Abstract
Objective
The purpose of this prospective study was to evaluate the efficacy and safety of screw fixation without bone fusion for unstable thoracolumbar and lumbar burst fracture.
Methods
Nine patients younger than 40 years underwent screw fixation without bone fusion, following postural reduction using a soft roll at the involved vertebra, in cases of burst fracture. Their motor power was intact in spite of severe canal compromise. The surgical procedure included postural reduction for 3 days and screw fixations at one level above, one level below and at the fractured level itself. The patients underwent removal of implants 12 months after the initial operation, due to possibility of implant failure. Imaging and clinical findings, including canal encroachment, vertebral height, clinical outcome, and complications were analyzed.
Results
Prior to surgery, the mean pain score (visual analogue scale) was 8.2, which decreased to 2.2 at 12 months after screw fixation. None of the patients complained of worsening of pain during 6 months after implant removal. All patients were graded as having excellent or good outcomes at 6 months after implant removal. The proportion of canal compromise at the fractured level improved from 55% to 35% at 12 months after surgery. The mean preoperative vertebral height loss was 45.3%, which improved to 20.6% at 6 months after implant removal. There were no neurological deficits related to neural injury. The improved vertebral height and canal compromise were maintained at 6 months after implant removal.
Conclusion
Short segment pedicle screw fixation, including fractured level itself, without bone fusion following postural reduction can be an effective and safe operative technique in the management of selected young patients suffering from unstable burst fracture.
Keywords: Screw fixation, Burst fracture, Bone fusion
INTRODUCTION
Both thoracolumbar and lumbar burst fractures are common in spine injuries and occur predominantly in younger patients. They are common in spine injures and occur predominantly in younger patients. The goals of surgical treatment for thoracolumbar burst fractures are to restore stability of the vertebral column and to decompress the spinal canal, leading to early mobilization of the patients. Despite the general agreement on the goals of surgical treatment, the treatment of unstable burst fractures of the thoracolumbar and lumbar spine without neurologic deficits still remains controversial. Conservative treatment for burst fractures without neurologic deficit has been reported to have good results, in spite of increased residual kyphotic angle10). On the other hand, surgical methods provide immediate spinal stability and more reliably restore the sagittal alignment, as well as vertebral and canal dimensions1,11,15,16). Regardless of the approach used, one important goal of internal fixation is to minimize the number of fused levels by using short segment fixation2,6,7). Nowadays, some good clinical outcomes were also reported with short segment fixation without bone fusion11,16). However, there are few reports for burst fracture prospectively investigating the clinical outcome of short segment fixation without bone fusion. We designed a prospective study to evaluate the clinical outcome of short segment fixation without bone fusion of unstable burst fractures of the thoracolumbar and lumbar spine. We also studied whether implant removal would lead to increased loss of vertebral height and poor clinical outcome. The hypotheses of this study were that removal of screws could not affect the stability of the spine and stability could be maintained if natural bone healing and solid union could be simultaneously achieved.
