Abstract
BACKGROUND
Despite federal guidelines calling for the reduction of obesity and elimination of health disparities, black–white differences in obesity prevalence and in medical expenditures and utilization of health care services persist.
OBJECTIVES
To examine black–white differences in medical expenditures and utilization of health care services (office-based visits, hospital outpatient visits, ER visits, inpatient stays and prescription medication) within body weight categories.
STUDY DESIGN
This study used data from the 2006 Medical Expenditures Panel Survey (MEPS) and included 15,164 non-Hispanic white and non-Hispanic black adults. We used a standard two-part econometric model to examine black–white differences in how expenditures (total annual medical expenditures and expenditures for each type of service) vary within body weight categories.
KEY RESULTS
Blacks in each weight category were less likely to use any medical care than their white counterparts, even after controlling for socio-demographic characteristics, perceived health status, health conditions and health beliefs. Among those who received medical care, there is no significant difference in the total amount spent on care between blacks and whites. Compared to whites, blacks in each body weight category were significantly less likely to use office-based visits, hospital outpatient visits, and medications. Among those who used medications, blacks had significantly lower expenditures than whites. Blacks in obese class II/III were significantly less likely to have any medical expenditures on inpatient care than their white counterparts.
CONCLUSIONS
Black–white racial differences in total medical expenditures were observed in each body weight category and were significantly different in the obese I class, overweight, and healthy weight categories. Obese blacks also spent a smaller amount than obese whites—the insignificance might be due to the smaller sample size. These differences cannot be fully explained by socio-demographics, health conditions, or health beliefs. Black–white differences in medical expenditures may be largely due to relatively inexpensive types of care (office-based visits, outpatient care, medication) rather than more costly ones (inpatient care, ER).
KEY WORD: obesity, body weight, medical expenditures, disparity
INTRODUCTION
Reducing obesity and eliminating disparities in health care are national priorities identified in the U.S. Department of Health and Human Services’ Healthy People 2020 initiative.1 Obesity (defined as having a body mass index [BMI] ≥30 kg/m2) affects one-third of adults,2 is a leading cause of preventable death in the United States, is estimated to cost $147 billion annually,3 and is highest in minority populations.4 Within these minority populations, blacks are at particularly high risk.
Consistent with two decades of literature documenting race-based disparities in health care access and utilization across a broad spectrum of diseases and conditions,4–8 racial disparities in obesity care have recently been explored. Wee et al.’s research (2005 indicates that white obese individuals spend roughly $600 more on health care than black obese individuals.9 However, there is limited evidence as to why medical expenditures associated with obesity vary by race. What is available suggests that racial differences are partially due to clinical need and preferences for health care services,10 and to other factors imbedded in health care systems such as geographic availability.
The purpose of this study was to examine whether black–white differences in medical expenditures and utilization of health care services (office-based visits, hospital outpatient visits, ER visits, inpatient stays and prescription medication) exist in each body weight category, and to explore the possible reasons of such differences. Our analysis is guided by two conceptual models: Andersen’s Behavioral Model,11,12 which suggests that two major factors (environmental and population characteristics) affect health behaviors and utilizations; and the Health Belief Model developed by Janz and Becker,13 which suggests that both the perceived benefits of using healthcare and the perceived barriers to using health care affect care utilization. We sought to explore the reasons for such black–white differences in obesity-related medical expenditures and utilization of care in the following dimensions: population characteristics include predisposing characteristics such as age, gender and educational level, enabling resources such as need to access these services as perceived by the individual and the provider; and beliefs in and attitudes towards medical care and insurance.
A better understanding of race-based disparities in obesity-related medical expenditures may help facilitate more accurate projections of future medical costs and help to lead to the development of well-targeted and appropriately designd interventions to close gaps in access to medical care between blacks and whites.
METHODS
Data
Data from the 2006 Medical Expenditures Panel Survey (MEPS) were used to estimate obesity attributable expenditures by race and by body weight category. MEPS is an annual nationally representative large-scale survey of non-institutionalized Americans’ health care expenditures and utilizations, conducted by the Agency for Healthcare Research and Quality. We use MEPS household component in this study: it is a household survey, using a nationally representative subsample of households that participated in the prior year’s National Health Interview Survey. During the household surveys, one informed household member provides information about all household members on medical expenditures, which are then aggregated over a year and include those covered by insurance and those paid out-of-pocket. The MEPS also included information about health conditions (e.g., BMI) and socio-demographic characteristics (e.g., health insurance coverage, race/ethnicity, age, education and poverty status). Using computer assisted personal interviewing (CAPI) technology, we collected information about each household member. We restricted our analytical sample to non-Hispanic whites (hereafter referred to as whites) and non-Hispanic blacks (hereafter referred to as blacks). Participants who self-described as white Hispanics or black Hispanics are therefore excluded from our study. We excluded individuals who did not have a measure of body weight (approximately 3% of the sample) or who were classified as underweight (approximately 3% of the sample). Our final analytic sample included 15,164 adults (aged 18 or above).
