Abstract
Objective
To investigate the relationship between blood pressure and medication adherence using electronic pillboxes (MEMS).
Setting
Five general practices in Bristol, UK.
Subjects
A total of 239 individuals with a clinical diagnosis of hypertension and being prescribed at least one blood pressure-lowering medication. Participants were asked to use the electronic pillbox as their drug bottle for at least one month.
Main outcome measures
“Timing adherence” (correct inter-dose intervals) as measured through MEMS and systolic (SBP) and diastolic (DBP) office blood pressure.
Results
Mean (±SD) timing adherence was 88% (±17),>80% in 175 (73%), and less than 50% in 11 (5%) participants. Adherence was monitored for a mean of 33 (±6) days. Mean (±SD) SBP was 147.9±19.1 mmHg and DBP 82.3±10.1 mmHg. There was no evidence to suggest that timing adherence was associated with SBP or DBP (overall correlation coefficients −0.01 and −0.02 respectively). According to current guidelines, about one in four of all participants had controlled SBP (only 6% of diabetic patients). DBP was under control in 66% of the individuals.
Conclusions
No relationship between adherence and blood pressure in patients with hypertension recruited from primary care was found. Average timing adherence measured by electronic monitors was high (88%) and blood pressure was controlled in a minority of patients. Our findings suggest that in terms of poor blood pressure control pharmacological non-response to or insufficient intensity of blood pressure-lowering medication might be more important than poor adherence to antihypertensive drug therapy.
Keywords: Adherence, blood pressure control, compliance, family practice, hypertension, primary care
Poor adherence to medication is often considered as a possible cause for uncontrolled hypertension.
No obvious relationship between adherence to antihypertensive medication and achieved blood pressure was found.
Average adherence to antihypertensive medication – measured by electronic monitors – was high (88%).
Systolic blood pressure was controlled in a minority of patients.
Blood pressure control is crucial to reduce the incidence of cardiovascular morbidity and mortality [1]. Although antihypertensive drugs are considered as powerful tools to reduce elevated blood pressure, arterial hypertension remains often poorly controlled [2]. Poor adherence to medication might be one explanation for unsatisfactory blood pressure control [3]. To date, there is little evidence as to whether adequate medication taking is directly related to achieved blood pressure. Studies using more imprecise methods such as serum assays [4], self-report [5], or pharmacy records [6] showed a positive correlation between adherence rates and blood pressure control. However, results from the few studies in which adherence to antihypertensive therapy was assessed by electronic monitors showed no convincing evidence of an association between medication taking and blood pressure control [7–9].
This study aimed to investigate the relationship between blood pressure and medikation taking using the “gold standard” for measuring adherence (electronic pillboxes, MEMS).
Material and methods
Subjects
Individuals were recruited prospectively from five general practices in Bristol, UK. The study was approved by the local Research Ethics Committee. Written informed consent was obtained from all participants.
During a three-month period, 374 patients attending their general practices with the clinical diagnosis of hypertension [10], [11] and being prescribed at least one blood pressure-lowering medication were identified using the GP's medical record system EMIS®. Forty-three (11.5%) patients were excluded because of severe cognitive impairment, known secondary cause of hypertension, use of a dose organizer, or other reasons given by the treating GP. Of the remaining 331 potentially eligible patients, 92 declined to take part in the study (no consent, too confusing to use electronic pill box, not attending their consultation). Eventually, 239 subjects agreed to participate.
Measuring adherence
Adherence was assessed by electronic pillboxes (Medical Event Monitoring System, MEMS, AARDEX, Ltd, Zug, Switzerland, http://www.aardex.ch). The electronic monitor consists of a container similar to traditional drug bottles and a larger lid, which holds a microchip and a pressure-release system. The monitor stores the exact time and date of each opening sequence and summary data can be downloaded onto a personal computer. Patients were asked to put a month's supply of one antihypertensive agent into the monitor. For cost and feasibility reasons, MEMS was used for only one antihypertensive drug per person. More commonly prescribed drugs (diuretics and beta-blockers) and medication with fewer daily doses were preferred.
