Abstract
AIM: To develop a better understanding of scapulohumeral rhythm during scapular plane shoulder elevation.
METHODS: Thirteen healthy, college-aged subjects participated in this study. Subjects were free from any upper extremity, neck or back pathology. A modified digital inclinometer was utilized to measure scapular upward rotation of the subject’s dominant shoulder. Upward rotation was measured statically as subjects performed clinically relevant amounts of shoulder elevation in the scapular plane. Testing order was randomized by arm position. Scapular upward rotation was assessed over the entire arc of motion and over a series of increments. The percent contributions to shoulder elevation for the scapula and glenohumeral joint were calculated. Scapulohumeral rhythm was assessed and represented the ratio of glenohumeral motion to scapulothoracic motion (glenohumeral elevation: scapular upward rotation). A one-way ANOVA was used to compare scapular upward rotation between elevation increments.
RESULTS: Scapulohumeral rhythm for the entire arc of shoulder elevation was equal to a ratio of 2.34 :1 and ranged from 40.01:1 to 0.90:1 when assessed across the different increments of humeral elevation. Total scapular motion increased over the arc of shoulder elevation. The scapula contributed 2.53% of total motion for the first 30 degrees of shoulder elevation, between 20.87% and 37.53% for 30o-90o of shoulder elevation, and 52.73% for 90o-120o of shoulder elevation. Statistically significant differences in scapular upward rotation were identified across the shoulder elevation increments [F(3,48) = 12.63, P = 0.0001].
CONCLUSION: Clinically, we must recognize the usefulness of the inclinometer in documenting the variable nature of scapulohumeral rhythm in healthy and injured shoulders.
Keywords: Biomechanics, Kinematics, Scapula, Shoulder
INTRODUCTION
Optimal function of the shoulder is reliant on the coordinated movement of the scapula and the humerus[1]. Alterations in scapular position and control afforded by the scapula stabilizing muscles are believed to disrupt stability and function of the glenohumeral joint[1-3], thereby contributing to shoulder impingement, rotator cuff pathology and shoulder instability[4]. Given the role of the scapula in shoulder function, the ability to monitor the coordinated motion of the scapula and humerus, or scapulohumeral rhythm[5,6], may have clinical implications when dealing with overhead athletes and patients with shoulder pathologies.
Inman, Saunders and Abbott[7] were the first to measure scapulohumeral rhythm using radiography and suggested what became the widely accepted 2:1 ratio between glenohumeral elevation and scapulothoracic upward rotation (SUR). Since then imaging modalities (X-ray and magnetic resonance imaging)[8], cinematography[9], goniometry[10-12], and more recently 3-dimensional tracking systems[13-16] have been used to gain a better appreciation of shoulder kinematics. This evolution in kinematic assessment has resulted in new understandings of scapulohumeral rhythm in both healthy and injured populations. Some of the literature suggests the 2:1 ratio is not consistent across an entire arc of shoulder elevation[8-10,17,18] and that variability in this ratio may increase when considering the scapulohumeral rhythm exhibited by shoulder injured subjects[19,20].
Instrumentation accessibility has often precluded clinicians from being able to quantify glenohumeral and scapulothoracic joint contributions to scapulohumeral rhythm. Whether we consider exposure to electromagnetic radiation associated with radiography or the expense and time intensive nature of electromagnetic tracking systems, there are some limitations associated with quantifying the relative contributions of the glenohumeral and scapulothoracic joints to shoulder elevation in clinical settings. To enhance accessibility, Johnson et al[12] validated use of a digital inclinometer to quantify SUR, which has since been incorporated into a variety of clinically oriented research studies[21-27]. While many studies involving digital inclinometers have been successful in quantifying SUR, no studies involving digital inclinometers have attempted to examine scapulohumeral rhythm specifically. Although the aforementioned studies provide valuable information relative to scapulothoracic joint motion, return to activity following shoulder injury is dependent on function of both the scapulothoracic and the glenohumeral joint, and how both joints function together. The ability to utilize the inclinometer for quantifying scapulohumeral rhythm will provide clinicians with a means to monitor the often variable nature of scapulohumeral rhythm while also comparing the functional capacity of the shoulder to the established 2:1 scapulohumeral movement ratio. Therefore, the purpose of this study was to develop a better understanding of the coordinated movement of the scapula and humerus in order to enhance the evaluation and rehabilitation efforts of clinicians. We hypothesized that the coordinated movement of the scapula and humerus as measured by a digital inclinometer, would be different than the widely accepted 2:1 scapulohumeral rhythm ratio (glenohumeral:scapulothoracic motion) initially described by Inman[7]. Furthermore, we hypothesized that scapular contributions to incremental increases in glenohumeral elevation would not be consistent.
MATERIALS AND METHODS
Subjects
Thirteen healthy subjects (21.46 ± 1.13 years, 1.76 ± 0.11 meters, 76.18 ± 12.57 kg; 8 male, 5 female; 11 right, 2 left) were recruited to participate in this study. All subjects completed an informed consent document approved by the University’s Institutional Review Board. Participants provided demographic data and completed a health history questionnaire. Subjects also underwent a brief physical examination, which involved measures of shoulder range of motion, strength normalized to body weight, and a subset of evaluative special tests to ensure a healthy dominant shoulder free of any current or previous upper extremity, neck or back injuries or conditions that would result in muscle weakness or reduced shoulder range of motion. The dominant shoulder was selected based upon which hand subjects chose to throw a ball with and sign their name.
