Abstract
Objective
Based on conceptual models of addiction and affect regulation, this study examined the mechanisms linking current major depressive syndrome (MDS) and anxiety syndrome (AS) to postpartum smoking relapse.
Method
Data were collected in a randomized clinical trial from 251 women who quit smoking during pregnancy. Simple and multiple mediation models of the relations of MDS and AS with postpartum relapse were examined using linear regression, continuation ratio logit models, and a Bootstrapping procedure to test the indirect effects.
Results
Both MDS and AS significantly predicted postpartum smoking relapse. After adjusting for MDS, AS significantly predicted relapse. However, after adjusting for AS, MDS no longer predicted relapse. Situationally-based self-efficacy, expectancies of controlling negative affect by means other than smoking, and various dimensions of primary and secondary tobacco dependence individually mediated the effect of both MDS and AS on relapse. In multiple mediation models, self-efficacy in negative/affective situations significantly mediated the effect of MDS and AS on relapse.
Conclusion
The findings underscore the negative impact of depression and anxiety on postpartum smoking relapse, and suggest that the effects of MDS on postpartum relapse may be largely explained by comorbid AS. The current investigation provided mixed support for affect regulation models of addiction. Cognitive and tobacco dependence-related aspects of negative and positive reinforcement significantly mediated the relationship of depression and anxiety with relapse, while affect and stress did not. The findings emphasize the unique role of low agency with respect to abstaining from smoking in negative affective situations as a key predictor of postpartum smoking relapse.
Keywords: postpartum smoking relapse, mediators, depression, anxiety
Approximately 35-60% of women who smoke cigarettes quit after becoming pregnant (Tong, Jones, Dietz, D’Angelo, & Bombard, 2009). The majority of these women quit during the first trimester and stay quit until the end of their pregnancy (Solomon & Quinn, 2004). However, even after achieving these relatively long periods of abstinence, relapse rates during the postpartum period range from approximately 45% at 2-3 months postpartum up to 80% at one year (Mullen, 2004; Ratner, Johnson, Bottorff, Dahinten, & Hall, 2000). Thus, the tremendous public health opportunity to protect women against tobacco-related health problems, protect infants from environmental tobacco smoke, and decrease the risk of poor outcomes in future pregnancies is not being fully realized.
Unfortunately, reviews have concluded that interventions designed to prevent postpartum relapse are not effective (Agboola, McNeill, Coleman, & Leonardi Bee, 2010), although some recent interventions show promise (French, Groner, Wewers, & Ahijevych, 2007; Reitzel et al., 2010). The development of effective interventions for this special population may be constrained by insufficient knowledge of the specific mechanisms underlying postpartum smoking relapse. A more complete conceptual understanding of postpartum smoking relapse could aid in identifying subgroups of mothers at higher risk of relapse and in more effective tailoring of interventions to sustain long-term quitting.
Depression, Anxiety, and Postpartum Smoking Relapse
Among the more potent and consistent predictors of smoking prevalence and relapse following a cessation attempt are mental health disorders, with depression playing a particularly prominent role. Depression is more prevalent among smokers than non-smokers (Ziedonis et al., 2008) with smoking rates of nearly 50% in depressed individuals. Further, a current or past diagnosis of major depression is associated with early smoking lapses (Japuntich et al., 2007). Pregnant smokers are also more likely to have a major depressive disorder compared to pregnant women who do not smoke (Goodwin, Keyes, & Simuro, 2007), and those with current depressive disorders have lower abstinence rates at one month postpartum (Blalock, Robinson, Wetter, & Cinciripini, 2006). Among women who quit smoking during pregnancy, a history of depression is associated with postpartum smoking relapse (Park, Chang, Quinn, Regan, & Cohen, 2009).
Compared to depression, the body of research on the role of anxiety disorders in smoking prevalence and relapse is more limited. Nevertheless, there is evidence indicating that anxiety disorders are associated with smoking status among both in the general population (Ziedonis et al., 2008) and among pregnant women (Goodwin et al., 2007), and that a current or past history of an anxiety disorder predicts relapse (Piper, Cook, Schlam, Jorenby, & Baker, 2011). Thus, both depression and anxiety disorders play an important role in smoking behaviors and these relationships may be particularly important among women (Borrelli, Bock, King, Pinto, & Marcus, 1996).
Although the relationship of depression and anxiety with smoking relapse has been documented, few studies have examined the mechanisms underlying these relationships. Moreover, because depression and anxiety are highly comorbid conditions, the independent contribution of depression or anxiety to relapse is unclear (Japuntich et al., 2007; Mykletun, Overland, Aaro, Liabo, & Stewart, 2008; Piper et al., 2010). In addition, to the best of our knowledge, no studies have investigated the specific mechanisms linking current depression and anxiety to postpartum smoking relapse. However, a variety of factors have been shown to predict relapse in the general population, with a number of constructs appearing likely to help explain the relationship of depression and anxiety with postpartum smoking relapse. The purpose of the current study was to address this gap.
Hypothesized Mechanisms Underlying the Association of Depression and Anxiety with Postpartum Smoking Relapse
Negative Reinforcement/Negative Affect
Conceptual models of addiction have featured affect regulation as a major mechanism underlying addiction and relapse, with negative reinforcement playing a particularly prominent role (Baker, Piper, McCarthy, Majeskie, & Fiore, 2004). According to these models, negative affect is construed as a prototypical setting event or high risk situation that, in conjunction with cognitions, influences a person’s vulnerability to relapse. Escape, avoidance, or relief of negative affect (i.e. negative reinforcement) is hypothesized to be a principal motive for addictive drug use and relapse. In negative affective states, outcome expectancies for coping with negative affect via smoking or some other response, as well as self-efficacy for abstaining from smoking, are key mechanisms influencing whether the individual relapses or not (Baker et al.; Witkiewitz & Marlatt, 2004).
Empirical studies have provided general support for such models in that specific indicators of negative reinforcement such as negative affect, stress, self-efficacy in negative affect situations, and negative affect control expectancies have been among the better predictors of smoking relapse (Gwaltney, Shiffman, Balabanis, & Paty, 2005; Schleicher, Harris, Catley, & Nazir, 2009; Shiffman, 2005; Shiffman & Waters, 2004; Wetter et al., 1994). In fact, self-efficacy has been shown to partially mediate the relationship between depressive symptoms and relapse in the general population (Cinciripini et al., 2003). In both prospective and retrospective studies, negative affect and stress are among the most frequently identified factors for postpartum smoking relapse (Park et al., 2009; Polanska, Hanke, Sobala, Lowe, & Jaakkola, 2010; Solomon et al., 2007). Although there are few empirical data addressing the influence of self-efficacy and negative affect control expectancies on postpartum relapse (de Vries & Backbier, 1994), qualitative inquiries indicate that women frequently attribute postpartum smoking relapse to using smoking as a means of coping with negative affect and stressful situations (Park et al., 2009). In this study, indicators of Negative Reinforcement/Negative Affect included negative affect, stress, self-efficacy in negative affect situations, negative affect control expectancies, and the negative reinforcement dimension of tobacco dependence.
Positive Reinforcement/Positive Affect
Positive reinforcement is another factor used to explain addictive drug use and relapse. According to a multidimensional model of tobacco dependence, positive reinforcement is characterized by the desire to smoke to experience a “high” or to enhance an already positive feeling or experience (Piper et al., 2004). In addition, positive affect may increase the likelihood of relapse by signaling reward or serving to inflate the incentive value of smoking, or increase in anticipation of smoking or as a consequence of smoking (Robinson & Berridge, 2008). Unfortunately, affect measured when not in the specific context (e.g. the typical questionnaire format) may make it difficult to adequately distinguish amongst these various functions.
Compared to negative reinforcement, the relation of potential indicators of positive reinforcement/positive affect with relapse has received less empirical support. Some evidence suggests that positive affect predicts urges to smoke (Zinser, Baker, Sherman, & Cannon, 1992), and is associated with relapse (Brandon, Tiffany, Obremski, & Baker, 1990), particularly when the individual has low self-efficacy to refrain from smoking in the presence of positive affect (Velicer, DiClemente, Rossi, & Prochaska, 1990). However, some recent prospective studies have failed to support positive affect as a predictor of relapse (Shiffman & Gwaltney, 2008). Positive affect has also been found to protect against smoking relapse during and following pregnancy (Levine, Marcus, Kalarchian, Houck, & Cheng, 2010), perhaps because it may also serve as an indicator of low anhedonia or negative affect. Thus, the influence of positive reinforcement and positive affect on postpartum smoking relapse warrants further study. In this investigation, the indicators of Positive Reinforcement/Positive Affect include positive affect, self-efficacy in positive/social situations, and positive reinforcement motives for smoking.
Primary Tobacco Dependence
Tobacco dependence is a primary factor influencing relapse. Beyond the traditional concept of physical addiction, dependence has been conceptualized as a multidimensional construct (Piper, McCarthy et al., 2008) with one model categorizing various dimensions into higher order factors reflecting the primary (i.e. physical) and secondary (i.e. affective, contextual) aspects of dependence (Piper, Bolt et al., 2008). For instance, primary dependence refers to a pattern of smoking that is heavy, automatic, unrelated to consequences and generally unresponsive to instrumental contingencies. In contrast, secondary dependence involves more conscious instrumental motives guided by internal or external cues and the anticipated consequences of smoking. Greater primary dependence increases risk for relapse (Piper, Bolt et al., 2008) and has been hypothesized to account for the affect-smoking relationship (Baker et al., 2004).
