Abstract
Background
Patients consider multiple parameters in adjusting prandial insulin doses for optimal glycemic control. Difficulties in calculations can lead to incorrect doses or induce patients to administer fixed doses, rely on empirical estimates, or skip boluses.
Method
A multicenter study was conducted with 205 diabetes subjects who were on multiple daily injections of rapid/short-acting insulin. Using the formula provided, the subjects manually calculated two prandial insulin doses based on one high and one normal glucose test result, respectively. They also determined the two doses using the FreeStyle InsuLinx Blood Glucose Monitoring System, which has a built-in, automated bolus calculator. After dose determinations, the subjects completed opinion surveys.
Results
Of the 409 insulin doses manually calculated by the subjects, 256 (63%) were incorrect. Only 23 (6%) of the same 409 dose determinations were incorrect using the meter, and these errors were due to either confirmed or potential deviations from the study instructions by the subjects when determining dose with meter. In the survey, 83% of the subjects expressed more confidence in the meter-calculated doses than the manually calculated doses. Furthermore, 87% of the subjects preferred to use the meter than manual calculation to determine prandial insulin doses.
Conclusions
Insulin-using patients made errors in more than half of the manually calculated insulin doses. Use of the automated bolus calculator in the FreeStyle InsuLinx meter minimized errors in dose determination. The patients also expressed confidence and preference for using the meter. This may increase adherence and help optimize the use of mealtime insulin.
Keywords: blood glucose monitoring, bolus calculator, insulin dose, manual calculation
Introduction
There are many challenges for patients on multiple daily injections (MDIs) of insulin in managing their diabetes. Accurate calculation of insulin boluses is one of the challenges in intensive insulin regimens. Patients must take into account multiple parameters, including carbohydrate intake, insulin-to-carbohydrate ratio (insulin sensitivity factor), blood glucose levels, glucose correction factor, and correction target. Difficulties in performing manual calculation can lead to incorrect dose determinations or induce patients to administer fixed doses, rely on empirical estimates, or skip boluses.1 We evaluated the frequency of errors for insulin-using patients to calculate mealtime doses of short/rapid-acting insulin and compared it with using a glucose meter that has a built-in, automated bolus calculator for patients on MDI therapy.
Methods
Insulin Calculator
The FreeStyle InsuLinx Blood Glucose Monitoring System (Abbott Diabetes Care, Alameda, CA) has a built-in, automated bolus calculator. It also provides the user with electronic logbook functions that store data such as insulin and medication doses, food intake, amount of exercise, and health information. There are two modes of operation: easy mode for patients who use fixed doses of rapid-acting insulin for meals and advanced mode for patients who count carbohydrates, in grams or servings, to adjust their rapid-acting insulin doses for meals. An access code is provided by the manufacturer to the health care professional for setting up the meter by selecting either easy mode or advanced mode and entering parameters (e.g., insulin-to-carbohydrate ratio, glucose correction factor, correction target) specific to each patient. If the meter is set up for easy mode, a calculator button will be displayed with each blood glucose test result on the meter touch screen (Figure 1). When the user taps the calculator button, a display will prompt the user to choose the type of meal (breakfast, lunch, dinner, no meal). Once the user selects a meal, the meter will display a suggested insulin dose. The user may tap the up/down button to adjust the dose, tap the log dose button to log the dose, or tap the i button to view details of what is included in the suggested dose. If the meter is set up for advanced mode, instead of selecting a meal, the user will be prompted to enter the grams or servings of carbohydrates to be eaten. The suggested dose in both easy mode and advanced mode also includes an insulin dose to correct blood glucose to target.
Figure 1.
