Abstract
Objective
To investigate the use of laboratory tests and which factors influence the use in Norwegian out-of-hours (OOH) services.
Design
Cross-sectional observational study.
Setting
Out-of-hours services in Norway.
Subjects
All electronic reimbursement claims from doctors at OOH services in Norway in 2007.
Main outcome measures
Number of contacts and laboratory tests in relation to patients’ and doctors’ characteristics.
Results
1 323 281 consultations and home visits were reported. Laboratory tests were used in 31% of the contacts. C-reactive protein (CRP) was the most common test (27% of all contacts), especially in respiratory illness (55%) and infants (44%). Electrocardiogram and rapid strep A test were used in 4% of the contacts. Young doctors, female doctors, and doctors in central areas used laboratory tests more often.
Conclusion
CRP is extensively used in OOH services, especially by young and inexperienced doctors, and in central areas. Further investigations are required to see if this extensive use of CRP is of importance for correct diagnosis and treatment.
Key Words: Clinical chemistry tests, CRP, diagnostic tests, emergency medical services, primary health care
A few point-of-care laboratory tests are available for diagnostic use in out-of-hours services in Norway.
A laboratory test was taken in 31% of all consultations/home calls.
C-reactive protein (CRP) was the dominating test (27% of all contacts), and the rate was especially high in small children.
Test use was most frequent in out-of-hours services in central areas and by younger doctors.
Introduction
In Norway every municipality is responsible for the emergency primary health care for their inhabitants and visitors, both during office hours and out-of-hours (OOH). OOH work is with few exceptions compulsory for regular general practitioners (RGPs), but because the duty comes in addition to ordinary work it is often seen as a burden. At least half of the OOH consultations are done by other doctors (ODs) than RGPs [1–3]. The majority of RGPs are qualified specialists in general practice. The ODs may be newly qualified doctors serving a compulsory practice period, or temporary employed doctors who work in the daytime in hospitals or universities. In many rural districts doctors are working at OOH alone from their daytime surgeries, while larger districts usually run casualty clinics staffed with nurses in addition to the doctors. Many municipalities have now organised OOH services as larger inter-municipality cooperatives, and in some cities there are specialized emergency clinics with direct access [4,5].
Generally, the OOH services are well equipped with laboratory and diagnostic instruments. In a previous study we found that all OOH services have at least six point-of-care laboratory tests available. These were C-reactive protein (CRP), haemoglobin, glucose, urine analysis, u-HCG pregnancy test, and rapid Strep A test [6]. Laboratory tests are used in approximately 30% of the OOH consultations [3].
The use of point-of-care testing in primary care has increased for the purpose of reducing the time taken to make decisions on patient management. Thus, the availability of a limited number of laboratory tests is especially welcome for OOH services, with its high patient turnover. Infections and inflammatory conditions are prevalent among patients using OOH services, but with the low prevalence of serious bacterial infections it is challenging to discriminate them from self-limiting illness. CRP is the dominating inflammation marker available at every OOH service while just a few OOH services have cell counters [6].
The aim of the present study was to investigate to what extent laboratory tests are used in OOH services in Norway, and how factors like patients’ and doctors’ characteristics, diagnostic groups, and geography may influence their use. We wanted especially to analyse the usage pattern of the CRP test, which is the most frequently used test.
Material and methods
The material comprises all electronic compensation claims from identified doctors working in OOH services in Norway in 2007. The claims are sent to the Norwegian Health Economics Administration (HELFO) which is responsible for remuneration.
The claims are usually electronically transferred to HELFO, but in 2007 a small proportion were still sent on paper (not included in our material). In 2006 it was estimated that paper-based claims accounted for 4.9% of all contacts with the OOH services [7]. At some OOH services the doctors have a fixed salary, and the compensation claims are registered for the OOH service/municipality, and not for an identified doctor. Some simple consultations are paid in full by the patients, and may not be registered by HELFO if there are no extra fees like fee for laboratory tests or procedures. The extent of underreporting has been estimated at 8% of consultations and home visits in the age group 12 + and almost nothing for younger children because of full reimbursement of all costs [3,7].
We received an anonymous data file from HELFO with the following variables: patient's sex, age, centrality of the municipality, diagnosis, doctor's age, sex, and type (RGP or OD), and the specific fees that were claimed. The centrality is defined as a municipality's geographical location in relation to a centre where there are important functions (central functions) and is measured on a scale of 0–3 where 0 is the least and 3 is the most central [8].
