Abstract
Hypothesis
Most clinically-available small molecule kinase inhibitors are multitargeted and can inhibit multiple kinases. Our driving hypothesis was that one of these multitargeted tyrosine kinase inhibitors (TKIs) would have anti-proliferative activity against ROS1 translocated non-small-cell lung cancer (NSCLC).
Methods
We selected NSCLC cell lines - A549 (KRAS G12S), NCI-H3255 (EGFR L858R), NCI-H3122 (EML4-ALK E13;A20) and HCC78 (SLC34A2-ROS1) - to evaluate the anti-proliferative effects of submicromolar concentrations of the multitargeted TKIs imatinib, sorafenib, erlotinib and crizotinib.
Results
Imatinib and sorafenib were unable to significantly inhibit proliferation of the aforementioned cell lines. Erlotinib only inhibited EGFR mutated NCI-H3255, as expected. Crizotinib displayed dose-dependent inhibition of ALK translocated NCI-H3122 and also ROS1 translocated HCC78. The SLC34A2-ROS1 translocated HCC78 cell line had phosphorylated levels of ROS, AKT and ERK inhibited by submicromolar doses of crizotinib, and subsequently underwent apoptosis.
Conclusions
The ROS1 translocated HCC78 cell line was sensitive to inhibition by the multitargeted ALK/MET/RON/ROS1 inhibitor crizotinib. Preclinical data supports the clinical development of crizotinib for ROS1 translocated NSCLC.
Keywords: lung cancer, non-small-cell lung cancer, tyrosine kinase, kinase inhibitor, epidermal growth factor receptor, EGFR, anaplastic lymphoma kinase, ALK, ROS1, crizotinib
INTRODUCTION
The human kinome consists of over five hundred structurally-related enzymes that either phosphorylate the amino acids tyrosine, or serine and threonine, or both. Kinase inhibitors have revolutionized the palliative care of advanced cancer patients. These drugs usually compete with adenosine triphosphate (ATP) within the active binding pocket of these enzymes. Most - if not all - of the currently clinically-available and approved small molecule kinase inhibitors are multitargeted and can inhibit multiple kinases (1). As examples, one can cite imatinib, sorafenib, erlotinib and crizotinib. Imatinib was approved for use in Philadelphia chromosome-positive chronic myeloid leukemia and stem cell factor/proto-oncogene c-Kit (KIT)-positive metastatic gastrointestinal stromal tumor, and has inhibitory activity against v-abl Abelson murine leukemia viral oncogene homolog 1 (ABL), platelet-derived growth factor receptor (PDGFR), KIT, among other kinases (1). Sorafenib was approved for use in advanced renal cell and hepatocellular carcinomas, and has activity against v-raf-1 murine leukemia viral oncogene homolog 1 (CRAF), v-raf murine sarcoma viral oncogene homolog B1 (BRAF), KIT, Fms-like tyrosine kinase 3 (FLT-3), Ret proto-oncogene (RET), vascular endothelial growth factor receptor (VEGFR)-1, VEGFR-2, VEGFR-3, PDGFR, among other kinases (2). Erlotinib was approved for metastatic non-small-cell lung cancer (NSCLC) and pancreatic cancer, and has activity against epidermal growth factor receptor (EGFR), mitogen-activated protein kinase 1 (MAP3K1), integrin-linked kinase (ILK), tyrosine-protein kinase abelson-related gene (ARG), among other tyrosine and serine/threonine kinases (3). Crizotinib was approved for use in metastatic NSCLC that is anaplastic lymphoma kinase (ALK)-positive, and can inhibit ALK, hepatocyte growth factor receptor (MET), recepteur d’origine nantais (RON), among other kinases (4; 5).
NSCLCs are the leading cause of cancer mortality worldwide and even small subgroups constitute important cohorts for which effective therapies are needed. Over the last decade, the molecular heterogeneity of NSCLCs has begun to be unraveled and it is now clear that some tumors are characterized by “driver” oncogene mutations in kinases (6). The most prevalent mutated oncogenes identified in NSCLCs are v-ki-ras2 Kirsten rat sarcoma viral oncogene homolog (KRAS), EGFR, ALK (where translocations and not mutations are present), proto-oncogene tyrosine kinase c-ROS 1 (ROS1) [again, where translocations and not mutations are seen], ERBB2, BRAF, and PIK3CA (7).
