Abstract
Background
Many employers are now providing wellness programs to help employees make changes in diet and exercise behaviors. Improving health outcomes and reducing costs will depend on whether employees sustain lifestyle changes and maintain a healthy weight over time.
Purpose
To determine if a 9-month maintenance intervention immediately following a 10-week worksite exercise and nutrition program would prevent regain of the weight lost during the program.
Design
RCT.
Setting/participants
In 2008, a total of 330 employees from 24 teams completed a 10-week exercise and nutrition program at a large hospital worksite and were randomized by team to maintenance or control (usual care) for 9 months.
Intervention
Internet support with a website for goal-setting and self-monitoring of weight and exercise plus minimal personal support.
Main outcome measures
Weight loss, percentage weight loss, time spent in physical activity, and frequency of consumption of fruits/vegetables, fatty foods, and sugary foods at 1 year compared to baseline. One-year follow-up was completed in 2010, and data were analyzed in 2011.
Results
At 1 year, 238 subjects (72%) completed follow-up assessments. Mean baseline BMI was 27.6 and did not differ between intervention and control. Compared to baseline, both groups lost weight during the 10-week program and maintained 65% of weight loss at 1 year (p<0.001). There was no difference in weight loss between groups at end of the 10-week program (4.8 lbs vs 4.3 lbs, p=0.53 for group×time interaction) or end of maintenance at 1 year (3.4 lbs vs 2.5 lbs, p=0.40 for group×time interaction). All subjects had improvements in physical activity and nutrition (increased fruits/vegetables and decreased fat and sugar intake) at 1 year but did not differ by group.
Conclusions
An intensive 10-week team-based worksite exercise and nutrition program resulted in moderate weight loss and improvements in diet and exercise behaviors at 1 year, but an Internet-based maintenance program immediately following the 10-week program did not improve these outcomes.
Introduction
Population-based strategies to prevent excess weight gain are needed to decrease the health and economic burdens of obesity.1–5 In the U.S., adults gain an average of 1–2 pounds per year,6 and reversing this trend will require a multilevel approach.1 Worksite-based wellness programs have potential for preventing obesity among employee populations, and provisions in the Affordable Care Act will encourage more of these programs in the future.7, 8 A systematic review of worksite nutrition and physical activity interventions showed modest short-term weight loss, but few studies have evaluated longer-term interventions for prevention of weight gain in a worksite setting.9
Internet technology for weight gain prevention has potential for use by a large population of workers at relatively low cost over a long period of time.10 Internet-based weight interventions have been successful in some settings11–24 but are most effective when tailored to the individual or combined with personal contact.18, 20, 21, 23, 25 The worksite is ideal for an Internet-based intervention because employees often have computer access and established channels of communication, such as e-mail. Results from studies of worksite-based Internet interventions for weight loss and physical activity are promising but have mixed results.13, 14, 19, 21
A previous evaluation by the authors of a 10-week worksite team-based nutrition and exercise program demonstrated a mean weight loss of 4.2 pounds, but by 1-year follow-up, employees had regained much of the weight.26 The purpose of the current study was to conduct an RCT to test the efficacy of a 9-month Internet-based intervention to prevent weight gain immediately following the 10-week nutrition and exercise program.
Methods
This study received approval from the Partners Healthcare IRB in September 2007.
Setting and Participants
Massachusetts General Hospital (MGH), a teaching hospital in Boston, Massachusetts with over 23,000 employees, offers a 10-week nutrition and physical activity program called “Be Fit” at no cost to employees. The details of this program have been previously described.26 Approximately 150 employees (six teams) participate during each 10-week Be Fit program. The teams meet together weekly at a 30-minute “rally,” and individual teams meet for 45 minutes with a nutritionist and personal trainer.
Teams compete on weekly weight loss, exercise, completion of food logs, and pedometer steps. Participants are taught strategies including goal-setting, self-monitoring, and relapse prevention. All participants receive a free on-site gym membership and personal training sessions and are given a coupon for one healthy meal in the cafeteria per week. Employees were eligible for the current study if they enrolled in one of the four Be Fit programs offered between March 2008 and December 2008. Exclusion criteria included pregnancy or plans to leave employment in the 3 months following enrollment in Be Fit.