MATERIALS AND METHODS
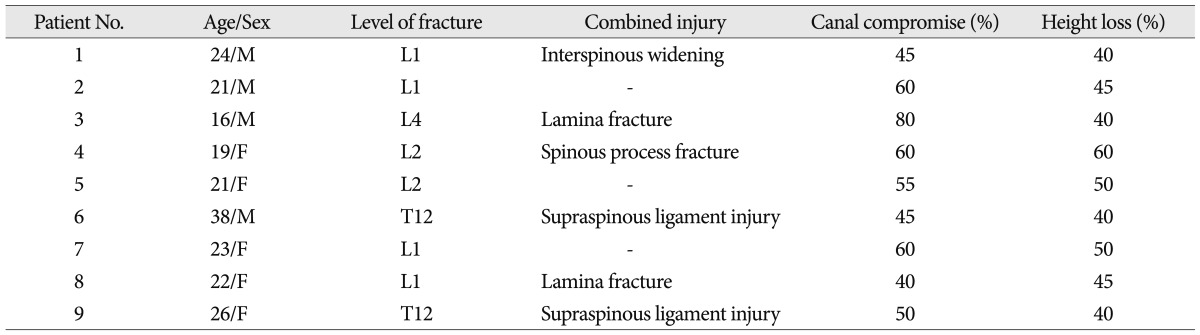
This study included 9 patients (5 male, 4 female) with unstable thoracolumbar or lumbar burst fractures. The inclusion criteria were limited toneurologically intact patients in spite of severe canal compromise (more than 50%) or more than 40% height loss from original height, intact bilateral pedicles, which enabled surgeons to insert the screws at the fractured vertebra, and no osteoporotic spine (T-score on bone mineral densitometry >1.0) in patients younger than 40 years. Patients with conditions requiring anterior decompression for neurologic deficits, and conditions when screws could not be inserted at the fractured level were excluded. However, posterior column injuries including lamina or spinous process fractures and ligamentous injury were not an exclusion criterion in this study (Table 1). We did not perform aggressive decompressive laminectomy because there were neurological deficits identified. All patients underwent removal of implants 12 months after screw fixation, due to possibility of implant failure, and this was explained in full before surgery. After postural reduction for 3 days using a soft roll under the collapsed vertebra in the supine position, standard posterior midline approach was undertaken in all patients. This included short segment transpedicular fixation with one level above and one level below the injured segment, thus including the fractured level itself. The facets and spinal processes were not exposed as widely as in fusion surgery. Intraoperative instrumental reduction was performed to provide anterior force by insertion of the rod to push the injured vertebra ventrally and simultaneously correct the kyphotic deformity to lordosis. On postoperative day 3, after removal of the suction drain, the patients were allowed to ambulate in a thoracolumbosacral orthosis (TLSO) brace. The TLSO brace was used for 3 months after operation. Lateral radiographs and computed tomography (CT) scans were taken and analyzed at three different time points; at preoperative, at 12 months after surgery, just before implant removal, and at six months after implant removal.
Table 1.
Clinical and radiological data of the patients in this series
The vertebral height loss was quantified using the vertebral heights at the anterior collapse on lateral radiographs or sagittal CT scan. The vertebral heights were reported as fractions of anterior height between fractured vertebra and normal height of adjacent one level below the fractured vertebra. The axial CT scan showing the largest canal encroachment by the retropulsed bone fragment was selected for the measurement of canal compromise.
Safety and outcome evaluation
The pain score using VAS was evaluated at three different time points. At six months after implant removal, the patients were evaluated according to a modified version of MacNab's criteria for characterizing the clinical outcome after spinal surgery.
Statistics
Statistical analysis, including mean values and standard deviations, was performed using the SAS software version 6.12 (SAS Institute, Inc., Cary, NC, USA). Comparisons between different time points were conducted using the paired t-test. Differences were considered statistically significant at p<0.05.
RESULTS
The most commonly involved level was L1 (n=4), followed by T12 (n=2), L2 (n=2), and L4 (n=1). The mean age of the participants at the time of injury was 23.2 years (range 16-38 years). The average operative time was 91 minutes (range 70 to 128 min). The average intraoperative blood loss was 90 mL (80-175 mL) and no case required blood transfusion. As mentioned above, all patients were young and they had no osteoporotic spine, and the mean T-score of the patients included in this study was 2.05.
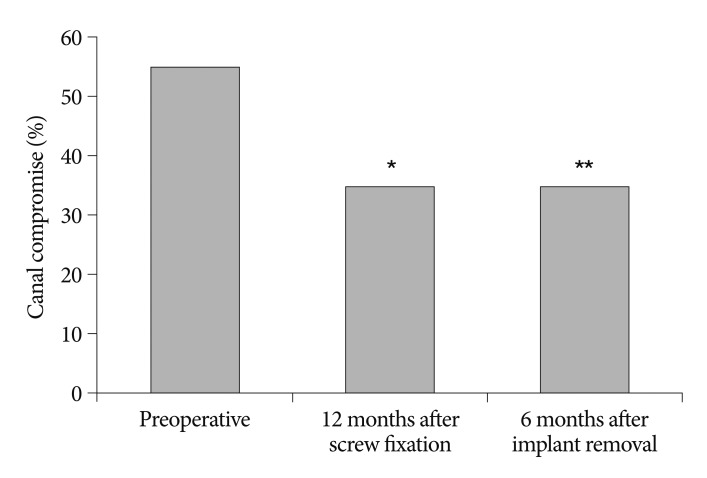
Proportion of canal compromise
The mean preoperative canal encroachment, due to retropulsed bony fragments, was 55%. CT scans at 1 year follow-up, just before implant removal, revealed improved canal compromise to 35%. The improved canal compromise was maintained on CT scans 6 months after implant removal (Fig. 1). Compared to preoperative period, the difference was statistically significant. No patient experienced neurological deterioration due to retropulsed bony fragments, as a result of implant removal.