We sought to screen NSCLC cell lines driven by mutated/translocated KRAS, EGFR, ALK and ROS1 against multitargeted tyrosine kinase inhibitors (TKIs) that are already approved. Our driving hypothesis was that one of these clinically-available multitargeted TKIs, due to their known promiscuity (1), could have anti-proliferative activity against ROS1-driven tumors. ROS1 is a tyrosine kinase with similarities - much like ALK - to the insulin growth factor receptor family (8; 9). It has unknown ligands and function, but has been found to be translocated in a diverse array of tumor types including glioblastomas, cholangiocarcinomas and NSCLCs (9–11). Identification of a commercially-available multitargeted TKI with preclinical activity against ROS1-driven cancers would, hopefully, lead to a rapid translation into confirmatory clinical studies.
MATERIALS AND METHODS
Reagents
Erlotinib, sorafenib, imatinib and crizotinib were purchased from LC Laboratories (Woburn, MA). All reagents were dissolved in dimethyl sulfoxide (DMSO) and stored at −80°C.
Cell culture
A549, NCI-H3122 (H3122), NCI-H3255 (H3255) and HCC78 cells were maintained in RPMI 1640 medium (Mediatech, Manassas, VA) supplemented with 10% fetal bovine serum (FBS). All cells were grown at 37°C in a humidified atmosphere with 5% CO2.
Cell line proliferation assays
Cells were plated in 96-well plates, allowed to attach and then treated with or without tyrosine kinase inhibitors for 72 hours. Cell viability was determined by CellTiter 96 Aqueous One solution proliferation kit (Promega, Madison, WI) according to the manufacture’s protocol.
Western blotting and antibodies
Cells were lysed in cell lysis buffer containing 20 mM Tris-HCl (pH 7.5), 150 mM NaCl, 1 mM EDTA, 1 mM EGTA, 1% Triton, 1 mM beta-glycerophosphate, 1 mM Na3VO4 and 1 mM NaF. Protease inhibitor cocktail set III (Calbiochem, La Jolla, CA) and 1 mM PMSF was added to inhibit the degradation of protein. Lysates were cleared by centrifugation (14000 rpm for 5 minutes) and boiled with SDS sample buffer for 3 minutes. 40 µg of lysates were separated by 8% SDS-polyacrylamide gel, transferred to PVDF membrane, and analyzed with the use of Pierce ECL western blotting substrate (Thermo Scientific, Waltham, MA). Total EGFR antibody was purchased from Santa Cruz Biotechnology (Santa Cruz, CA). Total extracellular signal regulating kinase 1/2 (ERK 1/2) antibody was purchased from BD Transduction Laboratories (Lexington, KY). Phospho-EGFR (pT1068) antibody was purchased from Invitrogen (Carlsbad, CA). Protein kinase B (AKT), phospho-AKT (pS473), phospho-ERK 1/2 (pT202/pY204), phospho-ALK, ALK, phospho-ROS (pT2274) and ROS were purchased from Cell Signaling Technology (Beverly, MA). Poly (ADP-ribose) polymerase (PARP) and cleaved PARP were purchased from Cell Signaling Technology (Beverly, MA). All primary antibodies were diluted 1:1000, while their recommended secondary antibodies were diluted 1:10000.
Statistical analysis
The paired Student’s t-test was used to determine the difference in cell viability between DMSO and inhibitor treated cells.
RESULTS
Proliferation of oncogene driven NSCLC cell lines upon exposure to multitargeted kinase inhibitors
We selected four representative cell lines with known oncogenic mutations: A549 (KRAS G12S), H3255 (EGFR L858R), H3122 (EML4-ALK E13;A20) and HCC78 (SLC34A2-ROS1).
