Executive Summary
Objective
The Ontario Health Technology Advisory Committee asked the Medical Advisory Secretariat (MAS) to conduct a health technology assessment on energy delivery systems for the treatment of benign prostatic hyperplasia (BPH).
Clinical Need: Target Population and Condition
BPH is a noncancerous enlargement of the prostate gland and the most common benign tumour in aging men. (1) It is the most common cause of lower urinary tract symptoms (LUTS) and bladder outlet obstruction (BOO) and is an important cause of diminished quality of life among aging men. (2) The primary goal in the management of BPH for most patients is a subjective improvement in urinary symptoms and quality of life.
Until the 1930s, open prostatectomy, though invasive, was the most effective form of surgical treatment for BPH. Today, the benchmark surgical treatment for BPH is transurethral resection of the prostate (TURP), which produces significant changes of all subjective and objective outcome parameters. Complications after TURP include hemorrhage during or after the procedure, which often necessitates blood transfusion; transurethral resection (TUR) syndrome; urinary incontinence; bladder neck stricture; and sexual dysfunction. A retrospective review of 4,031 TURP procedures performed by one surgeon between 1979 and 2003 showed that the incidence of complications was 2.4% for blood transfusion, 0.3% for TUR syndrome, 1.5% for hemostatic procedures, 2.8% for bladder neck contracture, and 1% for urinary stricture. However, the incidence of blood transfusion and TUR syndrome decreased as the surgeon’s skills improved.
During the 1990s, a variety of endoscopic techniques using a range of energy sources have been developed as alternative treatments for BPH. These techniques include the use of light amplification by stimulated emission of radiation (laser), radiofrequency, microwave, and ultrasound, to heat prostate tissue and cause coagulation or vaporization. In addition, new electrosurgical techniques that use higher amounts of energy to cut, coagulate, and vaporize prostatic tissue have entered the market as competitors to TURP. The driving force behind these new treatment modalities is the potential of producing good hemostasis, thereby reducing catheterization time and length of hospital stay. Some have the potential to be used in an office environment and performed under local anesthesia. Therefore, these new procedures have the potential to rival TURP if their effectiveness is proven over the long term.
The Technology Being Reviewed
The following energy-based techniques were considered for assessment:
transurethral electrovaporization of the prostate (TUVP)
transurethral electrovapor resection of the prostate (TUVRP)
transurethral electrovaporization of the prostate using bipolar energy (plasmakinetic vaporization of the prostate [PKVP])
visual laser ablation of the prostate (VLAP)
transurethral ultrasound guided laser incision prostatectomy (TULIP)
contact laser vaporization of the prostate (CLV)
interstitial laser coagulation (ILC)
holmium laser resection of the prostate (HoLRP)
holmium laser enucleation of the prostate (HoLEP)
holmium laser ablation of the prostate (HoLAP)
potassium titanyl phosphate (KTP) laser
transurethral microwave thermotherapy (TUMT)
transurethral needle ablation (TUNA)
Review Strategy
A search of electronic databases (OVID MEDLINE, MEDLINE In-Process & Other Non-Indexed Citations, EMBASE, The Cochrane Library, and the International Agency for Health Technology Assessment [INAHTA] database) was undertaken to identify evidence published from January 1, 2000 to June 21, 2006. The search was limited to English-language articles and human studies. The literature search identified 284 citations, of which 38 randomized controlled trials (RCTs) met the inclusion criteria.
Since the application of high-power (80 W) KTP laser (photoselective vaporization of the prostate [PVP]) has been supported in the United States and has resulted in a rapid diffusion of this technology in the absence of any RCTs, the MAS decided that any comparative studies on PVP should be identified and evaluated. Hence, the literature was searched and one prospective cohort study (3) was identified but evaluated separately.
Findings of Literature Review and Analysis
Meta-analysis of the results of RCTs shows that monopolar electrovaporization is as clinically effective as TURP for the relief of urinary symptoms caused by BPH (based on 5-year follow-up data).
Meta-analysis of the results of RCTs shows that bipolar electrovaporization (PKVP) is clinically as effective as TURP for the relief of urinary symptoms caused by BPH (based on 1-year follow-up data).
Two of the three RCTs on VLAP have shown that patients undergoing VLAP had a significantly lesser improvement in urinary symptom scores compared with patients undergoing TURP.
RCTs showed that the time to catheter removal was significantly longer in patients undergoing VLAP compared with patients undergoing TURP.
Meta-analysis of the rate of reoperation showed that patients undergoing VLAP had a significantly higher rate of reoperation compared with patients undergoing TURP.
Meta-analysis showed that patients undergoing CLV had a significantly lesser improvement in urinary symptom scores compared with TURP at 2 years and at 3 or more years of follow-up.
Two RCTs with 6-month and 2-year follow-up showed similar improvement in symptom scores for ILC and TURP.
Time to catheter removal was significantly longer in patients undergoing ILC compared with patients undergoing TURP.
The results of RCTs on HoLEP with 1-year follow-up showed excellent clinical outcomes with regard to the urinary symptom score and peak urinary flow.
Meta-analysis showed that at 1-year follow-up, patients undergoing HoLEP had a significantly greater improvement in urinary symptom scores and peak flow rate compared with patients undergoing TURP.
Procedural time is significantly longer in HoLEP compared with TURP.
The results of one RCT with 4-year follow-up showed that HoLRP and TURP provided equivalent improvement in urinary symptom scores.
The results of one RCT with 1-year follow-up showed that patients undergoing KTP had a lesser improvement in urinary symptom scores than did patients undergoing TURP. However, the results were not significant at longer-term follow-up periods.
Two RCTs that provided 3-year follow-up data reported that patients undergoing TUMT had a significantly lesser improvement in symptom score compared with patients undergoing TURP.
RCTs reported a longer duration of catheterization for TUMT compared with TURP (P values are not reported).
The results of a large RCT with 5-year follow-up showed a significantly lesser improvement in symptom scores in patients undergoing TUNA compared with patients undergoing TURP.
Meta-analysis of the rate of reoperation showed that patients undergoing TUNA had a significantly higher rate of reoperation compared with patients undergoing TURP.
Based on the results of RCTs, TURP is associated with a 0.5% risk of TUR syndrome, while no cases of TUR syndrome have been reported in patients undergoing monopolar or bipolar electrovaporization, laser-based procedures, TUMT, or TUNA.
Based on the results of RCTs, the rate of blood transfusion ranges from 0% to 8.3% in patients undergoing TURP. The rate is about 1.7% in monopolar electrovaporization, 1.4% in bipolar electrovaporization, and 0.4% in the VLAP procedure. No patients undergoing CLV, ILC, HoLEP, HoLRP, KTP, TUMT, and TUNA required blood transfusion.
The mean length of hospital stay is between 2 and 5 days for patients undergoing TURP, about 3 days for electrovaporization, about 2 to 4 days for Nd:YAG laser procedures, and about 1 to 2 days for holmium laser procedures. TUMT and TUNA can each be performed as a day procedure in an outpatient setting (0.5 and 1 day respectively).
Based on a prospective cohort study, PVP is clinically as effective as TURP for the relief of urinary symptoms caused by BPH (based on 6-month follow-up data). Time to catheter removal was significantly shorter in patients undergoing PVP than in those undergoing TURP. Operating room time was significantly longer in PVP than in TURP. PVP has the potential to reduce health care expenses due to shorter hospital stays.
Economic Analysis
In the three most recent fiscal years (FY) reported, an average of approximately 5,000 TURP procedures per year were performed in Ontario. From FY 2002 to FY 2004, the total number of surgical interventions decreased by approximately 500 procedures. During this time, the increase in costs of drugs to the government was estimated at approximately $10 million (Cdn); however, there was a concurrent decrease in costs due to a decline in the total number of surgical procedures, estimated at approximately $1.9 million (Cdn). From FY 2002 to FY 2004, the increase in costs associated with the increase in utilization of drugs for the treatment of BPH translates into $353 (Cdn) per patient while the cost savings associated with a decrease in the total number of surgical procedures translates into a savings of $3,906 (Cdn) per patient.
The following table summarizes the change in the current budget, depending on various estimates of the total percentage of the 5,000 TURP procedures that might be replaced by other energy-based interventions for the treatment of BPH in the future.
Executive Summary Table 1: Budget Impact With Various Estimates of the Percentage of TURP Procedures Captured by Energy-based Interventions for the Treatment of BPH.
| Technology | Cost per procedure, $ |
Budget Impact of 25% diffusion, $M | Budget Impact of 50% diffusion, $M | Budget Impact of 75% diffusion, $M | Budget Impact of 100% diffusion, $M | Incremental Budget Impact, $M |
|---|---|---|---|---|---|---|
| TURP | 3,887 | 19.4 | ||||
| Bipolar Electrovaporization | 4,011 | 19.6 | 19.7 | 19.9 | 20.0 | 0.6 |
| Monopolar Electrovaporization | 4,130 | 19.7 | 20.0 | 20.3 | 20.6 | 1.2 |
| TUMT | 1,529 | 16.5 | 13.5 | 10.6 | 7.6 | (11.8) |
| TUNA | 4,804 | 20.6 | 21.7 | 22.9 | 24.0 | 4.6 |
| PVP | 1,184 | 16.0 | 12.7 | 9.3 | 5.9 | (13.5) |
| Holmium Laser | 3,892 | 19.4 | 19.4 | 19.4 | 19.4 | 0.02 |
| VLAP Nd:YAG | 4,663 | 20.4 | 21.4 | 22.3 | 23.3 | 3.9 |
| CLAP Nd:YAG | 4,615 | 20.3 | 21.2 | 22.4 | 23.0 | 3.6 |
All costs are in Canadian currency. Parentheses indicative of cost reduction.
Objective
The Ontario Health Technology Advisory Committee asked the Medical Advisory Secretariat (MAS) to conduct a health technology assessment on energy delivery systems for treatment of benign prostatic hyperplasia (BPH).
Background
Clinical Need: Target Population and Condition
BPH is a noncancerous enlargement of the prostate gland and the most common benign tumour in aging men. (1) It is the most common cause of lower urinary tract symptoms (LUTS) and bladder outlet obstruction (BOO) and is an important cause of diminished quality of life among aging men. (2) The primary goal in the management of BPH for most patients is a subjective improvement in urinary symptoms and quality of life.
Until the 1930s, open prostatectomy, though invasive, was the most effective form of surgical treatment for BPH. Today, the benchmark surgical treatment for BPH is transurethral resection of the prostate (TURP), which produces significant changes of all subjective and objective outcome parameters. Complications after TURP include hemorrhage during or after the procedure, which often necessitates blood transfusion; transurethral resection (TUR) syndrome; urinary incontinence; bladder neck stricture; and sexual dysfunction. (4;5) A retrospective review (6) of 4,031 TURP procedures performed by one surgeon between 1979 and 2003 showed that the incidence of complications was 2.4% for blood transfusion, 0.3% for TUR syndrome, 1.5% for hemostatic procedures, 2.8% for bladder neck contracture, and 1% for urinary stricture. However, the incidence of blood transfusion and TUR syndrome decreased as the surgeon’s skills improved.
During the 1990s, endoscopic techniques using a range of energy sources have been developed as alternative treatments for BPH. These techniques include the use of light amplification by stimulated emission of radiation (laser), radiofrequency, microwave, and ultrasound to heat prostate tissue and cause coagulation or vaporization. In addition, new electrosurgical techniques that use higher amounts of energy to cut, coagulate, and vaporize prostatic tissue have entered the market as competitors to TURP. The driving force behind these new treatment modalities is the potential of producing good hemostasis, thereby reducing catheterization time and length of hospital stay. Some have the potential to be used in an office environment, and performed under local anesthesia. Therefore, these new procedures have the potential to rival TURP if their effectiveness is proven over the long term.
Benign Prostatic Hyperplasia (BPH)
The normal prostate reaches 20 g (standard deviation = 6) in men between 21 and 30 years old, and this weight remains essentially constant with increasing age, BPH develops. (7) Symptoms of BPH are caused by irritation or obstruction. Irritation symptoms include frequency, urgency, and nocturia. Obstructive symptoms include a weakened urinary stream, hesitancy, and a need to push to initiate micturition. Urinary symptoms commonly attributed to BPH, however, are nonspecific and may result from a variety of other causes including diabetes mellitus, Parkinson’s disease, and stroke. (8)
The severity of bothersome symptoms and how those symptoms affect the patient’s quality of life are paramount in the decision to treat. Over the years, the management of patients with BPH has changed, resulting in a decline in the number of TURPs performed. (9) Recent thinking is that many patients can be managed by alternative means of therapy. Also, many patients with LUTS who do not have prostate enlargement do not require prostate debulking.
Incidence and Prevalence
BPH is one of the most common conditions for which male patients seek treatment. (8) Prevalence of BPH differs considerably between countries. These differences may be due to different cultural perceptions and comprehension of the questions designed to identify and measure LUTS, and poor perception of health status. (10) Differences in prevalence can also be explained by variations in definitions and criteria that investigators use for the evaluation of BPH and LUTS.
International studies have shown an increasing prevalence with increasing age, to the point that autopsy data indicate anatomical or microscopic evidence of BPH in almost all elderly men. (7) Autopsy studies (1,075 human autopsies) have shown that the prevalence of BPH is about 8% in men 30 to 39 years, 40% to 50% in men 50 to 59 years, and more than 80% in men over 80 years. (7)
Norman et al. (11) conducted a telephone survey in a sample of 508 Canadian men, which showed that overall, 23% of the men 50 years of age or older experienced moderate to severe symptoms associated with BPH. Another questionnaire-based survey evaluated the frequency and severity of LUTS and the prevalence of enlarged prostate in more than 1,000 American men aged more than 50 years of age. One-quarter of men suffered moderate to severe LUTS, and 55% of those consulting a doctor had an enlarged prostate. (12) Almost 20% of men with an enlarged prostate had undergone surgery, including energy-based interventions. The rate of surgery was similar among men with mild versus moderate to severe symptoms and increased with increasing age (see Figure 1).
Figure 1: Proportion of Men Who Have Had Surgery for BPH, by Age Group.
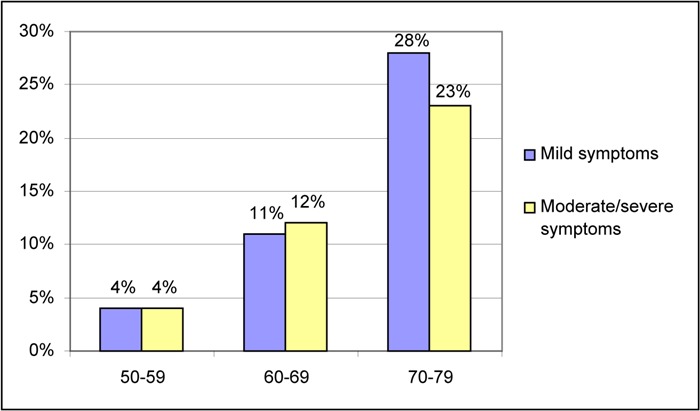
Source: Roehrborn CG, Marks L, Harkaway R. Enlarged prostate: a landmark national survey of its prevalence and impact on US men and their partners. Prostate Cancer & Prostatic Diseases 2006;9(1):30–34.
A study from Austria used a validated German translation of the International Prostatic Symptom Score (IPSS) in addition to a detailed urological history and a physical evaluation including a digital rectal examination. Based on a community sample of 2,096 Austrian men aged 20 years or older who participated in this study, the authors found that 26.9% of the men aged 50 years or older had moderate LUTS and a further 2.8% had severe LUTS (using a definition of BPH as IPSS > 7, maximum urinary flow rate [Qmax] < 15 mL/s, and prostate size > 30 g). The prevalence of moderate/severe LUTS was found to be 6.3% in men aged 20 to 29 years, 8.4% in men aged 30 to 39 years, 11.1% in men aged 40 to 49 years, 27.1% in men aged 50 to 59 years, 28.3% in men aged 60 to 69 years, 36.0% in men aged 70 to 79 years, and 35.7% in men aged 80 years or older.
Data from the General Practice Research Database (GPRD) in the United Kingdom (13) illustrate the age-specific incidence and prevalence of reported LUTS from 1992 to 2001. The prevalence of LUTS increased from 3.5% for patients 45 to 49 years old, to 15% at age 60 to 69, and to more than 30% for patients older than 85 years (see Figure 2).
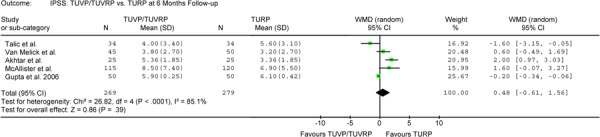
Figure 2-A: TUVP/TUVRP Versus TURP at 6-Month Follow-up Assessment – Outcome: IPSS.
A large Swedish study (14) estimated the age-specific prevalence and severity of LUTS among men 45 to 79 years living in 2 counties in Sweden. Overall, 18.5% of the men had moderate symptoms, and 4.8% had severe symptoms. Table 1 shows the frequency distribution of the level of severity of LUTS according to age.
Table 1: Frequency Distribution of the Severity of Lower Urinary Tract Symptoms in Sweden (Men Aged 45–70 Years in 1997).
| Age Group | None (Score 0) |
Mild (Score 1–7) |
Moderate (Score 8–19) |
Severe (Score 20–35) |
Age Group % |
|---|---|---|---|---|---|
| 45–49 | 28.3 | 60.0 | 10.0 | 1.8 | 16.8 |
| 50–54 | 22.0 | 62.3 | 13.1 | 2.5 | 20.0 |
| 55–59 | 18.1 | 61.6 | 16.5 | 3.7 | 16.5 |
| 60–64 | 13.2 | 62.1 | 19.8 | 4.8 | 13.3 |
| 65–69 | 12.1 | 57.7 | 23.4 | 6.7 | 13.6 |
| 70–74 | 8.9 | 55.5 | 27.1 | 8.6 | 11.5 |
| 75–79 | 7.5 | 51.9 | 30.9 | 9.7 | 8.2 |
| Total, % | 17.2 | 59.5 | 18.5 | 4.8 | 100.0 |
Source: Andersson SO, Rashidkhani B, Karlberg L, Wolk A, Johansson JE. Prevalence of lower urinary tract symptoms in men aged 45–79 years: a population-based study of 40 000 Swedish men. BJU International 2004;94(3):327–331.
Diagnosis of BPH
About 50% of patients with BPH will seek medical attention for LUTS. (2) Establishing a clinical diagnosis of BPH requires the patient’s medical history and performing a physical examination, as not all LUTS are caused by BPH and not all men with BPH have LUTS. (15) Physical examination includes a digital rectal examination to determine the size and texture of the prostate and a focused neurological exam to assess the lower extremity for peripheral neuropathy or saddle anesthesia. Patients with these conditions are more likely to have a neurologic disorder affecting the bladder than BPH. (15)
A urinalysis should be performed for evidence of hematuria or urinary infection. Prostate specific antigen (PSA) measurement as a screening test for prostate cancer should be performed in selected patients. According to Canadian Urological Association (CUA) guidelines for the management of BPH, (16) PSA testing should be offered to patients who have at least a 10-year life expectancy and for whom the knowledge of the presence of prostate cancer would change management of the disease, as well as to those for whom PSA measurement would change the management of their voiding symptoms.
Due to variation across individuals, symptoms alone do not define the extent of prostate disease; therefore, determining the degree of the problem is important and should be done before treatment. A variety of tests are available that evaluate patient complaints. Tests previously used to evaluate the patient prior to treatment, such as upper urinary tract imaging studies, diagnostic cystoscopy, or renal ultrasonography, are less valuable and less reliable than the newly established tests or scales showing the impact of symptoms on the patient’s quality of life.
The CUA guidelines (16) have described mandatory, recommended, optional, and not recommended tests for BPH (see Table 2).
Table 2: Canadian Urological Association Guidelines for the Diagnosis of BPH.
| Mandatory | |
| History | |
| Physical examination including digital rectal examination | |
| Urinalysis | |
| Recommended | |
| Formal symptom inventory | |
| PSA | |
| Optional | |
| Creatinine | |
| Voiding diary | |
| Uroflow | |
| Postvoid residual | |
| Sexual function questionnaire | |
| Not recommended | |
| Cystoscopy | |
| Cytology | |
| Urodynamics | |
| Radiological evaluation of upper urinary tract | |
| Prostate ultrasound | |
| Prostate biopsy | |
Source: Nickel JC, Herschorn S, Corcos J, Donnelly B, Drover D, Elhilali M, et al. Canadian guidelines for the management of benign prostatic hyperplasia. Can J Uroy 2005;12(3):2677–2683.
International Prostatic Symptom Score
The IPSS is the current recommendation from the World Health Organization (WHO). (17) This scale is based on the American Urological Association (AUA) symptom score and quantifies urinary problems in terms of the frequency and severity of the symptoms, thus allowing measurement of symptomatic improvement.
The questions in the AUA symptom score address seven separate but related urinary symptoms associated with BPH. This seven-item questionnaire elicits the symptoms of nocturia, frequency, weak urinary stream, hesitancy, intermittency, incomplete emptying, and urgency. (18) Responses are scored from 0 to 5 based on the frequency of occurrence of each symptom, and added to give a total score from 0 to 35. (19) Based on this, patients can be categorized as having either mild (0–7 points), moderate (8–19 points), or severe (20–35 points) symptoms. That is simply, the higher the AUA score, the more severe the condition (see Appendix 2).
The AUA symptom score has been extensively validated and found to have good construct and criterion validity. (18;19) The instrument has high test-retest reliability (r = .92) and internal consistency (Cronbach’s alpha = .86). (19)
In addition, an impact question, designed to assess the overall quality of life, has been added to the AUA symptom score. The quality-of-life question with the initial seven questions from the AUA questionnaire comprise the IPSS. (8;15) The IPSS questionnaire has been translated into many languages (20) and has been used worldwide as a benchmark to measure the incidence and prevalence of BPH in many countries, and to determine the response to surgical and medical therapy.
Uroflowmetry
Urinary flow rate (uroflowmetry) can be analyzed in a urologist’s office (15) as the test is simple to perform and is noninvasive. Uroflowmetry is considered as an optional test in the work-up of patients with BPH, considering the fact that elderly patients with LUTS may have age-related urodynamic changes. (21) Although obstruction can be diagnosed with uroflowmetry, flow rates should be interpreted with caution because slow urinary flow may be equally due to detrusor failure.
The most clinically useful measurement is the Qmax, which is measured in millilitres per second. Other information that can be obtained includes the average flow rate, the flow pattern, the flow curve, the flow shape, the flow time, and the time to maximum flow. In general, a Qmax of less than 10 mL/s is considered abnormal, a Qmax of 10 to 15 mL/s is equivocal, and a Qmax of greater than 15 mL/s is considered normal.
Postvoid Residual Volume
Measurement of postvoid residual volume (PVR) by ultrasonography is part of the standard assessment of BOO and is helpful in the assessment of the patients desiring surgical intervention for bothersome BPH symptoms. The test is simple, accurate, and noninvasive. As with uroflowmetry, PVR is an optional test in work-up of patients with BPH.
Pressure-Flow Urodynamic Measurement
In any patient with LUTS, it should be determined whether or not there is a BOO. The pressure-flow urodynamic study is considered the gold standard for the diagnosis of BOO. (22) The test requires catheterization and is considered optional in the work-up of men before surgical therapy. (15) There is, however, controversy with regard to the importance of routinely obtaining pressure-flow urodynamic measurement to prove obstruction. Some authors believe it is vital, while others (23) consider the test optional and point to its invasive nature, cost, and questionable ability to predict outcomes. Thus, some believe that the test should be utilized only in patients suspected of having neurological disease or other comorbidities.
The procedure itself involves inserting a small catheter into the bladder to measure internal bladder pressure and to determine how effectively the bladder contracts. The test takes about 30 to 60 minutes to complete is particularly helpful in patients with concomitant neurological disease affecting bladder function. (15)
Surgical Treatment of BPH
Surgery is recommended for patients with bothersome BPH symptoms refractory to medical treatment. Recurrent urinary tract infection, refractory urinary retention, recurrent hematuria, renal insufficiency, and bladder stones are complications of BPH that require surgery. (24) The three surgical treatment options for BPH are open prostatectomy, TURP, and transurethral incision of the prostate (TUIP).
Open Prostatectomy
In open prostatectomy, the enlarged prostate is surgically removed to relieve the obstruction. The procedure can be performed via a perineal, retropubic, or suprapubic approach. Open prostatectomy is recommended for cases of severe prostate enlargement.
Transurethral Resection of the Prostate
TURP is the most effective treatment of BPH in patients who have clinical symptoms caused by BOO and it is regarded as the gold standard method. TURP is recommended for moderately enlarged prostate glands. The technique was first described by Nesbitt in 1943 and has remained essentially unchanged since that time, (17) however, the resection technique may differ according to prostate size and from centre to centre. (17) TURP is generally performed in the dorsal lithotomy position and the prostate is accessed through the urethral meatus. The procedure requires general or spinal anesthesia and the choice of anesthesia should be tailored to the patient’s need at the anesthetist’s direction. A cystoscopy is generally performed in the operating room prior to TURP so that diseases of the bladder, urethra, and the prostate can be detected. In case of urethral stricture, to allow easy passage of the resectoscope, the urethra can first be gently dilated with a urethral sound (a flexible probe). If a urethral stricture is noticed prior to TURP, it might be suspected as the cause of LUTS and the surgeon may consider the possibility of cancelling the procedure to assess the patient’s response to urethrotomy. (8) If bladder calculi are diagnosed through cystoscopy, removal of the calculi should precede TURP.
Instruments
The essential requirements for TURP are a resectoscope, a cautery loop, and a generator. A resectoscope is a device that accommodates all elements required for TURP. Each of its segments can be altered to fit the needs and the preferences of the surgeon. (8) Components of a resectoscope are the bridge (which contains the loop for resection and/or cauterization), the cystoscopy lens, the cystoscopy sheet, and the inner and outer portion of a flow sheet for continuous irrigation. The outer portion of the continuous flow sheet is connected to suction for aspiration of the irrigation fluid.
Procedure
Essentially, the TURP procedure is a slice by slice resection of prostatic tissue. Usually resection starts ventrolaterally at the 11 o’clock position to secure the main arteries. Deep resection and undermining of the bladder neck should be avoided as resection beyond the verumontanum increases the risk of injury to the sphincter. After completion of the resection, all prostatic chips should be evacuated to prevent urethral occlusion, the bleeding sites should be cauterized, and a three-way urethral catheter should be inserted. If necessary, the three-way catheter is connected to continuous irrigation. In order to prevent the entrance of prostatic fossa blood into the bladder, a gentle traction on the catheter may be applied by attaching it to the patient’s leg with tape. The patient is then transported to the postanesthesia recovery unit, and continuous bladder irrigation may be performed until the effluent is clear.
During TURP, when the prostate tissue is incised, bleeding obscures visualization; irrigation is, therefore, required. This may lead to the development of TUR syndrome, which is a potentially fatal complication of TURP. (5) TUR syndrome occurs when opening of the venous sinuses results in the passage of irrigation fluid into systemic circulation, and in a decrease in sodium concentration (dilutional hyponatremia). TUR syndrome may result in pulmonary oedema, convulsions, and occasionally, cardiac arrest when the plasma sodium falls below 100 mmol/L. (25) Cerebral edema and neurological symptoms, restlessness, and epileptic seizures are signs of massive absorption of irrigants. (26)
Sterile water was initially used for irrigation but resulted in complications such as hyponatremia and hemolysis. The use of isotonic solution to increase osmolarity has been effective in reducing the incidence of hemolysis and is currently the standard of care. Iso-osmotic solutions such as 1.5% glycine, sorbitol, or mannitol are nonhemolytic fluids, and their osmolarity is close to the serum osmolarity. (26) Glycine is most commonly used in the United Kingdom and North America. (26) Although the likelihood of TUR syndrome is very low because of the use of iso-osmotic solutions, dilutional hyponatremia may result if they are absorbed in high volumes. (8)
Morbidity and Mortality
A retrospective review of 3,885 cases of TURP (5) showed a mortality rate of 0.2% and an immediate postoperative morbidity rate of 18%. Increased morbidity was found in patients with a resection time of more than 90 minutes, patients with a gland size of more than 45 grams, patients aged greater than 80 years, and patients with acute urinary retention, which was more common in the black population.
Transurethral Incision of the Prostate (TUIP)
TUIP was introduced by Orandi et al. (27) in 1973 as an alternative to TURP. This method does not lead to the removal of the hypertrophied tissue; rather, a cut is made in the bladder neck or along the length of the prostate to relieve the pressure on the urethra. TUIP is suitable for patients with a small prostate and is performed with the use of a cystoscope. The procedure has less risk of complications than TURP and does not require an overnight hospital stay. The procedure may need to be repeated, as it is not as effective as other methods in relieving urinary symptoms.
New Technology Being Reviewed
Over the last decade, a number of energy-based techniques have been developed as alternatives to TURP. The potential advantages of these techniques compared with TURP are less morbidity and a shorter hospital stay. The disadvantage, however, is that most of these techniques do not permit tissue recovery for histological examination. This includes electrovaporization techniques, laser techniques (excluding the holmium laser), TUMT, TUNA, and HIFU.
The type of current and mechanism of action for all these techniques differ. Obstructing prostatic tissue can be removed using either coagulation or vaporization, or a combination of both. With coagulation, removal of abundant tissue can be obtained by heating to a maximum of 100°C, causing the coagulated tissue to slough. With vaporization, application of the energy to the prostate results in rapid rise in tissue temperature, causing a boiling of intracellular water leading to cellular disruption and destruction. Most of the energy delivered to the gland results in instantaneous vaporization and a zone of coagulation is created beneath the vaporized tissue with improved hemostasis. (28) Is important to recognize, however, that coagulation increases electrical resistance and consequently prevents further vaporization. (17)
Vaporization of the prostate can be achieved using either electrosurgery or laser surgery. During a laser procedure, the extent of coagulation and vaporization can be controlled by adjusting the power setting, the wavelength, the irradiation time, the exit angle, and the beam profile of the laser. (29) Power density depends on the power output of the laser source, the transmission of the fibre, the irradiated surface area, and the characteristics of the side-firing fibre and its distance to the tissue.
Transurethral Electrovaporization of the Prostate Using Monopolar Energy
Transurethral electrovaporization of the prostate using monopolar energy entered mainstream urology in 1995. Transurethral electrovaporization techniques include the following:
Transurethral electrovaporization of the prostate (TUVP)
Transurethral electrovapor resection of the prostate (TUVRP)
TUVRP specifically refers to the use of a thick loop electrode by which tissue removal can be performed more quickly than by TUVP. (28)
Electrovaporization is a modification of TURP and entails the simultaneous vaporization, desiccation, and coagulation of prostatic tissue, using a rollerball electrode. This simultaneous action involves a thin leading edge that vaporizes the tissue in its path and a trailing edge that coagulates and seals the vessels in tissues that have been freshly vaporized. In electrovaporization, the tissue cells are heated rapidly and turn into steam, leaving a void where the cells were. Most of the heat is dissipated as steam and not conducted into adjacent tissues. (30)
Electrovaporization uses a radiofrequency electric current to cut and fulgurate prostatic tissue for hemostasis. The frequency selected is important to achieve the desired effects without adverse effect. A low frequency (~100,000 Hz) will stimulate muscles and nerves and may electrocute the patient. A high frequency (~4,000,000 Hz) produces a reactive phenomenon because it is difficult to confine these high radiofrequencies to wires. Electrosurgical tools thus typically operate between 400,000 and 1,000,000 Hz depending on the manufacturer. (30)
TUVP requires the use of a more powerful generator to deliver a high-voltage current, an electrode with a grooved or rollerball design, and a slower loop resection speed. (8) Generator specification is an important factor for successful vaporization as some older generators have been shown to be less efficient. (30). In electrosurgery, heat is created from the electrical resistance of the tissue to current flow. The rate of energy delivery (W) is given by the equation W = I2R, where I is the current flow through the tissue and R is the tissue resistance. (28) The electrical current delivered by the generator changes continuously to accommodate the constantly changing tissue resistance. (31) Tissue resistance can rapidly increase as it dries out. This means that to achieve the same power, the generator must deliver an increasing level of current to compensate for the increase in the tissue resistance. (31) The older generators did not have this capability and most of the generators available prior to 1995 had other design limitations and constraints that limited the amount power being delivered to the surgical site. (31)
An advantage of electrovaporization is that it is simple and requires no special skills other than those of performing conventional TURP. The disadvantage of the technique is that it does not provide tissue for histological examination. To obtain a sample during the procedure, the electrode must be replaced by a standard loop electrode.
Transurethral Electrovaporization of the Prostate using Bipolar Energy
In bipolar electrosurgery, two mutually isolated electrodes (active and return) are used to form a complete circuit with the tissue lying between them. The prime electrical conduction path is formed by a saline irrigant and radiofrequency is used to convert the conductive medium into a plasma field, which vaporizes tissue upon contact. (32) The advantage of the technique is that the current flows only through the volume of tissue between the poles of each electrode and hence its effect is both safe and precise. Unlike monopolar electrosurgery, with bipolar electrosurgery, the current does not flow through any other part of the body. (31) The instrumentation operates at 160 Ω in a radiofrequency range of 320 to 450 Hz and a voltage range of 254 to 350 V. (33)
Plasma kinetic vaporization of the prostate is carried out using The PlasmaKinetic Tissue Management System (Gyrus Medical Ltd., Buckinghamshire, United Kingdom), which consists of the PlasmaKinetic generator, the PlasmaKinetic resectoscope, and the Plasma-V™ vaporization device. The theoretical advantages of the Plasma Kinetic surgery over conventional TURP are reduced bleeding, reduced TUR syndrome, and reduced risk of nerve injury. (31)
Laser Techniques
Laser treatment of BPH encompasses a variety of techniques using different laser wavelengths and surgical techniques. The term “laser prostatectomy” encompasses two distinct techniques: contact and noncontact laser treatment. Noncontact laser treatment relies on thermal coagulation and delayed sloughing of the tissue (coagulative necrosis). (34) The method, therefore, requires postoperative catheterization for a few weeks. In contrast, with contact laser treatment the laser probe directly touches the prostatic tissue to immediately vaporize obstructing tissue (in a similar fashion to the TURP procedure), resulting in a rapid improvement in urinary flow. (34) Laser techniques include:
Noncontact Laser Techniques
Visual laser ablation of the prostate (VLAP)
Transurethral ultrasound guided laser incision prostatectomy (TULIP)
Contact Laser Techniques
Contact laser vaporization of the prostate (CLV)
Interstitial laser coagulation (ILC)
Visual Laser Ablation of the Prostate (VLAP)
In VLAP, a free-beam laser that is deflected at a right angle to the axis of the fibre is used to produce deep coagulation of the prostatic tissue. This technique coagulates the tissue predominantly with a minimum of vaporization and debulking. (35) After VLAP, the tissues undergo coagulation necrosis and gradually slough off in the urinary system.
The neodymium: yttrium-aluminum-garnet (Nd:YAG) laser, with its deep tissue penetration property, has most often been used for VLAP. (36) Energy from the Nd:YAG laser is absorbed by cellular proteins and penetrates up to 7 mm into tissue. Because the laser energy affects such a large volume of tissue, heating occurs relatively slowly, and the result is coagulation and desiccation of both the irradiated and the surrounding tissues. The potassium-titanyl-phosphate (KTP) laser has also been used in a few small case series. In VLAP, the side-firing delivery fibre is held close to the prostatic tissue without contact and the laser energy is applied continuously for 60 to 90 seconds.
Transurethral Ultrasound Guided Laser Incision Prostatectomy (TULIP)
In this technique, a laser probe is placed in the urethra and ultrasonography is used to guide the Nd:YAG laser to selected sites within the prostate.
Contact Laser Vaporization of the Prostate (CLV)
In CLV, the laser tip is in contact with the prostatic tissue and free-beam energy is delivered at a high power density output to cause prostatic tissue vaporization. The Nd:YAG laser is applied to cut and instantly remove the obstructing tissue in a manner similar to TURP. (4)
Interstitial Laser Coagulation (ILC)
The Indigo Laser System (Ethicon Endo-Surgery, Cincinnati, Ohio) consists of a laser generator, a quartz fibre, and an eye protector specific to laser-wavelength light. The techniques is ultrasound guided and the generator operates on standard voltage without any special electrical consideration. (8) A 1 cm diffuser tip radiates heat in all directions, resulting in an olive-shaped area of coagulation necrosis of about 2×2.5 cm, or a volume of approximately 4 cm3. (37)
Laser Techniques using Holmium:YAG Laser
Holmium:YAG (Ho:YAG) laser techniques include the following:
holmium laser resection of the prostate (HoLRP),
holmium laser enucleation of the prostate (HoLEP), and
holmium laser ablation of the prostate (HoLAP).
The high-powered holmium:YAG (Ho:YAG) laser became commercially available in 1994. (38) It’s a pulsed laser (wavelength 2,140 nm) that can be used for incision, ablation, resection, and more recently, enucleation of the prostatic tissues. (39) It has a shallow penetration depth, excellent hemostatic properties, and the ability to be used with normal saline irrigation. (40)
The Ho:YAG laser is also highly absorbed by water and has the unique ability to cut, vaporize, and coagulate tissue types regardless of composition or color. (30) The property of absorption in water increases the margin of safety as tissues not in contact with the laser fibre will not be harmed.
Holmium Laser Resection of the Prostate (HoLRP)
The technique of HoLRP differs from TURP in that with HoLRP, the adenoma is dissected off the surgical capsule in a retrograde direction. (41) Originally pioneered by Gilling et al. (42) in 1996, the technique has been superseded by HoLEP. (41) The potential drawback of HoLRP is that it has a steep learning curve requiring significant skill. The operative time is also usually longer than that for TURP because of the time taken to cut the lobes into pieces small enough for extraction via the urethra.
Holmium Laser Enucleation of the Prostate (HoLEP)
HoLEP is the most recent development in the evolution of holmium laser prostatectomy. (40) The technique involves enucleation of the whole prostate through holmium laser fibre, acting much as the surgeon’s index finger during open prostatectomy in shelling out the adenoma. (40) The high power (60–100 W) holmium:YAG (Ho:YAG) laser is a potent incision tool that has the ability to cut large amounts of prostatic tissue. Enucleated tissue can then be removed from the bladder using a transurethral tissue morcellator. (40) The development of mechanical tissue morcellators has resulted in the application of HoLEP to larger prostate glands. (43)
The learning curve associated with this procedure and a lack of structured training programs have interfered with widespread acceptance of this technology. (44) A novice has to undertake 10 to 30 cases in a properly structured training environment in order to achieve outcomes similar to those published in the literature.
Holmium Laser Ablation of the Prostate (HoLAP)
HoLAP involves using holmium laser to vaporize obstructive prostatic tissue. Patients who undergo HoLAP usually do not require overnight hospitalization and in most cases, the catheter can be removed within 12-24 hours of the procedure.
Potassium Titanyl Phosphate (KTP) Laser
Potassium Titanyl Phosphate (KTP) laser is a variation of Nd:YAG, produced by doubling the frequency and halving the wavelength of the laser from 1,064 nm to 532 nm. (45) This wavelength is visible to the human eye (green band of the electromagnetic spectrum). Malek et al. (46) developed the technique and have reported on a series of 55 patients with significant improvement in flow rates and symptom scores over 2 years. (46)
The 532 nm wavelength KTP laser and the 1,064 nm Nd:YAG laser produce considerably different tissue effects. Unlike the 7 mm penetration of ND:YAG laser energy, which results in more widespread coagulation of tissue, KTP laser energy is strongly absorbed by hemoglobin and penetrates only 1 to 2 mm of tissue. Heat is thus concentrated into a small volume and prostatic tissue is ablated by rapid vaporization of cellular water, leaving only a 2 mm rim of coagulated tissue. (47)
The efficiency of KTP laser in vaporizing tissue is due to selective absorption of photons by hemoglobin and the consequent release of superficially trapped vaporizing thermal energy. The procedure is, therefore, often referred to as photoselective vaporization of the prostate (PVP). (48)
The early generation of KTP (20 W) has now been replaced by the high-powered 80 W unit (GreenLight®, San Jose, California). This laser was developed with the aim of providing more rapid and effective photothermolytic vaporization of prostatic tissue.
The PVP procedure can be performed with regional or general anesthesia and is particularly suited to high risk patients, such as those with severe cardiac or pulmonary comorbidities. One of the proposed benefits of PVP is the ability to successfully discharge patients on the day of surgery without a catheter. (44)
Transurethral Microwave Thermotherapy (TUMT)
In TUMT, coagulation necrosis of the prostatic tissue is achieved using thermotherapy devices that transfer energy into the tissue in the form of heat. In this procedure, a catheter is placed transurethrally into the prostatic fossa and a microwave antenna is used to heat the prostatic tissue to a minimum 45°C. The procedure can be done without anesthesia in the office as an outpatient procedure and postoperative catheterization time remains in the range of 2 weeks. (49) TUMT does not lead to immediate improvement and it usually takes up to 4 weeks for urinary symptoms to completely resolve.
Transurethral Needle Ablation (TUNA)
Transurethral needle ablation (TUNA) uses radiofrequency waves (940 KHz) to heat prostatic tissue. In TUNA, two small needles are placed inside the prostate lobes by piercing the urethra under endoscopic control. Application of the radiofrequency energy between the electrodes causes a significant temperature rise (about 100°C) leading to coagulative necrosis of prostatic tissue. Both needles have insulating sheets to protect the urethral mucosa from heating. The needles are subsequently placed in different areas of the prostate at 1 cm intervals. (49) Tissue necrosis from ablation occurs at the time of the procedure; however, because the urethral mucosa is preserved, there is little tissue sloughing and tissue absorption occurs over a two month period following the procedure. (50) Patients often note little improvement in voiding symptoms for the first 2 to 3 weeks, that is, until necrotic tissue absorption begins.
High-intensity Focused Ultrasound (HIFU)
High intensity focused ultrasound (HIFU) was introduced in 1992 as a minimally invasive treatment option for patients with BPH. (51) It produces selective and trackless tissue destruction in deep-seated targets in the body, without damage to overlying tissues. (24) It is the only technique permitting contact-and irradiation-free, in-depth tissue ablation. (51) Due to very high energy, HIFU can precisely reach a target with a very short emission time. An ultrasound beam is brought to a tight focus at a distance from its source and, if sufficient energy is concentrated within the focus, the cells lying within this focal volume are killed, sparing the surrounding cells.
HIFU has a demonstrated potential in the treatment of prostate cancer and several studies have shown its efficacy. (52) The application of HIFU to the prostate has been described by transrectal and transabdominal approaches. In general, the procedure is well tolerated but requires general anesthesia or heavy intravenous sedation. (24)
Regulatory Status
The equipment and instruments for electrovaporization (monopolar and bipolar energy), Nd:YAG laser, Ho:YAG laser, KTP laser, TUMT, TUNA, and HIFU have been issued licenses by Health Canada.
Evidence-Based Analysis of Safety and Effectiveness
Objective
To assess the therapeutic effectiveness and safety of energy-based surgical interventions compared with TURP in treating patients with symptomatic BPH.
Research Question
How do outcomes of treatment with energy delivery systems compare with those obtained with the gold standard (TURP) in the treatment of patients with BPH?
Methods
Search Strategy
A search of electronic databases (OVID MEDLINE, MEDLINE In-Process & Other Non-Indexed Citations, EMBASE, The Cochrane Library, and the International Agency for Health Technology Assessment [INAHTA] database was undertaken to identify evidence published from January 1, 2000, to June 21, 2006. The search was limited to English-language articles and human studies. The search strategy is detailed in Appendix 1.
The literature search identified 284 citations, of which 38 RCTs met inclusion criteria (see Table 3). Randomized controlled trials meeting the inclusion criteria were selected from the search results. Data on the study characteristics, patient characteristics, primary and secondary treatment outcomes, and adverse events were abstracted.
Table 3: Quality of Evidence of Included Studies.
| Study Design | Level of Evidence† |
Number of Eligible Studies |
|---|---|---|
| Large RCT, systematic review of RCTs | 1 | 36 |
| Large RCT unpublished but reported to an international scientific meeting | 1(g) | |
| Small RCT | 2 | 2 |
| Small RCT unpublished but reported to an international scientific meeting | 2(g) | |
| Non-RCT with contemporaneous controls | 3a | |
| Non-RCT with historical controls | 3b | |
| Non-RCT presented at international conference | 3(g) | |
| Surveillance (database or register) | 4a | |
| Case series (multisite) | 4b | |
| Case series (single site) | 4c | |
| Retrospective review, modelling | 4d | |
| Case series presented at international conference | 4(g) | |
| Total | 38 |
RCT refers to randomized controlled trial.
g indicates grey literature.
Since the application of high-power (80 W) KTP laser PVP has been supported in the United States and resulted in a rapid diffusion of this technology in the absence of any RCTs. The MAS, therefore, decided that any comparative studies on PVP should be identified and evaluated. The literature was searched and a single prospective cohort study (3) was identified and evaluated separately.
Primary Outcomes
Improvement in urinary tract symptoms based on changes in:
IPSS/AUA Symptom score
Qmax
Secondary Outcomes
rate of TUR syndrome
rate of transfusion
rate of reoperation
rate of urinary stricture
rate of sexual dysfunction
operation/procedure time
duration of catheterization
length of hospital stay
Inclusion Criteria
randomized controlled trials (RCTs) comparing energy-based surgical interventions with the gold standard (TURP)
Exclusion Criteria
nonrandomized controlled trials
studies with less than 3 months’ follow-up
studies that do not report patient outcomes
studies comparing different techniques without a TURP arm
studies comparing a combination of electrosurgical techniques with TURP
studies comparing a combination of 2 Nd:YAG procedures with TURP
Statistical Methods
The data was analyzed on the primary outcomes using Review Manager (RevMan 4.2) software. Weighted mean difference (WMD) and 95% confidence interval (CI) between the treatments at different follow-up periods were calculated. Weighted relative risk and 95% CI were calculated for categorical events where the data permitted. A random-effects model was used to allow for heterogeneity between studies.
Grading the Body of Evidence
To grade the strength of the body of evidence, the grading system formulated by the GRADE working group (53) and adopted by the MAS was applied. The GRADE system classifies quality of evidence as high (Grade A), moderate (Grade B), or low (Grade C) according to 4 key elements: study design, study quality, consistency across studies, and directness (see Appendix 3).
Results of Literature Review
The combined search strategies identified 38 trials, of which 3 were 3-arm studies. (54-56) A total of 4,043 patients were randomized to the new technologies and 1,964 to the gold standard, TURP.
Table 5 lists the equipment and instruments used in the RCTs listed in Table 4.
Table 5: Equipment and Instruments Used in the Randomized Controlled Trials of Surgical Treatment of BPH.
| Method | Generator | Electrode | Resectoscope |
|---|---|---|---|
| TURP |
|
|
|
| TUVP |
|
|
|
| TUVRP |
|
|
|
| PKVP | PKVP system consists of a PK generator, a PK resectoscope, and a PlasmaSect electrode
|
|
|
| CLV |
|
|
|
| VLAP |
|
||
| ILC |
|
||
| HoLEP |
|
|
|
| HoLRP | NR | Storz continuous flow resectoscope (26 F) incorporating a fibre guide in the inner sheath | |
| PVP |
|
|
|
| TUMT |
|
||
| TUNA | Vidamed® Inc. | ||
| HIFU | NR |
Table 4: Studies Included in the Assessment of Energy Delivery Systems for Treatment of BPH.
| Procedure | Randomized Controlled Trial | |
|---|---|---|
| Transurethral vaporization of the prostate (TUVP) | Nuhoglu et al. 2005 Akhtar et al. 2004 McAllister et al. 2003 van Malick et al. 2003 (same as van Malick et al. 2003 & van Malick et al. 2002) (3-arm study; TUVP vs. TURP vs. CLV) Hammadeh et al. 2003 & 2000 |
|
| Electrovaporization Monopolar Energy | Transurethral vapor resection of the prostate (TUVRP) | Liu 2006 et al. 2006 Gupta et al. 2006 (3-arm study; TUVRP vs. HoLEP vs. TURP) Gupta et al. 2002 Helke et al. 2001 Kupeli et al. 2001 Talic et al. 2000 (same as Talic et al. 1998) Ekengren et al. 2000 |
| Electrovaporization Bipolar energy: Plasmakinetic vaporization of the prostate (PKVP) |
Hon et al. 2006 De Sio et al. 2006 Nuhoglu et al. 2006 Seckiner et al. 2006 Tefekli et al. 2005 Fung et al. 2005 Dunsmuir et al. 2003 |
|
| Transurethral Ultrasound-Guided Laser Incision of the Prostate (TULIP) | No RCT was found | |
| Visual Laser Ablation (VLAP) | Chacko et al. 2001 Donovan et al. 2000 Gujral et al. 2000 |
|
| Contact Laser Vaporization (CLV) | Tuhkanan et al. 2003 Van Malick et al. 2003 (3-arm study; TUVP vs. TURP vs. CLV) Keoghane et al. 2000 (same as Keoghane et al. 2002) |
|
| Interstitial Laser Coagulation (ILC) | Kursh et al. 2003 Idelberg et al. 2003 Norby et al. et al. 2002 (3-arm study; TUMT vs. ILC vs. TURP) |
|
| Holmium Laser Resection of the Prostate (HoLRP) | Westenberg et al. 2004 (Same as Fraundorfer et al. 2001 & Gilling et al. 2000) | |
| Holmium Laser Enucleation of the Prostate (HoLEP) | Rigatti et al. 2006 Gupta et al. 2006 (3-arm study; TUVRP vs. HoLEP vs. TURP) Kuntz et al. 2004 (same as Kuntz et al. 2002) Montorsi et al. 2004 Tan et al. 2003 |
|
| HoLEP vs. Open Prostatectomy | Kuntz et al. 2004 | |
| Holmium laser ablation of the prostate (HoLAP) | No RCT was found | |
| Potassium Titanyl Phosphate (KTP) | Shingleton et al. 2002 (same as Shingleton et al. 1999) | |
| Photoselective vaporization of the prostate (PVP) | No RCT was found | |
| Microwave Thermotherapy (TUMT) | Wagrell et al. 2004 (same as Wagrell et al. 2002) Norby et al. 2002 (3-arm study; TUMT vs. ILC vs. TURP) Floratos et al. 2001 Francisca et al. 2000 |
|
| Transurethral Needle Ablation (TUNA) | Hill et al. 2004 Cimentepe et al. 2003 |
|
| High Intensity Focused Ultrasound (HIFU) | No RCT was found | |
Summary of the MAS Review
Electrovaporization Studies
Monopolar Electrovaporization
Twelve RCTs comparing electrovaporization using monopolar energy with TURP were analyzed (mean sample size of 104; range 50–235). Overall, 622 and 623 patients were randomized to electrovaporization and TURP respectively. The mean duration of follow-up in the trials ranged from 6 months to 5 years.
Nine of the 12 studies reported that there was no significant difference between monopolar electrovaporization and TURP at any follow-up period in terms of symptom scores and peak urinary flow. Two studies (57;58) reported superior results for electrovaporization for 3-year and 6-month follow-up. Only one study with 6-month follow-up (59) reported superior results for TURP. According to the authors, however, this was partly due to a lack of experience with the electrovaporization technique and to a high rate of illiteracy in the patient population that may have had an impact on the subjective interpretation of the symptom scores.
The MAS conducted a meta-analysis of the studies that provided mean and SD data for the primary outcomes of this assessment. However, not all the studies provided data for all follow-up intervals. Figures 2-A to 2-D show the results of meta-analysis at different follow-up periods for symptom score. Figures 3-A to 3-D show the results of meta-analysis at different follow-up periods for peak urinary flow.
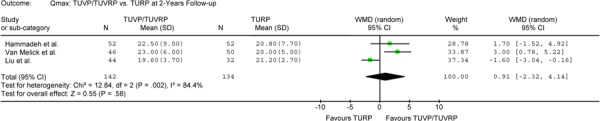
Figure 2-D: TUVP/TUVRP Versus TURP at 5-Year Follow-up Assessment – Outcome: IPSS.