Randomization
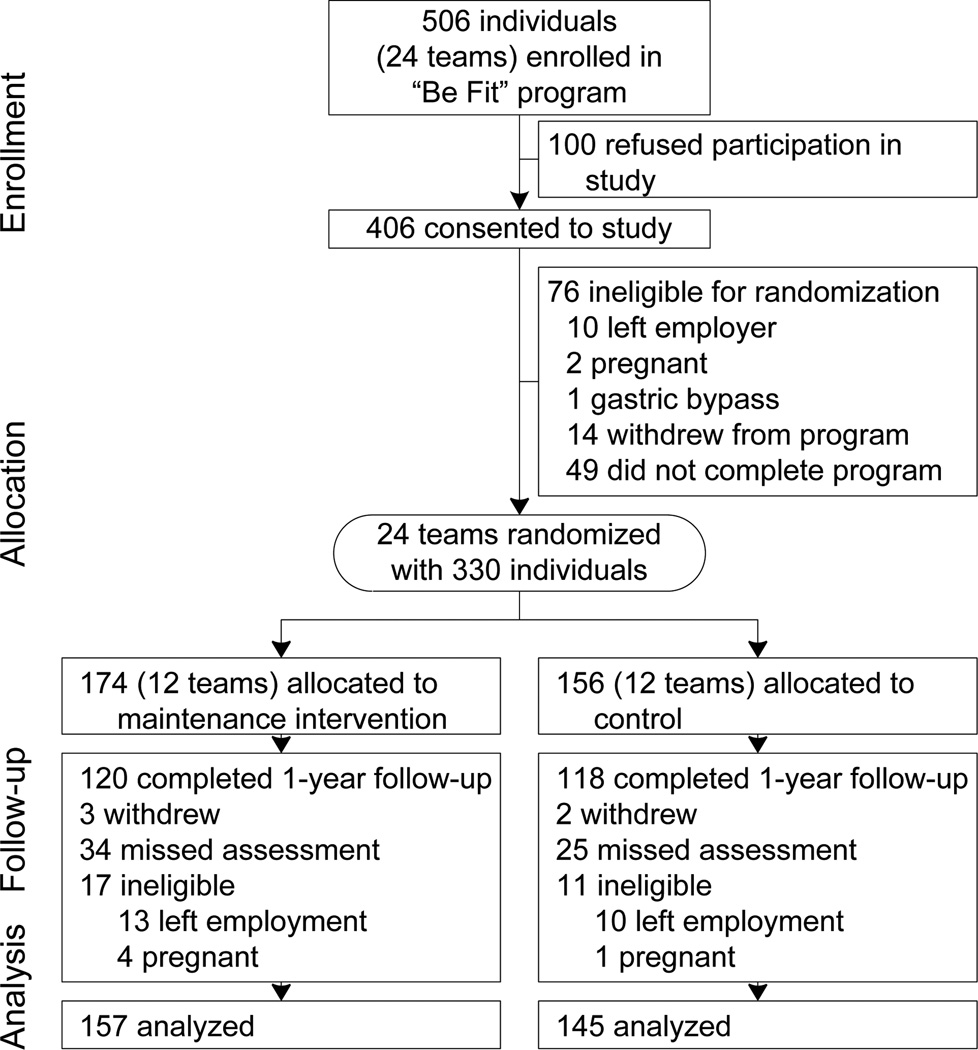
Subjects signed consent prior to starting Be Fit but were not randomized until the end of the program. Subjects who did not complete Be Fit were not eligible to be randomized. Reasons for not completing Be Fit included leaving employment, pregnancy, gastric bypass surgery, or withdrawal or failure to follow-up for unknown reasons (Figure 1). Teams were matched based on a composite index of mean weight loss and proportion of participants attending weekly sessions. One team in each pair was randomly allocated to the intervention or the control arm. A total of 24 teams (six teams from four consecutive Be Fit programs) were randomized.
Figure 1.
