Abstract
OBJECTIVE
To examine whether the association between gestational diabetes mellitus (GDM) and BMI category varies by racial/ethnic group.
RESEARCH DESIGN AND METHODS
In a cohort of 123,040 women without recognized pregravid diabetes who delivered babies between 1995 and 2006 at Kaiser Permanente of Northern California, we examined racial/ethnic disparities in the prevalence of GDM by BMI category and the population-attributable risk (PAR) associated with overweight/obesity.
RESULTS
Among all racial/ethnic groups, the age-adjusted prevalence of GDM increased with increasing BMI (kg/m2) category. However, Asian and Filipina women had a prevalence of GDM of 9.9 and 8.5%, respectively, at a BMI of 22.0–24.9 kg/m2, whereas in Hispanic, non-Hispanic white, and African American women, the prevalence of GDM was >8.0% at a higher BMI, such as 28–30, 34–36, and ≥37 kg/m2, respectively. The estimated PARs suggest that the percentage of GDM that could be prevented if all pregnant women were of normal weight (BMI <25.0 kg/m2) ranging from 65% for African American women to only 23% among Asian women.
CONCLUSIONS
Clinicians should be aware that the BMI thresholds for increased risk of GDM varies by racial/ethnic group and that the risk is high even at relatively low BMI cutoffs in Asian and Filipina women. Asian women may benefit from different prevention strategies in addition to weight management.
Gestational diabetes mellitus (GDM) is carbohydrate intolerance with onset of or first recognition during pregnancy and is one of the most common pregnancy complications in the U.S. GDM is associated with increased risk for perinatal morbidity (1,2), and, in the long-term, women with GDM have an almost sevenfold increased risk of developing type 2 diabetes after pregnancy (3). The prevalence of GDM has increased in all racial/ethnic groups, and this has been observed in several populations in recent decades (4,5). Recent data suggest that the association between glucose and risk of adverse outcomes is continuous; gestational impaired glucose tolerance (IGT) is also associated with both pregnancy complications (6) and subsequent diabetes and cardiometabolic risk (7).
Race/ethnicity and obesity are the two strongest independent risk factors for GDM (8–11). However, the demographic distribution of obesity (highest among African Americans and lowest among Asians) does not mirror the demographic distribution of GDM (lowest among African Americans and highest among Asians) (12). Yet there is ongoing debate surrounding the definition of overweight and obesity in Asian populations: the World Health Organization proposed a BMI cutoff of 23.0 kg/m2 for overweight among Asians in 2000 (13), compared with a cutoff of 25.0 kg/m2 for non-Asian populations. More recently, the World Health Organization stated that the definition of overweight in Asians likely varies depending on the outcome of interest (14). Currently, little is known about racial disparities in the risk of GDM by BMI categories.
In a cohort of 123,040 women without recognized pregravid diabetes who delivered babies between 1995 and 2006 at Kaiser Permanente of Northern California (KPNC), we examined racial/ethnic disparities in the prevalence of GDM and IGT in pregnancy by BMI category and the estimated proportion of cases that could be prevented if overweight/obesity in pregnant women were eliminated (the population-attributable risk [PAR]).
RESEARCH DESIGN AND METHODS
The study setting was KPNC, which provides comprehensive medical services through 14 delivery hospitals and 23 outpatient clinics to >3 million members located in a 14-county region of Northern California. The demographic make-up of the KPNC membership is well representative of the population living in the geographical area served by this large, integrated health care delivery system, except that the KPNC population has slightly lower representation at the extremes of income and age (15,16).
Cohort identification
The study cohort was identified through the KPNC Gestational Diabetes Registry, which has been described in detail elsewhere (17). In brief, this registry identifies all pregnant women without recognized pregravid diabetes and classifies them according to glucose values obtained from a 50-g glucose challenge test (hereafter referred to as the screening test); those with an abnormal screening-test result (≥140 mg/dL) were given the follow-up 100-g, 3-h oral glucose tolerance test (OGTT; hereafter referred to as the diagnostic test). At KPNC, 94% of women delivering live-born singletons underwent the recommended screening test for GDM (18).
Maternal age at delivery, height, pregnancy body weight (assessed on average at 17 weeks’ gestation [range 6–26]; 98.6% had maternal weight measured between 15 and 20 weeks’ gestation), and gestational age at the weight measurement were obtained from the KPNC electronic medical records. A previous study in this setting during the same period (19) reported 98.5% agreement between gestational age in the electronic medical records and estimates from ultrasonographic data collected prior to 24 weeks. Pregnancy BMI was calculated as the maternal weight (in kilograms) divided by the square of height (in meters).