Figure 3-A: TUVP/TUVRP Versus TURP at 6-Month Follow-up Assessment – Outcome: Qmax.

Figure 3-D: TUVP/TUVRP Versus TURP at 5-Year Follow-up Assessment – Outcome: Qmax.
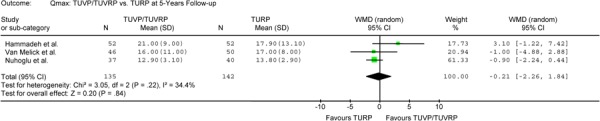
The results of the meta-analysis showed that there was no significant difference between electrovaporization and TURP for symptom scores and peak urinary flow for up to 5 years after the procedure. The weighted mean difference at 1-year follow-up was -0.23 (95% CI, -0.53, 0.07) for symptom score and 1.39 (95% CI, -0.86, 3.63) for peak urinary flow. The weighted mean difference at 5-year follow-up was –0.65 (95% CI, -2.46, 1.15) for symptom score and -0.21 (95% CI, -2.26, 1.84) for peak urinary flow.
No patient undergoing electrovaporization developed TUR syndrome, while this event occurred in 3 of 623 patients (0.5%) undergoing TURP. The rate of blood transfusion was also lower in patients undergoing electrovaporization (1.68%) versus TURP (5.6%). Operating room (OR) time was similar for the two procedures (mean of 45.7 minutes for electrovaporization and mean of 47.6 minutes for TURP). However, duration of catheterization was shorter in electrovaporization compared with TURP (32.2 vs. 57.5 hours) and patients were discharged from the hospital about 1 day earlier (3.0 days vs. 3.9 days).
Rates of urinary stricture and incontinence were also similar between the techniques. Urinary stricture occurred in 3.4% of patients in the electrovaporization group and in 3.9% of the TURP group, and incontinence occurred in 3.9% and 3.7% of electrovaporization and TURP patients, respectively. One of the purported advantages of electrovaporization technique is that there should be no residual sloughing and patients should not experience significant postoperative irritative symptoms. However, the overall incidence of irritative urinary symptoms was 16.3% in electrovaporization and 11.7% in TURP patients.
The incidence of impotence and/or retrograde ejaculation was reported in 7 RCTs (57-63). The rate of retrograde ejaculation and impotence was 30.7% versus 33.9% and 8.2% versus 12.4% for monopolar electrovaporization and TURP respectively. Both techniques had a similar rate of reoperation (4%) but two studies (60;62) did not report whether patients underwent another TURP procedure.
Figure 2-B: TUVP/TUVRP Versus TURP at 1-Year Follow-up Assessment – Outcome: IPSS.

Figure 2-C: TUVP/TUVRP Versus TURP at 2-Year Follow-up Assessment – Outcome: IPSS.
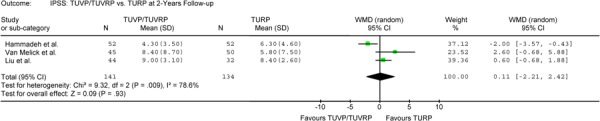
Figure 3-B: TUVP/TUVRP Versus TURP at 1-Year Follow-up Assessment – Outcome: Qmax.

Figure 3-C: TUVP/TUVRP Versus TURP at 2-Year Follow-up Assessment – Outcome: Qmax.
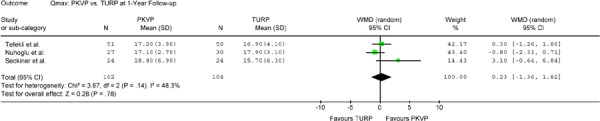
Bipolar Electrovaporization
A total of 496 patients in six trials were randomized to bipolar electrovaporization (PKVP) and TURP: 247 patients to PKVP and 249 to TURP. Four of these studies (32;64-66) provided 1-year follow-up data and reported no statistically significant difference between the techniques for symptom score and peak urinary flow. One of the studies (32), however, reported significantly better peak urinary flow for PKVP at 1-year follow-up (P < .05).
A meta-analysis was conducted on the results of symptom scores and peak urinary flow. No statistically significant difference was found between the two techniques for up to 1-year follow-up.
None of the patients undergoing either technique developed TUR syndrome. Rate of blood transfusion in PKVP patients was about half of that for patients undergoing TURP (1.4% vs. 3.2% in PKVP and TURP respectively).
Operating room time and catheterization time were not different between the 2 techniques (OR time 44.4 vs. 46.2 and catheterization time 55.2 vs. 55.8 for PKVP and TURP respectively). Patients in the PKVP group were discharged from hospital 1.3 days earlier.
Urinary stricture was more common in the PKVP group (PKVP 2.8%, TURP 1.6%). This difference was mainly due to the patients experiencing this complication in the study by Tefekli et al. (32), who also reported a statistically significant difference in irritative urinary symptoms (KVP 12.2%, TURP 4.3%, P = .0014). The authors indicated that a possibly higher current with lower frequency exerted to the tissues may have caused edema and irritation symptoms in PKVP patients.
Sexual functions were not reported in these RCTs. Only Tefekli et al. (32) reported the rate of retrograde ejaculation, which was not different between the 2 techniques (PKVP 59.2%, TURP 63.2%, P > .05).
Rate of reoperation due to persistent obstruction was reported only by Tefekli et al. (32) and it was 4.1% for PKVP and 2.1% for TURP.
Figures 4-A to 4-B show the results of the meta-analysis at different follow-up periods for symptom score.
Figure 4-A: PKVP Versus TURP at 6-Month Follow-up Assessment – Outcome: IPSS.
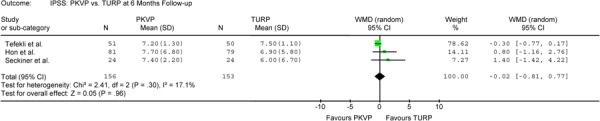
Figure 4-B: PKVP Versus TURP at 1-Year Follow-up Assessment – Outcome: IPSS.

Figures 5-A to 5-B show the results of the meta-analysis at different follow-up periods for peak urinary flow.
Figure 5-A: PKVP Versus TURP at 6-Month Follow-up Assessment – Outcome: Qmax.
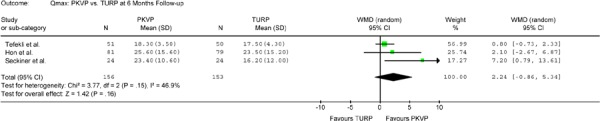
Figure 5-B: PKVP Versus TURP at 1-Year Follow-up Assessment – Outcome: Qmax.
Visual Laser Ablation of the Prostate
Three RCTs (67-69) compared the VLAP technique with TURP for the treatment of BPH. These studies were separate but linked trials from a multicentre pragmatic RCT (CLasP trial) that selected different patient populations. Chacko et al. (67) included 148 men with acute urinary retention, Gujral et al. (68;69) included 82 patients with chronic urinary retention, and Donovan et al. (69) included 234 symptomatic patients with no acute or chronic urinary retention. All three studies had a follow-up of 7.5 months.
These studies used both quantitative and categorical version (good, moderate, and poor outcomes) for reporting symptom score and peak urinary flow. The study on patients with acute urinary retention found no difference in symptom scores in either version, but the other studies reported a significant difference in at least one version favouring TURP. The study on chronic patients (68) reported marginally significant difference in the quantitative version of symptom score (P = .048) in favour of TURP, and a statistically significant difference (P = .035) in the categorical version of symptom score. The study on symptomatic patients (69) found a statistically significant difference in symptom score (P < .05) only in the categorical version of symptom score, which again favoured TURP.
The study on patients with acute urinary retention (67) showed a significantly greater improvement in peak urinary flow in patients undergoing TURP compared with similar patients undergoing VLAP. This difference was found in both quantitative and categorical versions (P = .0097, and P = .0007 respectively). The study on patients with chronic urinary retention (68) found a significant difference only in the categorical version (P = .029), and the study on symptomatic patients (69) found a significant difference in the quantitative version (P < .05) both in favour of TURP.
Hospital stay was significantly shorter in the VLAP group in all three studies (P < .001). On the other hand, the studies showed that time to catheter removal was significantly longer in the VLAP group compared with the TURP group (P < .001). Average time from surgery to final catheter removal was about 9-fold longer after VLAP in two studies (67;68) and 5-fold longer in one study (69). Patients undergoing TURP were kept in hospital until they could void freely, and this resulted in a longer hospital stay, while patients in the VLAP group were sent home earlier with a urethral catheter, which according to the protocol, was in place until tissue sloughed. Any advantage for VLAP over the TURP in terms of shorter hospital stay can, therefore, be ruled out. In two of the three studies (68;69), significantly more patients in the VLAP group required further surgery compared with patients undergoing TURP (P = .029 and P = .0014 respectively).
Contact Laser Vaporization
Three RCTs (34;54;70) compared the effectiveness and safety of CLV with those of TURP. One study was a three-arm design (54) comparing the results of TUVP and CLV with those of TURP.
Tuhkanen et al. (70) found no statistically significant difference for Danish symptom scores (DanPSS-1) and peak urinary flow at 4-year follow-up; however, this small study did not have enough power to detect differences between the study groups. At 4-year follow-up, 32% of the CLV patients were urodynamically obstructed compared with only 10% of the TURP patients. PVR was also significantly greater after CLV compared with TURP patients (P< .05). The rate of reoperation was similar between the two groups (3.8%). Van Melick et al. (54) found no statistically significant difference in IPSS scores and peak urinary flow between the treatment groups at any follow-up interval.
Keoghane et al. (34) reported a statistically significant difference in symptom scores favouring TURP at 1-, 2-, and 3-year follow-up (P = .006, P = .018, and P = .001 respectively). The improvement in peak urinary flow was greater for patients undergoing TURP at 1 and 2 years’ follow-up but not in the third year, but the difference between the two groups was not statistically significant at any follow-up period.
The MAS conducted a meta-analysis on the two studies reporting both mean and SD for symptom score and peak urinary flow. The results show that there is no difference between CLV and TURP in symptom scores at 1-year follow-up. A statistically significant difference in favour of TURP was found at 2 and 3 or more years follow-up. The weighted mean difference was 2.64 for 2-year follow-up (95% CI, 1.04–4.24, P = .001) and 1.87 for 3 or more years’ follow-up (95% CI, 0.21–3.54, P = .03). The results of the meta-analysis on the peak urinary flow show no statistically significant difference between the groups at any interval.
Figures 6-A to 6-C show the results of meta-analysis at different follow-up periods for symptom score.
Figure 6-A: CLV Versus TURP at 1-Year Follow-up Assessment – Outcome: IPSS.
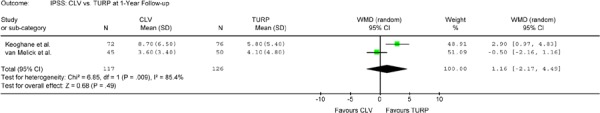
Figure 6-C: CLV Versus TURP at 3-Year Follow-up Assessment – Outcome: IPSS.

Figures 7-A to 7-C show the results of meta-analysis at different follow-up periods for symptom score.
Figure 7-A: CLV Versus TURP at 1-Year Follow-up Assessment – Outcome: Qmax.

Figure 7-C: CLV Versus TURP at 3-Year Follow-up Assessment – Outcome: Qmax.
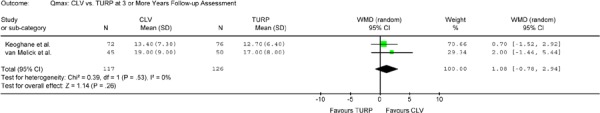
Figure 6-B: CLV Versus TURP at 2-Year Follow-up Assessment – Outcome: IPSS.
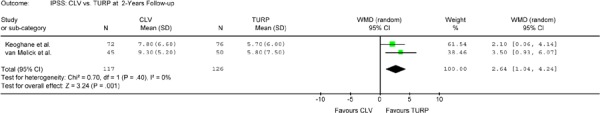
Figure 7-B: CLV Versus TURP at 2-Year Follow-up Assessment – Outcome: Qmax.