Strong associations of tobacco dependence with depression and anxiety disorders have been found both among the general population (Ziedonis et al., 2008) and among pregnant women (Goodwin et al., 2007). Some markers of dependence, such as urges and number of cigarettes smoked, have predicted postpartum relapse (Mullen, 2004; Polanska et al., 2010; Ratner et al., 2000). However, whether specific dimensions of primary tobacco dependence operate as mediators of the relationship between depression and anxiety with postpartum smoking relapse remains to be determined. In this study, craving, tolerance, automaticity, and loss of control were used to index Primary Tobacco Dependence.
Social Support
Social support has also been studied as a potential factor influencing the affect-smoking relationship and smoking relapse. Abstinence-specific support from family, friends, and co-workers has been associated with lower relapse rates (Gulliver, Hughes, Solomon, & Dey, 1995). Specifically, high positive support appears to promote initial periods of abstinence, whereas low negative support predicts the maintenance of abstinence (Lawhon, Humfleet, Hall, Munoz, & Reus, 2009). Among types of social support, partner support is particularly important in the maintenance of abstinence and has accounted for nearly one third of the variance in relapse in some research (Coppotelli & Orleans, 1985). Further, both social support and partner support can decrease negative affective states (including stress and depression), increase positive affect, and reinforce self-efficacy (Lawhon et al.; Paykel, 1994). Research on the influence of social and partner support on postpartum relapse has yielded mixed results. Some research suggests that partner support is not associated with relapse (McBride et al., 1998), while other research identified partner support as a protective factor against postpartum relapse (Polanska et al., 2010). Consequently, whether social and partner support influence postpartum smoking relapse, and potentially account for the relationship between affective vulnerability and relapse, remains to be empirically determined. In this study, appraisal, belonging, and tangible dimensions of social support as well as positive and negative partner support, served as indicators of Social Support.
Study Purpose
In sum, multiple factors have been related to relapse both in the general population of smokers and among pregnant/postpartum women, many of which have been hypothesized to account for the affect-smoking relationship. To the best of our knowledge, there are no published studies that examine the mediating factors linking current depression and anxiety syndromes with postpartum relapse to smoking. The identification of such mechanisms may be useful in identifying treatment targets and developing effective interventions aimed at reducing relapse in this unique population. Thus, the specific objective of this study was to assess the mediating effects of indicators of Negative Reinforcement/Negative Affect, Positive Reinforcement/Positive Affect, Primary Tobacco Dependence, and Social Support on the relationship between current depression or anxiety syndrome and postpartum smoking relapse.
Method
Participants
The current study utilized data from a randomized clinical trial evaluating the efficacy of a postpartum smoking relapse prevention intervention (Reitzel et al., 2010). Participants were 251 pregnant women recruited from the Houston metropolitan area via a local health care organization, and through radio, newspaper, clinic, and bus advertisements. To be eligible, women aged 18 years or older must have smoked an average of at least one cigarette per day during the year prior to pregnancy, have stopped smoking during their pregnancy or within two months prior to becoming pregnant, and have a gestational age of 30-33 weeks at the time of study enrollment. Prepartum abstinence was biochemically verified at the onsite visit conducted between 30-33 weeks of pregnancy by an expired carbon monoxide (CO) level of less than 10ppm (Reitzel et al., 2010). Women who reported a high risk pregnancy were excluded from the sample.
Procedures
The study was approved by the Institutional Review Board. Written informed consent was obtained at the baseline visit (i.e. 30-33 weeks of pregnancy). At the conclusion of the baseline visit, women were randomized to one of three intervention groups: Usual Care (UC), Motivation and Problem Solving (MAPS), or an enhanced Motivation and Problem Solving (MAPS+). UC participants received self-help materials and Guideline-based (Fiore et al., 2008) brief relapse prevention advice, whereas both the MAPS and MAPS+ groups were provided with six telephone counseling sessions (weeks 34 and 36 prepartum, and weeks 2, 4, 7 and 16 postpartum). MAPS+ participants also received in-person counseling sessions at the baseline and 8 week visits. Follow-up data were collected at 8 and 26 weeks postpartum. Attrition rates were 20.7% at week 8, and 25.9% at week 26. More in-depth details regarding the study design, treatments, and outcome have been published previously (Reitzel et al., 2010).
Measures
All demographics, diagnoses, and proposed mediator variables were measured at the baseline visit. The outcome variable (i.e., relapse) was assessed at 8 and 26 weeks postpartum.
Demographics
Demographic data included age, partner status, education, and race/ethnicity.
Major Depressive Syndrome and Anxiety Syndrome
Major Depressive Syndrome (MDS) and Anxiety Syndrome (AS) were derived using the Patient Health Questionnaire (PHQ; Kroenke, Spitzer, Williams, & Lowe, 2010), a widely used screening instrument that utilizes diagnostic criteria from the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV;American Psychiatric Association, 2000). The PHQ MDS scale is composed of 9 items capturing how much the person was bothered by each depressive symptom during the last 2 weeks. Response options are not at all, several days, more than half the days, and nearly every day. Presence of MDS is indicated by endorsement of five or more symptoms at the more than half the days/nearly every day level, including at least one of the first two criteria (i.e. little interest or pleasure in doing things; or feeling down, depressed, or hopeless). The item related to suicidal thoughts is counted toward the total if endorsed as several days or more. The PHQ AS scale is comprised of 7 items with response options of not at all, several days and, more than half the days. Presence of AS is indicated by endorsement of the first criteria (i.e. feeling anxious or worrying a lot) and three additional symptoms at the more than half the days level for the last 4 weeks. The PHQ has been shown to be a reliable and valid screener for a diagnosis of depression and anxiety disorders, and is highly related, with good sensitivity and specificity, to clinical diagnoses of Major Depressive Disorder and Generalized Anxiety Disorder. Internal reliability coefficients are .86-.89 for the depression scale and .92 for the anxiety scale (Kroenke et al., 2010).
Affect
Affect over the previous week was measured by the Positive and Negative Affect Schedule (PANAS; Watson, Clark, & Tellegen, 1988) which consists of 20 adjectives comprising two subscales: Positive Affect and Negative Affect. Subscale scores range from 10 to 50, and higher scores indicate higher positive and negative affect. The PANAS is a reliable and valid measure of affect (Crawford & Henry, 2004) and the subscales predict relapse (Businelle et al., 2010).
Stress
The short form of the Perceived Stress Scale (PSS; Cohen, Kamarck, & Mermelstein, 1983) is a 4-item instrument designed to measure the degree to which individuals perceive their lives as stressful. Scores range from 0 to 16 and higher scores indicate greater perceived stress. Internal consistency is high (Nosek, Hughes, & Wright, 2003) and elevated scores are predictive of relapse (Wetter et al., 1994).
Self-efficacy
The Self-efficacy/Confidence Inventory is a 9-item scale that measures confidence for coping with high-risk situations without smoking (Velicer et al., 1990). In addition to a total score, this instrument comprises three subscales: Positive/Social, Negative/Affective, and Habit/Addictive. Higher scores are indicative of increased self-efficacy, and predict a lower likelihood of relapse (Businelle et al., 2010).
Negative affect control expectancies
The Affective Information Processing Questionnaire (AIPQ; Wetter, Brandon, & Baker, 1992) measures expectancies related to affect regulation. Participants read 10 vignettes characterized by negative affect and rate the controllability of their negative affect in that situation both by smoking and by means other than smoking. Higher scores are related to greater likelihood of relapse (Businelle et al., 2010).
Tobacco dependence
The Wisconsin Inventory of Smoking Dependence Motives (WISDM; Piper, Bolt et al., 2008) was used to assess tobacco dependence. The WISDM is a multidimentional measure of dependence composed of 13 subscales that are further grouped into two higher order dimensions yielding scores for Primary Dependence (Automaticity, Craving, Loss of Control, and Tolerance) and Secondary Dependence (Affiliative Attachment, Behavioral Choice, Cognitive Enhancement, Cue Exposure, Negative Reinforcement, Positive Reinforcement, Social Environmental Goads, Taste/Sensory Processes, and Weight Control). Of particular interest in the current study were the Primary Dependence subscales and the Secondary Dependence subscales relevant to the proposed conceptual models (i.e. Negative Reinforcement, Positive Reinforcement). However, each of the WISDM subscales was examined as a potential mediator. The WISDM has adequate internal consistency, and higher scores are predictive of smoking relapse (Piper, Bolt et al., 2008).
Social support
The Interpersonal Support Evaluation List (ISEL; Cohen, Mermelstein, Kamarck, & Hoberman, 1985) is comprised of 12 items encompassing three subscales assessing specific functions of social support including Appraisal (availability of someone to talk with about problems), Belonging (availability of people with whom one can do activities), and Tangible (availability of others in a time of need), as well a total score. Low social support predicts smoking relapse (Businelle et al., 2010).