Measures
Outcome Variables
The outcomes of interest were total annual medical expenditures, and medical expenditures by service type (office-based visits, hospital outpatient visits, ER visits, inpatient stays and prescription medication). The total annual medical expenditures represents the accrued medical spending including inpatient hospital and physician services, ambulatory physician and non-physician services, prescribed medicines, home health services, dental services, and various medical equipment during the calendar year. It excludes over-the-counter medications and complementary and alternative medical care services.14
Independent Variables
The key explanatory variables were race and body weight categories. Individuals were divided into standard body weight categories15 based on their BMI (calculated from self-reported weight and height): healthy weight (18.5-24.9 kg/m2), overweight (25.0-29.9 kg/m2), obese class I (30.0-34.9 kg/m2), and obese class II or III (35 kg/m2 and above). Obese class II and III are combined due to smaller sample sizes.
Covariates included: age group (18–24, 25–34, 35–44, 45–54, 55–64, 65–74, 75–84, and 85 and above), gender, poverty status (<100% federal poverty level, 100%–125%, 125%–200%, 200%–400% and ≥400%), education (less than high school, high school, college, graduate school, and other degrees), married, census region (Northeast, Midwest, South, and West), health insurance (any private insurance, Medicare only, Medicaid only, and uninsured), smoking status (smoker vs. nonsmoker), health conditions (binary variables of diagnosed conditions including diabetes, asthma, hypertension, high cholesterol level, and heart diseases), and health status (self-perceived physical and mental health defined dichotomously where those with poor or fair status were compared to those with good, very good, or excellent status). All covariates were included based on previous research suggesting that they are associated with medical expenditures.16,17 The inclusion of health conditions allowed us to examine whether co-morbidities, rather than body weight, were responsible for black–white race differences in medical expenditures by body weight categories. Previous research has shown that clinical needs or preferences are difficult to measure directly, and suggests including several health status variables (gender, age, functional limitation, and self-assessed health scores) when using MEPS.11
Finally, we also included four questions regarding attitudes towards medical care and insurance: Adults age 18 and over were asked whether they strongly agree, agree, are uncertain, disagree, or strongly disagree with each of the following statements: “I’m healthy enough that I really don’t need health insurance;” “Health insurance is not worth the money it costs;” “I’m more likely to take risks than the average person;” and “I can overcome illness without help from a medically trained person.” We created binary variables for each of the four questions, with “1” indicating “strongly agreed” or “agreed” responses, and “0” for the other response categories. A previous report found blacks were more likely than whites to feel they were healthy and did not need health insurance.18
Analysis
Building upon the approach used by Finkelstein and colleagues,19 we developed a two-part model that included interactions between each weight category and the binary variable of “black.” Including the interaction terms allow us test whether the effects of race vary by weight category. In the first part of the model, a logistic regression was used to estimate differences in the probability of utilization by race and obesity status, and in the second part of the model, a generalized linear model with a log link function and a gamma family distribution of the error term was used to estimate differences in the quantity of use (either in terms of dollars or amount of services) among those who used any care. The first part of the model estimated the probability that a person utilized any care. The second part of the model estimated medical care utilization or expenditures conditional on a person having positive utilization or expenditures.
To be able to examine dimensions of the black–white differences, we added the covariates in stages. First, we included socio-demographic factors as predisposing characteristics. Next, we included health conditions, behavior and perceived physical and mental health status as enabling resources as Andersen’s Behavioral Model suggests. Finally, we added the four variables indicating one’s attitudes towards medical care and insurance as suggested by the Health Belief Model (the full model). We then used the full model to further examine expenditures by specific services.
In a sensitivity analysis, we included SF-12 health status measures; both the Physical Component Summary (PCS) and the Mental Component Summary (MCS) of the SF-12 have been shown to improve predictions of medical expenditures.20 We used age-specific, standardized PCS and MCS scores in the sensitivity analysis.
RESULTS
Table 1 describes the unadjusted annual medical expenditures from 2006 by body weight category. Whites spent more on medical care than blacks in each body weight category, and the race difference in medical expenditures was statistically significant for those in obese class II/III and obese class I: whites in obese class II/III spent $1,792 more on annual medical care than their black counterparts (p < 0.01), and whites in obese class I spent $1,461 more annually (p < 0.01). Blacks had a higher average BMI than whites in each body weight category, although this difference was not statistically significant.
