Abstract
Objective
Cardiac myxomas are the most common primary neoplasms of heart. The present study was performed on the 61 cases of patients with cardiac myxoma, in order to investigate the tumors’ clinical and pathological features, and to identify the relationship between the pathological characteristics and clinical behaviors.
Methods
A total of 61 cardiac myxoma cases were analyzed and reviewed retrospectively, including the clinical presentations, physical examinations, and echocardiography, electrocardiography, and pathology documents.
Results
The total patient cohort was made up of 37 women and 24 men. The average age at diagnosis was 48.8 years in males and 51.9 years in females. The most common complaint was dyspnea (37 cases, 60.7%) and the most common sign was systolic murmur (30 cases, 49.2%). Two surface structures and three tumor cell arrangement patterns were observed, and statistical analysis revealed the surface structure was related to the cell arrangement pattern. However, neither the cell arrangement pattern nor the tumor surface structure showed a significant correlation with the clinical presentation.
Conclusions
The present study showed the pathological profiles of cardiac myxomas were not related to the clinical presentations. The results of our study indicate morphologic classifications of cardiac myxomas may not be significant for clinical practice.
Key Words: Cardiac neoplasms; myxoma; immunohistochemistry; pathology, surgical; neoplasm recurrence, local
Introduction
Primary tumors of the heart are extremely rare, with an estimated incidence ranged from 0.0017% to 0.33% at autopsy (1). Cardiac myxomas represent the most frequent benign cardiac tumors. In most surgical series, they account for almost 80% of cases (2). The cells giving rise to the tumor are considered to be multipotential mesenchymal cells that persist as embryonal residues during septation of the heart (3,4). They also are thought to arise from cardiomyocyte progenitor cells, subendothelial vasoformative reserve cells or primitive cells which reside in the fossa ovalis and surrounding endocardium or endocardial sensory nerve (5-8). Occasionally, mucous glandular epithelium may present, which may represent rests of entrapped embryonic foregut (9,10). Two types of macroscopic appearance are observed: polypoid type and papillary type (11,12). The histopathological diagnosis of a cardiac myxoma depends on the identification of the myxoma cell, which has occasionally been called the lepidic cell (13). The cells are arranged singly or in small clusters, or formed capillary like channels (2). Some morphological and immunohistochemical features may be related to the clinical presentations. Burke found that embolic myxomas were less often fibrotic than nonembolic myxomas and were more likely thrombosed and extensively myxoid with an irregular frond-like surface. Fibrotic and non-thrombosed tumors had a longer mean duration of clinical symptoms and were found in older persons. Recurrent, multiple, and familial myxomas were more often found in younger women and, more likely irregular surfaced and histologically myxoid (4). Endo’s group reported that tumors associated with constitutional signs were significantly more likely to be large, multiple, or recurrent than those unassociated with constitutional signs (14). Papillary surface myxomas are thought to be related to embolism, and large left atrial tumors are related to atrial fibrillation. Myxoma cells usually express IL-6, and some tumors have abnormal cellular DNA content (15). A C769T PRKAR1a mutation has been observed in “familial myxomas” (16).
Previous studies have reported a large series of myxomas, however, little was focusing on the histopathologic classifications, and the origin of the myxoma cells is still controversial (8). Moreover, there is still no study related to cardiac myxoma in Shandong Peninsula. Therefore, we presented a retrospective review of our institution’s experience to investigate the clinical and pathological features of cardiac myxomas, and to identify the relationship between the pathological characteristics and clinical presentations.
Materials and methods
Materials
61 consecutive cases of cardiac myxomas, surgically resected at the Cardiac Surgery Department of the Affiliated Hospital of Medical College, Qingdao University, were identified by searching the surgical pathology database during the seven-year period between 2004 through 2010. During the seven years’ period, a total of 71 primary cardiac or pericardiac tumors had been identified, including myxomas (61 cases, occupied about 85.9%), malignant fibrohistiocytomas (2 cases), non-Hodgkin’s lymphomas (2 cases), low grade myxofibrosarcoma (1 case), liposarcoma (1 case) (17), angiosarcoma (1 case), hemangioma (1 case), papillary fibroelastoma (1 case), and rhabdomyoma (1 case). Approval for this study was obtained from the Institutional Review Board. The medical records were reviewed with clinical presentations, methods of diagnosis, management. Follow-up was made by contacting with referring physicians or by telephone.
Pathologic study
All tumors underwent surgical resection after imaging diagnosis. The tumor location and maximal diameter were evaluated in all cases. All specimens were fixed in 10% buffered formalin and embedded in paraffin, and then treated with Hematoxylin and Eosin (H&E) staining and immunohistochemical staining. The latest ten cases were treated with Alcian blue-Periodic acid schiff (AB-PAS) staining to determine and identify carbohydrate macromolecules of the myxoid stroma. When detected by AB-PAS staining, neutral mucopolysaccharides are stained “purple-magenta” by schiff’s reagent, acid mucopolysaccharides are stained “blue” by alcian blue, and the complex of the both are stained “purplish red”. A panel of antibodies, including CD34, CD68, smooth muscle actin (SMA), epithelial membrane antigen (EMA), Vimentin, and cytokeratin (CK), was used for immunohistochemical staining (all antibodies were from Santa Cruz, Beijing, China). The specificity of immunolabeling was demonstrated by the absence of labeling of the antigen when the primary antibody was omitted. All slides were reviewed by two independent pathologists using an Olympus BX-51 microscope (Tokyo, Japan). Only the brown particles that were easily visible with a low power objective was categorized positive staining.