Instrumentation
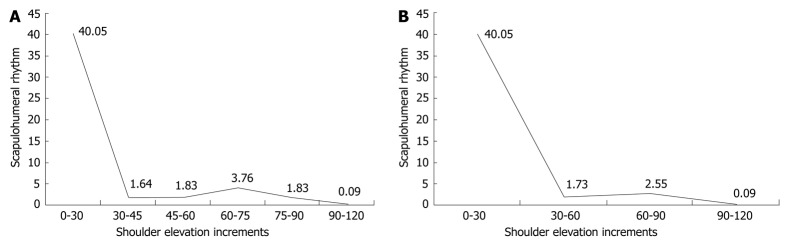
A digital inclinometer (Pro 360, Baseline®, Fabrication Enterprises, White Plains, NY) was used to assess scapular upward rotation during static humeral elevation trials. Using an electromagnetic tracking system, Johnson et al[12] validated use of the digital inclinometer to quantify SUR associated with varying amounts of humeral elevation (r = 0.66 to 0.89). A series of modifications were made to the inclinometer, consistent with the work of Johnson et al, to make it suitable for measuring SUR. Specially designed wooden locator rods were used with the inclinometer in order to appropriately align the inclinometer with the contours of the scapular spine. A custom made plate (Lexan, SABIC Innovative Plastics, Pittsfield, MA) was attached to the inclinometer, allowing for adjustable spacing of the rods (Figure 1A and B). Each locator rod was attached to the Lexan plate using hardware. A bubble level was also affixed to the inclinometer to maintain its position perpendicular orientation relative to the horizontal plane of the inclinometer[12]. With the modifications the inclinometer was aligned with the root of the spine of the scapula and the posterolateral corner of the acromion process[12].
Figure 1.
Modified digital inclinometer (A) and scapular upward rotation measurement (B).
A hand held dynamometer (ergoFET 300, Hogan Health Industries©, West Jordon, UT) was used to assess maximal strength during the initial screening process. Maximal strength tests for shoulder flexion, abduction, and internal and external rotation were performed according to the manual muscle testing guidelines presented by Hislop and Montgomery[28]. When applying the manual resistance for each test the hand held dynamometer was used in order to obtain force measures. Two trials were performed for each shoulder motion; means were calculated and were normalized to body weight.
Intervention
Subjects were seated on a plastic stool one arm’s length from a stationary screen. Subjects were seated to minimize compensatory changes of the lower extremity and trunk, which could impact shoulder biomechanics. Subjects were asked to move their hands to selected points along the screen that corresponded to specific shoulder ranges of motion (rest, 30o, 45o, 60o, 75o, 90o, 120o) in the scapular plane. Shoulder ranges of motion were monitored with a digital inclinometer and hand placement was marked on the screen for each of the respective shoulder ranges of motion. The reliability and validity of our humeral elevation protocol was established previously in our laboratory using an electromagnetic tracking system. When performing humeral elevation in the scapular plane, our intra-session reliability ranged from ICC(3,1) = 0.935 to ICC(3,1) = 0.947, while scapular kinematic reliability ranged from ICC(3,1) = 0.964 to ICC(3,1) = 0.999. Similarly, we were able to report significant correlations between the electromagnetic tracking system and the digital inclinometer for shoulder elevation in the scapular plane with Pearson correlation coefficients ranging from 0.846 to 0.986. In addition to having used the inclinometer as part of a previous study to measure scapular upward rotation, intra-rater reliability for the primary investigator has been determined to be excellent when used to quantify scapular rotation [ICC(3,1) = 0.951 to ICC(3,1) = 0.996] with the inclinometer.
Testing order was randomized by arm position for each subject. Subjects began with their dominant hand at his/her side and were then asked to move their hand to a selected position and to hold that position while SUR was measured. Each trial lasted 10-15 s, and subjects were provided with 5-10 s rest in between each trial. For all inclinometer measures, the primary investigator relied on palpation to identify the position of the medial border and spine of the scapula and the posterolateral corner of the acromion. The primary investigator was responsible for all measures taken with the inclinometer. The inclinometer was repositioned each trial, and inclinometer values were confirmed and recorded by a laboratory assistant for each trial to eliminate investigator bias.
Statistical analysis
Means and standard deviations were calculated for the demographic data. Mean scapular rotation was calculated at 15 and 30 degree increments. Scapular motion was examined over several increments (Table 1).
Table 1.
Humeral elevation increments, mean scapular upward rotation measures, and scapulohumeral rhythm ratios
| Shoulder elevation increments | Mean scapular upward rotation (± SD) | Scapulohumeral rhythm |
| 0o-120o | 35.95 (6.50) | 2.34:1 |
| 0o-30o | 0.73 (4.91) | 40.05:1 |
| 30o-60o | 10.99 (7.18) | 1.73:1 |
| 60o-90o | 8.45 (6.17) | 2.55:1 |
| 90o-120o | 15.78 (7.01) | 0.90:1 |
| 0o-30o | 0.73 (4.91) | 40.05:1 |
| 30o-45o | 5.69 (2.33) | 1.64:1 |
| 45o-60o | 5.29 (6.15) | 1.83:1 |
| 60o-75o | 3.15 (3.67) | 3.76:1 |
| 75o-90o | 5.29 (5.83) | 1.83:1 |
| 90o-120o | 15.78 (7.01) | 0.09:1 |
For each shoulder elevation increment mean ± SD were calculated for scapular upward rotation. Scapular rotation was subtracted from each 15, 30, or 120 degree increment to determine glenohumeral contribution to shoulder elevation. Using the glenohumeral and scapular rotation values, scapulohumeral rhythm (glenohumeral:scapular) was calculated for each increment. SD represents standard deviation.