Maternal glucose values from the screening and diagnostic tests were obtained from the KPNC regional laboratory database, which captures all laboratory tests and results performed at the KPNC regional laboratory. Women were classified as having GDM if two or more of the four plasma glucose values obtained during the diagnostic test were abnormal according to the American Diabetes Association criteria (20) used during the study period (plasma glucose thresholds: fasting 5.3 mmol/L [95 mg/dL], 1-h glucose 10.0 mmol/L [180 mg/dL], 2-h glucose 8.6 mmol/L [155 mg/dL], and 3-h glucose 7.8 mmol/L [140 mg/dL]; gestational IGT glucose challenge test ≥140 mg/dL; and OGTT with only one abnormal result) (7).
Among women without recognized diabetes prior to pregnancy, we identified 371,557 live-birth deliveries to women aged 15–45 years at delivery that matched a California birth certificate record between 1995 and 2006 (99% successful linkage) (21). Women missing plasma glucose values for the screening test or who failed to have a diagnostic test after an abnormal screening test were excluded (n = 25,640 [6.9%]), as were those missing data on height or pregnancy weight (n = 183,346 [53%]) and with an unknown racial/ethnic group (n = 1,050 [0.3%]). Among the 161,521 deliveries with complete data, we selected the first pregnancy during the study period, leaving 125,682 women. We then further excluded 425 women with other race/ethnicity, 2,101 women who were missing one or more values from the 100-g, 3-h OGTT, and 116 women with missing parity and/or gestation at pregnancy weight ascertainment data. Thus, the final analytic cohort consisted of 123,040 women.
The subset of women who were excluded as a result of missing BMIs were statistically significantly older (mean age 29.2 vs. 28.5 years) and were slightly more likely to have had two or more prior live births (21.3 vs. 17.1%), to have a high school degree or less education (42.0 vs. 37.5%), and to be white (44.2 vs. 39.3%), and they were slightly less likely to be Filipina (5.9 vs. 7.8%). However, there were no differences between the excluded subset and our analytic cohort in the prevalence of GDM overall (6.4 and 6.5%, respectively) or the prevalence of GDM by race/ethnicity.
The state of California electronic birth certificate records were used to obtain information on self-reported maternal education, parity, and race/ethnicity. We included the following racial/ethnic groups: non-Hispanic white, African American, Hispanic, Asian, and Filipina.
Statistical analysis
The age-adjusted prevalence of GDM and 95% CIs were calculated within each BMI category (<19.0, 19.0–21.9, 22.0–24.9, 25–27.9, 28.0–30.9, 31.0–33.9, 34.0–36.9, and ≥37.0 kg/m2) and further stratified by racial/ethnic group; estimates were standardized using the direct method, with the age distribution of the entire study cohort used as the reference. Unconditional logistic regression analyses were used to obtain odds ratios (ORs) estimating the relative risk of GDM associated with each category of BMI, separately for the five racial/ethnic groups. Multiple logistic regression was used to adjust for age at delivery (aged 18–24 [reference group], 25–29, 30–34, and 35–45 years), education (high school graduate or less [reference group], partial college, college graduate or higher, and unknown), parity (0 [reference group], 1, and ≥2), and gestational age (<15 [reference group], 15–17, 18–20, and ≥21 weeks’ gestational age) at the pregnancy weight measurement. Heterogeneity in associations by race/ethnicity was assessed by inclusion of appropriate cross-product (interaction) terms in regression models. We calculated partial PARs for being overweight or obese in pregnancy by the method described by Spiegelman et al. (22), using a publicly available SAS Macro (http://www.hsph.harvard.edu/faculty/donna-spiegelman/software/par/index.html). We used the KPNC population data to estimate the prevalence of GDM for the PAR calculations. SAS version 9.1 (SAS Institute, Cary, NC) was used for all analyses. This study was approved by the institutional review boards of the Kaiser Foundation Research Institute and the state of California.
