In 2001, more than 500,000 people died from cancer in the U.S. Seven million people worldwide. That’s equivalent to the population of Chicago today. At the time, the standard treatment for cancer patients included surgery, radiation, and chemotherapy, which all too often had limited success. Years of immunological research focused on leveraging the human immune system to attack cancer had reached a point where advances were on the cusp of being ready to test in humans. The time was ripe to begin clinical trials, and Dr. Lloyd Old, then scientific director of the Ludwig Institute for Cancer Research (LICR) and director of the Cancer Research Institute’s (CRI) Scientific Advisory Council, recognized the cancer field needed to seize the moment. His vision: to create what he called “a grand instrument of clinical discovery” for cancer vaccines.
Under the leadership of Dr. Old and Ed McDermott, president of LICR, LICR had built a strong clinical trial infrastructure and had for some time been conducting clinical trials at its branches to further discoveries generated by the Institute around the world. CRI, on the other hand, had been supporting clinical research utilizing the typical academic model of a call for papers followed by peer review, but this model was not generating the impact the Institute had hoped for. This prompted a series of long discussions and debates between Dr. Old and Jill O’Donnell-Tormey, CRI’s executive director, about the need for a new way for CRI to fund clinical research.
“Wouldn’t it be remarkable,” Dr. Old said one day, “if we could set up a consortium of laboratory and clinical investigators carrying out early-phase clinical trials aimed at establishing the principles of effective vaccination with cancer antigens.” And, with that, the seed of the Cancer Vaccine Collaborative—CVC for short—was planted. Over the ensuing months, as the seed germinated and grew, it became clear that this new vision would require a worldwide network of scientists and clinicians. And so a long and fruitful partnership between CRI and LICR was forged. Our institutions shared common objectives—understanding the immunological response to cancer, harnessing that knowledge for patient benefit, and accelerating the translation of basic research into new cancer therapies—and appreciated that this could be accomplished most effectively by pooling our resources and complementary expertise. It was Lloyd who “brokered” the relationship, and Ed McDermott often joked about the administrative “dating service” he was running.
So our organizations set out to establish a coordinated academic research program to develop therapeutic vaccines for the treatment of cancer. Underpinning the effort was our common belief that if cancer vaccines were ever to enter routine clinical practice, they would need to be rigorously studied in a far-reaching, goal-oriented manner. Such an undertaking was beyond the reach of any individual researcher and too experimental to capture the interest of industry. We viewed the CVC as the “missing link” in biomedical research—bridging the divide between hypothesis-based investigation in academic laboratories and drug development in the pharmaceutical industry. Importantly, the CVC would not only empower the research community, but would ultimately benefit cancer patients by making available to them an increased arsenal of therapeutic options.
To rationally design optimally effective cancer vaccines, we believed that it would be necessary to: (1) identify and access multiple agents, each of which would play a unique and complementary role in stimulating the anti-tumor immune response; and (2) integrate clinical studies with in-depth immunological monitoring to gain insights into a vaccine’s effect on the immune response. This approach, we hoped, would enable the continuous improvement of vaccine formulations to maximize the immune response, as well as allow us to correlate immune response parameters with clinical outcomes. As we fleshed the model out more, the focus and mandate of the CVC sharpened. The network would design and run early-phase, single-variable, iterative trials. The objective would be to establish the very principles of effective immunization with defined cancer antigens, parsing the true effect of each vaccine component, as well as its synergistic contribution to the efficacy of the vaccine as a whole. Thus, through the CVC, we would put to the test one of Lloyd’s favorite mantras: “You won’t know how to vaccinate until you know how to immunize. And you won’t know how to immunize until you know how to monitor.”
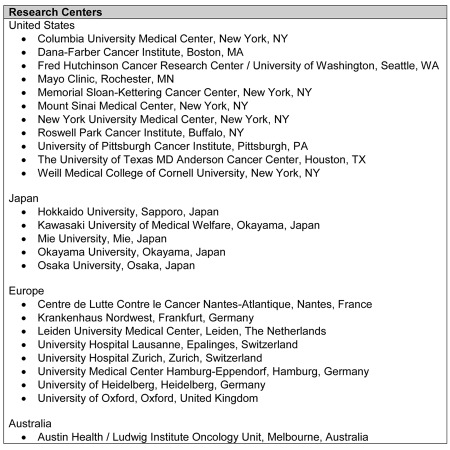
CVC trial sites would be selected based on their immunological excellence and expertise, access to patients, interest in cancer vaccine development, and willingness to work together. Employing these criteria, we chose the first three sites: Weill Cornell Medical College, to carry out a program in non-small cell lung cancer (NSCLC); Columbia Presbyterian Medical Center, to focus on clinical trials of melanoma; and Mount Sinai Medical Center, which would test therapeutic vaccines for prostate cancer. The network quickly expanded, and today includes 22 sites on four continents. A list of sites participating in the CVC since its inception is provided in Table 1.