Scapulohumeral rhythm was calculated using both the 15 degree and 30 degree increments by subtracting scapular rotation from shoulder elevation to determine glenohumeral joint contribution to shoulder elevation (Equation 1). The ratio of glenohumeral motion to scapular motion was then calculated to derive scapulohumeral rhythm (Equation 2).
(Eq. 1) Glenohumeral motion = (Total shoulder motion) - (scapular upward rotation)
(Eq. 2) Scapulohumeral rhythm = (Glenohumeral elevation)/(Scapular upward rotation)
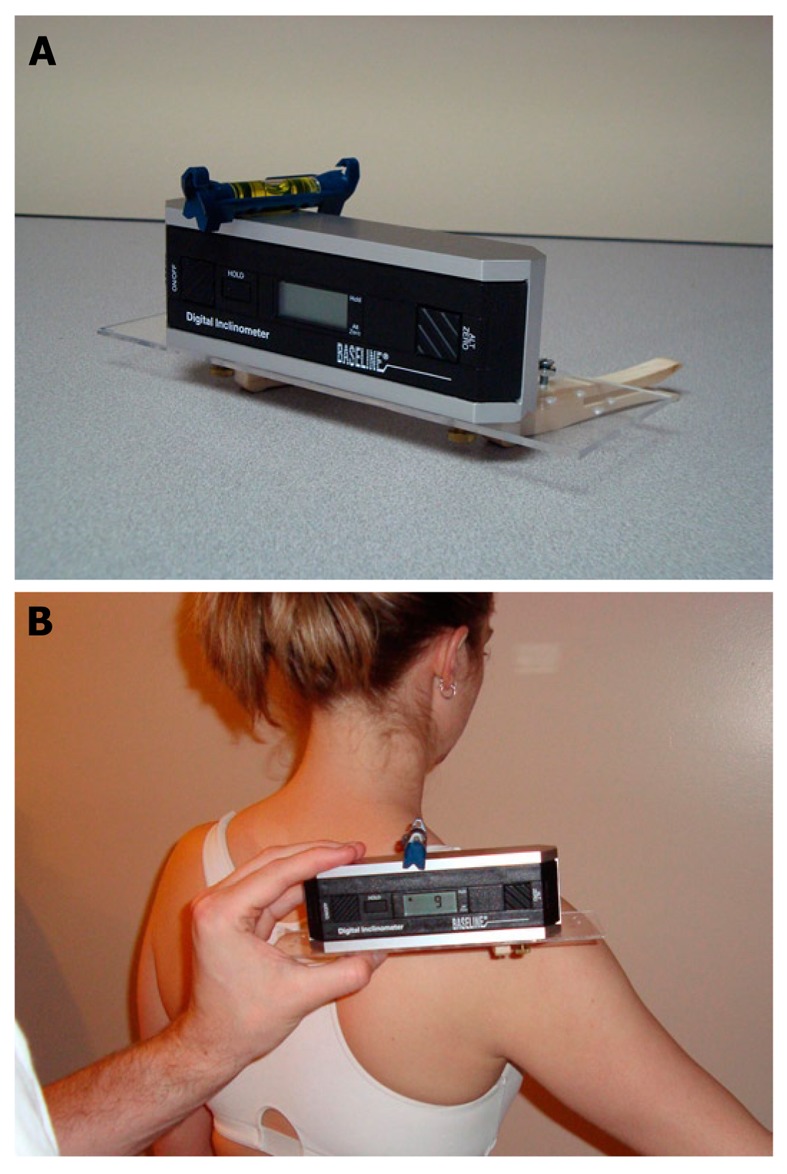
Figure 2.
Scapulohumeral rhythm for 15 shoulder elevation increments (A) and 30 degree shoulder elevation Increments (B). Shoulder elevation increments represent degrees of shoulder elevation in the scapular plane. Values listed in the figure represents degrees of glenohumeral motion for every 1o of scapular upward rotation.
Scapular contributions to shoulder elevation were calculated and percent contributions were calculated according to the aforementioned increment (Equation 3).
(Eq. 3)% Contribution Scapula = (Scapular rotation)/(Total shoulder elevation).
Figure 3.
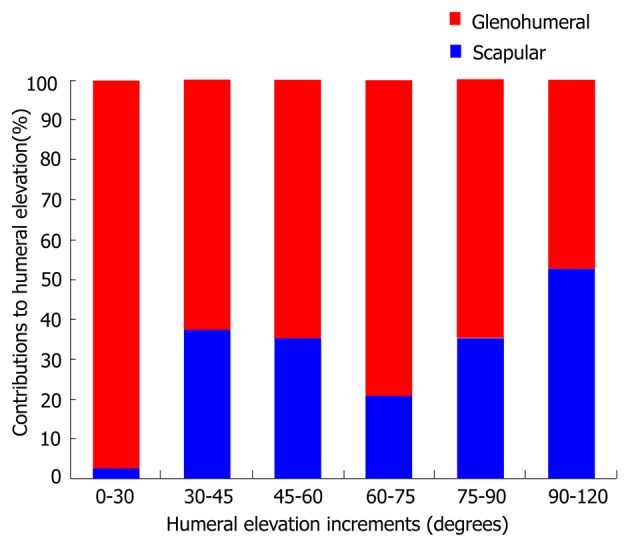
Glenohumeral and scapular upward rotation contributions to shoulder elevation.
Excel (Microsoft, Redmond, WA) and SPSS version 17.0 (IBM Corporation, Armonk, NY) were used for all statistical analyses. A one-way ANOVA was performed to compare mean SUR between 30 degree elevation increments. A Bonferroni t-test was used to address multiple comparisons between the elevation increments. An α = 0.05 was set a priori.