OR time differed in only of the studies (70), which reported a significantly longer OR time in the CLV group (51 vs. 34 for CLV and TURP respectively).
The incidence of incontinence was reported in one study (54) and was higher in the CLV group compared with the TURP and TUVP groups: 39% for CLV, 8% for TURP, and 15% for TUVP. At 4- to 7-year follow-up, nocturia was significantly greater in the CLV group (mean 1.9). The authors could not find an explanation for this difference.
Two studies (54;70) reported a longer duration of catheterization for CLV, but the third (34) reported that the duration of catheterization was shorter in the CLV group (1 vs. 2 days), though 28% of the patients in the CLV arm in this study required recatherization compared with 12% of TURP patients (P < .05).
The rate of reoperation was similar in two of the studies (54;70), while one study (34) reported that at 3 years, 18% of the CLV patients and 9% of the TURP patients had undergone reoperation.
Interstitial Laser Coagulation
Three RCTs compared the safety and effectiveness of the ILC technique compared with TURP in the treatment of patients with BPH. In one (37), a multicentre trial consisting of 72 patients, enrolment was stopped early, as patients preferred to undergo the outpatient ILC procedure rather than enrol in the trial and risk assignment to the inpatient TURP procedure. One RCT (56) was a three-arm study comparing ILC, TUMT, and TURP.
In the study by Kursh et al. (37), reduction in IPSS scores was similar in both groups (70% in the TURP group and 63% in the ILC group). The TURP patients had a higher median peak flow rate at 2 years (higher by 2.6 mL/s), with a median increase of 81%, while in the ILC group it increased by 51% and remained below the 15 mL/s upper cut-off point for inclusion in the study (13.9 mL/s). The difference between the groups, however, was not significant. Postoperative urinary tract infection occurred more frequently in the ILC group (20%) compared with the TURP patients (11%). Six (16%) patients in the ILC group had reoperation within 1 year while no patient in the TURP group required retreatment.
In the study by Liedberg et al. (71), some measures, including IPSS scores, could not be evaluated due to limited patient enrolment. Of those criteria that were evaluated, increase in peak urinary flow was found to be significantly higher in the TURP group (P < .02) and mean duration of catheterization was much longer in the ILC group compared with the TURP group (24 days vs. 2 days, P < .001). The study was discontinued early due to the need for prolonged catheterization and high rates of urinary tract infections.
Norby et al. (56) compared the efficacy and safety of ILC (n = 48), TUMT (n = 46) and TURP (n = 24). At 1 and 3 months post-surgery, patients undergoing TURP had significantly lower IPSS scores than the ILC patients (P < .002), but at 6-month follow-up, theis difference became nonsignificant (P = .105). Patients were thus asked to estimate when they first noted symptom reduction. The median time from surgery to symptom improvement was 45 days in ILC and 12 days in TURP patients. The lag in the ILC group was found to be due to treatment-induced lesions that needed to heal. TURP patients exhibited greater improvement in peak urinary flow but the difference (4.4 points) was not statistically significant. The power of this study was reduced from 90% to 85% as the trial had to be stopped for financial restrictions (the recalculated power was based on the final number of patients evaluated at 6 months). Generally, a difference in peak urinary flow of 4.4 points may be considered clinically significant.
A significantly higher rate of urinary tract infection occurred in the ILC group compared with the TURP group (P < .001). Overall, 36% of the patients in ILC group and 73% of the patients in TURP group had no complications (P =.005). None of the patients in the study required reoperation within 6 months.
Holmium Laser Enucleation of the Prostate
Four RCTs (39;40;55;72) with sample sizes ranging from 61 to 200 compared HoLEP to TURP. Overall, 233 and 228 patients were randomized to the HoLEP and TURP arms, respectively, and were followed for 1 year postoperatively. The mean prostate size reported by these studies ranged from 53.5 to 77.8 mL in HoLEP patients and from 49.9 to 70 mL in TURP patients. The results of these trials show excellent clinical outcomes at 1-year follow-up. Both techniques provided similar positive results in urinary symptom score and peak urinary flow rate. Kuntz et al. (39) found the HoLEP technique to be more effective in reducing symptom scores at 6-month and 1-year follow-up (P = .006 and P = .0001, respectively).
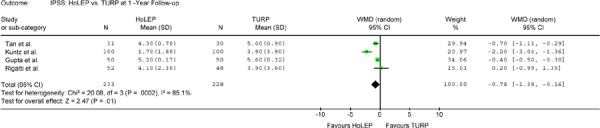
A meta-analysis was conducted on all four studies. The weighted mean difference at 1-year follow-up was -0.78 for IPSS (95% CI, -1.39 to -0.16, P = .01) and 1.75 for Qmax (95% CI, 0.31 to 3.19; P = .02), both in favour of HoLEP.
Figures 8-A and 8-B show the meta-analysis of urinary symptom scores at 6-month and 1-year follow-up.
Figure 8-A: HoLEP Versus TURP at 6-Month Follow-up Assessment – Outcome: IPSS.
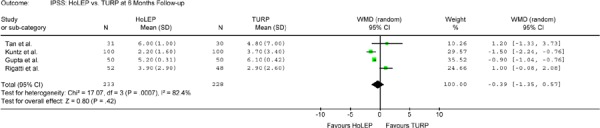
Figure 8-B: HoLEP Versus TURP at 1-Year Follow-up Assessment – Outcome: IPSS.
Figures 9-A and 9-B show the meta-analysis of peak urinary flow at 6-month and 1-year follow-up.
Figure 9-A: HoLEP Versus TURP at 6-Month Follow-up Assessment – Outcome: Qmax.

Figure 9-B: HoLEP Versus TURP at 1-Year Follow-up Assessment – Outcome: Qmax.

None of the patients treated with HoLEP developed TUR syndrome or required blood transfusion. Overall, in the TURP patients, one (0.4%) developed TUR syndrome and five (2.2%) required blood transfusion. The pooled mean OR time was 23 minutes longer in HoLEP arm at 85.5 minutes, compared with 62.6 minutes in the TURP arm. This was mainly due to the time required for the use of a morcellator in the HoLEP group. Larger prostates also require more OR time and the longest HoLEP OR times were reported by Tan et al., (40) who operated on relatively larger prostates. Reoperation was reported in the same study and was 0% for HoLEP versus 6.7%for TURP.
Despite the extended OR time in the HoLEP arm, pooled mean catheterization time and pooled mean hospital stay were about 1 day shorter among these patients. Catheterization time was 26.2 and 48.0 hours in the HoLEP and TURP arms, respectively, and hospital stay was 1.9 and 3.1 days, respectively.
Ten patients (4.3%) in the HoLEP arm and 13 TURP patients (5.7%) underwent recatheterization. The rate of developing urinary stricture was also similar between the two arms at 4.3% and 4.4% in the HoLEP and TURP arms, respectively. Stress incontinence occurred in four patients (1.7%) who underwent HoLEP and in three TURP patients (1.3%). Rigatti et al. (72) reported that 25 (44%) of the HoLEP group and 17 (38.6%) of the TURP group also developed urge incontinence. Two of the trials reported that postoperative irritative voiding symptoms (burning) were more frequent in the HoLEP arm compared with the TURP arm. Rigatti et al. (72) reported burning symptoms in 33 (58.9%) of the HoLEP patients and 13 (29.5%) of the TURP patients. Gupta et al. (55) reported a higher rate of burning in the HoLEP arm (10%) compared with the TURP arm (2%).
Sexual outcomes were reported by Kuntz et al. (39). In the HoLEP arm, 10 patients (11.2%) developed impotence and 66 (74%) developed retrograde ejaculation. Similar outcomes were reported in the TURP arm, with nine patients (10.5%) developing impotence and 61 (70.3%) developing retrograde ejaculation. From a clinical perspective, HoLEP is superior to TURP in terms of a number of key indicators. The improvement in urinary symptom scores and peak urinary flow was better with HoLEP for up to 1-year follow-up. Longer-term efficacy of the HoLEP technique could not be determined through this assessment. TUR syndrome, blood transfusion, duration of catheterization, and length of hospital stay were all less with HoLEP compared with TURP. This technique appears to maintain hemostasis and to prevent absorption of irrigation fluid. Detracting from the procedure, however, were a slight increase in the risk of postoperative irritative voiding symptoms compared to TURP and a number of bladder mucosal injuries that were reported in some studies.
Holmium Laser Enucleation of the Prostate versus Transurethral Electrovaporization of the Prostate
A study by Gupta et al. (55) compared the results of HoLEP, TUVRP, and TURP. No significant difference was found between the HoLEP and TUVRP arms in measures of symptom scores and peak urinary flow at 6-month and 1-year follow-up. Further, no patients from either group developed TUR syndrome or required a blood transfusion, and only one patient from each group developed urinary stricture
OR time was significantly longer (by 20 minutes) in the HoLEP arm but catheterization duration was significantly shorter in this group (by 7.6 hours). Two patients in the HoLEP arm and three patients in the TUVRP arm required recatheterization.
Concerning side-effects, one patient in the HoLEP arm developed incontinence, compared with none in the TUVRP arm. Transient dysuria occurred more frequently in TUVRP patients: five (10%) in HoLEP versus nine (18%) in TUVRP patients. However, the risk of injury was higher with HoLEP than TUVRP.
There was one case of capsular perforation and two cases of bladder mucosal injury in the HoLEP arm compared with none in the TUVRP arm (total risk of injury in the HoLEP arm was 6%).
Holmium Laser Enucleation of the Prostate versus Open Prostatectomy
A randomized controlled trial (73) compared the results of HoLEP procedure with those of open prostatectomy. The study concluded that HoLEP appears to be a safe and effective alternative to open prostatectomy of large (>40 grams) prostates. Both HoLEP and open prostatectomy resulted in significant improvement in symptom scores and peak urinary flow (P < .0001) and the differences between the two techniques were not significant at any interval.
There were however, significant differences in mean hemoglobin loss (1.9% vs. 2.8 g/dL; P < .0001), median catheter time (1 vs. 6 days; P < .0001), and median hospital stay (2 vs. 10 days; P < .0001), all favouring HoLEP. None of the HoLEP patients required blood transfusions, while eight open prostatectomy patients did (P = .003). Mean operation time was significantly longer in HoLEP group (136 vs. 91 min; P < .0001).
Reoperations had to be performed for postoperative bleeding (three patients in each group) and apical resections (two patients in HoLEP group). Bladder neck incision for treatment of postoperative contracture was performed in two patients of the open prostatectomy group and urethrotomy was performed in two patients of the HOLEP group.
Holmium Laser Resection of the Prostate
One RCT (74) with a 4-year follow-up (n = 120) compared HoLRP with TURP. Both treatments were equally effective in reducing urinary symptom scores but HoLRP was shown to be significantly more effective in improving urinary flow at 1-year and 1.5-year follow-up (P < .05 and P < .01 respectively). At 2- and 4-year follow-up, improvement in urinary flow was still better with HoLRP than TURP but did not reach statistical significance. No patient in the HoLRP arm required blood transfusion, compared with four patients (6.8%) in the TURP arm. None of the patients in this trial developed TUR syndrome.
The rate of urinary stricture was the same in both groups with six cases in each arm. Incontinence occurred in two patients (3.3%) in the HoLRP arm and in one patient (1.7%) in the TURP arm. The incidence of postoperative irritating voiding symptoms was not reported in this study. Impotence occurred less frequently in the HoLRP arm with five patients in the group (8%) developing the condition compared to 10 (17%) in the TURP group.
Operating room time was significantly longer with HoLRP than TURP. This was again attributable to the time-consuming process of fragmenting the lobes to ensure safe removal. Catheterization time and hospital stay were both significantly shorter in the HoLRP arm: 20 versus 37 minutes (P < .001) for catheterization time and 1.1 versus 2 days (P < .001) for hospital stay. Five of the 61 (8.2%) HoLRP patients and eight of the 59 (13.6%) TURP patients required reoperation.
Potassium Titanyl Phosphate
One RCT (n = 100) with long-term follow-up (3–6 years) (75) compared laser prostatectomy using KTP with TURP in smaller size prostates. Mean symptom scores were significantly lower in the TURP group at 1-year follow-up. At 3 to 6 years, however, the difference became insignificant. There was no statistically significant difference in flow rate between the groups at 12 months of follow-up. The mean prostate volume in both groups decreased approximately 25% after treatment, but the volume increased to the pretreatment size and mean peak flow rate decreased in both arms at 36–72 month follow-up.
No patients developed TUR syndrome or required a blood transfusion. Operation time, duration of catheterization, and hospital length of stay were not reported. Urinary stricture was more common in the KTP arm with four (8%) patients developing the condition in the group, versus one (2%) in the TURP arm. In contrast, the rate of incontinence was the same in both arms (one patient in each) and none of the patients in this study developed postoperative irritating voiding symptoms to such a degree that additional medications were required beyond those routinely provided upon discharge.
Two patients (4%) in each arm developed retrograde ejaculation and more patients in the KTP arm reported decreased ejaculate volume compared with those in the TURP arm. There was minimal change in patients experiencing impotence in the TURP arm, while the number of patients in the KTP arm with impotence increased at 6-month follow-up (30%–37.5% had no erection). The authors have stated that the increase in impotence is somewhat puzzling.
Microwave Thermotherapy
The MAS identified four trials (56;76-78) that compared the results of TUMT with TURP. Baseline IPSS and Qmax were comparable in all studies with just one exception: in the study by Francisca et al. (78), baseline peak urinary flow was significantly higher (P < .01) in the TUMT arm, favouring TURP. At 1-year follow-up, there was no statistically significant difference between the arms in symptom score.
Figures 10-A to 10-B show the results of meta-analysis at different follow-up periods for symptom score. Figures 11-A to 11-B show results of meta-analysis at different follow-up periods for peak urinary flow.
Figure 10-A: TUMT Versus TURP at 6-Month Follow-up Assessment – Outcome: IPSS.
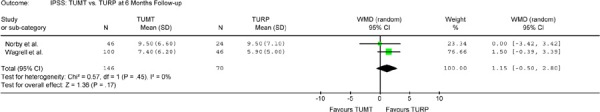
Figure 10-B: TUMT Versus TURP at 1-Year Follow up Assessment – Outcome: IPSS.

Figure 11-A: TUMT Versus TURP at 6-Month Follow-up Assessment – Outcome: Qmax.
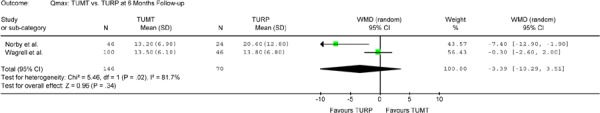
Figure 11-B: TUMT Versus TURP at 1-Year Follow-up Assessment – Outcome: Qmax.

Two studies (77;79) that provided 3-year follow-up data, reported a statistically significant difference in symptom scores between the two arms favouring TURP (P = .024 and P = .000).
Results for peak urinary flow were not consistent between the two studies that provided long-term follow-up. Although both studies showed that patients in the TURP arm had significantly better results in Qmax at 2-year follow-up, the results at 3-year follow-up were significant in only one study (77) (P = .000) and not significant (P = .584) in the other (76).
No patients in the TUMT arm required a blood transfusion, compared with 8.3% of the patients in the TURP arm. Operative time and hospital stay were reported in only 1 study. Wagrell et al. (76) reported that the TUMT procedure took 57 minutes and Norby et al. (56) reported that TUMT was performed as an outpatient procedure in the majority of patients. However, four patients required a night in hospital, and one patient required two nights.
Duration of catheterization was much longer in patients undergoing TUMT compared with TURP. Wagrell et al. (76) reported a mean duration of catheterization of 336 hours for TUMT and 72 hours for TURP. Norby et al. (56) reported that the median durations of catheterization for TUMT were 168 and 336 hours with the use of two different types of software, compared with the median duration of 48 hours in patients undergoing TURP.
The rates of urinary stricture, retrograde ejaculation, and impotence were are found to be significantly less in the TUMT arm, however, a greater number of TUMT patients required reoperation compared to TURP (5% versus 0.5%, respectively).
Transurethral Needle Ablation of the Prostate
Two RCTs (80;81) with sample sizes of 121 and 59, compared the results of TUNA with those of TURP. In both studies, patients had similar symptom scores and peak urinary flow rates at baseline. Hill et al. provided long-term follow-up data and reported that patients undergoing TURP had significantly greater improvement in symptom score at 1-, 2-, 3-, and 4-year follow-up (P = .0049, P = .0028, P = .0079, and P = .0137 respectively). They found no significant difference between the two arms at 5-year follow-up (P = .9813). Cimentepe et al. reported no difference in symptom score at 1.5-year follow-up (P = .899).
Both studies reported that patients treated with TURP had significantly greater improvement in Qmax (P < .001 and P = .004). Hill et al. (80) reported that improvement in peak urinary flow was significantly greater in patients undergoing TURP at all follow-up intervals (P < .0001, P < .0001, P = .0106, P = .0142, and P = .0143 at 1-, 2-, 3-, 4-, and 5-years).
Urinary stricture occurred in 1.1% of the TUNA patients and 6.7% of the TURP patients. None of the patients in the TUNA arm developed retrograde ejaculation, compared with 43.8% of the TURP patients. Impotence occurred in 2.2% of the TUNA patients and 18% of the TURP patients. Patients undergoing TUNA had a higher rate of reoperation compared with the TURP patients (12.1% vs. 1.1%).
Perioperative Data
TUR syndrome was seen only in TURP patients, the incidence being nine out of 1,964 total patients (0.5%). No patient undergoing laser therapy (except those undergoing VLAP procedure), TUMT, or TUNA received a blood transfusion. The rate of blood transfusion in patients undergoing TURP ranged from 0% to 8.3% and was highest in microwave studies (see Figure 12).
Figure 12: Rate of Blood Transfusion: New Techniques Versus TURP.
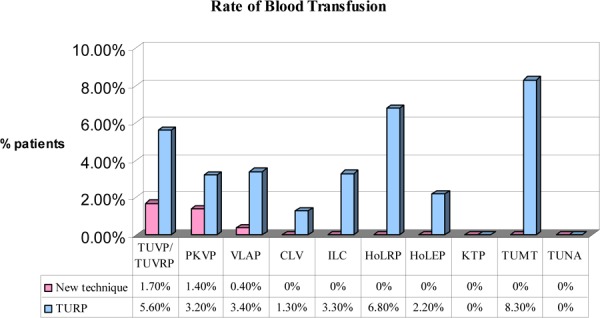
The mean operation time was reported by the studies on electrovaporization, PKVP, CLV, HoLEP, TUMT, and TUNA. The HoLEP operation took longer than the other procedures (see Figure 13).
Figure 13: Mean Operation Time: New Techniques Versus TURP.
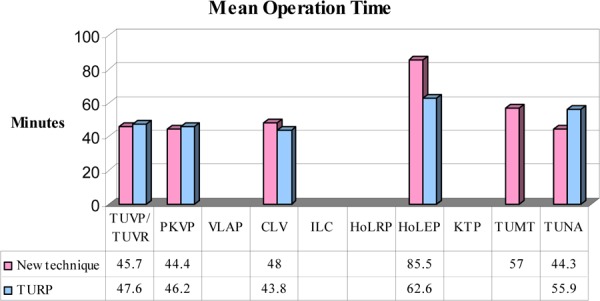
The range of hospital stay for TURP patients was 2 to 5 days. Hospital stays for other surgical procedures ranged from 1 to 3 days, while patients undergoing TUMT or TUNA stayed from 0.5 days to 1 day (see Figure 14). A long duration of catheterization was reported in the VLAP, ILC, and TUMT studies. The mean duration of catheterization for TURP ranged from 2 to 3 days (see Figure 15).
Figure 14: Mean Hospital Stay: New Techniques Versus TURP.

Figure 15: Mean Duration of Catheterization: New Techniques Versus TURP.
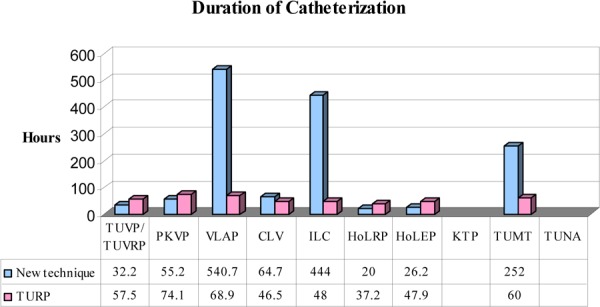
Postoperative Data
Rate of Urinary Stricture
Urinary stricture occurred in 0% to 10.2% of patients undergoing TURP (see Figure 16).
Figure 16: Rate of Urinary Stricture: New Techniques Versus TURP.

Rate of Retrograde Ejaculation and Impotence
Sexual outcomes were reported by several studies, all of which showed a substantial amount of heterogeneity in this outcome among TURP patients (see Figures 17–18).
Figure 17: Rate of Retrograde Ejaculation: New Techniques Versus TURP.
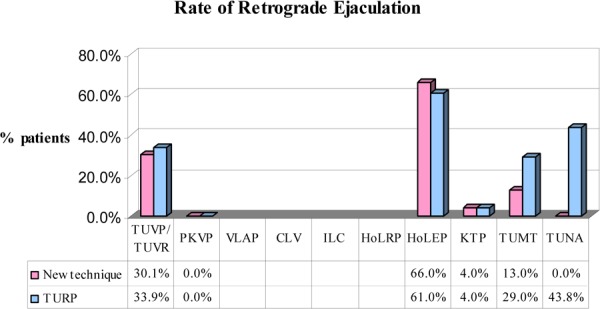
Figure 18: Rate of Impotence: New Techniques Versus TURP.
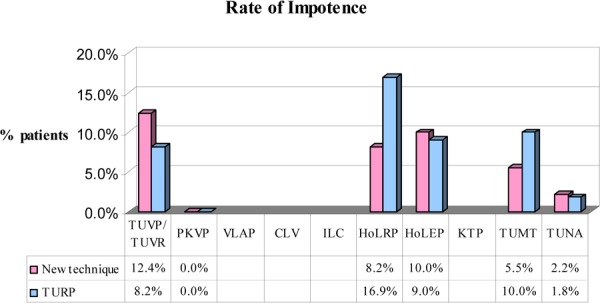
Rate of Reoperation
A meta-analysis on the rate of reoperation showed that patients undergoing either VLAP or TUNA had significantly higher rates of reoperation (see Figures 19-A to 19-F).
Figure 19-A: TUVP/TUVRP Versus TURP – Outcome: Rate of Reoperation.

Figure 19-F: TUNA Versus TURP – Outcome: Rate of Reoperation.

Figure 19-B: VLAP Versus TURP – Outcome: Rate of Reoperation.

Figure 19-C: CLV Versus TURP – Outcome: Rate of Reoperation.

