Abstract
Objective
The objective of this study is to provide a comprehensive update of the outcome of the ileo-pouch anal anastomosis (IPAA).
Data sources
An extensive search in PubMed, EMBASE, and The Cochrane Library was conducted.
Study selection and data extraction
All studies published after 2000 reporting on complications or functional outcome after a primary open IPAA procedure for UC or FAP were selected. Study characteristics, functional outcome, and complications were extracted.
Data synthesis
A review with similar methodology conducted 10 years earlier was used to evaluate developments in outcome over time. Pooled estimates were compared using a random-effects logistic meta-analyzing technique. Analyses focusing on the effect of time of study conductance, centralization, and variation in surgical techniques were performed.
Results
Fifty-three studies including 14,966 patients were included. Pooled rates of pouch failure and pelvic sepsis were 4.3% (95% CI, 3.5–6.3) and 7.5% (95% CI 6.1–9.1), respectively. Compared to studies published before 2000, a reduction of 2.5% was observed in the pouch failure rate (p = 0.0038). Analysis on the effect of the time of study conductance confirmed a decline in pouch failure. Functional outcome remained stable over time, with a 24-h defecation frequency of 5.9 (95% CI, 5.0–6.9). Technical surgery aspects did not have an important effect on outcome.
Conclusion
This review provides up to date outcome estimates of the IPAA procedure that can be useful as reference values for practice and research. It is also shows a reduction in pouch failure over time.
Keywords: Functional outcome, Ileo-pouch anal anastomosis, Meta-analysis
Introduction
Restorative proctocolectomy by means of an ileo-pouch anal anastomosis (IPAA) is the procedure of choice for the surgical treatment of ulcerative colitis (UC) and familial adenomatous polyposis (FAP). The IPAA procedure generally results in acceptable long-term functional outcomes and improvement of quality of life. It is, however, associated with substantial morbidity with complications up to 50% of patients [1]. Since its introduction in 1978, the IPAA procedure has continuously been subjected to attempts of improvements in technique [55]. Additionally, much has been achieved in improving the perioperative care. Centralization of complex surgery has been a recent development in many countries. All these developments may have resulted in improved outcomes.
A large number of observational studies have reported outcomes of the IPAA procedure, most commonly from a selected group of patients in one hospital. This review aims to provide an overview of the available evidence and to evaluate the effect of the continuous developments on outcomes. Previously, a systematic review summarizing complications and functional results after an IPAA procedure in studies published until 2000 was conducted. This current systematic review provides an update regarding the outcomes of the IPAA procedure and uses the combined data set of both reviews to analyze changes in the outcomes of the IPAA procedure.
Methods
This systematic review aims to provide an overview regarding the outcomes of the open IPAA procedure. Additionally, it evaluates the effect of development of practice on the most important outcomes over time.
Search strategy
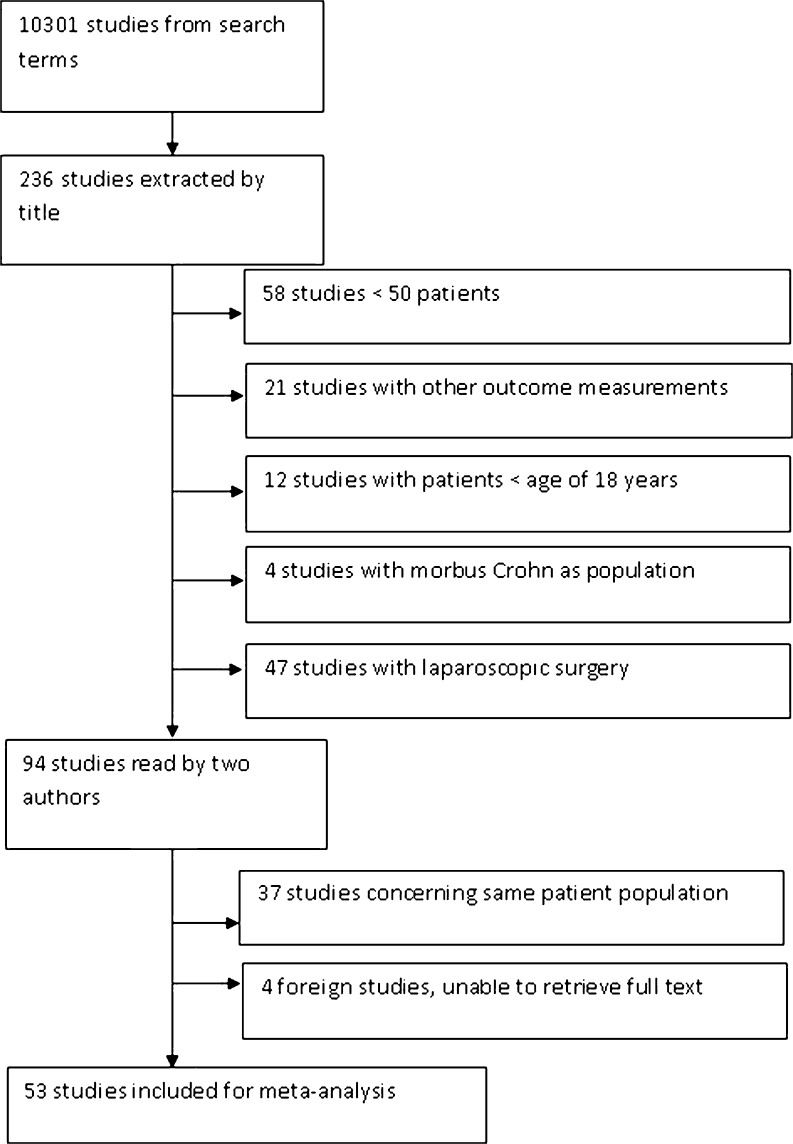
A systematic literature search with predefined search terms was carried out in four electronic databases: Medline (1–1–2000 to 1–1–2010), EMBASE (1–1–2000 to 1–1–2010), and the Cochrane Library (Issue 1, 2010) (Fig. 1). Two authors (SZ and UAA) independently performed the selection of the publications according to inclusion criteria. Disagreements were discussed with a third reviewer (FK). Additional relevant studies were looked for by cross-reference checking of all included studies. Language restrictions were not applied.
Fig. 1.
Flowchart of study selection resulting in the 53 included studies
Selection of studies
Inclusion criteria
Title and abstract of all identified publications (prospective and retrospective and observational and comparison studies) were screened according to the following inclusion criteria: The study population consists of adult patients with established UC or FAP undergoing a primary IPAA procedure; the intervention is a clearly documented open IPAA procedure in an elective setting with or without a diverting ileostomy and irrespective of the number of stages of the operation; the study reports at least one of the primary outcomes reported below; and the study includes a consecutive series with a minimal sample size of 50 patients.
Exclusion criteria
Studies were excluded from this systematic review if they included children (<18 years) or primarily elderly patients (>65 years). Studies were excluded as well when the IPAA was performed for other indications than UC or FAP (e.g., Morbus Crohn) or when a secondary IPAA was performed (e.g., after ileo-rectal anastomosis). Studies were also excluded when there was selective outcome reporting, i.e., studies focusing on one parameter (e.g., pouchitits) without reporting of any additional outcomes.
Outcomes of interest and definitions
Primary outcomes were pouch failure, pelvic sepsis, and severe day incontinence. Secondary outcomes included other complications (stricture, fistula, small bowel obstruction, pouchitis, and sexual dysfunction) and parameters of functional outcome (defecation frequency and incontinence). Table 1 shows the definitions of all outcomes.
Table 1.