Fig. 1.
Fraction of canal compromise. *p=0.008 for preoperative versus 12 months after screw fixation. **p=0.008 for preoperative versus 6 months implant removal.
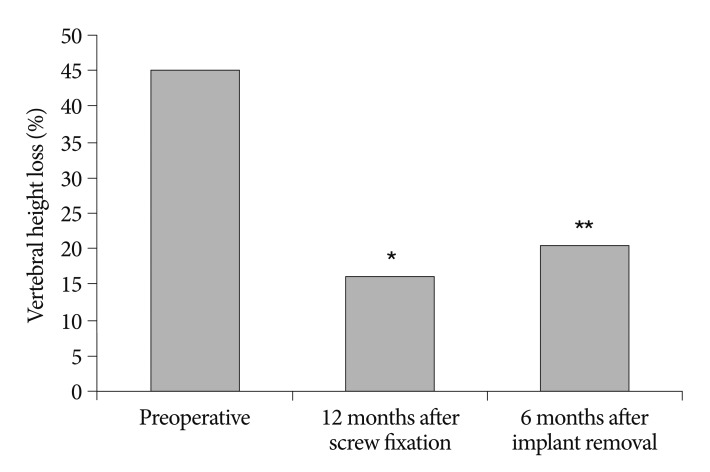
Restoration of vertebral height
The average preoperative percentage of vertebral body height loss was 45.3%. Simple lateral radiograph and CT scans at 1 year follow-up, just before implant removal, showed improved vertebral height loss to 16.3%. At 6 months after implant removal, the average percentage of vertebral body height loss was 20.6%. In spite of some degree of increased vertebral height loss after implant removal, the difference was statistically significant compared to preoperative period (Fig. 2).
Fig. 2.
Restoration of vertebral height. *p=0.001 for preoperative versus 12 months after screw fixation. **p=0.005 for preoperative versus 6 months implant removal.
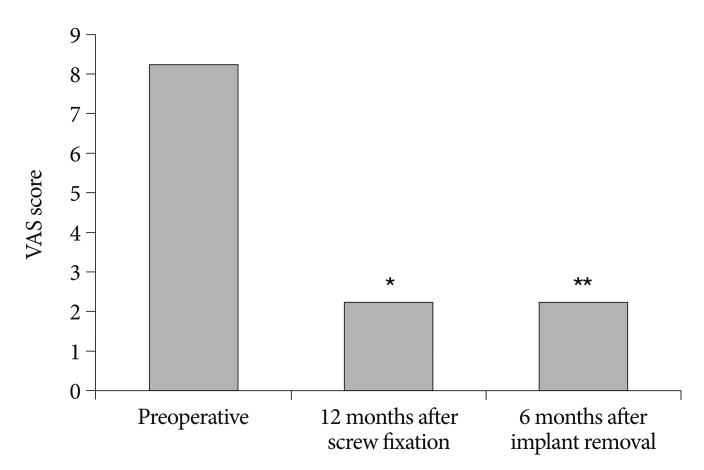
Clinical outcome
At 6 months after implant removal, all patients were graded as having either excellent or good outcomes (Excellent : 7 patients and Good : 2 patients). Prior to surgery, the mean pain score was 8.2, and decreased to 2.2 at 12 months after screw fixation. The improved pain score was maintained at 6 months after implant removal (Fig. 3). There were no significant complications or neurological deterioration after screw removal in any patient (Fig. 4, 5).