Table 1.
Unadjusted Annual per Capita Black–White Medical Spending by Body Weight Category
| White | Black | Difference in spending, | ||||||
|---|---|---|---|---|---|---|---|---|
| Weight category | N | Average BMI | Annual medical spending | N | Average BMI | Annual medical spending | White–Black | |
| Obese II/III | 1,320 | 40.3 | $7,132 | 650 | 41.2 | $5,340 | $1,792 | *** |
| Obese I | 2,056 | 32.1 | $5,179 | 756 | 32.2 | $3,718 | $1,461 | *** |
| Overweight | 4,281 | 27.1 | $4,272 | 1,260 | 27.3 | $4,202 | $70 | |
| Healthy weight | 4,433 | 22.3 | $3,826 | 1,089 | 22.4 | $3,347 | $479 | |
Healthy weight (18.5-24.9), overweight (25.0-29.9), obese class I (30.0-34.9), obese class II/III (35.0 and above)
Numbers in this table are obtained from MEPS 2006; health care spending is unadjusted
*** p < 0.01
Tables 2 and 3 present the results of the three models examining the total medical expenditures. Odds ratios and 95% Confidence Intervals were presented for each variable, where odds ratios greater than 1 are consistent with a higher probability to use any care. All differences between estimates discussed in the text are statistically significant at the 0.05 level unless otherwise noted. Model 1 shows that blacks in obese class I, overweight, and healthy weight category were significantly less likely to use any care as compared to their white counterparts, after controlling for demographic and socioeconomic factors. Blacks in obese class II/III also had lower odds of using any care than whites in obese class II/III although the differences were not statistically significant. For example, blacks in obese class I had 43% lower odds of using any care than whites in obese class I, and blacks with a healthy weight had 58% lower odds of using any care than their white counterparts. However, when looking at the part 2 of the model 1, where a positive coefficient implies higher spending, blacks did seek care, there was no statistically significant difference in the amount of medical expenditures between blacks and whites.
Table 2.
Total Annual Medical Expenditures, MEPS 2006 (Model 1)
| Model 1 | ||||||
|---|---|---|---|---|---|---|
| Part 1, N = 15,164 | Part 2, N = 13,214 | |||||
| Probability of use | Amount of $ spent | |||||
| Key explanatory variables | OR | 95% CI | Coef | 95% CI | ||
| Obese II/III, black vs. white (ref) | 0.72 | (0.50 | 1.03) | -0.16 | (-0.43 | 0.10) |
| Obese I, black vs. white (ref) | 0.57 | (0.41 | 0.79) | -0.21 | (-0.46 | 0.04) |
| Overweight, black vs. white (ref) | 0.54 | (0.44 | 0.68) | 0.07 | (-0.10 | 0.25) |
| Healthy weight black vs. white (ref) | 0.42 | (0.34 | 0.53) | -0.06 | (-0.28 | 0.16) |
| Demographics & SES & Insurance (omitted) | ||||||
The white reference group for each category is at the same body weight (e.g., black obese II/III compared to white obese II/III). In the part 1 of the model, we predicted the probability of incurring any expenditures; in the part 2 of the model, we predicted the amount spent on medical care, among those who actually had a positive spending. The demographic, socioeconomic and insurance variables are controlled but omitted from the tables due to space limit
Table 3.