Definition of outcomes
| Pouch failure | Pouch excision or a nonfunctioning pouch at 12 months after IPAA |
| Pelvic sepsis | Pelvic abscess, anastomotic leakage or dehiscence, pelvic/perineal wound infection |
| Fistula | Any pouch-related fistula |
| Stricture | Anastomotic fibrosis necessitating dilatation |
| Mild fecal incontinence | Soiling, spotting in underwear |
| Severe fecal incontinence | Regularly severe leakage or fecal loss passive fecal incontinence |
Data extraction
After assessment for eligibility, two authors (SZ and UAA) independently extracted the following data if available: numbers of patients, patient characteristics, dates of start and end of the inclusion period, duration of follow-up, variations in surgical technique, numbers and type of complications, and parameters of pouch functional outcome. Authors were contacted when data were missing. One author provided updated unpublished information [66]. Double publications describing identical populations were considered as one study.
Data of studies published until 2000
Previously, a systematic review was performed summarizing complications and functional results after an IPAA procedure in studies published until 2000 [39]. For time-frame analyses regarding the development of clinical practice and its effect on outcomes, data from both reviews were combined. Both reviews were conducted with similar methodology, and the full data set from the previous review was available.
Statistical analysis
Relevant study characteristics and outcomes were extracted and presented for each study individually. Outcomes were subsequently pooled, and cumulative probabilities were calculated with 95% confidence intervals (95% CI). Data were pooled using a “random-effects model, based on the restricted maximum likelihood estimator in order to incorporate the heterogeneity between studies. Pooled results of this review (all studies published since 2000) were compared with pooled results of the previously published review (all studies published before 2000) by analyzing the complete set in one random-effects model and incorporating a dummy variable that coded for period. The Knapp and Hartung adjustment was used to obtain estimates and confidence intervals [33]. Additionally, analysis focusing on the effect of time of study conductance, centralization, and variation in techniques were performed using linear regression and one-way ANOVA as appropriate. Data management and statistical analyses were conducted using SPSS (version 15) and R Statistical Software (R Development Core Team, version 2.11.1) with the metafor package [52, 70].
Results
Selection process
The search resulted in a total of 10,301 hits. Initial selections based on titles identified 236 potentially relevant articles. Further selections based on abstracts excluded 142 studies. The full text of the remaining 94 studies was evaluated. Finally, a total of 53 studies with 14,966 patients were included (Fig. 1).
Description of identified studies
The most important characteristics of the included studies are presented in Table 2. Most studies were retrospective cohort studies (70%). The median sample size was 127 (range, 50–2,490) over a median inclusion periods of 12 years (range, 4–30). A diverting ileostomy was used in 79% (range, 5–100%) of all the IPAA procedures. A hand-sewn anastomosis was used in 40% of the procedures (range, 0–100%). Median duration of follow-up was 75 months (range, 6–180). Thirty-one studies mentioned postoperative mortality with a median of 0% (range, 0–2.9%).
Table 2.
Characteristics of studies and selected outcomes following IPAA in the 53 included studies published since 2000
| Author | Year of publication | Inclusion period | Number of patients | FU (months) | Age | Gender (% female) | Type of disease | Handsewn anastomosis (%) | With diverting ileostoma (%) |
|---|---|---|---|---|---|---|---|---|---|
| Fonkalsrud et al. [20] | 2000 | 1993–1997 | 77 | 34.5 | 50 | UC | 57.1 | 100 | |
| Karlbom et al. [36] | 2000 | 1983–1996 | 168 | 29 | 32 | 39.3 | UC | 58.9 | 70.8 |
| Seidel et al. [60] | 2000 | 1985–1996 | 55 | 31.2 | 45.5 | Both | |||
| Simchuk [61] | 2000 | 1987–1996 | 114 | 38 | 43.9 | Both | 100 | ||
| Gullberg and Liljeqvist [25] | 2001 | 1990–1995 | 86 | 72 | 34.1 | 45.3 | Both | 2.3 | 10.5 |