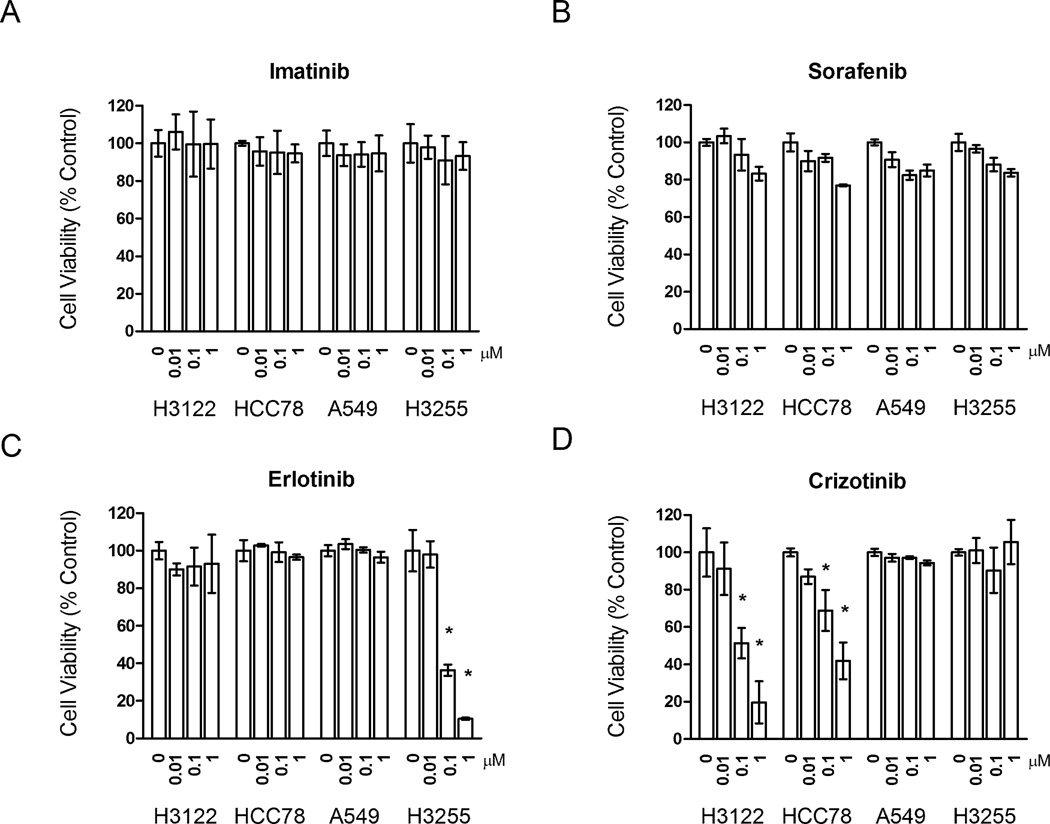
Imatinib was not able to significantly alter viability of any of the cell lines tested (Figure 1A). Sorafenib minimally decreased the proliferation rate of all cell lines, but in none of the cells the cell viability fell below seventy percent of control conditions (Figure 1B). Erlotinib was only able to inhibit the proliferation of the EGFR mutated H3255 cell line in submicromolar concentrations (Figure 1C), achieving 63.6% inhibition at 1µM (p=0.0012) and 89.4% inhibition at 1µM (p=0.0031).
FIGURE 1.
Proliferation assay evaluating multitargeted tyrosine kinase inhibitors (TKIs) in NSCLC cell lines. Cells were plated at a density of 1500 cells/well for A549, 2500 cells/well for H3122, 5000 cells/well for H3255 and 2000 cells/well for HCC78. All experiments were performed in triplicate. A. Inhibitory profile of imatinib (0, 0.01, 0.1 and 1µM). B. Inhibitory profile of sorafenib (0, 0.01, 0.1 and 1µM). C. Inhibitory profile of erlotinib (0, 0.01, 0.1 and 1µM). D. Inhibitory profile of crizotinib (0, 0.01, 0.1 and 1µM). Results are displayed in bar columns with standard deviation in relation to cell viability. Treatment with DMSO (indicated as a concentration of 0) was used as the standard for 100% cell viability in each cell line. * indicates a p-value <0.05 (see text for exact p-values) for erlotinib and crizotinib-treated cells.
Crizotinib had dose-dependent inhibitory activity against H3122 and HCC78 in submicromolar concentrations (Figure 1D). At 0.1µM, crizotinib achieved 48.6% inhibition of H3122 (p=0.0087) and 31.1% inhibition of HCC78 (p=0.0349). At 1µM, crizotinib achieved 80.3% inhibition of H3122 (p=0.0013) and 58.1% inhibition of HCC78 (p=0.0072). These results indicated that crizotinib had anti-proliferative activity in ALK and ROS1 translocated cells.
