Abstract
Objective
To examine the extent and composition of pharmaceutical industry representatives’ marketing techniques with a particular focus on drug sampling in relation to drug age.
Design
A group of 47 GPs prospectively collected data on drug promotional activities during a six-month period, and a sub-sample of 10 GPs furthermore recorded the representatives’ marketing techniques in detail.
Setting
Primary healthcare.
Subjects
General practitioners in the County of Funen, Denmark.
Main outcome measures.
Promotional visits and corresponding marketing techniques.
Results
The 47 GPs recorded 1050 visits corresponding to a median of 19 (range 3 to 63) per GP in the six months. The majority of drugs promoted (52%) were marketed more than five years ago. There was a statistically significant decline in the proportion of visits where drug samples were offered with drug age, but the decline was small OR 0.97 (95% CI 0.95;0.98) per year. Leaflets (68%), suggestions on how to improve therapy for a specific patient registered with the practice (53%), drug samples (48%), and gifts (36%) were the most frequently used marketing techniques.
Conclusion
Drug-industry representatives use a variety of promotional methods. The tendency to hand out drug samples was statistically significantly associated with drug age, but the decline was small.
Keywords: Advertising, drug industry, drug information services, family practice, physicians' practice patterns, prescriptions, primary healthcare
Little is known about the extent and composition of pharmaceutical industry representatives’ marketing techniques.
Gift-giving (offering leaflets, books, drug samples, and other types of gifts) was the most frequently used marketing method.
Drug sampling declined with “drug age”, but 52% of the drugs offered had been on the market for more than five years.
GPs often prescribe new expensive drugs even if they have no advantages compared with the older alternatives, and the frequent interaction between general practitioners (GPs) and pharmaceutical companies is often blamed [1–4]. This interaction extends from supporting research and medical education to providing up-to-date details and educational material targeted at patients and doctors [3]. Among the marketing approaches, pharmaceutical sales representatives constitute one of the most expensive and extensively used methods of giving information to physicians [5]. Many GPs regard drug representative visits as an efficient source of information not provided by other parts of the healthcare system [6], but frequent contacts between GPs and drug representatives seem to be strongly associated with irrational prescribing [7–9]. We lack systematic studies on the frequency and composition of representative visits, but it appears that they use a wide variety of techniques, of which giving the GPs drug samples seems to be a key determinant for impact on prescribing [10–12]. The pharmaceutical industry's purposes in giving drug samples may be to let the GPs become acquainted with the drugs by “testing” them on their patients. Consequently, drug sampling is supposedly a phenomenon related to new drugs. However, to our knowledge this hypothesis has not been tested in a primary care setting.
The purpose of the present study was to examine the extent and composition of the pharmaceutical industry representatives’ marketing techniques with a particular focus on analysing the association between drug age and sampling.
Material and methods
We invited 208 GPs from the County of Funen to collect data on drug promotional activities prospectively during a six-month period from January to July 2002, and a total of 47 GPs accepted (23%). For each pharmaceutical representative visit, the GPs recorded the company name and each drug's trade name on a form together with information on whether drug samples were offered. In addition, a sub-sample of 10 GPs recorded the representatives’ marketing techniques in detail (leaflets, gifts, drug samples, invitations to courses and meetings, proposals to improve therapy for specific or hypothetical patients, alleged economic benefits, reference to other GPs’ or specialists’ views and experiences, and scientific articles).
The forms were pilot tested, and all GPs were carefully coached in data recording and collection and received written instructions. The authors used follow-up visits, regular telephone calls, and letters to encourage the participants to continued data collection. The 10 more involved GPs were paid DKK 6000 each for collecting data and the other 37 GPs were paid DKK 4000 each.
From the Danish Medicines Agency we retrieved information on the date of approval of each drug for use on the Danish market. The association between the length of time a drug had been on the market (drug age) and the proportion of visits where it was offered was investigated using logistic regression.
P-values less than 0.05 were considered statistically significant. Analyses were performed using the statistical software STATA 8.2.