Total Annual Medical Expenditures, MEPS 2006 (Model 2 & 3)
| Model 2 | Model 3 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Part 1, N = 14,967 | Part 2, N = 13,081 | Part 1, N = 13,413 | Part 2, N = 11,804 | |||||||||
| Probability of use | Amount of $ spent | Probability of use | Amount of $ spent | |||||||||
| Key explanatory variables | OR | 95% CI | Coef | 95% CI | OR | 95% CI | Coef | 95% CI | ||||
| Obese II/III, black vs. white (ref) | 0.68 | (0.45 | 1.02) | -0.17 | (-0.43 | 0.10) | 0.70 | (0.45 | 1.09) | -0.14 | (-0.41 | 0.12) |
| Obese I, black vs. white (ref) | 0.57 | (0.40 | 0.81) | -0.25 | (-0.46 | -0.05) | 0.55 | (0.38 | 0.80) | -0.30 | (-0.51 | -0.10) |
| Overweight, black vs. white (ref) | 0.53 | (0.42 | 0.67) | -0.02 | (-0.19 | 0.16) | 0.54 | (0.42 | 0.70) | -0.02 | (-0.20 | 0.16) |
| Normal weight black vs. white (ref) | 0.42 | (0.33 | 0.53) | -0.07 | (-0.30 | 0.17) | 0.41 | (0.32 | 0.53) | -0.03 | (-0.27 | 0.21) |
| Demographics & SES & Insurance (omitted) | ||||||||||||
| Health conditions | ||||||||||||
| Perceived poor/fair physical health | 1.76 | (1.35 | 2.28) | 0.65 | (0.54 | 0.75) | 1.60 | (1.22 | 2.12) | 0.66 | (0.54 | 0.77) |
| Perceived poor/fair mental health | 1.84 | (1.34 | 2.53) | 0.25 | (0.10 | 0.39) | 1.82 | (1.30 | 2.54) | 0.19 | (0.04 | 0.34) |
| Smokers | 1.08 | (1.04 | 1.12) | 0.03 | (0.01 | 0.05) | 1.04 | (0.98 | 1.09) | 0.03 | (0.01 | 0.05) |
| Diabetes | 8.13 | (3.61 | 18.34) | 0.36 | (0.25 | 0.46) | 7.77 | (3.24 | 18.62) | 0.34 | (0.23 | 0.44) |
| Asthma | 2.26 | (1.72 | 2.97) | 0.19 | (0.09 | 0.29) | 2.14 | (1.61 | 2.85) | 0.16 | (0.06 | 0.26) |
| Hypertension | 4.28 | (3.29 | 5.58) | 0.25 | (0.16 | 0.34) | 3.92 | (2.96 | 5.20) | 0.24 | (0.16 | 0.33) |
| High Cholesterol | 2.97 | (2.25 | 3.93) | 0.15 | (0.07 | 0.23) | 3.11 | (2.30 | 4.21) | 0.15 | (0.07 | 0.23) |
| Heart diseases | 2.18 | (1.46 | 3.28) | 0.48 | (0.39 | 0.57) | 1.78 | (1.17 | 2.71) | 0.47 | (0.37 | 0.56) |
| Attitudes toward health care & insurance | ||||||||||||
| Don't need health insurance | - | - | - | - | - | - | 0.74 | (0.59 | 0.92) | -0.31 | (-0.48 | -0.13) |
| Health insurance not worth the cost | - | - | - | - | - | - | 0.92 | (0.78 | 1.09) | -0.17 | (-0.26 | -0.08) |
| More likely to take risk | - | - | - | - | - | - | 1.07 | (0.91 | 1.27) | 0.09 | (-0.01 | 0.19) |
| Can overcome illness without medical care | - | - | - | - | - | - | 0.75 | (0.63 | 0.89) | -0.17 | (-0.27 | -0.07) |
The white reference group for each category is at the same body weight (e.g., black obese II/III compared to white obese II/III). In the part 1 of the model, we predicted the probability of incurring any expenditures; in the part 2 of the model, we predicted the amount spent on medical care, among those who actually had a positive spending. The demographic, socioeconomic and insurance variables are controlled but omitted from the tables due to space limit
Model 2 (Table 3) suggests that, significant black–white differences in medical expenditures persist even after controlling for health conditions, smoking status, and perceived physical and mental health. As compared to whites, blacks in obese class I, overweight, and healthy weight category again had significantly lower odds of using any care: OR = 0.57 (CI = 0.40, 0.81), OR = 0.53 (CI = 0.42, 0.67), OR = 0.42 (CI = 0.33, 0.53), respectively for each weight category. Again, blacks in obese class II/III showed insignificant lower odds than whites in obese class II/III (OR = 0.68, CI = 0.45, 1.02). When blacks did use any care, they had lower expenditures; this difference was only significant for blacks in obese class I who spent approximately 22% less than their white counterparts (Coefficient = –0.25, CI = -0.46, –0.05).
Model 3 (the full model; Table 3) included the four variables indicating one’s attitudes towards medical care and insurance. Respondents who agreed to the questions of “I’m healthy enough that I really don’t need health insurance” and “I can overcome illness without help from a medically trained person” were found to be significantly less likely to use care: OR = 0.74 (CI = 0.59, 0.92) and OR = 0.75 (CI = 0.63, 0.89), respectively. When they did use any care, they had significantly lower expenditures: people who believed they were healthy enough and did not need health insurance spent 31% less and people who believed they could overcome illness without medical care spent 17% less. Including these health belief variables did not change our main findings: blacks in obese class I, overweight, and healthy weight categories were again found significantly less likely to use care than white counterparts.