Partner support
Perceived Partner Support was assessed using a 5-item scale from McBride et al. (1998) that provides a measure of both Positive Support and Negative Support. The scales have good psychometric properties and have been previously validated among pregnant women (McBride et al., 1998).
Smoking status
Continuous smoking abstinence was assessed via a self-report of no smoking since the delivery date, and was biochemically verified by an expired carbon monoxide (CO) level of less than 10ppm or a saliva cotinine value of less than 20ng/ml (Reitzel et al., 2010). These measures were obtained for both the 8 and 26 week follow up assessments. For the purpose of this study, relapse was coded as 1 and abstinence was coded as 0. Following an intent-to-treat procedure, individuals lost to follow up were coded as relapsed.
Data Analyses
Several conceptual models were created and tested. Each of the conceptual models (i.e. Negative Reinforcement/Negative Affect, Positive Reinforcement/Positive Affect, Primary Dependence, and Social Support) included specific indicators that were tested as potential mediators both individually and in conjunction with the other indicators within the same conceptual model.
Criteria for mediation (Baron & Kenny, 1986) of the relationship of MDS with relapse include the following: (1) MDS (predictor variable) must be significantly associated with smoking relapse (path c); (2) MDS must be significantly associated with hypothesized mediator (affect, stress, self-efficacy, etc.; path a); (3) the hypothesized mediator must be significantly related to relapse (path b); and (4) the relationship between MDS and relapse (path c’) must be meaningfully reduced or eliminated when the mediator is added to the model. These criteria are identical for testing mediators of the relationship between AS and postpartum smoking relapse.
To test the criteria for mediation, continuation ratio (CR) logit models were used to explore the relationships between predictor variables (i.e. MDS and AS) and relapse. CR logit models are appropriate when ordered categories represent a progression through stages (e.g., relapsed at week 8, abstinent at week 8 but relapsed at week 26, and abstinent through week 26;Agresti, 2002). CR logit models operate by modeling the conditional probability of being abstinent at the current assessment point, given that the participant has been abstinent through the most recent assessment. Second, linear regressions were performed to examine associations between the predictor variables and hypothesized mediators. Third, CR logit models were also used to explore the relationships between hypothesized mediators and relapse, controlling for the predictor variable (Baron & Kenny, 1986; Preacher & Hayes, 2008).
To test the final criterion, simple mediation models were formed and tested for each candidate mediator that was related to both the predictor and outcome variables in the previous steps at a significance level of p < .10. Because the outcome was binary, paths b and c were standardized; and the proportion of the effect between the predictor and the outcome that was accounted for by the hypothesized mediator was calculated (MacKinnon, 2008). Simple mediation was conducted using a Bootstrapping procedure to test the indirect effects by performing 5000 resamples from the dataset. This approach has been recommended since it is a nonparametric method that does not assume normality of the sampling distribution, and has high power and a better control over Type I errors (Preacher & Hayes, 2008). Given that a participant could contribute data at more than one time point (e.g. week 8 and week 26), random sampling of the dataset was performed on subjects rather than on data points at each time period. Finally, within each conceptual model, significant mediators from the simple models were tested simultaneously in a multiple mediation model.
In addition to testing the specific conceptual models, an “empirical” multiple mediation model was created that included all of the significant simple mediators from the different conceptual models, as well as other secondary dependence subscales. To identify a reduced model, backward selection was conducted by consecutively dropping the least significant mediator from the model and re-fitting it until all remaining mediators were related to relapse at p < 0.20. Analyses were performed using PASW 17.0 and R version 2.11.1. Missing data were limited and were removed from analyses on a case-wise basis.
Results
Participant Characteristics
Participant characteristics by MDS and AS diagnoses are presented in Table 1. The sample was racially/ethnically diverse (36% White, 32% African American, 30% Latina, and 2% other). Mean age was 24.6 (SD = 5.3) years and 19% of women reported having less than a high school education. The majority of the women (63%) were married or living with their significant other. Eleven percent of the women (n = 28) met criteria for MDS and 13.5% (n = 34) met criteria for AS. No statistically significant differences were found between women with or without MDS, or between women with or without AS with respect to age, partner status, or race/ethnicity, although the association of education and MDS approached significance (Table 1).
Table 1. Participant characteristics by diagnosis of Major Depressive Syndrome (MDS) and Anxiety Syndrome (AS).
| MDS |
AS |
|||||
|---|---|---|---|---|---|---|
| Variables | Yes | No | p | Yes | No | p |
| Age, years; M (SD) | 23.1 (4.8) | 24.8 (5.3) | .120 | 23.3 (4.3) | 24.8 (5.4) | .111 |
| Education | .053 | .518 | ||||
| ≥ high school; n (%) | 19 (68) | 185 (83) | 29 (85) | 175 (81) | ||
| < high school; n (%) | 9 (32) | 38 (17) | 5 (15) | 42 (19) | ||
| Partner Status | ||||||
| married/married-like ; n (%) | 15 (54) | 143 (64) | .276 | 22 (65) | 136 (63) | .819 |
| single/divorced; n (%) | 13 (46) | 80 (36) | 12 (35) | 81 (37) | ||
| Race/Ethnicity | .595 | .120 | ||||
| White; n (%) | 8 (29) | 81 (36) | 8 (24) | 80 (37) | ||
| African American; n (%) | 9 (32) | 72 (32) | 9 (27) | 72 (33) | ||
| Latina; n (%) | 11 (39) | 65 (29) | 15 (41) | 62 (29) | ||
| Other; n (%) | 0 (0) | 5 (2) | 2 (6) | 3 (1) | ||
Note. Covariates include age, education, partner status and race/ethnicity.
Associations of MDS and AS with Postpartum Relapse
Controlling for demographics (i.e. age, education, partner status, race/ethnicity) and treatment, separate CR logit models were used to examine the effects of MDS and AS on relapse (path c). Women with MDS were significantly more likely to relapse than women without MDS (OR = 2.29, 95% CI = 1.01-5.74, p = .047). Similarly, women with AS were significantly more likely to relapse than women without AS (OR = 3.03, 95% CI = 1.38-7.30, p = .005). The relapse rates for both MDS and AS were 79% at 8 weeks and 93% at 26 weeks.
Associations of MDS and AS with Hypothesized Mediators
Controlling for demographics, separate linear regression analyses were performed to evaluate the associations of MDS and AS with hypothesized mediators (path a). Both MDS and AS were significantly associated with all indicators of the Negative Reinforcement/Negative Affect, Positive Reinforcement/Positive Affect, and Primary Dependence models, with three indicators of the Social Support model, and all indicators of Secondary Dependence Motives. Specifically, both MDS and AS were predictive of higher levels of negative affect, perceived stress, negative affect control expectancies by smoking, negative reinforcement motives, positive reinforcement motives, automaticity, loss of control, craving, tolerance, affiliative attachment, behavioral choice, cognitive enhancement, cue exposure, social-environmental goads, taste/sensory processes, and weight control (all p’s < .05). Also, both MDS and AS predicted lower levels of positive affect, self-efficacy for negative/affective situations, self-efficacy for positive/social situations, self-efficacy for habit/addictive situations, and negative affect control expectancies by means other than smoking (all p’s < .05).
Associations of Hypothesized Mediators with Postpartum Relapse
Separate CR logit models were conducted to test the relationships between the hypothesized mediators and postpartum relapse (path b), adjusting for demographics, treatment, and MDS or AS, respectively. Results are shown in Table 2.
Table 2. Relationships of hypothesized mediators with postpartum smoking relapse.
