Abstract
Tendon injuries are the second most common injuries of the hand and therefore an important topic in trauma and orthopedic patients. Most injuries are open injuries to the flexor or extensor tendons, but less frequent injuries, e.g., damage to the functional system tendon sheath and pulley or dull avulsions, also need to be considered. After clinical examination, ultrasound and magnetic resonance imaging have proved to be important diagnostic tools. Tendon injuries mostly require surgical repair, dull avulsions of the distal phalanges extensor tendon can receive conservative therapy. Injuries of the flexor tendon sheath or single pulley injuries are treated conservatively and multiple pulley injuries receive surgical repair. In the postoperative course of flexor tendon injuries, the principle of early passive movement is important to trigger an “intrinsic” tendon healing to guarantee a good outcome. Many substances were evaluated to see if they improved tendon healing; however, little evidence was found. Nevertheless, hyaluronic acid may improve intrinsic tendon healing.
Keywords: Flexor tendon, Extensor tendon, Tendon sheath, Pulley injury, Tendon lesion
EPIDEMIOLOGY
The hand, as the human executing organ, is in the center of daily life activities in professions and sports. In this outstanding position, the hand is always exposed to injuries and overuse. With the change of our society from a industrial society to a service-based society, surprisingly, an assumed decrease in hand injuries has not been detected, probably due to an increase in private activities, such as sports and do-it-yourself work[1]. Based on 50 272 injured persons, Angermann and Lohmann[2] showed that 28.6% of treated patients in emergency care were caused by hand injuries, a risk of 3.7 injuries in 100 000 individuals of the Danish population. On average, hand injuries count for 14% to 30% of all treated patients in emergency care. Tendon lesions are in 2nd position (29%), whereas fractures are 1st (42%) and skin lesions 3rd of all patients treated for hand injuries. Even although only 2% of the patients are hospitalized, hand injuries, especially tendon lesions, play a key role in orthopedic and traumatic treatment. Degenerative lesions must be counted as well.
ANATOMY AND BIOMECHANICS
To begin with, flexor and extensor tendons must be looked at separately anatomically, even although the tendons of the mm. lumbricalis take an exceptional position.
EXTENSOR TENDONS
The long fingers hold 4 common extension tendons, namely extensores digitorum communes, and additionally the extensor indices for the 2nd and the extensor digiti minimi for the 5th finger. The tendon of the extensor digiti minimi runs through the 5th tendon compartment, all the others through the 4th compartment. On the level with the dorsum of the hand and the metacarpophalangeal joints, many cross-connections are found, the connexi intertendinei. On level with the proximal interphalangeal joint (PIP), the extensor tendon separates into two lateral reins and one central rein (tractus intermedius). Two different extensor tendons reach to the thumb, the extensor pollicis longus (3rd extensor compartment) and the extensor pollicis brevis (1st extensor compartment). All named tendons form the so called extrinsic system, tendons of muscles which originate proximal of the hand itself. The extrinsic system is supported by the intrinsic system, muscles originated within in the hand, to the mm. lumbricales, the mm. interossei and the thenar and hypothenar muscles.
FUNCTIONAL SYSTEM “FLEXOR TENDONS”, TENDON SHEATH AND PULLEY
The system of flexor tendons is not looked at individually but as a functional unit of tendons, tendon sheath and pulleys. A differentiation between the thumb and the index finger is also necessary. Both flexor tendons of the long fingers, the flexor digitorum profundus (FDP) and m. flexor digitorum superficial (FDS) run commonly through the carpal tunnel and pulleys and subsequently intersect at the chiasm. The flexor tendon of the thumb (m. flexor pollicis longus) runs through the carpal tunnel on the radial side of the forearm and, strengthened by 2 pulleys, the muscle passes through an osteofibrous channel to the basis of the distal phalanx (Figure 1).
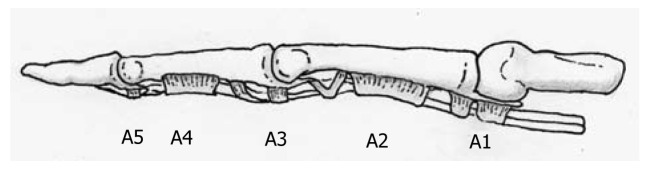
Figure 1.
The pulley system of the long fingers (modified according to Schmidt and Lanz[8]).
The annular ligaments and crucial ligaments are seen as a re-enforcement system of the flexor tendons along the osteofibrous channels of the fingers and hereby are fixed to the phalanges[3]. Four to 5 annular (A1-A5) and 3 weaker crucial ligaments (C1-C3) are distinguished (Figure 1)[3]. The pattern and arrangement of these ligaments vary. All pulleys have different functions in stabilising the flexor tendons at the palmar sides of the phalanges[4,5]. The main function of the flexor tendon digital pulley system is to maintain the flexor tendons close to the bone, thus converting linear translation and force developed in the flexor muscle-tendon unit into rotation and torque at the finger joints[6]. The A2 crucial ligament plays the most important role in guidance of the flexor tendons, whereas opinions concerning the A3 and A4 vary considerably (Figures 2 and 3). A smaller role in strength transmission and tendon deflection is performed by the A1 and A5[6]. The pulley system suppresses the tendon excursion and the strength of the flexor tendons is redirected efficiently in flexion and hyperextension to reach the full range of motion[6]. The mm. lumbricalis and mm. interossei are exceptions as they originate from the flexor tendons themselves and end in the tendinous hood of the extensor tendons. Their function is flexion in the metacarpophalangeal joint (MCP), extension in the proximal (PIP) and distal interphalangeal joint (DIP).
Figure 2.
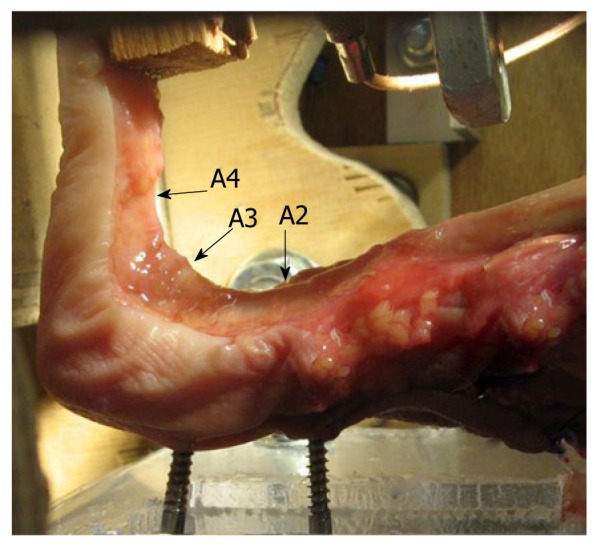
Complete pulley system during a stress test in the biomechanical laboratory. (Figure with permission of Schöffl V, MD, PhD, Institute of Anatomy, University of Erlangen-Nuremberg, Germany[9]).