RESULTS
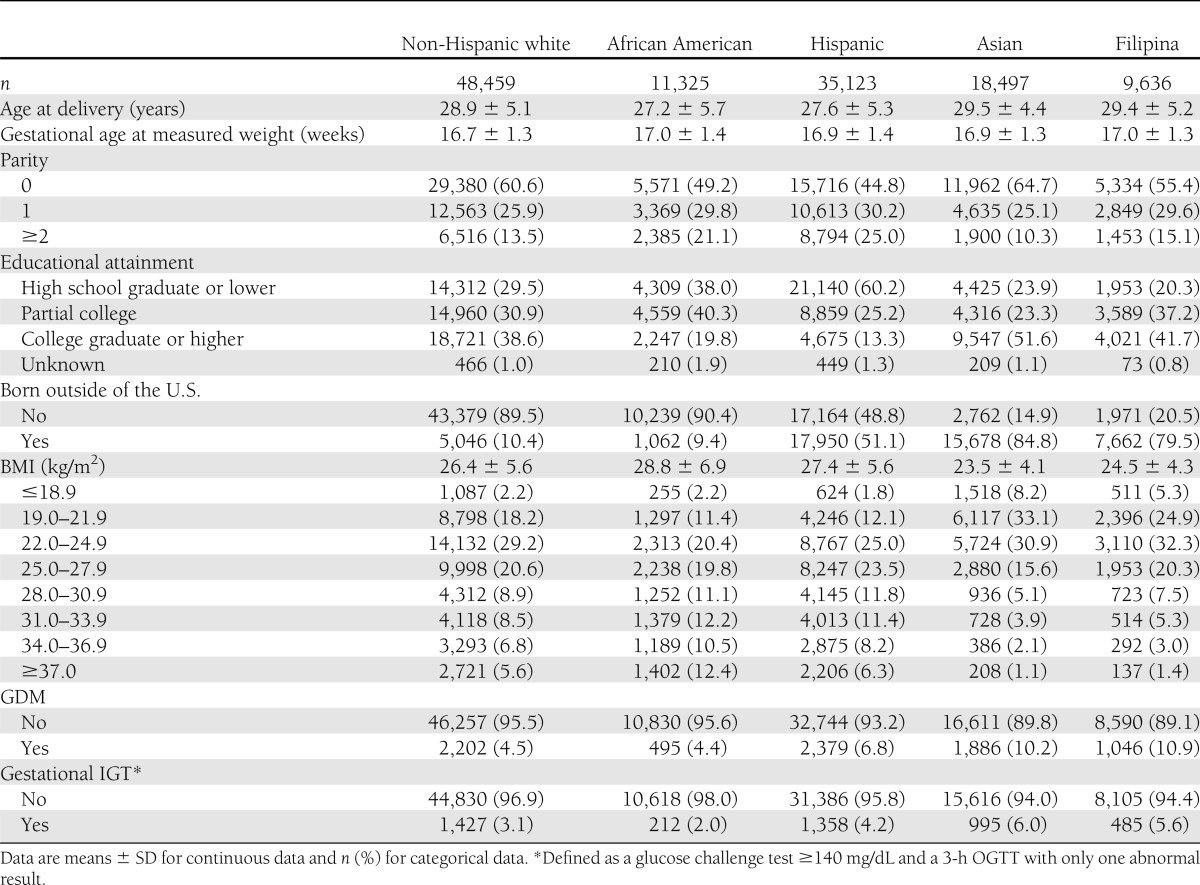
Table 1 displays the characteristics of the analytic cohort by maternal race/ethnicity. Asian women were more educated and less likely to be overweight (BMI >25.0 kg/m2) or obese (BMI >30.0 kg/m2) compared with women from other racial/ethnic groups. African American and Hispanic women were more likely to have only a high school education and two or more prior live births. Overall, the prevalence of GDM varied by racial/ethnic group; it was lowest among non-Hispanic white women (4.5%) and African Americans (4.4%), intermediate among Hispanics (6.8%), and highest among Asians (10.2%) and Filipinas (10.9%) (Table 1).
Table 1.
Characteristics of the study cohort by race/ethnicity; KPNC 1996–2006
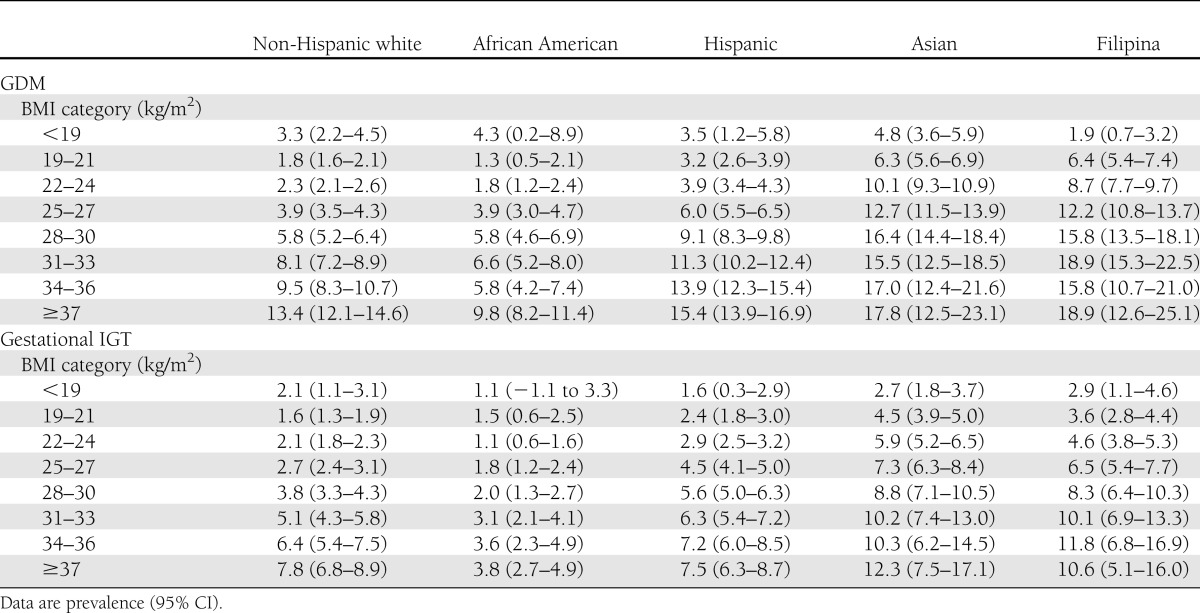
Among all racial/ethnic groups, the age-adjusted prevalence of GDM increased with increasing category of BMI (kg/m2) (Table 2). However, there were significant variations in the association between BMI and GDM by racial/ethnic group: Asian and Filipina women had a prevalence of 9.9 and 8.5%, respectively, at a BMI of 22.0–24.9 kg/m2. In Hispanic, non-Hispanic white, and African American women, the prevalence was >8.0% at BMI 28.0–30.9, 34.0–36.9, and ≥37.0 kg/m2, respectively. Even at a BMI of 19.0–21.9 kg/m2, the prevalence of GDM was more than three times higher among Asian and Filipina women (6.3 and 6.4%, respectively) compared with non-Hispanic white and African American women (1.8 and 1.3%, respectively) (Table 2). We observed similar variations in the associations between IGT and BMI category by race/ethnicity (Table 2).
Table 2.
Age-adjusted prevalence of GDM and gestational IGT by BMI category and race/ethnicity; KPNC 1996–2006
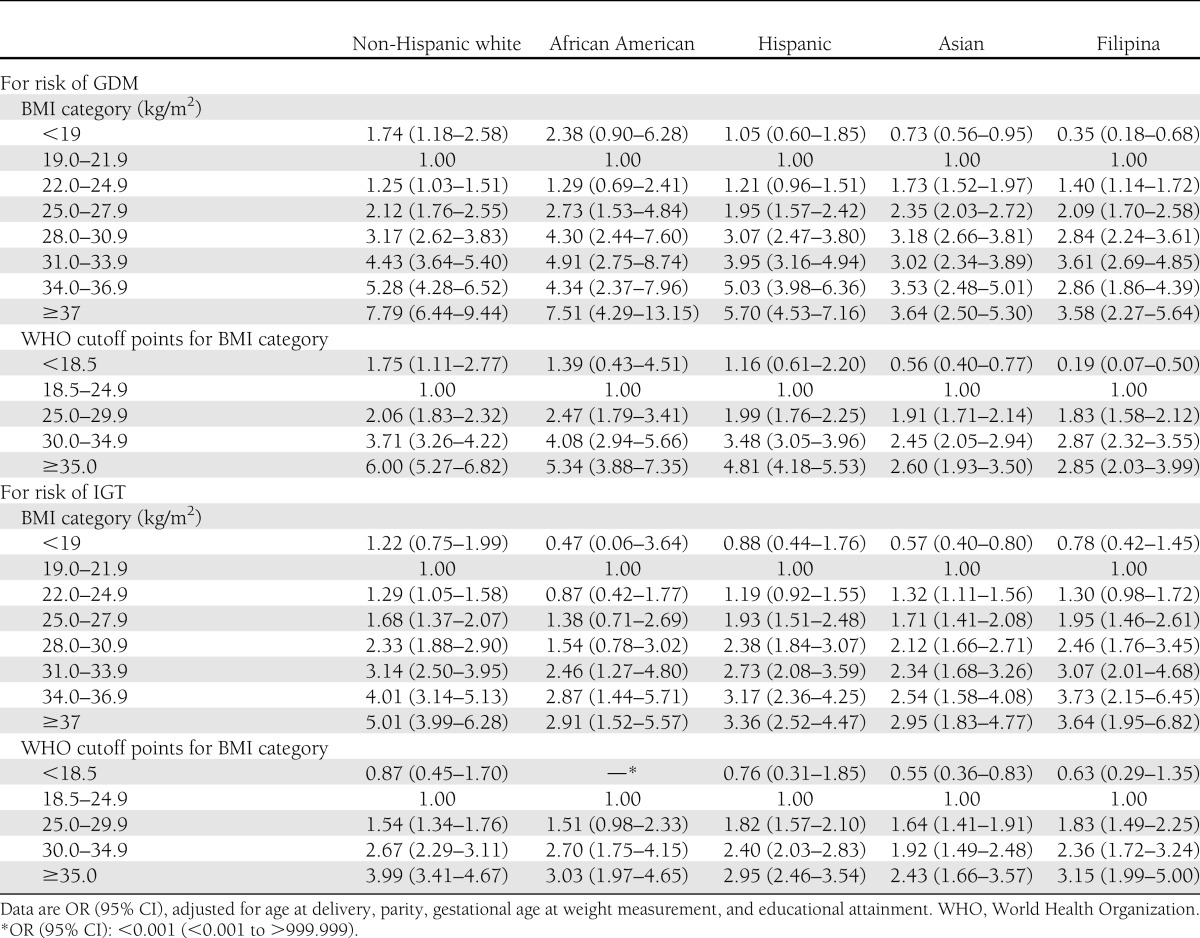