Flow of participant recruitment, randomization, and assessment
Intervention
Subjects were notified by e-mail about their randomization assignment. The maintenance program consisted of two components—Internet and personal contact—and was designed to incorporate goal-setting, self-monitoring, and behavioral support.10
Internet contact
Each subject was given access to a website with a personalized web page for the entire 9-month intervention period. Subjects were asked to attend a training session to learn about the website. If a subject could not attend, study staff contacted the individual to offer a more convenient time. When subjects first logged on to the website, they entered their weight, exercise, and nutrition goals for the first 3 months of the maintenance program. Weekly exercise goals included: amount of time spent doing aerobic exercise, number of strength workouts, and average daily pedometer steps. The nutrition goal was the number of food logs the subject aimed to complete weekly. The study nutritionist monitored goals. Subjects were notified by e-mail to set new goals every 3 months.
Subjects were encouraged to log weight, exercise, steps, and food logs at least once a week on a webpage called “Progress Toward Your Goals.” At the end of each week, staff provided short personalized feedback messages on the individual’s page, such as “Keep up the good work with the food logs!” or “It’s not too late to get back on track.” The website also included a page to keep a personal journal and a page with links to exercise and nutrition resources, such as healthy recipes and fitness websites.
Personal contact
Every 3 months during the intervention, subjects were given the option to meet individually with the study nutritionist and/or the personal trainer and were also invited to participate in one lunchtime group seminar. After notification of their randomization assignment, control subjects were not contacted until 1 year follow-up.
Measures and Outcomes
All subjects underwent assessments at baseline, 10 weeks, and 1 year. Assessments were conducted after subjects had fasted for 12 hours. Height was recorded at baseline, and weight, waist circumference, and blood pressure were measured at all visits. Height and weight were measured with clothes on and shoes off. Waist circumference was measured with a flexible tape in the horizontal plane at the level of the iliac crest. The blood pressure machine (Dinamap XL Model 9350) and weight scale (Salter Lithium Electronic scale model 9037) were calibrated monthly.
All subjects completed a survey at baseline, 10 weeks, and 1 year. Subjects reported medications and medical history. Physical activity was assessed by asking participants to estimate: 1) time spent per week during the past 3 months in walking or running, other aerobic exercise, or lower intensity exercise, such as yoga, 2) average flights of stairs climbed daily, and 3) normal walking pace.27 Nutrition behaviors were assessed by estimating the number of times a day over the last month that a participant had eaten the following categories of food: fruits and vegetables, fatty foods and snacks, and sugary foods and drinks. Subjects rated their overall health as “excellent, very good, good, fair, or poor.” For the intervention group, participation was assessed by collecting data on the number of times a participant logged on to the website and the attendance at nutrition appointments, personal trainer appointments, and group seminars.
Data Analysis
Women who became pregnant were excluded from the analyses because weight gain would be expected, and subjects who left employment were excluded because they were unable to participate in the intervention and follow-up as a non-employee. For all other participants who did not follow-up, a baseline observation carried forward method was used to analyze weight and secondary outcomes.
Baseline differences between intervention and control groups were assessed using chi-squared, Wilcoxon rank sum, and t-tests. To assess the effect of the intervention on weight, BMI, waist, blood pressure, cholesterol, and glucose, random-effects regression models were used for panel data with robust SEs adjusted for clustering within team. Intervention effect was modeled as the interaction of study arm and time. Changes in nutrition and exercise behaviors were assessed from baseline to 1 year. Dichotomous variables for food frequency (eating fruits/vegetables ≥ 3 times a day vs <3 times a day; eating fatty foods and snacks never/rarely vs ≥1 time per day; eating sugary foods and drinks never/rarely vs ≥1 time per day), and global health (excellent vs very good or worse) were assessed in individual logistic regression models for panel data with the intervention effect modeled as the interaction of study arm and time. Change in moderate physical activity (excluding walking <3 mph and stretching) was assessed in a chi-squared test. Subgroup analyses were conducted within the intervention arm to assess whether level of exposure to the maintenance program predicted weight loss at 1 year. Participation in the Internet portion was based on number of log-ins, and participation in the personal contact was based on attendance at individual meetings and group seminars. Weight differences at 1 year were assessed by t-tests. All analyses were conducted in 2011 and carried out using Stata statistical software, version 10. A sample size of 355 was calculated accounting for clustering to detect a between- group difference of 2 pounds at 1 year with an 80% power and two-sided 0.05 significance level.