Every claim contains a fee indicating the type of contact (e.g. home visit or consultation in surgery/casualty clinic) and various fees for different procedures. There is one basic fee for all laboratory tests; in addition there are specific fees for different laboratory tests done at the service, except for haemoglobin, sedimentation rate, and urine analysis. All contacts are coded with ICPC2 diagnoses (International Classification for Primary Care).
HELFO and the Privacy Ombudsman for Research (Norwegian social scientific data services) assessed the project. As it is not possible to identify individuals in this material, directly or indirectly, the project was not subject to obligatory notification. The data were analysed in SPSS 18.0 with simple frequencies analysis and cross-tables. In order to evaluate the significance of different doctors’ characteristics a binary logistic regression analysis was performed. The use of a laboratory test (the basic lab fee) per contact for each doctor was used as a dependent variable (dichotomized by the median value 0.2756) and the doctor's age (dichotomized by the median value 38), sex, type of doctor (RGP vs. OD), and centrality (0/1 vs. 2/3) as independent variables to calculate odds ratios with 95% confidence intervals.
Results
The material consisted of 1 240 235 claims for consultations and 83 046 for home visits. RGPs sent 47% of the claims while other doctors sent 53%. Mean age for RGPs was 44 years, for other doctors 38. Female physicians were younger than male physicians (37 vs. 42 years) and sent 22% of the claims.
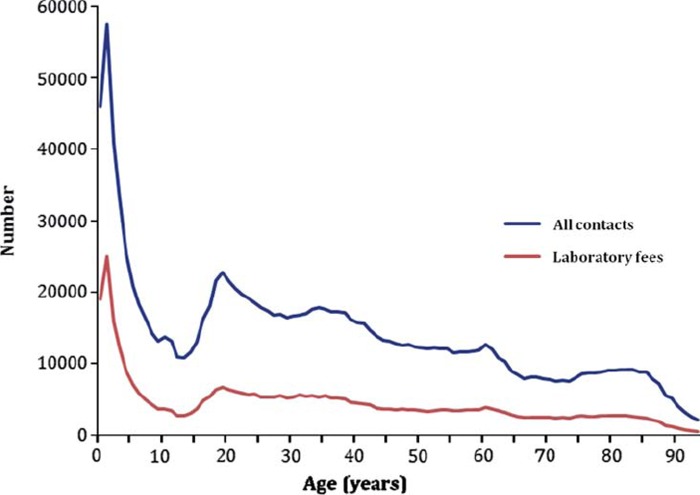
The age distribution of the patients is shown in Figure 1, revealing a peak of contacts for the age group 0–1 year, and a smaller peak around age 20. There were only minor differences in distribution of contacts by gender.
Figure 1.
Distribution of all contacts and laboratory fees by age.
Laboratory/diagnostic tests
Fees for laboratory or diagnostic tests were found in 31% of the contacts (consultations and home visits). The distribution of laboratory claims by age was similar to the distribution of contacts (Figure 1). The absolute numbers of various tests and rates per 1000 contacts are given in Table I.
Table I.
Total numbers of various laboratory tests and numbers per 1000 out-of-hours contacts (n = 1 323 281 consultations or home visits).
| Laboratory test | n | Per 1000 contacts |
| Any laboratory test | 411 170 | 311 |
| C-reactive protein (CRP) | 361 905 | 273 |
| Electrocardiogram | 55 527 | 42 |
| Rapid strep A test | 53 524 | 40 |
| Glucose | 24 741 | 19 |
| Secondary test to external laboratory | 16 242 | 14 |
| Pregnancy test (urine HCG) | 9212 | 7 |
| Haematological analysis with blood counter | 6256 | 5 |
| Mononucleosis test | 5323 | 4 |
| Urine culture | 3981 | 3 |
| Faecal occult blood test | 2396 | 2 |
| Incubated urine sample to external laboratory | 1940 | 2 |
| Cholesterol, potassium, creatinine, GGT, ALAT | 1418 | 1 |
| Prothrombin time (INR) | 1411 | 1 |
| Microalbuminuria | 864 | < 1 |
| Chlamydia test | 822 | < 1 |
| Glycated haemoglobin (HbA1c) | 527 | < 1 |
| Microscopic examination of preparation | 91 | < 1 |
| Trichomonas in vaginal secretion | 91 | < 1 |
| Test for scabies or fungus | 75 | < 1 |
| Helicobacter pylori test | 64 | < 1 |
| Immune fluorescein test for herpes virus | 41 | < 1 |
| Glucose tolerance test | 29 | < 1 |
| Manual colouring and examination of blood smear | 27 | < 1 |
Simple frequency analyses of test use indicated that younger doctors tend to use laboratory tests more often than older doctors (Table II). Similar analyses also indicated that RGPs make less use of laboratory tests than other doctors, but this difference disappeared in the multiple regression analysis. Tests were used significantly more by doctors in central OOH services, and slightly more by female doctors (Table III).
