Abstract
The vast majority of diabetes-related self-management technology utilizes small visual displays (SVDs) that often produce a low level of contrast and suffer from high levels of reflection (glare). This is a major accessibility issue for the 3.5 million Americans with diabetes who have reduced vision. The purpose of this article is to gather comparative data on the key display attributes of the SVDs used in blood glucose meters (BGMs) and home blood pressure monitors (HBPMs) on the market today and determine which displays offer the best prospect for being accessible to people with reduced vision.
Nine BGMs and eight HBPMs were identified for this study on the basis of amount of devices sold, full-functionality speech output, and advanced display technologies. An optical instrumentation system obtained contrast, reflection (glare), and font height measurements for all 17 displays.
The contrast, reflection, and font-height values for the BGMs and HBPMs varied greatly between models. The Michelson contrast values for the BGMs ranged from 11% to 98% and font heights ranged 0.39–1.00 in. for the measurement results. The HBPMs had Michelson contrast values ranging 55–96% and font height ranging 0.28–0.94 in. for the measurement results.
Due largely to the lack of display design standards for the technical requirements of SVDs, there is tremendous variability in the quality and readability of BGM and HBPM displays. There were two BGMs and one HBPM that exhibited high-contrast values and large font heights, but most of the devices exhibited either poor contrast or exceptionally high reflection.
Keywords: accessibility, blood glucose meters, blood pressure monitors, diabetes, displays, reduced vision, visual impairment
Introduction
Since the early 2000s, the American Foundation for the Blind has been focusing on the interface design of diabetes-related self-management technology such as blood glucose meters (BGMs), insulin pumps, home blood pressure monitors (HBPMs), and insulin pens. The reason for this is that, of the over 18 million people diagnosed with diabetes, 13.6% (2.5 million) are reported to have low vision brought on by diabetic retinopathy.1 An additional 1.3 million persons with diabetes report having visual impairments not caused by diabetic retinopathy, which includes age-related vision loss.2
The ability to use home diabetes-related self-management technology properly is recognized as of critical importance for persons with both type 1 and type 2 diabetes. The American Diabetes Association recommends self-monitoring of blood glucose for all persons with type 1 and type 2 diabetes being treated with insulin to be carried out three or more times daily.3 Additionally, persons with type 2 diabetes have an increased risk for hypertension and cardiovascular disease, and organizations such as the American Heart Association recommend that persons with type 2 diabetes and hypertension monitor their blood pressure regularly through the use of HBPMs.4,5
The vast majority of BGMs and HBPMs currently on the market do not offer any speech output and provide the critical data only through a small visual display (SVD).6 Furthermore, the vast majority of diabetes equipment utilize SVDs that produce a low level of contrast and often suffer from high levels of reflection (glare). There is a clear need for diabetes-related self-management tech-nology that is accessible to the 3.8 million visually impaired persons with diabetes.2 The purpose of this article is to gather comparative data on the key attributes of the SVDs used in BGMs and HBPMs on the market today and determine which displays offer the best prospect for being accessible to those visually impaired persons who have sufficient remaining vision to be able to read print.
The most significant changes that can be made to improve the accessibility of a display involve increasing the display’s contrast, improving the size and type of displayed characters, and reducing the effect of reflection on the screen.7–9 There are accepted standards for the minimum display characteristics of these types of displays, but none of these standards account for the specific needs of low-vision users.10,11
Typically, most high-quality displays exhibit Michelson contrast levels of 70–90%, with anything above 90% being excellent, and the American Printing House for the Blind (APH) defines large print for low-vision users as any text size above 18 point.12 Printed Arial 18-point font has a physical height of 0.18 in., which should serve as the minimum standard for font height. High levels of reflection caused by a display’s clear protective covering can reduce the perceived contrast of the display by as much as 90% in extreme cases. It is therefore reasonable to set guidelines for display accessibility as a high level of contrast that is not heavily affected by reflection and a font size of at least 0.18 in.