Figure 3.
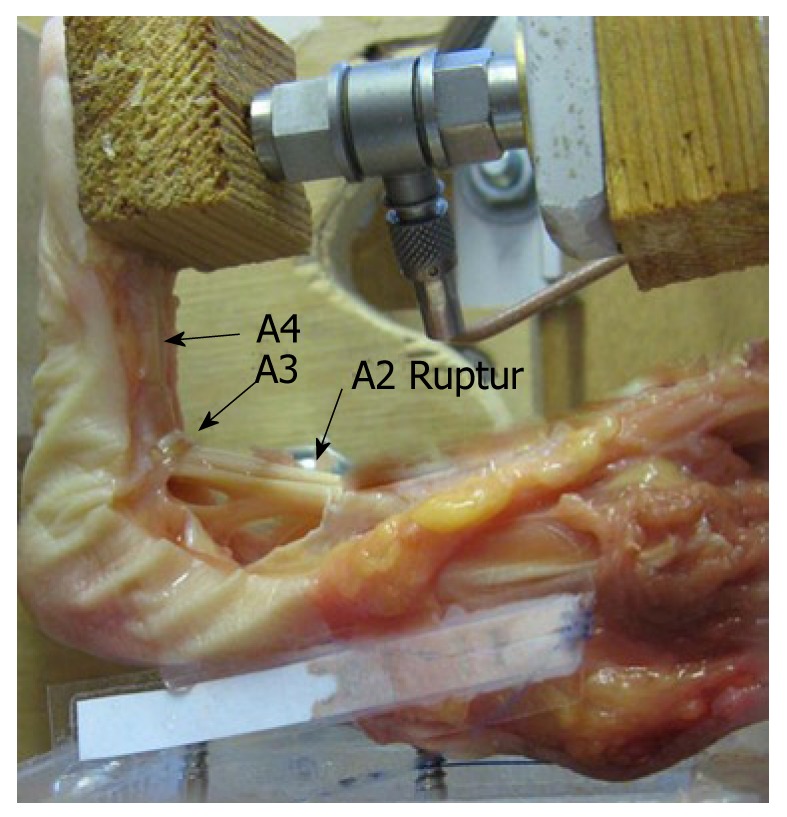
A2-pulley rupture during a stress test in the biomechanical laboratory. Note the increased distance between the flexor tendons and the bone. The A3-pulley is unharmed. (Figure with permission of Schöffl V, MD, PhD, Institute of Anatomy, University of Erlangen-Nuremberg, Germany[9]).
Blood supply of the flexor tendons is guaranteed through the “vincula tendinae” in the region of the osseous insertion of the tendon as well as in the osteofibrous channel. Venous drainage is performed through the same system. Verdan[7] subsequently divided the flexor and extensor tendons into different regions of interest regarding injuries, prognosis and nutrition[1].
TENDON HEALING
Histologically, tendons consist of extremely long collagenous fibers that are arranged into bundles. Similar to a rope ladder, elastic fibers and vessels are entangled in between those bundles[10]. To provide the necessary slippage, a peritendeum or a tendon sheath covers tendons. Pulleys strengthen these structures along the phalanges. Friction plays an important role in the origin of injuries and chronic inflammatory diseases of the tendons, their sheath and pulleys[4,5,11,12]. Following an injury, the healing process emerges from the peritendeum and the peritendinous tissue; therefore a distinction of an extrinsic to an intrinsic healing process has to be made[9,10,12,13]. Characteristic for an extrinsic healing process is a distinctive inflammatory response followed by proliferation and remodeling. Fibroblasts of the paratenon play an important role in migration which leads to adhesions. Immobilization supports the adhesion process[12-16]. The intrinsic healing process, supported by movement of the tendon, is characterized by immigration of “fibroblast-like tenocytes”, which produce the collagenous tissue and carry out the remodeling process[10,12-16]. If the inflammatory response is minimal, the clinical outcome is better. This is the ratio of the widely recommended early passive movement therapy, which leads to better nutrition and strength of the tendon[10,12-16]. The following factors predict the tendon healing: age, overall health condition, scar formation disposition, motivation, injury risk based on Verdan’s zones[7], injury type, synovial containment as well as the surgical technique[12]. Three phases of tendon healing are defined. Firstly, a migration of peripheral cells and invasion of blood vessels occur and secondly, the tendon and surrounding tissues heals. Remodeling happens in the third phase of healing due to movement and function of the tendon[17].
The tendon gains its daily life loading capacity after 12 wk of healing and sporting activities are allowed 4 mo after injury at the earliest. The remodeling process can last up to 12 mo.
INJURY PATTERN
Injury patterns are differentiated into open or closed, sharp or blunt, traumatic or degenerative lesions, as well as injury to the dorsal or palmar part. Further subdivisions are osseous tendon lesions, complex lesions with concomitant trauma or injury of the tendon sheath and pulley system.
Closed tendon injuries are quite common[18] (Figure 4). Among others are the “mallet finger”, the “boutonnière deformity”, avulsions and injuries to the connexus intertendineus. The “mallet finger”, also named baseball finger, is a blunt extensor tendon injury to the distal interphalangeal joint[13,18,19]. An osseous disrupture of the extensor tendon is called mallet fracture[13]. This injury used to be named “Bush-fracture”; a term no longer used[1,9]. The rupture of the tractus intermedius, the “Boutonnière deformity” (French for button hole), is an interruption of the central reins of the extensor tendons at the level of the proximal interphalangeal joint and a subsequent slip of both lateral reins resulting in hyperflexion in the proximal and hyperextension in the distal interphalangeal joint. The full clinical signs of this injury often appear only secondary to a palmar dislocation of the PIP joint. Leddy and Cole[18,20] divide three different types of these injuries. Blunt disruptions, usually due to a direct trauma, of the radial sagittal ligament of the extensor tendon hood at level of the MCP joints lead to subluxation or luxation of the ligament, the majority to the ulnar side[21]. The “boxers knuckle”, following repetitive blunt trauma to the MCP joints, should be taken into differential diagnostic considerations; however, this injury represents an injury of the extensor tendon hood as well but without luxation of the tendon. Avulsions, first mentioned by von Zander[22] in 1989, mostly affect the insertion of the FDP tendon at the distal phalanx. Usually this injury is seen on the 4th finger, as the FDP tendon is embedded in between the double-sided lumbrical tendons, as shown by Manske and Lesker[23] in cadaver dissection. We can verify this injury, especially in rock climbers, based on chronic degenerative damages to the tendon[9,24]. These injuries often result in poor postoperative outcomes[25]. Four factors determine the prognosis of avulsion injuries: the extent of the retraction of the tendon, the remaining blood supply, the time interval between trauma and surgery and the presence and size of an osseous fragment[18]. According to Leddy and Parker[18,20], three different injury types with varying prognosis and therapy exist. Characteristics for type 1 are retractions of the tendon into the palm, the Vinculae are ruptured, the blood supply is interrupted and surgery is needed within 7 d to 10 d after trauma. In type 2 injuries, the tendon retracts to the PIP joint only and is held by an intact vinculum. Therefore, the blood supply is not compromised and surgery can be delayed without risking a poor outcome. Type 3 injuries are osseous ruptures of the FDP tendon at the distal phalanx. Thank to the intact vinculum, these injuries have a good prognosis. Blunt trauma, in terms of ruptures, also happen to the tendon sheath and the pulleys[3,11,13,26-28]. Rarely, blunt disruptions of the lumbricalis origins at the flexor tendon on the palm level do occur in high stress finger activity (e.g., rock climbing) (Figure 4).