Outcome measures
The first principal outcome was adherence measured by MEMS. Adherence was defined on the basis of “timing adherence”, the strictest definition for medication taking, which is the number of doses taken at 24±6 h for a once-daily regimen or 12±3 h for a twice-daily regimen, divided by the total number of days and multiplied by 100%. Patients were informed that their adherence would be monitored.
The second principal outcome was controlled systolic (SBP) and diastolic (DBP) blood pressure (<140 mmHg and < 90 mmHg in non-diabetic patients,<130 mmHg and < 80 mmHg in diabetics) [10], [11]. Blood pressure was measured by an automatic inflation blood pressure monitor (Omron® Healthcare Inc., Bannockburn, Illinois) by the practice nurse, who was instructed to apply the British Hypertension Society Guidelines [11].
Statistical analyses
Means and standard deviations (SDs) were calculated for each continuous measure, with unpaired t-tests used for differences between groups. Pearson's correlation coefficients (r) were calculated and scatter plots constructed to investigate the relationship between adherence and blood pressure. All analyses were performed using Stata®.
Results
Baseline characteristics of the study population are given in Table I. Two-thirds of participants were retired, 9 out of 10 were of Caucasian origin, and half had suffered from hypertension for more than five years. Participants were being prescribed a mean of 1.9 antihypertensive substances and they had been on this regimen for 6.5 months. Diuretics were the most frequently dispensed drug group from the pillboxes (41.4%), followed by beta blockers (20.1%), ACE inhibitors (19.3%), calcium channel blockers (12.1%), and others (7.1%). Three-quarters of participants took one (37.7%) or two (38.1%) antihypertensive medication(s). The vast majority of patients were on a once-daily regimen (96.7%). Adherence was monitored on a mean (±SD) of 33 (±6) days and a majority of participants returned administered pillboxes (90%). There was no difference between baseline systolic or diastolic blood pressure in patients who returned (n = 216) or did not return (n = 23) MEMS devices (respectively, SBP 145 mmHg vs. 148 mmHg, p = 0.46; DBP 83 mmHg vs. 82 mmHg, p = 0.57).
Table I.
Baseline characteristics of the study population (n = 216).
| Characteristic | Description |
| Mean age (years)±SD | 66.7±10.3 |
| Gender male, n (%) | 125 (52.3) |
| Mean body mass index (kg /m2)±SD | 29.4±5.9 |
| Non-smokers, n (%) | 203 (85) |
| Diabetes mellitus, n (%) | 74 (31) |
| SBP in all participants | 147.9±19.1 mmHg |
| DBP in all participants | 82.3±10.1 mmHg |
| SBP in non-diabetics (mean±SD) | 148 mmHg±19 |
| DBP in non-diabetics (mean±SD) | 82 mmHg±10 |
| SBP in diabetics (mean±SD) | 147 mmHg±19 |
| DBP in diabetics (mean±SD) | 83 mmHg±9 |
| Pillboxes available for analyses, n (%) | 216 of 239 (90) |
SBP relates to systolic blood pressure, DBP relates to diastolic blood pressure.