Statistical analysis
Data were analyzed using SPSS software for Microsoft Windows. Mean values between two groups were compared by Student t-tests. The associations between the morphological features and clinical presentations were determined by Pearson’s chi-square tests with correction for the continuity. The criterion level of significance was P<0.05 for all comparisons.
Results
Clinical findings
60 cases were sporadic myxomas and 1 case was familial myxoma. The total patient cohort was made up of 37 women and 24 men (female/male ratio was 1.5). Patients’ age ranged from 12 to 76 years (mean age was 50.7±15.7 years). Most patients were in the fifth, sixth and seventh decades of life (39 of the total 61 cases, account for 60.7%). It was rare in individuals younger than 30 years (5 cases, less than 10%). The average age at diagnosis was 48.8 years in males and 51.9 years in females (P=0.46, no significant difference between males and females).
The myxomas involved predominantly the left atrial cavities (54 cases, 88.5%). Besides, there were six right atrial myxomas (9.8%) and one right ventricular myxoma (1.7%) (Figure 1A). The detailed descriptions of the six right atrial myxomas and one right ventricular myxoma are offered in Table 1. Most myxomas were attached to the septum by a stalk (57 cases, 93.4%). The right ventricular myxoma was originated from the regulating bundle branch.
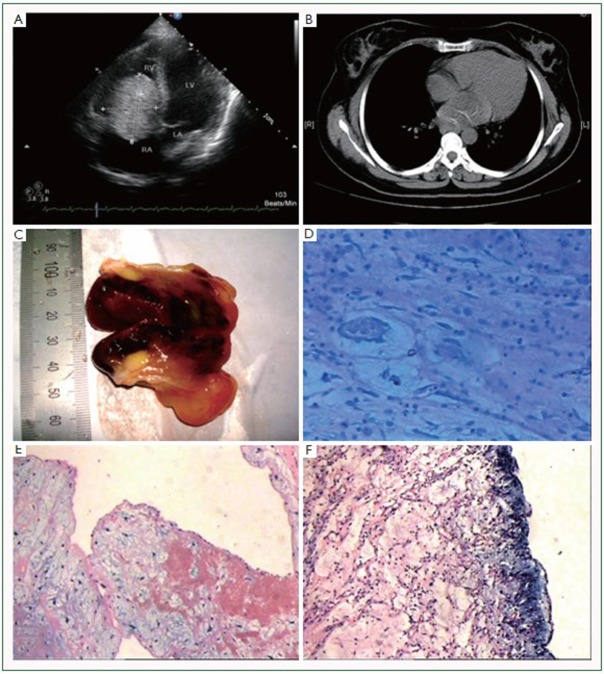
Figure 1.
Echocardiography, computed tomography, gross appearance, AB-PAS staining, and surface appearance of myxomas. A: echocardiography could well identify a right ventricle myxoma; B: computed tomography showed a low density mass located in the left atrium; C: on gross examination, the tumors often have a pedicle. The tumor mass is soft, gelatinous, and very friable; D: AB-PAS staining showed the stromal matrix appeared to purplish red (positive for AB and PAS), while the mucous halo showed blue color (positive for AB); E: the tumor surface showed a papillary appearance (H&E staining); F: the tumor surface showed a smooth and solid appearance (H&E staining). (original magnifications: D, ×100; E, F, ×40).
Table 1. Clinicopathologic features of 6 right atrial and 1 right ventricular myxomas.
| Age (years)/sex | Symptoms/signs | Location | Tumor size (cm) | Macro/histopathology | Follow-up |
|---|---|---|---|---|---|
| 69/Male |
Dyspnea and palpitation |
Right atrium (atrial septum) |
6×3×3 |
Papillary/significant hemorrhage and necrosis |
Recovered |
| 30/Male |
Found during echocardiography after a “biatial and right ventricular myxoma excision” operation seven years ago |
Right atrium (atrial septum), tricuspid valve |
4×4×2, 1 |
Solid/ cell cord predominant |
Recovered |
| 49/Female |
Asymptomatic |
Right atrium (atrial septum) |
3.5×2.4×2 |
Papillary/significant hemorrhage and necrosis |
Recovered |
| 50/Male |
Dyspnea and angina |
Right atrium (atrial septum) |
3×2.2×2 |
Solid/cell cord predominant |
Recovered |
| 35/Female |
Dyspnea and palpitation |
Right atrium (atrial septum) |
6×5×3 |
Papillary/single cell predominant |
Recovered |
| 19/Female |
Cough |
Right atrium (atrial septum) |
7×7×5 |
Papillary/cell cord predominant |
Recovered |
| 34/Male | Syncope | Right ventricle, originated from the regulating bundle branch | 7×5×3.5 | Solid/single cell predominant | Recovered |
Clinical presentations are described in Table 2. Dyspnea was the most frequent complaint at diagnosis (60.7%). The course of disease at presentation ranged from two days to twenty years. Four cases (6.6%) were asymptomatic. Of these four myxomas, three were located in the left atrium and one located in the right atrium. The four myxomas were incidentally found during other preoperative examination or routine examination.