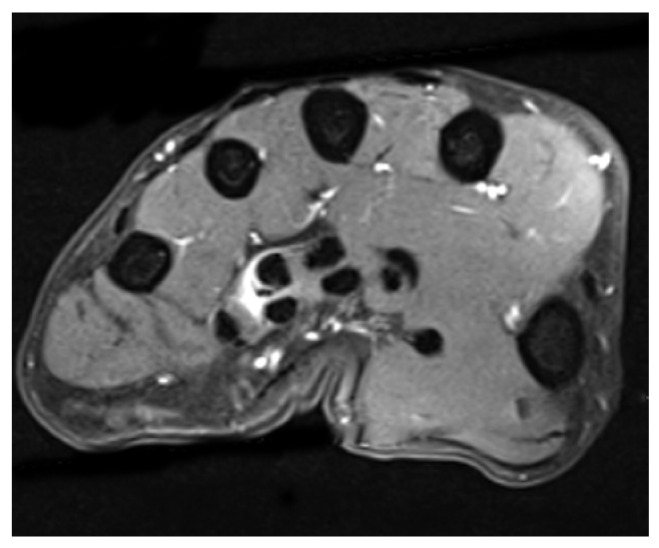
Figure 4.
Closed flexor tendon rupture of the flexor digitorum profundus at the level of the middle phalanx (rock climber)[9].
Open tendon injuries are common findings in trauma and orthopedic patients and need primary surgical treatment. A differentiation between complete or partial rupture has to be made. A lesion of less than 60% of the tendon’s diameter should be treated conservatively[13]. Multiple biomechanical in vivo and ex vivo studies proved that conservatively treated partial tendon ruptures showed a higher tear-resistance (P < 0.05) compared to the surgically treated ones[13]. Chronic degenerative tendon ruptures as seen in rheumatic patients must be distinguished from these traumatic ruptures. A combined entity we see in our patients, mostly in rock climbers, is a chronic tendinosis and degeneration and then finally an acute tear (Figures 5 and 6). High intensive stress combined with chronic tenosynovitis (peritendinosis) and tendinosis (endotendinitis) can lead to a rupture of the tendon, even although only minor stress was applied[25]. Additional to the poor blood supply of the tendon, microtrauma and microscopic structural damage can lead to a modest prognosis.
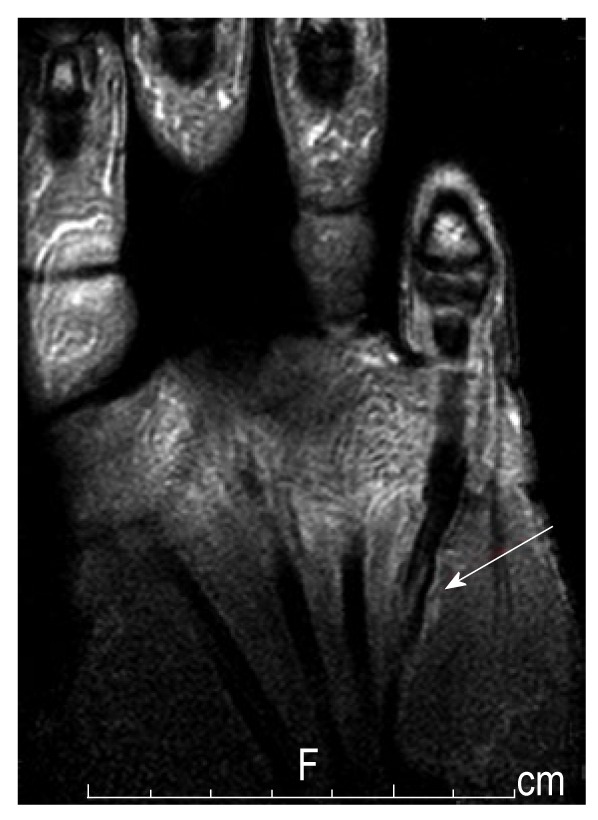
Figure 5.
Lumbrical tendon rupture (note the edema and the dislocated lumbrical tendon from the flexor tendon).
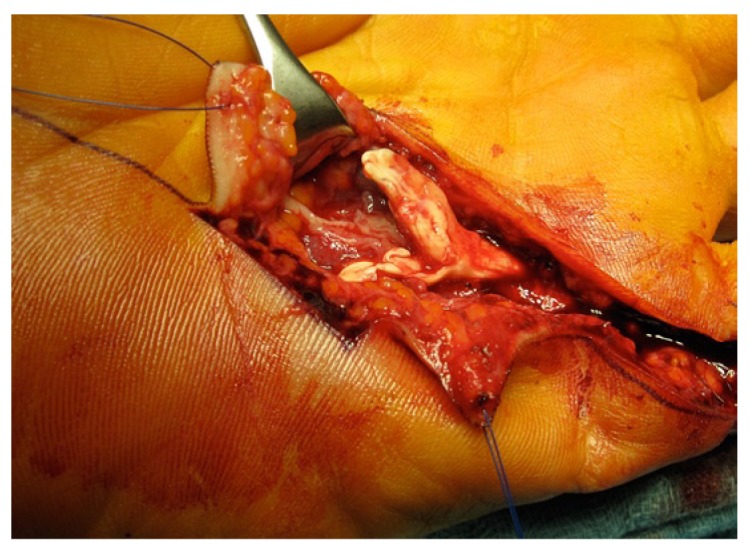
Figure 6.
Degenerative flexor tendon rupture in a long term rock climber with chronic tendinosis.
TENDON SHEATH AND PULLEY LESIONS
Injuries of the tendon sheath and the pulley system are often associated with flexor tendon injuries as these structures form a functional unit[1-3,5,6,10,13,29]. In open lesions, these structures must be repaired as exactly as possible to guarantee biomechanical efficiency and nutrition of the tendon[12,13]. Closed injuries, especially pulley and c-ligament lesions, are common findings in athletes (climbers)[3,6,25,30-32] and only casually in other patients groups[33].