With respect to the covariates, we found that age and gender were strong predictors of medical expenditures; older adults spent more than younger adults and females used more care than males. Similarly, we found that socio-demographic characteristics (e.g., poverty level, education, marital status, and census region) predicted medical expenditures and that health insurance was related to significantly higher likelihood of health care utilization. We also found that health conditions (diabetes, asthma, hypertension, high cholesterol level, and heart diseases), smoking status and perceived health status were all significantly associated with medical expenditures. Again, two of the health belief variables (“I’m healthy enough that I really don’t need health insurance” and “I can overcome illness without help from a medically trained person”) are significantly associated with less medical expenditures.
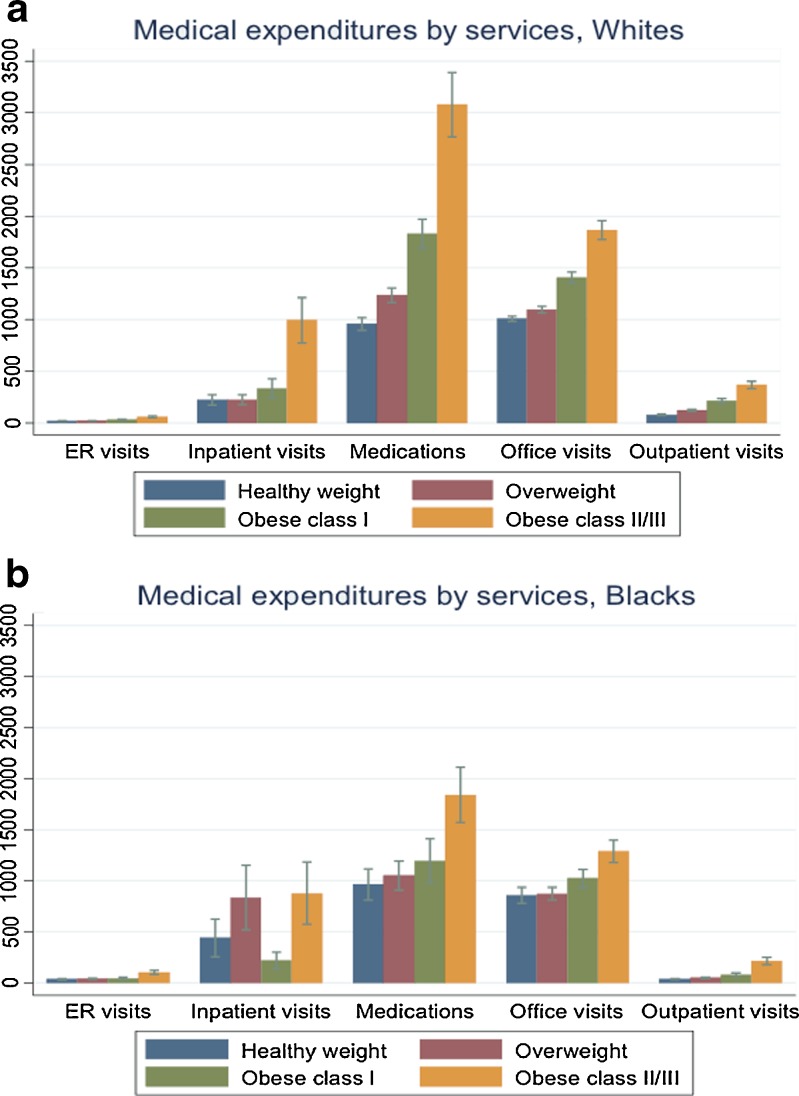
Table 4 presents the results of the full model with expenditures of each service type as the outcome. After adjusting for all covariates presented in the full model (Table 3: model 3), blacks were significantly less likely to have any office-based visits or hospital outpatient visits than whites in each body weight category (non-significant lower odds for healthy weight blacks using hospital outpatient care). For example, blacks in obese class II/III had 44% lower odds of having any office-based visits as compared to whites in the same body weight category (OR = 0.56, CI = 0.40, 0.78). Among those who did have a visit, blacks spent a meaningfully smaller, but not significant smaller, amount: approximately 23% less expenditures than whites (Coefficient = -0.26, CI = -0.58, 0.07). Compared to their white counterparts, blacks in each body weight category were significantly less likely to take any medication, and when they did take medications, they took significantly smaller amount than whites (except for those with healthy weight). For example, blacks in obese class II/III had 53% lower odds (OR = 0.47, CI = 0.32, 0.67) of taking any medication than whites, and when they did spend on medication, they spent approximately 44% less amount (Coefficent = -0.58, CI = 0.87, -0.29). For inpatient services, blacks in obese class II/III were significantly less likely to have any medical expenditures on inpatient care than their white counterparts (OR = 0.67, CI = 0.45, 0.99). No significant black–white differences in expenditures on ER visits were observed. Figure 1a and b depict the estimated medical expenditures by service and by race. After adjusting for all the covariates, whites in overweight, obese I class and II/III class significantly spent more on medications, office visits, and outpatient visits than their black counterparts. Overweight blacks spent more on inpatient than overweight whites.