Table 1.
CVC Sites, 2001-present
More than 50 CVC clinical trials have been conducted over the past 11 years, the majority focusing on NY-ESO-1, a Cancer/Testis (CT) antigen discovered and patented by LICR. Research by investigators in the CVC and elsewhere has shown that patients who have preexisting immunity to NY-ESO-1 are more likely to respond to immunotherapy treatments. In addition, CVC trials have compiled the largest survey of the immunological response to a single tumor antigen, which established that NY-ESO-1 is one of the most immunogenic antigens tested to date. As Dr. Old would often remark, more is known about the immune response to NY-ESO-1 vaccination than is known about the immune response to flu, which was one of the most well-researched antigens at the time.
It should be noted that, in addition to conducting these early-phase clinical trials, the CVC has also made great advances in developing new tools to enable better measurement of immune responses to cancer vaccination, determining the relationship between these responses and clinical outcomes, developing strategies to acquire and produce clinic-grade vaccine agents, identifying new cancer antigens that can be developed and tested as vaccine targets, and refining tests and biomarkers that will better predict patients’ immune responses to particular vaccine constructs. It is also gratifying to see that CVC activities have encouraged significantly expanded infrastructure and support for cancer vaccine clinical trials throughout the world.
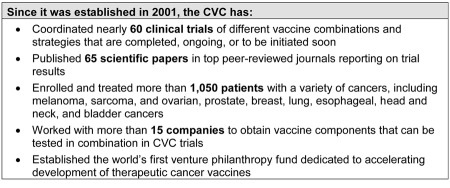
With its collective knowledge and sophisticated immune monitoring capabilities, the CVC has now developed vaccines that can consistently produce integrated immune responses in a significant percentage of patients in CVC trials and monitor these responses with a degree of precision that was impossible just ten years ago, fulfilling a key initial goal of the CVC. The CVC’s major accomplishments to date are highlighted in Table 2.
Table 2.
Select accomplishments of the CRI/LICR Cancer Vaccine Collaborative
Our experience, however, has also revealed that the puzzle is even more complex than originally anticipated. We have learned some important lessons along the way: that careful patient selection is paramount if vaccines are to have an optimal effect; that vaccines must be designed to contemplate heterogeneous antigen expression; and that controlling the power of the immune system—by either harnessing it to attack tumors or, on the contrary, releasing the breaks to enable therapies to work—is essential. The successes and the failures have provided invaluable insights that have informed the design of each new iteration of clinical trials in the network. And all of it is documented in the more than 60 published papers reporting on the results of CVC trials.
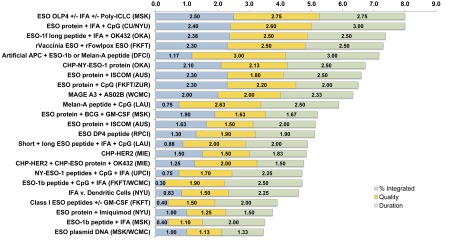
To obtain a global picture of these results and assess the evolution of CVC trials toward our ultimate goal of developing an optimal vaccine formulation, last year, in anticipation of the CVC’s 10th anniversary, we conducted an analysis of the immunological results from all CVC trials completed to date. Taking the published data from 22 completed CVC trials, as well as unpublished data from a recently completed trial, we asked five separate CVC labs to evaluate the data and score the results. The immunological response data were evaluated within three categories: (1) percentage of patients who demonstrated integrated immune responses, defined as antibody, CD4 T cell, and CD8 T cell responses; (2) quality of immune responses, as demonstrated by such factors as epitope spreading, recognition of naturally processed antigen, TCR avidity, ex vivo detection, and/or polyfunctionality; and (3) duration of immune responses, i.e., length of time that immune responses could be detected after the last vaccine dose. Reviewers provided a score of 0 to 3 for each category, the scores in each category were averaged, and the three averages were then summed to obtain an overall score for each trial (highest possible = 9). The results of this are shown in Figure 1.