DIAGNOSIS
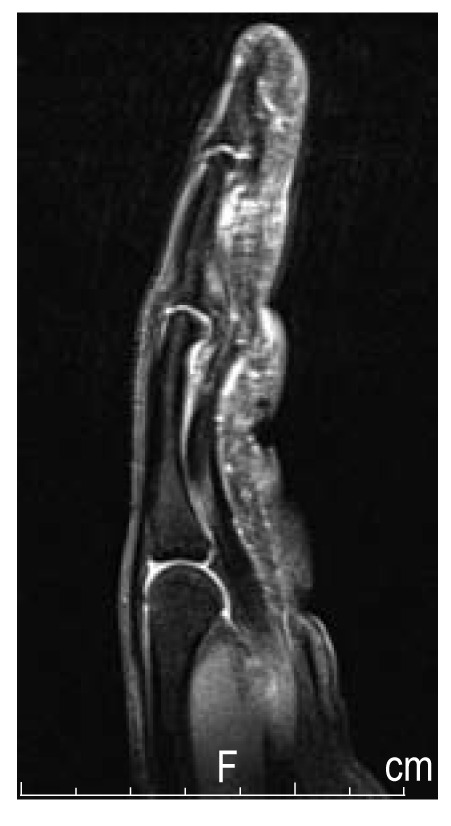
Compared to closed injuries, open lesions are easy to diagnose. Closed injuries should especially be looked at carefully, not only to get a specific diagnosis but also to locate the topographical region of the injury. In clinical examinations of lacerations, one has to remember that even small cuts can cause severe damage underneath the surface, for example, a partial rupture of 90% of the tendon can appear to be functionally intact but after a couple of days this tendon will rupture secondary to relatively minor stress[13]. The function of the FDS and FDP tendons need to be examined separately. A pulley lesion may become apparent with a bowstring phenomenon (Figures 7 and 8). Concomitant injuries of the bundle of nerves and vessels or open joint capsule injuries combined with palmar plate injuries need to be excluded. In addition to the clinical examination, ultrasound and magnetic resonance imaging (MRI) are well established tools to detect closed tendon injuries, as well as to assess injuries to the pulleys and tendon sheaths. Ultrasound is performed in the supine position with longitudinal and transversal planes using a linear transducer (10-13 MHz). For signal enhancement, a gel standoff pad or examination in a warm water basin is used. Only in rare cases an additional MRI [or (computed tomography) CT] needs to be performed[3,30,34]. A considerably advantage of the ultrasound is the possibility of dynamic examination, which can demonstrate tendons excursions through “forced flexion” better than a static method[35-37]. Additionally, inflammatory processes can be easily demonstrated (effusion, increased blood flow) and cellulitis, ganglion cysts and phlegmonia can also be visualized and detected[38]. Diagnosis of a pulley lesion is performed in forced flexion of the finger, meaning active pressure of the finger towards the transducer[3,39]. Thereby quantifications of the enhanced distance between bone and flexor tendon, as seen in pulley ruptures, can be made[3,39]. If no specific diagnosis can be made using the ultrasound, CT and MRI are available as other diagnostic tools[30,40]. The ultrasound has the advantage that dynamic examinations[30] can be made[41]. Using the MRI, a more specific differentiation of inflammatory processes or post traumatic edema can be made[37].
Figure 7.
Degenerative flexor tendon rupture in a long term rock climber with chronic tendinosis. The histology showed a mucoid degeneration with numerous blood vessel proliferations and a siderosis as a sign of an older bleed[9].
Figure 8.
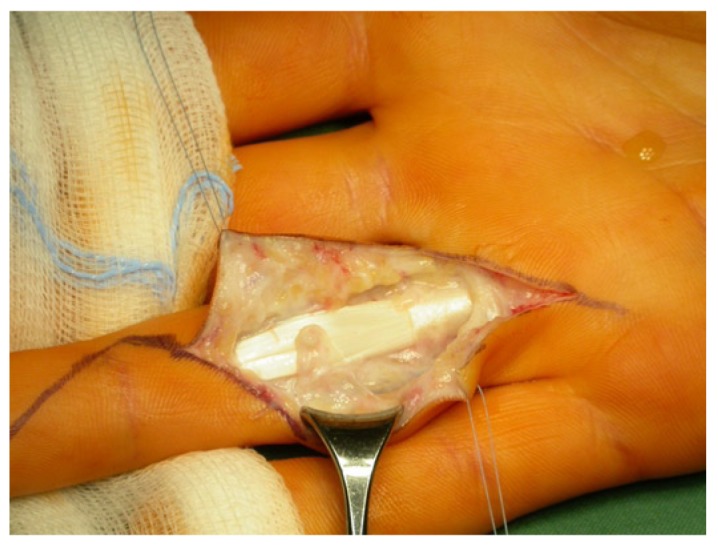
Ruptured A3 pulley (the tendon sheath with chronic inflammation is already removed).
THERAPY
In the following section, the essential therapeutic approach is presented. Nevertheless, focus is kept on considerably rare injuries, as the treatment of common injuries, e.g., flexor tendon ruptures, is standardized and well described elsewhere[1,10,13,14,17-20,42-50].
EXTENSOR TENDON INJURIES
Blunt disrupters of the extensor tendons of the DIP (“mallet finger”) (Verdan Zone 1[7]) can be treated conservatively using a stack splint if the injury is just a partial rupture in which the collateral fibers of the “Landsmeer ligaments” (lig. retinaculare obliquum) are intact[19]. A surgical treatment analogous to open injuries is required if a extension deficit of more than 45° is present[18]. A solemnly percutaneous wire fixation in hyperextension is not recommended any more[19] and instead “mallet” fractures are treated by using osteosynthesis techniques, such as screws, tension band or K wiring.
In the extensor tendons, their specific shape has to be acknowledged in performing repairs. The further distal the muscular part, the flatter the diameter of the tendon gets. Therefore, suturing techniques used in flexor tendon repairs, a central suture and circular fine adaptation of fibers, cannot be used[1]. In open injuries, the wound itself should be used as a surgical approach and extended Z-shaped. Due to the diameter of the tendon, several U-shaped sutures should be used, optionally combined with fine adaptation sutures using PDS (5-0, 6-0). In treatment of the tractus intermedius (PIP joint) and extensor tendon injuries at the level of the DIP joint, the suture should be secondarily stabilized with a temporary K-wire arthrodesis (diameter 0.8-1.0 mm) (6 weeks immobilization in a neutral position). The wire should be inserted diagonal to the joint space, not longitudinal through the fingertip, to avoid bacterial transmission[19]. The use of the “Lengemann wire suture” is no longer recommended[1,19]. Extensor tendon injuries of the hand require immobilization using the intrinsic plus position. Accompanying injuries of the finger joints need to be treated adequately and the articular capsule needs to be fixed. Extensor tendon subluxations and luxations on level with the MCP joint are mostly revealed subsequently and require a surgical repair or secondarily, a plastic reconstruction[18]. Osteophytic irritations of the extensor tendons (“extensor hood syndrome”) can usually be treated conservatively[51].