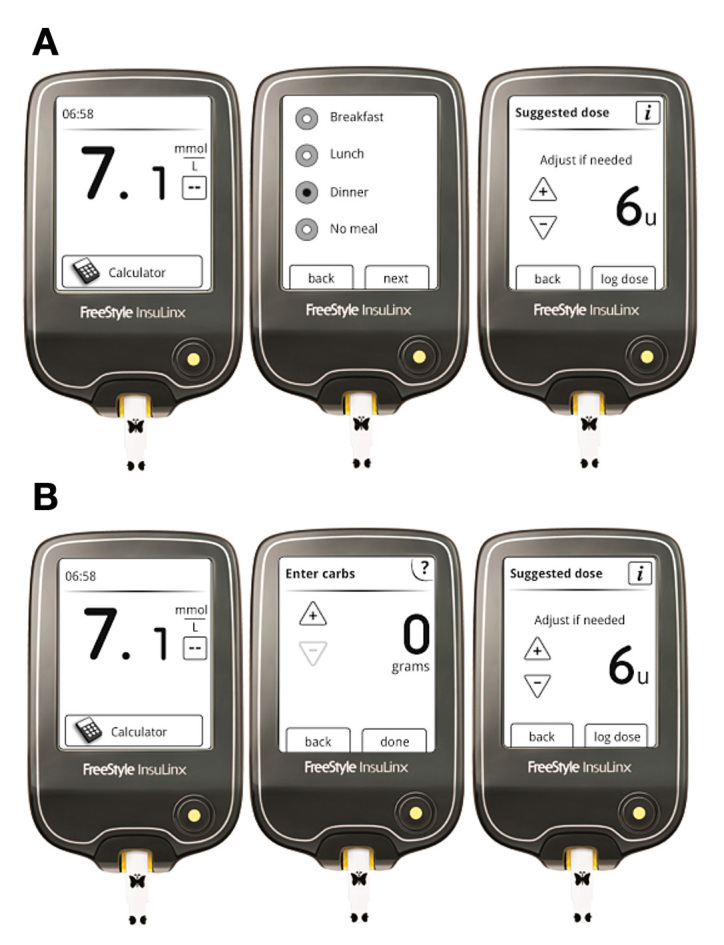
FreeStyle InsuLinx Blood Glucose Monitoring System. When the blood glucose result is displayed in (A) easy mode testing, the user taps “calculator” on the touch screen and selects meal to instantly obtain a suggested dose of mealtime insulin. When used in (B) advanced mode testing, the user will be prompted to enter carbohydrate rather than to select a meal.
Study Design
The objective of the study was to evaluate the number of errors and subject confidence and preference with manual calculation of insulin dose compared with using the FreeStyle InsuLinx meter. Up to 104 diabetes patients on MDIs of rapid/short-acting insulin were recruited at each of two study sites. Each study site aimed to recruit 52 subjects into each of two cohorts: cohort 1 for non-carbohydrate counters and cohort 2 for carbohydrate counters. Inclusion criteria were type 1 or 2 diabetes, currently using rapid/short-acting insulin at least two times per day to cover meals, aged 13 years or older, carbohydrate counting for cohort 2, able to read and write English without assistance, and participating in this study for the first time. Exclusion criteria were aged under 13 years, unable to write or use a touch screen device, or used bolus calculator on an insulin pump. An institutional review board approved the study, and allsubjects gave their informed consent prior to participation.
Subjects were provided two scenarios: normal glucose and high glucose. They were asked to manually calculate the insulin dose and then asked to determine the dose using the meter. Using the formula provided, the subjects manually calculated two mealtime insulin doses based on one high and one normal glucose value, respectively (Table 1). The non-carbohydrate-counting subjects in cohort 1 were provided the easy formula, a mealtime fixed dose value (meal bolus), a glucose value, and a correction factor to calculate the correction bolus based on the glucose value.
Table 1.
Insulin Dose Determination by the Subjects
| Cohort 1 (Non-carbohydrate counters) | Cohort 2 (Carbohydrate counters) | ||
|---|---|---|---|
| Scenario 1 | High glucose | Calculate an insulin dose using the easy formulaa | Calculate an insulin dose using the advanced formulaa |
| Scenario 2 | Determine an insulin dose using meter in easy mode | Determine an insulin dose using meter in advanced mode | |
| Scenario 3 | Normal glucose | Calculate an insulin dose using the easy formula | Calculate an insulin dose using the advanced formula |
| Scenario 4 | Determine an insulin dose using meter in easy mode | Determine an insulin dose using meter in advanced mode | |
See Methods section.