Table 2. Clinical presentations of 61 patients.
| Symptoms | Course of disease | Total [61] |
Left atrial [54] |
Right atrial [6] |
Right ventricular [1] |
||||
|---|---|---|---|---|---|---|---|---|---|
| Cases | % | Cases | % | Cases | % | Cases | % | ||
| Cardiac |
|||||||||
| Dyspnea |
5 days - 20 years |
37 |
60.7 |
34 |
63.0 |
3 |
50 |
- |
- |
| Palpitation |
2 days - 20 years |
28 |
45.9 |
26 |
48.1 |
2 |
33.3 |
- |
- |
| Cough |
8 days - 6months |
4 |
6.6 |
3 |
5.6 |
1 |
16.7 |
- |
- |
| Angina |
1 week - 30 years |
3 |
4.9 |
2 |
3.7 |
1 |
16.7 |
- |
- |
| Edema of lower limbs |
1 year |
1 |
1.6 |
1 |
1.6 |
- |
- |
- |
- |
| Central nervous |
|||||||||
| Vertigo |
6 months - 6 years |
4 |
6.6 |
4 |
7.4 |
- |
- |
- |
- |
| Cerebral infarction |
10 days - 7 months |
2 |
3.3 |
2 |
3.7 |
- |
- |
- |
- |
| Syncope |
3 days |
1 |
1.6 |
- |
- |
- |
1 |
100 |
|
| Systemic |
|||||||||
| Fatigue |
6 months - 2 years |
4 |
6.6 |
4 |
7.3 |
- |
- |
- |
- |
| Fever |
2 months - 4 months |
3 |
4.9 |
3 |
5.6 |
- |
- |
- |
- |
| Asymptomatic | - | 4 | 6.6 | 2 | 3.7 | 2 | 33.3 | - | - |
Abnormal physical examination findings were recorded in 54 cases (88.5%). The most common sign was the systolic murmur (30 cases, 49.2%), and then followed by the diastolic murmur (19 cases, 31.1%). The murmur was often altered along with the body position. Tumor plop could be heard in 10 patients (16.4%). Other abnormal cardiac signs included the loud first sound (15 cases, 24.6%), the loud second sound (10 cases, 16.4%), and the opening snap (6 cases, 7.4%). Two-dimensional echocardiography was performed in all patients, which could well determine the tumor location, size, shape, attachment and mobility. There was no misdiagnosis with echocardiography. Radiological examinations (computed tomography or magnetic resonance imaging) of the chest were only available in several cases (Figure 1B). Electrocardiography documents were available in 55 cases, and abnormal findings were reported in 30 cases (54.5%), including signs of atrial hypertrophy (20 cases, 36.4%), atrial fibrillation (7 cases, 12.7%), arrhythmia (2 cases, 3.6%), and tachycardia (1 cases, 1.8%).
All patients underwent complete myxoma excisions with cardiopulmonary bypass after echocardiographic diagnosis. The patient with the recurrent right atrial myxoma also received tricuspid valve repairing surgery. There were 50 cases available for follow-up (ranged from 6 months to 7 years). Two cases died of other diseases. There was one case bear a recurrence during the follow-up period (2 years after the first surgery). The patient underwent second surgery and recovered uneventfully after that. Other 47 cases recovered uneventfully. Among them two cases had accepted “myxoma resection” surgery at other institutions 7 years and 20 years before. Unfortunately, it is impossible for us to get the detailed information at that time.
Gross pathology
The mean maximal diameter was 5.8±1.8 cm (ranged from 2 to 11 cm). There was no significant difference between the left and right (left: 5.9±1.8 cm, right: 4.8±1.8 cm, P=0.13). The maximal diameter of four asymptomatic cases was 6, 4, 3, and 3 cm, respectively. On gross examination, the tumors had broad base, and most have pedicles (57 cases). The tumor mass was soft, gelatinous, and very friable. They were smooth and glistening (solid type, 18 of 30 available cases with gross description) or had multiple papillary, villous, finger-like projections (papillary type, 12 of 30 cases). Two cases presented with cerebral infarction symptoms were papillary type. The cut surface was variable; most cases were soft, gelatinous, pale grey with hemorrhage areas, others were a little firmer, or with calcification (Figure 1B, 1C).