Fig. 3.
Improvement of pain score. *p=0.001 for preoperative versus 12 months after screw fixation. **p=0.002 for preoperative versus 6 months implant removal.
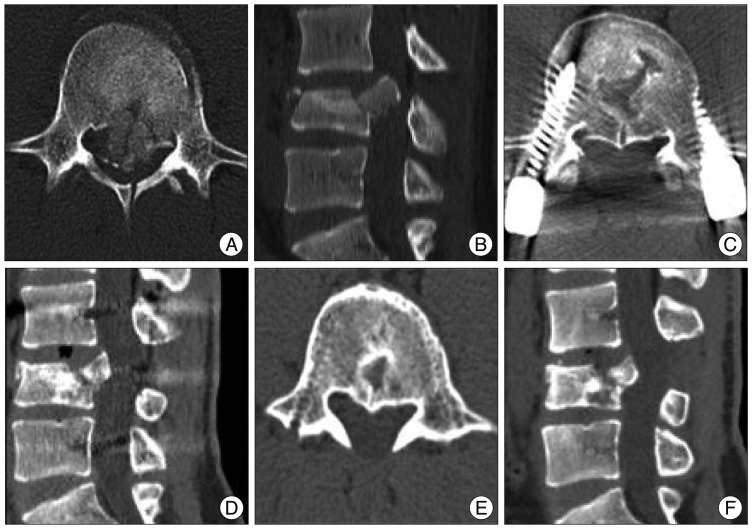
Fig. 4.
A neurologically intact 16-year-old male patient fell down and sustained L4 bursting fracture. A and B : Preoperative computed tomography scans show severe canal compromise (about 80%) and spinous process fracture. C and D : Computed tomographic scans at 12 months follow-up, just before implant removal demonstrate bone healing and canal remodeling with improved canal compromise. E and F : Computed tomographic scans at 6 months after implant removal reveal well-maintained improved canal compromise.
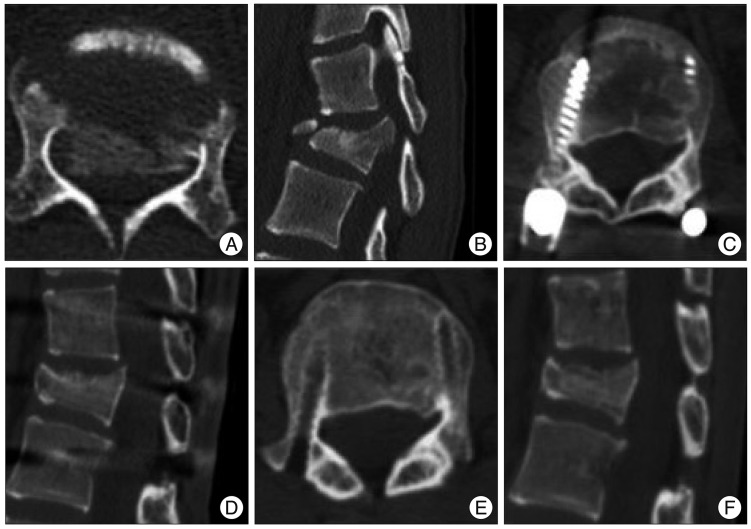
Fig. 5.
A neurologically intact 19-year-old female patient fell down and sustained L2 bursting fracture. A and B : Preoperative computed tomography scans show severe canal compromise (about 60%) and spinous process fracture. C and D : Computed tomographic scans at 12 months follow-up, just before implant removal demonstrate bone healing and canal remodeling with improved canal compromise. E and F : Computed tomographic scans at 6 months after implant removal reveal well-maintained improved canal compromise.