FLEXOR TENDON INJURIES
Open flexor tendon injuries require a surgical procedure using magnifying glasses[1]. Surgery should be performed under plexus or general anesthesia with the use of a tourniquet. Surgery should be performed in the operating room using perioperative antibiotic prophylaxis. As flexor tendon injuries are often combined with injuries to the vessels and nerves, these structures must be thoroughly displayed[1,9,10,12,13,17,42-45,52-59]. A palmar “Bruner” incision is followed by a modified (Zechner) Kirchmayr-Kessler suture with non absorbable plaited 4-0 yarn. For fine adaptation “running-sutures”, a monofil 6-0 yarn is used, either absorbable or non absorbable (e.g., PDS)[1,9,10,12,13,17,42-45]. If annular pulleys need to be released, a double door wing shaped incision is performed and secondarily reconstructed as an extension plastic[42]. Extensive retracted proximal tendon stumps can be produced and refixed, using an additional incision to insert a flexible catheter through the tendon sheath-pulley system and fix the tendon stump to it, to pull the tendon further distally[18]. Blunt flexor tendon disruptions are sutured, osseous avulsions are refixed transosseus (using a periosteal flap if necessary[18]). A primary arthrodesis of the DIP should be considered in excessive degenerative tendon lesions. If tendon tissue is resected, the tendon must be lengthened using a Z-plastic or a forearm tendon recession[9].
INJURIES OF TENDON SHEATH AND PULLEY SYSTEM
Injuries of the tendon sheath and pulley system are often combined with flexor tendon lesions as these structures form a functional unit[1,2,6,9,10,13,34,60]. Open lacerations should be reconstructed, even with lengthening if necessary. Therapy of closed pulley lesions should be treated according to Figure 9. Singular pulley injuries should be treated conservatively, whereas multiple injuries should be treated surgically using pulley plastic surgery (Palmaris longus transplant as a 1.5 loop according to Widstroem[61,62] or Schöffl et al[63] or a Retinaculum Extensorum Flap, performed according to Lister[64], Moutet et al[65] or Gabl et al[60]).
Figure 9.
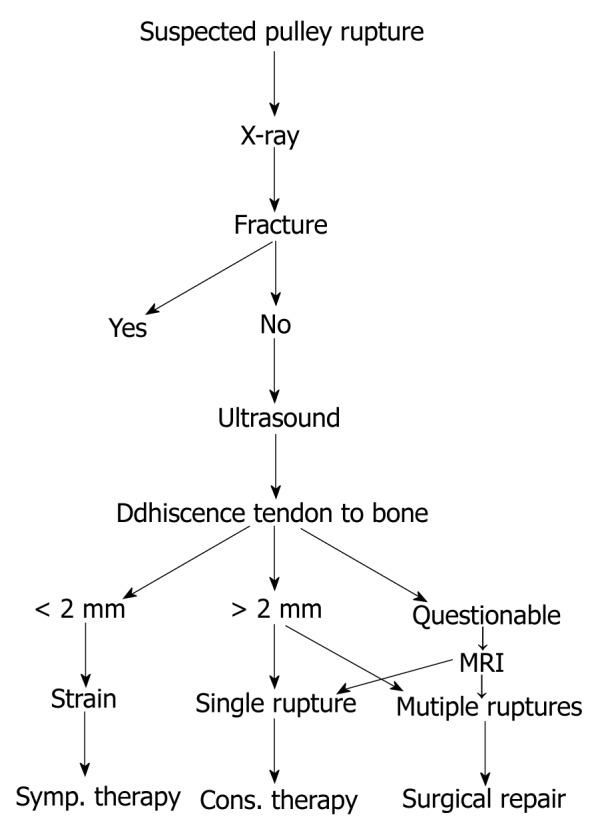
Algorithm for pulley injuries[3]. MRI: Magnetic resonance imaging.
POSTOPERATIVE CARE
Extensor tendon injuries require immobilization (transfixation or an “intrinsic plus” cast)[1,13,18,19]. A dynamic aftercare using a reversed “Kleinert“ extension splint for extensor tendon injuries of the zones VI-VIII was discussed recently[19]. Studies show a similar outcome for Verdan type II-IV injuries[7], whereas type V-VII seem to have a better outcome if treated with dynamic aftercare[19]. Aftercare of flexor tendon injuries should follow the scheme of dynamic early mobilisation, as proposed by Kleinert[66], which allows passive flexion, carried out by a rubber string and active extension[1,10,13,17,42,43,45]. The wrist flexion of the cast is reduced gradually and after 3 wk, a Kleinert-bandage with rubber band restraints can be applied. Free functional movement is allowed after 5 wk, full exposure after 3-4 mo. An “intrinsic tendon healing” is sought for, which requires intermittent tension stress[42], achieved by the “early passive movement” principle[10,43,45]. Recently, more progressive aftercare schemes postulate active flexion of the tendon immediately after surgery but are not yet commonly established[10]. Lohmeyer et al[44] evaluated standards in therapy of combined flexor tendon and nerve injuries in German centers of hand surgery. Isolated injuries of type II-IV were treated with schemes of early dynamic movement in all hand surgery centers; combined injuries were treated dynamically immediately after surgery by 55% of the interviewed centers. Pulley plastic aftercare is treated with 2 wk of immobilization, followed by early functional treatment using an external pulley support, first as a thermoplastic ring and later through a protective tape (h-tape)[67].
PROGNOSIS AND COMPLICATIONS
The most concerning complications in flexor tendon surgery are adhesions and suture dehiscence, maybe due to prematurely active movement[12]. This is an expression of “extrinsic tendon healing”, characterized by a distinctive inflammatory phase with migration of peritendinous fibroblasts[14,15]. For an intrinsic healing, an intact system of tendon sheath and pulleys is essential, which produces a synovial fluid-like environment that supports the healing process until the vascular system is regenerated. Scrubbing of the tendon along the tendon sheath pumps nutritive synovial fluid into the tenocytes and adhesions are prevented[12] (Figure 9). Many papers report excellent outcomes in 70% after flexor tendon sutures, similarly to Brug[42], who reports 71.8% excellent, 13% good and 8.8% poor results, according to the Buck-Gramcko-Score[68], in a study of 258 patients. According to Geldmacher, even with optimal premises, less than 90% excellent outcomes are to be expected and only 13% with poor premises[42]. Blunt and degenerative avulsion injuries show an even worse outcome[12].