Results
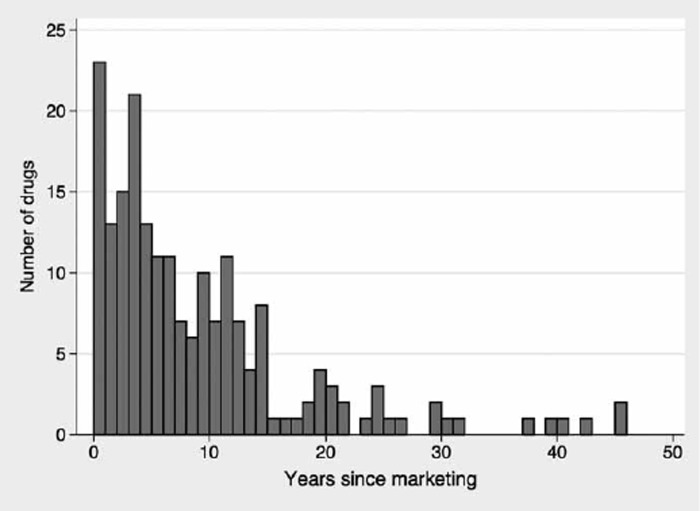
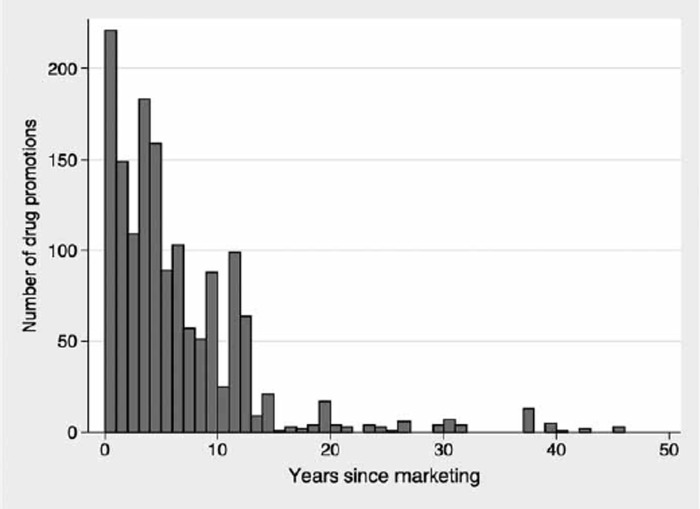
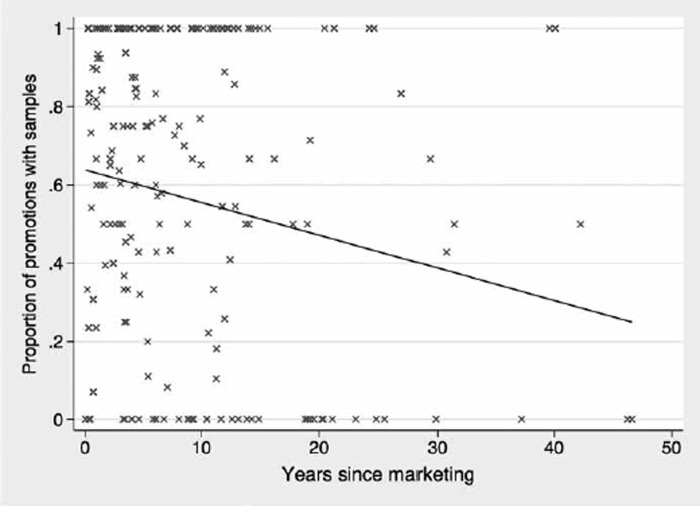
The 47 GPs recorded 1050 visits corresponding to a mean of 22.3 and a median of 19 (range 3 to 63) per GP during the six-month period. Some 38 companies visited the GPs, and a total of 197 different drugs were promoted. Some 103 of the 197 promoted drugs (52% (95% CI 45;59)) had been on the Danish market for more than five years. A total of 1514 drug promotions were undertaken, corresponding to an average of 1.4 drug promotions per visit. In 56% of the visits only one drug was promoted. According to the frequency of the pharmaceutical representative visits the top 10 drugs were cardiovascular drugs (atorvastin with 53 visits, simvastatin with 31 visits, losartan with 30 visits), non-steroidal anti-inflammatory drugs belonging to the COX2 selective group (rofecoxib with 56 visits and celecoxib with 43 visits), the new antidepressants (mirtazapin with 35 visits and citalopram with 26 visits), a triptan (sumatriptan with 26 visits), an asthma drug (fluticasone/salmeterol with 55 visits), and a drug to combat erectile dysfunction (sildenafil with 38 visits). The frequency of visits was not statistically associated with practice type (single-handed versus partnership), GP age, or sex. A drug sample was offered in 490 of the 1050 visits (47%) and 885 times during the 1514 promotions, corresponding to 58% of all promotions. Figure 1 shows the age distribution of drugs promoted. The median (IQR) drug age was 6 (3–12) years. Figure 2 shows that the number of promotions likewise declined for elderly drugs, with 54% of all promotions taking place less than 5 years and 80% less than 10 years after marketing. Figure 3 shows that the proportion of visits where a drug sample was offered declined weakly with increasing drug age. Logistic regression analysis showed an odds ratio of 0.97 (95% CI 0.95;0.98) per year for handing out drug samples as a function of drug age. Some 378 of the 885 offered drug samples (43% (95% CI 39%;46%) had been on the Danish market for more than five years.