Easy Formula:
The carbohydrate-counting patients in cohort 2 were provided the advanced formula, an insulin-to-carbohydrate ratio to calculate the meal bolus based on the carbohydrate value given, and a correction factor to calculate the correction bolus based on the glucose value:
Advanced Formula:
When using the meter, the two scenarios (high and normal glucose values) were obtained by testing high and normal control solutions, respectively. The FreeStyle InsuLinx easy mode and advanced mode use the same easy formula and advanced formula, respectively, as provided to the subjects for manual calculations. Insulin-to-carbohydrate ratio or fixed meal dose, glucose correction factor, and correction target had been preset in the meter by the study staff to simulate how the meter is normally set up by the health care professional for the patient by entering these patient-specific parameters. No training was provided to the subjects on how to determine insulin dose with the manual formula or with the meter. The order of insulin determinations was not randomized. This was to avoid potential mistakes by the study staff in administering the eight different scenarios resulting from the two glucose levels, two formulas, and two calculation methods. The insulin-to-carbohydrate ratio and the correction factor were presented to the subjects clearly in the study instructions for determining insulin doses. For example, “The doctor tells you to take 1 unit of insulin for every 20 grams of carbohydrate you eat (that means your insulin-to-carbohydrate ratio is 20) and 1 unit of insulin for every 30 mg/dl of blood glucose above your target (that means your correction factor is 30).”
After the high glucose and normal glucose scenarios, respectively, the subjects completed a survey on their confidence and preference in manual calculation versus the use of the meter.
Results
A total of 207 diabetes patients were recruited at the two study sites. One subject was excluded in accordance with the exclusion criterion for using a bolus calculator; another subject withdrew from the study. Among the 205 subjects who completed the study, 104 were non-carbohydrate counters and were enrolled into cohort 1; 101 were carbohydrate counters and were enrolled into cohort 2. The subjects aged 13 to 83 (mean 51, median 54) years. Other demographic information of the study subjects is shown in Table 2.
Table 2.
Demographic Information of Subjects
| Demographic | Frequency | |
|---|---|---|
| Sex | Female | 36.4% |
| Male | 63.6% | |
| Diabetes type | Type 1 | 47.6% |
| Type 2 | 52.4% | |
| Highest education | College or higher | 61.2% |
| Years of having diabetes | 0 to 10 | 26.2% |
| 10 to 20 | 40.8% | |
| 20 to 30 | 21.4% | |
| 30 to 40 | 8.7% | |
| 40+ | 2.9% | |
| Years of taking insulin | 0 to 10 | 60.2% |
| 10 to 20 | 25.7% | |
| 20 to 30 | 8.3% | |
| 30 to 40 | 4.4% | |
| 40+ | 1.5% | |
A total of 409 insulin doses were determined, each by manual calculation and by using the meter. Of the insulin doses manually calculated, 256 (63%) were incorrect. There were 10 times fewer errors in insulin doses obtained using the meter versus manual calculation (p < .0001, calculated using McNemar’s test with Obuchowski’s adjustment for clusters2 to compare the overall frequency of errors made when using manual calculations versus the meter; Table 3). Results of the two cohorts were similar. The meter had 17 times fewer errors than manual calculations in cohort 1 and 8 times fewer errors in cohort 2. The errors in the insulin doses ranged from -7 to +16 U (mean absolute error = 0.2 U or 7%; median absolute error = 0 U or 0%; n = 409) when using the meter and from -12 to +135 U (mean absolute error = 3.8 U or 49%; median absolute error = 1 U or 9%; n = 409) when using manual calculations.
Table 3.