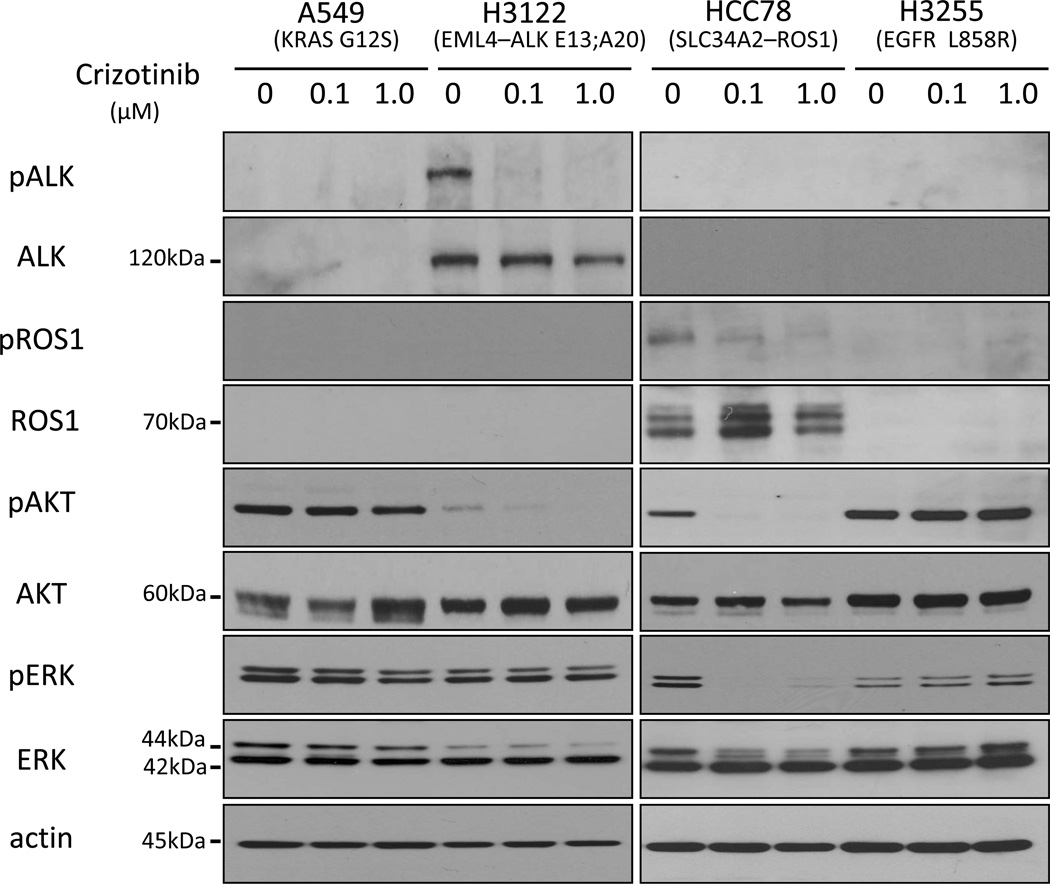
Crizotinib and inhibition of ROS1 and downstream targets in HCC78
We next evaluated the ability of crizotinib to inhibit ROS1, the phosphatidylinositol-3-kinases (PI3K)/AKT and the ERK/mitogen-activated protein kinase (MAPK) pathways. HCC78 cells had levels of phosphorylated ROS1, corresponding to the expected size of fusion oncogene SLC34A2-ROS1, inhibited by concentrations of 0.1 and 1µM of crizotinib (Figure 2). Both phosphorylated AKT and ERK 1/2 were similarly inhibited by 0.1 and 1µM of crizotinib in HCC78 cells but not in the EGFR mutant H3255 cell or KRAS mutated A549 cell (Figure 2). H3122 cells, with an ALK translocation, had levels of phosphorylated ALK, corresponding to the expected size of fusion oncogene EML4-ALK E13;A20, inhibited by concentrations of 0.1 and 1µM of crizotinib (Figure 2). Phosphorylated AKT was inhibited by crizotinib in H3122 cells similarly to HCC78, while levels of ERK1/2 were less inhibited (Figure 2).
FIGURE 2.