| Postpartum Smoking Relapse |
||||||
|---|---|---|---|---|---|---|
| Controlling for MDS |
Controlling for AS |
|||||
| Hypothesized Mediators | OR | 95% CI | p | OR | 95% CI | p |
| Negative Reinforcement/Negative Affect | ||||||
| Negative Affect | 1.010 | (0.979, 1.042) | 0.521 | 1.006 | (0.976, 1.037) | 0.703 |
| Perceived Stress | 1.066 | (0.981, 1.159) | 0.131 | 1.056 | (0.975, 1.144) | 0.182 |
| Self-efficacy Negative/Affective | 0.650 | (0.525, 0.805) | <0.001 | 0.644 | (0.521, 0.796) | <0.001 |
| Negative Affect control by other means | 0.816 | (0.683, 0.976) | 0.024 | 0.822 | (0.688, 0.982) | 0.028 |
| Affect control by smoking | 1.047 | (0.913, 1.201) | 0.509 | 1.030 | (0.897, 1.183) | 0.673 |
| Negative Reinforcement Motives | 1.219 | (1.061, 1.401) | 0.005 | 1.208 | (1.052, 1.387) | 0.007 |
| Positive Reinforcement/Positive Affect | ||||||
| Positive Affect | 0.994 | (0.965, 1.023) | 0.663 | 0.996 | (0.968, 1.024) | 0.761 |
| Self-efficacy Positive/Social | 0.620 | (0.474, 0.812) | <0.001 | 0.627 | (0.479, 0.821) | <0.001 |
| Positive Reinforcement Motives | 1.166 | (0.996, 1.366) | 0.053 | 1.160 | (0.991, 1.358) | 0.061 |
| Primary Dependence | ||||||
| Automaticity | 1.248 | (1.057, 1.473) | 0.008 | 1.227 | (1.037, 1.451) | 0.015 |
| Loss of Control | 1.054 | (0.886, 1.255) | 0.550 | 1.055 | (0.885, 1.257) | 0.549 |
| Craving | 1.126 | (0.966, 1.312) | 0.125 | 1.120 | (0.961, 1.306) | 0.143 |
| Tolerance | 1.161 | (0.985, 1.367) | 0.070 | 1.148 | (0.972, 1.356) | 0.099 |
| Self-efficacy Habit/Addictive | 0.695 | (0.508, 0.951) | 0.020 | 0.697 | (0.509, 0.954) | 0.022 |
| Social Support | ||||||
| Appraisal | 1.020 | (0.938, 1.109) | 0.640 | 1.031 | (0.948, 1.121) | 0.473 |
| Belonging | 1.026 | (0.939, 1.120) | 0.572 | 1.017 | (0.934, 1.107) | 0.700 |
| Tangible | 1.027 | (0.930, 1.134) | 0.598 | 1.021 | (0.928, 1.122) | 0.674 |
| Positive Partner Support | 0.855 | (0.653, 1.117) | 0.251 | 0.862 | (0.659, 1.128) | 0.280 |
| Negative Partner Support | 1.182 | (0.815, 1.714) | 0.378 | 1.158 | (0.798, 1.682) | 0.440 |
| Other Secondary Dependence Motives | ||||||
| Affiliative Attachment | 1.154 | (0.935, 1.425) | 0.174 | 1.131 | (0.914, 1.399) | 0.253 |
| Behavioral Choice | 1.113 | (0.886, 1.398) | 0.353 | 1.111 | (0.888, 1.389) | 0.354 |
| Cognitive Enhancement | 1.102 | (0.937, 1.294) | 0.237 | 1.072 | (0.910, 1.264) | 0.404 |
| Cue Exposure | 1.232 | (1.059, 1.434) | 0.006 | 1.223 | (1.051, 1.423) | 0.009 |
| Social Environmental | 1.125 | (0.994, 1.273) | 0.061 | 1.130 | (0.999, 1.276) | 0.050 |
| Taste/Sensory | 1.095 | (0.945, 1.268) | 0.223 | 1.076 | (0.927, 1.248) | 0.334 |
| Weight Control | 1.079 | (0.945, 1.231) | 0.258 | 1.082 | (0.951, 1.231) | 0.231 |
Note. Covariates include age, education, race/ethnicity, partner status, and treatment group. Variables with p < .10 are shown in bold.
Mediation Analyses
Conceptual models
Because both MDS and AS significantly predicted postpartum relapse, the indirect effects of potential mediators significant at p < .10 in the a and b paths were examined using a bootstrapping approach. Within the Negative Reinforcement/Negative Affect model, potential mediators included negative affect control expectancies by means other than smoking, self-efficacy in negative/affective situations, and negative reinforcement motives. Within the Positive Reinforcement/Positive Affect model, potential mediators included self-efficacy in positive/social situations and positive reinforcement motives. Within the Primary Dependence model, potential mediators included automaticity, tolerance, and self-efficacy in habitual/addictive situations. Each of these potential mediators significantly mediated the effect of MDS on relapse after adjusting for demographics and treatment (all p’s ≤ .05; Table 3). Similarly, each of these potential mediators significantly mediated the effect of AS on postpartum smoking relapse after adjusting for demographics and treatment (all p’s ≤ .05; Table 3).
Table 3. Indirect effect of hypothesized mediators on the relationship of Major Depressive Syndrome (MDS) or Anxiety Syndrome (AS) with postpartum relapse.
| MDS |
AS |
|||||
|---|---|---|---|---|---|---|
| Hypothesized mediators | B | BC 95% CI | PME | B | BC 95% CI | PME |
| Simple Mediation | ||||||
|
| ||||||
| Negative Reinforcement/Negative Affect | ||||||
| Negative afffect control by other means | .06* | (0.00, 0.19) | 15.3 | .07* | (0.01, 0.18) | 11.8 |
| Self-efficacy Negative/Affective | .19*** | (0.08, 0.38) | 44.0 | .12* | (0.02, 0.27) | 21.0 |
| Negative Reinforcement Motives | .18** | (0.06, 0.36) | 39.0 | .13** | (0.04, 0.28) | 23.4 |
| Positive Reinforcement/Positive Affect | ||||||
| Self-efficacy Positive/Social | .11* | (0.02, 0.27) | 23.0 | .11* | (0.03, 0.27) | 19.4 |
| Positive Reinforcement Motives | .10* | (0.01, 0.25) | 21.0 | .08* | (0.01, 0.21) | 13.6 |
| Primary Dependence | ||||||
| Automaticity | .12** | (0.03, 0.31) | 25.9 | .12** | (0.03, 0.30) | 21.1 |
| Tolerance | .08* | (0.01, 0.22) | 16.5 | .07* | (0.00, 0.21) | 12.4 |
| Self-efficacy Habitual/Addictive | .10* | (0.02, 0.27) | 22.9 | .08* | (0.01, 0.22) | 14.2 |
| Other Secondary Dependence Motives | ||||||
| Cue Exposure | .14** | (0.05, 0.29) | 30.3 | .13** | (0.05, 0.27) | 21.9 |
| Social Environmental Goads | .11* | (0.00, 0.25) | 24.3 | .07* | (0.01, 0.19) | 11.6 |
|
| ||||||
| Multiple Mediation | ||||||
|
| ||||||
| Negative Reinforcement/Negative Affect | ||||||
| Negative Affect control by other means | .02 | (−0.05, 0.12) | 3.9 | .01 | (−0.06, 0.11) | 2.0 |
| Self-efficacy Negative/Affective | .15** | (0.04, 0.35) | 35.1 | .10* | (0.02, 0.26) | 16.6 |
| Negative Reinforcement Motives | .08 | (−0.05, 0.24) | 17.8 | .05 | (−0.05, 0.18) | 7.5 |
| Overall Model | .25** | (0.11, 0.45) | 56.8 | .16* | (0.03, 0.33) | 26.1 |
| Positive Reinforcement/Positive Affect | ||||||
| Self-efficacy Positive/Social | .10* | (0.01, 0.27) | 20.9 | .10* | (0.02, 0.26) | 16.6 |
| Positive Reinforcement Motives | .05 | (−0.04, 0.19) | 9.8 | .04 | (−0.03, 0.16) | 6.2 |
| Overall Model | .15* | (0.03, 0.32) | 30.7 | .14* | (0.03, 0.30) | 22.8 |
| Primary Dependence | ||||||
| Tolerance | −.01 | (−0.15, 0.11) | 2.2 | −.01 | (−0.15, 0.11) | 1.7 |
| Automaticity | .10 | (−0.01, 0.34) | 15.9 | .10 | (−0.03, 0.32) | 13.3 |
| Self-efficacy Habit/Addictive | .07 | (−0.01, 0.22) | 11.1 | .06 | (−0.004, 0.20) | 7.6 |
| Overall Model | .16* | (0.03, 0.34) | 24.7 | .15* | (0.04, 0.32) | 19.2 |
| Other Secondary Dependence Motives | ||||||
| Cue Exposure | .12** | (0.03, 0.27) | 26.4 | .11* | (0.02, 0.24) | 17.4 |
| Social Environmental Goads | .07 | (−0.05, 0.21) | 14.5 | .04 | (−0.02, 0.14) | 7.0 |
| Overall Model | .18** | (0.05, 0.36) | 40.9 | .15** | (0.05, 0.31) | 24.4 |
Note. Only variables related to MDS or AS and relapse at p < .10 were included in calculating indirect effects. Covariates include age, education, ethnicity/race, partner status, and treatment group. BC= Bias Corrected; PME= Proportion of mediated effect.
p ≤ .05
p ≤ .01
p ≤ .001
None of the indicators of the Social Support model were potential mediators. Among the other Secondary Dependence Motives, cue exposure and social environmental goads were potential mediators, and each of these constructs significantly mediated the effect of both MDS and AS on postpartum relapse (all p’s < .05; Table 3).
For each conceptual model, the individual mediators of the association of MDS and postpartum relapse were simultaneously examined in a multiple mediator model (Table 3). The indirect effect of the overall set of mediators in the Negative Reinforcement/Negative Affect model was significant. Examination of the individual effects of each mediating variable in the set revealed that only self-efficacy in negative/affective situations was a unique significant mediator. The indirect effect of the overall set of mediators in the Positive Reinforcement/Positive Affect model was also significant. When examining the individual effects of each mediating variable in this model, only self-efficacy in positive affect/social situations was a unique significant mediator. In addition, the indirect effect of the overall set of mediators in the Primary Dependence model was significant. However, none of the individual indirect effects of the indicators of Primary Tobacco Dependence were significant when entered as a set. Although not statistically significant, tolerance exhibited a small negative indirect path when included in the same model as automaticity and self-efficacy in habit/addictive situations. This is known as “inconsistent mediation”, and is not uncommon in multiple mediator models as the effect of a variable could be explained by the effects of other variables in the model (MacKinnon, Fairchild, & Fritz, 2007; Preacher & Hayes, 2008). Finally, the indirect effect of the overall set of indicators for Secondary Dependence Motives was significant. Examination of the individual effects of each mediating variable in this model revealed that cue exposure was a unique significant mediator.