Histopathology
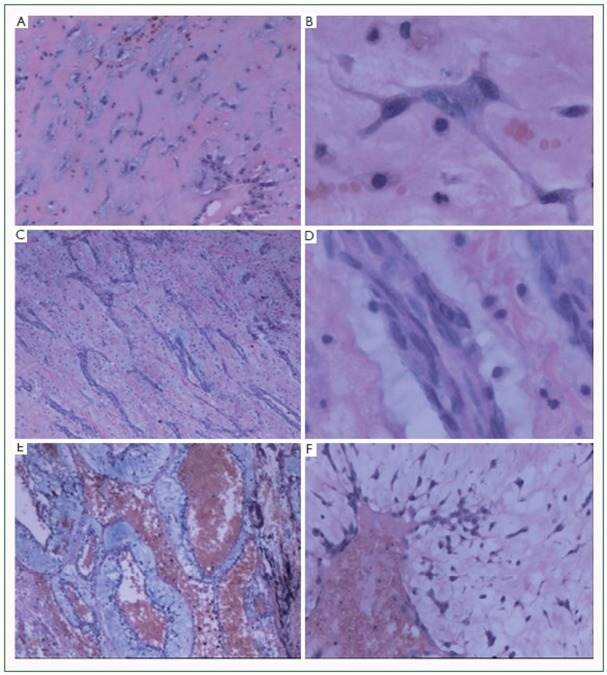
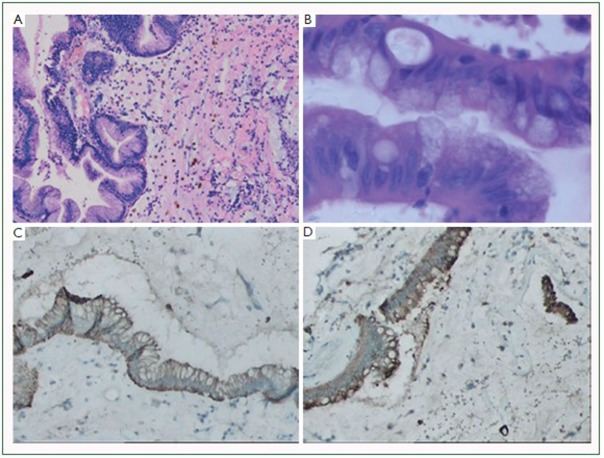
On microscopy, myxoma was made up of a myxoid stroma with variable myxoma cells. The stromal matrix was loose, homogenized and red-stained, which contained variable amounts of proteoglycans, collagen and elastin. Using AB-PAS staining, we found that the stromal matrix appeared to be purplish red (positive for AB and PAS), while the mucous halo showed blue color (positive for AB) (Figure 1D). Variable amounts of thin walled blood sinus or thick walled blood vessels were often present. Hemorrhagic foci, fibrinoid necrosis, hemasiderin-laden macrophages, and inflammatory cells were also frequent. The tumor cells may be spindle, polygonal, or stellate, and have round to oval nuclei with inconspicuous nucleoli, eosinophilic cytoplasm, and indistinct borders. Mitoses are rare. The cells could be arranged in single, in nests or cords, or in vasoformative ring structures. Small or large mucous halos were frequently observed to surround the myxoid cells, the cords or vasoformative ring structures. In fact, most myxomas were combined with the above two or three structures. 2 cases had extensive hemorrhage and necrosis, which made it difficult to classify. According to the arrangement pattern of tumor cells, we categorized the other 59 myxomas into three subtypes: Single cell predominant subtype, cell cord predominant subtype, and vasoformative ring predominant subtype (Figure 2). The majority of myxomas were belonging to single cell predominant subtype (28 cases, 47.5%). The cell cord predominant type often showed rudimentary “chicken-wire” vessels like appearance, with few and scattered single myxoid cells in the stroma. There were 21 cases belonging to this subtype (35.6%). The vasoformative ring predominant subtype showed a hemangioma-like appearance, containing distended blood sinus and positive alcian blue stained myxiod halo. 10 cases were categorized into this subtype (16.9%). Calcification was observed in 3 cases. Besides, well-defined mucous glands, containing goblet cells interspersed between cells, formed by columnar epithelium were found in 2 cases (Figure 3A, 3B).
Figure 2.
Three cell arrangement subtypes of myxomas. A, B: single cell predominant subtype; the single myxoid cells were scattered; C, D: cell cord predominant subtype; myxomas of this type showed a rudimentary “chicken-wire” vessels like appearance, with few and scattered single myxoid cells in the stroma; E, F: vasoformative ring predominant subtype; myxomas of this type showed a hemangioma-like appearance, containing distended blood sinus and distinct mucous halo. (H&E staining, original magnifications: A, C, E, ×40; B, D, ×400; F, ×200).
Figure 3.
Typical glandular structures in myxomas. A, B: Well-defined mucous glands, containing goblet cells interspersed between cells, formed by columnar epithelium were observed (H&E staining); C, D: the glandular structures bear positive expression of CK and EMA. (original magnifications: A, C, D, ×100; B, ×400).
According to the microscopic appearance of tumor surface, all myxomas also could be divided into two subtypes: solid subtype (29 cases) and papillary subtype (30 cases) (Figure 1E, 1F). Sometimes the tumor with clefted area made the differentiation between the two subtypes difficult. In the present study, we categorized such tumors into the former subtype. Only those observed with obvious papillary architecture under low power were categorized into papillary subtype. We found the two subtypes have different cell arrangement patterns. The papillary subtype appeared more likely to form a single cell predominant pattern, whereas the solid subtype was more likely to form rudimentary vessels (Table 3). Moreover, statistical analysis revealed there was no significant difference between these morphological features and clinical symptoms (Table 4).
Table 3. Morphologic features of 59 myxomas (cases).
| Solid | Papillary | |
|---|---|---|
| Single cell predominant |
7 |
21 |
| Cell cord predominant |
13 |
8 |
| Vasoformative ring predominant | 9 | 1 |
The cell has expected count less than 5. Chi-square test showed the solid subtype and papillary subtype have different cell arrangement architectures (x2=13.163, P=0.001).