Figure 1.
Distribution of drug age (years since marketing) for the 197 drugs promoted.
Figure 2.
Number of promotions and drug age.
Figure 3.
Proportion of visits where a drug sample was handed out and drug age. Each X represents a drug.
Detailed records from the sub-sample of 10 GPs who received 233 visits showed that offering leaflets or books (68%), proposals to improve therapy for a specific patient registered with the practice (53%), drug samples (48%), and other types of gifts (36%) were the most common techniques used by the pharmaceutical representatives (Table I).
Table I.
Marketing techniques recorded by a sub-sample of 10 GPs who received 233 drug representative visits (100%).
| No. | |
| Promotions with | Percentage (95% CI) |
| Leaflets or books | 159 |
| 68 (62;74) | |
| Proposals to improve therapy for a specific patient registered with the practice | 123 |
| 53 (46;59) | |
| Drug samples | 113 |
| 48 (42;55) | |
| Other types of gifts | 85 |
| 36 (30;43) | |
| Proposals to improve therapy for hypothetical patients | 81 |
| 35 (29;41) | |
| Reference to scientific articles | 71 |
| 30 (25;37) | |
| Alleged economic benefits for patients | 50 |
| 21 (16;27) | |
| Reference to a specialist's views and experiences | 45 |
| 19 (14;25) | |
| Invitation to course or meeting | 13 |
| 6 (3;9) | |
| Reference to other GPs’ views and experiences | 10 |
| 4 (2;7) |
Discussion
The drug representatives frequently visited the general practitioners and frequently used a wide variety of techniques, including drug samples, promotional gifts, and different kinds of educational material. The considerable range in visiting frequency (range 3–63) is glaring. Whether this is caused by some GPs being highly selective when receiving representatives of the pharmaceutical industry or the reason is that the industry offers most attention to those GPs with the biggest perceived potential for marketing impact should be addressed in future studies. It is noteworthy that drug representatives continued to promote drugs long after they had been approved for sale. At more than half of the visits a drug sample was offered, and the probability of handing out drug samples declined slowly with increasing drug age.
A number of factors must, however, be considered. First, despite our attempts to ensure optimal data collection, we cannot exclude the possibility that it was incomplete and that we may therefore have underestimated the extent of the promotional activities. However, the majority of previous studies are retrospective questionnaire surveys based on GPs’ perceptions of amount and composition of marketing, and recall bias is presumably substantial in those studies compared with our prospective data collection over a well-defined and limited time span [13]. Second, we cannot rule out that some drug representatives may have discovered the data-collection activities and adapted their behaviour accordingly. Third, we were able to recruit only 23% of practitioners, but analyses showed that the participants did not differ from other general practitioners with respect to sex, age, and practice size, and we believe that our sample is representative although it does not include the few doctors who always decline visits from pharmaceutical sales representatives. The difference between the proportion of visits where a drug sample was offered in the total sample of 47 GPs (58%) and the same proportion in the sub-sample of 10 GPs (48%) could be caused by statistical chance or be a minor selection bias. However, there were no major differences in the frequency of visits with a mean 22.3 in the large sample versus 23.3 in the small sample, and therefore we believe that no substantial selection bias is present.