Western blot analysis of protein extracts from cells treated with crizotinib. A549, H3122, HCC78 and H3255 cells were treated with DMSO (indicated as concentration of 0), 0.1 or 1µM of crizotinib for 24 hours. The figure shows the levels of phosphorylated ALK, total ALK (expected size of EML4-ALK E13;A20 of approximately 120kDa), phosphorylated ROS (pROS), total ROS (expected size of SLC34A2-ROS of approximately 70kDa with 3 identified isoforms of 85, 70 and 59kDa; wild-type ROS has a size of 258kDa), phosphorylated AKT (pAKT), total AKT (size of 60kDa), phosphorylated ERK 1/2 (pERK), total ERK 1/2 (sizes of 42 and 44kDa) and actin (size of 45kDa). Wild-type ROS was not detected in either HCC78 or H3255 (data not shown).
Hence, crizotinib was able to inhibit ALK and ROS1, and its putative downstream targets.
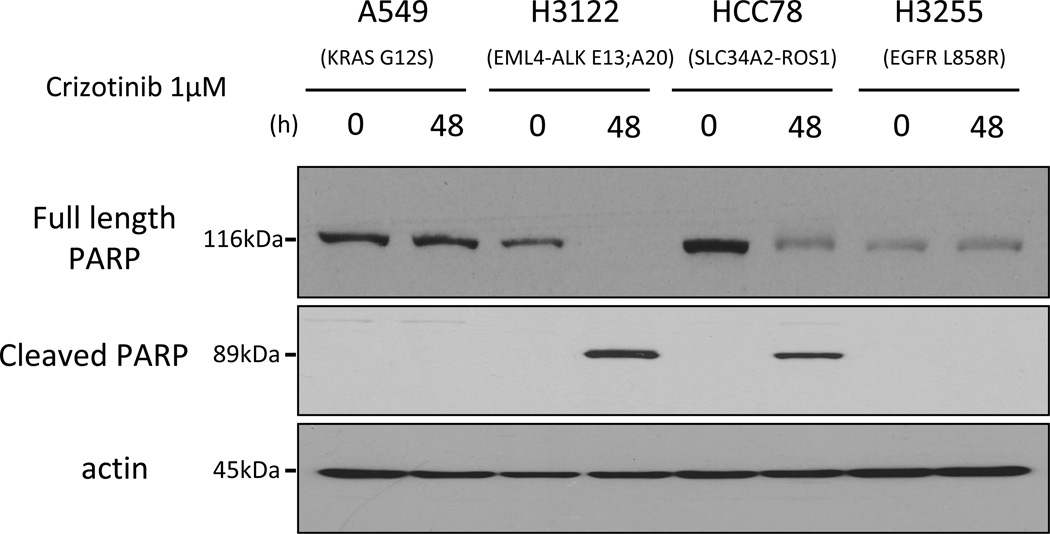
Crizotinib and apoptosis in HCC78
We also evaluated the ability of crizotinib to induce apoptosis in the ROS1 translocated cell line HCC78. Exposure to 1µM of crizotinib, for 48 hours, induced cleavage of PARP - a marker of caspase cleavage of PARP and hence apoptosis - in H3122 and HCC78 but not in H3255 or A549 cells (Figure 3).
FIGURE 3.
Western blot analysis of protein extracts from cells treated with crizotinib. A549, H3122, HCC78 and H3255 cells were treated with 1µM of crizotinib for 48 hours. The figure shows levels of full length PARP, detected by using a PARP antibody, and cleaved PARP, detected by using a cleaved PARP antibody, in these cells. PARP cleavage was only observed in H3122 and HCC78 cell extracts.
These results indicate that crizotinib not only inhibits proliferation (Figure 1) but also induces apoptosis (Figure 3) in NSCLC cells driven by ALK or ROS1 fusion genes.
DISCUSSION
We screened four multitargeted kinase inhibitors (imatinib, sorafenib, erlotinib and crizotinib) against cells driven by oncogenic KRAS (A549), EGFR (H3255), ALK (H3122) and ROS1 (HCC78). Our results confirmed that EGFR mutated and ALK translocated NSCLCs were only sensitive to TKIs that inhibit EGFR (erlotinib) and ALK (crizotinib), respectively. Of most interest, we were able to demonstrate that the ROS1 translocated HCC78 NSCLC cell line was sensitive to crizotinib, and that crizotinib inhibited ROS and its downstream targets with induction of apoptosis in this cell line.