Table II.
Use of various laboratory tests according to doctors’ sex and age: Numbers per 1000 out-of-hours contacts (n = 928 169 by male doctors and n = 268 861 by female doctors).
| Basic fee |
CRP |
Strep A test |
U-HCG |
Glucose |
ECG |
|||||||
| Age group | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female |
| < 31 | 330 | 350 | 300 | 330 | 30 | 45 | 9 | 9 | 24 | 22 | 50 | 46 |
| 31–39 | 310 | 330 | 270 | 300 | 40 | 40 | 7 | 11 | 18 | 24 | 45 | 43 |
| 40–49 | 320 | 300 | 270 | 250 | 46 | 45 | 6 | 6 | 21 | 15 | 38 | 35 |
| > 49 | 264 | 269 | 235 | 232 | 40 | 48 | 4 | 6 | 13 | 16 | 34 | 30 |
| Total | 310 | 320 | 270 | 290 | 40 | 44 | 6 | 9 | 20 | 20 | 42 | 41 |
Table III.
Odds ratio for using laboratory tests: Use of basic lab fee per contact, dichotomized by median value (0.2756) (3802 doctors were included in the analysis).
| Odds ratio | 95% confidence interval | |
| Old vs. young doctor1 | 0.53 | 0.46–0.62 |
| Female vs. male doctor | 1.23 | 1.07–1.42 |
| RGP vs. other doctor | 0.99 | 0.86–1.15 |
| Central vs. rural OOH service2 | 1.98 | 1.72–2.27 |
Notes: 1Dichotomized by median age (38). 2Central is two highest centrality categories, rural two lowest.
Use of CRP
Respiratory disorders were the most frequent ICPC-2 diagnoses used (24% of all contacts), and CRP was taken in 55% of these contacts. For age group 0–1 years 42% of the contacts included a CRP test and for age group 2–6 years 34%. For older patients 23–26% of the contacts included a CRP test. There was slightly less use of CRP in the most rural municipalities (24%) compared with more central municipalities (28%), with largest difference in the youngest group (36% vs. 44%).
Home visits were more frequent in the most rural districts compared with more central areas (11% vs. 5%). With increasing centrality the rate of CRP use per 1000 home visits were 76, 56, 55, and 28. CRP use was most frequent during home visits in the age group 0–6 years (130 per 1000 contacts), 59 in age group 7–20, 37 in age group 21–60, and 44 in age group > 60. There were no significant differences for CRP use during home visits by doctors’ age, sex, or type.
Discussion
The data on which this study is based are comprehensive and almost complete. The differences shown are therefore real and not in need of significance testing. However, the use of fees may not always reflect practice. Some doctors may forget to claim fees they are entitled to. On the other hand, economic motives may cause doctors to order more tests than clinically indicated or even claim fees for tests not performed. We have no reason to believe that this is a common occurrence.
There were significant age differences between different types of doctors. RGPs were older than other doctors, and male doctors were older than female doctors. This age difference is a confounder that has to be taken into account when interpreting the found differences in ordering tests. The bivariate difference between RGPs and OD disappeared in the multiple regression analysis, and is explained by the age difference in the groups. However, the other differences like age, centrality, and sex remained significant even after controlling for other variables.