Insulin Dose Determinations by the Subjectsa
| All subjects | Meter | Total | ||
|---|---|---|---|---|
| Correct | Incorrect | |||
| Manual method | Correct | 145 (35%) | 8 (2%) | 153 (37%) |
| Incorrect | 241 (59%) | 15 (4%) | 256 (63%) | |
| Total | 386 (94%) | 23 (6%) | 409 | |
| Cohort 1 (easy) | Meter | Total | ||
|---|---|---|---|---|
| Correct | Incorrect | |||
| Manual method | Correct | 64 (31%) | 2 (1%) | 66 (32%) |
| Incorrect | 136 (65%) | 6 (3%) | 142 (68%) | |
| Total | 200 (96%) | 8 (4%) | 208 | |
| Cohort 2 (advanced) | Meter | Total | ||
|---|---|---|---|---|
| Correct | Incorrect | |||
| Manual method | Correct | 81 (40%) | 6 (3%) | 87 (43%) |
| Incorrect | 105 (52%) | 9 (4%) | 114 (57%) | |
| Total | 186 (93%) | 15 (7%) | 201 | |
Each subject determined two insulin doses by manual calculation and two insulin doses by using the FreeStyle InsuLinx meter. Cohort 1 (104 subjects) used the easy formula in manual calculation and the easy mode on the meter. Cohort 2 (101 subjects) used the advanced formula in manual calculation and the advanced mode on the meter.
An investigation into the cause of the 23 meter errors in the study revealed that about half of the errors were results of the users not performing the tests as instructed, rather than the meter calculating the wrong suggested dose. The remaining half were believed to be also related to the users not performing the tests as instructed, but the meter downloads were not available to confirm this. An example of confirmed deviation from study instructions is that several subjects logged an insulin dose in the meter despite being instructed not to do so in the study. Such insulin logging was evidenced in the meter memory. The logged dose altered the meter-suggested dose on the next glucose test performed within 3 to 8 h in accordance with the FreeStyle InsuLinx calculation algorithm that takes active insulin (insulin remaining in the body from a previous dose) into consideration.
The surveys showed that 83% of the subjects felt more confident using the meter than manual calculation in determining insulin doses (Table 4). Furthermore, 87% of the subjects preferred using the meter over manual calculation.
Table 4.
Subjects Survey Resultsa
| Statement | Cohort | Meter | Manual calculation | P value |
|---|---|---|---|---|
| Are you more confident that the calculated insulin dose is correct using the meter or manual calculation? | 1 | 186/206 (90%) | 20/206 (10%) | <.0001 |
| 2 | 153/202 (76%) | 49/202 (24%) | <.0001 | |
| Combined | 339/408 (83%) | 69/408 (17%) | <.0001 | |
| To determine an accurate insulin dose, would you prefer to use the meter or manual calculation? | 1 | 195/208 (94%) | 13/208 (6%) | <.0001 |
| 2 | 161/202 (80%) | 41/202 (20%) | <.0001 | |
| Combined | 356/410 (87%) | 54/410 (13%) | <.0001 | |
Each subject completed a survey containing these two questions after each of the two scenarios (normal glucose and high glucose). A binomial test for a proportion was used to statistically compare the survey responses on meter versus manual calculation.
Discussion
For insulin-using patients to achieve optimal glycemic control, adjustments of insulin dose at mealtimes must take into account multiple parameters, including current blood glucose level, target blood glucose, carbohydrate-to-insulin ratio, and carbohydrate intake. Difficulties in performing dose calculations often induce patients to administer fixed prandial insulin doses or to maintain an established amount of carbohydrates in their meals.1,3
Many insulin users find it challenging to manually calculate prandial insulin doses. Patients frequently make errors in calculating insulin dosages.4 Calculation of accurate insulin boluses is one of the major problems related to intensive insulin regimens. Results of this study showed that 63% of the manual calculations were incorrect among insulin-using patients. Carbohydrate-counting patients in cohort 2 used the advanced formula to adjust for both carbohydrate intake and blood glucose level; only 43% of their manually calculated doses were correct. This is consistent with a 2008 study5 that evaluated diabetes-related numeracy and found that only 41% of the 398 diabetes patients were able to calculate an insulin dose that required adjustment for both carbohydrate intake and blood glucose level. A 2004 study4 on adolescents with diabetes found that 50–64% of the subjects made errors in calculating premeal insulin dosages by conventional method. In a 2010 study,6 64% of 331 type 1 diabetes patients estimated their prandial insulin need inappropriately, as reflected by the frequency of postprandial hypoglycemia and hyperglycemia, suggesting that estimation of the optimal prandial insulin dose is not easy, even after a long duration of diabetes.