| Barton et al. [5] | 2001 | 1983–2000 | 110 | 30 | 36.8 | Both | 100 | 100 | |
| Heuschen et al. [29] | 2001 | 1991–2000 | 171 | 30 | 36.7 | 45.6 | UC | 100 | 66.7 |
| Regimbeau et al. [53] | 2001 | 1984–1998 | 172 | 60 | 36 | 47.1 | Both | 100 | 100 |
| Blumberg et al. [12] | 2001 | 1982–1995 | 145 | 34 | 49 | Both | 15.2 | ||
| Dayton et al. [16] | 2002 | 1982–2001 | 644 | 79 | 37.2 | 39.4 | UC | ||
| Rossi et al. [56] | 2002 | 1989–2000 | 75 | 40 | 33.3 | Both | 54.7 | 100 | |
| Bullard et al. [13] | 2002 | 1980–1992 | 154 | 151 | 34 | 44.2 | Both | 64 | |
| Gignoux et al. [22] | 2002 | 1993–1998 | 84 | 22 | 33 | 42.9 | Both | 100 | |
| Mukhtar et al. [47] | 2002 | 1990–1997 | 50 | 35 | 44 | Both | 2 | 98 | |
| Rudolph et al. [57] | 2002 | 1991–1999 | 71 | 47 | 38 | 56 | UC | 84.5 | |
| Carmon et al. [14] | 2003 | 1990–2001 | 77 | 51 | 38 | 55.8 | UC | 72.7 | |
| Teixeira et al. [63] | 2003 | 1986–2000 | 80 | 108 | 50 | UC | 11.3 | 77.5 | |
| Michelassi et al. [46] | 2003 | 1987–2002 | 391 | 37 | 33.7 | 44.2 | Both | 29.9 | 65 |
| Holubar and Hyman [32] | 2003 | 51 | 85 | 42.1 | 51 | UC | 70.6 | ||
| Fowler et al. [21] | 2003 | 1984–2001 | 106 | 40 | 50 | Both | 39.4 | 41.3 | |
| Parc et al. [49] | 2004 | 1983–1990 | 110 | 175 | 26.5 | 43.6 | FAP | 100 | |
| Lin et al. [43] | 2004 | 1985–2002 | 61 | 60 | 37 | 54 | Both | 67.2 | |
| Hueting et al. [34] | 2004 | 1989–2000 | 111 | 42 | 35.4 | 68.5 | UC | ||
| Gosselink et al. [23] | 2004 | 1989–2001 | 127 | 56 | 36 | 42.5 | UC | 21.6 | |
| Krausz et al. [40] | 2005 | 1984–2004 | 174 | 64 | 34.1 | 47.7 | Both | 54 | 87.4 |
| Hallberg et al. [26] | 2005 | 1990–1997 | 100 | 53 | 32 | 39 | UC | 17 | |
| Swenson et al. [62] | 2005 | 1995–2003 | 54 | 22 | 35 | 35.2 | 57.4 | ||
| Chapman et al. [15] | 2005 | 1981–2000 | 2002 | 121 | 33.5 | 46.6 | Both | 5 | |
| Kok Sun Ho et al. [30] | 2005 | 1989–2001 | 330 | 32 | 59.1 | UC | |||
| Ikeuchi et al. [35] | 2005 | 1999–2003 | 242 | 32.1 | 50.8 | UC | 100 | 38 | |
| Arai et al. [3] | 2005 | 1993–2003 | 296 | 53 | 33.8 | 43.2 | UC | 96.3 | 55.4 |
| Araki et a l. [4] | 2006 | 1998–2003 | 220 | 34.5 | 46.8 | Both | 47.3 | ||
| Rickard et al. [54] | 2006 | 1982–2002 | 516 | 33 | 45.2 | Both | 32.4 | 88 | |
| Bednarz et al. [6] | 2007 | 1994–2005 | 108 | 60 | 50 | Both | 18.5 | 100 | |
| Berndtsson et al. [8] | 2007 | 1982–1995 | 370 | 180 | 34 | 45.7 | UC | ||
| Gualdrini et al. [24] | 2007 | 1987–2005 | 391 | 45.6 | 35.4 | 51.7 | Both | ||
| Kiran et al. [38] | 2008 | 2016 | 180 | 37.7 | 43.9 | Both | 15.4 | 85.9 | |
| Tulchinsky et al. [66] | 2008 | 1986–2005 | 211 | 124.6 | 35.4 | 58.3 | UC | 16.5 | 79 |
| Walker and Bulow [67] | 2008 | 1987–2004 | 178 | 84 | 31 | 44.9 | Both | 6.7 | 100 |
| Ferrante et al. [18] | 2008 | 1990–2004 | 173 | 78 | 39 | 38.7 | UC | 2.3 | 85 |
| Leal et al. [41] | 2008 | 1984–2006 | 69 | 82 | 29.6 | 59.4 | FAP | 100 | 100 |
| Zarate et al. [71] | 2008 | 1984–2006 | 107 | 34.4 | 57 | Both | 12.1 | 100 | |
| Pinto et al. [50] | 2009 | 2001–2008 | 66 | 21.1 | 52.8 | 66.7 | Both | 18.2 | 100 |
| Leowardi et al. [42] | 2009 | 1988–1996 | 197 | 147.6 | 33 | 45.2 | UC | 100 | 100 |
| Norwood et al. [48] | 2009 | 1997–2007 | 107 | 77 | 38 | 45.8 | Both | 99 | |
| Loftus et al. [44] | 2009 | 2001–2005 | 237 | 5.9 | 38.9 | 45 | UC | ||
| Tekkis et al. [64] | 2009 | 1976–2006 | 2491 | 74.4 | 35.9 | 47.9 | Both | 33.3 | 67.3 |
| Scarpa et al. [58] | 2009 | 1984–2004 | 58 | 136 | 38 | 34.5 | UC | 0 | |
| Wasmuth et al. [68] | 2009 | 1984–2006 | 304 | 120 | 34.4 | 38.8 | Both | 40.1 | 84 |
| Andersson et al. [2] | 2009 | 1984–2003 | 110 | 144 | 35 | 45.5 | Both | 47.3 | |
| Fichera et al. [19] | 2009 | 2002–2007 | 106 | 24.8 | 36.9 | 42.2 | UC | 71.6 | |
| Rink et al. [55] | 2009 | 1990–2002 | 131 | 85 | 33 | 46.6 | UC | 84 | |
| Pricolo [51] | 2009 | 1991–2008 | 312 | 36 | 46.8 | Both | 8 |
Outcomes
Complications
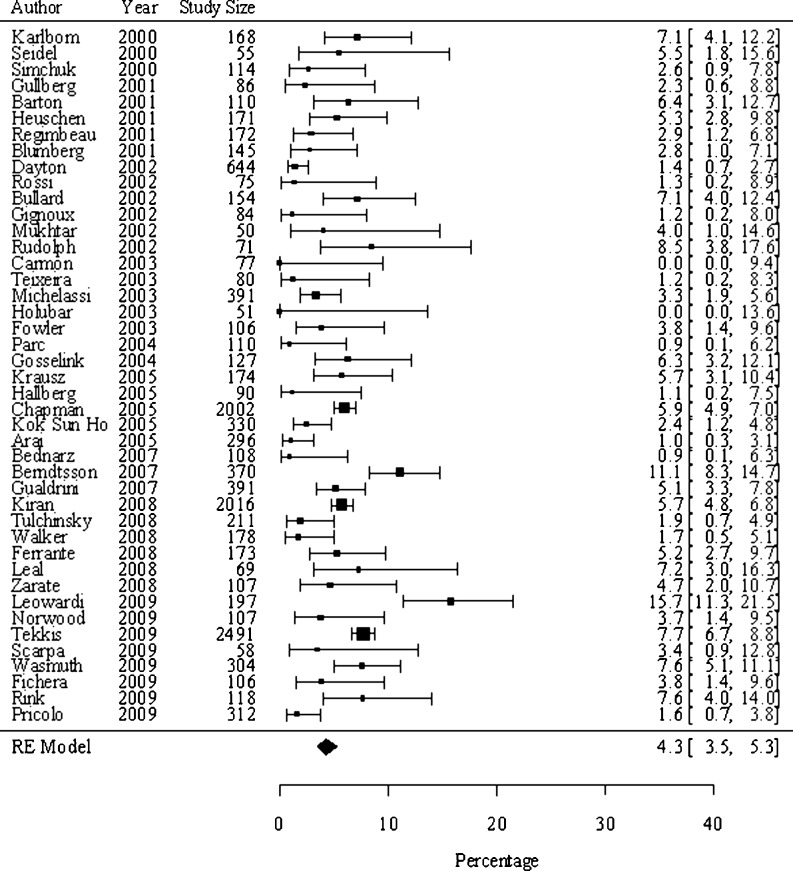
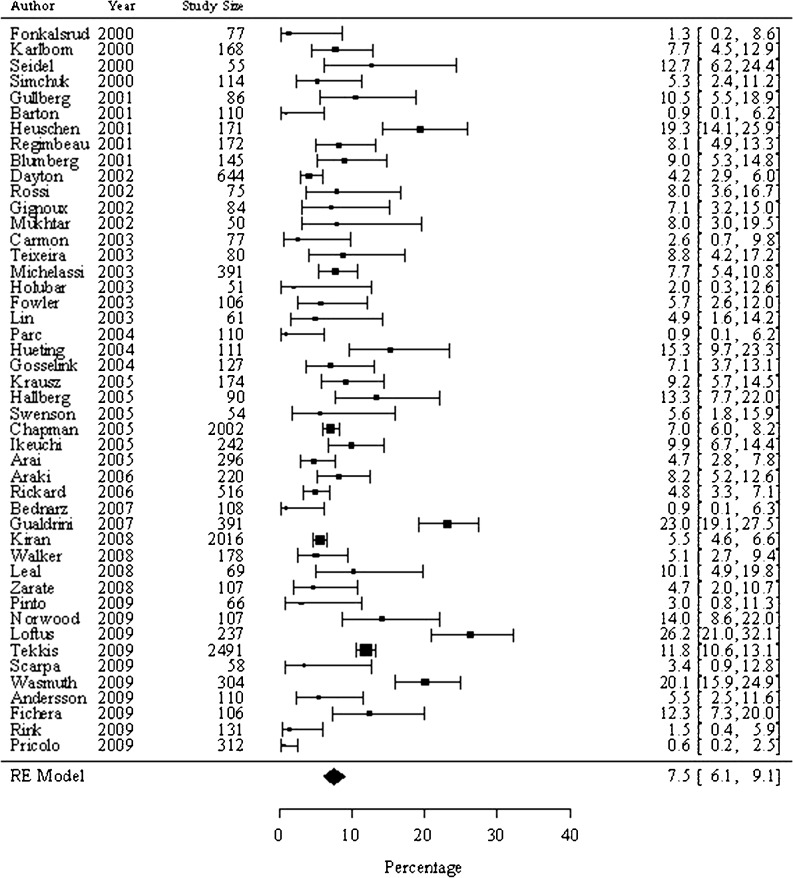
Data on complications were available from all 53 studies. We found a pooled incidence of pouch failure of 4.3% (95% CI, 3.5–6.3; Fig. 2). A sensitivity analysis including only studies with minimal follow-up of 5 years showed a pouch failure rate of 4.7%. The pooled incidence of pelvic sepsis was 7.5% (95% CI, 6.1–9.1; Fig. 3). Pooled incidence rates for other important complications are presented in Table 3.
Fig. 2.