There was evidence that the association between BMI and GDM risk varied by race/ethnicity (P value interaction term <0.001). Table 3 shows the results of racial/ethnic group–specific, multiple-adjusted regression models assessing the association between the BMI categories and GDM risk. In the fully adjusted models, there was an increased risk of GDM associated with increasing BMI category for all racial/ethnic groups. However, the magnitude of the ORs for higher BMI categories (>30.9 kg/m2) was lower among Asian and Filipina women compared with non-Hispanic white, Hispanic, and African American women (Table 3). Among non-Hispanic white, Hispanic, and African American women, the relative risk of GDM increased with each BMI category up to a BMI of 37.0 kg/m2 or higher compared with women with a BMI of 19.0–21.9 kg/m2, whereas among Asians and Filipinas the increased risk of GDM seemed to plateau at a BMI of 28.0 kg/m2. Among non-Hispanic white women, there also seemed to be an increased risk of GDM associated with a BMI <19.0 kg/m2 when 19.0–21.9 kg/m2 served as the reference group, whereas Asian and Filipina women with a BMI <19.0 kg/m2 had a decreased risk of GDM compared with the referent (Table 3). Similar trends were observed between increasing BMI categories and increasing risk of gestational IGT across racial/ethnic groups; however, the magnitude of the ORs for IGT were smaller among all racial/ethnic groups compared with GDM.
Table 3.
Adjusted* ORs associated with overweight/obesity categories and risk of GDM or gestational IGT by racial/ethnic group
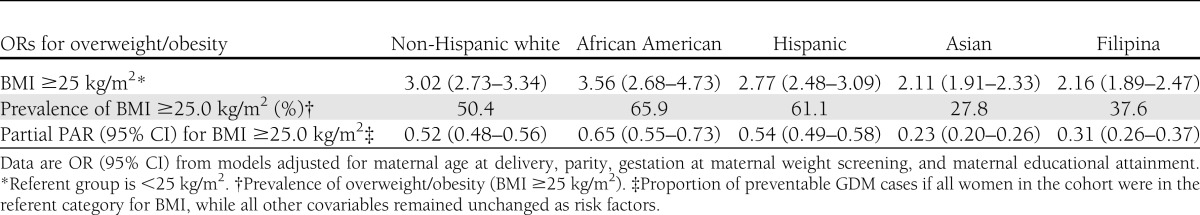
The ORs associated with pregnancy overweight or obesity (BMI ≥25.0 kg/m2) ranged from 3.56 (95% CI 2.68–4.73) for African Americans to 2.11 (1.91–2.33) for Asians. The prevalence of pregnancy overweight or obesity ranged from 23% among Asian women to 65% among African American women (Table 4). When we used the cutoff for pregnancy overweight suggested for Asian populations (≥23.0 kg/m2), all PARs increased but remained lower among Asian and Filipina women (35 and 43%, respectively) (data not shown).