Empirical models
Finally, an “empirical” multiple mediation model was created for both MDS and AS that included all of the significant simple mediators from the different conceptual models, including the other secondary dependence constructs. For the effect of MDS on postpartum relapse, a backward selection procedure yielded a final model composed of self-efficacy in negative/affective situations, automaticity, and social environmental goads, accounting for 68.7% of the effect of MDS on postpartum relapse (Table 4). Moreover, in the presence of automaticity and social environmental goads, only the confidence to resist smoking in negative/affective situations significantly mediated the effect of MDS on relapse, accounting for 38.5% of the total effect (Table 4). With respect to the effect of AS on postpartum relapse, the backward selection procedure yielded a final model comprised of self-efficacy in negative/affective situations, automaticity, and social environmental goads, accounting for 32.2% of the effect of AS on postpartum relapse (Table 4). In the presence of automaticity and social environmental goads, only the confidence to refrain from smoking in negative affect situations significantly mediated the effect of AS on relapse, accounting for 16.8% of the total effect (Table 4).
Table 4. Empirical multiple mediator model of the indirect effect of hypothesized mediators on the relationship of Major Depressive Syndrome (MDS) or Anxiety Syndrome (AS) with postpartum relapse.
| MDS |
AS |
|||||
|---|---|---|---|---|---|---|
| Mediators | B | BC 95% CI | PME | B | BC 95% CI | PME |
| Self-efficacy Negative/Affective | .17*** | (0.06, 0.34) | 38.5 | .17* | ( 0.02, 0.25) | 16.8 |
| Automaticity | .07 | (−0.01, 0.22) | 14.7 | .07 | (−0.03, 0.21) | 8.8 |
| Social Environmental Goads | .07 | (−0.05, 0.19) | 15.5 | .07 | (−0.01, 0.15) | 6.6 |
| Overall effect | .30*** | ( 0.14, 0.54) | 68.7 | .30** | ( 0.07, 0.40) | 32.2 |
Note. Only variables related to MDS or AS and relapse at p < .10 were included in calculating indirect effects. All individual mediators were included in a multiple mediator model, and a backward selection procedure was conducted by consecutively dropping the least significant mediator and re-fitting the model until all remaining mediators were related to relapse at p ≤ 0.20.
Covariates include age, education, race/ethnicity, partner status and treatment group.
BC= Bias Corrected; PME= Proportion of mediated effect.
*p ≤ .05
p ≤ .01
p ≤ .001
Additional Analyses
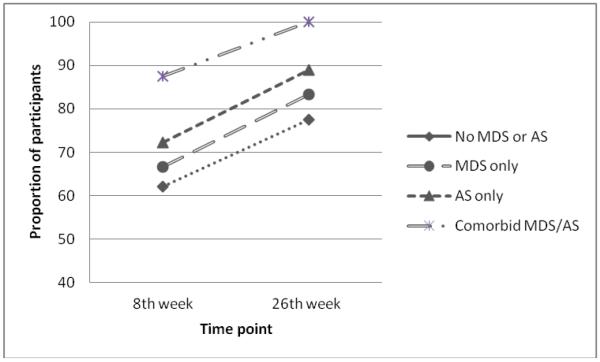
Given the almost identical relapse rates and mediation results for MDS and AS, the correlation between MDS and AS was calculated, and the effect of each disorder on postpartum relapse was examined after controlling for the effect of the other. Spearman’s rho correlation coefficient between MDS and AS was .451, indicating a correlation of a medium effect size (Cohen, 1988). After adjusting for MDS, AS significantly predicted postpartum relapse (p = .03). However, when adjusting for AS, MDS did not significantly predict relapse (p = .31). In addition, relapse rates were compared across four diagnostic categories: women with no MDS or AS disorder, MDS disorder only, AS disorder only, and those with comorbid MDS and AS disorders. As shown in Figure 1, when women met criteria for both disorders, their relapse rates were higher at both time points in comparison with women who had only a MDS or AS disorder, or no disorder Unfortunately, due to a small number of participants in some cells, further statistical analyses could not be conducted using this categorization scheme.
Figure 1.
Proportion of women relapsed at the 8th week and the 26th week, by diagnosis of MDS and AS
Discussion
The current study assessed the impact of a current depressive or anxiety syndrome on postpartum smoking relapse, as well as the potential mediators of these relationships. There were several key findings. First, among pregnant women, either a MDS or AS disorder was strongly predictive of postpartum smoking relapse. Second, the effect of MDS on postpartum relapse appeared to be due primarily to comorbid AS disorder given that AS continued to significantly predict postpartum relapse after controlling for MDS, but MDS no longer predicted postpartum relapse after controlling for AS. Third, the most potent mediator of the increased relapse risk posed by either AS or MDS was the woman’s belief regarding her ability to successfully cope with emotional distress without smoking. Indicators of both primary and secondary tobacco dependence motives also contributed.
Regarding the specific conceptual models, there was mixed support for factors related to Negative and Positive Reinforcement in mediating the effect of MDS and AS on postpartum relapse. Specifically, the cognitive (i.e., self-efficacy and negative affect control expectancies) and tobacco dependence dimensions of the Negative and Positive Reinforcement models were significant mediators of the association of both MDS and AS on relapse. Further, even in the presence of other significant mediators, situationally-based self-efficacy (negative/affective situations for Negative Reinforcement/Negative Affect and positive/social situations for Positive Reinforcement/Positive Affect) was a unique mediator of the effect of both MDS and AS on postpartum relapse. However, the affective components (i.e., negative affect and perceived stress in the Negative Reinforcement/Negative Affect model, and positive affect in the Positive Reinforcement/Positive Affect model) did not predict postpartum relapse. Finally, both primary and secondary aspects of Tobacco Dependence mediated the effects of MDS and AS on relapse. From the Primary Dependence model, automaticity, tolerance, and self-efficacy for habit/addictive situations significantly mediated the effects of MDS and AS on postpartum smoking relapse. Among the other Secondary Dependence Motives, significant mediation effects were found for cue exposure and social environmental goads. None of the indicators of the Social Support model were significant mediators between MDS or AS and postpartum smoking relapse.
Association of Depression and Anxiety with Postpartum Smoking Relapse
The findings of higher smoking relapse rates in women with a current prepartum depressive or anxiety syndrome are consistent with previous reports (Goodwin et al., 2007; Japuntich et al., 2007; Piper et al., 2011), highlighting the importance of current affective disorder as a risk factor for postpartum smoking relapse. These findings are particularly relevant given that previous research focusing on lifetime history of depression and long term smoking cessation outcomes, both in the general population and among pregnant women, have yielded mixed results (Hitsman, Borrelli, McChargue, Spring, & Niaura, 2003; Japuntich et al., 2007; Park et al., 2009). However, the significant association between depressive disorder and postpartum smoking relapse was eliminated after controlling for anxiety disorder, consistent with some previous findings indicating that the relationship between depressive disorder and smoking relapse may be explained in part by a comorbid anxiety disorder (Piper et al., 2010). These findings suggest that in comparison with depression, anxiety may have a stronger impact on postpartum relapse, and that some studies that do not account for the effects of anxiety could potentially overestimate the association between depression and smoking behaviors (Japuntich et al., 2007; Mykletun et al., 2008; Piper et al., 2010). Although the current study could not statistically evaluate the association of comorbid MDS and AS on postpartum smoking relapse due to small cell sizes, relapse rates were even higher for women with comorbid MDS and AS, consistent with Piper and colleagues’ findings. These findings across studies suggest that comorbid MDS and AS may raise the risk of smoking relapse above that attributable to either MDS and AS alone. Future studies evaluating the linkages among current depression, anxiety, and smoking relapse are clearly needed.
Role of Negative and Positive Reinforcement
There was mixed support for various components of affect regulation models of addiction (Baker et al., 2004). In particular, cognitive constructs significantly mediated the association of MDS and AS with postpartum relapse, but affect and stress did not. Consistent with the hypotheses, each of the situationally-based self-efficacy dimensions mediated the associations of depression and anxiety with postpartum relapse. In fact, self-efficacy for refraining from smoking in situations characterized by negative affect remained a significant mediator when all the potential mediators were included in an empirically-based multiple mediation model. In addition, expectancies for control of negative affect by means other than smoking, another cognitive component in the Negative Reinforcement/Negative Affect model, was a significant mediator of the association of MDS and AS with postpartum smoking relapse, in contrast to expectancies for controlling negative affect via smoking. These results parallel previous research in which self-efficacy mediated the association of depressive mood and smoking abstinence (Cinciripini et al., 2003), and underscore the crucial role of self-efficacy in accounting for the effects of depression and anxiety on smoking relapse. Importantly, this investigation extends previous work by illuminating the potent role of perceptions of human agency on behavior, particularly with respect to situations characterized by negative affect. These findings suggest that perceived agency is more influential in postpartum relapse than are negative affect or the expected effect of smoking on negative affect. Additional post hoc analyses indicated that self-efficacy for affective situations may not be more predictive than general self-efficacy (as measured by summing the three self-efficacy subscales; analyses not shown), suggesting that future research might attempt to disentangle any unique effects of self-efficacy in negative affect situations from those of more general self-efficacy.