Figure 19-D: ILC Versus TURP – Outcome: Rate of Reoperation.
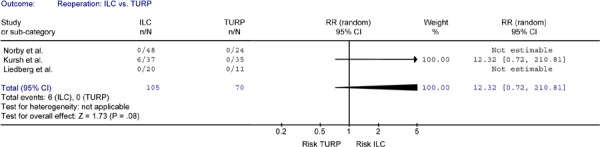
Figure 19-E: TUMT Versus TURP – Outcome: Rate of Reoperation.
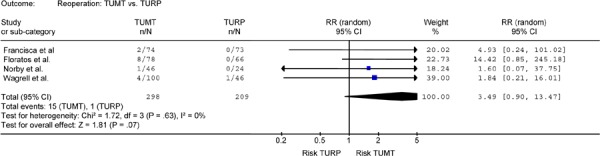
Photoselective Vaporization of the Prostate
As discussed in the “Method of Review”, the only available RCT on KTP laser treatment (75) used a low-power laser generator. To compare high-power KTP with TURP, this section therefore discusses the results of a prospective cohort study.
Bachmann et al. (3) compared the early follow-up and perioperative morbidity of PVP and TURP in a nonrandomized bicentre prospective cohort study. The study included 101 patients (64 PVP and 37 TURP) with the PVP and TURP procedures being carried out at separate hospitals. Inclusion criteria for surgery were a Qmax of 15 mL/s or less, or a transvesically measured PVR greater than 100 mL in conjunction with an IPSS score of greater than 7. PVP was performed using a GreenLight PV laser generator (GreenLight PV™ Laserscope, San Jose, Calif). In all patients receiving PVP, a 14-day postoperative antibiotic prophylaxis was prescribed. Patients were followed for a period of 6 months. Fifteen patients (PVP n = 9; TURP n = 6) did not complete the 6-month follow-up.
Baseline characteristics were similar between the two groups. Patients undergoing PVP had a higher baseline PVR but without clinical importance. In both groups, an immediate and highly significant improvement in symptom score and peak urinary flow was evident. At 6-month follow-up, no significant difference was observed between PVP and TURP in symptom score or peak urinary flow (see Table 6).
Table 6: Subjective and Objective Measures of Effectiveness: Photoselective Vaporization of the Prostate Versus Transurethral Resection of the Prostate.
| Technique | IPSS | Peak urinary flow (Qmax) | ||||
|---|---|---|---|---|---|---|
| Preoperative | 3 months | 6 months | Preoperative | 3 months | 6 months | |
| PVP | 18.1 (5.9) | 6.7 (4.2) | 5.2 (2.1) | 6.9 (1.9) | 17.5 (8.1) | 18.1 (10.3) |
| TURP | 17.3 (6.3) | 6.8 (3.8) | 4.8 (1.6) | 6.9 (2.2) | 21.6 (14.7) | 19.1 (11.0) |
Operating room time was significantly longer for the PVP procedure (59.6±24.4 min vs. 49.9±16 min, P =.039), but the transurethral catheter could be removed earlier for patients in this group (1.8±1.8 days vs. 3±1.5 days, P < .001).
None of the patients in either group developed TUR syndrome or required a blood transfusion. Slightly higher transient urinary retention (7.8% vs. 2.7%, P >.05) and a higher incidence of urethral stricture (7.8% vs. 2.7%, P >.05) were seen after PVP. The rate of urinary tract infection was similar in both groups. Impotence developed in 1 patient undergoing TURP (2.7%).
Summary and Conclusion
A review of the RCTs and a meta-analysis of the RCT results showed that monopolar electrovaporization is as clinically effective as TURP for the relief of urinary symptoms caused by BPH (based on 5-year follow-up data).
A review of the RCTs and a meta-analysis of the RCT results showed that bipolar electrovaporization is as clinically effective as TURP for the relief of urinary symptoms caused by BPH (based on 1-year follow-up data).
Two of the three RCTs on the VLAP procedure have shown that patients undergoing TURP exhibited significantly greater improvement in urinary symptom scores compared with patients undergoing VLAP.
RCTs showed that the time to catheter removal was significantly longer in patients undergoing VLAP compared with patients undergoing TURP.
A meta-analysis of the rate of reoperation showed that patients undergoing VLAP had a significantly higher rate of reoperation compared with patients undergoing TURP.
Results of a meta-analysis showed that patients undergoing TURP exhibited significantly greater improvement in urinary symptom scores compared with CLV at 2 and at ≥3 year follow-up.
Two RCTs with 6-month and 2-year follow-up showed similar improvement in symptom scores for ILC and TURP.
Time to catheter removal was significantly longer in patients undergoing ILC compared with patients undergoing TURP.
The results of RCTs on HoLEP with 1-year follow-up showed excellent clinical outcomes with regard to the urinary symptom score and peak urinary flow.
A meta-analysis showed that at 1-year follow-up, patients undergoing HoLEP had a significantly greater improvement in urinary symptom scores and peak flow rate than did the patients undergoing TURP.
Procedural time is significantly longer for HoLEP compared with TURP.
The results of one RCT with 4-year follow-up showed that HoLRP and TURP provided equivalent improvement in urinary symptom scores.
The results of one RCT with 1-year follow-up showed that patients undergoing TURP had a greater improvement in urinary symptom scores than did patients undergoing KTP; however, the results were not significant at longer-term follow-up periods.
Two RCTs that provided 3-year follow-up data reported that patients undergoing TURP had a significantly greater improvement in symptom score than did patients undergoing the TUMT procedure.
Two RCTs reported a longer duration of catheterization for TUMT compared with TURP (P values were not reported).
The results of a large RCT with 5-year follow-up showed a significantly greater improvement in symptom scores in patients undergoing TURP compared with patients undergoing TUNA.
A meta-analysis on the rate of reoperation showed that patients undergoing TUNA had a significantly higher rate of reoperation compared with patients undergoing TURP.
Based on the results of RCTs, TURP is associated with a 0.5% risk of TUR syndrome, while no cases of TUR syndrome have been reported in patients undergoing monopolar or bipolar electrovaporization, laser-based procedures, TUMT, or TUNA.
Based on the results of RCTs, the rate of blood transfusion ranges from 0% to 8.3% in patients undergoing TURP. The rate is about 1.7% for monopolar electrovaporization, 1.4% for bipolar electrovaporization, and 0.4% for VLAP. No patients undergoing CLV, ILC, HoLEP, HoLRP, KTP, TUMT, and TUNA required blood transfusion.
The mean length of hospital stay ranges from 2 to 5 days for patients undergoing TURP, about 3 days for electrovaporization, about 2 to 4 days for Nd:YAG laser procedures, and about 1 to 2 days for holmium laser procedures. TUMT and TUNA can be performed as a day procedure in an outpatient setting (0.5 and 1 day respectively).
Based on 6-month follow-up data from a prospective cohort study, PVP is as clinically effective as TURP for the relief of urinary symptoms caused by BPH. Time to catheter removal was significantly shorter in patients undergoing PVP than TURP; OR time was significantly longer for the PVP procedure than for TURP. PVP has the potential to reduce health care expenses by shortening hospital stays.
Economic Analysis
Notes and Disclaimer
MAS uses a standardized costing methodology for all of its economic analyses of technologies. The main cost categories and the associated methods from the province’s perspective are as follows:
Hospital: Ontario Case Costing Initiative (OCCI) cost data is used for all program costs when there are 10 or more hospital separations, or one-third or more of hospital separations in the Ministry’s data warehouse are for the designated International Classification of Diseases-10 diagnosis codes and Canadian Classification of Health Interventions procedure codes. Where appropriate, costs are adjusted for hospital-specific or peer-specific effects. In cases where the technology under review falls outside the hospitals that report to the OCCI, PAC-10 weights converted into monetary units are used. Adjustments may need to be made to ensure the relevant case mix group is reflective of the diagnosis and procedures under consideration. Due to the difficulties of estimating indirect costs in hospitals associated with a particular diagnosis or procedure, MAS normally defaults to considering direct treatment costs only. Historical costs have been adjusted upward by 3% per annum, representing a 5% inflation rate assumption less a 2% implicit expectation of efficiency gains by hospitals.
Non-Hospital: These include physician services costs obtained from the Provider Services Branch of the Ontario Ministry of Health and Long-Term Care, device costs from the perspective of local health care institutions, and drug costs from the Ontario Drug Benefit formulary list price.
Discounting: For all cost-effective analyses, discount rates of 5% and 3% are used as per the Canadian Agency for Drugs and Technologies in Health (CADTH) and the Washington Panel of Cost-Effectiveness, respectively.
Downstream cost savings: All cost avoidance and cost savings are based on assumptions of utilization, care patterns, funding, and other factors. These may or may not be realized by the system or individual institutions.
In cases where a deviation from this standard is used, an explanation is given as to the reasons, the assumptions and the revised approach employed.
The economic analysis represents an estimate only, based on assumptions and costing methods that have been explicitly stated above. These estimates will change if different assumptions and costing methods are applied for the purpose of developing implementation plans for the technology.
Ontario-Based Economic Analysis/Budget Impact Analysis
Diffusion
The delivery of the various energy-based interventions for the treatment of BPH is currently controlled by hospitals from within their global hospital budgets.
Table 7 illustrates the total number of TURP procedures and energy-based interventions for the treatment of BPH that were performed in Ontario in FY2002, FY2003, and FY2004.
Table 7: Total Number of TURP and Energy-Based Interventions for BPH Treatment in Ontario.
| Technology | FY2002 | FY2003 | FY2004 |
|---|---|---|---|
| Transurethral resection of the prostate (TURP) | 5,208 | 4,922 | 4,899 |
| Transurethral electrovapor resection of the prostate (TUVRP) | 78 | 33 | 16 |
| Transurethral microwave thermotherapy (TUMT) | 0 | 0 | 0 |
| Transurethral needle ablation (TUNA) | 29 | 9 | 8 |
| Laser Therapies | 155 | 78 | 49 |
| Transurethral incision of the prostate (TUIP) | 1 | 5 | 2 |
FY indicates fiscal year.
The various laser technologies for the treatment of BPH have all been classified using the same Canadian Classification of Intervention (CCI) procedural codes. As a result, the total number of procedures using a particular laser technology could not be distinguished. Similarly, monopolar and bipolar electrovaporization procedures could not be distinguished from each other so their numbers are reported together.
Figure 20 illustrates the inverse relationship between patient utilization of drugs and the total number of surgical interventions performed for the treatment of BPH in Ontario. The data on utilization and costs of drugs used for the treatment of BPH was obtained from the Ontario Drug Benefit (ODB) programs branch. The drugs included in this graph are tamsulosin HCL 0.4 mg cap and alfuzosin hydrochloride 10 mg prolonged-release tabs in the alpha-blocker class of drugs, and finasteride 5 mg tab and dutasteride 0.5 mg cap in the 5-alpha-reductase inhibitor class of drugs. Among the alpha-blocker class of drugs, terazosin, doxazosin, and prazosin had data available but were not included in the analysis as these drugs are also used for the management of high blood pressure. The indication of use could not be determined from the available data set. The y-axis on the left illustrates the total number of patients utilizing drugs for the treatment of BPH while the y-axis on the right represents the total number of surgical interventions undertaken each year for the treatment of BPH.
Figure 20: Utilization of Drugs Versus Surgical Interventions for the Treatment of BPH in Ontario.
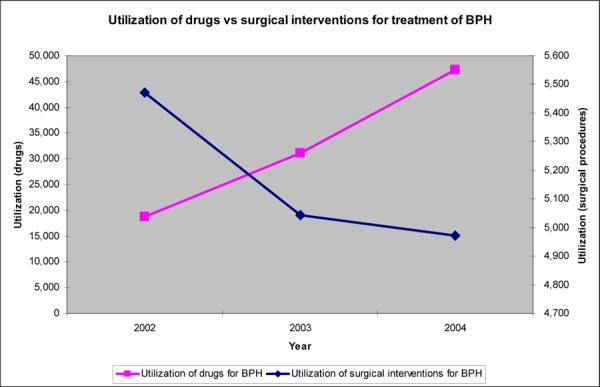
It is important to note that this figure illustrates utilization only amongst males who were recipients of the Ontario Drug Benefit program and were probably those who showed mild symptoms of BPH. This Figure simply illustrates the “trend” and not the exact figures associated with the utilization of drugs for the treatment of BPH. From fiscal year 2002 to fiscal year 2004, the total number of surgical interventions decreased by approximately 500 procedures. Figure 21 illustrates costs associated with the utilization of drugs as well as surgical interventions for the treatment of BPH.
Figure 21: Costs of Drugs Versus Surgical Interventions for the Treatment of BPH in Ontario.
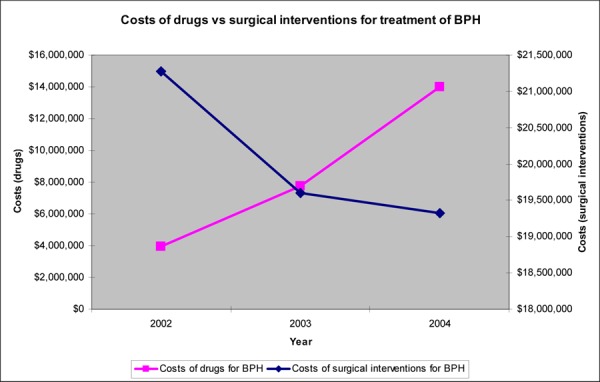
From fiscal year 2002 to fiscal year 2004, the increase in costs of drugs to the government was estimated at approximately $10 million (Cdn), while the decrease in costs, due to a decline in the total number of surgical procedures, was estimated at approximately $1.9 million (Cdn). This data shows that from FY2002 to FY2004, the increase in costs associated with the increase in utilization of drugs for the treatment of BPH translates into $353/patient, while the cost savings associated with a decrease in the total number of surgical procedures translates into a savings of $3,906/patient. An important consideration in the above illustration is that drug therapy is a long-term treatment for the management of BPH. Therefore, the costs associated with drugs are compounded over time, i.e. they are annual costs incurred by the province each year, while the cost of an intervention is a one-time cost to the province.
Costs
All costs are in Canadian currency unless otherwise noted.
Professional Costs
Total professional costs (including anesthetist and assistant costs) of a surgical procedure for the treatment of BPH is estimated at $522.66 (Ontario Schedule of Benefits Physician Claims, 2005).
Hospital Costs
The hospital costs were calculated using a combination of the PAC-10 weights1 from the Provincial Health Planning Database (PHPDB), operating room (OR) time and the cost of blood transfusion specific to each procedure. The OR time and blood transfusion rates were obtained from the literature. All associated hospital costs are listed in Table 8 below.
Table 8: Professional, Hospital, Device and Total Costs per Procedure Associated With the Various Energy-Based Interventions for the Treatment of BPH*.
| Technology | Physician Costs, $ | Hospital Costs, $ | Device Cost (Capital), $ | Device Cost (Consumables), $ | Total Cost per Procedure, $ |
|---|---|---|---|---|---|
| TURP | 450 | 3,314 | 135,000 | 123 | 3,887 |
| Bipolar Electrovaporization | 450 | 3,301 | 169,000 | 260 | 4,011 |
| Monopolar Electrovaporization | 450 | 3,404 | 135,000 | 276 | 4,130 |
| TUMT | 450 | 84 | 25,000 | 995 | 1,529 |
| TUNA | 450 | 3,119 | 36,500 | 1,235 | 4,804 |
| PVP (Green) | 450 | 85 | 100,000 | 650 | 1,184 |
| Holmium Laser | 450 | 3,213 | 240,000 | 229 | 3,892 |
| VLAP Nd:YAG | 450 | 3,213 | 120,000 | 1,000 | 4,663 |
| CLV Nd:YAG | 450 | 3,165 | 120,000 | 1,000 | 4,615 |
All costs are in Canadian dollars.
Total Costs
The total cost of each procedure was estimated by adding all professional, hospital, and device costs associated with a particular procedure for the treatment of BPH. The cost of each device was provided by the various manufacturer(s) of the particular technology. Each of these costs is listed in Table 2 above. Only the cost of consumables was included in the overall cost calculation. The reasoning behind this was twofold. Firstly, for some of the technologies, the generators were already diffused in the majority of hospitals and health care facilities. Secondly, the capital costs were low compared with the overall costs of each procedure for the treatment of BPH.
Budget Impact
As is illustrated in Table 7, an average of approximately 5,000 TURP procedures were performed in Ontario in the three most recent fiscal years. Table 9 summarizes the change in the current budget, depending on various estimates of the total percentage of the 5,000 TURP procedures that might be replaced by other energy-based interventions for the treatment of BPH in the future.
Table 9: Budget Impact With Estimates of the Percentage of TURP Procedures Captured by Energy-Based Interventions for the Treatment of BPH.
| Technology | Cost per procedure, $ | Budget Impact of 25% diffusion, $M | Budget Impact of 50% diffusion, $M | Budget Impact of 75% diffusion, $M | Budget Impact of 100% diffusion, $M | Incremental Budget Impact, $M |
|---|---|---|---|---|---|---|
| TURP | 3,887 | 19.4 | ||||
| Bipolar Electrovaporization | 4,011 | 19.6 | 19.7 | 19.9 | 20.0 | 0.6 |
| Monopolar Electrovaporization | 4,130 | 19.7 | 20.0 | 20.3 | 20.6 | 1.2 |
| TUMT | 1,529 | 16.5 | 13.5 | 10.6 | 7.6 | (11.8) |
| TUNA | 4,804 | 20.6 | 21.7 | 22.9 | 24.0 | 4.6 |
| PVP | 1,184 | 16.0 | 12.7 | 9.3 | 5.9 | (13.5) |
| Holmium Laser | 3,892 | 19.4 | 19.4 | 19.4 | 19.4 | 0.02 |
| VLAP Nd:YAG | 4,663 | 20.4 | 21.4 | 22.3 | 23.3 | 3.9 |
| CLAP Nd:YAG | 4,615 | 20.3 | 21.2 | 22.4 | 23.0 | 3.6 |
All costs are in Canadian currency. Parentheses indicative of cost reduction.
Unmeasured Costs
It is important to consider downstream cost savings that were not quantifiable in the economic analysis. Due to a lack of data on the energy-based interventions, the total costs did not include other cost savings that might be realized in the future, e.g. a decrease in urinary tract infection rates, a decrease in sexual dysfunction rates, as well as increased quality of life and patient comfort, etc... Since the reoperation rates were not consistently reported in the literature, it was not possible to assess cost savings due to a “possible” decrease in reoperation rates for energy-based treatments compared with TURP.
Existing Guidelines for Use of Technology
Canadian guidelines for the management of BPH, 2005 (16) have been developed as an evidence-based consensus provided by the CUA in collaboration with the Canadian Prostate Health Council.
The 2003 AUA guideline on the management of BPH (82) has a different perspective than the Canadian guideline and has had a profound effect on clinical urologic practice in the United States. The European guidelines published in 2001 on BPH (24) have also made recommendations for assessment, therapeutic options, and follow-up of patients with BPH.
Appraisal/Policy Development
For many years, TURP has been the gold standard in the treatment of BPH. Newer transurethral surgical treatments have been developed as an alternative to TURP in an effort to minimize the risk of TUR syndrome, which occurs in 0.5% of cases and blood loss, as well as to shorten hospital stay.
Diffusion – International, National, Provincial
In Canada, the new technologies to treat BPH have not achieved a significant level of diffusion. The techniques are not at all used in Alberta, Saskatchewan, Prince Edward Island, New Brunswick, or Nova Scotia. Holmium laser procedures are used in Quebec, British Columbia and in Manitoba where VLAP, and CLV are also being used. In Quebec, one procedure code covers all nonsurgical prostatectomy techniques used to treat BHP and it is not possible to determine which technique is used without requesting the attending physician’s clinical notes or report.
In the United States, PVP currently accounts for about 50% of the surgical procedures performed for the treatment of BPH (Personal communication, Specialist advisor, August 2006). Among patients, PVP is popular as they can be discharged on the same day as the surgery. Other techniques that can be performed in an outpatient setting such as TUMT have also achieved significant diffusion in the US.
Diffusion in Ontario
In Ontario, the overall uptake of new techniques is less than 5% to 10% of all TURP procedures (4.8% in 2002, 2.4% in 2003, and 1.5% in 2004) (Personal communication, July 2006) (see Table 7). Availability of the techniques and a steep learning curve are the two major factors limiting the use of new energy-based techniques. Across Canada as a whole, TURP comprises more than 90% of the surgical interventions for treatment of BPH (Personal communication, August 2006).
Table 10 shows the number of health care facilities in Ontario that treat patient with BPH with new energy-based techniques.
Table 10: Number of Ontario Hospitals and Clinics Treating Patients with BPH With New Energy-based Techniques.
| Technique | N |
|---|---|
| Monopolar electrovaporization | 91 |
| Bipolar electrovaporization | 10 |
| Holmium laser | 4 |
| PVP | 6 |
| TUMT | 3 |
| TUNA | 0 |
Patient Outcomes – Medical, Clinical
TURP allows the surgeon to obtain tissue for pathological examination. The absence of tissue sampling is one disadvantage for most of the new procedures, the common exception being HoLEP, which can provide tissue for sampling through the use of a tissue morcellator. With monopolar electrovaporization it is also possible to obtain a tissue sample by changing the vaporizing electrode to a standard loop electrode, but in doing so the benefit of tissue vaporization is lost.
The requirement for obtaining pathological specimens depends on the site at which cancers appears in the prostate gland. Most prostate cancers occur in the peripheral zone near the rectum, while the transition zone surrounding the urethra, is the usual site of BPH. The majority of cancers sampled at TURP are of transition zone origin, while less than 20% of peripheral zone cancers are sampled in TURP (83). As a result, most prostate cancers are out of reach for TURP. This can be deleterious, as the peripheral zone cancers have a higher grade and are more frequently associated with extraprostatic spread of cancer than transition zone cancers. (84)
It is, however, unlikely that cases of significant cancer would be missed because of a lack of tissue samples (Personal communication, specialist advisor, August 2006). To rule out cancer before BPH surgery, it is necessary to perform a thorough preoperative work-up by digital rectal examination and, if needed, transrectal ultrasound and prostate specific antigen level.
Financial Impact
A decline in TURP procedures performed has been documented in several countries (9;85), possibly representing the impact of new methods of treatment. Some of the procedures delivered on a day-case basis may be acceptable to many patients and physicians, but the key measure of effectiveness remains the durability of good patient outcomes. Temporarily effective therapies that may be more attractive to the patient should not be allowed to change practice patterns in the management of BPH. Treatment failures may become costly over time as the need for additional surgeries, or a cascade of mixed therapies, may impose a greater expenditure on the health care system.
With new energy-based techniques, the risks of TUR syndrome and blood transfusion are minimized, imparting a major advantage over TURP in terms of both patient outcome and cost. It also appears that some of these new techniques reduce the demand on hospital beds by shortening hospital stays. For example, ninety percent of patients undergoing PVP can be discharged the same day (Personal communication, specialist opinion, August 2006). In the context of day-surgery, PVP has the potential for cost-saving if its long-term effectiveness is proven. Similarly, HoLEP has been shown to be effective in the treatment of patients with BPH and also has a short hospital stay (average 1.9 days according to RCT evidence). Slightly further out, monopolar and bipolar electrovaporization have been shown to be effective and require 2.5 to 3 days in hospital.
Lastly, resource use including nursing time is an important consideration (Personal communication, specialist opinion, August 2006). Techniques that can be used in an outpatient setting save nursing time, as well as hospital beds.
Other Applications of Lasers in Urology
Holmium lasers have several alternative applications in urology including the management of stone diseases, urinary tumours, and urinary tract stenoses. Older generations of holmium laser generators are generally of low-power (20 W) and cannot be used for the treatment of BPH. Only a few hospitals in Ontario have purchased a high-power (80-W) holmium laser generator, which is capable of being used for BPH treatment. On the other hand, the wavelength needed for PVP does not allow the laser to be used for conditions other than BPH.
Funding in Ontario
TUMT, TUNA, and HIFU are currently not insured in Ontario, while monopolar and bipolar electrovaporization and laser-based techniques are. Since there are no specific codes for the laser types, it is not currently possible to distinguish between different types of laser procedures for funding purposes.
Training Requirement
HoLEP has a considerable learning curve, necessitating urological surgeons to perform a minimum of 20 to 30 procedures to become familiar with the technique. PVP also requires training and has a learning curve of 15 to 20 procedures. In contrast, monopolar and bipolar techniques are similar to TURP and do not require extensive training. With bipolar electrovaporization, physicians need perform only 4 to 5 procedures to become familiar with the technique. (Personal communication, specialist opinion, July 2006)
Other Considerations
The U.S. Food and Drug Administration (FDA) issued a Public Health Notification in October 2000 concerning the potential for serious thermal injury associated with the use of microwave energy for the treatment of patients with BPH. The complications associated with thermal injury included fistula formation and tissue damage to the penis or urethra, potentially requiring therapeutic intervention. (86)
All of the leading urological device manufacturers make equipment capable of performing TURP, TUIP, and TUVP/TUVRP. In general, there is little difference between manufacturers for these technologies. There are, however, significant differences between them for the various lasers and TUMT. (Personal communication, specialist opinion, July 18, 2006)
Glossary
- Acute urinary retention
Inability to urinate
- Disuria
Painful or difficult passage of urine
- Impotence
Inability to achieve or sustain a penile erection
- Gold standard procedure
A procedure that is widely recognized as the best available
- Hemolysis
Disruption of the integrity of the red cell membrane causing release of hemoglobin
- Hesitancy
Difficulty starting or maintaining urinary stream
- Intermittency
Urinary stream starts and stops
- Isotonic solution
A solution that has the same salt concentration as the cells and blood
- Meta-analysis
A quantitative method of combining the results of independent studies and synthesizing summaries and conclusions
- Morcellator
A device that divides and removes small pieces of the tumour
- Resectoscope
A special endoscopic instrument for the transurethral removal of lesions involving the bladder, prostate gland, and urethra
- Prostatic urethra
A portion of the male urethra surrounded by the prostate gland
- Retrograde ejaculation
Ejaculation that goes backward into the bladder instead of forward through the urethra
- Saddle anesthesia
Anesthesia limited to the area of buttocks, perineum, and inner surfaces of the thighs
- Sphincter
A ring-like band of muscle fibres that constrict a passage or close a natural orifice
- Thermotherapy
Treatment of disease by the application of heat
- Urethral stricture
A narrowing of the urethra
- Urgency
The sudden compelling urge to urinate
- Urinary incontinence
Inability to control urination
- Urinary meatus
The external urinary orifice
- Urodynamic tests