Methods
A total of nine BGMs and eight HBPMs on the U.S. market in 2011 were acquired and measured as part of this study. The selection of devices provides a sampling of the best-selling devices from a major retailer as well as any devices that offer full-functionality speech output and any devices that utilize advanced display technology.
Nearly all BGMs use liquid crystal display (LCD) technology, which is the most prevalent display technology in SVDs. Two BGMs that use organic light emitting diode (OLED) displays were included as part of this study, the G90 from Fora Care Inc. (Newbury Park, CA) and Contour USB from Bayer Diabetes Care (Tarrytown, NY). Additionally, four BGMs that were identified in a separate study as having full-functionality speech output were included, the Embrace No Code from Omnis Health (Conway, AR), V20 from Fora Care Inc., Prodigy Voice from Prodigy Diabetes Care LLC (Charlotte, NC), and Solo V2 from BioSense Medical Devices (Duluth, GA).6 Also included were the three top-selling BGMs from a major retailer, TRUE2go from Nipro Diagnostics (Fort Lauderdale, FL) and the OneTouch UltraMini and OneTouch Ultra2 from LifeScan Inc. (Milpitas, CA).13
The HBPMs included as part of this study followed the same criteria as the BGMs. The only HBPM identified that did not use LCD technology, the BP785 from Omron Healthcare Inc. (Lake Forest, IL), was included as part of this study. There are several HBPMs on the market that offer full-functionality speech output, such as the UA-767T from A&D Medical (Milpitas, CA) and the Reizen from MaxiAids (Farmingdale, NY), but the displays from these HBPMs had been measured in a previous study.14 The remaining HBPMs were identified as the top-selling HBPMs from a major retailer and include both wrist and arm HBPMs: the BP-103H from NatureSpirit (Dallas, TX), TV3649 from Jobar International Inc. (Carson, CA), BP652 from Omron Healthcare Inc., BP2M from Ozeri USA (San Diego, CA), EW3109 from Panasonic Corporation of North America (Secaucus, NJ), BP3MC1-PC from Microlife USA Inc. (Clearwater, FL), and the HEM-741CREL from ReliOn (Bannockburn, IL).15 Figures 1 and 2 show images of all the HBPMs and BGMs included in this study.
Figure 1.
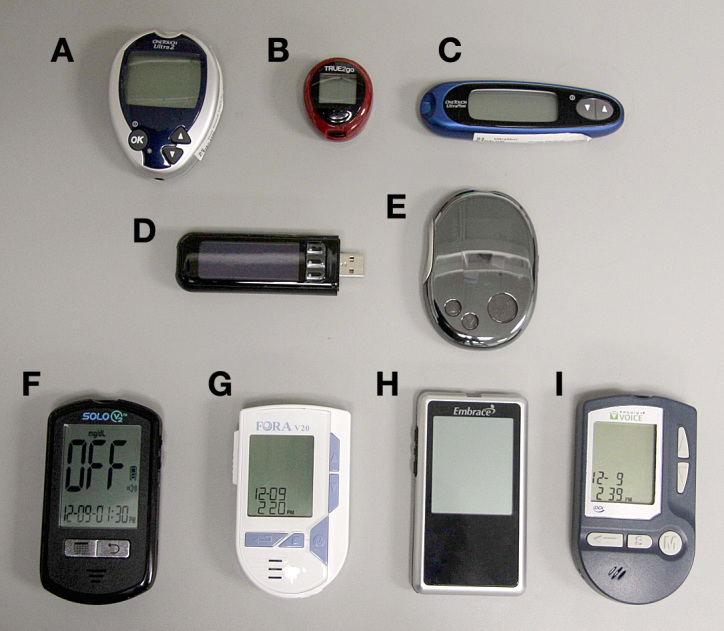
The BGMs included in this study: (A) OneTouch Ultra2, (B) TRUE2go, (C) OneTouch UltraMini, (D) Contour USB, (E) Fora G90, (F) Solo V2, (G) Fora V20, (H) Embrace No Code, and (I) Prodigy Voice.