Results
A total of 406 of 506 Be Fit program participants (80%) consented to the study prior to starting the 10-week program, and 330 (81%) were randomized. Twelve teams (174 individuals) were assigned to maintenance intervention and 12 teams (156 individuals) to control (Figure 1). There were 28 subjects (17 intervention and 11 control) who were ineligible for 1-year follow-up and were not included in final analyses. Follow-up rates at 1 year were 76% (120/157) in Intervention and 81% (118/145) in Control (p=0.29).
Table 1 shows baseline characteristics. The intervention group had more women, but otherwise the groups did not have significant differences. Overall, 64% of subjects were overweight or obese. Compared to the 330 randomized subjects, the 76 subjects who were not eligible for randomization had higher baseline BMI (27.6 vs 30.2, p<0.001) and were less likely to be white (83% vs 69%, p=0.01).
Table 1.
Baseline characteristics of subjects randomized to maintenance intervention and control groups
| Intervention group n=174 |
Control group n=156 |
p-valuea | |
|---|---|---|---|
| Age, M (SD) | 44.2 (11.8) | 41.6 (13.6) | 0.06 |
| Gender, % female | 90 | 82 | 0.03 |
| Race, % white | 85 | 80 | 0.22 |
| Education, % with college degree or greater | 94 | 92 | 0.49 |
| Marital status, % married | 63 | 53 | 0.10 |
| Employment for 5 years or greater, % | 51 | 44 | 0.22 |
| Weight category,% Normal weight (BMI<25) Overweight (BMI 25–29.9) Obese (BMI≥30) |
34 39 27 |
38 33 28 |
0.60 |
| Smoking, % Current Past Never |
5 31 64 |
4 27 69 |
0.66 |
| Diagnosis, Hypertension, % |
17 |
19 |
0.62 |
| Hyperlipidemia, % | 19 | 19 | 0.94 |
| Diabetes mellitus, % | 1 | 3 | 0.35 |
| Cardiovascular disease, % | 3 | 1 | 0.30 |
| Amount of physical activity/week, hours, median (IQR) | 2.6 (1–6.0) | 3.5 (1–5.8) | 0.67 |
For differences between groups.
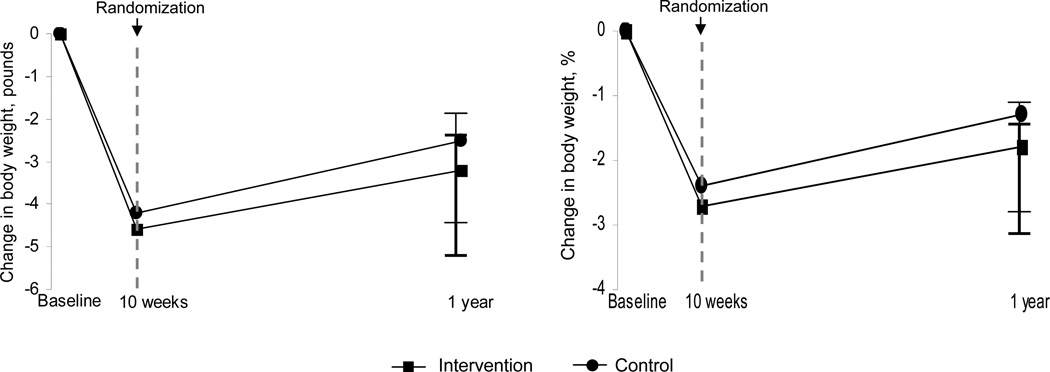
At baseline, intervention and control groups did not differ in weight, BMI, waist, blood pressure, cholesterol, or glucose (p>0.05 for all). Figure 2 shows that intervention and control groups lost similar amounts of weight during the 10-week program (4.8 lbs vs 4.3 lbs, p=0.40) and at 1-year follow up (3.4 lbs vs 2.5 lbs, p=0.39). Percent body weight lost was also similar at 10 weeks (2.7% vs 2.4%, p=0.54) and 1 year (1.8% vs 1.3%, p=0.48). Overall at 1 year, all study participants maintained a mean weight loss of 3.0 (SD 8.8) pounds or 65% of the 4.6 (SD 5.5) pound mean weight loss during the 10-week program.