In various studies, different agents to improve slippage after tendon sutures and prevent adhesions were evaluated. Alpha-Aminproprionitrile is said to prevent cross links of collagen but appeared to be toxic[12]. D-Penicillamine, cis-Hydroxyproline, Triamcinolone, Polyvinylpyrrolidone and others have not been proven to have a reliable effect or have been shown to be impracticable[12]. Hyaluronic acid may improve intrinsic tendon healing but studies have not shown reliable data[12]. Besides adhesions and following essential intense physiotherapy, Quengel treatment and tenolysis, dreaded complications are contractures, secondary ruptures, pulley malfunction, snapping finger and infection. Pulley malfunction either by rupture or insufficient initial reconstruction indicates secondary pulley plastic[3,12,28].
SECONDARY TENDON REPLACEMENT AND TRANSFER
If flexor tendon lesions were not treated adequately at first, secondary reconstruction is necessary. Decision to perform a one or two step reconstruction of the tendon is dependent, among other reasons, on the localization of the injury, the extent of scar tissue and an intact pulley system[13,43]. In 1912, Lexer had already reported free tendon transplants[13]. In 1918, Bunnel called for an atraumatic approach to surgery: usage of the palmaris longus tendon as well as a tourniquet and conservation of the pulley system for secondary reconstruction[13,69]. Even although inconsistent, nowadays the tendon of the m. palmaris longus is usually used for reconstruction[13]. The tendon is found in 85% of patients[13]. As an alternative, the tendon of the m. plantaris can be used, which is found in 93% in patients[13]. Extensor tendons of fingers and toes can be other alternatives, as well as the FDP tendon of the fifth finger[12,13]. After reconstruction of the flexor tendon channel via insertion of a silastic bar and secondary transplantation, further reconstruction follows either in one or two steps. Other possibilities are tendon transfers and compensational replacement surgery, which are not discussed in this paper.
CONCLUSION
Open and blunt tendon injuries of the hand, especially injuries of flexor tendons, are serious injuries that should be treated by a skilled surgeon. Blunt injuries need to be detected and treated consequently as well as open lesions. If in doubt, ultrasound and MRI can be of great diagnostic benefit. Consistent initial therapy is as important for a good overall outcome as is proper aftercare. Close cooperation of the surgeon and the patient is essential, as well as physiotherapy and occupational therapy.
Footnotes
Peer reviewer: Stefan Grote, MD, Department of Orthopaedic and Trauma Surgery, University of Munich, Nußbaumstr. 20, 80336 Munich, Germany
S- Editor Yang XC L- Editor Roemmele A E- Editor Yang XC
References
- 1.Voigt C. [Tendon injuries of the hand] Chirurg. 2002;73:744–64; quiz 765-7. doi: 10.1007/s00104-002-0497-2. [DOI] [PubMed] [Google Scholar]
- 2.Angermann P, Lohmann M. Injuries to the hand and wrist. A study of 50,272 injuries. J Hand Surg Br. 1993;18:642–644. doi: 10.1016/0266-7681(93)90024-a. [DOI] [PubMed] [Google Scholar]
- 3.Schöffl VR, Schöffl I. Injuries to the finger flexor pulley system in rock climbers: current concepts. J Hand Surg Am. 2006;31:647–654. doi: 10.1016/j.jhsa.2006.02.011. [DOI] [PubMed] [Google Scholar]
- 4.Schöffl I, Oppelt K, Jüngert J, Schweizer A, Bayer T, Neuhuber W, Schöffl V. The influence of concentric and eccentric loading on the finger pulley system. J Biomech. 2009;42:2124–2128. doi: 10.1016/j.jbiomech.2009.05.033. [DOI] [PubMed] [Google Scholar]
- 5.Schöffl I, Oppelt K, Jüngert J, Schweizer A, Neuhuber W, Schöffl V. The influence of the crimp and slope grip position on the finger pulley system. J Biomech. 2009;42:2183–2187. doi: 10.1016/j.jbiomech.2009.04.049. [DOI] [PubMed] [Google Scholar]
- 6.Roloff I, Schöffl VR, Vigouroux L, Quaine F. Biomechanical model for the determination of the forces acting on the finger pulley system. J Biomech. 2006;39:915–923. doi: 10.1016/j.jbiomech.2005.01.028. [DOI] [PubMed] [Google Scholar]
- 7.Verdan CE. Primary and secondary repair of flexor and extensor tendon injuries. In: Hand Surgery, Flynn JE (ed), editors. Williams & Willkins: Baltimore; 1966. pp. 220–242. [Google Scholar]
- 8.Schmidt HM, Lanz U. Chirurgische Anatomie der Hand [Surgical anatomy of the hand] Hippokrates Verlag: Stuttgart; 2003. pp. 186–187. [Google Scholar]
- 9.Schöffl V, Winkelmann HP. [Traumatic and degenerative tendon lesions of the hand] Orthopade. 2010;39:1108–1116. doi: 10.1007/s00132-010-1688-z. [DOI] [PubMed] [Google Scholar]
- 10.Werdin F, Schaller HE. [Combined flexor tendon and nerve injury of the hand] Orthopade. 2008;37:1202–1209. doi: 10.1007/s00132-008-1327-0. [DOI] [PubMed] [Google Scholar]
- 11.Schweizer A, Frank O, Ochsner PE, Jacob HA. Friction between human finger flexor tendons and pulleys at high loads. J Biomech. 2003;36:63–71. doi: 10.1016/s0021-9290(02)00242-7. [DOI] [PubMed] [Google Scholar]
- 12.Taras JS, Gray RM, Culp RW. Complications of flexor tendon injuries. Hand Clin. 1994;10:93–109. [PubMed] [Google Scholar]
- 13.Boyer MI, Strickland JW, Engles D, Sachar K, Leversedge FJ. Flexor tendon repair and rehabilitation: state of the art in 2002. Instr Course Lect. 2003;52:137–161. [PubMed] [Google Scholar]
- 14.Strickland JW. The scientific basis for advances in flexor tendon surgery. J Hand Ther. 2005;18:94–110; quiz 111. doi: 10.1197/j.jht.2005.01.013. [DOI] [PubMed] [Google Scholar]