Table 4. Correlation of clinical presentations and morphologic features (cases).
| Symptoms | Total | Surface |
P value | Cell arrangement |
P value | |||
|---|---|---|---|---|---|---|---|---|
| Solid [29] | Papillary [30] | Single [28] | Cord [21] | Ring [10] | ||||
| Cardiac |
0.904 | 0.520 | ||||||
| Dyspnea |
37* |
18 (62.1%) |
18 (60.0%) |
19 (67.9%) |
11 (52.4%) |
6 (60.0%) |
||
| Palpitation |
28* |
13 (44.8%) |
14 (46.7%) |
14 (50.0%) |
9 (42.9%) |
4 (40.0%) |
||
| Cough |
4 |
3 (10.3%) |
1 (3.3%) |
3 (10.7%) |
1 (4.8%) |
0 |
||
| Angina |
3 |
2 (6.9%) |
1 (3.3%) |
0 |
3 (14.3%) |
0 |
||
| Edema of lower limbs |
1 |
1 (3.4%) |
0 |
0 |
0 |
3 (30.0%) |
||
| Central nervous |
||||||||
| Vertigo |
4 |
2 (6.9%) |
2 (6.7%) |
1 (3.6%) |
1 (4.8%) |
2 (20.0%) |
||
| Cerebral infarction |
2 |
0 |
2 (6.7%) |
2 (7.1%) |
0 |
0 |
||
| Syncope |
1 |
1 (3.4%) |
0 |
1 (3.6%) |
0 |
0 |
||
| Systemic |
||||||||
| Fatigue |
4 |
3 (10.3%) |
1 (3.3%) |
1 (3.6%) |
1 (4.8%) |
2 (20.0%) |
||
| Fever |
3 |
1 (3.4%) |
2 (6.7%) |
3 (10.7%) |
0 |
0 |
||
| Asymptomatic | 4* | 2 (6.9%) | 1 (3.3%) | 0 | 2 (9.5%) | 1 (10.0%) | ||
*Case with extensive hemorrhage and necrosis was excluded. Little sample size made the exact analysis testing of every number difficult. To reduce the errors, we combined data of each group, and performed Pearson’s chi-square tests with correction for the continuity.
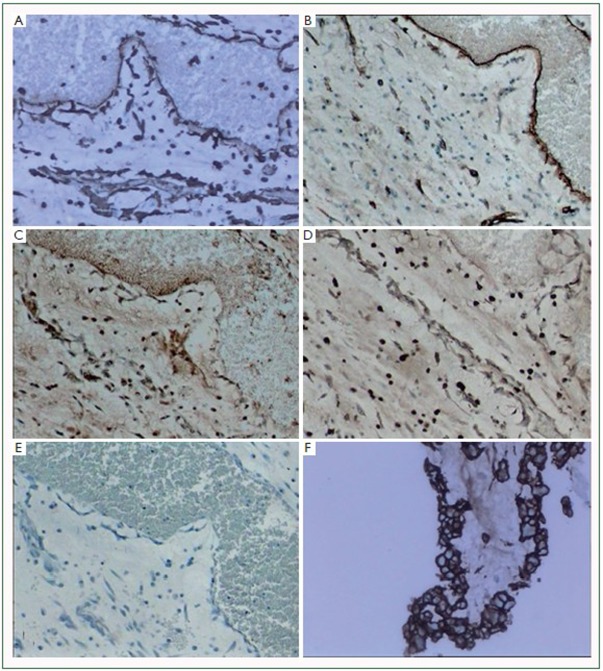
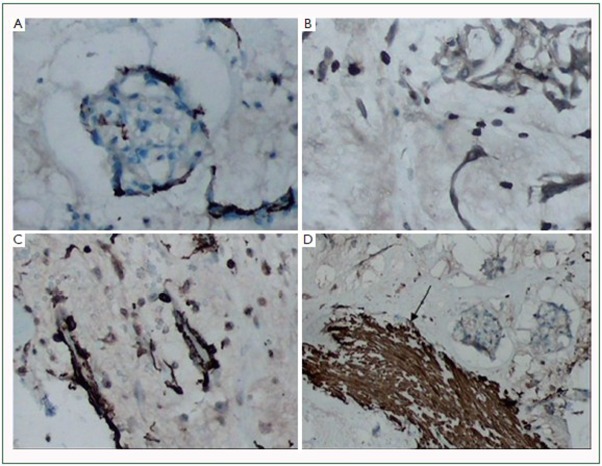
Immuohistochemical staining was carried out in 10 cases. Vimentin was diffusely and strongly reactive with all tumor cells and blood vessels, also reactive with surface lining cells. SMA, CD34 and CD68 were expressed variably (Figure 4,5). Only part of tumor cells showed positive immunoreactivity for these antibodies. The surface lining cells were only positively stained for Vimentin and CD34 (Figure 4F). The glandular cells showed positive CK and EMA expressions (Figure 3C, 3D).
Figure 4.
Immunohistochemical staining for Vimentin, CD34, CD68 and SMA in myxomas. A: Vimentin was diffusely and strongly reactive with all tumor cells and blood vessels; B: CD34 staining; C: SMA staining; D: CD68 staining; E: negative control. We observed that SMA, CD34 and CD68 were expressed variably in myxomas; F: the surface lining cells were immunoreactive for CD34. (original magnifications: A, B, C, D, E, ×40; F, ×100).
Figure 5.
Immunohistochemical staining for CD34, CD68 and SMA in myxomas. A: CD34; B: CD68; C, D: SMA. Our immunostaining results showed only part of tumor cells showed positive immunoreactivity for these antibodies. Note the arrow in figure 5D, smooth muscle of blood vessel bear strong immunoreactivity for SMA. (original magnifications: A, ×200; B, C, D, ×100).