Figure 2.
Absolute and percentage weight loss in the 10-week program and maintenance intervention
Note: Means estimated at 1 year with a baseline observation carried forward method for missing data. Error bars indicate 95% CIs.
Weight, BMI, waist, and total and low-density lipoprotein cholesterol were lower for both groups at 10 weeks and 1 year (Table 2). Blood pressure was lower for both groups at 10 weeks. There was no effect of group or the interaction between time and group for any of the outcomes.
Table 2.
Change in body composition and cardiovascular risk factors during the 10-week program and maintenance intervention.
| Assessment Period | p-Value | |||||||
|---|---|---|---|---|---|---|---|---|
| Pre-randomization (Be Fit program) |
Post- randomization (Maintenance) |
Time | Group | Time × Group | ||||
|
Outcome variable |
Baseline, M (SD) |
10 weeks, M (SD) |
1 yeara, M (SD) |
10 weeks vs baseline |
1 year vs baseline |
Baseline to 10 weeks |
Baseline to 1 year |
|
|
Weight, lbs Maintenance intervention (n=157) |
169.2 (37.0) | 164.4 (34.8) | 165.8 (35.0) |
<0.001 |
<0.001 |
0.79 |
0.53 |
0.40 |
| Control (n=145) | 167.5 (39.3) | 163.2 (37.8) | 164.9 (38.8) | |||||
|
BMI Maintenance intervention (n=157) |
28.0 (5.8) | 27.2 (5.4) | 27.5 (5.6) |
<0.001 |
<0.001 |
0.62 |
0.49 |
0.31 |
| Control (n=145) | 27.5 (5.9) | 26.8 (5.7) | 27.1 (6.0) | |||||
|
Waist, inches Maintenance intervention (n=157) |
35.1 (5.7) | 33.9 (5.6) | 33.7 (5.8) |
<0.001 |
<0.001 |
0.55 |
0.90 |
0.80 |
| Control (n=145) | 34.5 (6.2) | 33.3 (6.0) | 33.1 (6.3) | |||||
|
Systolic BP, mm Hg Maintenance intervention (n=157) |
124.6 (16.3) | 122.2 (14.7) | 122.6 (16.5) |
<0.001 |
0.10 |
0.37 |
0.22 |
0.70 |
| Control (n=145) | 126.7 (16.2) | 122.2 (15.8) | 125.4 (16.2) | |||||
|
Diastolic BP, mm Hg Maintenance intervention (n=157) |
71.3 (9.0) | 70.4 (8.7) | 70.6 (9.4) |
0.003 |
0.62 |
0.37 |
0.17 |
0.55 |
| Control (n=145) | 72.3 (10.7) | 69.9 (8.5) | 72.2 (10.0) | |||||
|
Total cholesterol, mg/dL Maintenance intervention (n=157) |
188.6 (34.0) | 184.4 (32.7) | 184.4 (33.6) | <0.001 | 0.05 | 0.19 | 0.30 | 0.31 |
| Control (n=145) | 194.3 (33.5) | 187.4 (32.4) | 192.0 (31.2) | |||||
|
LDL cholesterol, mg/dL Maintenance intervention (n=157) |
111.2 (30.1) | 109.4 (28.7) | 107.5 (29.4) |
0.005 |
0.02 |
0.29 |
0.23 |
0.69 |
| Control (n=145) | 115.1 (31.2) | 110.6 (29.6) | 112.1 (29.2) | |||||
|
HDL cholesterol, mg/dL Maintenance intervention (n=157) |
58.1 (13.9) | 57.0 (13.5) | 58.8 (13.9) |
0.20 |
0.16 |
0.29 |
0.74 |
0.97 |
| Control (n=145) | 60.4 (16.4) | 59.5 (16.9) | 61.1 (16.9) | |||||
|
Triglycerides, mg/dL Maintenance intervention (n=157) |
96.5 (49.1) | 90.0 (45.0) | 90.7 (47.1) |
<0.001 |
0.89 |
0.71 |
0.75 |
0.10 |
| Control (n=145) | 93.8 (48.4) | 86.3 (49.7) | 93.5 (50.3) | |||||
|
Fasting serum glucose, mg/dL Maintenance intervention (n=157) |
92.5 (9.7) | 90.5 (10.1) | 89.5 (12.8) |
0.007 |
0.11 |
0.72 |
0.71 |
0.23 |
| Control (n=145) | 93.3 (19.7) | 91.7 (20.8) | 91.7 (22.0) | |||||
Baseline observation carried forward method for missing data.