Tests that show how well the bladder contracts and how blocked the flow of urine is
- Uroflow tests
Tests that determine how fast the urine flows out
Appendices
Appendix 1: Literature Search Strategy
Search date: June 21, 2006
Databases searched: OVID MEDLINE, MEDLINE In Process & Other Non-Indexed Citations, EMBASE, Cochrane Library, INAHTA
Database: Ovid MEDLINE(R) <1996 to June Week 2 2006>
Search Strategy:
--------------------------------------------------------------------------------
exp Prostatic Hyperplasia/ (5543)
(benign prostat$ hyperplasia or benign prostat$ hypertrophy).mp. [mp=title, original title, abstract, name of substance word, subject heading word] (4512)
1 or 2 (6592)
exp “Transurethral Resection of Prostate”/ (796)
(transurethral adj2 (resection or prostatectomy)).mp. [mp=title, original title, abstract, name of substance word, subject heading word] (3017)
turp.mp. (792)
or/4-6 (3135)
3 and 7 (1089)
(VLAP or visual la#er ablation).mp. [mp=title, original title, abstract, name of substance word, subject heading word] (47)
(tuep or tuvp or clv or clp or clap).mp. [mp=title, original title, abstract, name of substance word, subject heading word] (1495)
(((holmium or YAG) adj4 la#er adj6 prostat$) or holrp or holap or holep).mp. [mp=title, original title, abstract, name of substance word, subject heading word] (100)
((photo-selective or photoselective) adj vapo?ri#ation).mp. [mp=title, original title, abstract, name of substance word, subject heading word] (10)
(interstitial la#er adj2 (coagulation or photocoagulation or electrocoagulation)).mp. [mp=title, original title, abstract, name of substance word, subject heading word] (129)
(transurethral microwave thermal therapy or TUMT).mp. [mp=title, original title, abstract, name of substance word, subject heading word] (158)
(transurethral needle ablation or tuna).mp. [mp=title, original title, abstract, name of substance word, subject heading word] (529)
(bipolar adj2 (TURP or electrocautery or resection or electrosurgery or prostate$)).mp. [mp=title, original title, abstract, name of substance word, subject heading word] (72)
(plasma kinetic or plasmakinetic or PKRP or gyrus).mp. [mp=title, original title, abstract, name of substance word, subject heading word] (10869)
(thermeablation or enucleation or photocoagulation or electroresection or thermotherapy or thermoablation or evapo$ or electrovapo$ or vapo?r$).mp. [mp=title, original title, abstract, name of substance word, subject heading word] (19574)
exp Electrocoagulation/ or exp Electrosurgery/ or exp Ultrasonic Therapy/ or exp Volatilization/ (15908)
exp Catheter Ablation/ (7250)
*laser surgery/ or exp laser coagulation/ (8356)
laser$.mp. or exp Lasers/ (57863)
(high intensity focused ultrasound or HIFU).mp. [mp=title, original title, abstract, name of substance word, subject heading word] (292)
(Transurethral incision of the prostate or tuip).mp. [mp=title, original title, abstract, name of substance word, subject heading word] (41)
(Potassium titanyl phosphate or KTP).mp. [mp=title, original title, abstract, name of substance word, subject heading word] (305)
or/9-25 (100813)
(3 or 8) and 26 (992)
limit 27 to (humans and english language and yr=“2000 - 2006”) (433)
(systematic review$ or metaanalysis or meta-analysis).mp. [mp=title, original title, abstract, name of substance word, subject heading word] (23816)
28 and 29 (16)
28 (433)
limit 31 to (case reports or comment or editorial or letter or “review”) (125)
31 not 32 (308)
30 or 33 (317)
Database: EMBASE <1980 to 2006 Week 24>
Search Strategy:
--------------------------------------------------------------------------------
exp Prostate Hypertrophy/ (11080)
(benign prostat$ hyperplasia or benign prostat$ hypertrophy).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] (7304)
1 or 2 (12119)
exp Transurethral Resection/ (5964)
(transurethral adj2 (resection or prostatectomy)).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] (7376)
turp.mp. (1189)
or/4-6 (7503)
3 and 7 (2013)
(VLAP or visual la#er ablation).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] (81)
(tuep or tuvp or clv or clp or clap).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] (1575)
exp Holmium Laser/ (806)
(((holmium or YAG) adj4 la#er adj6 prostat$) or holrp or holap or holep).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] (139)
((photo-selective or photoselective) adj vapo?ri#ation).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] (12)
exp Vaporization/ (1518)
(interstitial la#er adj2 (coagulation or photocoagulation or electrocoagulation)).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] (174)
laser$.mp. or exp Lasers/ (87080)
(Potassium titanyl phosphate or KTP).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] (513)
exp Laser Coagulation/ (9037)
(transurethral microwave thermal therapy or TUMT).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] (168)
exp Microwave Therapy/ (155)
(transurethral needle ablation or tuna).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] (787)
exp TRANSURETHRAL NEEDLE ABLATION/ (87)
(Transurethral incision of the prostate or tuip).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] (80)
(plasma kinetic or plasmakinetic or PKRP or gyrus).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] (18130)
(bipolar adj2 (TURP or electrocautery or resection or electrosurgery or prostate$)).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] (94)
exp ELECTROCOAGULATION/ (2203)
exp ELECTROSURGERY/ (3817)
exp VOLATILIZATION/ (2062)
(thermeablation or enucleation or photocoagulation or electroresection or thermotherapy or thermoablation or evapo$ or electrovapo$ or vapo?r$).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] (38355)
exp High Intensity Focused Ultrasound/ (201)
(high intensity focused ultrasound or HIFU).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] (415)
or/9-28 (113601)
8 and 32 (602)
3 and 32 (1056)
33 or 34 (1056)
limit 35 to (human and english language and yr=“2000 - 2006”) (395)
(systematic review$ or metaanalysis or meta-analysis).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] (39096)
36 and 37 (20)
36 (395)
limit 39 to (editorial or letter or note or “review”) (114)
Case Report/ (889259)
39 not (40 or 41) (271)
38 or 42 (284)
Appendix 2: The American Urological Association Symptom Index
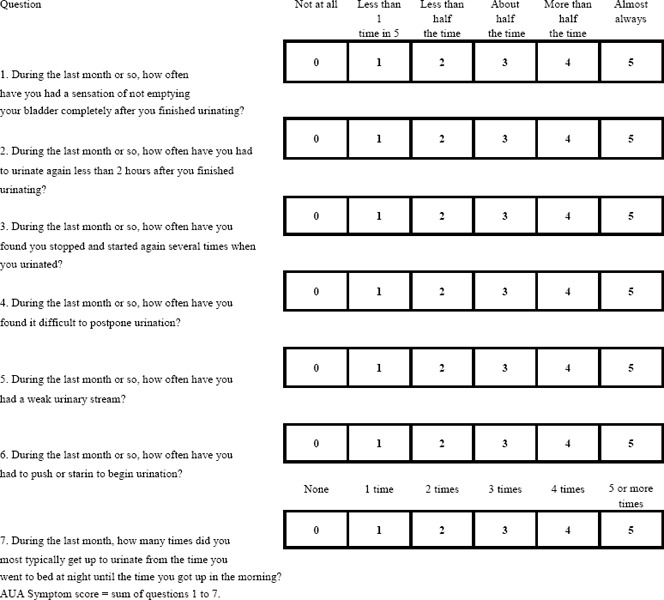
Source: Barry MJ, Fowler FJ, Jr., O’Leary MP, Bruskewitz RC, Holtgrewe HL, Mebust WK et al. The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. Journal of Urology 1992;148 (5):1549–1557.
Appendix 3: Grade Score for the Body of Evidence
| Number of Studies | Study Design | Quality of Studies | Consistency | Directness | Other Modifying Factors |
|---|---|---|---|---|---|
| N | RCT=High Observational=Low Any other evidence =Very low |
Serious limitation (−1) Very serious limitation (−2) |
Important inconsistency (−1) |
Same uncertainty (−1) Major uncertainty (−2) |
|
Source: Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S et al. Grading quality of evidence and strength of recommendations. BMJ 2004;328(7454):1490
Grading System Applied to Included Studies for Meta-Analysis.
| Number of Studies | Study Design | Quality of Studies | Consistency | Directness | Other Modifying Factors | Overall Quality of Evidence |
|---|---|---|---|---|---|---|
| 38 | RCTs=High | High/medium | +/− | Yes | Not applicable | High |
Appendix 4: Data Tables
Electrovaporization using Monopolar Energy
Table 1: Patient Characteristics; Electrovaporization Using Monopolar Energy Versus TURP.
| Study, Year | Patients, No. (Treatment, control) | Inclusion criteria | Prostate size Mean (SD), mL | Mean follow-up, Years, Months | Type of Electrode used for electrovaporization | No. available for follow-up |
|---|---|---|---|---|---|---|
| Liu et al. 2006 (60) | 76 (44, 32) | Patients on the waiting list for surgery for BPH (IPSS ≥15, QOL score ≥3, Qmax=<12 mL/s) | TUVP: 60.5 (10.9) TURP: 58.4 (8.4) NS |
2 | Wedge | TUVP: IPSS: 42; QOL: 36; Qmax: 9;PVR: 23 TURP IPSS: 30; QOL: 26; Qmax: 21; PVR: 21 |
| Gupta et al. 2006 (55) 3-arm study |
100 (50, 50) Third arm: HoLEP: 50 |
Patients with BPH who were candidates for TURP and gland size of >40 g | TUVP: 62.6 (14.8) TURP: 59.8 (16.5) |
1 | Wolf-Wing | NR |
| Nuhoglu et al. 2005 (61) | 77 (37, 40) |
Patients with BPH who had IPSS >15 and Qmax <10 mL/s | TUVP: 39 (8.1) TURP: 39 (7.7) |
TUVP: 5.7 (0.6) TURP: 5.6 (0.9) |
Spike | TUVP: 21 TURP: 23 |
| Akhtar 2004 (59) | 50 (25, 25) |
Patients with BPH; prostate size ≤ 50 gr | 37.6 (11.1) 38.6 (11.8) |
0.5 | NR | NR |
| McAllister et al. 2003 (62;87) Multicentre | 235 (115, 120) |
Patients with symptomatic BPH and suitable for bladder outlet surgery | TUVP: 51.1 TURP: 54.3 |
2 | Vaportrude | TUVP: 90 TURP: 77 |
| Van Melick 2002 (88;89) 3-arm study | 96 (46, 50) Third arm: contact laser: 45 |
Patients older than 45 years of age and LUTS due to BPH (Schafer’s obstruction grade ≥2) and prostate volume 20–65 cm3 | TUVP: 35 (11) TURP: 37 (11) |
TUVP 1–4 years: 2.8 (1) 4–7 years: 5.4 (1) TURP 1–4 years: 2.7 (0.8) 4–7 years: 5.7 (0.8) |
Vaportrude |
1 year TUVP: 34 TURP: 41 1–4 years TUVP: 12 TURP: 15 4–7 years TUVP: 24 TURP: 30 |
| Hammadeh et al. 2003 (57;90) | 104 (52, 52) |
Patients with BBO due to BPH on the waiting list for TURP (IPSS ≥13, quality-of-life index ≥3, Qmax <15 mL/s) | TUVP: 32 (9.1) TURP: 27 (12.2) P =.02 |
5 | Vaportrude | TUVP: 27 TURP: 26 |
| Gupta et al. 2002 (91) | 100 (50, 50) |
Patients with BOO secondary to BPH who had indications for prostatectomy and prostate size >40 | TUVRP: 63 TUVP: 54 |
1 | Wolf-Wing | NR |
| Helke et al. 2001 | 185 (93, 92) |
Patients with BPH, moderate to severe LUTS (IPSS>10, and/or PVR<60 mL) | TUVRP: 48.8 TURP: 49.9 |
1 | Wolf-Wing | TUVRP: 80, 80, and 79 for 3, 6 and 12 months TURP: 69,74, and 73 for 3, 6, and 12 months |
| Kupeli et al. 2001 (63) | 100 (50, 50) |
Patients with BBO due to BPH on the waiting list expecting TURP (IPSS ≥8 and Qmax <15 mL/s) | TUVRP: 57.8 (4.1) TURP: 56.7 (6.3) |
6.7 months | Wolf-Wing | NR |
| Talic et al. 2000 (58) | 68 (34, 34) |
Patients with moderate to severe BBO due to BPH (IPSS >15 and Qmax <15 mL/s) | TUVRP: 52.4 (18.7) TURP: 57.2 (22.5) |
Months TUVRP: 9.2 TURP: 8.8 |
Wolf-Wing | 68 |
| Ekengren et al. 2000 (92) | 54 (26, 28) |
Patients with BPH between 48 and 83 years old scheduled for surgery | Median TUVP: 50 TURP: 39 |
1 | Roller-ball | NR |
BBO refers to bladder outlet obstruction; BPH, benign prostatic hyperplasia; HoLEP, holmium laser enucleation of the prostate; IPSS, International Prostate Symptom Score; LUTS, Lower urinary tract symptoms; NR, not reported; PVR, postvoid residual urine; Qmax, maximum flow rate; QOL, Quality of life; TURP, transurethral resection of the prostate; TUVP, Transurethral electrovaporization of the prostate; TUVRP, transurethral electrovapor resection of the prostate
Table 2: Subjective Measures of Effectiveness; Electrovaporization Using Monopolar Energy Versus TURP.
| Study, Year | IPSS, Mean (SD) | QOL score, Mean (SD) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 3 months | 6 months | 12 months | > 1 year | Baseline | 3 months | 6 months | 12 months | > 1 year | ||
| Liu et al. 2006 (60) TUVRP TURP |
26.8 (4.7) 25.6 (3.5) P = .65 |
8.2 (2.2) 7.9 (1.8) P = .53 |
NR | NR |
2 years: 9.0 (3.1) 8.4 (2.6) P =.45 |
4.1 (0.6) 4.0 (0.7) P = .75 |
1.7 (0.5) 1.5 (0.7) P = .57 |
NR | NR |
2 Years 16 (0.6) 14 (0.7) P =.48 |
|
| Gupta et al. 2006 TUVRP TURP |
24.9 (3.9) 23.3 (3.9) P = .1 (between 3 groups) |
NR | 5.9 (0.25) 6.1 (0.42) P = .14 (between 3 groups) |
5.4 (0.28) 5.6 (0.32) P = .6 (between 3 groups) |
NR | NR | NR | NR | NR | NR | |
| Nuhoglu et al. 2005 (61) TUVP TURP |
17.3 (6.8) 17.6 (7.2) |
4.7 (3.1) 4.8 (4.2) P >.05 |
NR | NR |
>5 years 6.5 (3.2) 6.1 (3.5) P >.05 |
NR | NR | NR | NR | NR | |
| Akhtar 2004 (59) TUVP TURP |
NR | 8.72 (2.23) 6.04 (2.42) P =.0001 |
5.36 (1.85) 3.36 (1.85) P =.0002 |
NR | NR | NR | NR | NR | NR | NR | |
| McAllister et al. 2005 (62;87) TUVP TURP |
20.7 (7.3) 20.7 (6.9) P >.05 |
2 months 11.8 (7.7) 9.8 (7.2) P >.05 |
8.5 (7.4) 6.9 (5.5) P >.05 |
NR |
2 years 8.6 (7.2) 7.5 (5.8) P >.05 |
4.6 (1.17) 4.9 (0.98) P >.05 |
2 months 2.6 (1.82) 2.3 (1.73) P >.05 |
2.0 (1.63) 1.6 (1.34) P >.05 |
NR |
2 years 1.9 (1.62) 1.8 (1.34) P >.05 |
|
| Van Melick et al. 2003 (88;89) TUVP TURP |
20.3 (6.8) 16.6 (5.6) P >.05 |
NR | 3.8 (2.7) 3.2 (2.7) P >.05 |
4.8 (4.9) 4.1 (4.8) P >.05 |
1–4 years 8.4 (8.7) 5.8 (7.5) 4–7 years 7 (5.6) 7.3 (7.1) |
4.3 (1.3) 3.9 (1.6) P >.05 |
NR | 1 (0.8) 0.5 (0.5) P >.05 |
1 (0.9) 0.6 (0.8) P >.05 |
1–4 years 1 (1.2) 1.1 (1.2) 4–7 years 1.4 (0.8) 1.3 (1.3) |
|
| Hammadeh et al. 2003 (57;90) TUVP TURP |
26.5 (4.5) 26.6 (4.8) P = .9 |
NR | NR | 4.4 (3.8) 5.9 (5.2) P = .3 |
2 years 4.3 (3.5) 6.3 (4.6) P = .02 3 years 4.1 (3.3) 7.1 (6.2) P = .01 5 years 5.9 (6.3) 8.6 (7.1) P = .16 |
4.9 (0.9) 5 (0.7) P = .6 |
NR | NR | 1.2 (1) 1.5 (1) P = .3 |
2 years 1.1 (1) 1.7 (1.1) P =.004 3 years 1 (0.9) 1.6 (1.4) P = .04 5 years 1.1 (1.2) 1.7 (1.4) P = .09 |
|
| Gupta et al. 2002 TUVRP TURP |
24 22 |
NR | 4.79 5.82 |
5.28 5.9 |
NR | NR | NR | NR | NR | NR | |
| Helke et al. 2001 TUVRP TURP |
17.29 (6.06) 18.29 (7.49) P > .05 |
NR | NR | 4.66 (4.3) 5.21 (5.1) P > .05 |
NR | NR | NR | NR | NR | NR | |
| Kupeli et al. 2001 (63) TUVRP TURP |
19.4 21.6 |
NR | 4.0 5.0 P > .05 |
NR | NR | NR | NR | NR | NR | NR | |
| Talic et al. 2000 (58) TUVRP TURP |
24.9 (6) 20.1 (6.8) |
NR | 4 (3.4) 5.6 (3.1) P = .03 |
NR | NR | NR | NR | NR | NR | NR | |
| Ekengren et al. 2000 (92) TUVRP TURP |
Median 22 25 |
NR | NR | Median 4.5 4 |
NR | Median 4.5 5.5 |
NR | NR | Median 1.5 1 |
NR | |
NR refers to not reported; SD, standard deviation; TURP, transurethral resection of the prostate; TUVP, Transurethral electrovaporization of the prostate; TUVRP, transurethral electrovapor resection of the prostate
Table 3: Objective Measures of Effectiveness. Electrovaporization Using Monopolar Energy Versus TURP.
| Study, Year | Peak urinary flow (Qmax), Mean (SD), mL/s | Postvoid residual urine, Mean (SD), mL | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 3 months | 6 months | 1 year | > 1 year | Baseline | 3 months | 6 months | 1 year | > 1 year | ||
| Liu et al. 2006 (60) TUVRP TURP |
6.9 (2.1) 6.9 (1.9) P = .91 |
20.7 (2.8) 21.6 (2.0) P = .2 |
NR | NR |
2 years 19.6 (3.7) 21.2 (2.7) P = .12 |
142 (48) 131 (41) P = .31 |
34 (12) 35 (18) P = .25 |
NR | NR |
2 Years 33 (15) 28 (16) P = .29 |
|
| Gupta et al. 2006 TUVRP TURP |
4.65 (3.6) 4.5 (4.7) P = .73 (between 3 groups) |
NR | 22.5 (0.95) 20.7 (1.32) P = .33 (between 3 groups) |
23.6 (0.96) 23.7 (1.58) P = .62 (between 3 groups) |
NR | 103 (174.1) 84 (129.7) P = .65 (between 3 groups) |
NR | <20 <20 |
<20 <20 |
NR | |
| Nuhoglu et al. 2005 (61) TUVP TURP |
6.3 (2.1) 5.9 (2.6) |
17.7 (2.3) 17.5 (3.3) P >.05 |
NR | NR |
>5 years 12.9 (3.1) 13.8 (2.9) P >.05 |
88 (20) 95 (26) |
25 (13) 23 (12) P >.05 |
NR | NR |
>5 years 35 (15) 38 (17) P >.05 |
|
| Akhtar 2004 (59) TUVP TURP |
NR | 14.44 (3.31) 15.6 (1.70) P = .114 |
13.84 (1.75) 15.88 (3.02) P = .0028 |
NR | NR | NR | 35.2 (21.24) 26.4 (16.04) P = .091 |
28.4 (19.56) 11.48 (2.18) P = .003 |
NR | NR | |
| McAllister et al. 2005 (62;87) TUVP TURP |
10.1 (4.35) 10.5 2 (5.04) P >.05 |
2 months 19.12 (11.76) 21.23 (10.2) P >.05 |
19.6 (11.04) 22.29 (10.25) P >.05 |
NR | NR | 181.1 (162.4) 170.8 (184.3) P > .05 |
2 months 59.3 (59.5) 77.8 (120.7) P > .05 |
71.0 (72) 71.8 (87.4) P >.05 |
NR | NR | |
| Van Melick 2003 (88;89) TUVP TURP |
9 (3) 13 (4) P >.05 |
NR | 24 (11) 26 (6) P >.05 |
28 (6) 23 (10) P >.05 |
1–4 years 23 (6) 20 (5) 4–7 years 16 (11) 17 (8) |
NR | NR | NR | NR | NR | |
| Hammadeh et al. 2003 (57;90) TUVP TURP |
8.9 (3.2) 8.6 (3.2) P = .7 |
NR | NR | 22.5 (9) 20.8 (7.7) P = .4 |
2 years 22.4 (7.7) 21.2 (8.5) P =.5 3 years 22.2 (8.5) 18 (7.1) P =.02 5 years 21 (9) 17.9 (13.1) P =.17 |
131 (78.5) 101 (87.9) P =.1 |
NR | NR | 24.3 (33.1) 25.8 (25.6) P =.1 |
2 years 18.8 (21.2) 22.8 (29.8) P =.5 3 years 30 (38) 21.9 (26.2) P =.27 5 years 27.3 (44.3) 10.7 (13.1) P =.08 |
|
| Gupta et al. 2002 TUVRP TURP |
6.4 7 |
22.55 25.14 |
NR |
22 26 |
NR | 82 78 |
NR | <10 <10 |
Nil Nil |
NR | |
| Helke et al. 2001 TUVRP TURP |
10.8 (4.76) 8.5 (5.19) P <.02 |
NR | NR | 22.19 (12.3) 22.12 (10.6) P >.05 |
NR | 76 (60.50) 101.8 (84.1) NS |
NR | NR | 6.81 (21.3) 7.58 (27.5) P >.05 |
NR | |
| Kupeli et al. 2001 (63) TUVRP TURP |
7.9 (2.1) 9.2 (2.6) |
NR | 26.7 (3.7) 24.6 (3.4) P-value NR |
NR | NR | NR | NR | NR | NR | NR | |
| Talic et al. 2000 (58) TUVRP TURP |
7.5 (3.5) 9.1 (6.3) |
NR | 19 (6.5) 15.2 (10) P =.01 |
NR | NR | NR | NR | NR | NR | NR | |
| Ekengren et al. 2000 (92) TUVRP TURP |
Median 4 2 |
NR | NR | Median 10 11 |
NR | Median 55 100 |
NR | NR | Median 17 57 |
NR | |
NR refers to not reported; SD, standard deviation; TURP, transurethral resection of the prostate; TUVP, Transurethral electrovaporization of the prostate; TUVRP, transurethral electrovapor resection of the prostate
Table 4: Perioperative Outcomes. Electrovaporization Using Monopolar Energy Versus TURP.
| Study, Year | Operative time Mean (SD), Min | Hospital stay Mean (SD), Days | Catheterization time Mean (SD), Hours | Hemoglobin decrease, Mean (SD), g/dL | Transfusion, N (%) | Intraoperative irrigant requirement, Mean (SD), L | TUR syndrome No. N (%) | Irritating voiding symptoms N (%) |
|---|---|---|---|---|---|---|---|---|
| Liu et al. 2006 (60) TUVRP TURP |
49.4 (8.0) 52.9 (6.0) P =.04 |
1.65 (0.2) 2.06 (0.35) P <.0001 |
25.4 (4.3) 39.8 (9.0) P =.0001 |
% decrease 11.6 (1.8) 16.3 (4.8) P <.0001 |
1 (2.3) 2 (6.3) P =.38 |
25.5 (8.3) 33 (8.1) P.003 |
0 2 P =.17 |
NR |
| Gupta et al. 2006 TUVRP TURP |
55.9 (18.1) 64.1 (13.1) P < .001 between 3 arms |
NR | 36.2 (8.3) 45.7 (12.7) P < .001 between 3 arms |
0.96 (0.9) 1.1 (0.8) |
0 1 (2%) |
18 (7.6) 24.2 (11.8) P <.001 between 3 arms |
0 0 |
9 (18%) 1 (2%) |
| Nuhoglu et al. 2005 (61) TUVP TURP |
45 (13.2) 42 (9.5) NS |
NR | 22 (5.7) 75.7 (12.5) P < .001 |
0.5 (P > .05) 0.7 (P < .05) |
0 2 |
NR | 0 0 |
NR |
| Akhtar 2004 (59) TUVP TURP |
20.6 (9.5) 35.8 (17.12) P = .0046 |
4.4 (0.91) 6.25 (1.23) P = .0046 |
24 (0) 74.88 (19.98) P = .0001 |
1 (4) 6 (24) P = .033 |
8.28 (3.23) 11.7 (5.2) P = .007 |
0 1 (4) P = .31 |
NR | |
| McAllister et al. 2005 (62;87) TUVP TURP |
49 44.7 NS |
4.4 (3) 4.6 (4) NS |
NR |
Hct 0.23 0.039 P = .039 |
2 (1.7) 9 (7.5) P = .04 |
NR | 0 0 |
NR |
| Van Melick 2003 (88;89) TUVP TURP |
50 (16) 58 (26) P = .09 |
3.4 (0.9) 3.9 (0.9) P > .05 |
45.6 (14.4) 50.4 (16.8) P > .05 |
0.32 1.29 P < .001 |
0 1 |
14 (8) 16 (7) |
0 0 |
0–5% 0–5% |
| Hammadeh et al. 2003 (57;90) TUVP TURP |
25.9 (8.3) 21.6 (8.4) P = .01 |
2.2 (0.59) 3.1 (0.76) P < .001 |
20.9 (7) 46.6 (12.5) P < .001 |
0.8 1.2 P < .003 |
0 1 (2%) P = .3 |
0 17.5 (6.8) P < .001 |
0 0 |
13 (25%) 18 (35%) P = .36 |
| Gupta et al. 2002 TUVRP TURP |
45 60 P < .0001 |
2.5 3 P > .05 |
44.88 52.32 P < .001 |
1.32 1.96 P > .05 |
0 2 |
16.4 21 P < .0001 |
0 0 |
6 (12%) 2 (4%) |
| Kupeli et al. 2001 (63) TUVRP TURP |
48.2 42.7 P < .05 |
2.5 4.5 P < .05 |
48 96 P < .05 |
Hct 1.0 4.3 |
0 0 |
NR | 0 0 |
NR |
| Helke et al. 2001 TUVRP TURP |
Resection time 71.02 (27.5) 65.68 (25.8) P = .18 |
NR | NR | 1.77 2.06 NS |
6 9 |
NR | Serum sodium <128 mmol/L 5 6 |
NR |
| Talic et al. 2000 (58) TUVRP TURP |
Resection time 42.4 (15) 35.9 (12.8) P = .02 |
NR | 23.1 (10.3) 36 (17.3) P <.0001 |
0.4 (NS) 0.6 (P =.03) |
0 0 |
NR | 0 0 |
NR |
| Ekengren et al. 2000 (92) TUVRP TURP |
Median 30 33 |
NR | NR | NR | NR | NR | 0 0 |
1 0 |
Mean decrease in hemoglobin unless otherwise stated; Hct, hematocrit; NR refers to not reported; SD, standard deviation; TUR, transurethral resection; TURP, transurethral resection of the prostate; TUVP, Transurethral electrovaporization of the prostate; TUVRP, transurethral electrovapor resection of the prostate
Table 5: Postoperative and Long-Term Adverse Events. Electrovaporization Using Monopolar Energy Versus TURP.
| RCT | Urinary complications | Sexual dysfunction | Reoperation N (%) | Mortality N (%) | |||
|---|---|---|---|---|---|---|---|
| Urinary retention N (%) | Bladder neck/urethral stricture, N (%) | Incontinence, N (%) | Impotence, N (%) | Retrograde ejaculation, N (%) | |||
| Liu et al. 2006 (60) TUVRP TURP |
0 0 Recatheterization 3 0 |
3 (6.8%) 2 (6.3%) NS |
2 (4.5%) 1 (3.1%) NS |
6 months 4 (9.1%) 3 (9.4%) P =.66 |
6 months 10 (22.7%) 7 (21.9%) P =.54 |
Further surgery: 2 years 2 (4.5%) 3 (9.4%) |
0 0 |
| Gupta et al. 2006 TUVRP TURP |
0 0 Recatheterization 3 3 |
1 (2%) 2 (4%) |
0 1 (2%) |
NR | NR | 0 0 |
0 1 (pneumonia) |
| Nuhoglu et al. 2005 (61) TUVP TURP |
1 (2.7%) 0 (0%) |
1 (2.7%) 0 (0%) |
0 0 |
4 (16%) 2 (10%) P-value NR |
5 (14%) 4 (17%) P-value NR |
4 years 1 0 |
NR |
| Akhtar 2004 (59) TUVP TURP |
0 1 (4%) |
1 (4) 1 (4) NS |
0 0 |
NR | 6 (24) 10 (40) P =.22 |
0 0 |
NR |
| McAllister et al. 2005 (62;87) TUVP TURP |
0 0 |
0 0 |
1 1 |
2 years 12/69 (17%) 5/58 (9%) |
6 months 31/64 (48%) 35/59 (59%) NS |
Further surgery 1 4 |
1 (arm NR) |
| Van Melick 2003 (88;89) TUVP TURP |
0 0 |
1 3 |
7 (15%) 4 (8%) |
NR | NR | At 4.3 years 3 (6%) 4 (9%) |
At 4.3 years 4 (8%) 2 (4%)(all unrelated causes) |
| Hammadeh et al. 2003 (57;90) TUVP TURP |
12 (23%) 4 (8%) P =.04 |
3 4 |
0 0 |
5 (17%) 3 (11 %) P =.49 |
21 (72%) 25 (89%) P =.47 |
7 (13%) 7 (13%) |
3 (cardio-pulmonary) 6 (cardio-pulmonary) |
| Gupta et al. 2002 TUVRP TUP |
0 0 Recatheterization 1 2 |
1 1 |
0 2 |
NR | NR | 0 1 |
0 0 |
| Helke et al. 2001 TUVRP TURP |
NR | 5/93 7/92 |
Urge incontinence 5 6 Stress incontinence 9 8 |
NR | NR | 9 5 |
0 0 |
| Kupeli et al. 2001 (63) TUVRP TURP |
0 0 |
0 0 |
0 0 |
12 (24%) 11 (22%) |
26 (52%) 27 (54%) |
0 0 |
0 0 |
| Talic et al. 2000 (58) TUVRP TURP |
0 0 |
3 4 |
0 0 |
0 0 |
NR | 0 0 |
NR |
| Ekengren et al. 2000 (92) TUVRP TURP |
0 1 |
2 0 |
0 0 |
NR | NR | 2 1 |
1 (due to MI) 0 |
NR refers to not reported; TURP, transurethral resection of the prostate; TUVP, Transurethral electrovaporization of the prostate; TUVRP, transurethral electrovapor resection of the prostate
Electrovaporization using Bipolar Energy
Table 6: Patient Characteristics. Electrovaporization Using Bipolar Energy Versus Transurethral Resection of the Prostate.
| Study, Year | Patients, No (Treatment, control) | Inclusion criteria | Prostate size Mean (SD), mL | Mean follow-up Years (months where specified) | No available for follow-up |
|---|---|---|---|---|---|
| Hon et al. 2006 (93) | 160 (81, 79) |
Patients with BPH; prostate size =<80 cc. | PKVP: 38 (17.5) TURP: 40 (17.1) P =.49 |
Months PKVP: 8.8 (5.1) TURP: 8.2 (4.4) |
PKVP: 76 TURP: 73 |
| De Sio et al. 2006 (66) | 70 (35, 35) |
Patients with BPH >50 years, good performance status, acute urinary retention if the removal of the catheter failed after therapy with alpha blockers and chronic urinary retention unresponsive to medical therapy, IPSS>18, Qmax<15 mL/s | PKVP: 51.6 (3.9) TURP: 47.5 (5.1) |
Months 9 |
70 PKVP: 35 TURP: 35 |
| Nuhoglu et al. 2006 (64) | 57 (27, 30) |
Patients with BPH (IPSS >15 and Qmax <10 mL/s) | PKVP: 49 (8.1) TURP: 47 (7.7) |
1 | 50 PKVP: 24 TURP: 26 |
| Seckiner et al. 2006 (65) | 48 (24, 24) |
Patients with BPH 50 years or older; prostate size 30–70 gr; IPSS≥8; Qmax <15 mL/s | PKVP: 49.4 (18.9) TURP: 41.4 (14.5) P = .128 |
Months PKVP: 14.5 (6) TURP: 13.9 (4.1) |
44 PKVP: 23 TURP: 21 |
| Tefekli et al. 2005 (32) | 101 (51, 50) |
Patients with BPH who failed medical therapy: 72 (71.3%); Patients with recurrent urinary retention due to BPH: 29 (28.7%) | PKVP: 50.1 (17.3) TURP: 54 (15.2) NS |
Months 18.3 (6.7) |
96 PKVP: 49 TURP: 47 |
| Fung et al. 2005 (94) | 60 (29, 31) |
Patients on the waiting list for surgery for BPH (acute urinary retention and failure to remove the catheter, chronic urinary retention due to BPH causing renal impairment and severe LOST [IPSS >20 and Qmax <10 mL/s) | NR | Months 3 |
51 PKVP: 21 TURP: 30 |
BPH refers to benign prostatic hyperplasia; IPSS, International Prostate Symptom Score; NR, not reported;; Qmax, maximum flow rate; PKVP, Plasmakinetic vaporization of the prostate; TURP, transurethral resection of the prostate
Table 7: Subjective Outcome Measures of Effectiveness. Electrovaporization Using Bipolar Energy Versus TURP.
| Study, Year | IPSS, Mean (SD) | QOL score, Mean (SD) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 3 months | 6 months | 12 months | > 1 year | Baseline | 3 months | 6 months | 12 months | > 1 year | |
| Hon et al. 2006 (93) PKVP TURP |
21.3 (6.2) 20.6 (7) P =.58 |
NR | 8.6 months 7.7 (6.8) 6.9 (5.8) P =.44 |
NR | NR | 4.2 (1.1) 4.3 (1.3) P =.84 |
NR | 8.6 Months 1.7 (1.5) 1.5 (1.5) P =.64 |
NR | NR |
| De Sio et al. 2006 (66) | 24.18 (4) 24.3 (5) NS |
Graph only | Graph only | Graph only | NR | 4.2 (1) 3.9 (1) NS |
Graph only | Graph only | Graph only | NR |
| Nuhoglu et al. 2006 (64) PKVP TURP |
17.6 (6.1) 17.3 (5.8) P >.05 |
NR | NR | 5.4 (3.7) 5.2 (3.2) P >.05 |
NR | NR | NR | NR | NR | NR |
| Seckiner et al. 2006 (65) PKVP TURP |
24.1 (5.2) 23.2 (4.9) P =.635 |
9.3 (3.9) 10.6 (6.3) P >.05 |
7.4 (2.2) 6 (6.7) P >.05 |
8.7 (4.1) 8.3 (2.9) P >.05 |
NR | 4.4 (0.6) 4.7 (0.9) P >.05 |
1.8 (1) 2.1 (1.2) P >.05 |
1.6 (0.7) 1.6 (1.3) P >.05 |
1.8 (0.8) 2 (0.8) P >.05 |
NR |
| Tefekli et al. 2005 (32) PKVP TURP |
NR | 9.2 (2.1) 9.8 (2.9) P-value; NR |
7.2 (1.3) 7.5 (1.1) P >.05 |
7.9 (1.5) 7.3 (1.6) P >.05 |
NR | NR | NR | NR | NR | NR |
| Fung et al. 2005 (94) PKVP TURP |
15.82 19.36 P =.457 |
Mean change 8.81 9.63 P =.862 |
NR | NR | NR | 3.55 3.64 P =.875 |
Mean change 0.55 1.54 P =.169 |
NR | NR | NR |
BPH refers to benign prostatic hyperplasia; IPSS, International Prostate Symptom Score; NR, not reported; Qmax, maximum flow rate; PKVP, Plasmakinetic vaporization of the prostate; SD, standard deviation; TURP, transurethral resection of the prostate
Table 8: Objective Measures of Effectiveness. Electrovaporization Using Bipolar Energy Versus TURP.
| Study, Year | Peak urinary flow (Qmax), Mean (SD), mL/s | Postvoid residual urine, Mean (SD), mL | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 3 months | 6 months | 1 year | > 1 year | Baseline | 3 months | 6 months 1 year | 1 year | > 1 year | |
| Hon et al. 2006 (93) PKVP TURP |
12 (6.4) 11.9 (6) P = .79 |
NR |
8.6 mon 25.6 (15.6) 23.5 (15.2) P =.41 |
NR | NR | 147 (156) 182 (180) P =.26 |
NR |
8.6 months 64 (65) 69 (67) P =.68 |
NR | NR |
| De Sio et al. 2006 (66) | 7.1 (2) 6.3 (3) NS |
Graph only | Graph only | Graph only | NR | 80 (22.5) 75 (35.5) NS |
Graph only | Graph only | Graph only | NR |
| Nuhoglu et al. 2006 (64) PKVP TURP |
6.9 (2.8) 7.3 (2.1) P > .05 |
NR | NR | 17.1 (2.7) 17.9 (3.1) P > .05 |
NR | 96 (27) 88 (20) P > .05 |
NR | NR | 33 (19) 35 (15) P > .05 |
NR |
| Seckiner et al. 2006 (65) PKVP TURP |
8.5 (2.9) 8.3 (3.1) P =.800 |
17.7 (9.1) 18.6 (9.1) P >.05 |
23.4 (10.6) 16.2 (12) P >.05 |
18.8 (6.9) 15.7 (6.3) P >.05 |
NR | 88 (74) 138 (115) P =.148 |
NR | NR | NR | NR |
| Tefekli et al. 2005 (32) PKVP TURP |
NR | 16.9 (2.8) 15.8 (3.7) P-value; NR |
18.3 (3.5) 17.5 (4.3) P-value; NR |
17.2 (3.9) 16.9 (4.1) P <.05 |
NR | NR | NR | NR | NR | NR |
| Fung et al. 2005 (94) PKVP TURP |
NR |
Mean change 16.57 14.7 P =.96 |
NR | NR | NR | NR | NR | NR | NR | NR |
NR refers to not reported; NS, not significant; Qmax, maximum flow rate; PKVP, Plasmakinetic vaporization of the prostate; Qmax, maximum flow rate; SD, standard deviation; TURP, transurethral resection of the prostate
Table 9: Perioperative Outcomes. Electrovaporization Using Bipolar Energy Versus TURP.