- 15.Choueka J, Heminger H, Mass DP. Cyclical testing of zone II flexor tendon repairs. J Hand Surg Am. 2000;25:1127–1134. doi: 10.1053/jhsu.2000.20155. [DOI] [PubMed] [Google Scholar]
- 16.Stein T, Ali A, Hamman J, Mass DP. A randomized biomechanical study of zone II human flexor tendon repairs analyzed in a linear model. J Hand Surg Am. 1998;23:1043–1045. doi: 10.1016/S0363-5023(98)80013-0. [DOI] [PubMed] [Google Scholar]
- 17.Werber KD. [Flexor tendon injuries of the hand] Unfallchirurg. 2005;108:873–81; quiz 882. doi: 10.1007/s00113-005-1021-1. [DOI] [PubMed] [Google Scholar]
- 18.Aronowitz ER, Leddy JP. Closed tendon injuries of the hand and wrist in athletes. Clin Sports Med. 1998;17:449–467. doi: 10.1016/s0278-5919(05)70096-x. [DOI] [PubMed] [Google Scholar]
- 19.Partecke BD, Peterhof G. [Management and after-care of extensor tendon injuries of the hand] Unfallchirurg. 1998;101:807–812. doi: 10.1007/s001130050343. [DOI] [PubMed] [Google Scholar]
- 20.Leddy JP, Packer JW. Avulsion of the profundus tendon insertion in athletes. J Hand Surg Am. 1977;2:66–69. doi: 10.1016/s0363-5023(77)80012-9. [DOI] [PubMed] [Google Scholar]
- 21.Kettelkamp DB, Flatt AE, Moulds R. Traumatic dislocation of the long-finger extensor tendon. A clinical, anatomical, and biomechanical study. J Bone Joint Surg Am. 1971;53:229–240. [PubMed] [Google Scholar]
- 22.Von Zander. Trommlerl?hmung. Berlin; 1891. [Google Scholar]
- 23.Manske PR, Lesker PA. Avulsion of the ring finger flexor digitorum profundus tendon: an experimental study. Hand. 1978;10:52–55. doi: 10.1016/s0072-968x(78)80025-4. [DOI] [PubMed] [Google Scholar]
- 24.Schöffl V. Rock Climbing. In: Sports Injuries, Engelhardt M (ed), editors. Elsevier: Munich-Jena; 2011. [Google Scholar]
- 25.Schöffl VR, Schöffl I. Finger pain in rock climbers: reaching the right differential diagnosis and therapy. J Sports Med Phys Fitness. 2007;47:70–78. [PubMed] [Google Scholar]
- 26.Schöffl V, Schöffl I. Isolated cruciate pulley injuries in rock climbers. J Hand Surg Eur Vol. 2010;35:245–246. doi: 10.1177/1753193408337887. [DOI] [PubMed] [Google Scholar]
- 27.Bollen SR. Injury to the A2 pulley in rock climbers. J Hand Surg Br. 1990;15:268–270. doi: 10.1016/0266-7681_90_90135-q. [DOI] [PubMed] [Google Scholar]
- 28.Schöffl I, Baier T, Schöffl V. Flap irritation phenomenon (FLIP): etiology of chronic tenosynovitis after finger pulley rupture. J Appl Biomech. 2011;27:291–296. doi: 10.1123/jab.27.4.291. [DOI] [PubMed] [Google Scholar]
- 29.Schweizer A. Biomechanical properties of the crimp grip position in rock climbers. J Biomech. 2001;34:217–223. doi: 10.1016/s0021-9290(00)00184-6. [DOI] [PubMed] [Google Scholar]
- 30.Martinoli C, Bianchi S, Cotten A. Imaging of rock climbing injuries. Semin Musculoskelet Radiol. 2005;9:334–345. doi: 10.1055/s-2005-923378. [DOI] [PubMed] [Google Scholar]
- 31.Schöffl V, Morrison A, Schwarz U, Schöffl I, Küpper T. Evaluation of injury and fatality risk in rock and ice climbing. Sports Med. 2010;40:657–679. doi: 10.2165/11533690-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 32.Schweizer A. Biomechanical effectiveness of taping the A2 pulley in rock climbers. J Hand Surg Br. 2000;25:102–107. doi: 10.1054/jhsb.1999.0335. [DOI] [PubMed] [Google Scholar]
- 33.Schöffl VR, Jüngert J. Closed flexor pulley injuries in nonclimbing activities. J Hand Surg Am. 2006;31:806–810. doi: 10.1016/j.jhsa.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 34.Schöffl V, Hochholzer T, Winkelmann HP, Strecker W. Pulley injuries in rock climbers. Wilderness Environ Med. 2003;14:94–100. doi: 10.1580/1080-6032(2003)014[0094:piirc]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 35.Klauser A, Frauscher F, Bodner G, Halpern EJ, Schocke MF, Springer P, Gabl M, Judmaier W, zur Nedden D. Finger pulley injuries in extreme rock climbers: depiction with dynamic US. Radiology. 2002;222:755–761. doi: 10.1148/radiol.2223010752. [DOI] [PubMed] [Google Scholar]
- 36.Klauser A, Frauscher F, Bodner G, Cihak C, Gabl M, Schocke M, Smekal V, Helweg G, Zur Nedden D. [Value of high-resolution ultrasound in the evaluation of finger injuries in extreme sport climbers] Ultraschall Med. 2000;21:73–78. doi: 10.1055/s-2000-316. [DOI] [PubMed] [Google Scholar]
- 37.Bodner G, Rudisch A, Gabl M, Judmaier W, Springer P, Klauser A. Diagnosis of digital flexor tendon annular pulley disruption: comparison of high frequency ultrasound and MRI. Ultraschall Med. 1999;20:131–136. doi: 10.1055/s-1999-8904. [DOI] [PubMed] [Google Scholar]
- 38.McGeorge DD, McGeorge S. Diagnostic medical ultrasound in the management of hand injuries. J Hand Surg Br. 1990;15:256–261. doi: 10.1016/0266-7681_90_90133-o. [DOI] [PubMed] [Google Scholar]
- 39.Klauser A, Stadlbauer KH, Frauscher F, Herold M, Klima G, Schirmer M, zur Nedden D. Value of transducer positions in the measurement of finger flexor tendon thickness by sonography. J Ultrasound Med. 2004;23:331–337. doi: 10.7863/jum.2004.23.3.331. [DOI] [PubMed] [Google Scholar]
- 40.Bencardino JT. MR imaging of tendon lesions of the hand and wrist. Magn Reson Imaging Clin N Am. 2004;12:333–47, vii. doi: 10.1016/j.mric.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 41.Martinoli C, Bianchi S, Nebiolo M, Derchi LE, Garcia JF. Sonographic evaluation of digital annular pulley tears. Skeletal Radiol. 2000;29:387–391. doi: 10.1007/s002560000226. [DOI] [PubMed] [Google Scholar]
- 42.Brug E. [Primary management of flexor tendon injuries of the hand] Unfallchirurg. 1997;100:602–612. doi: 10.1007/s001130050165. [DOI] [PubMed] [Google Scholar]