Overall, subjects reported improved nutrition and exercise behaviors at follow-up. At 1 year compared to baseline, more subjects reported eating fruits and vegetables ≥ 3 times a day (57% vs 38%, p<0.001), and more subjects reported “never/rarely” eating fatty foods and snacks (70% vs 51%, p<0.001) and sugary foods and beverages (42% vs 26%, p<0.001). At 1 year, the time spent in moderate physical activity increased by ≥2 hours per week for 30% of subjects, and the proportion who reported climbing ≥ 5 flights of stairs a day increased from 42% to 49% (p=0.018). More subjects rated their overall health as “excellent” at 1 year compared to baseline (25% vs 13%, p<0.001). One-year changes in nutrition, exercise, and health rating did not differ between control and intervention groups.
In the intervention group, 108 subjects (69%) logged on to the website at least once, and 68 (63%) visited the website ≥5 times. There were 86 subjects (55%) who participated in personal contact by meeting with a study nutritionist and/or personal trainer or attending a seminar. Overall, 116 of the intervention subjects (74%) participated in any aspect (Internet and/or personal contact) of maintenance. These subjects lost more weight at 1 year than intervention subjects who did not participate (4.2 vs 1.2 lbs, p=0.08).
Discussion
In this large worksite, a 10-week team-based exercise and nutrition program was effective for promoting weight loss and exercise and nutrition changes, but a 9-month maintenance intervention immediately following the 10-week program did not improve 1-year outcomes more than usual care. The Internet-based maintenance program did appear to be effective for the subset of participants who actively participated in the program, but overall usage of the website was low. The results of this study have implications for designing future wellness programs to prevent long-term weight gain among employee populations.
In this study, employees participated in a structured 10-week program that not only provided nutrition and exercise education and access to an on-site exercise facility but also took advantage of workplace social networks by creating teams of employees. The maintenance intervention was designed as a tool for participants to continue utilizing self-monitoring, goal-setting, and relapse prevention techniques learned during the 10-week program. Advantages of this Internet-based maintenance intervention included relatively low cost to the employer, flexibility for employees, and potential for use over a long period of time.
It is important to consider possible reasons that the maintenance intervention was not more effective than usual care. After completing the 10-week program, employees may have been less motivated to participate in the less intensive maintenance intervention. Other weight maintenance trials following intensive weight loss programs have had similar findings.11, 20 Although the Internet program in our study was convenient for employees, utilization of the website was relatively low. The SHED-IT trial of an Internet-based weight loss intervention for university employees and students had similar results, with only 41% of participants complying with the online component.14 Other studies of Internet-based weight interventions have found relatively low utilization of the Internet, especially over time.11, 15, 21, 23, 25
The current results should not discourage further study of technology-based interventions at worksites. The Internet is a powerful tool for health behavior change because of its population-level reach, and even small improvements in behaviors can be translated to large public health benefits.10 The current results demonstrate that employees were highly engaged in the 10-week program, but only a few participated in the Internet-based maintenance program. This intervention may have been more effective if it had utilized the social network and team competition aspect of the 10-week program.
There are some limitations to this study. Subjects could not be blinded to their treatment assignment. To minimize contamination between groups, subjects were randomized by team. The actual sample was slightly lower than the original sample size calculation. However, the observed 1-year difference was 0.9 pounds, which was lower than what was considered a clinically important difference.
With rising healthcare costs, employers are initiating wellness programs, but few data are available to guide the design of worksite interventions that will result in sustained improvements in employees’ health. The current study demonstrated that employees who participated in an intensive team-based program over 10 weeks maintained moderate weight and behavior changes at 1 year, but the 9-month Internet-based maintenance program did not result in better outcomes than usual care. Future interventions to prevent long-term weight gain should take advantage of social networks and opportunities for more-personalized contact in the workplace.
