level, total disc arthroplasty on sagittal balance parameters: a prospective study. Eur Spine J. 2005;14:480–486. doi: 10.1007/s00586-004-0843-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lemaire JP, Skalli W, Lavaste F, Templier A, Mendes F, Diop A, Sauty V, Laloux E. Intervertebral disc prosthesis. Results and prospects for the year 2000. Clin Orthop Relat Res. 1997;337:64–76. doi: 10.1097/00003086-199704000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Liu J, Ebraheim NA, Haman SP, Shafiq Q, Karkare N, Biyani A, Goel VK, Woldenberg L. Effect of the increase in the height of lumbar disc space on facet joint articulation area in sagittal plane. Spine. 2006;31:E198–E202. doi: 10.1097/01.brs.0000206387.67098.a0. [DOI] [PubMed] [Google Scholar]
- 19.Myklebust JB, Pintar F, Yoganandan N, Cusick JF, Maiman D, Myers TJ, Sances A., Jr Tensile strength of spinal ligaments. Spine. 1988;13:526–531. doi: 10.1097/00007632-198805000-00016. [DOI] [PubMed] [Google Scholar]
- 20.Panjabi MM, Goel VK, Takata K. Physiologic strains in the lumbar spinal ligaments. An in vitro biomechanical study 1981 Volvo Award in biomechanics. Spine. 1982;7:192–203. doi: 10.1097/00007632-198205000-00003. [DOI] [PubMed] [Google Scholar]
- 21.Rohlmann A, Zander T, Bergmann G. Effect of total disc replacement with ProDisc on intersegmental rotation of the lumbar spine. Spine. 2005;30:738–743. doi: 10.1097/01.brs.0000157413.72276.c4. [DOI] [PubMed] [Google Scholar]
- 22.Schendel MJ, Wood KB, Buttermann GR, Lewis JL, Ogilvie JW. Experimental measurement of ligament force, facet force, and segment motion in the human lumbar spine. J Biomech. 1993;26:427–438. doi: 10.1016/0021-9290(93)90006-Z. [DOI] [PubMed] [Google Scholar]
- 23.Schmidt H, Midderhoff S, Adkins K, Wilke HJ. The effect of different design concepts in lumbar total disc arthroplasty on the range of motion, facet joint forces and instantaneous center of rotation of a L4–5 segment. Eur Spine J. 2009;18:1695–1705. doi: 10.1007/s00586-009-1146-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shufflebarger HL, Clark CE. Thoracolumbar osteotomy for postsurgical sagittal imbalance. Spine. 1992;17:S287–S290. doi: 10.1097/00007632-199208001-00013. [DOI] [PubMed] [Google Scholar]
- 25.Tournier C, Aunoble S, Le Huec JC, Lemaire JP, Tropiano P, Lafage V, Skalli W. Total disc arthroplasty: consequences for sagittal balance and lumbar spine movement. Eur Spine J. 2007;16:411–421. doi: 10.1007/s00586-006-0208-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Weisskopf M, Ohnsorge JA, Martini F, Niethard FU, Birnbaum K. Influence of inlay height on motion characteristics of lumbar segments in total disc replacement. Z Orthop Unfall. 2008;146:452–457. doi: 10.1055/s-2008-1038400. [DOI] [PubMed] [Google Scholar]
- 27.Wilke HJ, Claes L, Schmitt H, Wolf S. A universal spine tester for in vitro experiments with muscle force simulation. Eur Spine J. 1994;3:91–97. doi: 10.1007/BF02221446. [DOI] [PubMed] [Google Scholar]
- 28.Wilke HJ, Wenger K, Claes L. Testing criteria for spinal implants: recommendations for the standardization of in vitro stability testing of spinal implants. Eur Spine J. 1998;7:148–154. doi: 10.1007/s005860050045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zander T, Rohlmann A, Bergmann G. Influence of different artificial disc kinematics on spine biomechanics. Clin Biomech (Bristol, Avon) 2009;24:135–142. doi: 10.1016/j.clinbiomech.2008.11.008. [DOI] [PubMed] [Google Scholar]