RESULTS
Means and standard deviations for shoulder ranges of motion and strength are provided in Table 2. Ranges of shoulder motion and strength were within clinically acceptable normal limits and were representative of subjects reporting healthy shoulders.
Table 2.
Dominant shoulder range of motion and normalized strength
| Active range ofmotion (± SD) | Passive range of motion (± SD) | Normalized strength (%) (± SD) | |
| Flexion | 175.86o (7.04o) | 179.86o (0.53o) | 19.29 (4.80) |
| Abduction | 179.07o (1.86o) | 180.00o (0.00o) | 18.53 (3.90) |
| Internal rotation | 52.43o (12.11o) | 60.21o (13.72o) | 17.25 (4.43) |
| External rotation | 107.79o (7.78o) | 129.14o (11.95o) | 12.54 (3.37) |
The assessment of scapulohumeral rhythm across the entire arc of humeral elevation was very consistent with the 2:1 ratio defined by Inman. Scapulohumeral rhythm for the observed range represented a ratio of 2.34:1. However, when assessing scapulohumeral rhythm across the different increments of humeral elevation ratios ranged from 40.01:1 to 0.90:1. Following minimal contributions from the scapula during the first 30 degrees of humeral elevation mean scapulohumeral rhythm ratios when assessed over 15 and 30 degree increments ranged from 0.90:1 to 3.76:1 (Figure 2 A and B).
Total scapular motion increased over the arc of shoulder elevation. Contributions of the scapula to overall shoulder elevation were initially minimal when considering the first 30 degrees of shoulder elevation. These contributions continued to increase by varying degrees over the course of shoulder elevation. However, these increases did not appear to occur in a linear fashion. Assessing the scapula’s percent contributions to shoulder elevation across all subjects provided confirmation of this non-linear trend. Percent contributions of the scapula to shoulder elevation were substantially lower for the first 30 degrees of elevation, representing only 2.53% of the first 30 degrees of shoulder elevation. When examining 15o increments of shoulder elevation ranging from 30o to 90o, scapular rotation contributed between 20.87% and 37.53% to total shoulder motion. These contributions were not consistent across increments, and this trend continued when examining the increased scapular contributions percentage from 90o to 120o of elevation which reached 52.73% of total shoulder motion (Figure 3).
Statistically significant differences in scapular upward rotation were identified across the shoulder elevation increments [F(3,48) = 12.63, P = 0.0001]. The Boneferoni assessment revealed multiple significant differences between the 30 degree increments (Table 3). Differences in scapular rotation were not assessed for the 15 degree humeral elevation increments as this data was only obtained for a portion of the humeral elevation arc (30o-90o).
Table 3.
Multiple comparisons analyzing scapular upward rotation per 30 degree increments of shoulder elevation
| Increment1 | Increment2 | Mean difference | Significance | 95% confidence interval |
| 0o-30o | 30o-60o 1 | -10.26 | 0.001 | -17.14; -3.37 -14.60; -0.83 -21.94; -8.17 |
| 60o-90o 1 | -7.72 | 0.02 | ||
| 90o-120o 1 | -15.05 | ≤ 0.001 | ||
| 30o-60o | 0o-30o 1 | 10.26 | 0.001 | 3.37; 17.14 |
| 60o-90o | 2.54 | 1 | -4.35; 9.42 | |
| 90o-120o | -4.8 | 0.367 | -11.68; 2.09 | |
| 60o-90o | 0o-30o 1 | 7.72 | 0.02 | 0.83; 14.60 |
| 30o-60o | -2.53 | 1 | -9.42; 4.35 | |
| 90o-120o 1 | -7.33 | 0.031 | -14.22; -0.45 | |
| 90o-120o | 0o-30o 1 | 15.05 | ≤ 0.001 | 8.17; 21.94 |
| 30o-60o | 4.8 | 0.367 | -2.09; 11.68 | |
| 60o-90o 1 | 7.33 | 0.031 | 0.45; 14.22 |
One-way ANOVA revealed a statistically significant difference between 30 degree shoulder elevation increments for scapular rotation [F(3,48)= 12.63, P ≤ 0.0001]. Boneferoni t-tests revealed statistically significant differences. 1for scapular rotation between 30 degree elevation increments.
DISCUSSION
We were able to quantify the contributions of scapular upward rotation to shoulder elevation occurring in the scapular plane and we were able to provide evidence, using clinically available instrumentation, that scapulohumeral rhythm, as it relates to scapular upward rotation, does not conform entirely to the often accepted 2:1 ratio described by Inman[7]. While the overall ratio of 2.34:1 is in close agreement with the accepted norm, incremental observations of scapulohumeral rhythm were more consistent with recent observations, which are not entirely consistent with the 2:1 ratio[17,29,30]. We also observed increasingly more scapular upward rotation as the shoulder achieved greater amounts of elevation in the scapular plane, which is consistent with the scapula’s role as it relates to optimizing function of the glenohumeral joint during overhead activity. Much like scapulohumeral rhythm, upward rotation contributions of the scapula to shoulder elevation varied across the arc of shoulder elevation, which is both consistent with previous reports[23,26,31] and provides support for use of the digital inclinometer in clinical settings to effectively monitor scapular motion as part of both injury evaluation and rehabilitation.