The ROS1 tyrosine kinase is an orphan kinase with unknown ligands and unclear normal function (8). It is spatially and temporally regulated during normal development, and has been described as the kinase partner of translocations in some cancer types (9). In glioblastomas (12) and cholangiocarcinomas (10) translocations involving fused in glioblastoma (FIG) and ROS (FIG-ROS) have been identified. In NSCLCs, two translocations were described in 2007: CD74-ROS1 and SLC34A2-ROS1 (11). The frequency of ROS1 translocations in NSCLC seems to be below 2% (13; 14). One report disclosed that 1% of lung adenocarcinomas from never smokers harbored ROS1 translocations (13). Another report determined that 1.7% of the 1073 tumors screened were ROS translocated, with this gene abnormality enriched in never smokers (14). In Japanese patients with NSCLC, the frequency of ROS1 translocations was recently reported to be 0.9% (13/1476) for all NSCLCs and 1.2% (13/1116) for lung adenocarcinomas (15).
The concept of targeting ROS1 in ROS1 translocated NSCLCs with multitargeted kinase inhibitors was entertained by us weighing in observations made by other groups, who demonstrated that: 1) a NSCLC cell line with SLC34A2-ROS1 (HCC78) was dependent on ROS signaling for survival (11); 2) ROS1, similar to ALK, had similarities with the insulin growth factor receptor family (8); 3) an in vitro system driven by FIG-ROS1 was inhibited by the potent ALK TKI TAE684 (10); 4) the ALK TKI AP26113 was active against ROS1 using an in vitro kinase assay (16); and 5) novel ROS1 TKIs being developed had inhibitory activity against ABL, BRAF, RON, and MET among other kinases (12).
The aforementioned reports support our observation that the ROS1 translocated HCC78 NSCLC cell line was sensitive to inhibition by the multitargeted ALK/MET/RON/ROS1 inhibitor crizotinib. Indeed, others have recently shown that HCC78 cells were inhibited by crizotinib and that one patient with ROS1 translocated NSCLC achieved a partial response to 250 mg twice daily of crizotinib (14). The data presented here not only reproduced the results of those authors (the inhibition of HCC78 by crizotinib was similar in both reports) but also added important information to their observations. In their report, they did not evaluate other multitargeted TKIs against HCC78 or the ability of crizotinib to inhibit PI3K/AKT and ERK/MAPK in these cells. We demonstrated that inhibition of ROS was only achieved with crizotinib and was linked to inhibition of AKT and ERK. We also were able to show that crizotinib induces apoptosis in HCC78 cells.
Crizotinib has been extensively studied in humans (12). It is bioavailable, has a favorable pharmacokinetic profile, is generally safe (major side effects include nausea, vomiting, diarrhea, visual field disturbances, edema, liver function test abnormalities, among others) and was approved the Food and Drug Administration in 2011 for use in metastatic NSCLC that is positive for ALK translocations (3; 4;12). It also has clinical activity against ALK translocated anaplastic large cell lymphoma and MET amplified glioblastoma, NSCLC and esophagogastric tumors (12). Therefore, crizotinib is an attractive multitargeted TKI that could see its use expanded to a diverse array of tumor types that are dependent on kinases that it can inhibit.
In summary, our data provides preclinical rationale for further clinical testing of crizotinib for advanced ROS1 translocated NSCLCs.
ACKNOWLEDMENTS
We would like to thank Drs. Matthew Meyerson and Hideo Watanabe for providing HCC78 cells, Dr. Pasi Jänne for providing H3122 cells, and Dr. Daniel Tenen for providing imatinib.
Funding/Grant Support: This work was funded in part through fellowships from the American Society of Clinical Oncology Conquer Cancer Foundation (DBC), an American Cancer Society grant RSG 11-186 (DBC), and National Institutes of Health grants CA090578 (DBC, SK) and CA126026 (SK).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors: HY, DBC were involved in the conception of this study; HY, LLFP, SK and DBC were involved in data acquisition, analysis and interpretation; SK and DBC provided administrative and funding support; HY, LLFP, SK and DBC were involved in writing the report; all authors approved the final version.
Conflict of interest: DBC has received consulting fees from Pfizer, Roche and AstraZeneca. No other conflict of interest is stated.