Table 4.
PAR associated with overweight/obesity, by racial/ethnic group
CONCLUSIONS
In this multiethnic cohort of women undergoing universal screening for GDM, there was significant variation in the association between GDM and BMI by racial/ethnic group. Asian and Filipina women had an increased risk of GDM at a lower BMI cut point, particularly as compared with non-Hispanic white and African American women. The estimated PAR percentage for being overweight or obese during pregnancy ranged from 23% for Asians to 65% for African Americans, suggesting that the proportion of GDM that could theoretically have been prevented if all women had been normal weight (defined as a BMI <25.0 kg/m2) is much lower among Asian women. Even when a BMI cutoff of 23.0 kg/m2 is used, the PAR among Asian women is only 35%, significantly lower than that of other racial/ethnic groups.
There are notable differences in the epidemiology of type 2 diabetes and GDM, especially in terms of race/ethnicity, where African Americans consistently have a higher prevalence of type 2 diabetes (23) but not of GDM (17) when compared with non-Hispanic white women. We did not find that the lower prevalence of GDM was explained by the fact that more African American women were excluded as a result of pre-existing diabetes; in fact, a similar number of African American and Filipina women were excluded as a result of pre-existing diabetes (prevalence of recognized pregravid diabetes by racial/ethnic group: non-Hispanic white 1.4%, African American 2.2%, Hispanic 2.0%, Asian 1.3%, and Filipina 2.2%).