Proportions of pouch failure following an IPAA procedure in studies published since 2000. The size of the dot correlates with the population size of the study. The lines represent the 95% CI. The pooled incidence of all studies is 4.3%
Fig. 3.
Proportions of pelvic sepsis following an IPAA procedure in studies published since 2000. The size of the dot correlates with the population size of the study. The lines represent the 95% CI. The pooled incidence of all studies is 7.5%
Table 3.
Pooled incidences of complications and functional outcome following an IPAA procedures in studies published since 2000 compared to studies published before 2000
| Since 2000 | Before 2000 | P value | |||||
|---|---|---|---|---|---|---|---|
| Number of studies | Number of patients | Pooled incidences | Number of studies | No. of patients | Pooled incidences | ||
| Complications | % (95% CI) | % (95%CI) | |||||
| Pouch failure | 43 | 13,249 | 4.3 (3.5–5.3) | 39 | 8,877 | 6.8 (5.8–8.4) | 0.0038 |
| Pouch failure: FU > 5 years | 22 | 9,873 | 4.7 (3.4–6.4) | 11 | 3,198 | 8.5 (5.4–13.2) | |
| Pelvic sepsis | 46 | 13,450 | 7.5 (6.1–9.1) | 41 | 9,082 | 9.5 (8.2–10.9) | NS |
| Fistula | 38 | 12,398 | 4.5 (3.5–5.7) | 30 | 5,120 | 5.5 (4.3–7.0) | NS |
| Stricture | 35 | 12,219 | 10.7 (8.2–13.8) | 28 | 5,185 | 9.2 (6.8–12.4) | NS |
| Pouchitis | 39 | 12,685 | 26.8 (21.0–33.5) | 33 | 7,289 | 18.8 (15.7–22.4) | NS |
| Sexual dysfunction | 13 | 6,131 | 3.0 (1.7–5.2) | 21 | 5,112 | 3.6 (2.7–4.7) | NS |
| Small bowel obstruction | 34 | 11,895 | 11.4 (9.1–14.1) | 27 | 5,853 | 13.1 (11.0–15.7) | NS |
| Fecal incontinence | %(95%CI) | % (95%CI) | |||||
| Mild day incontinence | 21 | 6,988 | 14.3 (7.3–25.9) | 31 | 4,313 | 17.0 (12.8–22.2) | NS |
| Severe day incontinence | 13 | 3,718 | 6.1 (2.9–12.3) | 27 | 3,914 | 3.7 (2.8–4.8) | NS |
| Mild night incontinence | 9 | 5,423 | 17.3 (4.7–46.8) | 17 | 2,582 | 13.1 (9.5–17.9) | NS |
| Severe night incontinence | 10 | 3,614 | 7.6 (2.5–21.3) | 9 | 1,271 | 4.5 (3.0–6.7) | NS |
| Frequency | Mean (95%CI) | Mean (95%CI) | |||||
| Frequency day | 26 | 5,321 | 5.7 (4.9–6.7) | 13 | 2,277 | 5.2 (4.0–6.7) | NS |
| Frequency night | 22 | 7,117 | 1.5 (1.0–2.1) | 20 | 2,950 | 1.0 (0.6–1.6) | NS |
| Frequency 24 h | 26 | 5,132 | 5.9 (5.0–6.9) | 20 | 3,547 | 5.2 (4.4–6.1) | NS |
CI confidence interval, FU follow-up period
Functional results
Data on functional results after IPAA were available from 26 studies including 5,321 patients. The pooled incidence of mild and severe fecal incontinence during the day was 14.3% (%CI, 7.3–25.9) and 6.1% (2.9–12.3), respectively (Table 3). Mean defecation frequency was 5.9 (4.9–6.7) per 24 h with a mean nighttime frequency of 1.5 (1.0–2.1).
Comparison with studies published before 2000
The previous review of studies published before 2000 identified 43 studies with a total of 9,317 patients [33]. Median duration of follow-up was 36.7 months (range, 12–99). Detailed discussion of the characteristics of these studies is published elsewhere [33].
We compared incidences of the most important complications reported in studies published prior to 2000 versus the incidences reported in studies published since 2000 (Table 3). Pouch failure decreased between the two time periods from 6.8% to 4.3% (p = 0.0038). Pelvic sepsis showed a decrease from 9.5 to 7.4% (p = 0.1284). Other complications and the functional results showed no significant differences between the two groups of studies.
The effect of time of study conductance on IPAA outcomes
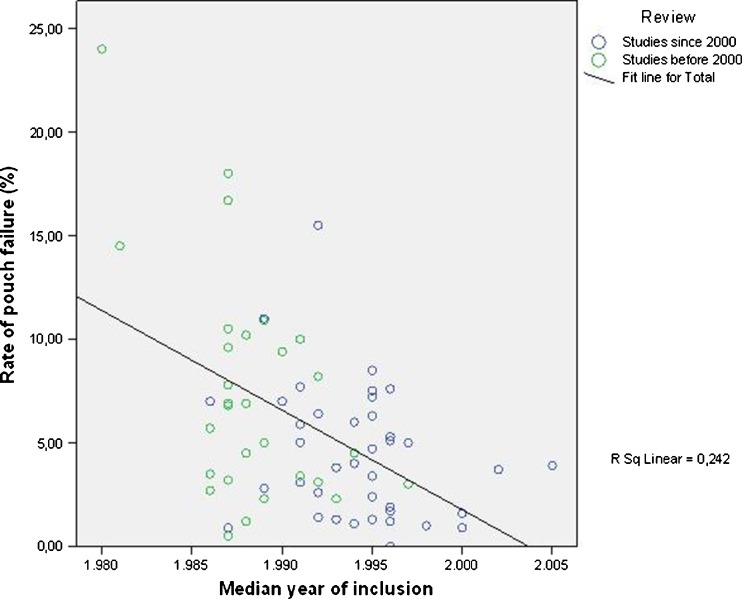
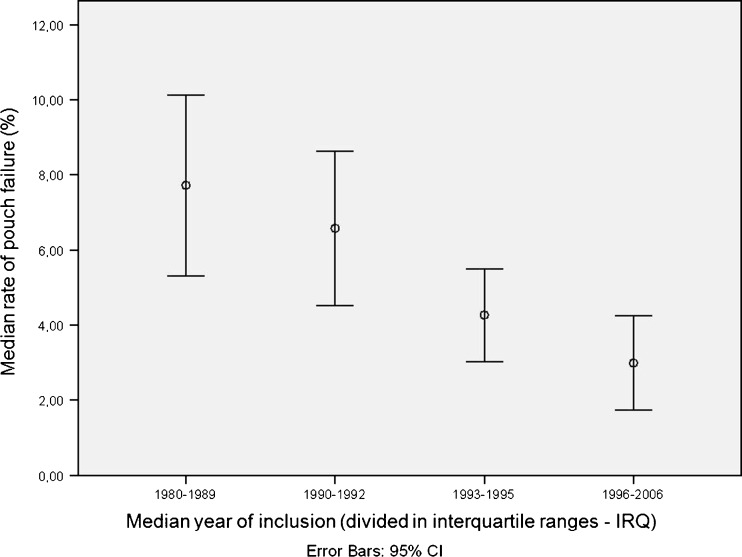
Results of both reviews were combined to analyze the effect of time of study conductance on the outcomes of the IPAA procedure. For this, the relationship between the median year of inclusion of each study and the outcomes observed in that study was evaluated. Regression analysis showed that studies with an earlier median year of inclusion have a higher rate of pouch failure than studies with a more recent median year of inclusion (p < 0.001). Figure 4 is a scatter plot depicting this relationship. In a sensitivity analysis excluding the five studies with a pouch failure rate of >12.5%, the relationship remained statistically significant (p = 0.009). Additionally, we categorized the median year of inclusion of all studies (published before and after 2000) into four interquartile ranges in order to evaluate the median rate of pouch failure over these four time periods. Figure 5 shows a consecutive decline in the pouch failure rate over these time periods (p = 0.005, one-way ANOVA analysis).