Recurrent myxomas
In our series, a 29-year-old male, who underwent a “biatrial and right ventricular myxoma excision” operation at other institution seven years ago (detailed operation and pathological information at that time was hardly available), presented with a recurrent tumor. He accepted a second surgery at our institution, and two recurrent tumor masses which respectively located in the right atrium and tricuspid valve were observed. Pathological analysis showed the tumor masses have solid surface and rumentary vessels, with foci of hemorrhage, hemorsiderin and patched calcification, which were similar to other sporadic myxomas. However, no pedicle was found. Although the patient denied any family history, we still regard him as a familial myxoma case according to the clinical features. A 16-year-old boy also bore recurrence at the same place (the upper atrial septum) with a pedicle (2 cm × 1.5 cm) after left myxoma resection two years before. The patient presented in April 2006 with dyspnea and palpitation over six months, and the tumor showed papillary surface and single cell predominant structure. In May 2008 the patient accepted the second surgery, however, the recurrent tumor showed a solid appearance and cell cord predominant arrangement structure. After that he recovered uneventfully. We consider the recurrence may attribute to the residual tumor cells. The other recurrent case was a 67-year-old female, who present with dyspnea and palpitation, with a history of “left atrial myxoma resection” twenty years before. The pathologic examination revealed the tumor had a pedicle and appeared a solid surface type and vasoformative ring predominant pattern. Unfortunately, the previous excision record was not available. The patient also recovered uneventfully after the second surgery. Histologically, we found the recurrent cases had no malignant histological characteristics, for instance, atypical nucleus and pathologic karyokinesis.
Discussion
In the present study we have retrospectively reviewed a series of 61 consecutive cardiac myxomas at a single institution of Shandong Peninsula. To the best of our knowledge, this is one of the largest populations related to myxomas during a decade’s period. Our report is similar to the previous studies, which have shown the tumors are the most common primary tumor, and roughly 90% of the tumors are located in the atria, with the left atrium accounting for 80% of those (18). Only 3-4% of myxomas are detected in the left ventricle, and only 3-4% in the right (11). Multilocular myxomas are extremely rare, which often result in local recurrences (19). Familial myxomas are estimated to account for 7% of atrial myxomas (20), are more often multiple, recurrent and right sided, as compared to sporadic myxomas. The affected patients are also younger, most presenting at 20-30 years of age (21-23). Moreover, our study demonstrated, for the first time, that the surface appearance is associated with the tumor cell arrangement structure. In addition, our study indicated that the clinical presentations have no relations with the pathological features, which may be different from the previous study (15).
The clinical presentation of myxomas is diverse and dependent upon tumor location, size and mobility (24-27). According to a previous study, the most common symptom is dyspnea (54%), and then followed by palpitation (35%) (15). Dyspnea and edema of lower limbs are thought to a consequence of atrioventricular valve obstruction. Nevertheless, the intracardiac obstruction may also lead to narrowing outflow tract and atrial fibrillation, which could contribute to dyspnea and palpitation. Cough is thought to result in pulmonary venous hypertension and frank pulmonary edema. Angina may be caused by insufficient blood supply. Embolism is also a classic symptom of myxomas, which have been reported to associate with the papillary surface (15). The cause of some constitutional disturbances is still unclear. Some findings suggest the cytokine interleukin-6 (IL-6) may be responsible for that. The relationship between IL-6 and constitutional syndromes is still controversial. In some cases, the right atrial myxomas may induce pulmonary hypertension because of embolism of tumor fragments. Right ventricular myxomas may mimic stenosis of pulmonary valve and cause syncope. In our series, both left and right atrial myxomas were observed with symptoms of dyspnea, palpitation, cough, and angina. Among them, one left atrial myxoma case was observed with edema of lower limbs and syncope, however, the patient also suffered from systemic lupus erythematosus (SLE), which made the pathophysiological process even puzzled. The symptoms disappeared after the myxoma resection. Unfortunately, the patient died of SLE four years later. Besides, two cases presented with cerebral infarction symptoms and one case with angina and vertigo showed papillary surface, which was consistent with previous studies (4,15). However, in the present study it is difficult to perform further exact analysis because of the little sample size. Other cerebral symptoms in cases of solid surface may only caused by cardiac obstruction and cerebral ischemia.
About 20% of cardiac myxomas are asymptomatic; they are usually smaller than 4 cm (28,29). The maximal diameter of four asymptomatic cases of the present report was 6, 4, 3, and 3 cm, respectively. We consider it is due to the small tumor size or long growth course, which may result in adaption to the tumor.
In our study, 54.5% of patients exhibited abnormal electrocardiography findings, compared with previous study report of 56% (15). The abnormalities found on the electrocardiography are usually nonspecific (11,12,15). They may only reflect the hemodynamic alterations, such as atrial overload or ventricular hypertrophy, which secondarily increased the chamber diameter and altered conduction. Echocardiography is widely recognized as a sensitive preoperative diagnostic method, although it appears nonspecific to some occupying lesions. We have an experience with a low grade cardiac myxofibrosarcoma, which was considered as a myxoma on echocardiography. Moreover, thrombus may be misdiagnosed as myxoma in some cases. Nevertheless, echocardiography is also demonstrated as the most accurate and reliable preoperative method with which to predict the diameter, location, attachment, mobility, and morphology of cardiac myxomas.