Contrary to expectations, affect and stress were not related to postpartum relapse. Failing to detect a significant effect of negative affect, positive affect, and perceived stress on relapse may have several explanations. On one hand, although affect and stress are hypothesized to serve as setting events/high risk situations for relapse, their impact may largely depend upon cognitive factors, such as self-efficacy and negative affect control expectancies. On the other hand, the measurement of negative affect, positive affect, and stress was temporally distant from measures of relapse, they were not measured in context, and there was a major life event (e.g., birth) intervening between the assessment of affect/stress and relapse, all of which could lead to a lack of relationship between affect and relapse likelihood. Thus, this temporal distance, lack of context, and the lability of affect and stress may have diminished any potential association. For example, fluctuations in positive affect that occur either in anticipation, or in response, to smoking and that raise the likelihood of relapse were not captured. Importantly, negative affect is conceptualized as a main component of both MDS and AS (Watson, 2005). As such, the inclusion of the disorders themselves in the models may have captured the trait-like component of negative affect that is more stable from the pre to postpartum period. In sum, the relationship of cognitive and affective variables with smoking relapse is complex and may require greater study of the dynamic interactions among proximal measures (Shiffman, 2005; Van Zundert, Ferguson, Shiffman, & Engels, 2011).
Role of Primary Tobacco Dependence
Various aspects of Primary Tobacco Dependence (i.e. automaticity, tolerance, and self-efficacy in habitual/addictive situations) significantly mediated the effects of MDS and AS on postpartum relapse. Given that women were abstinent from tobacco at the time that dependence was measured (generally for relatively long durations) and the substantial time gap between the assessment of dependence and relapse, it may not be surprising that the degree to which smoking had become overlearned (automaticity), and the need to smoke increasing amounts to experience a desired effect (tolerance) mediated the association of MDS and AS with postpartum relapse to a greater extent than what might be considered more labile aspects of dependence such as craving and loss of control. In addition, self-efficacy to refrain from smoking in habitual/addictive situations became nonsignificant when included in the model with automaticity and tolerance, suggesting that self-efficacy related to primary dependence processes may be less influential than self-efficacy related to affective processes. The latter conclusion is also bolstered by the findings from the purely empirically-based model and the potent mediating effect of self-efficacy for negative/affective situations.
Role of Social Support
Contrary to expectations, the various indicators of social support and perceived partner support were not related to postpartum relapse. Previous research has yielded mixed results with some studies finding that support is associated with a lower likelihood of relapse in both the general population (Gulliver et al., 1995; Lawhon et al., 2009) and postpartum women (Polanska et al., 2010), and other studies showing no relationship (McBride et al., 1998). Similar to the failure to find an association of affect and stress with relapse, future research might attempt to address the relationship using more proximal and dynamic measures of support, especially during the postpartum period.
Implications of Findings
The birth of a child represents a profound life transition that encompasses a myriad of unique changes in diverse areas of a woman’s life (e.g., physiological changes associated with lactation, resumption of menstruation, and other hormonal alterations; social, family, caregiver, and employment roles; partner and social support; sleep disruption; stress; negative affect and depression; weight-related issues; loss of a fetus and introduction of a baby; etc.). These changes may have significant motivational consequences and may be relatively unique in terms of their intensity, duration, and cumulative or interactive effects. Further, one might expect that these changes may influence depressive and anxiety disorders. Thus, the findings showing the relation between prepartum depressive and anxiety disorders, as well as multiple mediators, with postpartum relapse are somewhat striking. In particular, indicators of affective processes, tobacco dependence, and self-efficacy served as underlying mediators of the association of depression and anxiety with postpartum relapse.
The findings have implications for both research and clinical practice. The results partially support current theories regarding the role of affect regulation in relapse. Although cognitive constructs and the negative and positive reinforcement aspects of nicotine dependence functioned as mediators, the lack of association between negative affect and stress with relapse did not support the pivotal role that these constructs have often played in previous research (Kenford et al., 2002). Similarly, there was a failure to identify an association of social and partner support with postpartum smoking relapse. However, it may be the case that more fine-grained methodological strategies such as ecological momentary assessment are necessary to adequately assess these relationships. Although it may be a challenge for this particular population during this specific time of life, future research addressing relapse among postpartum women is still needed, with a special focus on modeling dynamic relationships over time among key factors influencing relapse.
Another key issue in future research will be to tease apart the independent effects of depression and anxiety on postpartum relapse. In addition, the mediators in the final models explained a much larger proportion of the effect of MDS on relapse as compared to the effect of AS on relapse, suggesting that greater attention may need to be directed towards identifying mediators of the association of anxiety disorders with postpartum smoking relapse.
In comparison with the Positive Reinforcement/Positive Affect, Primary Dependence, and Social Support models, the Negative Reinforcement/Negative Affect model seemed to have particular relevance in this population, at least as indexed by the proportion of the mediated effect in the multiple mediation models. This finding is consistent with Kenford and colleagues’ (2002) work contrasting physical and affective models of dependence. They found that affective models were more predictive of relapse and may account for predictive relations typically attributed to physical dependence. However, the physical dependence model that they tested did not use a multidimensional measure such as the WISDM, and may have been less predictive as a result. Of course, alternative indicators for each of the conceptual models could have changed the findings and altered these conclusions.
With respect to clinical practice, the study highlights the importance of enhancing clinical recognition of depression and anxiety in pregnant women and ensuring that these women are offered support for maintaining abstinence after delivery. Also, the identification of mediators of the association of MDS and AS with relapse suggests that the development of tailored treatments that account for these factors could improve the efficacy of interventions. Given that negative affect, positive affect, and stress were not mediators, intervention strategies solely focused on improving mood and reducing stress might not suffice to prevent smoking relapse in postpartum women. In fact, results point toward specifically incorporating strategies to: (1) directly target women’s perceptions of agency for coping with negative affect without smoking, (2) decrease automatic smoking, perhaps through treatments such as mindfulness-based relapse prevention (Bowen & Marlatt, 2009), and (3) reduce the impact of environmental and social cues that might trigger smoking. Interventions that directly target these areas might be useful in helping postpartum women to avoid relapse.
Strengths and Limitations of the Study
To the best of our knowledge, this is the first study to examine the mediating factors linking depressive and anxiety syndromes with postpartum smoking relapse. Strengths of the current study include the use of valid and reliable assessment instruments and biochemical confirmation of smoking status, a semi-longitudinal design (Maxwell & Cole, 2007) and the testing of multiple mediators. A relatively large sample size for the particular population involved is also a strength.
Our study should be interpreted in light of various limitations. The study sample consists of women who quit smoking early in pregnancy and who volunteered to be in a research study. Thus, the findings may not be equally applicable to women who quit smoking later in pregnancy or to women who do not volunteer for a study. Also, it is important to highlight that because subjects cannot be randomly assigned to a diagnostic category, causal inferences regarding the potential effect of the disorder on relapse cannot be made. Although mediation analysis implies causality because it involves a very specific temporal order of relationships, demonstrating statistical mediation alone is not sufficient to establish causality (Maxwell & Cole, 2007), since only a true manipulation of the predictor variable can do that. Importantly, this study estimates path a using a cross sectional methodology during the prepartum period, limiting the ability of the model to faithfully detect specific causal pathways (Imai, Keele, & Tingley, 2010), especially when considering the potential impact of delivery and postpartum phenomena on variables that may not be stable over time. Nevertheless, given the lack of studies exploring predictors and mediators of postpartum relapse, this study provides a novel contribution to the field and can encourage additional research in this important area. Specifically, future research examining the mechanisms linking depression and anxiety to postpartum relapse would benefit from using a complete longitudinal design (Maxwell & Cole, 2007) where independent variables, mediators, and outcomes are measured at multiple time points.
Conclusion
In sum, the results underscore the negative impact of depression and anxiety syndromes on postpartum smoking relapse, and provide some suggestion of an even greater detrimental effect of comorbid depression and anxiety. The findings also suggest that the impact of a depressive disorder on postpartum relapse might be largely explained by a comorbid anxiety disorder. Furthermore, the current investigation provided mixed support for affect regulation models of addiction in that cognitive and tobacco dependence aspects of Negative and Positive Reinforcement models significantly mediated the relationship of depression and anxiety with relapse, while affect and stress were not associated with postpartum relapse. In particular, findings emphasize the unique role of agency for abstaining from smoking in negative affective situations as a key predictor of postpartum smoking relapse.