REFERENCES
- 1.Krause DS, Van Etten RA. Tyrosine kinases as targets for cancer therapy. N Engl J Med. 2005;353(2):172–187. doi: 10.1056/NEJMra044389. [DOI] [PubMed] [Google Scholar]
- 2.Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, Blanc JF, et al. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med. 2008;359(4):378–390. doi: 10.1056/NEJMoa0708857. [DOI] [PubMed] [Google Scholar]
- 3.Gaughan EM, Costa DB. Genotype-driven therapies for non-small cell lung cancer: focus on EGFR, KRAS and ALK gene abnormalities. Ther Adv Med Oncol. 2011;3(3):113–125. doi: 10.1177/1758834010397569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kwak EL, Bang YJ, Camidge DR, Shaw AT, Solomon B, Maki RG, et al. Anaplastic lymphoma kinase inhibition in non-small-cell lung cancer. N Engl J Med. 2010;363(18):1693–1703. doi: 10.1056/NEJMoa1006448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zou HY, Li Q, Lee JH, Arango ME, McDonnell SR, Yamazaki S, et al. An orally available small-molecule inhibitor of c-Met, PF-2341066, exhibits cytoreductive antitumor efficacy through antiproliferative and antiangiogenic mechanisms. Cancer Res. 2007;67(9):4408–4417. doi: 10.1158/0008-5472.CAN-06-4443. [DOI] [PubMed] [Google Scholar]
- 6.Ding L, Getz G, Wheeler DA, Mardis ER, McLellan MD, Cibulskis K, et al. Somatic mutations affect key pathways in lung adenocarcinoma. Nature. 2008;455(7216):1069–1075. doi: 10.1038/nature07423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pao W, Girard N. New driver mutations in non-small-cell lung cancer. Lancet Oncol. 2011;12(2):175–180. doi: 10.1016/S1470-2045(10)70087-5. [DOI] [PubMed] [Google Scholar]
- 8.Keilhack H, Muller M, Bohmer SA, Frank C, Weidner KM, Birchmeier W, et al. Negative regulation of Ros receptor tyrosine kinase signaling. An epithelial function of the SH2 domain protein tyrosine phosphatase SHP-1. J Cell Biol. 2001;152(2):325–334. doi: 10.1083/jcb.152.2.325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Acquaviva J, Wong R, Charest A. The multifaceted roles of the receptor tyrosine kinase ROS in development and cancer. Biochim Biophys Acta. 2009;1795(1):37–52. doi: 10.1016/j.bbcan.2008.07.006. [DOI] [PubMed] [Google Scholar]
- 10.Gu TL, Deng X, Huang F, Tucker M, Crosby K, Rimkunas V, et al. Survey of tyrosine kinase signaling reveals ROS kinase fusions in human cholangiocarcinoma. PLoS One. 2011;6(1):e15640. doi: 10.1371/journal.pone.0015640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rikova K, Guo A, Zeng Q, Possemato A, Yu J, Haack H, et al. Global survey of phosphotyrosine signaling identifies oncogenic kinases in lung cancer. Cell. 2007;131(6):1190–1203. doi: 10.1016/j.cell.2007.11.025. [DOI] [PubMed] [Google Scholar]
- 12.Ou SH. Crizotinib: a novel and first-in-class multitargeted tyrosine kinase inhibitor for the treatment of anaplastic lymphoma kinase rearranged non-small cell lung cancer and beyond. Drug Des Devel Ther. 2011;5:471–485. doi: 10.2147/DDDT.S19045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li C, Fang R, Sun Y, Han X, Li F, Gao B, et al. Spectrum of oncogenic driver mutations in lung adenocarcinomas from East asian never smokers. PLoS One. 2011;6(11):e28204. doi: 10.1371/journal.pone.0028204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bergethon K, Shaw AT, Ou SI, Katayama R, Lovly CM, Mcdonald/ NT, et al. ROS1 rearrangements define a unique molecular class of lung cancers. J Clin Oncol. 2012 doi: 10.1200/JCO.2011.35.6345. 10.1200/JCO.2011.39.4197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Takeuchi K, Soda M, Togashi Y, Suzuki R, Sakata S, Hatano S, et al. RET, ROS1 and ALK fusions in lung cancer. Nat Med. 2012 doi: 10.1038/nm.2658. 10.1038/nm.2658. [DOI] [PubMed] [Google Scholar]
- 16.Katayama R, Khan TM, Benes C, Lifshits E, Ebi H, Rivera VM, et al. Therapeutic strategies to overcome crizotinib resistance in non-small cell lung cancers harboring the fusion oncogene EML4-ALK. Proc Natl Acad Sci U S A. 2011;108(18):7535–7540. doi: 10.1073/pnas.1019559108. [DOI] [PMC free article] [PubMed] [Google Scholar]