Two surface types and three cell arrangement patterns were observed in these cases. Statistical analysis revealed the tumor cells of solid type have a tendency to form vasoforming structures: the tumor cells may arranged in cords or rings. However, the morphological features have no correlation with the clinical presentations. The results indicate that the morphologic classifications of cardiac myxomas may not be significant for clinical practice. Imunohistochemical study showed the tumor cells bear a diffuse, and positive expression for Vimentin, and focal expressions for CD34, CD68, and SMA. The results support the hypothesis of myxoma originated from multipotential mesenchymal cells, capable of vessel, smooth muscle, and histiocyte differentiation. The typical mucous glands may represent rests of entrapped embryonic foregut. Furthermore, previous reports have showed the cells immunoreactive for neuropeptides (s-100, NSE) (7) and Calrectinin (6,30).
Bone and brain metastases from glandular cardiac myxomas have been reported in the recent literature (31-35). The most frequent metastatic site for cardiac myxomas is cerebrum (33). Several reports have reviewed cerebral metastasis cases (34,35). Since most myxomas are located in the left atrium, systemic embolism is particularly frequent. The tumor fragments metastasized to cerebral vessel walls may penetrate through the vessel wall, forming intra-atrial metastases. Some cytokines, such as CXC chemokines, may explain the metastasis potential of morphologically benign myxomas. In our series, no metastatic case was observed, including two cases with typical mucous glandular differentiation. Especially to deserve to be mentioned, there was an uncommon histological likeness between the glandular myxomas and mucinous adenocarcinomas. One case with glandular differentiation in the series was considered as metastatic mucinous adenocarcinoma at one time.
In conclusion, we have retrospectively reviewed a series of 61 myxoma cases at a single institution of Shandong Peninsula. The clinical presentations and pathological characteristics (particular on the relationship between the both) were investigated. Myxomas may cause varies kinds of symptoms, and mainly categorize into two surface subtypes and three cell arrangement patterns. However, further statistical analysis showed these morphological features have no relationship with the clinical presentations. The results of this study indicate the histopathologic classifications of cardiac myxomas may not be significant for clinical practice.
Acknowledgements
We thank Professor Xiang-Rui Ji for his skillful assistance with the English language.
Disclosure: The authors declare no conflict of interest.
References
- 1.Wold LE, Lie JT. Cardiac myxomas: a clinicopathologic profile. Am J Pathol. 1980;101:219-240 [PMC free article] [PubMed] [Google Scholar]
- 2.Burke AP, Tazelaar H, Gomez-Roman JJ, et al. Cardiac myxoma. In: Travis WD, Brambilla E, Muller-Hermelink HK, Harris CC, editors. Pathology and Genetics of Tumours of the Lung, Pleura, Thymus and Heart. Lyon: IARC Press, 2004: 260-3. [Google Scholar]
- 3.Lie JT. The identity and histogenesis of cardiac myxomas: a controversy put to rest. Arch Pathol Lab Med. 1989;113:724-726 [PubMed] [Google Scholar]
- 4.Burke AP, Virmani R. Cardiac myxoma. A clinicopathologic study. Am J Clin Pathol. 1993;100:671-680 [DOI] [PubMed] [Google Scholar]
- 5.Kodama H, Hirotani T, Suzuki Y, et al. Cardiomyogenic differentiation in cardiac myxoma expressing lineage-specific transcription factors. Am J Pathol. 2002;161:381-389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Terracciano LM, Mhawech P, Suess K, et al. Calretinin as a marker for cardiac myxoma. Diagnostic and histogenetic considerations. Am J Clin Pathol. 2000;114:754-759 [DOI] [PubMed] [Google Scholar]
- 7.Pucci A, Gagliardotto P, Zanini C, et al. Histopathologic and clinical characterization of cardiac myxoma: review of 53 cases from a single institution. Am Heart J. 2000;140:134-138 [DOI] [PubMed] [Google Scholar]
- 8.Amano J, Kono T, Wada Y, et al. Cardiac myxoma: its origin and tumor characteristics. Ann Thorac Cardiovasc Surg. 2003;9:215-221 [PubMed] [Google Scholar]
- 9.Johansson L. Histogenesis of cardiac myxomas. An immunohistochemical study of 19 cases, including one with glandular structures, and review of the literature. Arch Pathol Lab Med. 1989;113:735-741 [PubMed] [Google Scholar]
- 10.Pucci A, Bartoloni G, Tessitore E, et al. Cytokeratin profile and neuroendocrine cells in the glandular component of cardiac myxoma. Virchows Arch. 2003;443:618-624 [DOI] [PubMed] [Google Scholar]