Since a separate fee does not cover measurement of haemoglobin, sedimentation rate, and urine analysis, we do not know how frequently these tests are used or combined with other laboratory tests. Many tests (e.g. glycated haemoglobin, HbA1c) have little relevance in OOH settings and are therefore rarely used. Earlier we have found that only 13% of all OOH services have a cell counter [7]. Since it is used in only 0.5% of all contacts, it seems that few OOH services find it to be a valuable supplement to CRP. However, this may be different in other countries that have a stronger tradition of using white blood cell indicators. A comprehensive review has shown that white blood cell indicators are less valuable than inflammatory markers for ruling in serious infection, and have no value in ruling out serious infection [18].
Centralization to larger OOH services has reduced the number of home visits. Usually, patients are transported to the OOH service where a wider repertory of diagnostic equipment and laboratory tests are available. In smaller, rural OOH services the workload is less, and it is easier for the doctor to do home visits and also bring diagnostic equipment with him/her. This is reflected in a higher rate of home visits and CRP tests per home visits in these areas.
We are not aware of earlier studies on the frequency of laboratory tests in OOH services. Some have reported on the use of CRP in general practice, for different diagnostic groups, and related to antibiotic prescription for respiratory infections. Two Swedish primary care studies found that CRP was performed in 42% and 36% of patients with a respiratory diagnosis [15,16]. A possible explanation for the higher number in our material (55%) may be that many doctors at OOH services are more inexperienced than RGPs. In 2006 Norwegian RGPs did 88% of the consultations in the daytime, but at OOH services they did only 47% of the consultations [7]. In addition there might be more severe acute infections at OOH services than at daytime RGP practices.
The organization at central OOH services probably explains the significantly higher use of laboratory tests here. With ancillary staff it is easier to order laboratory analyses, and it may even be a routine to measure CRP in every febrile child.
CRP is being used as a universal test for bacterial infections in many organ systems, not only respiratory disorders. Many studies have tried to find a cut-off value for bacterial infections but still there is no conclusion [18,19]. CRP testing may be used as a kind of reassurance, but its utility has been questioned as a diagnostic and prognostic marker for serious bacterial infections. In small children it is of limited value alone as an indicator of serious illness, especially during the first 12 hours of sickness [11–13,17–19]. Also the test is painful and gives the child an unpleasant experience of the doctor's consultation. In any case, it is important that CRP is interpreted in relation to clinical findings.
Most studies of children and markers for bacterial infection are done at hospital/emergency departments where the prevalence of serious infections is higher than in primary care. Considering this and the low prevalence in primary care, the rate of CRP use among children seems unnecessarily high here. These findings probably also apply to primary care outside Norway.
In conclusion, CRP is by far the most frequent laboratory test in OOH services. It is most often used in respiratory illnesses and in small children. Older doctors use laboratory tests less frequently than younger doctors, probably reflecting different clinical experience. Centralization of OOH services results in higher use of laboratory tests. Further investigations are required to study the clinical relevance of this extensive use of CRP in primary care.
Declaration of interest
The authors report no conflict of interest. The authors alone are responsible for the content and writing of the paper.
References
- 1.Sandvik H, Zakariassen E, Hunskår S. Fastlegenes deltakelse i legevakt (Norwegian regular general practitioners participation in out-of-hours work. English version) Tidsskr Nor Laegeforen. 2007;127:2513–16. [PubMed] [Google Scholar]
- 2.Otterlei B, Bentzen N. Færre fastleger deltar i legevakt [Fewer regular practitioners participate in out-of-hours emergency services. English abstract] Tidsskr Nor Laegeforen. 2007;127:1351–3. [PubMed] [Google Scholar]