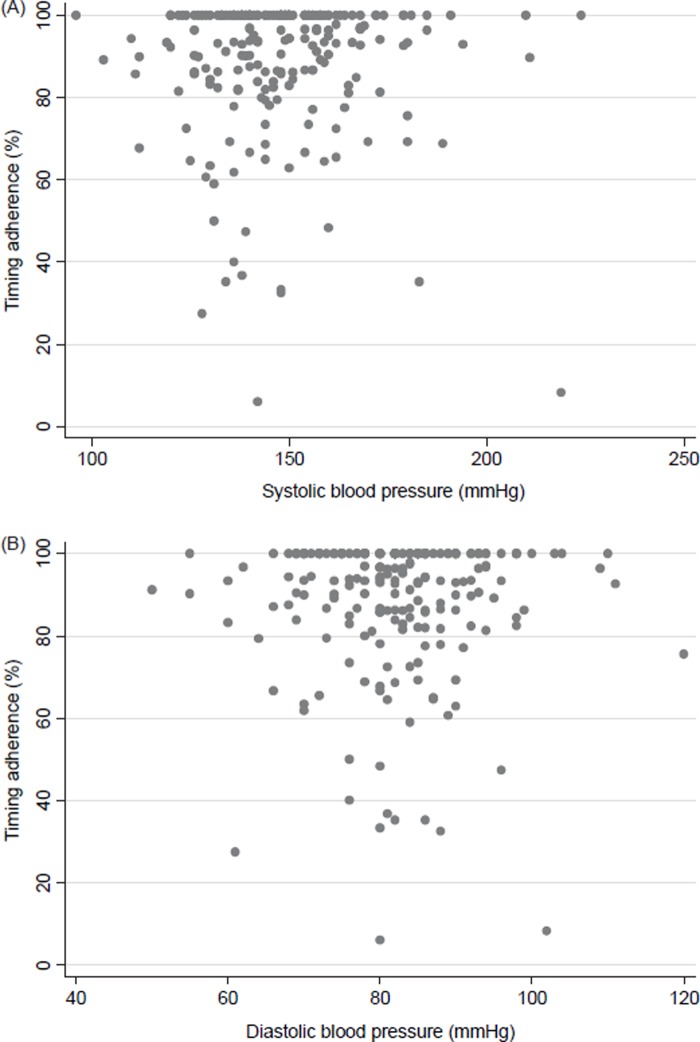
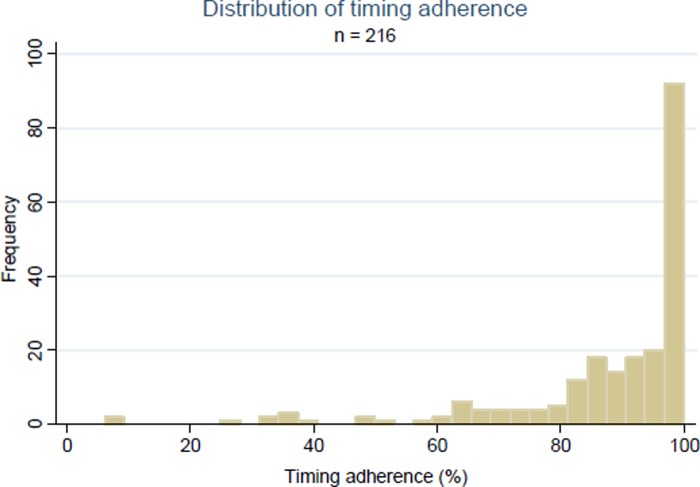
There was no evidence to suggest that timing adherence was associated with SBP (r = − 0.01) or DBP (r = − 0.02), with stratification by diabetes status having no effect on these results. Figure 1a and 1b show scatter plots of the relationship between timing adherence and blood pressure. Mean (±SD) timing adherence in all subjects with available adherence data (n = 216) was 88% (±17%). Timing adherence was > 80% in 175 (73%), and only in 11 (5%) patients was timing adherence less than 50% (Figure 2). To investigate a possible ceiling effect the correlations were recalculated after omitting the 88 individuals who had 100% timing adherence. No appreciable differences were found (r = − 0.02 for SBP, r = − 0.01 for DBP).
Figure 1.
Scatter plots of the relationship between timing adherence and systolic or diastolic blood pressure. (A) Mean systolic blood pressure±SD (upper panel) was 147.9±19.1 mmHg, (B) mean diastolic blood pressure (lower panel) was 82.3±10.1 mmHg.
Figure 2.
Distribution of timing adherence measured by MEMS in 216 individuals (follow-up rate 90%). Mean adherence in the whole sample 88%±17 (range 6–100). Frequency denotes number of participants.