The scapulohumeral rhythm ratios we observed ranged from 40:1 to 0.90:1. Although our results relative to scapulohumeral rhythm across the entire range of motion are in fairly close agreement with the 2:1 ratio suggested by Inman et al[7], the 2:1 ratio is an average that does not represent the substantial variability observed throughout the range. The exceptionally high ratio obtained during the first 30 degrees of humeral elevation is consistent with the scapular setting phase that is often described when discussing shoulder kinematics and confirmed the observations of some investigators[8,10,17]. The observed ratio not only suggests that the scapula engages in a minimal amount of upward rotation, but rather that during the initial stages of shoulder elevation a period of downward rotation may be encountered. Borsa et al[26] reported a similar decline in upward rotation during the first 30o of shoulder elevation in the scapular plane. It is unclear what may have caused this downward rotation and while it is beyond the scope of our study it is plausible that weakness of the scapula stabilizing muscles may have contributed to the observed pattern. Following the setting phase, scapulohumeral rhythm approached the norms of scapulohumeral rhythm in a fashion consistent with what others have presented[17,29,30,32-34]. Scapulohumeral rhythm ratios between 30o and 90o ranged from 1.64:1 to 3.76:1; but none were equal to the clinically accepted 2:1 ratio. We then observed a decline in scapulohumeral rhythm (0.90:1) as subjects elevated their shoulders from 90o to 120o of elevation. This decline in scapulohumeral rhythm adds to the degree of heterogeneity in the literature as it relates to scapulohumeral rhythm at higher ranges of shoulder elevation[8-10,17,26,29-31]. However, our results are more consistent with those investigators that have indicated that scapulohumeral rhythm ranges between a 1:1 and 2:1 ratio[8-10,17,18,29,30,32-35]. Factors that could explain this observed shift include increases in inferior glenohumeral ligament tension[34], required positioning of the scapula to maintain function and stability of the glenohumeral joint, and maintenance of the subacromial space to avoid impingement[4].
We observed increases in total scapular upward rotation as the level of shoulder elevation increased; however, these increases varied considerably between observed increments. Over the arc of shoulder elevation the scapula encountered 35.95o of upward rotation, resulting in a scapulohumeral rhythm of 2.34:1. Consistent function of the shoulder complex relies on reliable patterns of scapular and glenohumeral motion during shoulder elevation and lowering to ensure optimal stability and mobility[29,31]. The relative increase in scapular upward rotation is similar to both what has been observed with electromagnetic tracking systems[17,29,31-34] and modified digital inclinometers[12,21-27]. Although we noted a relative overall increase in scapular upward rotation, we identified significant differences in scapular rotation between 30 degree shoulder elevation increments, which served to support our secondary hypothesis. The results of Witwer and Sauer[23] and Borsa et al[23,26,31] relative to scapular upward rotation and Borstad and Ludewig[33] specific to scapular tilting foreshadowed our findings with each noting differences or variability in scapular motion when comparing increments of shoulder elevation. The differences we observed between the 0o-30o increment and all other increments are logical given the limited degree to which the scapula moved during the setting phase. Given the often reported stability in scapulohumeral motion between 30o and 90o it is not surprising that differences were not noted between the 30o-60o and 60o-90o increments. It is, however, interesting that the 90o-120o increment was not different when compared to all other increments in light of the scapulohumeral rhythm shift often observed when shoulder elevation occurs above 90o. One factor that may have contributed is the slightly higher relative variability in scapular rotation measures for the 30o-60o increment. This pattern in variability is not unlike what has been reported in other studies[23,26,31] and may have contributed to the lack of significant differences between the 30o-60o and 90o-120o increments. Ultimately, the pattern of scapular rotation we observed during shoulder elevation is similar to what clinicians might observe including (1) a scapular setting phase with little scapular rotation; (2) a relative but inconsistent increase in scapular contributions to shoulder elevation; followed finally by (3) increasingly more upward rotation of the scapula, which mirrors that of the humerus.
Contributions of the scapula to shoulder elevation reflected both inconsistencies in scapulohumeral rhythm and variable scapular upward rotation contributions to shoulder elevation. Again, the contributions of the scapula to shoulder elevation increments 0o-30o and 90o-120o were comparable to what has been reported in the literature, with the scapula contributing 2.53% and 52.73% of the total shoulder elevation, respectively. Examining the shoulder elevation arc incrementally from 30o to 90o, we noted fluctuations in percent scapular contributions to shoulder elevation, which mirrored the inconsistent patterns of scapulohumeral rhythm we observed. In order to be consistent with the 2:1 ratio scapular contributions needed to account for 33.33% of each increment while the glenohumeral joint accounted for the remaining 66.67%. The 15 degree increments 30o-45o, 45o-60o and the 75o-90o and the 30 degree increments (30o-60o and 60o-90o) approached but did not achieve these percent contributions. Reflecting on the scapular contributions across all increments of shoulder elevation, variability in scapular contributions are apparent, which suggests that while the 2:1 ratio may be easy to recall for clinical use, the 2:1 ratio does not accurately portray both scapular contributions and scapulohumeral rhythm observed during shoulder elevation in the scapular plane.
As healthcare and the focus on patient outcomes continue to evolve and our understanding of shoulder kinematics and shoulder pathologies changes as clinicians we must be prepared to add new measures to our clinical repertoires. A number of investigators have examined the contributions of the scapula to shoulder motion in pathologic shoulders using a variety of instruments[19,20,25,35-41], ultimately providing investigators and clinicians with a greater appreciation of scapular kinematics exhibited by various shoulder patient populations. While some have focused on scapulohumeral rhythm and changes in scapular upward rotation, many have expanded their efforts to consider the roles that the secondary scapular rotations (anterior-posterior tilt and medial-lateral tilt)[4] also have in shoulder function and shoulder pathologies. Much of our more recent understandings have come through the use of electromagnetic tracking systems, which are not always clinically viable options. Though visual inspection systems[42,43] may afford us the opportunity to globally identify scapular dysfunction, without the ability to quantify and fully appreciate these patterns in our patients the ability to deliver optimal care may be impacted. Our work and the recent work of others continues to support the clinical usefulness and applicability of the digital inclinometer for quantifying scapular kinematics. As our understanding of scapular kinematics continues to evolve and the needs for patient outcomes relative to these areas changes, the digital inclinometer will continue to provide an affordable and accessible means for quantifying shoulder and scapular kinematics.