Table 4.
Annual Medical Expenditures by Services, MEPS 2006
| Office-Based visits | Hospital outpatient visits | ER visits | Inpatient discharges | Medication | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Part 1 | Part 2 | Part 1 | Part 2 | Part 1 | Part 2 | Part 1 | Part 2 | Part 1 | Part 2 | |||||||||||
| OR | Coef | OR | Coef | OR | Coef | OR | Coef | OR | Coef | |||||||||||
| Obese II/III, black vs. white (ref) | 0.56 | -0.26 | 0.61 | 0.04 | 0.96 | 0.29 | 0.67 | -0.03 | 0.47 | -0.58 | ||||||||||
| (95% CI) | (0.40 | 0.78) | (-0.58 | 0.07) | (0.45 | 0.83) | (-0.69 | 0.76) | (0.71 | 1.30) | (-0.21 | 0.79) | (0.45 | 0.99) | (-0.63 | 0.56) | (0.32 | 0.67) | (-0.87 | -0.29) |
| Obese I, black vs. white (ref) | 0.61 | -0.14 | 0.67 | -0.42 | 1.00 | 0.02 | 0.78 | -0.55 | 0.55 | -0.56 | ||||||||||
| (95% CI) | (0.46 | 0.81) | -0.38 | 0.11) | (0.50 | 0.88) | (-0.96 | 0.12) | (0.74 | 1.36) | (-0.41 | 0.46) | (0.53 | 1.15) | (-1.14 | 0.05) | (0.41 | 0.73) | (-0.75 | -0.37) |
| Overweight, black vs. white (ref) | 0.58 | -0.08 | 0.69 | -0.50 | 0.88 | 0.24 | 1.07 | 0.51 | 0.49 | -0.42 | ||||||||||
| (95% CI) | (0.47 | 0.72) | (-0.32 | 0.16) | (0.54 | 0.88) | (-0.87 | -0.12) | (0.69 | 1.13) | (-0.19 | 0.67) | (0.79 | 1.43) | (0.01 | 1.00) | (0.40 | 0.61) | (-0.62 | -0.22) |
| Healthy weight black vs. white (ref) | 0.49 | 0.11 | 0.80 | -0.34 | 0.88 | 0.16 | 0.74 | 0.12 | 0.48 | -0.27 | ||||||||||
| (95% CI) | (0.39 | 0.61) | (-0.22 | 0.44) | (0.61 | 1.05) | (-0.80 | 0.11) | (0.68 | 1.12) | (-0.25 | 0.56) | (0.52 | 1.03) | (-0.48 | 0.73) | (0.38 | 0.60) | (-0.59 | 0.05) |
Results in this table are derived from the full model (model 3) presented in Table 3. Covariates are omitted due to space limits
The white reference group for each category is at the same body weight (e.g., black obese II/III compared to white obese II/III)
Figure 1.
a & b Estimated medical expenditures by services, whites vs. blacks. Note: Bars in the figures represent the average adjusted medical expenditures by services and race (based on the results presented in Table 4). The error bars represent the 95% confidence intervals.
Our sensitivity analysis of including age-specific, standardized PCS and MCS scores did not change the results of each of the models presented above, and therefore PCS and MCS were not included in the final models.
DISCUSSION
In this study, we examined factors that could explain the black–white differences in medical expenditures and service utilization in each body weight category, along the dimensions of predisposing socio-economic characteristics, perceived health, health conditions, and health beliefs. We found that blacks in obese I class, overweight, and healthy weight categories were significantly less likely to incur any medical expenditures as compared to whites in the corresponding body weight category. However, after adjusting for these covariates, the difference in possibility of having any medical expenditures between blacks and whites in obese II/III class was no longer significant, which is probably due to the small sample size in this weight category. Among those who used health care, the black–white difference always suggest that blacks used less but was significant only for those in obese I class. This suggests that black–white differences in total medical expenditures can be fully explained by the included covariates for those in obese II/III class, but not for those in obese I class, overweight, or healthy weight categories.