Figure 1.
Ranking of CVC trials by immune response data. The chart represents the results of an analysis of immune response data from all completed CVC trials to date. For each trial, immune response data were reviewed by 5 independent CVC investigators and given a score of 0 to 3 in each of three categories: (1) percentage of patients who demonstrated integrated immune responses, defined as antibody, CD4 T cell, and CD8 T cell responses; (2) quality of immune responses, as demonstrated by such factors as epitope spreading, recognition of naturally processed antigen, TCR avidity, ex vivo detection, and/or polyfunctionality; and (3) duration of immune responses, i.e., length of time that immune responses could be detected after the last vaccine dose. Reviewers’ scores were averaged within each category, and then the average for each category was summed to obtain an overall score for each trial. Overall scores ranged from 3.46 (NY-ESO-1 DNA vaccine) to 8.00 (NY-ESO-1 overlapping peptides + Montanide + Poly-ICLC; NY-ESO-1 recombinant protein + Montanide + CpG).
One of the most significant achievements of the CVC, as the chart demonstrates, is that it has helped to narrow the possibilities as to the best way to create an antigen-specific cancer vaccine that stimulates potent integrated immune responses of high quality and durability in patients. According to the data, the vaccines with the highest efficacy have utilized long peptides or protein combined with TLR agonists, potent stimulators of innate immunity. With this knowledge, we now have a strong guide for the design of cancer vaccines that can consistently induce broad, robust, and long-lasting immune responses in patients.
These insights, combined with observations of clinical benefit in some of these trials and advances in the field that have highlighted the need to combine vaccines with immune modulators such as checkpoint blockades, will allow the CVC in the near future to undertake more and more trials that will deliver consistent and real clinical benefit to the patients enrolled.
Resources that will enable the CVC to have access to the agents we need to combine with vaccines remains a challenge for the CVC. To overcome this, in 2008, we began to develop a strategy for a venture philanthropy fund that could enable us to obtain assured and sustained access to the very agents whose value for patients we had proven in our own trials. Our solution—the Cancer Vaccine Acceleration Fund—was launched in 2010, and has since brought two of the CVC’s highest-priority reagents into the CVC community for testing: Poly-ICLC, a TLR3 agonist that has proven to be one of the most powerful adjuvants tested in CVC trials to date; and an anti-GITR antibody, an immune modulator to be tested as a single agent in a first-in-human study and potentially later combined with the CVC’s vaccine formulation to potentiate the vaccine-induced anti-tumor response. Going forward, CVAF will be a core component of the CRI/LICR clinical strategy to accelerate the development and refinement of cancer immunotherapies that hold the most promise to benefit patients in the near term, bringing us closer to realizing Dr. Old’s full vision of what the CVC could achieve.
Recognizing the enormous challenge inherent in the development and refinement of immunotherapies, a decade ago LICR and CRI joined forces to develop the CVC, a global network of clinical investigators and immunology labs that could work alongside industry to improve cancer outcomes. Looking back, we realize how little was truly known about the human immune response to cancer antigens and to cancer vaccination. The phenomena of checkpoint blockade and tumor-induced immunosuppression were just beginning to be understood. Only the year before the CVC began, in 2000, were clinical trials of the anti-CTLA-4 antibody begun, and only a year after, in 2002, were the first studies published. But today, ten years later, we have the benefit of new knowledge, new resources, and a wealth of new opportunities—opportunities to incorporate anti-CTLA-4 into vaccine trials, to introduce into the mix new immune reagents that are emerging at an increasingly rapid pace, and to establish new partnerships with groups such as the NCI’s Cancer Immunotherapy Trials Network. These will enable us to more fully capitalize on the power of these medicines to bring to patients some of the most effective cancer immunotherapies seen to date. With the selection and installment of Dr. Jedd Wolchok of Memorial Sloan-Kettering Cancer Center—whose commentary in this issue can offer some additional details about the CVC’s plans moving forward—as Lloyd Old’s successor as the director of the CVC, we have new leadership and a renewed commitment to the clinical trial model that CRI and LICR brought to life. Over the next decade it is our hope and expectation that the CVC will have even greater impact on the development of effective immunotherapies, benefitting patients of all types of cancer.
Abbreviations
- LICR
Ludwig Institute for Cancer Research;
- CRI
Cancer Research Institute;
- CVC
Cancer Vaccine Collaborative