Adherence rates in diabetic patients were lower compared with non-diabetic subjects (91% vs. 82%, p = 0.0003), but still over 80% on average. No relevant difference for adherence rates was found in diabetic or non-diabetic patients comparing subjects with controlled and uncontrolled blood pressure values (data not shown).
SBP (mean±standard deviation) was 147.9±19.1 mmHg and DBP 82.3±10.1 mmHg. Blood pressure targets [10], [11] were not achieved in nearly one-third of the non-diabetic study population, and only 6% of the participants with diabetes had adequate blood pressure control (Table II). Overall, about one in four participants had controlled blood pressure according to currently applied guidelines [10], [11].
Table II.
Controlled [10], [11] blood pressure in non-diabetic (<140 and < 90 mmHg) and diabetic patients (<130 and < 80 mmHg).
| SBP and DBP controlled | SBP controlled | DBP controlled | |
| Non-diabetics | 48 of 151 (32%) | 49 of 151 (32%) | 122 of 151 (81%) |
| Diabetics | 4 of 65 (6%) | 9 of 65 (14%) | 21 of 65 (32%) |
| Total | 52 of 216 (24%) | 58 of 216 (27%) | 143 of 216 (66%) |
SBP = systolic blood pressure; DBP = diastolic blood pressure. MEMS adherence data were available in 216 participants (151 non-diabetic and 65 diabetic patients).
Discussion
In this study we found no relationship between adherence to antihypertensive medication and achieved blood pressure. One in four individuals had their blood pressure controlled and timing adherence, the strictest definition of adherence using electronic monitors, was > 80% in nearly three-quarters of study population during the monitored period.
From a clinical point of view a correlation between adherence to medication and decrease in blood pressure would be plausible. However, no evidence to support this was found. In fact, our findings highlight that systolic blood pressure was not under control despite comparatively high adherence rates. As a consequence the question may arise whether in the studied population inadequate blood pressure control relates rather to non-response to or insufficient intensity of drug treatment than to poor adherence. In clinical practice this distinction is important for successful blood pressure management. According to the World Health Organization the evaluation of non-response to drug therapy also needs to address physician-related factors, which may affect the success of a pharmacological therapy [12]. Indeed, it has been shown in Europe and in the US that doctors may not be aggressive enough in their management of hypertension [13], [14] and appear to overestimate their adherence to hypertensive guidelines, particularly with regard to the proportion of their patients with controlled blood pressure [15]. This attitude of healthcare providers has been described as “clinical inertia”, that is “the failure to initiate or intensify therapy when indicated” [16]. In a qualitative study conducted among general practitioners in Merseyside, UK, GPs were asked why they do not implement evidence-based guidelines [17]. They identified several barriers to the management of hypertension in the elderly, such as doubts about the applicability of trial data to particular patients, poor adherence of GPs to practice protocols for hypertension, ageist attitudes of some GPs, absence of effective computer systems, or the absence of an educational mentor.
Insufficiently controlled blood pressure in the community is common. The latest Health Survey for England in 2003 demonstrated that 46% of patients had their blood pressure controlled to less than 140/90 mmHg. Using the same blood pressure targets as in the Health Survey [11], in the present study only about a quarter of participants had their blood pressure controlled. This is possibly due to the age distribution (there were substantially more individuals under the age of 40 in the National Survey) and proportion of individuals with diabetes (less diabetics in the National Survey). Similar results were found in a cross-sectional study from primary healthcare in southern Sweden [18]. Only around one-fifth (22.1%) of the patients had blood pressure readings below recommended levels (<140/90 mmHg). Consistent with the literature was the finding that diastolic blood pressure was better controlled than systolic blood pressure [18], [19].