Fig. 4.
Scatter plot depicting the median year of inclusion and the rate of pouch failure of studies included in both reviews
Fig. 5.
Error bar chart depicting the median rate of pouch failure compared to the median year of inclusion (divided into interquartile ranges)
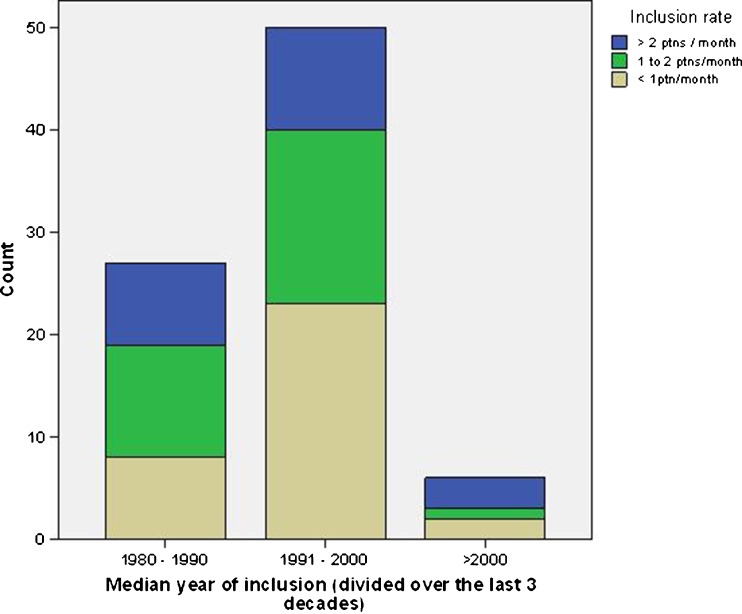
Centralization: trends over time
The median inclusion rate for all studies was 14 patients per year (range from 2.9 to 105). We evaluated the effect of time of study conductance (median year of inclusion) on the inclusion rate (Fig. 6). The figure shows that between 1991 and 2000, an increase was seen in studies from centers including less than one patient per month, from eight studies (30%) before 1991 to 23 studies (46%) between 1991 and 2000. It also shows that there are not yet enough studies available that have been conducted after 2000 to draw conclusions about the current situation. Analysis of the effect of the inclusion rate on the outcomes of the IPAA did not show any benefit on the outcomes of the IPAA.
Fig. 6.
Relationship between moment of study conductance (median year of inclusion) and inclusion rate of patients, divided in the past three decades
Technical aspects of the IPAA
Overall, 43 out of 78 studies (55%) used a protective ileostomy as a routine part of the IPAA procedure (routine use defined as ileostomy performed in more than 80% of patients). The percentage has decreased from almost 70% (16 out of 23) in studies conducted between 1980 and 1990 to 47% (21 out of 44) in studies conducted after 1990. The number of studies performing an ileostomy in <50% of patients increased from 11% to 32% over the same periods. The rate of ileostomy was not associated with any of the outcomes of the IPAA. Type of anastomosis (hand-sewn vs. stapled) was only available from 31 studies published since 2000 (the previous review did not register this characteristic). Fifteen studies (48%) still performed a hand-sewn anastomosis in more than 50% of patients. There were no differences in functional outcome or complications between studies performing different types of anastomosis.
Discussion
The open IPAA operation is the most common surgical reconstruction procedure in patients with UC and FAP. Randomized trials on IPAA are rare [1] due to low incidences as well as the complexity of patient selection and the intervention. Therefore, most studies are retrospective case series. Estimates of the outcomes of the IPAA procedure vary considerably. Acceptable complication and functional outcome rates are, therefore, difficult to set. This systematic review provides up to date and reliable incidences of important outcomes of the IPAA procedure, which could provide a reference values for these outcomes. Additionally, this review may provide insights in changes of practice over time and their effects on outcomes.
Several important finding are provided. First, it shows that the rate of pouch failure after an IPAA procedure has declined continuously over time. This decline was larger in the earlier period of the IPAA but seems to continue over time. Secondly, a large proportion of studies with this complex type of surgery are conducted in centers that include less than one patient per month. Thirdly, the functional outcome of the IPAA seems not to improve over time, despite several developments in surgical technique and perioperative care. This may represent an intrinsic limitation of the IPAA technique regarding functional outcome.
This review has some limitations. First, many of the included studies are retrospective cohort series, which may limit the reliability of the results. However, the overwhelming majority of the evidence in this field consists of this type of studies. This review provides an overview of this evidence, thereby increases its utility for clinicians and researchers. Moreover, the statistical techniques used are rather conservative to allow for incorporation of the heterogeneity of the studies.
Second, publication bias is a factor that should be taken into consideration. For this purpose, we excluded series with <50 patients. Studies with a small sample size do not only increase heterogeneity of results but are also more subject to publication bias; i.e., small studies with “unfavorable” results are less likely to get published. By introducing a threshold, we aimed to prevent including small studies with overestimated intervention effects.
Finally, the lack of individual patient data limits the analyses that could be performed. For example, many studies report a cohort in which several types of operative techniques have been used (e.g., several types of anastomses). This prohibits analyzing the effect of variations in technique on a patient level, since only aggregate outcomes of the complete cohorts are available. Collecting individual patient data of these large numbers of studies, especially considering the dated studies, is not feasible. We, therefore, limited our analyses to factors that could be analyzed reliably on an aggregate level.
Many factors may have contributed to the reduction of the rate of pouch failure observed. The additional analyses in this review were unable to pinpoint factors responsible for the observed reduction in pouch failure. This is probably caused by the lack of individual patient data (as discussed above), and we believe that general improvements in care over the past decades and the increased experience of surgeons with this approach are the most important factors contributing to this finding.
Another explanation that could be considered is the variation in the surgical techniques that have been introduced and sometimes largely employed over the last decades. Such variations include the various types of pouches used and the use of the double-stapled anastomosis. The routinely constructed deviating ileostoma does not seem to improve the frequency of postoperative complications but only their severity. Despite comparative studies and several large meta-analyses published previously, none of these variations in technique could be identified as factors associated with the reduction of postoperative complications, including pouch failure. [45, 69] This is in line with the findings in this review.
Fewer studies reported on other outcomes, which decreased the power of the analyses concerning these other outcomes. Secondly, it could be that the observed decrease in the rate of pouch failure may be, at least in part, a result of smaller decreases in various other postoperative complications. Complications like pelvic sepsis, fistulae, and strictures could all result in pouch failure, provided they were severe enough. Smaller decreases in these outcomes can be difficult to show statistically. Overall, however, they may have caused the observed substantial decrease in pouch failure rate.
Recently, discussions on the relation between volume of complex surgical interventions and outcomes have gained wide attention [7, 17, 27, 37]. Certain complex surgical interventions have been centralized in high-volume hospitals with improved outcomes [9–11, 31]. Centralization still has to be reflected in the data in the years to come. Therefore, this review was unable to evaluate the potential influence of this development on current practice. However, in the period from 1991 to 2000, nearly 50% of studies were performed in “low inclusion rate” centers (including less than one patient per month). This is a substantial increase from the 30% observed in the period from1980 to 1990. Taking into account that we only included series of 50 patients or more (Fig. 1) may mean that the true proportion of studies conducted in such “low inclusion rate” centers may be much higher. With the repeatedly established relationship between volume and outcome in several fields of surgery, this is a troublesome observation. Centralization of the complex IPAA procedure may offer a way to further improve outcomes in future.