Limitations
Even though we were able to demonstrate the clinical usefulness of the digital inclinometer for assessing scapulohumeral rhythm there were some areas of our study that may be viewed as weaknesses or that should be considered in future investigations. In our attempts to be more discriminate in our analysis of scapular kinematics we utilized 15 degree increments throughout the mid-range of the shoulder elevation arc. Unfortunately, we did not utilize this approach across the entire arc of elevation, focusing primarily on clinically relevant angles of shoulder elevation, thus limiting our ability to perform this detailed analysis throughout the observed motion. Future efforts should consider adding additional assessment increments and potentially extending the arc of shoulder elevation beyond 120o. Furthermore, it may have been useful to expand the study and include gender comparisons and bilateral comparison to ensure that the observed pattern occurred similarly in genders and in both the dominant and non-dominant shoulders. Future studies should also consider assessing scapula stabilizing strength at various points in the arc of shoulder elevation to determine if any relationships exist between scapular kinematics and stabilizing muscle strength. The roles of both generalized joint laxity and specifically shoulder ligament laxity should also be considered in future work in order to determine their respective impacts on scapulohumeral rhythm. Additionally, while we were able to call into question the widely accepted 2:1 ratio for scapulohumeral rhythm, greater attention should be directed at determining the clinical meaningfulness of this difference and the extent to which it may contribute to or the role it may have in perpetuating various shoulder pathologies.
In our efforts to gain a better appreciation of the coordinated movements of the scapula and humerus, while using a digital inclinometer we observed scapulohumeral rhythms that were not in total agreement with the widely accepted 2:1 ratio for shoulder elevation. Our observations were confirmed based upon percent contributions of the scapula to shoulder elevation and the significant differences in scapular contribution we noted when comparing shoulder elevation increments. Our findings confirm the presence of a scapular setting phase early in the arc of shoulder elevation, followed by a period of relatively stable scapulohumeral rhythms which then continue to decline as the shoulder moves above 90o of elevation. While our results do not fully support the accepted 2:1 ratio, as investigators and clinicians we must recognize the usefulness of the inclinometer in documenting not only the variable nature of scapulohumeral rhythm in healthy shoulders but the likelihood of increasingly more variant scapulohumeral rhythm patterns exhibited in shoulder injured patients.
ACKNOWLEDGMENTS
The authors would like to thank the Pennsylvania Athletic Trainers Society for providing the financial support (Grant # G0900028) to complete this work. We would also like to thank Colleen Emory, ATC and Molly Hart for their assistance with the data collection.
COMMENTS
Background
The introduction of electromagnetic tracking systems has resulted in an evolution in kinematic assessment as it relates to the understanding of scapulohumeral rhythm in both healthy and injured populations. Electromagnetic tracking systems have improved our understanding of shoulder kinematics; however, instrumentation accessibility has often precluded clinicians from being able to quantify glenohumeral and scapulothoracic joint contributions to shoulder motion. Although, the validation of the digital inclinometer for assessing scapular upward rotation has made scapular kinematic assessment more accessible, no studies involving digital inclinometers have attempted to examine scapulohumeral rhythm specifically.
Research frontiers
The ability to utilize the inclinometer for quantifying scapulohumeral rhythm will provide clinicians with a means to monitor the often variable nature of scapulohumeral rhythm while also comparing the functional capacity of the shoulder to the established 2:1 scapulohumeral movement ratio.
Innovations and breakthroughs
Scapulohumeral rhythm for the entire arc of shoulder elevation was equal to a ratio of 2.34:1 and ranged from 40.01:1 to 0.90:1, which was not entirely consistent with the accepted scapulohumeral rhythm ratio. Although the scapula experienced variable upward rotation throughout the arc of shoulder elevation, our findings confirmed the presence of a scapular setting phase early in the arc of shoulder elevation, followed by a period of relatively stable scapulohumeral rhythms, which proceeded to decline as the shoulder moved above 90o of elevation.
Applications
The significance of the study is that investigators and clinicians should consider the usefulness of the inclinometer in documenting the variable nature of scapulohumeral rhythm in healthy shoulders and shoulder injured patients.
Terminology
Scapulohumeral rhythm: the coordinated motion of the scapula and humerus experienced during shoulder movement and motion that has been traditionally viewed as occurring at a ratio of 2:1 (2 degrees of humeral flexion/abduction to 1 degree of scapular upward rotation).
Peer review
A modified digital inclinometer was used to measure scapular upward rotation of the subject’s dominant shoulder. The authors concluded that the scapulohumeral rhythms measured by a modified digital inclinometer were not consistent with the widely accepted 2:1 ratio for shoulder elevation. Future research should consider the role of hand dominance, gender, and ligamentous laxity as it relates to scapulohumeral rhythm.