It is interesting that some old drugs were marketed intensively. Plausible explanations could first be that handing out a drug sample to a patient is likely to be a strong predictor for the patient's future drug use, and second that when a GP becomes familiar with a drug he/she is more likely to prefer it and other of the company's drugs in the future [14].
The representatives used many different techniques to support their information, and it was of particular interest that sampling of drugs, even old ones, was frequently used. The frequency of visits and of handing out drug samples was to some extent dependent on the drug's age. This is in line with the observation that GPs regard drug representatives as an expedient means of acquiring drug information [15]. As to handing out drug samples, for new innovative drugs one purpose could be to give the doctor the opportunity to become acquainted with the drug, but for old drugs which the GPs already knows and may have prescribed many times there must also be other motives for the distribution of samples. In a marketing context, gifts are used to cultivate social relationships and to make the GPs feel grateful and indebted [11]. The rationale behind drug sampling may be a little more subtle. Personal “trialling” is crucial as to whether a drug becomes part of a GP's prescribing practice [16]. A sample also serves as a kind of gift from both the representative to the GP and from the GP to the patient [10], [11], [17]. Furthermore, patients who receive drug samples from physicians are exposed to the brand and therefore are likely to continue to use it.
Our results indicate that the industry representatives’ information on their drugs was supported by the handing out of leaflets or books produced by the drug companies and therefore to be regarded as containing biased drug information. In addition, the information strategies were based on using the GP's experiences with specific patients probably as springboard for a talk about the drug or using references to specialists’ and colleagues’ opinions. Some GPs do not prescribe new drugs until esteemed specialists use them [16]. In contrast to the huge impact of the drug industry's promotion, GPs often deny that this affects their prescribing [18], [19] and feel they can distinguish between reliable and misleading information from the pharmaceutical companies [19]. Hence, efforts should be concentrated on informing the GPs of how the pharmaceutical industry may influence their prescribing. It is well known that GPs’ prescribing frequently does not follow the recommendations and that authorities and medical associations have experienced great difficulties when attempting to influence GPs’ prescribing and patients’ drug use [20], [21]. In contrast, it is common belief that the drug industry strongly influences prescribing, but there is a lack of knowledge about the actual extent of this influence and the GP characteristics associated with susceptibility to influence. The pharmaceutical industry is a for-profit business and therefore is expected to market its products aggressively [4]. Contrary to this, physicians’ challenge is to ensure that their patients receive the best and least expensive drugs. How to extract the relevant elements of drug information from representatives and at the same time avoid inappropriate influence on prescribing is a challenge for physicians and medical societies.
In conclusion, drug industry representatives use a variety of promotional methods. The tendency to hand out drug samples was statistically significantly associated with drug age, but the decline was small.
Acknowledgements
The study was funded by a grant from the Institute for Rational Pharmacotherapy, the Danish Medicines Agency and the Foundation for Education and Quality Development.
Conflict of interests: None.