Finally, we found no statistically significant differences in pooled estimates of the functional outcome over time. There were also no differences in functional outcomes between various surgical factors studied in this review. This is in agreement with findings in literature showing no benefits in terms of functional outcome of technical developments of the IPAA procedure, like type of anastomosis [59] or laparoscopic approach [1]. In most patients, however, functional outcome of the IPAA is considered to be highly satisfactorily, allowing for an acceptable quality of life and social functioning [28, 65]. Therefore, reducing complications, especially severe complications like pelvic sepsis and pouch failure, seems to be a more important goal for future surgical developments.
Conclusions
This systematic review and meta-analysis summarizes the available evidence and provides up to date estimates for complications and functional outcome after an IPAA procedure that can be useful as reference values for practice and research. It also shows a reduction in pouch failure over time in patients operated on using the IPAA procedure. The functional results remain unchanged over time and between various operative factors.
Acknowledgment
We did not receive any financial or material support for the research and the work. The first two authors have full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Ahmed AU, Keus F, Heikens JT, Bemelman WA, Berdah SV, Gooszen HG, and van Laarhoven CJ (2009) Open versus laparoscopic (assisted) ileo pouch anal anastomosis for ulcerative colitis and familial adenomatous polyposis. Cochrane Database Syst Rev, CD006267 [DOI] [PubMed]
- 2.Andersson T, Lunde OC, Johnson E, Moum T, and Nesbakken A (2011) Long-term functional outcome and quality of life after restorative proctocolectomy with ileo-anal anastomosis for colitis. Colorectal Dis 13:431–437 [DOI] [PubMed]
- 3.Arai K, Koganei K, Kimura H, Akatani M, Kitoh F, Sugita A, Fukushima T. Incidence and outcome of complications following restorative proctocolectomy. Am J Surg. 2005;190:39–42. doi: 10.1016/j.amjsurg.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 4.Araki T, Parc Y, Lefevre J, Dehni N, Tiret E, Parc R. The effect on morbidity of mesentery lengthening techniques and the use of a covering stoma after ileoanal pouch surgery. Dis Colon Rectum. 2006;49:621–628. doi: 10.1007/s10350-005-0322-3. [DOI] [PubMed] [Google Scholar]
- 5.Barton JG, Paden MA, Lane M, Postier RG. Comparison of postoperative outcomes in ulcerative colitis and familial polyposis patients after ileoanal pouch operations. Am J Surg. 2001;182:616–620. doi: 10.1016/S0002-9610(01)00795-4. [DOI] [PubMed] [Google Scholar]
- 6.Bednarz W, Olewinski R, Woldan J. Ileal-pouch-anal anastomosis after restorative proctocolectomy in patients with ulcerative colitis or familial adenomatous polyposis—11 years of experience. Polski Przeglad Chirurgiczny. 2007;79:652–662. [Google Scholar]
- 7.Begg CB, Cramer LD, Hoskins WJ, Brennan MF. Impact of hospital volume on operative mortality for major cancer surgery. JAMA. 1998;280:1747–1751. doi: 10.1001/jama.280.20.1747. [DOI] [PubMed] [Google Scholar]
- 8.Berndtsson I, Lindholm E, Oresland T, Borjesson L. Long-term outcome after ileal pouch-anal anastomosis: function and health-related quality of life. Dis Colon Rectum. 2007;50:1545–1552. doi: 10.1007/s10350-007-0278-6. [DOI] [PubMed] [Google Scholar]
- 9.Birkmeyer JD, Siewers AE, Finlayson EV, Stukel TA, Lucas FL, Batista I, Welch HG, Wennberg DE. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346:1128–1137. doi: 10.1056/NEJMsa012337. [DOI] [PubMed] [Google Scholar]
- 10.Birkmeyer JD, Sun Y, Wong SL, Stukel TA. Hospital volume and late survival after cancer surgery. Ann Surg. 2007;245:777–783. doi: 10.1097/01.sla.0000252402.33814.dd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Birkmeyer NJ, Goodney PP, Stukel TA, Hillner BE, Birkmeyer JD. Do cancer centers designated by the National Cancer Institute have better surgical outcomes? Cancer. 2005;103:435–441. doi: 10.1002/cncr.20785. [DOI] [PubMed] [Google Scholar]
- 12.Blumberg D, Opelka FG, Hicks TC, Timmcke AE, Beck DE. Restorative proctocolectomy: Ochsner Clinic experience. South Med J. 2001;94:467–471. [PubMed] [Google Scholar]
- 13.Bullard KM, Madoff RD, Gemlo BT. Is ileoanal pouch function stable with time? Results of a prospective audit. Dis Colon Rectum. 2002;45:299–304. doi: 10.1007/s10350-004-6171-7. [DOI] [PubMed] [Google Scholar]
- 14.Carmon E, Keidar A, Ravid A, Goldman G, Rabau M. The correlation between quality of life and functional outcome in ulcerative colitis patients after proctocolectomy ileal pouch anal anastomosis. Colorectal Dis. 2003;5:228–232. doi: 10.1046/j.1463-1318.2003.00445.x. [DOI] [PubMed] [Google Scholar]
- 15.Chapman JR, Larson DW, Wolff BG, Dozois EJ, Cima RR, Pemberton JH, Crownhart BS, Larson DR. Ileal pouch-anal anastomosis: does age at the time of surgery affect outcome? Arch Surg. 2005;140:534–539. doi: 10.1001/archsurg.140.6.534. [DOI] [PubMed] [Google Scholar]
- 16.Dayton MT, Larsen KR, Christiansen DD. Similar functional results and complications after ileal pouch-anal anastomosis in patients with indeterminate vs ulcerative colitis. Arch Surg. 2002;137:690–694. doi: 10.1001/archsurg.137.6.690. [DOI] [PubMed] [Google Scholar]
- 17.Dudley RA, Johansen KL, Brand R, Rennie DJ, Milstein A. Selective referral to high-volume hospitals: estimating potentially avoidable deaths. JAMA. 2000;283:1159–1166. doi: 10.1001/jama.283.9.1159. [DOI] [PubMed] [Google Scholar]
- 18.Ferrante M, Declerck S, De HG, Van AG, Geboes K, Rutgeerts P, Penninckx F, Vermeire S, D'Hoore A. Outcome after proctocolectomy with ileal pouch-anal anastomosis for ulcerative colitis. Inflamm Bowel Dis. 2008;14:20–28. doi: 10.1002/ibd.20278. [DOI] [PubMed] [Google Scholar]
- 19.Fichera A, Silvestri MT, Hurst RD, Rubin MA, Michelassi F. Laparoscopic restorative proctocolectomy with ileal pouch anal anastomosis: a comparative observational study on long-term functional results. J Gastrointest Surg. 2009;13:526–532. doi: 10.1007/s11605-008-0755-9. [DOI] [PubMed] [Google Scholar]
- 20.Fonkalsrud EW, Thakur A, Roof L. Comparison of loop versus end ileostomy for fecal diversion after restorative proctocolectomy for ulcerative colitis. J Am Coll Surg. 2000;190:418–422. doi: 10.1016/S1072-7515(99)00295-1. [DOI] [PubMed] [Google Scholar]