Due to complexity and difficulties, manual bolus calculation can discourage adherence. Consequently, patients may skip boluses or rely on empirical estimates.7 It is not surprising that one study found only 28% of the insulin-treated patients adjusted their doses.8
Bolus calculators are intended for optimizing glucose control by recommending appropriate insulin doses and decreasing the risk of hypoglycemia due to insulin stacking. A bolus calculator estimates the dose of insulin to be administered at mealtimes and makes calculation easier and more accurate. Various software systems are available for bolus calculation, but they typically require a device such as computer or insulin pump. The FreeStyle InsuLinx Blood Glucose Monitoring System, recently introduced in Europe, has a built-in, automated bolus calculator. When used in easy mode, the meter suggests a bolus dose based on the sum of the fixed meal dose and a dose to correct blood glucose level to the target. Once a blood glucose test is performed, the user only needs to tap the calculator button and the meal type button on the meter’s touch screen, and a suggested insulin dose will be displayed instantly by the meter. When used in advanced mode, the user enters the carbohydrate intake in grams or servings, instead of selecting the meal type, to obtain the suggested dose. Once the meter displays a suggested dose, the screen display gives the user three options: (1) tap the back button to correct the meal or carbohydrate intake in the previous screen display, (2) tap the up/down button to adjust the dose, or (3) tap the log dose button, which is prominently displayed below the suggested dose and will log the dose and advance to the log book display. Thus, when a suggested dose is requested, the meter ushers the user to log the dose. There are concise instructions for use (owner’s booklet) that explain why it is important to log all rapid-acting insulin doses. When using the advanced mode with the active insulin feature enabled, the user is automatically prompted to enter any unlogged rapid-acting insulin dose before the meter will determine a suggested dose.
A well-designed bolus calculator can accurately determine bolus doses for carbohydrate intake and for correcting elevated glucose levels. It can also track residual bolus insulin and reduce bolus recommendations to minimize insulin stacking. The use of such automated bolus calculators has several advantages: prandial insulin can be calculated more accurately, which may improve postprandial glucose control; patients may remain for an increased time within target glucose range; and the risk of insulin stacking is minimized, because the calculator remembers the time and amount that the patient has bolused.7
In a study9 of type 1 diabetes pediatric patients treated with continuous subcutaneous insulin infusion, the use of a bolus calculator was found to provide significant reductions in preprandial and 2 h postprandial blood glucose with fewer correction boluses and supplemental carbohydrates, and there was a trend toward less hypoglycemia. The use of the bolus calculator was also associated with a high level of satisfaction in these patients.
In a 6-month study3 of type 1 diabetes patients on MDI therapy, use of a bolus calculator improved glycemic control, as shown by a significant reduction of hemoglobin A1c levels compared with standard methods used for calculating the required insulin doses.
While it is outside the scope of the present study, the FreeStyle InsuLinx meter tracks active insulin (insulin on board) and subtracts it from the correction bolus in the suggested dose. The compact size, touch screen, and ease of navigation of the meter make the process of calculating insulin dosage very simple. Indeed, 87% of the subjects in the present study preferred to use the meter than manual calculation to determine prandial insulin doses. This may increase adherence and help optimize the use of mealtime insulin. The FreeStyle InsuLinx Blood Glucose Monitoring System expands the value of current blood glucose meters beyond just measuring blood glucose. It was designed to translate blood glucose and individual patient data into accurately calculated insulin dosing suggestions. It offers the benefits of automated bolus calculation, found with insulin pumps, to patients with type 2 diabetes.
Conclusions
In this study, insulin-using patients made errors in 63% of the manually calculated insulin doses. Use of the automated bolus calculator in the FreeStyle InsuLinx meter minimized errors in insulin dose determination. More than 80% of the patients felt more confident using the meter and preferred it to manual calculation.