Our findings are in line with previous reports that have assessed the relationship between adherence and blood pressure. A prospective investigation conducted by our group, of 159 patients from general practice with uncontrolled hypertension, found no evidence of an effect of timing adherence on blood pressure [9]. Three studies compared adherence (measured by MEMS devices) in subgroups of patients categorized according to achieved blood pressure [20–22]. The studies consistently showed that adherence in patients who achieved the target blood pressure was not different from adherence in patients who did not. In contrast, some evidence exists that higher adherence rates are associated with a higher reduction in systolic and/or diastolic blood pressure or higher percentages of patients with normalized blood pressure [23], [24]. The inconsistency of results is also demonstrated in a recent systematic review in which the authors concluded that there was no convincing evidence of poor adherence resulting in inadequate blood pressure [8]. To give an appropriate explanation for the variation of results of adherence studies is difficult. One may speculate that, first, the lack of agreement in definitions of adherence is a serious constraint. If studies are performed using the gold standard (electronic monitors) for measuring medication-taking, different definitions such as taking adherence (percentage of doses taken as prescribed), correct dosing (percentage of days on which doses are taken correctly), or timing adherence (correct inter-dose intervals) can be applied. For example, correct dosing better reflects deviations in the dosing history than taking adherence. Therefore, it is not surprising that studies using taking adherence as outcome measure result in higher adherence rates than studies using the more stringent correct dosing. Second, in order to compare study results accurately it is important to realize how the cut-off between satisfactory and unsatisfactory adherence was defined. Depending on the cut-off chosen the proportion of individuals with poor adherence may vary substantially [8]. Third, according to previous studies an inverse association between dose regimen and adherence rates is probable, that is, mean adherence rates are higher on a once-daily regimen compared with a twice-daily regimen [25]. Consequently, when comparing results of adherence studies it is essential to understand on which dosing regimens patients’ adherence rates were assessed.
A remarkable finding was the high mean timing adherence detected (88%). Two studies assessed timing adherence by electronic monitors in a similar primary care population and found comparative values for timing adherence (73–93%) [9], [26]. To some extent this finding is unexpected and challenges the common belief that adherence among patients suffering from chronic disease (such as hypertension) generally averages around 50% [12], [27]. Adherence to antihypertensive medication might be better than commonly considered, even if applying the strictest definition of adherence and using the accepted gold standard to assess antihypertensive medication-taking.
The present study has limitations. An overriding problem in measuring adherence is the possibility of a “Hawthorne effect” – that is, a change in patient behaviour as a result of being monitored in a study [28]. This is particularly true when the patient knows the methods being used to measure adherence, or anticipates negative consequences resulting from non-adherence. There is, however, some evidence from previous studies that there is no better adherence in patients who were informed that their drug intake was being monitored compared with those unaware of the monitoring [29], [30]. Another possible limitation is the comparatively short monitoring period (mean of 33 days). According to a recent systematic review, though, average adherence was not higher in studies with shorter monitoring periods [8] and the impact of using the MEMS device on adherence is considered to be short-lived [31]. In the present study, blood pressure readings were assessed cross-sectionally before the monitored period. Large-scale surveys, such as the Health Survey for England, were also based on a single visit to collect blood pressure data [32]. There is a potential for response bias, as patients refusing to participate were perhaps deterred from taking part because of the design (monitoring adherence). The possibility that those patients were less were adherent to medication remains speculative, but this should be borne in mind when interpreting the present findings. We also recognize that there will be many reasons for non-response to antihypertensive medication, including inadequate dose and inappropriate treatment; for this study we selected the medication on the basis of an agreed hierarchy that prioritized commonly used drugs.
In conclusion, our data suggest that in patients reasonably representing a primary care setting, pharmacological non-response to blood pressure-lowering medication might be more important than non- or unsatisfactory adherence in terms of poor blood pressure control. To further elucidate the relationship between adherence and blood pressure, studies are needed that concentrate on patients who have been identified by objective measures as being non-adherent.
Acknowledgements
This study was funded by the Swiss National Science Foundation; electronic pillboxes were sponsored by AARDEX Ltd, Zug, Switzerland.