- 3.Sandvik S, Hunskår S. Arbeidsstil hos fastleger og andre leger på legevakt [Working style among regular general practitioners and other doctors in out-of-hours emergency services in Norway. English version] Tidsskr Nor Laegeforen. 2010;130:135–8. doi: 10.4045/tidsskr.09.0489. [DOI] [PubMed] [Google Scholar]
- 4.Zakariassen E, Blinkenberg J, Holm-Hansen E. Beliggenhet, lokaler og rutiner ved norske legevakter [Locations, facilities and routines in Norwegian out-of-hours services. English version] Tidsskr Nor Laegeforen. 2007;127:1339–42. [PubMed] [Google Scholar]
- 5.Nieber E, Holm-Hansen E, Bondevik G. Organisering av legevakt [Organization of Norwegian out-of-hours primary health care services. English version] Tidsskr Nor Laegeforen. 2007;127:1335–8. [PubMed] [Google Scholar]
- 7.Rebnord I, Thue G, Hunskår S. Utstyr, laboratorieanalyser og medikamenter ved kommunale legevakter [Equipment, laboratory analyses and drugs in out-of-hours services in Norway municipalities. English version] Tidsskr Nor Laegeforen. 2009;129:987–90. doi: 10.4045/tidsskr.08.0288. [DOI] [PubMed] [Google Scholar]
- 8.Nossen JP. Hva foregår på legekontorene? Konsultasjonsstatistikk for 2006 [What happens at the GPs'surgeries? Consultation statistics for 2006] Oslo: Norwegian Labour and Welfare Administration; 2007. Report No.4/2007. [Google Scholar]
- 9.Standard for kommuneklassifisering [Standard classification of municipalities] Oslo: Statistics Norway; 1994. Available at: http://www.ssb.no/kommuner/komklasse94.html (accessed February 11, 2012) [Google Scholar]
- 10.Cals JW, Schot MJ, de Jong SA, Dinant GJ, Hopstaken RM. Point-of-care C-reactive protein testing and antibiotic prescribing for respiratory tract infections: A randomized controlled trial. Ann Fam Med. 2010;8:124–33. doi: 10.1370/afm.1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pfäfflin A, Schleicher E. Inflammation markers in point-of-care testing (POCT) Anal Bioanal Chem. 2009;393:1473–80. doi: 10.1007/s00216-008-2561-3. [DOI] [PubMed] [Google Scholar]
- 11.Don M, Valent F, Korppi M, Canciani M. Differentiation of bacterial and viral community-acquired pneumonia in children. Pediatr Int. 2009;51:91–6. doi: 10.1111/j.1442-200X.2008.02678.x. [DOI] [PubMed] [Google Scholar]
- 12.Kim E, Subhas G, Mittal VK, Golladay ES. C-reactive protein estimation does not improve accuracy in the diagnosis of acute appendicitis in pediatric patients. Int J Sur. 2009;7:74–7. doi: 10.1016/j.ijsu.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 13.Sanders S, Barnett A, Correa-Velez I, Coulthard M, Doust J. Systematic review of the diagnostic accuracy of C-reactive protein to detect bacterial infection in nonhospitalized infants and children with fever. J Pediatr. 2008;153:570–4. doi: 10.1016/j.jpeds.2008.04.023. [DOI] [PubMed] [Google Scholar]
- 14.Keshet R, Boursi B, Maoz R, Shnell M, Guzner-Gur H. Diagnostic and prognostic significance of serum C-reactive protein levels in patients admitted to the department of medicine. Am J Med Sci. 2009;337:248–55. doi: 10.1097/MAJ.0b013e31818af6de. [DOI] [PubMed] [Google Scholar]
- 15.André M, Schwan Å, Odenholt I. The use of CRP tests in patients with respiratory tract infections in primary care in Sweden can be questioned. Scand J Infect Dis. 2004;36:192–7. doi: 10.1080/00365540410019372. [DOI] [PubMed] [Google Scholar]
- 16.Neumark T, Brudin L, Molstad S. Use of rapid diagnostic tests and choice of antibiotics in respiratory tract infections in primary healthcare: A 6-y follow-up study. Scand J Infect Dis. 2010;42:90–6. doi: 10.3109/00365540903352932. [DOI] [PubMed] [Google Scholar]
- 17.Heiskanen-Kosma T, Korppi M. Serum C-reactive protein cannot differentiate bacterial and viral aetiology of community-acquired pneumonia in children in primary healthcare settings. Scand J Infect Dis. 2000;32:399–402. doi: 10.1080/003655400750044971. [DOI] [PubMed] [Google Scholar]
- 18.Van den Bruel A, Thompson MJ, Haj-Hassan T, Stevens R, Moll H, Lakhanpaul M, Mant D. Diagnostic value of laboratory tests in identifying serious infections in febrile children: Systematic review. BMJ. 2011;342:d3082. doi: 10.1136/bmj.d3082. [DOI] [PubMed] [Google Scholar]
- 19.Manzano S, Bailey B, Gervaix A, Cousineau J, Delvin E, Girodias JB. Markers for bacterial infection in children with fever without source. Arch Dis Child. 2011;96:440–6. doi: 10.1136/adc.2010.203760. [DOI] [PubMed] [Google Scholar]