| Study, Year | Operative time Mean (SD), Min | Hospital stay Mean (SD), Days | Catheterization time Mean (SD), Hours | Hemoglobin decrease, Mean (SD), g/dL | Transfusion, N (%) | Intra-operative irrigant requirement, Mean (SD), L | TUR syndrome No N (%) | Irritative voiding symptoms N (%) |
|---|---|---|---|---|---|---|---|---|
| Hon et al. 2006 (93) PKVP TURP |
Resection time 32.6 (13.4) 28.5 (15.2) P = .08 |
3 (0.9) 3.4 (1.1) |
NR | 0.8 (0.9) 1.4 (1.3) P =.002 |
0 4 (5.3) |
NR | 0 0 |
NR |
| De Sio et al. 2006 (66) PKVP TURP PKVP TURP |
49 53 NS Resection time: 33 39 NS |
2.26 4.46 |
72 100 P <.05 |
0.8 1 |
1 0 NS |
NR | 0 0 |
NR |
| Nuhoglu et al. 2006 (64) PKVP TURP |
55 (9.7) 52 (13.2) NS |
NR | 47 (5.6) 75.7 (12.5) P < .009 |
0.3 0.5 NS |
1 2 |
NR | 0 0 |
NR |
| Seckiner et al. 2006 (65) PKVP TURP |
52.9 (12.8) 52.9 (16.3) P =.835 |
NR | 74.4 (33.6) 74.4 (14.4) NS |
0.6 1.5 |
0 0 |
8.3 (3.8) 6.9 (3.2) P = .213 |
0 0 |
NR |
| Tefekli et al. 2005 (32) PKVP TURP |
40.3 (11.4) 57.8 (13.4) P <.01 |
NR | 55.2 (16.8) 91.2 (16.8) P <.05 |
NR | 1 1 |
11.4 (45) 18.3 (13.6) P <.05 |
0 0 |
6 (12.2) 2 (4.3) |
| Fung et al. 2005 (94) PKVP TURP |
Resection time 36.6 32.9 P =.488 |
NR | 27.36 29.04 P =.594 |
0.24 NR NS |
NR | 11.6 12.2 P =.722 |
0 0 |
NR |
NR refers to not reported; NS, not significant; PKVP, Plasmakinetic vaporization of the prostate; SD, standard deviation; TUR, transurethral resection; TURP, transurethral resection of the prostate
Table 10: Postoperative and Long Term Adverse Events. Electrovaporization Using Bipolar Energy Versus TURP.
| RCT | Urinary complications | Sexual dysfunction | Reoperation N (%) | Mortality N (%) | |||
|---|---|---|---|---|---|---|---|
| Urinary retention N (%) |
Bladder neck/urethral stricture N (%) |
Incontinence N (%) | Impotence N (%) | Retrograde ejaculation N (%) | |||
| Hon et al. 2006 (93) PKVP TURP |
1 2 |
0 1 |
NR | NR | NR | Bladder neck incision 1 2 |
NR |
| De Sio et al. 2006 (66) PKVP TURP |
NR | 1 1 |
NR | NR | NR | For bladder neck contracture 1 1 |
NR |
| Nuhoglu et al. 2006 (64) PKVP TURP |
1 0 |
1 0 |
0 0 |
NR | NR | 0 0 |
1 (the group is not indicated) |
| Seckiner et al. 2006 (65) PKVP TURP |
NR | 2 1 |
NR | NR | NR | 0 0 |
NR |
| Tefekli et al. 2005 (32) PKVP TURP |
1 1 Recatheterization 2 0 |
3 (6.1%) 1 (2.1%) P =.002 |
0 1 |
0 0 |
29 (59.2%) 30 (63.8%) NS |
2 (4.1%) 1 (2.1%) (all persistent obstructive symptoms) |
0 1 (due to MI) |
| Fung et al. 2005 (94) PKVP TURP |
4 3 |
0 0 |
0 0 |
NR | NR | NR | NR |
NR refers to not reported; PKVP, Plasmakinetic vaporization of the prostate; TURP, transurethral resection of the prostate
Laser Studies
Visual Laser Ablation of the Prostate (VLAP)
Table 11: Patient Characteristics, Visual Laser Ablation Versus TURP.
| Study, Year | Patients, No. (Treatment, control) | Inclusion criteria | Prostate size Mean (SD), mL | Mean follow-up (Months) | No. available for follow-up |
|---|---|---|---|---|---|
| Chacko et al. 2001(67) Multicentre trial (CLasP study) 3- arm |
148 (74, 74) |
ClasP trial acute patients: Acute painful urinary retention: Patients with BPH | NR | VLAP: 7.3 months TURP: 7.5 months |
VLAP: 70 TURP: 73 |
| Gujral et al. 2000 (68) Multicentre trial (CLasP study) 3-arm |
82 (38, 44) |
ClasP trial chronic patients: Chronic retention: Patients with BPH with prostate size ≤120 cc; IPSS ≥8 with patient and physician agreement that symptoms justified intervention; low urinary flow rate <15, <13, or <10 mL/s when voided volume was >200, 150–200, and 100–149 mL respectively | 40.7 (19.9) 49.7 (21.8) |
7.5 months | VLAP: 38 TURP: 44 |
| Donovan et al. 2000 (69) Multicentre trial (ClasP trial) 3-arm |
234 (117, 117) Plus conservative management arm = 106 |
ClasP trial symptomatic patients: No acute or chronic urinary retention: Patients with BPH with prostate size ≤120 cc; IPSS ≥8 with patient and physician agreement that symptoms justified intervention; low urinary flow rate <15, <13, or <10 mL/s when voided volume was >200, 150–200, and 100–149 mL respectively | VLAP: 38.1 (19.1) TURP: 40.7 (21.4) |
7.5 months | VLAP: 116 TURP: 115 |
BPH refers to benign prostatic hyperplasia; IPSS, International Prostate Symptom Score; NR, not reported; SD, standard deviation; TURP, transurethral resection of the prostate; VLAP, visual laser ablation of the prostate
Table 12: Subjective Measures of Effectiveness, Visual Laser Ablation Versus Transurethral Resection of the Prostate.
| Study, Year | IPSS, Mean (SD) | QOL score, Mean (SD) | ||
|---|---|---|---|---|
| Baseline | 7.5 months | Baseline | 7.5 months | |
| Chacko et al. 2001(67) VLAP TURP |
17.6 (9.3) 19.4 (7.6) |
Mean change in quantitative scores (95% CI) ™10.06 (™12.80 to ™7.31) 13.52 (™15.81 to ™11.23) P =.26 Categorical version * Adjusted OR (95% CI): 2.14 (0.81–5.65) P =.12 |
Median 5 (4.6) 5 (4.6) |
Mean change (95% CI) -3.10 (-3.65 to -2.55) -3.42 (-3.89 to -2.95) |
| Gujral et al. 2000 (68) VLAP TURP |
20.9 (6.4) 19.5 97.2) |
Mean change in quantitative scores (95% CI) -12.2 (-15.7 to -8.7) -14.2 (-17.2 to -11.2) P = .048 Categorical version* Adjusted OR (95% CI): 3.9 (1−14.3) Favour TURP |
Median 5 (2.6) 4.5 (2.6) |
Mean change (95% CI) -2.8 (-3.4 to -2.1) -3.2 (-3.9 to -2.6) P = .97 |
| Donovan et al. 2000 (69) VLAP TURP |
19.2 (6.7) 19.1 (6.6) |
Mean change in quantitative scores (95% CI) -10.8 (-12.5 to -9) -12.3 (-13.8 to -10.7) P >.05 Categorical version* OR (95% CI): 2.4 (1.2–4.6) P <.05 Favour TURP |
Median 4 4 |
Mean change (95% CI) -1.9 (-2.3 to -1.6) -2.2 (-2.5 to -1.8) |
Categories of good, moderate, poor
IPSS refers to International Prostate Symptom Score; NR, not reported; QOL, quality of life; SD, standard deviation; TURP, transurethral resection of the prostate; VLAP, visual laser ablation of the prostate
Table 13: Objective Measures of Effectiveness, Visual Laser Ablation Versus TURP.
| Study, Year | Peak urinary flow (Qmax), Mean (SD), mL/s | Postvoid residual urine, Mean (SD), mL | ||
|---|---|---|---|---|
| Baseline | 7.5 months | Baseline | 7.5 months | |
| Chacko et al. 2001(67) VLAP TURP |
NR |
Adjusted difference between means at follow-up (95% CI) 4.37 mL/s (1.11–7.62) P =.0097 (Favour TURP) Categorical version* Relative risk (95% CI) 3.44 (1.65–7.16) P =.0007 (Favour TURP) |
NR | Adjusted difference between means at follow-up: ™3.70 (95% CI, -30.53 to 23.14) in favour of TURP |
| Gujral et al. 2000 (68) VLAP TURP |
11.2 (5.3) 8.5 (3.6) |
Mean change in quantitative scores (95% CI) 5.7 (2.6 to 8.8) 9.4 (6.5 to 12.2) P =.59 Categorical version* OR (95% CI): 2.9 (1.1–7.8) P =.029 Favour TURP |
438 (151) 545 (275) |
-329 (-377 to -281) -464 (-553 to -374) P =.19 |
| Donovan et al. 2000 (69) VLAP TURP |
10.4 (2.9) 10.3 (2.7) |
Mean change in quantitative scores (95% CI) 5.8 9.7 P <.05 Favour TURP |
104.2 (69.5) 123.7 (91.8) |
-73.4 -74 |
Categories of good, moderate, poor
CI refers to confidence interval; NR, not reported; Qmax, maximum urinary flow; SD, standard deviation; TURP, transurethral resection of the prostate; VLAP, visual laser ablation of the prostate
Table 14: Perioperative Outcomes: Visual Laser Ablation Versus TURP.
| Study, Year | Operative time Mean (%), Min | Hospital stay Mean (%), Days | Catheterization time Mean (%), Hours | Hemoglobin decrease, Mean, g/dL | Transfusion, N (%) | Intraoperative irrigant requirement, Mean (%), L | TUR syndrome No. N (%) |
|---|---|---|---|---|---|---|---|
| Chacko et al. 2001 (67) VLAP TURP |
NR | Geometric mean 3.4 5.8 (The ratio of geometric mean1.73 (95% CI, 1.40–2.14) P < .0001) |
Geometric mean 727 77 (The ratio of geometric mean 9.40 (95% CI, 7.04–12.5.) P < .0001) |
NR | 0 4 |
NR | 0 2 |
| Gujral et al. 2000 (68) VLAP TURP |
NR | Geometric mean 2.2 4.4 The ratio of geometric means2.01 (95% CI, 1.54–2.61) P < .0001 |
Geometric mean 612 72 The ratio of geometric means 8.62 (95% CI, 6.04–12.29) P < .0001 |
NR | 0 3 |
NR | 0 0 |
| Donovan et al. 2000 (69) VLAP TURP |
NR | Geometric mean 2.2 3.9 The ratio of geometric means 1.83 (95% CI, 1.58–2.11) P < .0001 |
Geometric mean 283 57.6 The ratio of geometric means 4.79 (95% CI, 3.88–5.91) P < .0001 |
NR | 1 1 |
NR | 0 0 |
CI refers to confidence interval; NR, not reported; Qmax, maximum urinary flow; TURP, transurethral resection of the prostate; VLAP, visual laser ablation of the prostate
Table 15: Postoperative and Long-term Adverse Events: Visual Laser Ablation Versus TURP.
| RCT | Urinary complications | Sexual dysfunction | Reoperation N (%) | Mortality N (%) | |||
|---|---|---|---|---|---|---|---|
| Urinary retention N (%) | Bladder neck/urethral stricture N (%) |
Incontinence N (%) | Impotence N (%) | Retrograde ejaculation N (%) | |||
| Chacko et al. 2001 (67) VLAP TURP |
0 0 |
0 0 |
0 3 |
NR | NR | 7 1 P =.029 |
2 4 (all unrelated to the procedure) |
| Gujral et al. 2000 (68) VLAP TURP |
NR | NR | NR | NR | NR | 3 0 P =.0014 |
0 1 (unrelated to the procedure) |
| Donovan et al. 2000 (69) VLAP TURP |
NR | NR | NR | NR | NR | 0 0 |
5 (not related to the procedure) 0 |
NR refers to not reported; TURP, transurethral resection of the prostate; VLAP, visual laser ablation of the prostate
Contact Laser Vaporization (CLV)
Table 16: Patient Characteristics: Contact Laser Vaporization Versus TURP.
| Study, Year | Patients, No (Treatment, control) | Inclusion criteria | Prostate size Mean (SD), mL | Mean follow-up (Years) | No available for follow-up |
|---|---|---|---|---|---|
| Tuhkanen et al. 2003 (70) | 52 (26, 26) |
Patients with symptomatic BPH with prostate size <40 mL; BOO confirmed by pressure-flow studies | CLV: 30 TURP: 28 NS |
4 | CLV: 22 TURP: 20 |
| Van Melick et al. 2003 (54) 3-arm study |
95 (45, 50) Third arm received TUVP, n=46 |
Patients older than 45 years of age and LUTS due to BPH (Schafer’s obstruction grade ≥2) and prostate volume 20–65 cm3 | CLV: 37 (11) TURP: 37 (11) |
CLV 1–4 year: 2.6 (0.(0 4–7 years 5.5 (0.7) TURP 1–4 years: 2.7 (0.8) 4–7 years: 5.7 (0.8) |
1 year CLV: 37 TURP: 41 1–4 years CLV: 10 TURP: 15 4–7 years CLV: 27 TURP: 30 |
| Keoghane et al. 2000 (34) | 148 (72, 76) |
Patients with BPH presenting for TURP | NR | 3 |
1 year CLV: 58 TURP: 64 2 years CLV:47 TURP: 53 3 years CLV: 43 TURP: 44 |
BBO refers to bladder outlet obstruction; BPH, benign prostatic hyperplasia; CLV, contact laser vaporization; LUTS, lower urinary tract symptoms; NR, not reported; SD, standard deviation; TURP, transurethral resection of the prostate; TUVP, Transurethral electrovaporization of the prostate
Table 17: Subjective Measures of Effectiveness: Contact Laser Vaporization Versus TURP.
| Study, Year | IPSS, Mean (SD) | QOL score, Mean (SD) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 3 months | 6 months | 12 months | > 1 year | Baseline | 3 months | 6 months | 12 months | > 1 year | ||
| Tuhkanen et al. 2003 (70) CLV TURP |
Median DANPSS-1 18 18 |
Graph only | Graph only | Graph only | Median DANPSS-1 5 4 |
NR | NR | NR | NR | NR | |
| Van Melick et al. 2003 (54) CLV TURP |
18.3 98.2) 16.6 (5.6) |
NR | 5.9 (5.5) 3.2 (2.7) |
3.6 (3.4) 4.1 (4.8) P >.05 |
1–4 years 9.3 (5.2) 5.8 (7.5) P >.05 4–7 years 8.3 (6.4) 7.3 (7.1) P >.05 |
3.6 (1.6) 3.9 (1.6) |
NR | 0.8 (1) 0.5 (0.5) |
0.6 (0.9) 0.6 (0.8) |
1–4 years 2 (1) 1.1 (1.2) 4–7 years 1.4 (1.2) 1.3 (1.3) |
|
| Keoghane et al. 2000 (34) CLV TURP |
19.9 (7.7) 19.4 (6.5) |
NR | NR | 8.7 (6.5) 5.8 (5.4) P =.006 |
2 years 7.8 (6.6) 5.7 (6) P =.018 3 years 8.9 (6.6) 6.5 (6.5) P =.001 |
NR | NR | NR | NR | NR | |
CLV refers to contact laser vaporization; DANPSS, Danish prostate symptom score; IPSS, International Prostate Symptom Score; NR, not reported; QOL, quality of life; SD, standard deviation; TURP, transurethral resection of the prostate
Table 18: Objective Measures of Effectiveness. Contact Laser Vaporization Versus TURP.
| Study, Year | Peak urinary flow (Qmax), Mean (SD), mL/s | Postvoid residual urine, Mean (SD), mL | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 3 months | 6 months | 1 year | > 1 year | Baseline | 3 months | 6 months 1 year | 1 year | > 1 year | ||
| Tuhkanen et al. 2003 (70) CLV TURP |
Median 8.3 8.6 |
Graph only | Graph only | Graph only |
Median 14.3 16.1 |
Median 87 83 |
Graph only | Graph only | Graph only |
Median 60 10 P <.05 |
|
| Van Melick et al. 2003 (54) CLV TURP |
9 (3) 13 (4) |
NR | 25 (9) 26 (6) |
27 (12) 23 (10) P >.05 |
1–4 years 19 (6) 20 (5) P >.05 4–7 years 19 (9) 17 (8) P >.05 |
NR | NR | NR | NR | NR | |
| Keoghane et al. 2000 (34) CLV TURP |
11.8 (4.5) 11.4 (5) |
NR | NR | 17.1 (13.2) 21.2 (12.4) |
Median 2 years 14.2 (7.4) 15.9 (8) 3 years 13.4 (7.3) 12.7 (6.4) |
NR | NR | NR | NR | NR | |
CLV refers to contact laser vaporization; NR, not reported; SD, standard deviation; TURP, transurethral resection of the prostate
Table 19: Perioperative Outcomes: Contact Laser Vaporization Versus TURP.
| Study, Year | Operative time Mean (SD), Min | Hospital stay Mean (Sd), Days | Catheterization time Mean (SD), Hours | Hemoglobin decrease, Mean (SD), g/dL | Transfusion, N (%) | Intraoperative irrigant requirement, Mean (SD), L | TUR syndrome, N (%) |
|---|---|---|---|---|---|---|---|
| Tuhkanen et al. 2003 (70) CLV TURP |
51 34 P <.001 |
3.4 2.9 NS |
103 41 P <.01 |
1.2 1 NS |
0 0 |
14.1 12.3 NS |
0 0 |
| Van Melick et al. 2003 (54) CLV TURP |
58 (11) 58 (26) P =.09 |
3.8 (1.3) 3.9 (0.9) NS |
67.2 (74.4) 50.4 (16.8) NS |
0.32 1.29 |
0 1 |
18 (4) 16 (7) P =.01 |
0 0 |
| Keoghane et al. 2000 (34) CLV TURP |
35 39.3 |
3.5 3.9 |
24 48 |
NR | NR | NR | 0 0 |
CLV refers to contact laser vaporization; NR, not reported; NS, not significant; SD, standard deviation; TUR, transurethral resection; TURP, transurethral resection of the prostate
Table 20: Postoperative and Long-term Adverse Events. Contact Laser Vaporization Versus TURP.
| RCT | Urinary complications | Sexual dysfunction | Reoperation N (%) | Mortality N (%) | |||
|---|---|---|---|---|---|---|---|
| Urinary retention N (%) | Bladder neck/urethral stricture N (%) |
Incontinence N (%) | Impotence N (%) | Retrograde ejaculation N (%) | |||
| Tuhkanen et al. 2003 (70) CLV TURP |
NR | 0 1 |
NR | NR | NR | 1 1 |
CLV: 3 TURP: 1 (all unrelated causes) |
| Van Melick et al. 2003 (54) CLV TURP |
5 0 |
2 3 |
18 (39%) 4 (8%) |
NR | NR | 3 3 |
3 2 |
| Keoghane et al. 2000 (34) CLV TURP |
Recatheterization 17 (28%) 9 (12%) P <.05 |
0 5 |
NR | NR | Similar | 13 (18) 7 (9) |
5 (7%) 5 (6.6%) |
CLV refers to contact laser vaporization; NR, not reported; TURP, transurethral resection of the prostate
Interstitial Laser Coagulation (ILC)
Table 21: Patient Characteristics. Interstitial Laser Coagulation Versus TURP.
| Study, Year | Patients, No (Treatment, control) | Inclusion criteria | Prostate size Mean (SD), mL | Mean follow-up (Years) | No. available for follow-up |
|---|---|---|---|---|---|
| Kursh et al. 2003 (37) Multicentre trial |
72 (37, 35) |
Patients with BPH with prostate size ≤75 cc; IPSS≥13; Qmax <15 for 2 seconds; PVR 30–300 mL; prostatic length ≥1.5 cm | ILC: 41.5 TURP: 40 NS |
2 | ILC: 28 TURP: 30 |
| Liedberg et al. 2003 (71) | 31 (20, 11) |
Patients with moderate to severe symptomatic BPH; IPSS≥12; Qmax ≤15 mL/s | NR | 1 | NR |
| Norby et al. 2002 (56) 3-arm study, 2 centres |
72 (48, 24) Third arm: 46 to TUMT |
Patients with BPH 50 years or older; IPSS ≥ 7; QOL ≥ 3; Qmax <12 mL/s | ILC: 44 TURP: 44 |
0.5 | 44 22 |
BPH refers to benign prostatic hyperplasia; ILC, interstitial laser coagulation; IPSS, International Prostate Symptom Score; NR, not reported; PVR, postvoid residual; Qmax, maximum flow rate; SD, standard deviation; TURP, transurethral resection of the prostate
Table 22: Subjective Measures of Effectiveness. Interstitial Laser Coagulation Versus TURP.
| Study, Year | IPSS, Mean (SD) | QOL score, Mean (SD) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 3 months | 6 months | 1 year | > 1 year | Baseline | 3 months | 6 months | 12 months | > 1 year | |
| Kursh et al. 2003 (37) ILC TURP |
Median 24 23 NS |
NR |
Median 7 6 NS |
NR |
Median 2 years 9 7 |
Median 11 11 |
NR |
Median 2 2 |
NR |
Median 2 years 3 2 |
| Liedberg et al. 2003 (71) ILC TURP |
19 17 |
10 4 |
Graph only | 11 6 |
NR | NR | NR | NR | NR | NR |
| Norby et al. 2002 (56) ILC TURP |
21.4 (5.8) 21.3 (6.6) |
NR | 9.5 (6.6) 6.8 (5.7) P =.105 |
NR | NR | 4 4 |
NR | 1 1 P =.640 |
NR | NR |
ILC refers to interstitial laser coagulation; IPSS, International Prostate Symptom Score; NR, not reported; QOL, quality of life; SD, standard deviation; TURP, transurethral resection of the prostate
Table 23: Objective Measures of Effectiveness. Interstitial Laser Coagulation Versus TURP.
| Study, Year | Peak urinary flow (Qmax), Mean (SD), mL/s | Postvoid residual urine, Mean (SD), mL | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 3 months | 6 months | 1 year | > 1 year | Baseline | 3 months | 6 months 1 year | 1 year | > 1 year | |
| Kursh et al. 2003 (37) ILC TURP |
Median 9.2 9.1 NS |
NR |
Median 14.3 16.6 NS |
NR |
Median 2 years 13.9 16.5 |
Median 81 87.5 NS |
NR |
Median 42.4 46 |
NR |
Median 2 years 57.7 44 |
| Liedberg et al. 2003 (71) ILC TURP |
8 8 |
11 12 |
Graph only | 11 14 P <.02 |
NR | 96 117 |
74 0 |
NR | 126 22 |
NR |
| Norby et al. 2002 (56) ILC TURP |
10.2 (4) 9.6 (3.2) |
NR | 16.2 (8.5) 20.6 (12.8) P =.104 |
NR | NR | 117 75 |
NR | 58 23 P =.02 |
NR | NR |
ILC refers to interstitial laser coagulation; NR, not reported; Qmax, maximum flow rate; SD, standard deviation; TURP, transurethral resection of the prostate
Table 24: Perioperative Outcomes. Interstitial Laser Coagulation Versus TURP.
| Study, Year | Operative time Mean (SD), Min. | Hospital stay Mean (SD), Days | Catheterization time Mean (SD), Hours | Hemoglobin decrease, Mean (SD), g/dL | Transfusion, N (%) | Intraoperative irrigant requirement, Mean (SD), L | TUR syndrome N (%) |
|---|---|---|---|---|---|---|---|
| Kursh et al. 2003 (37) ILC TURP |
NR |
Median 0.3 1.4 |
NR | NR | 0 0 |
NR | 0 0 |
| Liedberg et al. 2003 (71) ILC TURP |
NR | 2.5 3 |
576 48 P < .001 |
NR | NR | NR | 0 0 |
| Norby et al. 2002 (56) ILC TURP |
NR | Median 3 5 |
Median 312 48 |
NR | 0 2 (9%) |
NR | 0 1 (5%) |
ILC refers to interstitial laser coagulation; NR, not reported; SD, standard deviation; TUR, transurethral resection; TURP, transurethral resection of the prostate
Table 25: Postoperative and Long-term Adverse Events: Interstitial Laser Coagulation Versus TURP.
| RCT | Urinary complications | Sexual dysfunction | Reoperation N (%) | Mortality N (%) | |||
|---|---|---|---|---|---|---|---|
| Urinary retention N (%) | Bladder neck/urethral stricture N (%) |
Incontinence N (%) | Impotence N (%) | Retrograde ejaculation N (%) | |||
| Kursh et al. 2003 (37) ILC TURP |
NR | NR | 0 2 |
Median sexual function score Baseline ILC: 18 TURP: 17 6 months ILC: 19 TURP: 5 2 years ILC: 19.5 TURP: 10 |
6 (16.2%) 0 |
0 1 (unrelated to the procedure) |
|
| Liedberg et al. 2003 (71) ILC TURP |
NR | 0 0 |
NR | NR | 1 3 P = .84 |
0 0 |
NR |
| Norby et al. 2002 (56) ILC TURP |
4 1 |
1 (2%) 1 (2%) |
Stress incontinence 0 1 (5%) |
4 (29%) 1 (14%) |
9 (35%) 7 (50%) P = .343 |
0 0 |
NR |
ILC refers to interstitial laser coagulation; NR, not reported; TURP, transurethral resection of the prostate
Holmium laser resection of the prostate (HoLRP)
Table 26: Patient Characteristics. Holmium Laser Resection of the Prostate Versus TURP.
| Study, Year | Patients, No. (Treatment, control) | Inclusion criteria | Prostate size Mean (SD), mL | Mean follow-up (Year) | No. available for follow-up |
|---|---|---|---|---|---|
| Westenberg et al. 2004 (74) | 120 HoLRP: 61 TURP: 59 |
Age </=80 tears; AUA >/=8; Qmax </=15mL/s; Prostate volume<100cc; PVR<400 mL, Schafer grade or LinPURR >/=2 | TRUS vol.; cc HoLRP: 44.3 (19) TURP: 44.6 (20.7) P =.93 |
4 | 4 years HoLRP: 43 TURP: 30 |
AUA refers to American Urological Association; HoLRP, holmium laser resection of the prostate; LinPURR: Linearized passive urethral resistance relaxation; PVR, postvoid residual; Qmax, maximum urinary flow; TRUS, trans-rectal ultrasound; TURP, transurethral resection of the prostate
Table 27: Subjective Measures of Effectiveness. Holmium Laser Resection of the Prostate Versus TURP.
| Study, Year | IPSS, Mean (SD) | QOL score, Mean (SD) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 3 months | 6 months | 12 months | > 1 year | Baseline | 3 months | 6 months | 12 months | > 1 year | |
| Westenberg et al. 2004 (74) HoLRP TURP |
21.9 (6.2) 23.0 (5.9) P = .32 |
5.6 (5.1) 5.7 (5.2) P = .88 |
3.8 (3.8) 5.0 (4.5) P = .17 |
4.2 (6.0) 4.3 (4.1) P = .92 |
1.5 years 2.9 (5.3) 4.5 (5.3) P = .16 2 years 3.4 (4.9) 3.7 (4.9) P = .84 4 years 5.2 (5.9) 6.6 (5.0) P = .32 |
4.5 (1.1) 4.7 (1.1) P = .45 |
1.4 (1.5) 1.6 (1.4) P = .60 |
1.1 (1.3) 1.5 (1.4) P = .11 |
0.88 (1.4) 1.6 (1.5) P < .05 |
1.5 years 0.72 (1.1) 1.3 91.1) P = .58 2 years 0.98 (1.3) 1.0 (1.3) P = .88 4 years 1.1 (1.1) 1.4 (1.4) P = .37 |
AUA refers to American Urological Association; HoLRP, holmium laser resection of the prostate; IPSS, International Prostate Symptom Score; PVR, postvoid residual; Qmax, maximum urinary flow; QOL, quality of life; SD, standard deviation; TURP, transurethral resection of the prostate
Table 28: Objective Measures of Effectiveness. Holmium Laser Resection of the Prostate Versus TURP.
| Study, Year | Peak urinary flow (Qmax), Mean (SD), mL/s | Postvoid residual urine, Mean (SD), mL | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 3 months | 6 months | 1 year | > 1 year | Baseline | 3 months | 6 months 1 year | 1 year | > 1 year | |
| Westenberg et al. 2004 (74) HoLRP TURP |
8.9 (3.0) 9.1 (3.2) P = .81 |
22.8 (10.0) 20.2 (9.5) P = .16 |
23.9 (8.7) 22.4 (9.0) P = .35 |
25.2 (11.9) 20.4 (8.5) P < .05 |
1.5 years 25.1 (9.3) 19.2 (9.3) P <.01 2 years 25.0 (11.1) 20.9 (11.1) P =.14 4 years 22.3 (14.2) 18.5 (8.2) P =.23 |
87.8 (88.4) 84.7 (81.7) P = .85 |
NR | 26.7 34.3 NS |
NR | NR |
HoLRP refers to holmium laser resection of the prostate; NR, not reported; Qmax, maximum urinary flow; SD, standard deviation; TURP, transurethral resection of the prostate
Table 29: Perioperative Outcomes. Holmium Laser Resection of the Prostate Versus TURP.
| Study, Year | Operative time Mean (SD), Min | Hospital stay Mean (SD), Days | Catheterization time Mean (SD), Hours | Hemoglobin decrease, Mean (SD), g/dL | Transfusion, N (%) | Intraoperative irrigant requirement, Mean (SD), L | TUR syndrome N (%) | Irritating voiding symptoms |
|---|---|---|---|---|---|---|---|---|
| Westenberg et al. 2004 (74) HoLRP TURP |
Significantly longer in HoLRP (values not reported) | 1.1 (0.5) 1.98 (0.7) P < .001 |
20.0 (11.39) 37.2 (15.92) P < .001 |
NR | 0 4 |
NR | 0 0 |
NR |
HoLRP refers to holmium laser resection of the prostate; NR, not reported; SD, standard deviation; TUR, transurethral resection; TURP, transurethral resection of the prostate
Table 30: Postoperative and Long-term Adverse Events. Holmium Laser Resection of the Prostate Versus TURP.
| RCT | Urinary complications | Sexual dysfunction | Reoperation N (%) | Mortality N (%) | |||
|---|---|---|---|---|---|---|---|
| Urinary retention N (%) | Bladder neck/urethral stricture N (%) |
Incontinence N (%) | Impotence N (%) | Retrograde ejaculation N (%) | |||
| Westenberg et al. 2004 (74) HoLRP TURP |
Recatheterization 5 8 |
6 6 |
2 1 |
5 (8%) 10 (17%) |
NR | 1 4 |
2 7 (all unrelated causes) |
HoLRP refers to holmium laser resection of the prostate; NR, not reported; TURP, transurethral resection of the prostate
Holmium Laser Enucleation of the Prostate (HoLEP)
Table 31: Patient Characteristics: Holmium Laser Enucleation of the Prostate Versus TURP.
| Study, Year | Patients, No. (Treatment, control) | Inclusion criteria | Prostate size Mean (SD), mL | Mean follow-up Years (months where specified) | No. available for follow-up |
|---|---|---|---|---|---|
| Rigatti et al. 2006 (72) | 100 (52, 48) |
Patients with BPH younger than 72 years; prostate size 30–100 gr; Qmax <15 mL/s; PVR <100 mL, medical therapy failure; Schafer >2; obstruction on the International Continence Society nomogram, and Abram-Griffiths >40 | HoLEP: 60.3 (36.7) TURP: 56.2 (19.4) P =.05 |
1 | All |
| Gupta et al. 2006 (55) 3-arm study |
100 (50, 50) Plus 50 patients in TUVRP group |
Patients with BPH who were candidates for TURP and gland size of >40 g | HoLEP: 57.9 (17.6) TURP: 59.8 (16.5) |
1 | NR |
| Kuntz et al. 2004 (39) | 200 (100, 100) |
Patients with BPH who had AUA symptom score ≥12; Qmax ≤12mL/s; PVR>50mL; Schafer grade ≥ 2; Prostate volume <100 cc | HoLEP: 53.5 (20.0) TURP: 49.9 (21.1) |
1 | HoLEP: 89 TURP: 86 (13 patients with incidental carcinoma and 8 who developed stricture were excluded from analysis) |
| Tan et al. 2003 (40) | 61 (31, 30) |
Patients with BPH who had prostate volume 40–200 mL; Qmax </=15 mL/s; AUA score >/=8; PVR <400 mL; Schafer grade ≥2 | HoLEP: 77.8 (5.6) TURP: 70.0 (5.0) |
1 | HoLEP: 25 TURP: 27 |
AUA refers to American Urological Association; BPH, benign prostatic hyperplasia; HoLEP, holmium laser enucleation of the prostate; NR, not reported; PVR, postvoid residual; Qmax, maximum flow rate; TURP, transurethral resection of the prostate
Table 32: Subjective Measures of Effectiveness. Holmium Laser Enucleation of the Prostate Versus TURP.
| Study, Year | IPSS, Mean (SD) | QOL score, Mean (SD) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 3 months | 6 months | 12 months | > 1 year | Baseline | 3 months | 6 months | 12 months | > 1 year | |
| Rigatti et al. 2006 (72) HoLEP TURP |
21.6 (6.7) 21.9 (7.2) P =.83 |
NR | 3.9 (2.9) 2.9 (2.6) P =.72 |
4.1 (2.3) 3.9 (3.6) P = .58 |
NR | 4.6 (1.1) 4.7 (1) P = .7 |
NR | 1 (8) 0.6 (0.2) P =.25 |
1.4 (0.9) 0.8 (1.28) P =.31 |
NR |
| Gupta et al. 2006 (55) HoLEP TURP |
23.4 (4.5) 23.3 (3.9) P > .05 |
NR | 5.2 (0.31) 6.1 (0.42) P > .05 |
5.2 (0.17) 5.6 (0.32) P > .05 |
NR | NR | NR | NR | NR | NR |
| Kuntz et al. 2004 (39) HoLEP TURP |
22.1 (3.8) 21.4 (5.2) P =.56 |
NR | 2.2 (1.6) 3.7 (3.4) P =.006 |
1.7 (1.8) 3.9 (3.9) P =.0001 |
NR | NR | NR | NR | NR | NR |
| Tan et al. 2003 (40) HoLEP TURP |
26.0 (1.1) 23.7 (1.2) P >.05 |
4.8 (0.8) 3.4 (0.9) P >.05 |
6.0 (1.0) 4.8 (0.7) P >.05 |
4.3 (0.7) 5.0 (0.9) P >.05 |
NR | 4.8 (0.2) 4.7 (0.2) P >. 05 |
1.8 (0.4) 1.9 (0.6) P >.05 |
1.6 (0.3) 1.5 (0.2) P >.05 |
1.5 (0.5) 1.4 (0.3) P >.05 |
NR |
HoLEP refers to holmium laser enucleation of the prostate; IPSS, International Prostate Symptom Score; NR, not reported; QOL, quality of life; SD, standard deviation; TURP, transurethral resection of the prostate
Table 33: Objective Measures of Effectiveness. Holmium Laser Enucleation of the Prostate Versus TURP.
| Study, Year | Peak urinary flow (Qmax), Mean (SD), mL/s | Postvoid residual urine, Mean (SD), mL | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 3 months | 6 months | 1 year | > 1 year | Baseline | 3 months | 6 months | 1 year | > 1 year | |
| Rigatti et al. 2006 (72) HoLEP TURP |
8.2 (3.2) 7.8 (3.6) P = .61 |
NR | 23.1 (8.6) 26.5 (15.5) P = .007 |
25.1 (7.2) 24.7 (10) P = .25 |
NR | NR | NR | NR | NR | NR |
| Gupta et al. 2006 (55) HoLEP TURP |
5.15 (4.4) 4.5 (4.7) P > .05 |
NR | 23.1 (1.2) 20.7 (1.32) P > .05 |
25.1 (1.06) 23.7 (1.58) P > .05 |
NR | 112 (155.9) 84 (129.7) P > .05 |
NR | <20 <20 |
<20 <20 |
NR |
| Kuntz et al. 2004 (39) HoLEP TURP |
4.9 (3.8) 5.9 (3.9) P = .08 |
NR | 25.1 (6.9) 25.1 (9.4) P = .72 |
27.9 (9.9) 27.7 (12.2) P = .76 |
NR | 237 (163) 216 (177) P = .08 |
NR | 4.8 (12.5) 16.7 (16.9) P < .0001 |
5.3 (15.3) 26.6 (60.4) P < .0001 |
NR |
| Tan et al. 2003 (40) HoLEP TURP |
8.4 (0.5) 8.3 (0.4) P > .05 |
24.2 (1.7) 18.9 (1.9) P > .05 |
26.4 (1.8) 20.8 (2.3) P > .05 |
21.8 (2.1) 18.4 (2.8) P > .05 |
