Performance characteristics of devices that measure interstitial fluid glucose concentrations continue to improve. The overall accuracy of continuous glucose monitoring (CGM) systems depends on the sensor, the reference blood glucose concentrations used for calibration, and the calibration algorithm. We examined the accuracy of the iPro calibration algorithm when applied retrospectively to data collected with Sof-sensor CGM sensors.
A total of 768 sensors were worn by 71 adults (ages 19–72) and 61 children (ages 7–17) with type 1 diabetes. Sensor data from the first 3 days of wear, along with contemporaneous blood glucose (BG) concentrations measured by the Paradigm Link BG monitor, were supplied to the iPro algorithm to generate a data set of sensor glucose (SG) concentrations. The mean absolute relative difference (MARD) between SG and BG concentrations, the SG:BG agreement rate, and Clarke error grid analysis of paired SG and BG values were used to estimate the overall accuracy of the SG data.
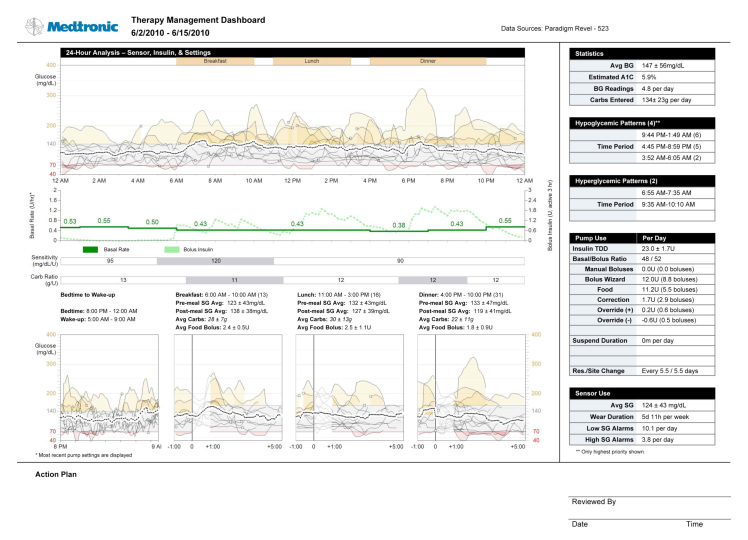
The MARD was 9.9% in adults and 10.1% in children, and were lowest in the 240–400 mg/dl range (6.8% in adults, 6.3% in children). The SG:BG agreement rate (i.e., the percentage of SG values within 20% of the reference BG value or the percentage within 20 mg/dl for reference values <80 mg/dl) was 89.1% for adults and 88.7% for children. The highest agreement rates were seen in the 240–400 mg/dl range (94.9% in adults, 95.2% in children). For values in the 40–80 mg/dl range, 88.7% of adult and 85.5% of pediatric SG values were within 20 mg/dl of the reference value, and for values in the 80–120 mg/dl range, 83.3% of adult and 81.2% of pediatric SG values were within 20% of the reference value. Clarke error grid analysis (Figure 1) showed that 99.0% (4849 of 4897) of adult and 98.4% (4116 of 4181) of pediatric-paired values were within zones A and B.
Figure 1.
Clarke error grid analysis of paired SG and BG values from adults and children.
The iPro algorithm is at the heart of the iPro Professional CGM system, which is used by clinicians to gain insights that are not apparent with finger stick and hemoglobin A1c testing alone. A CGM sensor and an attached iPro recording device are worn by the patient for 3 days, and four BG values are measured each day. Data from the BG meter and recording device are then uploaded for report generation and analysis. Therapy adjustments based on retrospectively-generated glycemic profiles have been shown to reduce the duration of hypoglycemia compared with therapy adjustments guided by BG values alone.1 Retrospective CGM was found to be well tolerated and beneficial in children2 and has been used to demonstrate frequent hypoglycemia in adults with poor control.3 It may be especially useful for those with hypoglycemia unawareness, for those with postprandial hyperglycemia, or during therapy regimen adjustments.4
The iPro algorithm provides SG readings that are in good agreement with respect to home BG meter readings when used in conjunction with Sof-sensor CGM sensors. The accuracy is maintained in both adults and children for at least 3 days.
Acknowledgments
iPro, Sof-sensor, and Paradigm Link are trademarks of Medtronic MiniMed, Inc., Northridge, CA.
Glossary
Abbreviations
- (BG)
blood glucose
- (CGM)
continuous glucose monitoring
- (MARD)
mean absolute relative difference
- (SG)
sensor glucose
Funding
This study was funded by Medtronic, Inc.
Disclosures
John B. Welsh, Francine R. Kaufman, and Scott W. Lee are employees of Medtronic, Inc.
References
- 1.Tanenberg R, Bode B, Lane W, Levetan C, Mestman J, Harmel AP, Tobian J, Gross T, Mastrototaro J. Use of the Continuous Glucose Monitoring System to guide therapy in patients with insulin-treated diabetes: a randomized controlled trial. Mayo Clin Proc. 2004;79(12):1521–1526. doi: 10.4065/79.12.1521. [DOI] [PubMed] [Google Scholar]
- 2.Kaufman FR, Gibson LC, Halvorson M, Carpenter S, Fisher LK, Pitukcheewanont P. A pilot study of the continuous glucose monitoring system: clinical decisions and glycemic control after its use in pediatric type 1 diabetic subjects. Diabetes Care. 2001;24(12):2030–2034. doi: 10.2337/diacare.24.12.2030. [DOI] [PubMed] [Google Scholar]
- 3.Munshi MN, Segal AR, Suhl E, Staum E, Desrochers L, Sternthal A, Giusti J, McCartney R, Lee Y, Bonsignore P, Weinger K. Frequent hypoglycemia among elderly patients with poor glycemic control. Arch Intern Med. 2011;171(4):362–364. doi: 10.1001/archinternmed.2010.539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Blevins TC, Bode BW, Garg SK, Grunberger G, Hirsch IB, Jovanovič L, Nardacci E, Orzeck EA, Roberts VL, Tamborlane WV; AACE Continuous Glucose Monitoring Task Force, Rothermel C. Statement by the American Association of Clinical Endocrinologists Consensus Panel on continuous glucose monitoring. Endocr Pract. 2010;16(5):730–745. doi: 10.4158/EP.16.5.730. [DOI] [PubMed] [Google Scholar]