Acknowledgments
This research was supported by grants from the National Cancer Institute (R01CA89350, 5P30CA016672-35, R25T CA57730, two CURE Diversity Supplements to the R25T CA57730, and K01 CA157689). This work was also supported in part by the U54 CA096297/CA096300: UPR/MDACC Partnership for Excellence in Cancer Research. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute. Authors thank the reviewers for their thoughtful comments on this manuscript.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/ccp
References
- Agboola S, McNeill A, Coleman T, Leonardi Bee J. A systematic review of the effectiveness of smoking relapse prevention interventions for abstinent smokers. Addiction. 2010;105(8):1362–1380. doi: 10.1111/j.1360-0443.2010.02996.x. doi:10.1111/j.1360-0443.2010.02996.x. [DOI] [PubMed] [Google Scholar]
- Agresti A. Categorical data analysis. 2nd ed. John Wiley & Sons; Hoboken, NJ: 2002. [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders text revised. 4th ed. Author; Washington, DC: 2000. [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, Fiore MC. Addiction motivation reformulated: an affective processing model of negative reinforcement. Psychological Review. 2004;111(1):33–51. doi: 10.1037/0033-295X.111.1.33. doi:10.1037/0033-295X.111.1.33. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. doi:10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Blalock JA, Robinson JD, Wetter DW, Cinciripini PM. Relationship of DSM-IV-based depressive disorders to smoking cessation and smoking reduction in pregnant smokers. American Journal of Addictions. 2006;15:268–277. doi: 10.1080/10550490600754309. doi:10.1080/10550490600754309. [DOI] [PubMed] [Google Scholar]
- Borrelli B, Bock B, King T, Pinto B, Marcus BH. The impact of depression on smoking cessation in women. American Journal of Preventive Medicine. 1996;12(5):378–387. [PubMed] [Google Scholar]
- Bowen S, Marlatt A. Surfing the urge: brief mindfulness-based intervention for college student smokers. Psychology of Addictive Behaviors. 2009;23(4):666–671. doi: 10.1037/a0017127. doi:10.1037/a0017127. [DOI] [PubMed] [Google Scholar]
- Brandon TH, Tiffany ST, Obremski KM, Baker TB. Postcessation cigarette use: the process of relapse. Addictive Behaviors. 1990;15:105–114. doi: 10.1016/0306-4603(90)90013-n. doi:10.1016/0306-4603(90)90013-N. [DOI] [PubMed] [Google Scholar]
- Businelle MS, Kendzor DE, Reitzel LR, Costello TJ, Cofta-Woerpel L, Li Y, et al. Mechanisms linking socioeconomic status to smoking cessation: A structural equation modeling approach. Health Psychology. 2010;29(3):262–273. doi: 10.1037/a0019285. doi:10.1037/a0019285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cinciripini PM, Wetter DW, Fouladi RT, Blalock JA, Carter BL, Cinciripini LG, et al. The effects of depressed mood on smoking cessation: mediation by postcessation self-efficacy. Journal of Consulting and Clinical Psychology. 2003;71(2):292–301. doi: 10.1037/0022-006x.71.2.292. doi:10.1037/0022-006x.71.2.292. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Lawrence Erlbaum; New Jersey: 1988. [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24(4):385–396. doi:10.1037/0022-006X.58.3.304. [PubMed] [Google Scholar]
- Cohen S, Mermelstein R, Kamarck T, Hoberman H. Measuring the functions of social support. In: Sarason I, Sarason B, editors. Social support: theory, research, and applications. Martinus Nijhoff; The Hague, The Netherlands: 1985. pp. 73–94. [Google Scholar]
- Coppotelli HC, Orleans CT. Partner support and other determinants of smoking cessation maintenance among women. Journal of Consulting and Clinical Psychology. 1985;53(4):455–460. doi: 10.1037//0022-006x.53.4.455. doi:10.1037//0022-006X.53.4.455. [DOI] [PubMed] [Google Scholar]
- Crawford JR, Henry JD. The positive and negative affect schedule (PANAS): construct validity, measurement properties and normative data in a large non-clinical sample. British Journal of Clinical Psychology. 2004;43(Pt 3):245–265. doi: 10.1348/0144665031752934. doi:10.1348/0144665031752934. [DOI] [PubMed] [Google Scholar]
- de Vries H, Backbier E. Self-efficacy as an important determinant of quitting among pregnant women who smoke: The ø-pattern. Preventive Medicine. 1994;23:167–174. doi: 10.1006/pmed.1994.1023. doi:10.1006/pmed.1994.1023. [DOI] [PubMed] [Google Scholar]
- Fiore MC, Jaen CR, Baker TB, Bailey WC, Benowitz NL, Curry SJ, et al. Clinical practice guideline. U.S. Department of Health and Human Services, Public Health Service; Rockville, MD: 2008. Treating tobacco use and dependence: 2008 update. [Google Scholar]
- French GM, Groner JA, Wewers ME, Ahijevych K. Staying smoke free: an intervention to prevent postpartum relapse. Nicotine & Tobacco Research. 2007;9(6):663–670. doi: 10.1080/14622200701365277. doi:10.1080/14622200701365277. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Keyes K, Simuro N. Mental disorders and nicotine dependence among pregnant women in the United States. Obstetrics & Gynecology. 2007;109(4):875–883. doi: 10.1097/01.AOG.0000255979.62280.e6. doi:10.1097/01.AOG.0000255979.62280.e6. [DOI] [PubMed] [Google Scholar]
- Gulliver SB, Hughes JR, Solomon LJ, Dey AN. An investigation of self-efficacy, partner support and daily stresses as predictors of relapse to smoking in self-quitters. Addiction. 1995;90(6):767–772. doi: 10.1046/j.1360-0443.1995.9067673.x. doi:10.1046/j.1360-0443.1995.9067673.x. [DOI] [PubMed] [Google Scholar]
- Gwaltney CJ, Shiffman S, Balabanis MH, Paty JA. Dynamic self-efficacy and outcome expectancies: prediction of smoking lapse and relapse. Journal of Abnormal Psychology. 2005;114(4):661–675. doi: 10.1037/0021-843X.114.4.661. doi:10.1037/0021-843X.114.4.661. [DOI] [PubMed] [Google Scholar]
- Hitsman B, Borrelli B, McChargue DE, Spring B, Niaura R. History of depression and smoking cessation outcome: a meta-analysis. Journal of Consulting and Clinical Psychology. 2003;71(4):657–663. doi: 10.1037/0022-006x.71.4.657. doi: 10.1037/002-006X.71.4.657. [DOI] [PubMed] [Google Scholar]
- Imai K, Keele L, Tingley D. A general approach to causal mediation analysis. Psychological Methods. 2010;15(4):309–334. doi: 10.1037/a0020761. 10.1037/a0020761. [DOI] [PubMed] [Google Scholar]
- Japuntich SJ, Smith SS, Jorenby DE, Piper ME, Fiore MC, Baker TB. Depression predicts smoking early but not late in a quit attempt. Nicotine & Tobacco Research. 2007;9(6):677–686. doi: 10.1080/14622200701365301. doi:10.1080/14622200701365301. [DOI] [PubMed] [Google Scholar]
- Kenford SL, Smith SS, Wetter DW, Jorenby DE, Fiore MC, Baker TB. Predicting relapse back to smoking: contrasting affective and physical models of dependence. Journal of Consulting and Clinical Psychology. 2002;70(1):216–227. doi:10.1037//0022-006X.70.1.216. [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB, Lowe B. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: a systematic review. General Hospital Psychiatry. 2010;32(4):345–359. doi: 10.1016/j.genhosppsych.2010.03.006. doi:10.1016/j.genhosppsych.2010.03.006. [DOI] [PubMed] [Google Scholar]
- Lawhon D, Humfleet GL, Hall SM, Munoz RF, Reus VI. Longitudinal analysis of abstinence-specific social support and smoking cessation. Health Psychology. 2009;28(4):465–472. doi: 10.1037/a0015206. doi:10.1037/a0015206. [DOI] [PubMed] [Google Scholar]
- Levine MD, Marcus MD, Kalarchian MA, Houck PR, Cheng Y. Weight concerns, mood, and postpartum smoking relapse. American Journal of Preventive Medicine. 2010;39(4):345–351. doi: 10.1016/j.amepre.2010.05.023. doi:10.1016/j.amepre.2010.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP. Introduction to statistical mediation analysis. Erlbaum; Mahwah, NJ: 2008. [Google Scholar]
- MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annual Review of Psychology. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. doi:10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell SE, Cole DA. Bias in cross-sectional analyses of longitudinal mediation. Psychological Methods. 2007;12(1):23–44. doi: 10.1037/1082-989X.12.1.23. doi:10.1037/1082-989X.12.1.23. [DOI] [PubMed] [Google Scholar]
- McBride CM, Curry SJ, Grothaus LC, Nelson JC, Lando H, Pirie PL. Partner smoking status and pregnant smoker’s perceptions of support for and likelihood of smoking cessation. Health Psychology. 1998;17(1):63–69. doi: 10.1037//0278-6133.17.1.63. doi:10.1037//0278-6133.17.1.63. [DOI] [PubMed] [Google Scholar]