Acknowledgments
This project was supported by the NIH/National Heart Lung and Blood Institute grant K23 HL93221 and by Partners Healthcare.
ANT is supported by the NIH/National Heart Lung and Blood Institute grant K23 HL93221.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Erica Healy was employed at Massachusetts General Hospital when this research was completed.
Neither the NIH nor Partners Healthcare had any role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; and preparation, review, or approval of the manuscript.
No other authors reported financial disclosures.
References
- 1.Kumanyika SK, Obarzanek E, Stettler N, et al. American Heart Association Council on Epidemiology and Prevention,Interdisciplinary Committee for Prevention. Population-based prevention of obesity: The need for comprehensive promotion of healthful eating, physical activity, and energy balance: A scientific statement from American Heart Association Council on Epidemiology and Prevention, Interdisciplinary Committee for Prevention. Circulation. 2008;118(4):428–464. doi: 10.1161/CIRCULATIONAHA.108.189702. [DOI] [PubMed] [Google Scholar]
- 2.Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet. 2011;378(9793):815–825. doi: 10.1016/S0140-6736(11)60814-3. [DOI] [PubMed] [Google Scholar]
- 3.Finkelstein EA, Trogdon J, Cohen JW, Dietz W. Annual medical spending attributable to obesity: Payer- and service-specific estimates. Health Affairs. 2009;28:w822–w831. doi: 10.1377/hlthaff.28.5.w822. [DOI] [PubMed] [Google Scholar]
- 4.Sturm R. The effects of obesity, smoking, and drinking on medical problems and costs. Health Aff (Millwood) 2002;21(2):245–253. doi: 10.1377/hlthaff.21.2.245. [DOI] [PubMed] [Google Scholar]
- 5.Thorpe KE, Florence CS, Howard DH, Joski P. The impact of obesity on rising medical spending. Health Aff (Millwood) 2004 doi: 10.1377/hlthaff.w4.480. Suppl Web Exclusives(Suppl Web Exclusives):W4-480-6. [DOI] [PubMed] [Google Scholar]
- 6.Lewis CE, Jacobs DR, Jr, McCreath H, et al. Weight gain continues in the 1990s: 10-year trends in weight and overweight from the CARDIA study. coronary artery risk development in young adults. Am J Epidemiol. 2000;151(12):1172–1181. doi: 10.1093/oxfordjournals.aje.a010167. [DOI] [PubMed] [Google Scholar]
- 7.Baicker K, Cutler D, Song Z. Workplace wellness programs can generate savings. Health affairs. 2010;29(2):1–8. doi: 10.1377/hlthaff.2009.0626. [DOI] [PubMed] [Google Scholar]
- 8.Koh HK, Sebelius KG. Promoting prevention through the affordable care act. N Engl J Med. 2010 doi: 10.1056/NEJMp1008560. 10.1056/NEJMp1008560. [DOI] [PubMed] [Google Scholar]
- 9.Anderson LM, Quinn TA, Glanz K, et al. The effectiveness of worksite nutrition and physical activity interventions for controlling employee overweight and obesity: A systematic review. Am J Prev Med. 2009;37(4):340–357. doi: 10.1016/j.amepre.2009.07.003. [DOI] [PubMed] [Google Scholar]
- 10.Winett RA, Tate DF, Anderson ES, Wojcik JR, Winett SG. Long-term weight gain prevention: A theoretically based internet approach. Prev Med. 2005;41(2):629–641. doi: 10.1016/j.ypmed.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 11.Harvey-Berino J, Pintauro S, Buzzell P, Gold EC. Effect of internet support on the long-term maintenance of weight loss. Obes Res. 2004;12(2):320–329. doi: 10.1038/oby.2004.40. [DOI] [PubMed] [Google Scholar]
- 12.Hunter CM, Peterson AL, Alvarez LM, et al. Weight management using the internet a randomized controlled trial. Am J Prev Med. 2008;34(2):119–126. doi: 10.1016/j.amepre.2007.09.026. [DOI] [PubMed] [Google Scholar]