- 11.Reynen K. Cardiac myxomas. N Engl J Med. 1995;333:1610-1617 [DOI] [PubMed] [Google Scholar]
- 12.Butany J, Nair V, Naseemuddin A, et al. Cardiac tumours: diagnosis and management. Lancet Oncol. 2005;6:219-228 [DOI] [PubMed] [Google Scholar]
- 13.St John Sutton MG, Mercier LA, Giuliani ER, et al. Atrial myxomas: a review of clinical experience in 40 patients. Mayo Clin Proc. 1980;55:371-376 [PubMed] [Google Scholar]
- 14.Endo A, Ohtahara A, Kinugawa T, et al. Characteristics of cardiac myxoma with constitutional signs: a multicenter study in Japan. Clin Cardiol. 2002;25:367-370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Acebo E, Val-Bernal JF, Gómez-Román JJ, et al. Clinicopathologic study and DNA analysis of 37 cardiac myxomas: a 28-year experience. Chest. 2003;123:1379-1385 [DOI] [PubMed] [Google Scholar]
- 16.Yokomuro H, Yoshihara K, Watanabe Y, et al. The variations in the immunologic features and interleukin-6 levels for the surgical treatment of cardiac myxomas. Surg Today. 2007;37:750-753 [DOI] [PubMed] [Google Scholar]
- 17.Wang JG, Wei ZM, Liu H, et al. Primary pleomorphic liposarcoma of pericardium. Interact Cardiovasc Thorac Surg. 2010;11:325-327 [DOI] [PubMed] [Google Scholar]
- 18.Kumar BV, Abbas AK, Fausto N, et al. Cardiac tumors. In: Kumar BV, Abbas AK, Fausto N, Mitchell R, editors. Robbins basic pathology, 8th edition. Philadelphia: Saunders, 2007: 417-8. [Google Scholar]
- 19.Martin LW, Wasserman AG, Goldstein H, et al. Multiple cardiac myxomas with multiple recurrences: unusual presentation of a “benign” tumor. Ann Thorac Surg. 1987;44:77-78 [DOI] [PubMed] [Google Scholar]
- 20.Casey M, Mah C, Merliss AD, et al. Identification of a novel genetic locus for familial cardiac myxomas and Carney complex. Circulation. 1998;98:2560-2566 [DOI] [PubMed] [Google Scholar]
- 21.Larsson S, Lepore V, Kennergren C. Atrial myxomas: results of 25 years’ experience and review of the literature. Surgery. 1989;105:695-698 [PubMed] [Google Scholar]
- 22.Edwards A, Bermudez C, Piwonka G, et al. Carney’s syndrome: complex myxomas. Report of four cases and review of the literature. Cardiovasc Surg. 2002;10:264-275 [DOI] [PubMed] [Google Scholar]
- 23.Papagiannopoulos K, Hughes S, Nicholson AG, et al. Cystic lung lesions in the pediatric and adult population: surgical experience at the Brompton Hospital. Ann Thorac Surg. 2002;73:1594-1598 [DOI] [PubMed] [Google Scholar]
- 24.Premaratne S, Hasaniya NW, Arakaki HY, et al. Atrial myxomas: experiences with 35 patients in Hawaii. Am J Surg. 1995;169:600-603 [DOI] [PubMed] [Google Scholar]
- 25.Bjessmo S, Ivert T. Cardiac myxoma: 40 years’ experience in 63 patients. Ann Thorac Surg. 1997;63:697-700 [DOI] [PubMed] [Google Scholar]
- 26.Pinede L, Duhaut P, Loire R. Clinical presentation of left atrial cardiac myxoma. A series of 112 consecutive cases. Medicine (Baltimore). 2001;80:159-172 [DOI] [PubMed] [Google Scholar]
- 27.Gabe ED, Rodríguez Correa C, Vigliano C, et al. Cardiac myxoma. Clinical-pathological correlation. Rev Esp Cardiol. 2002;55:505-513 [DOI] [PubMed] [Google Scholar]
- 28.Goswami KC, Shrivastava S, Bahl VK, et al. Cardiac myxomas: clinical and echocardiographic profile. Int J Cardiol. 1998;63:251-259 [DOI] [PubMed] [Google Scholar]
- 29.Grebenc ML, Rosado-de-Christenson ML, Green CE, et al. Cardiac myxoma: imaging features in 83 patients. Radiographics. 2002;22:673-689 [DOI] [PubMed] [Google Scholar]
- 30.Acebo E, Val-Bernal JF, Gómez-Roman JJ. Thrombomodulin, calretinin and c-kit (CD117) expression in cardiac myxoma. Histol Histopathol. 2001;16:1031-1036 [DOI] [PubMed] [Google Scholar]
- 31.Moiyadi AV, Moiyadi AA, Sampath S, et al. Intracranial metastasis from a glandular variant of atrial myxoma. Acta Neurochir (Wien). 2007;149:1157-1162 [DOI] [PubMed] [Google Scholar]
- 32.Uppin SG, Jambhekar N, Puri A, et al. Bone metastasis of glandular cardiac myxoma mimicking a metastatic carcinoma. Skeletal Radiol. 2011;40:107-111 [DOI] [PubMed] [Google Scholar]
- 33.Shimono T, Makino S, Kanamori Y, et al. Left atrial myxomas. Using gross anatomic tumor types to determine clinical features and coronary angiographic findings. Chest. 1995;107:674-679 [DOI] [PubMed] [Google Scholar]
- 34.Altundag MB, Ertas G, Ucer AR, et al. Brain metastasis of cardiac myxoma: case report and review of the literature. J Neurooncol. 2005;75:181-184 [DOI] [PubMed] [Google Scholar]
- 35.Rodrigues D, Matthews N, Scoones D, et al. Recurrent cerebral metastasis from a cardiac myxoma: case report and review of literature. Br J Neurosurg. 2006;20:318-320 [DOI] [PubMed] [Google Scholar]