The association between GDM and BMI by racial/ethnic group has not been previously studied. More is known about the relationship between BMI and the risk of type 2 diabetes by racial/ethnic group. The Nurses’ Health Study examined ethnicity, obesity, and type 2 diabetes among women and found that the risk of diabetes was higher among all nonwhite racial ethnic groups compared with whites; each five-unit increment in BMI was associated with an increased risk of diabetes that was strongest for Asians and Hispanics and lowest for blacks (24). This is in contrast to our findings in GDM risk, where the ORs for higher BMIs were higher among African Americans and lowest among Asians because of the fact that Asian women were at much higher risk even at a very low BMI. A recent study in New York City found that foreign-born south Asians had a higher reported prevalence of diabetes at lower BMI levels than all other racial/ethnic groups (23). In our study, the risk of GDM increased with BMI among all racial/ethnic groups, but the risk of GDM associated with increasing BMI was lower among Asian women, who had a high risk of GDM at low BMIs. In contrast, African Americans had a relatively low prevalence of GDM even at high BMIs.
The reasons why Asians have a higher risk of GDM at a lower BMI are unclear. It has been suggested that for a given BMI, Asians have a higher percentage of body fat and more visceral adipose tissue compared with other racial/ethnic groups (21). In a study of older Filipino, African American, and white women (aged 55–80 years), visceral adipose tissue among normal-weight Filipinas was significantly higher at every level of waist girth compared with normal-weight white and African American women (25). Some of the racial/ethnic differences in GDM risk by BMI category may be attributed to racial/ethnic differences in body fat distribution or abdominal visceral fat at a given BMI. The observed racial/ethnic differences in the association between BMI and GDM risk also may be attributed to differences in genetic predisposition (26). A large study using the National Health and Nutrition Examination Survey 1999–2004 found that among blacks and Hispanics, but not white subgroups, family history was a strong risk factor for diabetes, but this was less so among overweight or obese subjects (27). Unfortunately, the National Health and Nutrition Examination Survey did not examine the association between family history and diabetes separately among Asians due to the small numbers of Asians in their study, and we were unable to examine the role of family history in the current study.
One study of 233 women with GDM found that Asian women had higher postchallenge glucose levels than white women but had comparable levels of fasting glucose and insulin and no differences in insulin resistance or β-cell function (28). They concluded that although Asian women had GDM at a lower BMI, the etiology seemed similar. Studies of patients with type 2 diabetes also have found that Asians were more likely to have abnormal postchallenge glucose values (29,30). One study found that two-thirds of Filipino and Japanese subjects with diabetes had isolated postchallenge hyperglycemia and only one-third of Filipino and Japanese subjects would have been diagnosed with diabetes if testing criteria was limited to fasting glucose (30). In another study of lean, healthy subjects matched for age, BMI, waist circumference, birth weight, and current diet, Asians had significantly higher postprandial glycemia and lower insulin sensitivity than whites in response to a 75-g carbohydrate load (31). A previous study found that in pregnant women, racial/ethnic differences in glucose concentration were observed only in postchallenge values and not in the fasting state (32). If Asians have higher postchallenge glucose levels than other race/ethnic groups, it is possible that the current screening method for diagnosing GDM, a 50-g post challenge test, may favor diagnosis among Asians across BMI categories.
However, it also is possible that there are underlying etiologic differences between Asians and other ethnic groups that account for these differences. A study examining the pathophysiology of impaired fasting glucose versus IGT (2 h after a 75-g glucose load) found that patients with IGT but normal fasting had reduced second-phase insulin release and peripheral insulin resistance, suggesting that there may be preferential insulin resistance in the muscle in IGT (33). Therefore, it is possible that the increased risk of GDM in Asian women may be attributed to Asians having more insulin resistance in the muscle compared with other racial ethnic groups; however, this needs to be confirmed by additional studies.
A major strength of this study is the universal screening and diagnosis of GDM by standardized criteria. We also were able to exclude women with recognized pre-existing diabetes. Finally, a self-reported racial/ethnic group on the California birth certificate seems to be very accurate (34). This study also had some limitations. First, body weight measured during pregnancy was used to calculate BMI (measured on average at 17 weeks’ gestation). This combines prepregnancy BMI with early pregnancy weight gain, and if this varied by race/ethnicity we may have slightly over- or underestimated the effect of prepregnancy BMI. Height and weight data were missing on a fairly large percentage of our cohort. We did not have direct measures of adiposity or visceral fat, which may be more associated with insulin resistance than BMI. We lacked data on several potential confounding factors, including family history, physical activity, and diet. Finally, because of limited numbers, we were unable to examine these associations separately among Asian subgroups, among whom the risk of GDM has been shown to vary (12).