Acknowledgments
We thank the following individuals for their invaluable assistance: Steve Schroder, Pamela Martin, and Jenis Bhavsar in the execution of this study; Lynne Lyons in designing case report forms and reviewing the study protocol; Pam McElroy, Julie Mora, Jewel Renfro, Ted Nguyen, and Lance Williams for data management; Walter Amor and Heather Pryor for assistance in statistical analysis; and Lausanne Farrell for study site monitoring.
Glossary
Abbreviations
- (MDI)
multiple daily injection
Funding
This work was sponsored by Abbott Diabetes Care, Alameda, CA.
Disclosures
Mona Patel, Jeanne Ward, Shridhara Alva, Andrew Lawrence, and Ronald Ng are full-time employees of Abbott Diabetes Care. FreeStyle and related brand marks are trademarks of Abbott Diabetes Care Inc. in various jurisdictions.
References
- 1.Gross TM, Kayne D, King A, Rother C, Juth S. A bolus calculator is an effective means of controlling postprandial glycemia in patients on insulin pump therapy. Diabetes Technol Ther. 2003;5(3):365–369. doi: 10.1089/152091503765691848. [DOI] [PubMed] [Google Scholar]
- 2.McCarthy WF. Adjustment to the McNemar’s test for the analysis of clustered matched-pair data. COBRA Preprint Series. Article 29. http://biostats.bepress.com/cobra/ps/art29. Accessed December 2011.
- 3.Maurizi AR, Lauria A, Maggi D, Palermo A, Fioriti E, Manfrini S, Pozzilli P. A novel insulin unit calculator for the management of type 1 diabetes. Diabetes Technol Ther. 2011;13(4):425–428. doi: 10.1089/dia.2010.0190. [DOI] [PubMed] [Google Scholar]
- 4.Glaser NS, Iden SB, Green-Burgeson D, Bennett C, Hood-Johnson K,Styne DM, Goodlin-Jones B. Benefits of an insulin dosage calculation device for adolescents with type 1 diabetes mellitus. J Pediatr Endocrinol Metab. 2004;17(12):1641–1651. doi: 10.1515/jpem.2004.17.12.1641. [DOI] [PubMed] [Google Scholar]
- 5.Cavanaugh K, Huizinga MM, Wallston KA, Gebretsadik T, Shintani A, Davis D, Gregory RP, Fuchs L, Malone R, Cherrington A, Pignone M, DeWalt DA, Elasy TA, Rothman RL. Association of numeracy and diabetes control. Ann Intern Med. 2008;148(10):737–746. doi: 10.7326/0003-4819-148-10-200805200-00006. [DOI] [PubMed] [Google Scholar]
- 6.Ahola AJ, Mäkimattila S, Saraheimo M, Mikkilä V, Forsblom C, Freese R, Groop PH, FinnDIANE Study Group Many patients with type 1 diabetes estimate their prandial insulin need inappropriately. J Diabetes. 2010;2(3):194–202. doi: 10.1111/j.1753-0407.2010.00086.x. [DOI] [PubMed] [Google Scholar]
- 7.Lalic NM, Landers B. 3rd Annual Symposium on Self Monitoring of Blood Glucose (SMBG) Applications and Beyond, May 7-8, 2010, London, UK. Diabetes Technol Ther. 2010;12(11):859–872. doi: 10.1089/dia.2010.0165. [DOI] [PubMed] [Google Scholar]
- 8.Szymborska-Kajanek A, Psurek A, Hese R, Strojek K. Self-monitoring of blood glucose in treatment of type 2 diabetes. Diabetes Res Clin Pract. 2009;(86 Suppl 1):S49–52. doi: 10.1016/S0168-8227(09)70009-9. [DOI] [PubMed] [Google Scholar]
- 9.Shashaj B, Busetto E, Sulli N. Benefits of a bolus calculator in pre- and postprandial glycaemic control and meal flexibility of paediatric patients using continuous subcutaneous insulin infusion (CSII) Diabet Med. 2008;25(9):1036–1042. doi: 10.1111/j.1464-5491.2008.02549.x. [DOI] [PubMed] [Google Scholar]