Figure 2.

The HBPMs included in this study: (A) BP-103H, (B) HEM-741CREL, (C) BP3MC1-PC, (D) EW3109, (E) BP2M, (F) BP652, and (G) TV3649.
To measure the display characteristics of SVDs, an optical instrumentation system (shown and described in Figure 3) was used to capture and process images of the displays. Contrast and reflection measurements were obtained through measuring each display in three different lighting conditions: sunlight conditions (very high levels of ambient light, E = 20,000), office conditions (moderate levels of ambient light, E = 500), and night conditions (very low levels of ambient light, E = 1). Contrast measurements were calculated by measuring the luminance values of the displayed characters and background in each lighting condition and using the Michelson contrast formula to express the contrast as a percentage.8 For all devices with reflective displays that had a backlight that is under the user control, the measures were taken without the backlight.
Figure 3.

Optical instrumentation system. The system consists of a large sampling sphere that projects a specified level of light onto the target display. An image of the display is then taken with a Canon EOS digital camera and luminance measurements of the display are taken by the Minolta light meter. This information is sent to the dedicated personal computer for analysis.
Results
Table 1 shows the display measurements of the BGM displays. The display measurements for the BGMs varied significantly between models. All BGMs with LCD tech-nology use reflective displays, which maintain a constant contrast value in both sunlight and office conditions but are not readable at night or in low-level lighting. This can be an issue for any persons with diabetes needing to test their blood sugar in the middle of the night. The contrast values of the LCD BGMs varied from 34.6% to 91.8%, and the font heights for the measure-ment results ranged 0.38–1.00 in. (the font height does not refer to any of the auxiliary text or information). The two OLED BGMs also exhibited a wide range of contrast values. In night and office conditions, the two OLED BGMs had contrast values of 85.8% to 98.6%, but in sunlight conditions, the contrast value of both BGMs dropped by over 80%. The OLED BGMs both use a reverse polarity (white-on-black) color scheme, which is the preferred color scheme for many low-vision users.
Table 1.
Blood Glucose Meter Results
| Display technology | Display screen area (sq. in.) | Font height (in.) | Contrast (sunlight) | Contrast (office) | Contrast (night) | Reverse polarity | |
|---|---|---|---|---|---|---|---|
| TRUE2go | LCD | 0.48 | 0.39 | 89.8% | 89.8% | - | No |
| OneTouch UltraMini | LCD | 1.26 | 0.53 | 40.5% | 40.5% | - | No |
| OneTouch Ultra2 | LCD | 1.54 | 0.55 | 34.6% | 34.6% | - | No |
| Solo V2 | LCD | 2.90 | 1.00 | 73.9% | 73.9% | - | No |
| Embrace No Code | LCD | 2.95 | 0.55 | 91.8% | 91.8% | - | No |
| Fora V20 | LCD | 1.85 | 0.55 | 53.0% | 53.0% | - | No |
| Fora G90 | OLED | 1.21 | 0.40 | 11.7% | 85.8% | 98.6% | Yes |
| Prodigy Voice | LCD | 1.92 | 0.63 | 83.6% | 83.6% | - | No |
| Contour USB | OLED | 1.33 | 0.29 | 11.9% | 85.1% | 99.4% | Yes |
Table 2 shows the display measurements for the HBPM displays. As with LCD BGMs, all LCD HBPMs are reflective and not usable at night. With the exception of the BP3MCI-PC, the seven LCD HBPMs had very similar display characteristics, with contrast values ranging 71.9–82.1% in office and sunlight conditions. The three wrist HBPMs all had font heights for the measurement results ranging 0.29–0.39 in., whereas the arm HBPMs had significantly larger font sizes for the measurement results, ranging from 0.66 to 0.94. The BP785 was the only HBPM to feature an OLED display, and it demonstrated much higher contrast values than the LCD HBPMs in all light conditions.
Table 2.