To further investigate, we found that blacks were less likely to have office-based visits, hospital outpatient visits and medications than whites in each of the overweight, obese I and II/III class categories. While healthy weight and overweight blacks spent significantly more on inpatient and ER visits than whites in the corresponding weight categories. This suggests that black–white differences in medical expenditures are largely due to relatively inexpensive types of care (office-based visits, outpatient care, medication) rather than more costly ones (inpatient care, ER). Lower spending on office-based visits and medications among those blacks who already used such care may be an indication of low adherence among blacks. For example, poor adherence to medications among black hypertension patients has been well-documented.21
Previous research indicated that blacks used less necessary care than whites,22 which suggests that the racial differences we observed may be due more to blacks’ underuse of care than whites’ overuse of care. However, research also suggests that rates of obesity-care are low for both blacks and whites.23Assuming that obesity care is not optimized for blacks or whites, obesity expenditures and utilization may be low for both groups, making our finding of lower rates of spending among blacks particularly concerning, given their higher average BMI in each weight category. Also consistent with previous research,9 we found that socio-demographic characteristics, health conditions, smoking status and perceived health status predicted medical expenditures and that health insurance was related to significantly a higher likelihood of health care utilization. An interesting contribution of this study is to include the health beliefs in the analysis, and we found that were associated with lower medical expenditures, but still did not explain away the black–white differences for those in obese I class, overweight and healthy weight categories.
There are several limitations to this study. First, our reliance on cross-sectional data limits our ability to make causal inferences. Secondly, MEPS data relies on self-reported height and weight, which may underestimate the obese population. Although one study reported that self-reported weight was larger in telephone interviews than in-person interviews.24 Nevertheless, there is no nationally representative data set that includes both objectively measured height and weight and medical expenditures. The lack of direct measures of the operation of health care systems, the legal and regulatory climate, or discrimination22 precludes us from further segmenting the factors associated with black–white differences in medical expenditures. For example, studies using data from the Behavioral Risk Factor Surveillance System survey have reported that racial perceived discrimination in health care was much more prevalent for blacks than whites or Hispanics.25
CONCLUSION
Black–white racial differences in total medical expenditures exist in each weight category, which are significant in obese I class, overweight, and healthy weight categories. These differences cannot be fully explained by predisposing socio-demographics, health conditions, or health beliefs. Blacks-white differences in medical expenditures may be largely due to relatively inexpensive types of care (office-based visits, outpatient care, medication) rather than more costly ones (inpatient care, ER). Our study suggests that blacks, although more likely to be obese or overweight, spent less on obesity-related medical expenditures than whites. Future studies should focus on the factors that contribute to these black–white differences in medical expenditures and service utilization. In particular, direct measures on health care systems and perceived discriminations that may explain such differences are important. A better understanding in this area will help inform the development of interventions designed to close the gap in medical expenditures between blacks and whites.
Acknowledgements
This research was supported by grant# P60MD000214-01 from the National Center on Minority Health and Health Disparities (NCMHD) of the National Institutes of Health (NIH). The authors greatly appreciate the three anonymous reviewers’ constructive comments and suggestions.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Contributor Information
Sai Ma, Phone: +1-410-5029317, Email: sma@jhsph.edu.
Kevin D. Frick, Phone: 1-410-6144018, Email: kfrick@jhsph.edu.
Sara Bleich, Phone: +1-410-5026604, Email: sbleich@jhsph.edu.
Lisa Dubay, Phone: +1-202-2615417, Email: LDubay@urban.org.
References
- 1.US Department of Health and Human Services, Healthy People 2020. Available at: http://www.healthypeople.gov/2020/topicsobjectives2020/default.aspx Accessed on December 27, 2011.
- 2.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999-2008. JAMA. 2010;303(3):235–41. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 3.Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: payer- and service-specific estimates. Health Aff (Millwood) 2009;28(5):w822–31. doi: 10.1377/hlthaff.28.5.w822. [DOI] [PubMed] [Google Scholar]
- 4.Bach PB, Cramer LD, Warren JL, Begg CB. Racial differences in the treatment of early-stage lung cancer. N Engl J Med. 1999;341:1198–205. doi: 10.1056/NEJM199910143411606. [DOI] [PubMed] [Google Scholar]
- 5.Trivedi AN, Zaslavsky AM, Schneider EC, Ayanian JZ. Relationship between quality of care and racial disparities in Medicare health plans. JAMA. 2006;296(16):1998–2004. doi: 10.1001/jama.296.16.1998. [DOI] [PubMed] [Google Scholar]
- 6.Schneider EC, Zaslavsky AM, Epstein AM. Racial disparities in the quality of care for enrollees in Medicare managed care. JAMA. 2002;13(287(10)):1288–94. doi: 10.1001/jama.287.10.1288. [DOI] [PubMed] [Google Scholar]
- 7.Canto JG, Allison JJ, Kiefe CI, Fincher C, Farmer R, Sekar P, Person S, Weissman NW. Relation of race and sex to the use of reperfusion therapy in Medicare beneficiaries with acute myocardial infarction. N Engl J Med. 2000;342:1094–100. doi: 10.1056/NEJM200004133421505. [DOI] [PubMed] [Google Scholar]
- 8.Sheifer SE, Escarce JJ, Schulman KA. Race and sex differences in the management of coronary artery disease. Am Heart J. 2000;139:848–57. doi: 10.1016/S0002-8703(00)90017-6. [DOI] [PubMed] [Google Scholar]
- 9.Wee CC, Phillips RS, Legedza AT, Davis RB, Soukup JR, Colditz GA, Hamel MB. Health care expendituress associated with overweight and obesity among US adults: importance of age and race. Am J Public Health. 2005;95(1):159–65. doi: 10.2105/AJPH.2003.027946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Waidmann T. Estimating the cost of racial and ethnic health disparities. The Urban Institute. 2009.