DISCUSSION
According to the "three-column" concept of Denis, burst fracture is a 2 or 3 column injury that may lead to unstable spinal column when presenting with severe canal compromise, greater than 50% loss of vertebral height, angular deformity greater than 20°, multiple contiguous fractures or any neurologic injury2). Symptomatic, unstable burst fractures typically require surgical reduction and stabilization. However, there is no strict guideline or consensus regarding the proper approach for unstable burst fractures of the thoracolumbar or lumbar spine without neurologic deficits, and the issue still remains controversial. Conservative treatment for burst fractures without neurologic deficits has been reported to have good results, in spite of increased residual kyphotic angle10,14). However, non-operative treatment may lead to ongoing neurogenic pain, movement deficits and progressive spinal deformity. In addition, surgical treatment more reliably restores the sagittal alignment, translational deformities, and canal dimensions. Kostuik5) suggested that stabilization of thoracolumbar or lumbar burst fractures without neurologic deficits should be performed when the canal is more than 50% compromised, in conjunction with loss of height and local kyphosis, because of potential for bone fragment displacement and spinal stenosis, by degeneration related to disc and endplate injury. In general, a surgical approach is chosen in cases where conservative treatment is unlikely to produce satisfactory results. The intervention provides fracture reduction and rigid fixation, enhancing bony union or fusion. Most transpedicular screw instrumentation systems have been reported to provide satisfactory results in treating burst fractures of the thoracolumbar or lumbar spine with bone fusion8). Nowadays, however, some good clinical outcomes were also reported with short segment fixation, without bone fusion4,11,16). Theoretically, igamentotaxis allows posterior instrumentation to provide distractive forces, leading to fracture reduction and canal decompression. The annulus fibrosus attaching to the endplate is thought to play a critical role during the reduction of fragments near endplate9). On the basis of fracture reduction theory, in this study, short segment pedicle screw instrumentation was designed and applied in clinical practice. Initially, there were concerns that the insertion of pedicle screws into the fractured body might negatively affect canal restoration, because the increased pressure in the vertebra during screw insertion could push the fracture fragments backwards. However, after postural reduction, the intervertebral pressure has already been reduced to some degree, which, to a large extent, could allow the increased pressure caused by screw insertion. Insertion of pedicle screws at the level of the fracture resulting in a segmental construct that can improve the biomechanical stability by protection to the fractured vertebral body and supporting the anterior column indirectly1,13). Furthermore, spontaneous remodeling of the spinal canal after burst fractures was shown to occur, regardless of the way of treatment. Scapinelli and Candiotto12) insisted that the loss of mechanical loading and rhythmic respiratory oscillations in cerebrospinal fluid pressure would be important factors in the mechanism of bone remodeling. de Klerk et al.3) reported that the process of remodeling mainly takes place during the first year after injury; after this period, there is little further remodeling4). For this reason, we removed implants at 1 year after screw fixation. With short segment fixation without bone fusion, early ambulation was possible and we could preserve motion segments by removal of screws, compared with long level instrumentation and fusion. The advantages of short segment fixation without bone fusion also include immediate pain relief by elimination of donor site pain, reduced blood loss and short operative time. The major limitation of this study was the small number of patients, which precludes absolute conclusions with regards to the superiority of short segment fixation without fusion. The efficacy of short segment fixation without fusion was demonstrated for the patients with an unstable burst fracture in this study, but this by no means indicated that all patients with unstable burst fractures would be treated by this treatment. The patients with more unstable fractures and possibly more severe neurologic injures should be excluded. In the near future, randomized clinical trials for comparative studies in larger population samples are necessary. Nevertheless, we believe that results of this prospective study are significant, because the functional recovery and radiologic outcomes of the selected young patients were satisfactory.
CONCLUSION
Short segment fixation without bone fusion is an effective and reliable operative technique for the treatment of unstable burst fractures when properly indicated, especially in young patients without osteoporosis. The improved canal compromise and vertebral height were maintained during the follow-up period after removal of screws.