- 21.Fowler AL, Turner BN, Thomson WH. A study of the complications and pelvic visceral function after restorative proctocolectomy and W pouch construction. Colorectal Dis. 2003;5:342–346. doi: 10.1046/j.1463-1318.2003.00473.x. [DOI] [PubMed] [Google Scholar]
- 22.Gignoux B-M, Dehni N, Parc R, Tiret E. Ileal pouch anal-anastomosis without covering ileostomy. [French] Gastroenterol Clin Biol. 2002;26:671–674. [PubMed] [Google Scholar]
- 23.Gosselink MP, Schouten WR, van Lieshout LM, Hop WC, Laman JD, Ruseler-van Embden JG. Delay of the first onset of pouchitis by oral intake of the probiotic strain Lactobacillus rhamnosus GG. Dis Colon Rectum. 2004;47:876–884. doi: 10.1007/s10350-004-0525-z. [DOI] [PubMed] [Google Scholar]
- 24.Gualdrini U, Coraglio M, Filippa L, Masciangioli G, Gutierrez A, Lumi C, Graziano A. Long term functional outcomes after ileoanal pouch in patients with and without postoperative complications] Acta Gastroenterol Latinoam. 2007;37(3):143–149. [PubMed] [Google Scholar]
- 25.Gullberg K, Liljeqvist L. Stapled ileoanal pouches without loop ileostomy: a prospective study in 86 patients. Int. J. Colorectal Dis. 2001;16:221–227. doi: 10.1007/s003840100289. [DOI] [PubMed] [Google Scholar]
- 26.Hallberg H, Stahlberg D, Akerlund JE. Ileal pouch-anal anastomosis (IPAA): functional outcome after postoperative pelvic sepsis. A prospective study of 100 patients. Int J Colorectal Dis. 2005;20:529–533. doi: 10.1007/s00384-004-0717-y. [DOI] [PubMed] [Google Scholar]
- 27.Halm EA, Lee C, Chassin MR. Is volume related to outcome in health care? A systematic review and methodologic critique of the literature. Ann Intern Med. 2002;137:511–520. doi: 10.7326/0003-4819-137-6-200209170-00012. [DOI] [PubMed] [Google Scholar]
- 28.Heikens JT, de VJ, and van Laarhoven CJ (2011) Quality of life, health related quality of life and health status in patients having restorative proctocolectomy with ileal pouch-anal anastomosis for ulcerative colitis: a systematic review. Colorectal Dis 2010 Dec 22 doi:10.1111/j.1463-1318.2010.02538.x [DOI] [PubMed]
- 29.Heuschen UA, Hinz U, Allemeyer EH, Lucas M, Heuschen G, Herfarth C. One- or two-stage procedure for restorative proctocolectomy: rationale for a surgical strategy in ulcerative colitis. Ann Surg. 2001;234:788–794. doi: 10.1097/00000658-200112000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ho KS, Chang CC, Baig MK, Borjesson L, Nogueras JJ, Efron J, Weiss EG, Sands D, Vernava AM, III, Wexner SD. Ileal pouch anal anastomosis for ulcerative colitis is feasible for septuagenarians. Colorectal Dis. 2006;8:235–238. doi: 10.1111/j.1463-1318.2005.00885.x. [DOI] [PubMed] [Google Scholar]
- 31.Hollenbeck BK, Wei Y, Birkmeyer JD. Volume, process of care, and operative mortality for cystectomy for bladder cancer. Urology. 2007;69:871–875. doi: 10.1016/j.urology.2007.01.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Holubar S, Hyman N. Continence alterations after ileal pouch-anal anastomosis do not diminish quality of life. Dis Colon Rectum. 2003;46:1489–1491. doi: 10.1007/s10350-004-6799-3. [DOI] [PubMed] [Google Scholar]
- 33.Hueting WE, Buskens E, van der Tweel I, Gooszen HG, van Laarhoven CJ. Results and complications after ileal pouch anal anastomosis: a meta-analysis of 43 observational studies comprising 9,317 patients. Dig Surg. 2005;22:69–79. doi: 10.1159/000085356. [DOI] [PubMed] [Google Scholar]
- 34.Hueting WE, Gooszen HG, van Laarhoven CJ. Sexual function and continence after ileo pouch anal anastomosis: a comparison between a meta-analysis and a questionnaire survey. Int J Colorectal Dis. 2004;19:215–218. doi: 10.1007/s00384-003-0543-7. [DOI] [PubMed] [Google Scholar]
- 35.Ikeuchi H, Nakano H, Uchino M, Nakamura M, Noda M, Yanagi H, Yamamura T. Safety of one-stage restorative proctocolectomy for ulcerative colitis. Dis Colon Rectum. 2005;48:1550–1555. doi: 10.1007/s10350-005-0083-z. [DOI] [PubMed] [Google Scholar]
- 36.Karlbom U, Raab Y, Ejerblad S, Graf W, Thorn M, Pahlman L. Factors influencing the functional outcome of restorative proctocolectomy in ulcerative colitis. Br J Surg. 2000;87:1401–1408. doi: 10.1046/j.1365-2168.2000.01533.x. [DOI] [PubMed] [Google Scholar]
- 37.Killeen SD, O'Sullivan MJ, Coffey JC, Kirwan WO, Redmond HP. Provider volume and outcomes for oncological procedures. Br J Surg. 2005;92:389–402. doi: 10.1002/bjs.4954. [DOI] [PubMed] [Google Scholar]
- 38.Kiran RP, Remzi FH, Fazio VW, Lavery IC, Church JM, Strong SA, Hull TL. Complications and functional results after ileoanal pouch formation in obese patients. J Gastrointest Surg. 2008;12:668–674. doi: 10.1007/s11605-008-0465-3. [DOI] [PubMed] [Google Scholar]
- 39.Knapp G, Hartung J. Improved tests for a random effects meta-regression with a single covariate. Stat Med. 2003;22:2693–2710. doi: 10.1002/sim.1482. [DOI] [PubMed] [Google Scholar]
- 40.Krausz MM, Duek SD. Restorative proctocolectomy with ileal pouch-anal anastomosis for ulcerative colitis and familial adenomatous polyposis: twenty years follow-up in 174 patients. Isr Med Assoc J. 2005;7:23–27. [PubMed] [Google Scholar]
- 41.Leal RF, Ayrizono MDLS, Coy CSR, Fagundes JJ, Goes JRN. Short-term and long-term postoperative complications after ileal pouch-anal anastomosis in familial adenomatous polyposis. Arq Gastroenterol. 2008;45:106–110. doi: 10.1590/S0004-28032008000200003. [DOI] [PubMed] [Google Scholar]
- 42.Leowardi C, Hinz U, Tariverdian M, Kienle P, Herfarth C, Ulrich A, Kadmon M. Long-term outcome 10 years or more after restorative proctocolectomy and ileal pouch-anal anastomosis in patients with ulcerative colitis. Langenbecks Arch. Surg. 2010;395:49–56. doi: 10.1007/s00423-009-0479-7. [DOI] [PubMed] [Google Scholar]
- 43.Lin JJ, Song ZF, Xu JH. [The prognosis of the total proctocolectomy and ileal-pouch anal anastomosis. Zhonghua Wai Ke. Za Zhi. 2004;42(14):861–863. [PubMed] [Google Scholar]
- 44.Loftus EV, Jr, Friedman HS, Delgado DJ, Sandborn WJ. Colectomy subtypes, follow-up surgical procedures, postsurgical complications, and medical charges among ulcerative colitis patients with private health insurance in the United States. Inflamm Bowel Dis. 2009;15:566–575. doi: 10.1002/ibd.20810. [DOI] [PubMed] [Google Scholar]