NR | 113.5 (15.5) 126.7 (21.3) P > .05 |
NR | 33.7 (5.5) 51.8 (14.5) P > .05 |
NR | NR |
HoLEP refers to holmium laser enucleation of the prostate; NR, not reported; Qmax, maximum urinary flow; SD, standard deviation; TURP, transurethral resection of the prostate
Table 34: Perioperative Outcomes. Holmium Laser Enucleation of the Prostate Versus TURP.
| Study, Year | Operative time Mean (SD), Min | Hospital stay Mean (SD), Days | Catheterization time Mean (SD), Hours | Hemoglobin decrease, Mean (SD), g/dL | Transfusion N (%) | Intraoperative irrigant requirement, Mean (SD), L | TUR syndrome N (%) | Irritative urinary symptoms |
|---|---|---|---|---|---|---|---|---|
| Rigatti et al. 2006 (72) HoLEP TURP |
74 (19.5) 57 (15) P < .05 |
2.46 (0.83) 3.56 (0.79) P < .001 |
31 (13) 57.78 (17.5) P < .001 |
1.32 (1.8) 1.29 (2.1) P = .14 |
NR (Equivalent bleed loss) |
NR | 0 1 |
33 (58.9) 13 (29.5) P = .0002 |
| Gupta et al. 2006 (55) HoLEP TURP |
75.4 (22.8) 64.1 (13.1) P < .001 Between 3 arms |
NR | 28.6 (20.5) 45.7 (12.7) P < .001 Between 3 arms |
0.83 (0.7) 1.1 (0.8) |
0 1 (2%) P < .001 |
26.9 (8.5) 24.2 (11.8) P < .001 Between 3 arms |
0 0 |
5 1 P < .03 Between 3 arms |
| Kuntz et al. 2004 (39) HoLEP TURP |
94.6 (35.1) 73.8 (24.0) P < .0001 |
2.2 (0.6) 3.6 (1.6) P < .0001 |
27.6 (10.4) 43.4 (21.1) P < .0001 |
1.3 (1.0) 1.8 (1.4) P = .01 |
0 2 P = .5 |
NR | NR | NR |
| Tan et al. 2003 (40) HoLEP TURP |
109.5 61.3 |
1.15 (0.11) 2.08 (0.23) P < .001 |
17.7 (0.7) 44.9 (10.1) P < .01 |
NR | 0 1 |
23.4 (2.5) 14.0 (1.6) P < .01 |
NR | NR |
Mean decrease in hemoglobin unless otherwise stated;
HoLEP refers to holmium laser enucleation of the prostate; NR, not reported; Qmax, maximum urinary flow; SD, standard deviation; TURP, transurethral resection of the prostate
Table 35: Postoperative and Long Term Complications. Holmium Laser Enucleation of the Prostate Versus TURP.
| RCT | Urinary complications | Sexual dysfunction | Reoperation N (%) | Mortality N (%) | |||
|---|---|---|---|---|---|---|---|
| Urinary retention N (%) | Bladder neck/urethral stricture N (%) |
Incontinence N (%) | Impotence N (%) | Retrograde ejaculation N (%) | |||
| Rigatti et al. 2006 (72) HoLEP TURP |
Recatheterization 3 (5.3) 1 (2.2) |
2 (3.8) 4 (7.4) |
Transitory Urge incontinence HoLEP: 25 (44) TURP: 17 (38.6) Stress incontinence HoLEP: 1 (1.7) TURP: 1 (2.2) |
NR | NR | NR | NR |
| Gupta et al. 2006 (55) HoLEP TURP |
Recatheterization 2 3 P =.62 Between 3 arms |
1 2 |
1 1 |
NR | NR | NR | 0 1 (Pneumonia) |
| Kuntz et al. 2004 (39) HoLEP TURP |
0 5 (5) P =.06 |
6 (6.4) 2 (2.2) P =.62 |
Stress incontinence 1 (1.1) 1 (1.1) NS |
10 (11.2) 9 (10.5) P =NR |
66 (74) 61 (70.3) P =NR |
NR | 0 0 |
| Tan et al. 2003 (40) HoLEP TURP |
Recatheterization 5 4 |
1 3 |
15 (48%) 11 33% |
NR | NR | 0 2 |
1 (preoperation) 1 (cardio.) |
HoLEP refers to holmium laser enucleation of the prostate; NR, not reported; TURP, transurethral resection of the prostate
Holmium Laser Enucleation of the Prostate versus Open Prostatectomy
Table 36: Patient Characteristics. Holmium Laser Enucleation of the Prostate (HoLEP) Versus Open Prostatectomy.
| Study, Year | Patients, No. (Treatment, control) | Inclusion criteria | Prostate size Mean (SD), mL | Mean follow-up Years (months where specified) | No. available for follow-up |
|---|---|---|---|---|---|
| Kuntz et al. 2004 (73) | 120 (60, 60) |
Schafer grade > 3; AUA symptom score ≥ 8; Qmax ≤ 12 mL/s; PVR≥ 50mL; Schafer grade ≥ 3; Prostate size ≥ 100g | HoLEP: 114.6 (21.6) Open: 113 (19.2) P = .60 |
18 months | HoLEP: 50 Open: 44 |
AUA refers to American Urological Association; HoLEP, holmium laser enucleation of the prostate; Open, open prostatectomy; PVR, postvoid residual; Qmax, maximum urinary flow; SD, standard deviation
Table 37: Subjective Outcome Measures of Effectiveness. Transurethral Holmium Laser Enucleation of the Prostate (HoLEP) Versus Open Prostatectomy.
| Study, Year | IPSS, Mean (SD) | QOL score, Mean (SD) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 3 months | 6 months | 12 months | > 1 year | Baseline | 3 months | 6 months | 12 months | > 1 year | |
| Kuntz et al. 2004 (73) HoLEP Open |
22.1 (3.3) 21.0 (3.6) |
3.3 (2.7) 3.6 (2.7) |
2.4 (1.9) 2.8 (3.9) |
2.3 (2.0) 2.0 (1.7) |
NR | NR | NR | NR | NR | NR |
HoLEP refers to holmium laser enucleation of the prostate; IPSS, International Prostate Symptom Score; NR, not reported; Open, open prostatectomy; QOL, quality of life; SD, standard deviation
Table 38: Objective Outcome Measures of Effectiveness. Transurethral Holmium Laser Enucleation of the Prostate (HoLEP) Versus Open Prostatectomy.
| Study, Year | Peak urinary flow (Qmax), Mean (SD), mL/s | Postvoid residual urine, Mean (SD), mL | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 3 months | 6 months | 1 year | > 1 year 18 months | Baseline | 3 months | 6 months | 1 year | > 1 year 18 months | |
| Kuntz et al. 2004 (73) HoLEP |
3.8 +/-3.6 | 27.6 +/-7.0 | 29.9 +/-8.8 | 27.4 +/-9.7 | 27.4 +/-10.6 28.0 +/-5.7 |
280 +/-273 | 7.2 +/-18.8 3.0 +/-7.7 |
4.4 +/-11.0 2.1 +/-6.0 |
5.8 +/- 16.7 6.4 +/-12.3 |
7.1 +/-19.6 6.0 +/-11.7 |
| Open | 3.6 +/-3.8 | 27.3 +/-6.2 | 27.0 +/-0.5 | 28.8 +/-7.5 | 292 +/- 191 | |||||
HoLEP refers to holmium laser enucleation of the prostate; NR, not reported; Open, open prostatectomy; Qmax, maximum urinary flow; SD, standard deviation
Table 39: Perioperative Outcomes. Transurethral Holmium Laser Enucleation of the Prostate (HoLEP) Versus Open Prostatectomy.
| Study, Year | Operative time Mean (SD), Min | Hospital stay Mean (SD), Days | Catheterization time Mean (SD), Hours | Hemoglobin decrease, Mean (SD), g/dL | Transfusion, N (%) | Intraoperative irrigant requirement, Mean (SD), L | TUR syndrome N (%) |
|---|---|---|---|---|---|---|---|
| Kuntz et al. 2004 (73) HoLEP |
NR | NR | |||||
| Open | 135.9 +/-31.2 (80–216) 90.6 +/-19.5 (55–135) P < .0001 |
2.9 (1.3) 10.46 (1.9) P < .0001 |
30.8+/-17.3 (24–144) 194.4 +/-20.2 (168–288) P < .0001 |
1.9+/-1.3 (0.0–6.5) 2.8 +/-1.6 (0.6–6.9) P < .0001 |
0 8 (13.3) P =.003 |
Mean decrease in hemoglobin unless otherwise stated;
HoLEP refers to holmium laser enucleation of the prostate; NR, not reported; Open, open prostatectomy; SD, standard deviation
Table 40: Postoperative and Long Term Complications. Transurethral Holmium Laser Enucleation (HoLEP) Versus Open Prostatectomy.
| RCT | Urinary complications | Sexual dysfunction | Reoperation N (%) | Mortality N (%) | |||
|---|---|---|---|---|---|---|---|
| Urinary retention N (%) | Bladder neck/urethral stricture N (%) |
Incontinence N (%) | Impotence N (%) | Retrograde ejaculation N (%) | |||
| Kuntz et al. 2004 (73) HoLEP |
NR | NR | NR | ||||
| Open | 2 | 70% | 5 | NR | |||
| 2 | 79% | 3 | 1 | ||||
HoLEP refers to holmium laser enucleation of the prostate; NR, not reported; Open, open prostatectomy
Laser Prostatectomy using Potassium Titanyl Phosphate (KTP)/Nd:YAG
Table 41: Patient Characteristics. Laser Prostatectomy using Potassium Titanyl Phosphate (KTP) Versus TURP.
| Study, Year | Patients, No (Treatment, control) | Inclusion criteria | Prostate size Mean (SD), mL | Mean follow-up (Months) | No available for follow-up |
|---|---|---|---|---|---|
| Shingleton 2002 (75) | 100 (50, 50) |
Patients with BPH >45 years old; medical therapy failure; Qmax, 15 mL/s; ability to tolerate regional or general anesthesia | PVP: 32.2 (21.4) TURP: 29.6 (15.4) | 3 |
1 year KTP/Nd:YAG: 40 TURP: 33 1.5–2 years KTP/Nd:YAG :23 TURP: 19 3–6 years KTP/Nd:YAG :29 TURP: 33 |
BPH refers to benign prostatic hyperplasia; KTP, potassium titanyl phosphate; PVP, photoselective vaporization of the prostate; Qmax, maximum urinary flow; TURP, transurethral resection of the prostate
Table 42: Subjective Measures of Effectiveness. Laser Prostatectomy using Potassium Titanyl Phosphate (KTP) Versus TURP.
| Study, Year | IPSS, Mean (SD) | QOL score, Mean (SD) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 3 months | 6 months | 1 year | > 1 year | Baseline | 3 months | 6 months | 1 year | > 1 year | |
| Shingleton 2002 (75) KTP/Nd:YAG TURP |
22.5 (6) 21.2 (6.1) |
7 (48) 4 (48) P =.011 |
7 (46) 4 (48) P =.011 |
7 (43) 3 (35) P =.011 |
1.5–2 years 5.9 (5.7) 4.6 (4.2) 3–6 years 9.9 (6.7) 7.7 (5.6) P >.05 |
NR | NR | NR | NR | NR |
IPSS refers to International Prostate Symptom Score; KTP, potassium titanyl phosphate; QOL, quality of life; TURP, transurethral resection of the prostate
Table 43: Objective Measures of Effectiveness. Laser Prostatectomy using Potassium Titanyl Phosphate (KTP) Versus TURP.
| Study, Year | Peak urinary flow (Qmax), Mean (SD), mL/s | Postvoid residual urine, Mean (SD), mL | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 3 months | 6 months | 1 year | > 1 year | Baseline | 3 months | 6 months | 1 year | > 1 year | |
| Shingleton 2002 (75) KTP/Nd:YAG TURP |
8.2 (3.2) 7.3 (3.7) |
15 (5.7) 16 (0.8) P =.6 |
15.8 (6.9) 16.3 (6.4) P =.77 |
14.6 (5.9) 16.2 (7.2) P > .05 |
1.5–2 years 14.9 (5.4) 14.3 (6.3) 3–6 years 12.3 (5.3) 12.8 (5.6) |
NR | NR | NR | NR | NR |
KTP refers to potassium titanyl phosphate; NR, not reported; Qmax, maximum urinary flow; TURP, transurethral resection of the prostate
Table 44: Perioperative Outcomes. Laser Prostatectomy using Potassium Titanyl Phosphate (KTP) Versus TURP.
| Study, Year | Operative time Mean (SD), Min | Hospital stay Mean (SD), Days | Catheterization time Mean (SD), Hours | Hemoglobin decrease, Mean (SD), g/dL | Transfusion, N (%) | Intraoperative irrigant requirement, Mean (SD), L | TUR syndrome N (%) |
|---|---|---|---|---|---|---|---|
| Shingleton 2002 (75) KTP/Nd:YAG TURP |
NR | NR | NR | 0.6 0.8 |
0 0 |
NR | 0 0 |
KTP refers to potassium titanyl phosphate; NR, not reported; SD, standard deviation; TUR; transurethral resection; TURP, transurethral resection of the prostate
Table 45: Postoperative and Long-term Adverse Events. Laser Prostatectomy using Potassium Titanyl Phosphate (KTP) Versus TURP.
| RCT | Urinary complications | Sexual dysfunction | Reoperation N (%) | Mortality N (%) | |||
|---|---|---|---|---|---|---|---|
| Urinary retention N (%) | Bladder neck/urethral stricture N (%) |
Incontinence N (%) | Impotence N (%) | Retrograde ejaculation N (%) | |||
| Shingleton 2002 (75) KTP/Nd:YAG TURP |
3 1 |
3 1 |
1 1 |
15–19 (30–37.5) Minimal change |
2 2 |
3 (6%) 0 |
NR |
KTP refers to potassium titanyl phosphate; NR, not reported; TURP, transurethral resection of the prostate
Transurethral Microwave Thermotherapy (TUMT)
Table 46: Patient Characteristics. Transurethral Microwave Thermotherapy (TUMT) Versus TURP.
| Study, Year | Patients, No. (Treatment, control) | Inclusion criteria | Prostate size Mean (SD), mL | Mean follow-up Years (months where specified) | Equipment and software | No. available for follow-up |
|---|---|---|---|---|---|---|
| Wagrell, et al. 2004 & 2002 (76;79) (Multicentre trial) |
146 (100, 46) |
Symptomatic BPH, prostate size 30–100cm3; IPSS≥13; Qmax < 13mL/s | TUMT: 48.9 (15.8) TURP: 52.7 (17.3) |
3 | ProstaLund Feedback Treatment (PLFT) using Core Therm device |
3 years TUMT: IPSS: 68; QoL: 68; Qmax: 66; PVR: 68 TURP: IPSS: 35; QoL: 35; Qmax:34; PVR: 34 |
| Norby et al. 2002 (56) 3-arm study (multicentre) |
70 (46, 24) 3 of the control group received TUIP rather than TURP Third arm: contacle laser: 48 |
Patients with BPH 50 years or older; IPSS ≥ 7; QOL ≥3; Qmax <12 mL/s | TUMT: 43 TURP: 44 |
6 months | Prostatron system | TUMT: 44 TURP: 22 |
| Floratos et al. 2001 | 144 TUMT: 78 TURP: 66 |
Patients with BPH 45 years or older; LUTS > 3 months; Prostate volume ≥30 cm3; Prostatic urethral length ≥25 mm; Madsen symptom score ≥ 8; Qmax ≤ 15 mL/s; PVR≤350 mL | TUMT: 42 (30–82) TURP: 48 (31–84) |
TUMT: 32.4 TURP: 33.7 Months |
Prostatron system |
3 years TUMT IPSS:36; QOL: 36; Qmax: 27; PVR: 27 TURP IPSS: 32; QOL: 32; Qmax: 29; PVR: 29 |
| Francisca et al. 2000 | 147 TUMT: 74 TURP: 73 |
≥ 45 years; Prostate volume ≥ 30 cm3; Prostatic urethral length ≥ 25 mm; Madsen symptom score ≥8; Qmax ≤15 mL/s; postvoid residual ≤350 mL | TUMT: 50 (19.4) TURP: 52 (19.2) P =.70 |
1 | Prostatron system |
TUMT IPSS: 48; Qmax: 49; PVR: 47; Madsen: 38 TURP IPSS: 39 Qmax: 37 PVR: 38 Madsen: 35 |
BPH refers to benign prostatic hyperplasia; IPSS, International Prostate Symptom Score; LUTS, Lower urinary tract symptoms; PVR, postvoid residual urine; Qmax, maximum flow rate; QOL, Quality of life; TUIP, transurethral incision of the prostate; TUMT, transurethral microwave thermotherapy; TURP transurethral resection of the prostate
Table 47: Subjective Outcome Measures of Effectiveness. Transurethral Microwave Thermotherapy Versus TURP.
| Study, Year | IPSS, Mean (SD) | QOL score, Mean (SD) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 3 months | 6 months | 12 months | > 1 year | Baseline | 3 months | 6 months | 12 months | > 1 year | |
| Wagrell et al. 2004 & 2002 (76;79) TUMT TURP |
21.0 (5.4) 20.4 (5.9) NR |
8.4 (5.5) 6.7 (4.3) P =NR |
7.4 (6.2) 5.9 (5) P =NR |
7.2 (6.2) 7.1 (6.6) P =.578 |
2 years: 7.2 (5.9) 4.6 (4.4) P = .014 3 years: 8.2 (6.9) 5.0 (3.9) P = .024 |
DANPSS-1 4.3 (1.0) 4.2 (1.1) NR |
DANPSS-1 1.5 (1.4) 1.1 (1.6) P =NR |
DANPSS-1 1.3 (1.4) 1.0 (1.5) P =NR |
DANPSS-1 1.4 (1.3) 1.5 (1.7) P =.972 |
2 years: 1.3 (1.2) 0.9 (1.3) P = .108 3 Years 1.2 (1.2) 1.0 (1.4) P = .162 |
| Norby et al. 2002 (56) TUMT TURP |
20.5 (5.7) 21.3 (6.6) P =.640 |
NR | 9.5 (7.1) 6.8 (5.7) P =.128 |
NR | NR | 4 4 P =.828 |
NR | 2 1 P =.055 |
NR | NR |
| Floratos, et al. 2001 TUMT TURP |
21 20 |
NR | NR | 8 3 |
2 years: TUMT: 9 TURP: 4 3 years TUMT: 12 TURP: 3 P = .000 |
4 4 |
NR | NR | 2 1 |
2 years TUMT: 2 TURP: 1 3 years TUMT: 2 TURP: 1 P ≤ .000 |
| Francisca, et al 2000 TUMT TURP |
20.1 (6.5) 20.8 (6.2) P = .57 |
10.5 (7.9) 5.3 (5.2) P < .01 |
NR | 7.6 (5.6) 3.2 (2.5) P < .01 |
NR |
Madsen symptom score 14.9 (4) 15.1 (4.1) P = .38 |
Madsen symptom score 6.4 (5.7) 3.5 (3.7) P < .01 |
NR |
Madsen symptom score 5.5 (4.6) 2.1 (2.1) P < .01 |
NR |
BPH refers to benign prostatic hyperplasia; DANPSS, Danish Prostatic Symptom Score; IPSS, International Prostate Symptom Score; NR, not reported; QOL, Quality of life; TUMT, transurethral microwave thermotherapy; TURP transurethral resection of the prostate
Table 48: Objective Outcome Measures of Effectiveness. Transurethral Microwave Thermotherapy (TUMT) Versus TURP.
| Study, Year | Peak urinary flow (Qmax), Mean (SD), mL/s | Postvoid residual urine, Mean (SD), mL | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 3 months | 6 months | 1 year | > 1 year | Baseline | 3 months | 6 months | 1 year | > 1 year | |
| Wagrell et al. 2004; & 2002 (76;79) TUMT TURP |
7.6 (2.7) 7.9 (2.7) P =NR |
12.8 (6.1) 14.6 (9.0) P =NR |
13.5 (6.1) 13.8 (6.8) P =NR |
13.3 (6.0) 15.2 (7.8) P = .565 |
2 years: 12.4 (5.3) 15.6 (9.6) P = .020 3 years 11.9 (4.9) 13.5 (7.4) P =.584 |
106 (77) 94 (82) P =NR |
NR | NR | 49 (70) 54 (77) P = .68 |
2 years: 55 (63) 40 (48) P = .340 3 years 47 (62) 54 (118) P = .760 |
| Norby et al. 2002 (56) TUMT TURP |
9.1 (4.2) 9.6 (3.2) 0.639 |
NR | 13.2 (6.9) 20.6 (12.8) P = .019 |
NR | NR | 110 75 P = .273 |
NR | 48 23 P = .013 |
NR | NR |
| Floratos, et al. 2001 TUMT TURP |
9.2 7.6 |
NR | NR | 15.1 24.5 |
2 years 14.5 23 3 years 11.9 24.7 P =.000 |
34 61 |
NR | NR | 30 19 |
2 years 30 30 3 years 30 36 P < .05 |
| Francisca et al 2000 TUMT TURP |
9.6 (3.0) 7.9 (2.8) P < .01 |
15.5 (12.1) 25.0 (7.5) P < .01 |
NR | 15.2 (7.6) 23.5 (9.9) P < .01 |
NR | 64 (76) 84 (90) P = 16 |
64 (76) 14 (21) P < .01 |
NR | 58 (72) 19 (51) P =< .01 |
NR |
NR refers to not reported; Qmax, maximum urinary flow; SD, standard deviation; TUMT, transurethral microwave thermotherapy; TURP transurethral resection of the prostate
Table 49: Perioperative Outcomes. Transurethral Microwave Thermotherapy (TUMT) Versus TURP.
| Study, Year | Operative time Mean (SD), Min | Hospital stay Mean (SD), Days | Catheterization time Mean (SD), Hours | Hemoglobin decrease, Mean (SD), g/dL | Transfusion, N (%) | Intraoperative irrigant requirement, Mean (SD), L | TUR syndrome N (%) |
|---|---|---|---|---|---|---|---|
| Wagrell et al. 2004 & 2002 (76;79) TUMT TURP |
57 NR |
NR | 336 (192) 72 (96) |
NR | NR | NR | 0 1 |
| Norby et al. 2002 (56) TUMT TURP |
NR |
TUMT: Outpatient: 40 1 Night: 4 2 nights: 1 TURP: 5 (Median) |
Median TUMT: 168 & 336 with the use of 2 different software version TURP: 48 |
NR | 0 2 (9) |
NR | 0 1(5) |
| Floratos, et al. 2001 | NR | NR | NR | NR | NR | NR | NR |
| Francisca et al 2000 | NR | NR | NR | NR | NR | NR | NR |
Mean decrease in hemoglobin unless otherwise stated;
NR refers to not reported; Qmax, maximum urinary flow; SD, standard deviation; TUMT, transurethral microwave thermotherapy; TUR, transurethral resection; TURP transurethral resection of the prostate
Table 50: Postoperative and Long Term Complications. Transurethral Microwave Thermotherapy (TUMT) Versus TURP.
| RCT | Urinary complications | Sexual dysfunction | Reoperation N (%) | Mortality N (%) | |||
|---|---|---|---|---|---|---|---|
| Urinary retention N (%) | Bladder neck/urethral stricture N (%) |
Incontinence N (%) | Impotence N (%) | Retrograde ejaculation N (%) | |||
| Wagrell et al. 2004 & 2002 (76;79) TUMT TURP |
19% 13% |
NR |
Transient 3% 13% |
6 6 |
NR | 4 (5) 1 (2.6) Additional treatment (type not specified) |
0 1 |
| Norby et al. 2002 (56) TUMT TURP |
4 1 |
0 1 (5) |
0 1 (5) |
2 (9) 1 (14) |
6 (22) 7 (50) P =.07 |
1 0 |
NR |
| Floratos, et al. 2001 TUMT TURP |
NR 1 |
1 5 |
NR 1 |
8 0 |
2 (unrelated to TUMT) 2 (unrelated to TURP) |
||
| Francisca et al 2000 TUMT TURP |
2 0 |
1 2 |
1 2 |
NR | NR | 2 0 |
2 (prior to treatment) |
NR refers to not reported; TUMT, transurethral microwave thermotherapy; TURP transurethral resection of the prostate
Transurethral Needle Ablation (TUNA)
Table 51: Patient Characteristics. Transurethral Needle Ablation (TUNA) Versus TURP.
| Study, Year | Patients, No (Treatment, control) | Inclusion criteria | Prostate size Mean (SD), mL | Mean follow-up Years (months where specified) | Equipment and software | No available for follow-up |
|---|---|---|---|---|---|---|
| Hill et al. 2004 (80) | 121 (65, 56) |
Patients with BPH 50 years or older; prostate size 20–75 gr; LUTS ≥3 months; IPSS >13; Qmax ≤12 mL/s; minimum voided volume ≥125 mL | NR | 5 | NR |
5 years IPSS/QOL: TUNA: 18 TURP: 22 Qmax: TUNA: 13 TURP: 15 PVR: TUNA: 13 TURP: 17 |
| Cimentepe et al. 2003 (81) | 59 (26, 33) |
Patients with BPH >40 years old; prostate size >70 gr; IPSS >13’; Qmax <15 mL/s | 46.1 (11.2) 49.1 (17.7) P =.591 |
1.5 | Vidamed® Inc. | NR |
BPH refers to benign prostatic hyperplasia; IPSS, International Prostate Symptom Score; LUTS, Lower urinary tract symptoms; NR, not reported; PVR, postvoid residual urine; Qmax, maximum flow rate; QOL, Quality of life; SD, standard deviation; TUNA; transurethral needle ablation; TURP transurethral resection of the prostate
Table 52: Subjective Outcome Measures of Effectiveness. Transurethral Needle Ablation (TUNA) Versus TURP.
| Study, Year | IPSS, Mean (SD) | QOL score, Mean (SD) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 3 months | 6 months | 12 months | > 1 year | Baseline | 3 months | 6 months | 12 months | > 1 year | |
| Hill et al. 2004 (80) TUNA TURP |
24 (0.8) 24.1 (0.8) P =.91 |
NR | NR |
11.7 (1) 7.8 (0.9) P =.0049 |
2 years 15 (1.3) 9.5 (1.1) P =.0028 3 years 15.2 (1.3) 10.1 1.4) P =.0079 4 years 13.2 (1.5) 7.6 (1.6) P =.0137 5 years 10.7 (1.4) 10.8 (1.6) P =.9813 |
11.8 (0.5) 12.6 (0.5) P =.24 |
NR | NR |
4.3 (0.5) 3.7 (0.7) P =.4814 |
2 years 6 (0.7) 3.7 (0.7) P =.0309 3 years 5.4 (0.7) 4.7 (1) P =.5275 4 years 5.2 (0.9) 3.7 (1) P =.2316 5 years 3.8 (0.7) 4 (0.8) P =.8719 |
| Cimentepe et al. 2003 (81) TUNA TURP |
22.9 (3.8) 24.1 (3.8) P =.408 |
9.7 (2.8) 8.3 (2.9) P =.248 |
NR | NR |
1.5 years 8.5 (3.2) 8.6 (1.8) P =.899 |
4.8 (0.75) 5.2 (0.65) P =.111 |
2.1 (0.5) 1.9 (0.5) P =.296 |
NR | NR |
1.5 years 1.8 (1.3) 1.7 (0.5) P =.351 |
BPH refers to benign prostatic hyperplasia; IPSS, International Prostate Symptom Score; NR, not reported; QOL, Quality of life; SD, standard deviation; TUNA; transurethral needle ablation; TURP transurethral resection of the prostate
Table 53: Objective Outcome Measures of Effectiveness. Transurethral Needle Ablation (TUNA) Versus TURP.
| Study, Year | Peak urinary flow (Qmax), Mean (SD), mL/s | Postvoid residual urine, Mean (SD), mL | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 3 months | 6 months | 1 year | > 1 year | Baseline | 3 months | 6 months | 1 year | > 1 year | |
| Hill et al. 2004 (80) TUNA TURP |
8.8 (0.3) 8.8 (0.3) P =.99 |
NR | NR |
14.6 (1) 21.1 (1.3) P <.0001 |
2 years 12.5 (0.7) 21.3 (1.4) P <.0001 3 years 13 (1.3) 19.1 (2) P = .0106 4 years 11.7 (1.4) 18.9 (2.5) P = .0142 5 years 11.4 (1.2) 18.6 (2.3) P = .0143 |
91.8 (10) 81.9 (9.3) P =.47 |
NR | NR |
80.3 (11) 47.1 (7) P =.0173 |
2 years 74.1 (12.6) 34.6 (5.6) P =.0114 3 years 78.2 (13.7) 50.7 (10.4) P = .1285 4 years 138.2 (45.7) 39.5 (13.1) P = .0564 5 years 60.4 (21.8) 27.4 (7.9) P = .1281 |
| Cimentepe et al. 2003 (81) TUNA TURP |
9.8 (3.6) 9.2 (3.4) P =.656 |
16.7 (4.5) 23.1 (5.3) P =.002 |
NR | NR |
1.5 years 17.7 (4.2) 23.3 (4.9) P = .004 |
67.4 (29.4) 76.1 (50.1) P = .576 |
45.3 (16.7) 32.4 (17.4) P = .065 |
NR | NR | 46.4 (17.5) 30.3 (18.8) P = .031 |
NR refers to not reported; Qmax, maximum flow rate; SD, standard deviation; TUNA; transurethral needle ablation; TURP transurethral resection of the prostate
Table 54: Perioperative Outcomes. Transurethral Needle Ablation (TUNA) Versus TURP.
| Study, Year | Operative time Mean (SD), Min | Hospital stay Mean (SD), Days | Catheterization time Mean (SD), Hours | Hemoglobin decrease, Mean (SD), g/dL | Transfusion, N (%) | Intraoperative irrigant requirement, Mean (SD), L | TUR syndrome N (%) |
|---|---|---|---|---|---|---|---|
| Hill et al. 2004 (80) TUNA TURP |
NR | NR | NR | NR | NR | NR | NR |
| Cimentepe et al. 2003 (81) TUNA TURP |
44.3 (7.8) 55.9 (12.4) P = .06 |
≤1 ≥2 |
NR | NR | 0 0 |
NR | NR |
Mean decrease in hemoglobin unless otherwise stated;
NR refers to not reported; TUNA; transurethral needle ablation; TURP transurethral resection of the prostate
Table 55: Postoperative and Long Term Complications. Transurethral Needle Ablation (TUNA) Versus TURP.
| RCT | Urinary complications | Sexual dysfunction | Reoperation N (%) | Mortality N (%) | |||
|---|---|---|---|---|---|---|---|
| Urinary retention N (%) | Bladder neck/urethral stricture N (%) |
Incontinence N (%) | Impotence N (%) | Retrograde ejaculation N (%) | |||
| Hill et al. 2004 (80) TUNA TURP |
0 0 |
1 (1.5) 4 (7.1) |
2 (3.1) 12 (21.4)* |
2 (3.1) 12 (21.4) Significant (P-value NR) |
0 23 (41.1) |
9 (13.8) 1 (1.8) |
NR |
| Cimentepe et al. 2003 (81) TUNA TURP |
0 0 |
0 2 (6) |
0 1 (0.3) |
0 4 (12) |
0 16 (48.5) |
2 (7) 0 |
NR |
Authors indicated that this high rate is most likely due to the questionnaire used to report incontinence in this study
NR refers to not reported; RCT, randomized controlled trial; TUNA; transurethral needle ablation; TURP transurethral resection of the prostate
Suggested Citation
This report should be cited as follows:
Medical Advisory Secretariat. Energy delivery systems for treatment of benign prostatic hyperplasia: an evidence-based analysis. Ontario Health Technology Assessment Series 2006; 6(17).
Permission Requests
All inquiries regarding permission to reproduce any content in the Ontario Health Technology Assessment Series should be directed to MASinfo.moh@ontario.ca.
How to Obtain Issues in the Ontario Health Technology Assessment Series
All reports in the Ontario Health Technology Assessment Series are freely available in PDF format at the following URL: www.health.gov.on.ca/ohtas.
Print copies can be obtained by contacting MASinfo.moh@ontario.ca.
Conflict of Interest Statement
All analyses in the Ontario Health Technology Assessment Series are impartial and subject to a systematic evidence-based assessment process. There are no competing interests or conflicts of interest to declare.
Peer Review
All Medical Advisory Secretariat analyses are subject to external expert peer review. Additionally, the public consultation process is also available to individuals wishing to comment on an analysis prior to finalization. For more information, please visit http://www.health.gov.on.ca/english/providers/program/ohtac/public_engage_overview.html.
Contact Information
The Medical Advisory Secretariat
Ministry of Health and Long-Term Care
20 Dundas Street West, 10th floor
Toronto, Ontario
CANADA
M5G 2N6
Email: MASinfo.moh@ontario.ca
Telephone: 416-314-1092
ISSN 1915-7398 (Online)
ISBN 978-1-4249-4321-0 (PDF)
About the Medical Advisory Secretariat
The Medical Advisory Secretariat (MAS) is part of the Ontario Ministry of Health and Long-Term Care (MOHLTC). The mandate of MAS is to provide evidence-based policy advice on the coordinated uptake of health services and new health technologies in Ontario to the MOHLTC and to the healthcare system. The aim is to ensure that residents of Ontario have access to the best available new health technologies to improve patient outcomes.
The Secretariat also provides a secretariat function and evidence-based health technology policy analysis for review by the Ontario Health Technology Advisory Committee (OHTAC). It conducts systematic reviews of scientific evidence and consultations with experts in the health care services community to produce the Ontario Health Technology Assessment Series.
About the Ontario Health Technology Assessment Series
To conduct its comprehensive analyses, MAS systematically reviews available scientific literature, collaborates with partners across relevant government branches, and consults with clinical and other external experts and manufacturers, and solicits any necessary advice to gather information. The MAS makes every effort to ensure that all relevant research, nationally and internationally, is included in the systematic literature reviews conducted.
The information gathered is the foundation of the evidence to determine if a technology is effective and safe for use in a particular clinical population or setting. Information is collected to understand how a new technology fits within current practice and treatment alternatives. Details of the technology’s diffusion into current practice and input from practising medical experts and industry add important information to the review of the provision and delivery of the health technology in Ontario. Information concerning the health benefits; economic and human resources; and ethical, regulatory, social and legal issues relating to the technology assist policy makers to make timely and relevant decisions to optimize patient outcomes.
If you are aware of any current additional evidence to inform an existing evidence-based analysis, please contact the Medical Advisory Secretariat: MASinfo.moh@ontario.ca. The public consultation process is also available to individuals wishing to comment on an analysis prior to publication. For more information, please visit http://www.health.gov.on.ca/english/providers/program/ohtac/public_engage_overview.html.
Disclaimer
This evidence-based analysis was prepared by the Medical Advisory Secretariat, Ontario Ministry of Health and Long-Term Care, for the Ontario Health Technology Advisory Committee and developed from analysis, interpretation, and comparison of scientific research and/or technology assessments conducted by other organizations. It also incorporates, when available, Ontario data, and information provided by experts and applicants to the Medical Advisory Secretariat to inform the analysis. While every effort has been made to reflect all scientific research available, this document may not fully do so. Additionally, other relevant scientific findings may have been reported since completion of the review. This evidence-based analysis is current to the date of publication. This analysis may be superseded by an updated publication on the same topic. Please check the Medical Advisory Secretariat Website for a list of all evidence-based analyses: http://www.health.gov.on.ca/ohtas.