- 43.Hernandez JD, Stern PJ. Complex injuries including flexor tendon disruption. Hand Clin. 2005;21:187–197. doi: 10.1016/j.hcl.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 44.Lohmeyer JA, Siemers F, Mailänder P. [Therapy standards after flexor tendon and nerve injuries of the hand: results from a survey of German centres for hand surgery] Unfallchirurg. 2010;113:203–209. doi: 10.1007/s00113-009-1692-0. [DOI] [PubMed] [Google Scholar]
- 45.Bell Krotoski JA. Flexor tendon and peripheral nerve repair. Hand Surg. 2002;7:83–109. doi: 10.1142/s021881040200087x. [DOI] [PubMed] [Google Scholar]
- 46.Forster BB, Becker A, Andrews G, Gropper P. Answer to case of the month #118. Flexor tendon pulley injury. Can Assoc Radiol J. 2007;58:118–120. [PubMed] [Google Scholar]
- 47.Arora R, Fritz D, Zimmermann R, Lutz M, Kamelger F, Klauser AS, Gabl M. Reconstruction of the digital flexor pulley system: a retrospective comparison of two methods of treatment. J Hand Surg Eur Vol. 2007;32:60–66. doi: 10.1016/j.jhsb.2006.09.019. [DOI] [PubMed] [Google Scholar]
- 48.Peterson JJ, Bancroft LW. Injuries of the fingers and thumb in the athlete. Clin Sports Med. 2006;25:527–42, vii-viii. doi: 10.1016/j.csm.2006.02.001. [DOI] [PubMed] [Google Scholar]
- 49.Sharma P, Maffulli N. Tendon injury and tendinopathy: healing and repair. J Bone Joint Surg Am. 2005;87:187–202. doi: 10.2106/JBJS.D.01850. [DOI] [PubMed] [Google Scholar]
- 50.Vandeputte G, Dubert T. Closed traumatic rupture of the flexor pulleys of a long finger associated with avulsion of the flexor digitorum superficialis. J Hand Surg Br. 2001;26:266–268. doi: 10.1054/jhsb.2001.0559. [DOI] [PubMed] [Google Scholar]
- 51.Schöffl V, Hochholzer T, Schöffl I. Extensor hood syndrome--osteophytic irritation of digital extensor tendons in rock climbers. Wilderness Environ Med. 2010;21:253–256. doi: 10.1016/j.wem.2010.04.007. [DOI] [PubMed] [Google Scholar]
- 52.Azari KK, Meals RA. Flexor tenolysis. Hand Clin. 2005;21:211–217. doi: 10.1016/j.hcl.2004.11.008. [DOI] [PubMed] [Google Scholar]
- 53.Dennerlein JT, Diao E, Mote CD, Rempel DM. Tensions of the flexor digitorum superficialis are higher than a current model predicts. J Biomech. 1998;31:295–301. doi: 10.1016/s0021-9290(98)00006-2. [DOI] [PubMed] [Google Scholar]
- 54.Hamman J, Ali A, Phillips C, Cunningham B, Mass DP. A biomechanical study of the flexor digitorum superficialis: effects of digital pulley excision and loss of the flexor digitorum profundus. J Hand Surg Am. 1997;22:328–335. doi: 10.1016/S0363-5023(97)80172-4. [DOI] [PubMed] [Google Scholar]
- 55.Uchiyama S, Amadio PC, Ishikawa J, An KN. Boundary lubrication between the tendon and the pulley in the finger. J Bone Joint Surg Am. 1997;79:213–218. [PubMed] [Google Scholar]
- 56.Uchiyama S, Amadio PC, Coert JH, Berglund LJ, An KN. Gliding resistance of extrasynovial and intrasynovial tendons through the A2 pulley. J Bone Joint Surg Am. 1997;79:219–224. doi: 10.2106/00004623-199702000-00009. [DOI] [PubMed] [Google Scholar]
- 57.Coert JH, Uchiyama S, Amadio PC, Berglund LJ, An KN. Flexor tendon-pulley interaction after tendon repair. A biomechanical study. J Hand Surg Br. 1995;20:573–577. doi: 10.1016/s0266-7681(05)80113-5. [DOI] [PubMed] [Google Scholar]
- 58.Schuind F, Garcia-Elias M, Cooney WP, An KN. Flexor tendon forces: in vivo measurements. J Hand Surg Am. 1992;17:291–298. doi: 10.1016/0363-5023(92)90408-h. [DOI] [PubMed] [Google Scholar]
- 59.Deffino HL, Barbieri CH, Velludo MA. The fate of tendon grafts used to reconstruct the digital annular pulleys. J Hand Surg Br. 1991;16:40–46. doi: 10.1016/0266-7681(91)90125-8. [DOI] [PubMed] [Google Scholar]
- 60.Gabl M, Reinhart C, Lutz M, Bodner G, Angermann P, Pechlaner S. The use of a graft from the second extensor compartment to reconstruct the A2 flexor pulley in the long finger. J Hand Surg Br. 2000;25:98–101. doi: 10.1054/jhsb.1999.0278. [DOI] [PubMed] [Google Scholar]
- 61.Widstrom CJ, Doyle JR, Johnson G, Manske PR, McGee R. A mechanical study of six digital pulley reconstruction techniques: Part II. Strength of individual reconstructions. J Hand Surg Am. 1989;14:826–829. doi: 10.1016/s0363-5023(89)80083-8. [DOI] [PubMed] [Google Scholar]
- 62.Widstrom CJ, Johnson G, Doyle JR, Manske PR, Inhofe P. A mechanical study of six digital pulley reconstruction techniques: Part I. Mechanical effectiveness. J Hand Surg Am. 1989;14:821–825. doi: 10.1016/s0363-5023(89)80082-6. [DOI] [PubMed] [Google Scholar]
- 63.Schöffl V, Küpper T, Hartmann J, Schöffl I. Surgical repair of multiple pulley injuries--evaluation of a new combined pulley repair. J Hand Surg Am. 2012;37:224–230. doi: 10.1016/j.jhsa.2011.10.008. [DOI] [PubMed] [Google Scholar]
- 64.Lister G. Indications and techniques for repair of the flexor tendon sheath. Hand Clin. 1985;1:85–95. [PubMed] [Google Scholar]
- 65.Moutet F, Forli A, Voulliaume D. Pulley rupture and reconstruction in rock climbers. Tech Hand Up Extrem Surg. 2004;8:149–155. doi: 10.1097/01.bth.0000128545.94060.99. [DOI] [PubMed] [Google Scholar]
- 66.Kleinert HE, Kutz JE, Atasoy E, Stormo A. Primary repair of lacerated flexor tendons in "no-man´s land". J Bone Joint Surg (A) 1973;49:577. [Google Scholar]
- 67.Schoffl I, Einwag F, Strecker W, Hennig F, Schoffl V. Impact of taping after finger flexor tendon pulley ruptures in rock climbers. J Appl Biomech. 2007;23:52–62. doi: 10.1123/jab.23.1.52. [DOI] [PubMed] [Google Scholar]
- 68.Buck-Gramcko D, Dietrich FE, Gogge S. [Evaluation criteria in follow-up studies of flexor tendon therapy] Handchirurgie. 1976;8:65–69. [PubMed] [Google Scholar]
- 69.Bunnell S. Surgery of the Hand. JB Lippincott: Philadelphia; 1944. p. 315. [Google Scholar]