The prevalence of GDM has increased in several populations and in all racial/ethnic groups (4). Obesity is a strong risk factor for GDM in all racial/ethnic groups, but especially among non-Asian racial/ethnic groups. Strategies to increase the proportion of women entering pregnancy at an optimal weight could potentially eliminate 23–65% of GDM, depending on the racial/ethnic group. Development of effective approaches for weight management designed specifically for reproductive-aged women are urgently needed to help women achieve a healthy weight before and during pregnancy. More research is needed to determine why Asian women have a higher risk of GDM, even at a low BMIs; it may be attributed to a genetic predisposition toward increased insulin resistance in the muscle or increased levels of visceral fat. Additional research will better inform whether Asian women may benefit from different prevention strategies in addition to weight management.
Acknowledgments
No potential conflicts of interest relevant to this article were reported.
M.H. designed the study, collected the data, and wrote the manuscript. S.E. contributed to writing and editing the manuscript. S.S. assisted with the data analysis and contributed to writing and editing the manuscript. J.D. conducted the data analysis and contributed to writing the manuscript. S.M. provided consultation regarding how to present the data and edited the manuscript. A.F. provided consultation on the study design and edited the manuscript. M.H. and J.D. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Metzger BE. Summary and recommendations of the Third International Workshop-Conference on Gestational Diabetes Mellitus. Diabetes 1991;40(Suppl. 2):197–201 [DOI] [PubMed] [Google Scholar]
- 2.Jovanovic L, Pettitt DJ. Gestational diabetes mellitus. JAMA 2001;286:2516–2518 [DOI] [PubMed] [Google Scholar]
- 3.Bellamy L, Casas JP, Hingorani AD, Williams D. Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet 2009;373:1773–1779 [DOI] [PubMed] [Google Scholar]
- 4.Ferrara A. Increasing prevalence of gestational diabetes mellitus: a public health perspective. Diabetes Care 2007;30(Suppl. 2):S141–S146 [DOI] [PubMed] [Google Scholar]
- 5.Dabelea D, Snell-Bergeon JK, Hartsfield CL, Bischoff KJ, Hamman RF, McDuffie RS, Kaiser Permanente of Colorado GDM Screening Program Increasing prevalence of gestational diabetes mellitus (GDM) over time and by birth cohort: Kaiser Permanente of Colorado GDM Screening Program. Diabetes Care 2005;28:579–584 [DOI] [PubMed] [Google Scholar]
- 6.Gambineri A, Pelusi C, Manicardi E, et al. Glucose intolerance in a large cohort of mediterranean women with polycystic ovary syndrome: phenotype and associated factors. Diabetes 2004;53:2353–2358 [DOI] [PubMed] [Google Scholar]
- 7.Stuebe AM, Mantzoros C, Kleinman K, et al. Gestational glucose tolerance and maternal metabolic profile at 3 years postpartum. Obstet Gynecol 2011;118:1065–1073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Solomon CG, Willett WC, Carey VJ, et al. A prospective study of pregravid determinants of gestational diabetes mellitus. JAMA 1997;278:1078–1083 [PubMed] [Google Scholar]
- 9.Hedderson MM, Williams MA, Holt VL, Weiss NS, Ferrara A. Body mass index and weight gain prior to pregnancy and risk of gestational diabetes mellitus. Am J Obstet Gynecol 2008;198:409.e1–409.e7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hedderson MM, Gunderson EP, Ferrara A. Gestational weight gain and risk of gestational diabetes mellitus. Obstet Gynecol 2010;115:597–604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rudra CB, Sorensen TK, Leisenring WM, Dashow E, Williams MA. Weight characteristics and height in relation to risk of gestational diabetes mellitus. Am J Epidemiol 2007;165:302–308 [DOI] [PubMed] [Google Scholar]
- 12.Hedderson MM, Darbinian JA, Ferrara A. Disparities in the risk of gestational diabetes by race-ethnicity and country of birth. Paediatr Perinat Epidemiol 2010;24:441–448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization, International Association for the Study of Obesity, International Obesity Task Force. The Asia-Pacific Perspective: Redefining obesity and its treatment. Sydney, Health Communications, 2000
- 14.WHO Expert Consultation Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004;363:157–163 [DOI] [PubMed] [Google Scholar]