Abbreviations
- AUA
American Urological Association
- BOO
Bladder outlet obstruction
- BPH
Benign prostatic hyperplasia
- Cdn
Canadian
- CLV
Contact laser vaporization of the prostate
- CUA
Canadian Urological Association
- EM
Electromagnetic
- FY
Fiscal year
- Hct
Hematocrit
- HIFU
High intensity focused ultrasound
- Hz
Hertz
- HoLAP
Holmium laser ablation of the prostate
- HoLEP
Holmium laser enucleation of the prostate
- HoLRP
Holmium laser resection of the prostate
- ILC
Interstitial laser coagulation
- IPSS
International Prostate Symptom Score
- KTP
Potassium titanyl phosphate
- Laser
Light amplification by stimulated emission of radiation
- LUTS
Lower urinary tract symptoms
- Nd:YAG
Neodymium yttrium aluminum garnet
- nm
Nanometer
- OR
Operating room
- PAC-10
Prospective Complexity Adjustment-10
- PKVP
Plasmakinetic vaporization of the prostate
- PSA
Prostate specific antigen
- PVP
Photoselective vaporization of the prostate
- PVR
Postvoid residual urine
- Qmax
Maximum urinary flow rate
- QOL
Quality of life
- RCT
Randomized controlled trial
- SD
Standard deviation
- TUIP
Transurethral incision of the prostate
- TULIP
Transurethral ultrasound guided laser incision prostatectomy
- TUMT
Transurethral microwave thermotherapy
- TUNA
Transurethral needle ablation
- TUR
Transurethral resection
- TURP
Transurethral resection of the prostate
- TUVP
Transurethral electrovaporization of the prostate
- TUVRP
Transurethral electrovapor resection of the prostate
- VLAP
Visual laser ablation of the prostate
- WHO
World Health Organization
- YAG
Yttrium aluminum garnet
Footnotes
The hospital cost associated with a PAC-10 weight of 1 was estimated at $4,434 for FY2005/06. A unique PAC-10 weight for a procedure is the weighting of the resource utilization within a particular case mix group.
References
- 1.Roehrborn CG, Preminger G, Newhall P, Denstedt J, Razvi H, Chin LJ, et al. Microwave thermotherapy for benign prostatic hyperplasia with the Dornier Urowave: results of a randomized, double-blind, multicenter, sham-controlled trial. Urology. 1998;51(1):19–28. doi: 10.1016/s0090-4295(97)00571-2. [DOI] [PubMed] [Google Scholar]
- 2.McConnell JD, Barry MJ, Bruskewitz RC. Benign prostatic hyperplasia: diagnosis and treatment [monograph on the Internet] 1994. Feb, [[cited: 2006 Jul 6]]. AHCPR Pub. No. 94-0582. Available from: http://www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=hstat6.chapter.17571 . [PubMed]
- 3.Bachmann A, Schurch L, Ruszat R, Wyler SF, Seifert HH, Muller A, et al. Photoselective vaporization (PVP) versus transurethral resection of the prostate (TURP): a prospective bi-centre study of perioperative morbidity and early functional outcome. Eur Urol. 2005;48(6):965–71. doi: 10.1016/j.eururo.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 4.Wheelahan J, Scott NA, Cartmill R, Marshall V, Morton RP, Nacey J, et al. Minimally invasive laser techniques for prostatectomy: a systematic review. [The ASERNIP-S review group. Australian Safety and Efficacy Register of New Interventional Procedures--Surgical]. BJU Int. 2000;86(7):805–15. doi: 10.1046/j.1464-410x.2000.00920.x. [DOI] [PubMed] [Google Scholar]
- 5.Mebust WK, Holtgrewe HL, Cockett AT, Peters PC. Transurethral prostatectomy: immediate and postoperative complications. Cooperative study of 13 participating institutions evaluating 3,885 patients. J Urol. 2002;167(2:Pt 2):999–1003. [PubMed] [Google Scholar]
- 6.Furuya S, Furuya R, Ogura H, Araki T, Arita T. [A study of 4,031 patients of transurethral resection of the prostate performed by one surgeon: learning curve, surgical results and postoperative complications] Hinyokika Kiyo - Acta Urologica Japonica. 2006;52(8):609–14. [PubMed] [Google Scholar]
- 7.Berry SJ, Coffey DS, Walsh PC, Ewing LL. The development of human benign prostatic hyperplasia with age. J Urol. 1984;132(3):474–9. doi: 10.1016/s0022-5347(17)49698-4. [DOI] [PubMed] [Google Scholar]
- 8.McVary KT. Totowa NJ, editor. Management of benign prostatic hypertrophy. Humana Press Inc. 2004.
- 9.Holtgrewe HL. Current trends in management of men with lower urinary tract symptoms and benign prostatic hyperplasia. Urology. 1998;51(4A Suppl):1–7. doi: 10.1016/s0090-4295(98)00048-x. [DOI] [PubMed] [Google Scholar]
- 10.Apolone G, Cattaneo A, Colombo P, La Vecchia C, Cavazzuti L, Bamfi F. Knowledge and opinion on prostate and prevalence of self-reported BPH and prostate-related events. Eur J Cancer Prev. 2002;11(5):473–9. doi: 10.1097/00008469-200210000-00010. A cross-sectional survey in Italy. [DOI] [PubMed] [Google Scholar]
- 11.Norman RW, Nickel JC, Fish D, Pickett SN. ‘Prostate-related symptoms’ in Canadian men 50 years of age or older: prevalence and relationships among symptoms. Br J Urol. 1994;74(5):542–50. doi: 10.1111/j.1464-410x.1994.tb09181.x. [DOI] [PubMed] [Google Scholar]
- 12.Roehrborn CG, Marks L, Harkaway R. Enlarged prostate: a landmark national survey of its prevalence and impact on US men and their partners. Prostate Cancer Prostatic Dis. 2006;9(1):30–4. doi: 10.1038/sj.pcan.4500841. [DOI] [PubMed] [Google Scholar]
- 13.Logie J, Clifford GM, Farmer RD. Incidence, prevalence and management of lower urinary tract symptoms in men in the UK. BJU Int. 2005;95(4):557–62. doi: 10.1111/j.1464-410X.2005.05339.x. [DOI] [PubMed] [Google Scholar]
- 14.Andersson SO, Rashidkhani B, Karlberg L, Wolk A, Johansson JE. Prevalence of lower urinary tract symptoms in men aged 45-79 years: a population-based study of 40 000 Swedish men. BJU Int. 2004;94(3):327–31. doi: 10.1111/j.1464-410X.2004.04930.x. [DOI] [PubMed] [Google Scholar]
- 15.McNaughton-Collins M, Barry MJ. Managing patients with lower urinary tract symptoms suggestive of benign prostatic hyperplasia. Am J Med. 2005;118(12):1331–9. doi: 10.1016/j.amjmed.2004.12.033. [DOI] [PubMed] [Google Scholar]
- 16.Nickel JC, Herschorn S, Corcos J, Donnelly B, Drover D, Elhilali M, et al. Canadian guidelines for the management of benign prostatic hyperplasia. Can J Urol. 2005;12(3):2677–83. [PubMed] [Google Scholar]
- 17.Chapple CR, McConnell J, Tubaro A, editors. Benign prostatic hyperplasia: current therapy. London, UK: Martin Dunitz Ltd; 2000. [Google Scholar]
- 18.Welch G, Kawachi I, Barry MJ, Giovannucci E, Colditz GA, Willett WC. Distinction between symptoms of voiding and filling in benign prostatic hyperplasia: findings from the Health Professionals Follow-up Study. Urology. 1998;51(3):422–7. doi: 10.1016/s0090-4295(97)00626-2. [DOI] [PubMed] [Google Scholar]
- 19.Barry MJ, Fowler FJ Jr, O’Leary MP, Bruskewitz RC, Holtgrewe HL, Mebust WK, et al. The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. J Urol. 1992;148(5):1549–57. doi: 10.1016/s0022-5347(17)36966-5. [DOI] [PubMed] [Google Scholar]
- 20.Bailey A, Martin ML, Girman C, McNaughton-Collins M, Barry MJ. Development of a multiregional United States Spanish version of the international prostate symptom score and the benign prostatic hyperplasia impact index. J Urol. 2005;174(5):1896–901. doi: 10.1097/01.ju.0000177072.59090.f7. [DOI] [PubMed] [Google Scholar]
- 21.Madersbacher S, Klingler HC, Schatzl G, Stulnig T, Schmidbauer CP, Marberger M. Age related urodynamic changes in patients with benign prostatic hyperplasia. J Urol. 1996;156(5):1662–7. [PubMed] [Google Scholar]
- 22.Abrams P. In support of pressure-flow studies for evaluating men with lower urinary tract symptoms. Urology. 1994;44(2):153–5. doi: 10.1016/s0090-4295(94)80119-3. [DOI] [PubMed] [Google Scholar]
- 23.McConnell JD. Why pressure-flow studies should be optional and not mandatory studies for evaluating men with benign prostatic hyperplasia. Urology. 1994;44(2):156–8. doi: 10.1016/s0090-4295(94)80120-7. [DOI] [PubMed] [Google Scholar]
- 24.de la Rosette JJ, Alivizatos G, Madersbacher S, Perachino M, Thomas D, Desgrandchamps F, et al. EAU Guidelines on benign prostatic hyperplasia (BPH) Eur Urol. 2001;40(3):256–63. doi: 10.1159/000049784. [DOI] [PubMed] [Google Scholar]
- 25.Konarzewski WH. Disorders of sodium balance: hyponatraemia can occur during transurethral resection of prostate. BMJ. 2006;332(7545):853–4. doi: 10.1136/bmj.332.7545.853-c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Collins JW, Macdermott S, Bradbrook RA, Keeley FX Jr, Timoney AG. A comparison of the effect of 1.5% glycine and 5% glucose irrigants on plasma serum physiology and the incidence of transurethral resection syndrome during prostate resection. BJU Int. 2005;96(3):368–72. doi: 10.1111/j.1464-410X.2005.05633.x. [DOI] [PubMed] [Google Scholar]
- 27.Orandi A. Transurethral incision of the prostate. J Urol. 1973;110(2):229–31. doi: 10.1016/s0022-5347(17)60172-1. [DOI] [PubMed] [Google Scholar]
- 28.McAllister WJ, Gilling PJ. Vaporization of the prostate. Curr Opin Urol. 2004;14(1):31–4. doi: 10.1097/00042307-200401000-00007. [DOI] [PubMed] [Google Scholar]
- 29.van Swol CF te SE, Verdaasdonk RM de la, Rosette JJ, Boon TA. Variation in output power of laser prostatectomy fibers: a need for power measurements. Urology. 1996;47(5):672–7. doi: 10.1016/s0090-4295(96)00005-2. [DOI] [PubMed] [Google Scholar]
- 30.Koshiba K, Miki M, Terachi T, Uchida T. Treatment of benign prostatic hyperplasia. New York: Springer. 2000.
- 31.Miller PD, Eardley I, Kaplan SA, editors. Benign prostatic hyperplasia. London: Martin Dunitz Ltd; 2001. [Google Scholar]
- 32.Tefekli A, Muslumanoglu AY, Baykal M, Binbay M, Tas A, Altunrende F. A hybrid technique using bipolar energy in transurethral prostate surgery: a prospective, randomized comparison. J Urol. 2005;174(4 Pt 1):1339–43. doi: 10.1097/01.ju.0000173075.62504.73. [DOI] [PubMed] [Google Scholar]
- 33.Karaman MI, Kaya C, Ozturk M, Gurdal M, Kirecci S, Pirincci N. Comparison of transurethral vaporization using PlasmaKinetic energy and transurethral resection of prostate: 1-year follow-up. J Endourol. 2005;19(6):734–7. doi: 10.1089/end.2005.19.734. [DOI] [PubMed] [Google Scholar]
- 34.Keoghane SR, Lawrence KC, Gray AM, Doll HA, Hancock AM, Turner K, et al. A double-blind randomized controlled trial and economic evaluation of transurethral resection vs contact laser vaporization for benign prostatic enlargement: a 3-year follow-up. BJU Int. 2000;85(1):74–8. doi: 10.1046/j.1464-410x.2000.00407.x. [DOI] [PubMed] [Google Scholar]
- 35.Bryan NP, Hastie KJ, Chapple CR. Randomised prospective trial of contact laser prostatectomy (CLAP) versus visual laser coagulation of the prostate (VLAP) for the treatment of benign prostatic hyperplasia. Eur Urol. 2000;38(3):265–71. doi: 10.1159/000020292. 2-year follow-up. [DOI] [PubMed] [Google Scholar]
- 36.Planz B, Kalem T, Sprenger C, Deix T, Djavan B, Hanke P. A prospective randomized study of combined visual laser ablation and transurethral resection of the prostate versus transurethral prostatectomy alone. Urol Int. 2003;71(1):26–30. doi: 10.1159/000071089. [DOI] [PubMed] [Google Scholar]
- 37.Kursh ED, Concepcion R, Chan S, Hudson P, Ratner M, Eyre R. Interstitial laser coagulation versus transurethral prostate resection for treating benign prostatic obstruction: a randomized trial with 2-year follow-up. Urology. 2003;61(3):573–8. doi: 10.1016/s0090-4295(02)02420-2. [DOI] [PubMed] [Google Scholar]
- 38.Gilling PJ, Cass CB, Cresswell MD, Fraundorfer MR. Holmium laser resection of the prostate: preliminary results of a new method for the treatment of benign prostatic hyperplasia. Urology. 1996;47(1):48–51. doi: 10.1016/s0090-4295(99)80381-1. [DOI] [PubMed] [Google Scholar]
- 39.Kuntz RM, Ahyai S, Lehrich K, Fayad A. Transurethral holmium laser enucleation of the prostate versus transurethral electrocautery resection of the prostate: a randomized prospective trial in 200 patients. J Urol. 2004;172(3):1012–6. doi: 10.1097/01.ju.0000136218.11998.9e. [DOI] [PubMed] [Google Scholar]
- 40.Tan AH, Gilling PJ, Kennett KM, Frampton C, Westenberg AM, Fraundorfer MR. A randomized trial comparing holmium laser enucleation of the prostate with transurethral resection of the prostate for the treatment of bladder outlet obstruction secondary to benign prostatic hyperplasia in large glands (40 to 200 grams) J Urol. 2003;170(4 Pt 1):1270–4. doi: 10.1097/01.ju.0000086948.55973.00. [DOI] [PubMed] [Google Scholar]
- 41.Gilling PJ, Kennett KM, Fraundorfer MR. Holmium laser resection v transurethral resection of the prostate: results of a randomized trial with 2 years of follow-up. J Endourol. 2000;14(9):757–60. doi: 10.1089/end.2000.14.757. [DOI] [PubMed] [Google Scholar]
- 42.Gilling PJ, Cass CB, Cresswell MD, Fraundorfer MR. Holmium laser resection of the prostate: preliminary results of a new method for the treatment of benign prostatic hyperplasia. Urology. 1996;47(1):48–51. doi: 10.1016/s0090-4295(99)80381-1. [DOI] [PubMed] [Google Scholar]
- 43.Kuntz RM, Lehrich K. Transurethral holmium laser enucleation versus transvesical open enucleation for prostate adenoma greater than 100 gm.: a randomized prospective trial of 120 patients. J Urol. 2002;168(4 Pt 1):1465–9. doi: 10.1016/S0022-5347(05)64475-8. [DOI] [PubMed] [Google Scholar]
- 44.Tan AH, Gilling PJ. Lasers in the treatment of benign prostatic hyperplasia: an update. Curr Opin Urol. 2005;15(1):55–8. doi: 10.1097/00042307-200501000-00013. [DOI] [PubMed] [Google Scholar]
- 45.Bhatta KM. Lasers in urology. Lasers Surg Med. 1995;16(4):312–30. doi: 10.1002/lsm.1900160403. [DOI] [PubMed] [Google Scholar]
- 46.Malek RS, Kuntzman RS, Barrett DM. High power potassium-titanyl-phosphate laser vaporization prostatectomy. J Urol. 2000;163(6):1730–3. [PubMed] [Google Scholar]
- 47.Kuntzman RS, Malek RS, Barrett DM. High-power potassium titanyl phosphate laser vaporization prostatectomy. Mayo Clin Proc. 1998;73(8):798–801. doi: 10.4065/73.8.798. [DOI] [PubMed] [Google Scholar]
- 48.Malek RS, Kuntzman RS, Barrett DM. Photoselective potassium-titanyl-phosphate laser vaporization of the benign obstructive prostate: observations on long-term outcomes. J Urol. 2005;174(4:Pt 1):t–8. doi: 10.1097/01.ju.0000173913.41401.67. [DOI] [PubMed] [Google Scholar]
- 49.Tubaro A, Vicentini C, Renzetti R, Miano L. Invasive and minimally invasive treatment modalities for lower urinary tract symptoms: what are the relevant differences in randomised controlled trials? Eur Urol. 2000;38(SUPPL. 1):7–17. doi: 10.1159/000052397. [DOI] [PubMed] [Google Scholar]
- 50.Naslund MJ. Transurethral needle ablation of the prostate. Urology. 1997;50(2):167–72. doi: 10.1016/S0090-4295(97)00277-X. [DOI] [PubMed] [Google Scholar]
- 51.Madersbacher S, Kratzik C, Susani M, Marberger M. Tissue ablation in benign prostatic hyperplasia with high intensity focused ultrasound. J Urol. 1994;152(6:Pt 1):t–60. doi: 10.1016/s0022-5347(17)32278-4. [DOI] [PubMed] [Google Scholar]
- 52.Gardner TA, Koch MO. Prostate cancer therapy with high-intensity focused ultrasound. Clin Genitourin Cancer. 2005;4(3):187–92. doi: 10.3816/CGC.2005.n.031. [DOI] [PubMed] [Google Scholar]
- 53.Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, et al. Grading quality of evidence and strength of recommendations. BMJ. 2004;328(7454):1490. doi: 10.1136/bmj.328.7454.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.van Melick HH, van Venrooij GE, Boon TA. Long-term follow-up after transurethral resection of the prostate, contact laser prostatectomy, and electrovaporization. Urology. 2003;62(6):1029–34. doi: 10.1016/s0090-4295(03)00769-6. [DOI] [PubMed] [Google Scholar]
- 55.Gupta N, Sivaramakrishna Kumar R, Dogra PN, Seth A. Comparison of standard transurethral resection, transurethral vapour resection and holmium laser enucleation of the prostate for managing benign prostatic hyperplasia of >40 g. BJU Int. 2006;97(1):85–9. doi: 10.1111/j.1464-410X.2006.05862.x. [DOI] [PubMed] [Google Scholar]
- 56.Norby B, Nielsen HV, Frimodt-Moller PC. Transurethral interstitial laser coagulation of the prostate and transurethral microwave thermotherapy vs transurethral resection or incision of the prostate: results of a randomized, controlled study in patients with symptomatic benign prostatic hyperplasia. BJU Int. 2002;90(9):853–62. doi: 10.1046/j.1464-410x.2002.03031.x. [DOI] [PubMed] [Google Scholar]
- 57.Hammadeh MY, Madaan S, Hines J, Philp T. 5-year outcome of a prospective randomized trial to compare transurethral electrovaporization of the prostate and standard transurethral resection. Urology. 2003;61(6):1166–71. doi: 10.1016/s0090-4295(03)00109-2. [DOI] [PubMed] [Google Scholar]
- 58.Talic RF, El Tiraifi A, El Faqih SR, Hassan SH, Attassi RA, Abdel-Halim RE. Prospective randomized study of transurethral vaporization resection of the prostate using the thick loop and standard transurethral prostatectomy. Urology. 2000;55(6):886–90. doi: 10.1016/s0090-4295(00)00520-3. [DOI] [PubMed] [Google Scholar]
- 59.Akhtar MM, Orakzai N, Qureshi AM. Trans urethral electric vaporisation of prostate as an alternate to trans urethral resection in benign prostatic hyperplasia. J Ayub Med Coll. 2004;16(4):16–20. [PubMed] [Google Scholar]
- 60.Liu CK, Lee WK, Ko MC, Chiang HS, Wan KS. Transurethral electrovapor resection versus standard transurethral resection treatment for a large prostate: a 2-year follow-up study conducted in Taiwan. Urol Int. 2006;76(2):144–9. doi: 10.1159/000090878. [DOI] [PubMed] [Google Scholar]
- 61.Nuhoglu B, Ayyildiz A, Fidan V, Ersoy E, Huri E, Germiyanogu C. Transurethral electrovaporization of the prostate: is it any better than standard transurethral prostatectomy? 5-year follow-up. J Endourol. 2005;19(1):79–82. doi: 10.1089/end.2005.19.79. [DOI] [PubMed] [Google Scholar]
- 62.Fowler C, McAllister W, Plail R, Karim O, Yang Q. Health Technology Assessment [[cited: 2006 Jun 26]];Randomised evaluation of alternative electrosurgical modalities to treat bladder outflow obstruction in men with benign prostatic hyperplasia [report on the Internet] 2005 9(4) doi: 10.3310/hta9040. Available from: http://www.ncchta.org/execsumm/summ904.htm . [DOI] [PubMed] [Google Scholar]
- 63.Kupeli S, Yilmaz E, Soygur T, Budak M. Randomized study of transurethral resection of the prostate and combined transurethral resection and vaporization of the prostate as a therapeutic alternative in men with benign prostatic hyperplasia. J Endourol. 2001;15(3):317–21. doi: 10.1089/089277901750161935. [DOI] [PubMed] [Google Scholar]
- 64.Nuhoglu B, Ayyildiz A, Karaguzel E, Cebeci O, Germiyanoglu C. Plasmakinetic prostate resection in the treatment of benign prostate hyperplasia: results of 1-year follow up. Int J Urol. 2006;13(1):21–4. doi: 10.1111/j.1442-2042.2006.01218.x. [DOI] [PubMed] [Google Scholar]
- 65.Seckiner I, Yesilli C, Akduman B, Altan K, Mungan NA. A prospective randomized study for comparing bipolar plasmakinetic resection of the prostate with standard TURP. Urol Int. 2006;76(2):139–43. doi: 10.1159/000090877. [DOI] [PubMed] [Google Scholar]
- 66.de Sio M, Autorino R, Quarto G, Damiano R, Perdona S di, Lorenzo G, et al. Gyrus bipolar versus standard monopolar transurethral resection of the prostate: a randomized prospective trial. Urology. 2006;67(1):69–72. doi: 10.1016/j.urology.2005.07.033. [DOI] [PubMed] [Google Scholar]
- 67.Chacko KN, Donovan JL, Abrams P, Peters TJ, Brookes ST, Thorpe AC, et al. Transurethral prostatic resection or laser therapy for men with acute urinary retention: The CLasP randomized trial. J Urol. 2001;166(1):166–70. [PubMed] [Google Scholar]
- 68.Gujral S, Abrams P, Donovan JL, Neal DE, Brookes ST, Chacko KN, et al. A prospective randomized trial comparing transurethral resection of the prostate and laser therapy in men with chronic urinary retention: The CLasP study. J Urol. 2000;164(1):59–64. [PubMed] [Google Scholar]
- 69.Donovan JL, Peters TJ, Neal DE, Brookes ST, Gujral S, Chacko KN, et al. A randomized trial comparing transurethral resection of the prostate, laser therapy and conservative treatment of men with symptoms associated with benign prostatic enlargement: The CLasP study. J Urol. 2000;164(1):65–70. [PubMed] [Google Scholar]
- 70.Tuhkanen K, Heino A, Aaltomaa S, Ala-Opas M. Long-term results of contact laser versus transurethral resection of the prostate in the treatment of benign prostatic hyperplasia with small or moderately enlarged prostates. Scand J Urol Nephrol. 2003;37(6):487–93. doi: 10.1080/00365590310015769. [DOI] [PubMed] [Google Scholar]
- 71.Liedberg F, Adell L, Hagberg G, Palmqvist IB. Interstitial laser coagulation versus transurethral resection of the prostate for benign prostatic enlargement--a prospective randomized study. Scand J Urol Nephrol. 2003;37(6):494–7. doi: 10.1080/00365590310001773. [DOI] [PubMed] [Google Scholar]
- 72.Rigatti L, Naspro R, Salonia A, Centemero A, Ghezzi M, Guazzoni G, et al. Urodynamics after TURP and HoLEP in urodynamically obstructed patients: are there any differences at 1 year of follow-up? Urology. 2006;67(6):1193–8. doi: 10.1016/j.urology.2005.12.036. [DOI] [PubMed] [Google Scholar]
- 73.Kuntz RM, Lehrich K, Ahyai S. Transurethral holmium laser enucleation of the prostate compared with transvesical open prostatectomy: 18-month follow-up of a randomized trial. J Endourol. 2004;18(2):189–91. doi: 10.1089/089277904322959851. [DOI] [PubMed] [Google Scholar]
- 74.Westenberg A, Gilling P, Kennett K, Frampton C, Fraundorfer M. Holmium laser resection of the prostate versus transurethral resection of the prostate: results of a randomized trial with 4-year minimum long-term followup. J Urol. 2004;172(2):616–9. doi: 10.1097/01.ju.0000132739.57555.d8. [DOI] [PubMed] [Google Scholar]
- 75.Shingleton WB, Farabaugh P, May W. Three-year follow-up of laser prostatectomy versus transurethral resection of the prostate in men with benign prostatic hyperplasia. Urology. 2002;60(2):305–8. doi: 10.1016/s0090-4295(02)01697-7. [DOI] [PubMed] [Google Scholar]
- 76.Wagrell L, Schelin S, Nordling J, Richthoff J, Magnusson B, Schain M, et al. Three-year follow-up of feedback microwave thermotherapy versus TURP for clinical BPH: a prospective randomized multicenter study. Urology. 2004;64(4):698–702. doi: 10.1016/j.urology.2004.05.030. [DOI] [PubMed] [Google Scholar]
- 77.Floratos DL, Kiemeney LA, Rossi C, Kortmann BB, Debruyne FM de la, Rosette JJ. Long-term followup of randomized transurethral microwave thermotherapy versus transurethral prostatic resection study. J Urol. 2001;165(5):1533–8. [PubMed] [Google Scholar]
- 78.Francisca EA, d’Ancona FC, Hendriks JC, Kiemeney LA, Debruyne FM de la, Rosette JJ. A randomized study comparing high-energy TUMT to TURP: quality-of-life results. Eur Urol. 2000;38(5):569–75. doi: 10.1159/000020357. [DOI] [PubMed] [Google Scholar]
- 79.Wagrell L, Schelin S, Nordling J, Richthoff J, Magnusson B, Schain M, et al. Feedback microwave thermotherapy versus TURP for clinical BPH--a randomized controlled multicenter study. Urology. 2002;60(2):292–9. doi: 10.1016/s0090-4295(02)01740-5. [DOI] [PubMed] [Google Scholar]
- 80.Hill B, Belville W, Bruskewitz R, Issa M, Perez-Marrero R, Roehrborn C, et al. Transurethral needle ablation versus transurethral resection of the prostate for the treatment of symptomatic benign prostatic hyperplasia: 5-year results of a prospective, randomized, multicenter clinical trial. J Urol. 2004;171(6 Pt 1):2336–40. doi: 10.1097/01.ju.0000127761.87421.a0. [DOI] [PubMed] [Google Scholar]
- 81.Cimentepe E, Unsal A, Saglam R. Randomized clinical trial comparing transurethral needle ablation with transurethral resection of the prostate for the treatment of benign prostatic hyperplasia: results at 18 months. J Endourol. 2003;17(2):103–7. doi: 10.1089/08927790360587432. [DOI] [PubMed] [Google Scholar]
- 82.Nickel JC, Saad F. The American Urological Association 2003 guideline on management of benign prostatic hyperplasia: a Canadian opinion. Can J Urol. 2004;11(2):2186–93. [PubMed] [Google Scholar]
- 83.Greene DR, Wheeler TM. Clinical relevance of the individual prostate cancer focus. Cancer Invest. 1994;12(4):425–37. doi: 10.3109/07357909409038236. [DOI] [PubMed] [Google Scholar]
- 84.Greene DR, Fitzpatrick JM, Scardino PT. Anatomy of the prostate and distribution of early prostate cancer. Semin Surg Oncol. 1995;11(1):9–22. doi: 10.1002/ssu.2980110104. [DOI] [PubMed] [Google Scholar]
- 85.De La Rosette J, Baba S, Badlani G, Elhilali M, Gravas S, Muschter R, Natio S, Netto NR. Denis L, Khoury S, Cockett ATK, editors. New minimally invasive and surgical developments in the management of BPO. Plymouth, UK: Health Publications. 2005. pp. 195–233.
- 86.FDA Centre for Devices and Radiological Health. FDA public health notification: Serious injuries from Microwave thermotherapy for benign prostatic hyperplasia. 2000. [[cited: 2009 Apr 16]]. Available from: www.fda.gov/cdrh/safety/bph.html .
- 87.McAllister WJ, Karim O, Plail RO, Samra DR, Steggall MJ, Yang Q, et al. Transurethral electrovaporization of the prostate: is it any better than conventional transurethral resection of the prostate? BJU Int. 2003;91(3):211–4. doi: 10.1046/j.1464-410x.2003.04073.x. [DOI] [PubMed] [Google Scholar]
- 88.van Melick HH, van Venrooij GE, Eckhardt MD, Boon TA. A randomized controlled trial comparing transurethral resection of the prostate, contact laser prostatectomy and electrovaporization in men with benign prostatic hyperplasia: urodynamic effects. J Urol. 2002;168(3):1058–62. doi: 10.1016/S0022-5347(05)64574-0. [DOI] [PubMed] [Google Scholar]
- 89.van Melick HH, van Venrooij GE, Eckhardt MD, Boon TA. A randomized controlled trial comparing transurethral resection of the prostate, contact laser prostatectomy and electrovaporization in men with benign prostatic hyperplasia: analysis of subjective changes, morbidity and mortality. J Urol. 2003;169(4):1411–6. doi: 10.1097/01.ju.0000054657.59200.97. [DOI] [PubMed] [Google Scholar]
- 90.Hammadeh MY, Madaan S, Singh M, Philp T. A 3-year follow-up of a prospective randomized trial comparing transurethral electrovaporization of the prostate with standard transurethral prostatectomy. BJU Int. 2000;86(6):648–51. doi: 10.1046/j.1464-410x.2000.00879.x. [DOI] [PubMed] [Google Scholar]
- 91.Gupta NP, Doddamani D, Aron M, Hemal AK. Vapor resection: a good alternative to standard loop resection in the management of prostates >40 cc. J Endourol. 2002;16(10):767–71. doi: 10.1089/08927790260472944. [DOI] [PubMed] [Google Scholar]
- 92.Ekengren J, Haendler L, Hahn RG. Clinical outcome 1 year after transurethral vaporization and resection of the prostate. Urology. 2000;55(2):231–5. doi: 10.1016/s0090-4295(99)00416-1. [DOI] [PubMed] [Google Scholar]
- 93.Hon NH, Brathwaite D, Hussain Z, Ghiblawi S, Brace H, Hayne D, et al. A prospective, randomized trial comparing conventional transurethral prostate resection with PlasmaKinetic(R) vaporization of the prostate: physiological changes, early complications and long-term followup. J Urol. 2006;176(1):205–9. doi: 10.1016/S0022-5347(06)00492-7. [DOI] [PubMed] [Google Scholar]
- 94.Fung BT, Li SK, Yu CF, Lau BE, Hou SS. Prospective randomized controlled trial comparing plasmakinetic vaporesection and conventional transurethral resection of the prostate. Asian J Surg. 2005;28(1):24–8. doi: 10.1016/S1015-9584(09)60253-0. [DOI] [PubMed] [Google Scholar]