References
- 1.Major outcomes in high–risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) JAMA. 2002;288:2981–97. doi: 10.1001/jama.288.23.2981. [DOI] [PubMed] [Google Scholar]
- 2.Wolf-Maier K, Cooper RS, Kramer H, et al. Hypertension treatment and control in five European countries, Canada, and the United States. Hypertension. 2004;43:10–17. doi: 10.1161/01.HYP.0000103630.72812.10. [DOI] [PubMed] [Google Scholar]
- 3.Rudd P. Clinicians and patients with hypertension: Unsettled issues about compliance. Am Heart J. 1995;30:572–9. doi: 10.1016/0002-8703(95)90368-2. [DOI] [PubMed] [Google Scholar]
- 4.Briggs WA, Lowenthal DT, Cirksena WJ, Price WE, Gibson TP, Flamenbaum W. Propranolol in hypertensive dialysis patients: Efficacy and compliance. Clin Pharmacol Ther. 1975;18:606–12. doi: 10.1002/cpt1975185part1606. [DOI] [PubMed] [Google Scholar]
- 5.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24:67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Podell RN, Kent D, Keller K. Patient psychological defenses and physician response in the long-term treatment of hypertension. J Fam Pract. 1976;3:145–9. [PubMed] [Google Scholar]
- 7.Schroeder K, Fahey T, Hollinghurst S, Peters TJ. Nurse-led adherence support in hypertension: A randomized controlled trial. Fam Pract. 2005;22:144–51. doi: 10.1093/fampra/cmh717. [DOI] [PubMed] [Google Scholar]
- 8.Wetzels GE, Nelemans P, Schouten JS, Prins MH. Facts and fiction of poor compliance as a cause of inadequate blood pressure control: A systematic review. J Hypertens. 2004;22:1849–55. doi: 10.1097/00004872-200410000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Schroeder K, Fahey T, Hay AD, Montgomery A, Peters TJ. Relationship between medication adherence and blood pressure in primary care: Prospective study. J Hum Hypertens. 2006;20:625–7. doi: 10.1038/sj.jhh.1002011. [DOI] [PubMed] [Google Scholar]
- 10.2003 European Society of Hypertension–European Society of Cardiology guidelines for the management of arterial hypertension. J Hypertens. 2003;21:1011–53. doi: 10.1097/00004872-200306000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Williams B, Poulter NR, Brown MJ, et al. British Hypertension Society guidelines for hypertension management 2004 (BHS-IV): summary. BMJ. 2004;328:634–40. doi: 10.1136/bmj.328.7440.634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sabeté E, et al. Adherence to long-term therapy: Evidence for action. GenevaSwitzerland: World Health Organization; 2003. [Google Scholar]
- 13.Berlowitz DR, Ash AS, Hickey EC, et al. Inadequate management of blood pressure in a hypertensive population. N Engl J Med. 1998;339:1957–63. doi: 10.1056/NEJM199812313392701. [DOI] [PubMed] [Google Scholar]
- 14.Hosie J, Wiklund I. Managing hypertension in general practice: Can we do better? J Hum Hypertens. 1995;9:S15–18. [PubMed] [Google Scholar]
- 15.Steinman MA, Fischer MA, Shlipak MG, et al. Clinician awareness of adherence to hypertension guidelines. Am J Med. 2004;117:747–54. doi: 10.1016/j.amjmed.2004.03.035. [DOI] [PubMed] [Google Scholar]
- 16.Phillips LS, Branch WT, Cook CB, et al. Clinical inertia. Ann Intern Med. 2001;135:825–34. doi: 10.7326/0003-4819-135-9-200111060-00012. [DOI] [PubMed] [Google Scholar]
- 17.Cranney M, Warren E, Barton S, Gardner K, Walley T. Why do GPs not implement evidence-based guidelines? A descriptive study. Fam Pract. 2001;18:359–63. doi: 10.1093/fampra/18.4.359. [DOI] [PubMed] [Google Scholar]