- 15.Krieger N. Overcoming the absence of socioeconomic data in medical records: validation and application of a census-based methodology. Am J Public Health 1992;82:703–710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Go AS, Hylek EM, Phillips KA, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA 2001;285:2370–2375 [DOI] [PubMed] [Google Scholar]
- 17.Ferrara A, Kahn HS, Quesenberry CP, Riley C, Hedderson MM. An increase in the incidence of gestational diabetes mellitus: Northern California, 1991–2000. Obstet Gynecol 2004;103:526–533 [DOI] [PubMed] [Google Scholar]
- 18.Ferrara A, Weiss NS, Hedderson MM, et al. Pregnancy plasma glucose levels exceeding the American Diabetes Association thresholds, but below the National Diabetes Data Group thresholds for gestational diabetes mellitus, are related to the risk of neonatal macrosomia, hypoglycaemia and hyperbilirubinaemia. Diabetologia 2007;50:298–306 [DOI] [PubMed] [Google Scholar]
- 19.Hedderson MM, Ferrara A, Sacks DA. Gestational diabetes mellitus and lesser degrees of pregnancy hyperglycemia: association with increased risk of spontaneous preterm birth. Obstet Gynecol 2003;102:850–856 [DOI] [PubMed] [Google Scholar]
- 20.American Diabetes Association Gestational diabetes mellitus. Diabetes Care 2000;23(Suppl. 1):S77–S79 [PubMed] [Google Scholar]
- 21.Lear SA, Humphries KH, Kohli S, Chockalingam A, Frohlich JJ, Birmingham CL. Visceral adipose tissue accumulation differs according to ethnic background: results of the Multicultural Community Health Assessment Trial (M-CHAT). Am J Clin Nutr 2007;86:353–359 [DOI] [PubMed] [Google Scholar]
- 22.Spiegelman D, Hertzmark E, Wand HC. Point and interval estimates of partial population attributable risks in cohort studies: examples and software. Cancer Causes Control 2007;18:571–579 [DOI] [PubMed] [Google Scholar]
- 23.Gupta LS, Wu CC, Young S, Perlman SE. Prevalence of diabetes in New York City, 2002-2008: comparing foreign-born South Asians and other Asians with U.S.-born whites, blacks, and Hispanics. Diabetes Care 2011;34:1791–1793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shai I, Jiang R, Manson JE, et al. Ethnicity, obesity, and risk of type 2 diabetes in women: a 20-year follow-up study. Diabetes Care 2006;29:1585–1590 [DOI] [PubMed] [Google Scholar]
- 25.Araneta MR, Barrett-Connor E. Ethnic differences in visceral adipose tissue and type 2 diabetes: Filipino, African-American, and white women. Obes Res 2005;13:1458–1465 [DOI] [PubMed] [Google Scholar]
- 26.Hanson RL, Pettitt DJ, Bennett PH, et al. Familial relationships between obesity and NIDDM. Diabetes 1995;44:418–422 [DOI] [PubMed] [Google Scholar]
- 27.Suchindran S, Vana AM, Shaffer RA, Alcaraz JE, McCarthy JJ. Racial differences in the interaction between family history and risk factors associated with diabetes in the National Health and Nutritional Examination Survey, 1999–2004. Genet Med 2009;11:542–547 [DOI] [PubMed] [Google Scholar]
- 28.Gunton JE, Hitchman R, McElduff A. Effects of ethnicity on glucose tolerance, insulin resistance and beta cell function in 223 women with an abnormal glucose challenge test during pregnancy. Aust N Z J Obstet Gynaecol 2001;41:182–186 [DOI] [PubMed] [Google Scholar]
- 29.Ramachandran A, Ma RC, Snehalatha C. Diabetes in Asia. Lancet 2010;375:408–418 [DOI] [PubMed] [Google Scholar]
- 30.Araneta MR, Grandinetti A, Chang HK. A1C and diabetes diagnosis among Filipino Americans, Japanese Americans, and Native Hawaiians. Diabetes Care 2010;33:2626–2628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dickinson S, Colagiuri S, Faramus E, Petocz P, Brand-Miller JC. Postprandial hyperglycemia and insulin sensitivity differ among lean young adults of different ethnicities. J Nutr 2002;132:2574–2579 [DOI] [PubMed] [Google Scholar]
- 32.Chen X, Scholl TO. Ethnic differences in C-peptide/insulin/glucose dynamics in young pregnant women. J Clin Endocrinol Metab 2002;87:4642–4646 [DOI] [PubMed] [Google Scholar]
- 33.Meyer C, Pimenta W, Woerle HJ, et al. Different mechanisms for impaired fasting glucose and impaired postprandial glucose tolerance in humans. Diabetes Care 2006;29:1909–1914 [DOI] [PubMed] [Google Scholar]
- 34.Baumeister L, Marchi K, Pearl M, Williams R, Braveman P. The validity of information on “race” and “Hispanic ethnicity” in California birth certificate data. Health Serv Res 2000;35:869–883 [PMC free article] [PubMed] [Google Scholar]