- 45.Lovegrove RE, Constantinides VA, Heriot AG, Athanasiou T, Darzi A, Remzi FH, Nicholls RJ, Fazio VW, Tekkis PP. A comparison of hand-sewn versus stapled ileal pouch anal anastomosis (IPAA) following proctocolectomy: a meta-analysis of 4183 patients. Ann Surg. 2006;244:18–26. doi: 10.1097/01.sla.0000225031.15405.a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Michelassi F, Lee J, Rubin M, Fichera A, Kasza K, Karrison T, Hurst RD. Long-term functional results after ileal pouch anal restorative proctocolectomy for ulcerative colitis: a prospective observational study. Ann Surg. 2003;238:433–441. doi: 10.1097/01.sla.0000086658.60555.ea. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mukhtar H, Zak A, Berry AR. Restorative proctocolectomy: one surgeon's experience of a now routine procedure in a district general hospital. JR Coll Surg Edinb. 2002;47:400–406. [PubMed] [Google Scholar]
- 48.Norwood MG, Mann CD, West K, Miller AS, Hemingway D. Restorative proctocolectomy. Does ethnicity affect outcome? Colorectal Dis. 2009;11:972–975. doi: 10.1111/j.1463-1318.2008.01727.x. [DOI] [PubMed] [Google Scholar]
- 49.Parc Y, Piquard A, Dozois RR, Parc R, Tiret E. Long-term outcome of familial adenomatous polyposis patients after restorative coloproctectomy. Ann Surg. 2004;239:378–382. doi: 10.1097/01.sla.0000114216.90947.f6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pinto RA, Canedo J, Murad-Regadas S, Regadas SF, Weiss EG, Wexner SD. Ileal pouch anal anastomosis (IPAA) in the elderly: is there difference in the morbidity compared to younger patients? Colorectal Dis. 2009;13:177–183. doi: 10.1111/j.1463-1318.2009.02097.x. [DOI] [PubMed] [Google Scholar]
- 51.Pricolo VE. Ileal pouch-anal anastomosis for ulcerative colitis—the Rhode Island experience. Med Health R I. 2009;92:100–102. [PubMed] [Google Scholar]
- 52.R Development Core Team (2010) R: A language and environment for statistical computing. R Foundation forStatistical Computing, Vienna
- 53.Regimbeau JM, Panis Y, Pocard M, Hautefeuille P, Valleur P. Handsewn ileal pouch-anal anastomosis on the dentate line after total proctectomy: technique to avoid incomplete mucosectomy and the need for long-term follow-up of the anal transition zone. Dis Colon Rectum. 2001;44:43–50. doi: 10.1007/BF02234819. [DOI] [PubMed] [Google Scholar]
- 54.Rickard MJFX, Young CJ, Bissett IP, Stitz R, Solomon MJ. Ileal pouch-anal anastomosis: the Australasian experience. Color Dis. 2007;9:139–145. doi: 10.1111/j.1463-1318.2006.01151.x. [DOI] [PubMed] [Google Scholar]
- 55.Rink AD, Radinski I, Vestweber KH. Does mesorectal preservation protect the ileoanal anastomosis after restorative proctocolectomy? J Gastrointest Surg. 2009;13:120–128. doi: 10.1007/s11605-008-0665-x. [DOI] [PubMed] [Google Scholar]
- 56.Rossi HL, Brand MI, Saclarides TJ. Anal complications after restorative proctocolectomy (J-pouch) Am Surg. 2002;68:628–630. [PubMed] [Google Scholar]
- 57.Rudolph WG, Uthoff SM, McAuliffe TL, Goode ET, Petras RE, Galandiuk S. Indeterminate colitis: the real story. Dis Colon Rectum. 2002;45:1528–1534. doi: 10.1007/s10350-004-6461-0. [DOI] [PubMed] [Google Scholar]
- 58.Scarpa M, Mescoli C, Rugge M, D'Inca R, Ruffolo C, Polese L, D'Amico DF, Sturniolo GC, Angriman I. Restorative proctocolectomy for inflammatory bowel disease: the Padova prognostic score for colitis in predicting long-term outcome and quality of life. Int J Colorectal Dis. 2009;24:1049–1057. doi: 10.1007/s00384-009-0700-8. [DOI] [PubMed] [Google Scholar]
- 59.Schluender SJ, Mei L, Yang H, Fleshner PR. Can a meta-analysis answer the question: is mucosectomy and handsewn or double-stapled anastomosis better in ileal pouch-anal anastomosis? Am Surg. 2006;72:912–916. [PubMed] [Google Scholar]
- 60.Seidel SA, Newman M, Sharp KW. Ileoanal pouch versus ileostomy: is there a difference in quality of life? Am Surg. 2000;66:540–546. [PubMed] [Google Scholar]
- 61.Simchuk EJ, Thirlby RC. Risk factors and true incidence of pouchitis in patients after ileal pouch-anal anastomoses. World J Surg. 2000;24:851–856. doi: 10.1007/s002680010136. [DOI] [PubMed] [Google Scholar]
- 62.Swenson BR, Hollenbeak CS, Poritz LS, Koltun WA. Modified two-stage ileal pouch-anal anastomosis: equivalent outcomes with less resource utilization. Dis Colon Rectum. 2005;48:256–261. doi: 10.1007/s10350-004-0848-9. [DOI] [PubMed] [Google Scholar]
- 63.Teixeira MG, Ponte AC, Sousa M, Almeida MG, Silva FE, Calache JE, Habr-Gama A, Kiss DR. Short- and long-term outcomes of ileal pouch-anal anastomosis for ulcerative colitis. Rev Hosp Clin Fac Med. Sao Paulo. 2003;58:193–198. doi: 10.1590/s0041-87812003000400002. [DOI] [PubMed] [Google Scholar]
- 64.Tekkis PP, Lovegrove RE, Tilney HS, Smith JJ, Sagar PM, Shorthouse AJ, Mortensen NJ, and Nicholls RJ (2010) Long-term failure and function after restorative proctocolectomy—a multi-centre study of patients from the UK National Ileal Pouch Registry. Colorectal Dis 12:433–441 [DOI] [PubMed]
- 65.Thirlby RC, Sobrino MA, Randall JB. The long-term benefit of surgery on health-related quality of life in patients with inflammatory bowel disease. Arch Surg. 2001;136:521–527. doi: 10.1001/archsurg.136.5.521. [DOI] [PubMed] [Google Scholar]
- 66.Tulchinsky H, Dotan I, Alper A, Brazowski E, Klausner JM, Halpern Z, Rabau M. Comprehensive pouch clinic concept for follow-up of patients after ileal pouch anal anastomosis: report of 3 years' experience in a tertiary referral center. Inflamm. Bowel Dis. 2008;14:1125–1132. doi: 10.1002/ibd.20430. [DOI] [PubMed] [Google Scholar]
- 67.Walker LR, Bulow S. Restorative proctocolectomy with an ileoanal pouch. Postoperative course and long-term functional results. Ugeskr. Laege. 2008;170(20):1721–1725. [PubMed] [Google Scholar]
- 68.Wasmuth HH, Trano G, Endreseth B, Rydning A, Wibe A, Myrvold HE. Long-term surgical load in patients with ileal pouch-anal anastomosis. Color Dis. 2009;11:711–718. doi: 10.1111/j.1463-1318.2008.01671.x. [DOI] [PubMed] [Google Scholar]
- 69.Weston-Petrides GK, Lovegrove RE, Tilney HS, Heriot AG, Nicholls RJ, Mortensen NJ, Fazio VW, Tekkis PP. Comparison of outcomes after restorative proctocolectomy with or without defunctioning ileostomy. Arch Surg. 2008;143:406–412. doi: 10.1001/archsurg.143.4.406. [DOI] [PubMed] [Google Scholar]
- 70.Viechtbauer W. Conducting meta-analyses in R with the Metafor Package. J Stat Softw. 2010;36:1–48. [Google Scholar]
- 71.Zarate CA, Zuniga DA, Pinedo MG, Lopez KF, Molina PM, Viviani GP. Ileal pouch-anal anastomosis for ulcerative colitis: complications and long term functional results. Rev Med Chil. 2008;136:467–474. [PubMed] [Google Scholar]