- 18.Hedblad B, Nerbrand C, Ekesbo R, et al. High blood pressure despite treatment: Results from a cross-sectional primary healthcare-based study in southern Sweden. Scand J Prim Health Care. 2006;24:224–30. doi: 10.1080/02813430601002134. [DOI] [PubMed] [Google Scholar]
- 19.Lloyd-Jones DM, Evans JC, Larson MG, O'Donnell CJ, Roccella EJ, Levy D. Differential control of systolic and diastolic blood pressure: Factors associated with lack of blood pressure control in the community. Hypertension. 2000;36:594–9. doi: 10.1161/01.hyp.36.4.594. [DOI] [PubMed] [Google Scholar]
- 20.Bertholet N, Favrat B, Fallab-Stubi CL, Brunner HR, Burnier M. Why objective monitoring of compliance is important in the management of hypertension. J Clin Hypertens (Greenwich) 2000;2:258–62. [PubMed] [Google Scholar]
- 21.Burnier M, Schneider MP, Chiolero A, Stubi CL, Brunner HR. Electronic compliance monitoring in resistant hypertension: The basis for rational therapeutic decisions. J Hypertens. 2001;19:335–41. doi: 10.1097/00004872-200102000-00022. [DOI] [PubMed] [Google Scholar]
- 22.Nuesch R, Schroeder K, Dieterle T, Martina B, Battegay E. Relation between insufficient response to antihypertensive treatment and poor compliance with treatment: A prospective case-control study. BMJ. 2001;323:142–6. doi: 10.1136/bmj.323.7305.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mallion JM, Dutrey-Dupagne C, Vaur L, et al. Benefits of electronic pillboxes in evaluating treatment compliance of patients with mild to moderate hypertension. J Hypertens. 1996;14:137–44. [PubMed] [Google Scholar]
- 24.Vaur L, Vaisse B, Genes N, Elkik F, Legrand C, Poggi L. Use of electronic pill boxes to assess risk of poor treatment compliance: Results of a large-scale trial. Am J Hypertens. 1999;12:374–80. doi: 10.1016/s0895-7061(98)00274-x. [DOI] [PubMed] [Google Scholar]
- 25.Claxton AJ, Cramer J, Pierce C. A systematic review of the associations between dose regimens and medication compliance. Clin Ther. 2001;23:1296–310. doi: 10.1016/s0149-2918(01)80109-0. [DOI] [PubMed] [Google Scholar]
- 26.Leenen FH, Wilson TW, Bolli P, et al. Patterns of compliance with once versus twice daily antihypertensive drug therapy in primary care: A randomized clinical trial using electronic monitoring. Can J Cardiol. 1997;13:914–20. [PubMed] [Google Scholar]
- 27.Haynes RB. McDonald H. Garg AX. Montague P. Interventions for helping patients to follow prescriptions for medications. Cochrane Database Syst Rev. 2002 doi: 10.1002/14651858.CD000011. CD000011. [DOI] [PubMed] [Google Scholar]
- 28.Wickstrom G, Bendix T. The “Hawthorne effect”—What did the original Hawthorne studies actually show? Scand J Work Environ Health. 2000;26:363–7. [PubMed] [Google Scholar]
- 29.McKenney JM, Munroe WP, Wright JT., Jr Impact of an electronic medication compliance aid on long-term blood pressure control. J Clin Pharmacol. 1992;32:277–83. doi: 10.1002/j.1552-4604.1992.tb03837.x. [DOI] [PubMed] [Google Scholar]
- 30.Mengden T, Binswanger B, Spuhler T, Weisser B, Vetter W. The use of self-measured blood pressure determinations in assessing dynamics of drug compliance in a study with amlodipine once a day, morning versus evening. J Hypertens. 1993;11:1403–11. doi: 10.1097/00004872-199312000-00013. [DOI] [PubMed] [Google Scholar]
- 31.Cramer JA, Scheyer RD, Mattson RH. Compliance declines between clinic visits. Arch Intern Med. 1990;150:1509–10. [PubMed] [Google Scholar]
- 32.Primatesta P, Poulter NR. Improvement in hypertension management in England: Results from the Health Survey for England 2006. J Hypertens. 2003;24:1193–200. doi: 10.1097/01.hjh.0000226210.95936.bc. [DOI] [PubMed] [Google Scholar]