Footnotes
Supported by Pennsylvania Athletic Trainers’ Society Research Grant, No. G0900028
Peer reviewers: Nigel Zheng, PhD, Assistant Professor, UNC Charlotte, Duke Centennial Hall 201, 9201 University City Blvd, Charlotte, NC 28223, United States; Olaf Lorbach, MD, Department of Orthopedic Surgery, Saarland University, Kirrberger Str. D-66424 Homburg, Germany
S- Editor Yang XC L- Editor A E- Editor Yang XC
References
- 1.Kibler WB. The role of the scapula in athletic shoulder function. Am J Sports Med. 1998;26:325–337. doi: 10.1177/03635465980260022801. [DOI] [PubMed] [Google Scholar]
- 2.Itoi E. Scapular inclination and inferior stability of the shoulder. J Shoulder Elbow Surg. 1992;1:131–139. doi: 10.1016/1058-2746(92)90090-P. [DOI] [PubMed] [Google Scholar]
- 3.Weiser WM, Lee TQ, McMaster WC, McMahon PJ. Effects of simulated scapular protraction on anterior glenohumeral stability. Am J Sports Med. 1999;27:801–805. doi: 10.1177/03635465990270061901. [DOI] [PubMed] [Google Scholar]
- 4.Ludewig PM, Reynolds JF. The association of scapular kinematics and glenohumeral joint pathologies. J Orthop Sports Phys Ther. 2009;39:90–104. doi: 10.2519/jospt.2009.2808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Codman E. Chapter II: Normal motions of the shoulder. Boston, MA 1934, 32-63. [Google Scholar]
- 6.Lockhart RD. Movements of the Normal Shoulder Joint and of a case with Trapezius Paralysis studied by Radiogram and Experiment in the Living. J Anat. 1930;64:288–302. [PMC free article] [PubMed] [Google Scholar]
- 7.Inman VT, Saunders JB, Abbott LC. Observations of the function of the shoulder joint. 1944. Clin Orthop Relat Res. 1996;330:3–12. doi: 10.1097/00003086-199609000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Poppen NK, Walker PS. Normal and abnormal motion of the shoulder. J Bone Joint Surg Am. 1976;58:195–201. [PubMed] [Google Scholar]
- 9.Bagg SD, Forrest WJ. A biomechanical analysis of scapular rotation during arm abduction in the scapular plane. Am J Phys Med Rehabil. 1988;67:238–245. [PubMed] [Google Scholar]
- 10.Doody SG, Freedman L, Waterland JC. Shoulder movements during abduction in the scapular plane. Arch Phys Med Rehabil. 1970;51:595–604. [PubMed] [Google Scholar]
- 11.Doody SG, Waterland JC, Freedman L. Scapulo-humeral goniometer. Arch Phys Med Rehabil. 1970;51:711–713. [PubMed] [Google Scholar]
- 12.Johnson MP, McClure PW, Karduna AR. New method to assess scapular upward rotation in subjects with shoulder pathology. J Orthop Sports Phys Ther. 2001;31:81–89. doi: 10.2519/jospt.2001.31.2.81. [DOI] [PubMed] [Google Scholar]
- 13.An KN, Browne AO, Korinek S, Tanaka S, Morrey BF. Three-dimensional kinematics of glenohumeral elevation. J Orthop Res. 1991;9:143–149. doi: 10.1002/jor.1100090117. [DOI] [PubMed] [Google Scholar]
- 14.Johnson G, Stuart P, Mitchell S. A method for the measurement of three-dimensional scapular movement. Clin Biomech. 1993;8:269–273. doi: 10.1016/0268-0033(93)90037-I. [DOI] [PubMed] [Google Scholar]
- 15.Meskers CG, Fraterman H, van der Helm FC, Vermeulen HM, Rozing PM. Calibration of the "Flock of Birds" electromagnetic tracking device and its application in shoulder motion studies. J Biomech. 1999;32:629–633. doi: 10.1016/s0021-9290(99)00011-1. [DOI] [PubMed] [Google Scholar]
- 16.van der Helm FCT. A standardized protocol for motion recordings of the shoulder. First Conference of the International Shoulder Group, 1997; Delft, The Netherlands. [Google Scholar]
- 17.Crosbie J, Kilbreath SL, Hollmann L, York S. Scapulohumeral rhythm and associated spinal motion. Clin Biomech (Bristol, Avon) 2008;23:184–192. doi: 10.1016/j.clinbiomech.2007.09.012. [DOI] [PubMed] [Google Scholar]
- 18.Freedman L, Munro RR. Abduction of the arm in the scapular plane: scapular and glenohumeral movements. A roentgenographic study. J Bone Joint Surg Am. 1966;48:1503–1510. [PubMed] [Google Scholar]
- 19.Paletta GA, Warner JJ, Warren RF, Deutsch A, Altchek DW. Shoulder kinematics with two-plane x-ray evaluation in patients with anterior instability or rotator cuff tearing. J Shoulder Elbow Surg. 1997;6:516–527. doi: 10.1016/s1058-2746(97)90084-7. [DOI] [PubMed] [Google Scholar]
- 20.Scibek JS, Mell AG, Downie BK, Carpenter JE, Hughes RE. Shoulder kinematics in patients with full-thickness rotator cuff tears after a subacromial injection. J Shoulder Elbow Surg. 2008;17:172–181. doi: 10.1016/j.jse.2007.05.010. [DOI] [PubMed] [Google Scholar]
- 21.Downar JM, Sauers EL. Clinical Measures of Shoulder Mobility in the Professional Baseball Player. J Athl Train. 2005;40:23–29. [PMC free article] [PubMed] [Google Scholar]
- 22.Laudner KG, Stanek JM, Meister K. Differences in scapular upward rotation between baseball pitchers and position players. Am J Sports Med. 2007;35:2091–2095. doi: 10.1177/0363546507305098. [DOI] [PubMed] [Google Scholar]
- 23.Witwer A, Sauers EL. Clinical measures of shoulder mobility in college water-polo players. J Sport Rehabil. 2006;15:45–57. [Google Scholar]