- Mullen PD. How can more smoking suspension during pregnancy become lifelong abstinence? Lessons learned about predictors, interventions, and gaps in our accumulated knowledge. Nicotine & Tobacco Research. 2004;6(Supplement 2):S217–S238. doi: 10.1080/14622200410001669150. doi:10.1080/14622200410001669150. [DOI] [PubMed] [Google Scholar]
- Mykletun A, Overland S, Aaro LE, Liabo HM, Stewart R. Smoking in relation to anxiety and depression: evidence from a large population survey: the HUNT study. European Psychiatry. 2008;23(2):77–84. doi: 10.1016/j.eurpsy.2007.10.005. doi:10.1016/j.eurpsy.2007.10.005. [DOI] [PubMed] [Google Scholar]
- Nosek MA, Hughes RB, Wright G. Improving the health and wellness of women with disabilities: A symposium to establish a research agenda; 2003; Retrieved from www.crowdbcm.net/measures/Measures-I-Healthoutcomes.htm. [Google Scholar]
- Park ER, Chang Y, Quinn V, Regan S, Cohen L. The association of depressive, anxiety, and stress symptoms and postpartum relapse to smoking: A longitudinal study. Nicotine & Tobacco Research. 2009;11(6):707–714. doi: 10.1093/ntr/ntp053. doi:10.1093/ntr/ntp053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paykel ES. Life events, social support and depression. Acta Psychiatrica Scandinavica. 1994;89(377):50–58. doi: 10.1111/j.1600-0447.1994.tb05803.x. doi:10.1111/j.1600-0447.1994.tb05803.x. [DOI] [PubMed] [Google Scholar]
- Piper ME, Bolt DM, Kim S, Japuntich SJ, Smith SS, Niederdeppe J, et al. Refining the tobacco dependence phenotype using the Wisconsin Inventory of Smoking Dependence Motives (WISDM) Journal of Abnormal Psychology. 2008;117(4):747–761. doi: 10.1037/a0013298. doi:10.1037/a0013298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piper ME, Cook JW, Schlam TR, Jorenby DE, Baker TB. Anxiety disorders in smokers seeking cessation treatment: relations with tobacco dependence, withdrawal, outcome and response to treatment. Addiction. 2011;106(2):418–427. doi: 10.1111/j.1360-0443.2010.03173.x. doi:10.1111/j.1360-0443.2010.03173.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piper ME, McCarthy DE, Bolt DM, Smith SS, Lerman C, Benowitz N, et al. Assessing dimensions of nicotine dependence: An evaluation of the Nicotine Dependence Syndrome Scale (NDSS) and the Wisconsin Inventory of Smoking Dependence Motives (WISDM) Nicotine & Tobacco Research. 2008;10(6):1009–1020. doi: 10.1080/14622200802097563. doi:10.1080/14622200802097563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piper ME, Piasecki TM, Federman EB, Bolt DM, Smith SS, Fiore MC, et al. A multiple motives approach to tobacco dependence: The Wisconsin Inventory of Smoking Dependence Motives (WISDM-68) Journal of Consulting and Clinical Psychology. 2004;72(2):139–154. doi: 10.1037/0022-006X.72.2.139. doi:10.1037/0022-006X.72.2.139. [DOI] [PubMed] [Google Scholar]
- Piper ME, Smith SS, Schlam TR, Fleming MF, Bittrich AA, Brown JL, et al. Psychiatric disorders in smokers seeking treatment for tobacco dependence: relations with tobacco dependence and cessation. Journal of Consulting and Clinical Psychology. 2010;78(1):13–23. doi: 10.1037/a0018065. doi:10.1037/a0018065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polanska K, Hanke W, Sobala W, Lowe JB, Jaakkola JJK. Predictors of smoking relapse after delivery: prospective study in Central Poland. Maternal and Child Health Journal. 2010 doi: 10.1007/s10995-010-0639-y. doi:10.1007/s10995-010-0639-y. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. doi:10.3758/BRM.40.3.879. [DOI] [PubMed] [Google Scholar]
- Ratner PA, Johnson JL, Bottorff JL, Dahinten S, Hall W. Twelve-month follow-up of a smoking relapse prevention intervention for postpartum women. Addictive Behaviors. 2000;25:81–92. doi: 10.1016/s0306-4603(99)00033-7. doi:10.1016/S0306-4603(99)00033-7. [DOI] [PubMed] [Google Scholar]
- Reitzel LR, Irvin Vidrine J, Businelle MS, Kendzor DE, Costello TJ, Li Y, et al. Preventing postpartum smoking relapse among diverse low income women: a randomized clinical trial. Nicotine & Tobacco Research. 2010;12(4):326–335. doi: 10.1093/ntr/ntq001. doi:10.1093/ntr/ntq001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson TE, Berridge KC. The incentive sensitization theory of addiction: some current issues. Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences. 2008;363(1507):3137–3146. doi: 10.1098/rstb.2008.0093. Review. doi:10.1098/rstb.2008.0093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schleicher HE, Harris KJ, Catley D, Nazir N. The role of depression and negative affect regulation expectancies in tobacco smoking among collegue students. Journal of American College Health. 2009;57(5):507–512. doi: 10.3200/JACH.57.5.507-512. doi:10.3200/JACH.57.5.507-512. [DOI] [PubMed] [Google Scholar]
- Shiffman S. Dynamic influences on smoking relapse process. Journal of Personality. 2005;73:1715–1748. doi: 10.1111/j.0022-3506.2005.00364.x. doi:10.1111/j.0022-3506.2005.00364.x. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Gwaltney CJ. Does heightened affect make smoking cues more salient? Journal of Abnormal Psychology. 2008;117(3):618–624. doi: 10.1037/0021-843X.117.3.618. doi:10.1037/0021-843X.117.3.618. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Waters AJ. Negative affect and smoking lapses: a prospective analysis. J Consult Clin Psychol. 2004;72(2):192–201. doi: 10.1037/0022-006X.72.2.192. doi:10.1037/0022-006X.72.2.192. [DOI] [PubMed] [Google Scholar]
- Solomon L, Quinn V. Spontaneous quitting: self-initiated smoking cessation in early pregnancy. Nicotine & Tobacco Research. 2004;6(Suppl 2):S203–216. doi: 10.1080/14622200410001669132. doi:10.1080/14622200410001669132. [DOI] [PubMed] [Google Scholar]
- Solomon LJ, Higgins ST, Heil SH, Badger GJ, Thomas CS, Bernstein IM. Predictors of postpartum relapse to smoking. Drug and Alcohol Dependence. 2007;90:224–227. doi: 10.1016/j.drugalcdep.2007.03.012. doi:10.1016/j.drugalcdep.2007.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong VT, Jones JR, Dietz PM, D’Angelo D, Bombard JM. Trends in smoking before, during, and after pregnancy - Pregnancy Risk Assessment Monitoring System (PRAMS), United States, 31 sites, 2000-2005. MMWR Surveillance Summaries. 2009;58(4):1–29. [PubMed] [Google Scholar]
- Van Zundert RM, Ferguson SG, Shiffman S, Engels R. Dynamic effects of craving and negative affect on adolescent smoking relapse. Health Psychology. 2011 doi: 10.1037/a0025204. doi:10.1037/a0025204. [DOI] [PubMed] [Google Scholar]
- Velicer WF, DiClemente CC, Rossi JS, Prochaska JO. Relapse situations and self-efficacy: an integrative model. Addictive Behaviors. 1990;15:271–283. doi: 10.1016/0306-4603(90)90070-e. doi:10.1016/0306-4603(90)90070-E. [DOI] [PubMed] [Google Scholar]
- Watson D. Rethinking the mood and anxiety disorders: A quantitative hierarchical model for DSM-V. Journal of Abnormal Psychology. 2005;114(4):522–536. doi: 10.1037/0021-843X.114.4.522. doi:10.1037/0021-843X.114.4.522. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. Journal of Personality and Social Psychology. 1988;54(6):1063–1070. doi: 10.1037//0022-3514.54.6.1063. doi:10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Wetter DW, Brandon TH, Baker TB. The relation of affective processing measures and smoking motivation indices among college-age smokers. Advances in Behaviour Research & Therapy. 1992;14(3):169–193. doi:10.1016/0146-6402(92)90007-B. [Google Scholar]
- Wetter DW, Smith SS, Kenford SL, Jorenby DE, Fiore MC, Hurt RD, et al. Smoking outcome expectancies: factor structure, predictive validity, and discriminant validity. Journal of Abnormal Psychology. 1994;103(4):801–811. doi: 10.1037//0021-843x.103.4.801. doi:10.1037//0021-843X.103.4.801. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Marlatt GA. Relapse prevention for alcohol and drug problems: that was Zen, this is Tao. American Psychologist. 2004;59(4):224–235. doi: 10.1037/0003-066X.59.4.224. doi:10.1037/0003-066X.59.4.224. [DOI] [PubMed] [Google Scholar]
- Ziedonis D, Hitsman B, Beckham JC, Zvolensky M, Adler LE, Audrain-McGovern J, et al. Tobacco use and cessation in psychiatric disorders: National Institute of Mental Health report. Nicotine & Tobacco Research. 2008;10(12):1691–1715. doi: 10.1080/14622200802443569. doi:10.1080/14622200802443569. [DOI] [PubMed] [Google Scholar]
- Zinser MC, Baker TB, Sherman JE, Cannon DS. Relation between self-reported affect and drug urges and cravings in continuing and withdrawing smokers. Journal of Abnormal Psychology. 1992;101(4):617–629. doi: 10.1037//0021-843x.101.4.617. doi:10.1037/0021-843X.101.4.617. [DOI] [PubMed] [Google Scholar]