- 11.Andersen RM, McCutcheon A, Aday LA, Chiu GY, Bell R. Exploring dimensions of access to medical care. Health Serv Res. 1983;18(1):49–74. [PMC free article] [PubMed] [Google Scholar]
- 12.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1–10. doi: 10.2307/2137284. [DOI] [PubMed] [Google Scholar]
- 13.Janz NK, Becker MH. The health belief model: a decade later. Health Educ Q. 1984;11(1):1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- 14.Ezzati-Rice TM, Kashihara D, Machlin SR. Health care expenses in the United States. 2000 Rockville (MD): Agency for Healthcare Research and Quality; 2004. MEPS Research Findings No. 21. AHRQ Pub. No. 04-0022.
- 15.Executive summary of the clinical guidelines of the identification, evaluation, and treatment of overweight and obesity in adults, Arch Intern Med. 1998; 159:1855–1867. [DOI] [PubMed]
- 16.Singh GK, Kogan MD, Dyck PC, Siahpush M. Racial/ethnic, socioeconomic, and behavioral determinants of childhood and adolescent obesity in the United States: analyzing independent and joint associations. Ann Epidemiol. 2008;18(9):682–95. doi: 10.1016/j.annepidem.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 17.Finkelstein E, Fiebelkorn I, Wang G. National medical spending attributable to overweight and obesity: how much and who’s paying? Health Aff. 2003;W3:219–26. doi: 10.1377/hlthaff.w3.219. [DOI] [PubMed] [Google Scholar]
- 18.Cohen SB. Attitudes toward Health Insurance and Their Persistence over Time, Adults 2003–2004. Statistical Brief #161. February 2007. Agency for Healthcare Research and Quality, Rockville, Md. Available at: http://www.meps.ahrq.gov/mepsweb/data_files/publications/st161/stat161.pdf Accessed on December 27, 2011.
- 19.Finkelstein E, Trogdon JG, Brown DS, Allaire BT, Dellea PS, Kamal-Bahl SJ. The lifetime medical cost burden of overweight and obesity: implications for obesity prevention. Obesity. 2008;16(8):1843–8. doi: 10.1038/oby.2008.290. [DOI] [PubMed] [Google Scholar]
- 20.Fleishman JA, Cohen JW, Manning WG, Kosinski M. Using the SF-12 health status measure to improve predictions of medical expendituress. Med Care. 2006;44(5 Suppl):I54–63. doi: 10.1097/01.mlr.0000208141.02083.86. [DOI] [PubMed] [Google Scholar]
- 21.Dickson M, Plauschinat CA. Racial differences in medication compliance and healthcare utilization among hypertensive Medicaid recipients: fixed-dose vs. free-combination treatment. Ethn Dis. 2008;18(2):204–9. [PubMed] [Google Scholar]
- 22.Unequal treatment: confronting racial and ethnic disparities in health care. Washington: National Academies Press; 2002. [PubMed] [Google Scholar]
- 23.Bleich SN, Pickett-Blakely O, Cooper LA. Physician practice patterns of obesity diagnosis and weight-related counseling. Patient Educ Couns. 2011;82:123–9. doi: 10.1016/j.pec.2010.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ezzati M, Martin H, Skjold S, Hoorn SV, Murray CJ. Trends in national and state-level obesity in the USA after correction for self-report bias: analysis of health surveys. J R Soc Med. 2006;99:250–7. doi: 10.1258/jrsm.99.5.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hausmann LR, Jeong K, Bost JE, Ibrahim SA. Perceived discrimination in health care and health status in a racially diverse sample. Med Care. 2008;46(9):905–14. doi: 10.1097/MLR.0b013e3181792562. [DOI] [PMC free article] [PubMed] [Google Scholar]