- 13.Marcus BH, Lewis BA, Williams DM, et al. A comparison of internet and print-based physical activity interventions. Arch Intern Med. 2007;167(9):944–949. doi: 10.1001/archinte.167.9.944. [DOI] [PubMed] [Google Scholar]
- 14.Morgan PJ, Lubans DR, Collins CE, Warren JM, Callister R. The SHED-IT randomized controlled trial: Evaluation of an internet-based weight-loss program for men. Obesity (Silver Spring) 2009;17(11):2025–2032. doi: 10.1038/oby.2009.85. [DOI] [PubMed] [Google Scholar]
- 15.Petersen R, Sill S, Lu C, Young J, Edington DW. Effectiveness of employee internet-based weight management program. J Occup Environ Med. 2008;50(2):163–171. doi: 10.1097/JOM.0b013e31815c6cf6. [DOI] [PubMed] [Google Scholar]
- 16.Tate DF, Jackvony EH, Wing RR. A randomized trial comparing human e-mail counseling, computer-automated tailored counseling, and no counseling in an internet weight loss program. Arch Intern Med. 2006;166(15):1620–1625. doi: 10.1001/archinte.166.15.1620. [DOI] [PubMed] [Google Scholar]
- 17.Herman CW, Musich S, Lu C, Sill S, Young JM, Edington DW. Effectiveness of an incentive-based online physical activity intervention on employee health status. J Occup Environ Med. 2006;48(9):889–895. doi: 10.1097/01.jom.0000232526.27103.71. [DOI] [PubMed] [Google Scholar]
- 18.Rothert K, Strecher VJ, Doyle LA, et al. Web-based weight management programs in an integrated health care setting: A randomized, controlled trial. Obesity (Silver Spring) 2006;14(2):266–272. doi: 10.1038/oby.2006.34. [DOI] [PubMed] [Google Scholar]
- 19.Sternfeld B, Block C, Quesenberry CP, Jr, et al. Improving diet and physical activity with ALIVE: A worksite randomized trial. Am J Prev Med. 2009;36(6):475–483. doi: 10.1016/j.amepre.2009.01.036. [DOI] [PubMed] [Google Scholar]
- 20.Svetkey LP, Stevens VJ, Brantley PJ, et al. Comparison of strategies for sustaining weight loss: The weight loss maintenance randomized controlled trial. JAMA. 2008;299(10):1139–1148. doi: 10.1001/jama.299.10.1139. [DOI] [PubMed] [Google Scholar]
- 21.Tate DF, Wing RR, Winett RA. Using internet technology to deliver a behavioral weight loss program. JAMA. 2001;285(9):1172–1177. doi: 10.1001/jama.285.9.1172. [DOI] [PubMed] [Google Scholar]
- 22.Norman GJ, Zabinski MF, Adams MA, Rosenberg DE, Yaroch AL, Atienza AA. A review of eHealth interventions for physical activity and dietary behavior change. Am J Prev Med. 2007;33(4):336–345. doi: 10.1016/j.amepre.2007.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wing RR, Tate DF, Gorin AA, Raynor HA, Fava JL. A self-regulation program for maintenance of weight loss. N Engl J Med. 2006;355(15):1563–1571. doi: 10.1056/NEJMoa061883. [DOI] [PubMed] [Google Scholar]
- 24.Patrick K, Calfas KJ, Norman GJ, Rosenberg D, et al. Outcomes of a 12-month web-based intervention for overweight and obese men. Ann Behav Med. 2011;42:391–401. doi: 10.1007/s12160-011-9296-7. [DOI] [PubMed] [Google Scholar]
- 25.Tate DF, Jackvony EH, Wing RR. Effects of internet behavioral counseling on weight loss in adults at risk for type 2 diabetes: A randomized trial. JAMA. 2003;289(14):1833–1836. doi: 10.1001/jama.289.14.1833. [DOI] [PubMed] [Google Scholar]
- 26.Thorndike AN, Healey E, Sonnenberg L, Regan S. Participation and cardiovascular risk reduction in a voluntary worksite nutrition and physical activity program. Preventive medicine. 2011;52:164–166. doi: 10.1016/j.ypmed.2010.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wolf AM, Hunter DJ, Colditz GA, et al. Reproducibility and validity of a self-administered physical activity questionnaire. Int J Epidemiol. 1994;23(5):991–999. doi: 10.1093/ije/23.5.991. [DOI] [PubMed] [Google Scholar]