References
- 1.Carl AL, Tromanhauser SG, Roger DJ. Pedicle screw instrumentation for thoracolumbar burst fractures and fracture-dislocations. Spine (Phila Pa 1976) 1992;17:S317–S324. doi: 10.1097/00007632-199208001-00018. [DOI] [PubMed] [Google Scholar]
- 2.Cho WS, Chung CK, Jahng TA, Kim HJ. Post-laminectomy kyphosis in patients with cervical ossification of the posterior longitudinal ligament : does it cause neurological deterioration? J Korean Neurosurg Soc. 2008;43:259–264. doi: 10.3340/jkns.2008.43.6.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.de Klerk LW, Fontijne WP, Stijnen T, Braakman R, Tanghe HL, van Linge B. Spontaneous remodeling of the spinal canal after conservative management of thoracolumbar burst fractures. Spine (Phila Pa 1976) 1998;23:1057–1060. doi: 10.1097/00007632-199805010-00018. [DOI] [PubMed] [Google Scholar]
- 4.Jang KS, Ju CI, Kim SW, Lee SM. Screw fixation without fusion for low lumbar burst fracture : a severe canal compromise but neurologically intact case. J Korean Neurosurg Soc. 2011;49:128–130. doi: 10.3340/jkns.2011.49.2.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kostuik JP. Anterior fixation for burst fractures of the thoracic and lumbar spine with or without neurological involvement. Spine (Phila Pa 1976) 1988;13:286–293. doi: 10.1097/00007632-198803000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Lin HJ, Wang ST, Liu CL. Reduction fixation system in treating burst fractures of thoracolumbar spine. J Spine Surg ROC. 1996;2:102–111. [Google Scholar]
- 7.Liu CL, Dai LG, Wang ST. Surgical treatment of thoracic spine burst fractures. J Spine Surg ROC. 1996;2:92–101. [Google Scholar]
- 8.Liu CL, Wang ST, Lin HJ, Kao HC, Yu WK, Lo WH. Roy-Camille plating system in treating burst fractures of thoracolumbar spine. J Orthop Surg Roc. 1996;13:309–316. [Google Scholar]
- 9.Mueller LA, Mueller LP, Schmidt R, Forst R, Rudig L. The phenomenon and efficiency of ligamentotaxis after dorsal stabilization of thoracolumbar burst fractures. Arch Orthop Trauma Surg. 2006;126:364–368. doi: 10.1007/s00402-005-0065-6. [DOI] [PubMed] [Google Scholar]
- 10.Mumford J, Weinstein JN, Spratt KF, Goel VK. Thoracolumbar burst fractures. The clinical efficacy and outcome of nonoperative management. Spine (Phila Pa 1976) 1993;18:955–970. [PubMed] [Google Scholar]
- 11.Sanderson PL, Fraser RD, Hall DJ, Cain CM, Osti OL, Potter GR. Short segment fixation of thoracolumbar burst fractures without fusion. Eur Spine J. 1999;8:495–500. doi: 10.1007/s005860050212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Scapinelli R, Candiotto S. Spontaneous remodeling of the spinal canal after burst fractures of the low thoracic and lumbar region. J Spinal Disord. 1995;8:486–493. [PubMed] [Google Scholar]
- 13.Sjostrom L, Karlstrom G, Pech P, Rauschning W. Indirect spinal canal decompression in burst fractures treated with pedicle screw instrumentation. Spine (Phila Pa 1976) 1996;21:113–123. doi: 10.1097/00007632-199601010-00026. [DOI] [PubMed] [Google Scholar]
- 14.Shen WJ, Shen YS. Nonsurgical treatment of three-column thoracolumbar junction burst fractures without neurologic deficit. Spine (Phila Pa 1976) 1999;24:412–415. doi: 10.1097/00007632-199902150-00024. [DOI] [PubMed] [Google Scholar]
- 15.Siebenga J, Leferink VJ, Segers MJ, Elzinga MJ, Bakker FC, Haarman HJ, et al. Treatment of traumatic thoracolumbar spine fractures : a multicenter prospective randomized study of operative versus nonsurgical treatment. Spine (Phila Pa 1976) 2006;31:2881–2890. doi: 10.1097/01.brs.0000247804.91869.1e. [DOI] [PubMed] [Google Scholar]
- 16.Wang ST, Ma HL, Liu CL, Yu WK, Chang MC, Chen TH. Is fusion necessary for surgically treated burst fractures of the thoracolumbar and lumbar spine?: a prospective, randomized study. Spine (Phila Pa 1976) 2006;31:2646–2652. doi: 10.1097/01.brs.0000244555.28310.40. discussion 2653. [DOI] [PubMed] [Google Scholar]