- 24.Thomas SJ, Swanik KA, Swanik C, Huxel KC. Glenohumeral rotation and scapular position adaptations after a single high school female sports season. J Athl Train. 2009;44:230–237. doi: 10.4085/1062-6050-44.3.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Su KP, Johnson MP, Gracely EJ, Karduna AR. Scapular rotation in swimmers with and without impingement syndrome: practice effects. Med Sci Sports Exerc. 2004;36:1117–1123. doi: 10.1249/01.mss.0000131955.55786.1a. [DOI] [PubMed] [Google Scholar]
- 26.Borsa PA, Timmons MK, Sauers EL. Scapular-Positioning Patterns During Humeral Elevation in Unimpaired Shoulders. J Athl Train. 2003;38:12–17. [PMC free article] [PubMed] [Google Scholar]
- 27.Laudner KG, Stanek JM, Meister K. The relationship of periscapular strength on scapular upward rotation in professional baseball pitchers. J Sport Rehabil. 2008;17:95–105. doi: 10.1123/jsr.17.2.95. [DOI] [PubMed] [Google Scholar]
- 28.Hislop HJ, Montgomery J. Daniel's and Worthingham's Muscle Testing: Techniques of Manual Examination. St. Louis, MO: Saunders;; 2007. [Google Scholar]
- 29.Braman JP, Engel SC, Laprade RF, Ludewig PM. In vivo assessment of scapulohumeral rhythm during unconstrained overhead reaching in asymptomatic subjects. J Shoulder Elbow Surg. 2009;18:960–967. doi: 10.1016/j.jse.2009.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sugamoto K, Harada T, Machida A, Inui H, Miyamoto T, Takeuchi E, Yoshikawa H, Ochi T. Scapulohumeral rhythm: relationship between motion velocity and rhythm. Clin Orthop Relat Res. 2002:119–124. doi: 10.1097/00003086-200208000-00014. [DOI] [PubMed] [Google Scholar]
- 31.Yoshizaki K, Hamada J, Tamai K, Sahara R, Fujiwara T, Fujimoto T. Analysis of the scapulohumeral rhythm and electromyography of the shoulder muscles during elevation and lowering: comparison of dominant and nondominant shoulders. J Shoulder Elbow Surg. 2009;18:756–763. doi: 10.1016/j.jse.2009.02.021. [DOI] [PubMed] [Google Scholar]
- 32.Ludewig PM, Phadke V, Braman JP, Hassett DR, Cieminski CJ, LaPrade RF. Motion of the shoulder complex during multiplanar humeral elevation. J Bone Joint Surg Am. 2009;91:378–389. doi: 10.2106/JBJS.G.01483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Borstad JD, Ludewig PM. The effect of long versus short pectoralis minor resting length on scapular kinematics in healthy individuals. J Orthop Sports Phys Ther. 2005;35:227–238. doi: 10.2519/jospt.2005.35.4.227. [DOI] [PubMed] [Google Scholar]
- 34.Ebaugh DD, McClure PW, Karduna AR. Three-dimensional scapulothoracic motion during active and passive arm elevation. Clin Biomech (Bristol, Avon) 2005;20:700–709. doi: 10.1016/j.clinbiomech.2005.03.008. [DOI] [PubMed] [Google Scholar]
- 35.McClure PW, Bialker J, Neff N, Williams G, Karduna A. Shoulder function and 3-dimensional kinematics in people with shoulder impingement syndrome before and after a 6-week exercise program. Phys Ther. 2004;84:832–848. [PubMed] [Google Scholar]
- 36.Ludewig PM, Cook TM. Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Phys Ther. 2000;80:276–291. [PubMed] [Google Scholar]
- 37.Lukasiewicz AC, McClure P, Michener L, Pratt N, Sennett B. Comparison of 3-dimensional scapular position and orientation between subjects with and without shoulder impingement. J Orthop Sports Phys Ther. 1999;29:574–83; discussion 584-6. doi: 10.2519/jospt.1999.29.10.574. [DOI] [PubMed] [Google Scholar]
- 38.Mell AG, LaScalza S, Guffey P, Ray J, Maciejewski M, Carpenter JE, Hughes RE. Effect of rotator cuff pathology on shoulder rhythm. J Shoulder Elbow Surg. 2005;14:58S–64S. doi: 10.1016/j.jse.2004.09.018. [DOI] [PubMed] [Google Scholar]
- 39.Ogston JB, Ludewig PM. Differences in 3-dimensional shoulder kinematics between persons with multidirectional instability and asymptomatic controls. Am J Sports Med. 2007;35:1361–1370. doi: 10.1177/0363546507300820. [DOI] [PubMed] [Google Scholar]
- 40.Scibek JS, Carpenter JE, Hughes RE. Rotator cuff tear pain and tear size and scapulohumeral rhythm. J Athl Train. 2009;44:148–159. doi: 10.4085/1062-6050-44.2.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vermeulen HM, Stokdijk M, Eilers PH, Meskers CG, Rozing PM, Vliet Vlieland TP. Measurement of three dimensional shoulder movement patterns with an electromagnetic tracking device in patients with a frozen shoulder. Ann Rheum Dis. 2002;61:115–120. doi: 10.1136/ard.61.2.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McClure P, Tate AR, Kareha S, Irwin D, Zlupko E. A clinical method for identifying scapular dyskinesis, part 1: reliability. J Athl Train. 2009;44:160–164. doi: 10.4085/1062-6050-44.2.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tate AR, McClure P, Kareha S, Irwin D, Barbe MF. A clinical method for identifying scapular dyskinesis, part 2: validity. J Athl Train. 2009;44:165–173. doi: 10.4085/1062-6050-44.2.165. [DOI] [PMC free article] [PubMed] [Google Scholar]