Home Blood Pressure Monitor Results
| Display technology | Display screen area (sq. in.) | Font height (in.) | Contrast (sunlight) | Contrast (office) | Contrast (darkroom) | Reverse polarity | |
|---|---|---|---|---|---|---|---|
| BP-103H | LCD | 7.10 | 0.94 | 82.1% | 82.1% | - | No |
| TV3649 | LCD | 1.19 | 0.28 | 71.9% | 71.9% | - | No |
| BP652 | LCD | 2.24 | 0.39 | 76.8% | 76.8% | - | No |
| BP785 | OLED | 7.12 | 0.75 | 90.8% | 95.7% | 96.2% | Yes |
| BP2M | LCD | 1.49 | 0.30 | 74.3% | 74.3% | - | No |
| EW3109 | LCD | 4.05 | 0.66 | 79.1% | 79.1% | - | No |
| BP3MC1-PC | LCD | 5.50 | 0.70 | 54.8% | 54.8% | - | No |
| HEM-741CREL | LCD | 4.00 | 0.65 | 74.8% | 74.8% | - | No |
Discussion and Conclusion
There is a clear need for diabetes-related self-management technology that is accessible for users with reduced vision. Although there are existing standards for these types of displays that provide a framework for how to improve display quality, in particular, the AAMI/ANSI HE75 standard,10 none of these standards account for the specific needs of low-vision users. As such, there is tremendous variability in the quality and readability of BGM and HBPM displays. This variability is evidenced through the measurements taken of these devices—the contrast values in a typical office setting ranged 34–95%, and the font height for the measurement results ranged 0.28–1.00 in. Without seeing the devices firsthand, it can be difficult for a visually impaired person to realize the differences between displays. It is therefore conceivable that this person may choose a device with a SVD that they have difficulty reading or cannot read at all.
Of the BGMs measured for this study, it was the top-selling models that had the least accessible displays. The OneTouch UltraMini and Ultra2 exhibited the lowest contrast values of all the displays measured, and the TRUE2go had the smallest font height among the BGMs. The BGMs with the backlit OLED displays, the G90 and Contour USB, both had relatively small font height and poor sunlight contrast. It was the BGMs with speech output that offered the highest level of readability. In particular, the Prodigy Voice and Solo V2 both exhibited large and easily discernable characters with high contrast values. By offering a combination of a more easily readable display and full-functionality speech output, these two BGMs offer the highest level of accessibility for users with reduced vision.
The two OLED BGM displays both exhibited excessive reflection and relatively small fonts. However, the HBPM with an OLED display, the Omron BP785, was the most readable display measured. The BP785 exhibited contrast levels greater than 90%, even in sunlight conditions, and displayed large characters of 0.75 in. All HBPMs with LCD technology offered only average levels of contrast, but the font height for the arm HBPMs was significantly larger than the wrist HBPMs.
All the displays exhibited font heights of at least 0.28 in., well above the 0.18 in. recommended by the APH, but the lack of consistency in contrast values is problematic. It is also important to note that the lowest contrast values were exhibited by some of the top-selling BGM models on the market. These devices are far more well known, more likely to be prescribed by physicians, and more likely to be covered by insurance carriers. Fortunately, higher-quality backlit displays have become increasingly common in home medical devices, which offer the potential for more accessible devices, but too many of these products utilize poor quality displays. This problem of SVD inaccessibility is likely to continue until SVD design standards are developed for a minimum level of contrast and font height. Additionally, major BGM and HBPM manufacturers will need to implement those standards when designing new products.
Acknowledgments
The authors acknowledge the assistance provided by Marshall University interns William Reuschel and John Lilly.
Glossary
Abbreviations
- (APH)
American Printing House for the Blind
- (BGM)
blood glucose meter
- (HBPM)
home blood pressure monitor
- (LCD)
liquid crystal display
- (OLED)
organic light emitting diode
- (SVD)
small visual display
Funding
Support was provided by the National Institute for Disability and Rehabilitation Research.