References
- 1.Wazana A. Physicians and the pharmaceutical industry: Is a gift ever just a gift? JAMA. 2000;283:373–80. doi: 10.1001/jama.283.3.373. [DOI] [PubMed] [Google Scholar]
- 2.Rutledge P, Crookes D, McKinstry B, Maxwell SR. Do doctors rely on pharmaceutical industry funding to attend conferences and do they perceive that this creates a bias in their drug selection? Results from a questionnaire survey. Pharmacoepidemiol Drug Saf. 2003;12:663–7. doi: 10.1002/pds.884. [DOI] [PubMed] [Google Scholar]
- 3.Blumenthal D. Doctors and drug companies. N Engl J Med. 2004;351:1885–90. doi: 10.1056/NEJMhpr042734. [DOI] [PubMed] [Google Scholar]
- 4.Abbasi K, Smith R. No more free lunches. BMJ. 2003;326:1155–6. doi: 10.1136/bmj.326.7400.1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Caudill TS, Johnson MS, Rich EC, McKinney WP. Physicians, pharmaceutical sales representatives, and the cost of prescribing. Arch Fam Med. 1996;5:201–6. doi: 10.1001/archfami.5.4.201. [DOI] [PubMed] [Google Scholar]
- 6.Aasland OG, Forde R. [Physicians and drug industry: Attitudes and practice] Tidsskr Nor Laegeforen. 2004;124:2603–6. [PubMed] [Google Scholar]
- 7.Figueras A, Laporte JR. Failures of the therapeutic chain as a cause of drug ineffectiveness. BMJ. 2003;326:895–6. doi: 10.1136/bmj.326.7395.895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Caudill T, Lurie N, Rich E. The influence of pharmaceutical industry advertising on physician prescribing. J Drug Issues. 1992;22:331–8. [Google Scholar]
- 9.Watkins C, Harvey I, Carthy P, Moore L, Robinson E, Brawn R. Attitudes and behaviour of general practitioners and their prescribing costs: A national cross sectional survey. Qual Saf Health Care. 2003;12:29–34. doi: 10.1136/qhc.12.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Groves KE, Sketris I, Tett SE. Prescription drug samples: Does this marketing strategy counteract policies for quality use of medicines? J Clin Pharm Ther. 2003;28:259–71. doi: 10.1046/j.1365-2710.2003.00481.x. [DOI] [PubMed] [Google Scholar]
- 11.Morelli D, Koenigsberg MR. Sample medication dispensing in a residency practice. J Fam Pract. 1992;34:42–8. [PubMed] [Google Scholar]
- 12.Peay MY, Peay ER. Patterns of preference for information sources in the adoption of new drug by specialists. Soc Sci Med. 1990;31:467–76. doi: 10.1016/0277-9536(90)90042-q. [DOI] [PubMed] [Google Scholar]
- 13.Rotwitt L, Rosholm JU, Brøsen K, Gram LF. [Nature and extent of drug information to general practitioners: A questionnaire study] Ugeskr Laeger. 1989;151:647–50. [PubMed] [Google Scholar]
- 14.Andersen M, Kragstrup J, Søndergaard J. How conducting a clinical trial affects physicians’ guideline adherence and drug preferences. JAMA. 2006;23:2759–64. doi: 10.1001/jama.295.23.2759. [DOI] [PubMed] [Google Scholar]
- 15.Husby T. [Cooperation between physicians and pharmaceutical consultants: A questionnaire study] Tidsskr Nor Laegeforen. 1991;111:2758–60. [PubMed] [Google Scholar]
- 16.Prosser H, Walley T. New drug uptake: Qualitative comparison of high and low prescribing GPs’ attitudes and approach. Fam Pract. 2003;20:583–91. doi: 10.1093/fampra/cmg516. [DOI] [PubMed] [Google Scholar]
- 17.Peay MY, Peay ER. The role of commercial sources in the adoption of a new drug. Soc Sci Med. 1988;26:1183–9. doi: 10.1016/0277-9536(88)90149-9. [DOI] [PubMed] [Google Scholar]
- 18.Simon SR, Majumdar SR, Prosser LA, Salem-Schatz S, Warner C, Kleinman K, et al. Group versus individual academic detailing to improve the use of antihypertensive medications in primary care: A cluster-randomized controlled trial. Am J Med. 2005;118:521–8. doi: 10.1016/j.amjmed.2004.12.023. [DOI] [PubMed] [Google Scholar]
- 19.Prosser H, Almond S, Walley T. Influences on GPs’ decision to prescribe new drugs: The importance of who says what. Fam Pract. 2003;20:61–8. doi: 10.1093/fampra/20.1.61. [DOI] [PubMed] [Google Scholar]
- 20.Petursson P. GPs’ reasons for “non-pharmacological” prescribing of antibiotics: A phenomenological study. Scand J Prim Health Care. 2005;23:120–5. doi: 10.1080/02813430510018491. [DOI] [PubMed] [Google Scholar]
- 21.Søndergaard J, Foged A, Kragstrup J, Gaist D, Gram LF, Sindrup SH, et al. Intensive community pharmacy intervention had little impact on triptan consumption: A randomized controlled trial. Scand J Prim Health Care. 2006;24:16–21. doi: 10.1080/02813430500444916. [DOI] [PubMed] [Google Scholar]