Disclosure
The American Foundation for the Blind received a donation from Prodigy Diabetes Care in 2008.
References
- 1.Centers for Disease Control and Prevention. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention: 2011. National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011. http://www.cdc.gov/Diabetes/pubs/pdf/ndfs_2011.pdf. [Google Scholar]
- 2.Pleis JR, Ward BW, Lucas JW. Summary health statistics for U.S. adults: National Health Interview Survey, 2009. National Center for Health Statistics. Vital Health Stat 10(249) 2010. www.cdc.gov/nchs/data/series/sr_10/sr10_249.pdf. [PubMed]
- 3.American Diabetes Association. Standards of medical care in diabetes--2012. Diabetes Care. 2012;35(Suppl. 1):S11–63. doi: 10.2337/dc12-s011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American Heart Association. Cardiovascular disease & diabetes. 2010. http://www.heart.org/HEARTORG/Conditions/Diabetes/WhyDiabetesMatters/Cardiovascular-Disease-Diabetes_UCM_313865_Article.jsp#.TzIayOWil_Q.
- 5.American Heart Association. Home blood pressure monitoring. 2011 http://www.heart.org/HEARTORG/Conditions/HighBloodPressure/SymptomsDiagnosisMonitoringofHighBloodPressure/Home-Blood-Pressure-Monitoring_UCM_301874_Article.jsp#.TzIbGuWil_Q. [Google Scholar]
- 6.Burton DM, Enigk MG, Lilly JW. Blood glucose meters and accessibility to blind and visually impaired people. J Diabetes Sci Technol. 2012;6(2):242–245. doi: 10.1177/193229681200600205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rubin GS, Legge GE. Psychophysics of reading. VI--the role of contrast in low vision. Vision Res. 1989;29(1):79–91. doi: 10.1016/0042-6989(89)90175-2. [DOI] [PubMed] [Google Scholar]
- 8.Patching GR, Jordan TR. Spatial frequency sensitivity differences between adults of good and poor reading ability. Invest Ophthalmol Vis Sci. 2005;46(6):2219–2224. doi: 10.1167/iovs.03-1247. [DOI] [PubMed] [Google Scholar]
- 9.Schuchard RA, Naseer S, de Castro K. Characteristics of AMD patients with low vision receiving visual rehabilitation. J Rehabil Res Dev. 1999;36(4):294–302. [PubMed] [Google Scholar]
- 10.Association for the Advancement of Medical Instrumentation. Human factors engineering--design of medical devices. ANSI/AAMI HE75. 2009.
- 11.Netherlands Organisation for Applied Scientific Research. Portable in-vitro blood monitor systems for (self)-monitoring; general requirements and test methods. TNO PG/TG/2001.044. http://www.tnokeur.nl/connect/binary/retrieveFile?instanceid=20&itemid=131&filename=Algemene+eisen+voor+kwantitatieve+bloed+controle+systemen.pdf&style=home.
- 12.Kitchel JE. APH guidelines for print document design. http://www.aph.org/edresearch/lpguide.htm.
- 13.Amazon.com. Amazon best sellers: best sellers in blood glucose monitors. http://www.amazon.com/Best-Sellers-Health-Personal-Care-Blood-Glucose-Monitors/zgbs/hpc/3777171. Accessed November 15, 2011. [Google Scholar]
- 14.Uslan MM, Burton DM, Wilson TE, Taylor S, Chertow BS, Terry JE. Accessibility of home blood pressure monitors for blind and visually impaired people. J Diabetes Sci Technol. 2007;1(2):218–227. [PMC free article] [PubMed] [Google Scholar]
- 15.Amazon.com. Amazon best sellers: best sellers in blood pressure monitors. http://www.amazon.com/Best-Sellers-Health-Personal-Care-Blood-Pressure-Monitors/zgbs/hpc/3777151/ref=zg_bs_nav_hpc_4_3777171. Accessed November 15, 2011. [Google Scholar]


