Abstract
Background
This study explored the relatively neglected role of chronic stress in major depression, examining the independent contributions of co-occurring chronic and acute stress to depression, whether chronic stress predicts acute life events, and whether the two types of stress interact such that greater chronic stress confers greater sensitivity—or resistance—to the depressive effects of acute stressors.
Methods
From a sample of 816 community women, those who had a major depression onset in the past 9 months and those without major depressive episodes (MDE) onset and with no history of current or recent dysthymic disorder were compared on interview-based measures of antecedent acute and chronic stress. Chronic stress interviews rated objective stress in multiple everyday role domains, and acute stress was evaluated with contextual threat interviews.
Results
MDE onset was significantly associated with both chronic and acute stress; chronic stress was also associated with the occurrence of acute events, and there was a trend suggesting that increased acute stress is more strongly associated with depression in those with high versus low chronic stress.
Conclusions
Results suggest the importance of including assessment of chronic stress in fully understanding the extent and mechanisms of stress–depression relationships.
Keywords: depression, acute stress, chronic stress
INTRODUCTION
Much evidence validates the link between onset of a major depressive episode (MDE) and prior stressful life events, particularly major undesirable events.[1–3] However, the predominant research focus is on episodic (acute) life events, and commonly ignores the co-occurring effects of chronic, ongoing stressful conditions on depression. Examining episodic events that have relatively discreet beginnings and endings may tell only part of the story of the stress–depression association, as stressful life events occur within the ongoing conditions of a person’s life. For many, daily life experiences include continuing negative environmental circumstances (chronic stress) such as poor working conditions; financial difficulties; absent, intermittently or chronically unfulfilling or conflictual intimate relationships with romantic partners, parents, children, or friends; continuing health problems; and other ongoing burdens. Failure to assess and evaluate chronic stress in the stressor–depression relationship may mean that an important source of variability in the nature and strength of the association has been neglected.[4] It is also possible that depressive phenomena attributed to discrete stressful life events may reflect unmeasured associations with the ongoing chronic stress. Moreover, increasing research attention to the effects and mechanisms of stress includes topics such as the neurobiology of stress, gene–environment interactions, allostatic load, stress sensitization or “kindling,” and stress generation.[5–9] Research in these topics suggests somewhat different neurobiological and psychosocial processes, properties, and consequences of acute versus chronic stress.
Failure to distinguish between the effects of acute versus ongoing stressful conditions may impede efforts to fully understand the mechanisms by which depression results from stressors. Many stress–depression studies using questionnaires and checklists do not clearly distinguish between acute and chronic stress. Some of the early work using the well-validated Life Events and Difficulties Schedule[1,10] distinguished between severe “ongoing difficulties” and severe life events in their association with depression, but commonly operationalizes “provoking agents” as the occurrence of either a severe life event or an ongoing difficulty. There is a large volume of research on the depressive effects of chronic adversities such as marital conflict, parent–child discord, chronic illness or illness of a close family member, and social disadvantage (e.g., poverty, racial discrimination, neighborhood dysfunction, single motherhood).[11–14] Although such research certainly supports the idea of a link between these chronic stressors and distress, the focus is typically on life circumstances in a single domain. A limited focus does not provide a broad picture of chronic stress across multiple areas of a person’s life.
Also, research has not sufficiently evaluated the independent or joint effects of chronic and acute stress. An important exception was Brown and Harris’s[1] demonstration that likelihood of depression is increased with an acute event that “matches” an ongoing difficulty. A limited number of other studies have examined both types of stressors, and have suggested that the effects of acute stress–depression associations may be modified by chronic stress[15] or that the effects of the two types of stress may differ.[16–18]
Given the relative paucity of the research investigating both chronic and acute stress in the same investigation, several issues warrant further investigation. One goal of this study is to evaluate empirically the association between chronic stress and major depression, in addition to acute stress and depression. It is possible that research that focuses solely on acute stressors has underestimated or misattributed the link between stress and depression. Thus, an unresolved issue is whether and to what extent both chronic and acute stress have independent associations with depression such that our understanding of the stress–depression link is incomplete if both are not evaluated.
Furthermore, research on possible functional relationships between chronic and acute stress is needed. For instance, higher levels of chronic stress may portend higher levels of acute life events (such as a chronic health problem causing loss of a job or chronic marital difficulties giving rise to a bitter divorce). Turner and Turner[19] reported on predictors of stressors in a large community sample, and found results consistent with the idea that chronic difficulties and contextual factors contribute to the occurrence of acute stressors. The effects of chronic and acute stress may be independent of each other; both may have an impact, whereas neither moderates the other’s effects. An alternative is that chronic stress increases the depressive consequences of acute life events, a form of “sensitization” in which individuals who are challenged by high levels of chronic stress might be more likely to become depressed after an acute stressor.[20] A further model suggests that chronic stress decreases the effects of acute life events, a “steeling” or protective effect. McGonagle and Kessler[17] and Cairney et al.[21] found some support for the idea that higher chronic stress appeared to reduce the effects of acute stress on depression, arguing that “saturation” results from ongoing adversity such that acute negative events have less impact.
This study examines the impact of both chronic stress and acute stress to address the issues described. As noted, chronic stress in prior studies has been variously defined as a specific ongoing environmental condition (such as marital discord, caretaker burden) or as a stressor with enduring impact (defined by Brown and Harris[10] as 4 weeks, by Dougherty et al.[22] as 6 months, and by McGonagle and Kessler[17] as 12 months). Consistent with recommendations by Mazure,[3] we assess chronic stress as typical, ongoing conditions over at least a 6-month period across multiple domains of role functioning typical of adults. The goal is to capture the ongoing conditions of life in the salient aspects of individuals’ environments to provide a reasonably comprehensive profile of experiences. As Mazure notes, unless stressors are sampled from a broad array of domains, limited assessments will underestimate the true role of stress in the prediction of depression.
This study employs a large community sample of adult women, in which participants were initially selected to represent a wide array of histories (or no history) of depression. This study addresses the following questions:
Are chronic and acute stress independently associated with onset of major depression?
-
What are the functional relationships between levels of chronic and acute stress?
Are higher levels of chronic stress associated with the occurrence of more acute stressors? Further, is chronic stress a risk factor for stress generation, the occurrence of acute events that are at least partly caused by the person?
Does chronic stress moderate the effects of acute stress on the probability of depression. More specifically, is there a “sensitization” effect (the association between acute stress and depression becomes stronger with increases in chronic stress) or a “steeling” effect (the association between acute stress and depression decreases as women experience greater chronic stress)?
MATERIALS AND METHODS
PARTICIPANTS
Participants were 816 women selected from a larger research cohort (N=7,775) of women first studied in pregnancy with children born between 1981 and 1984 at the Mater Misericordiae Mother’s Hospital in Brisbane, Australia. The Mater-University Study of Pregnancy (MUSP) was originally designed to identify predictors of childhood health and development.[23] The present investigation was a separate substudy involving intensive followup of depressed and nondepressed women and their children at age 15. Participants were selected based on continued residency in the Brisbane area and on self-reports of depression on the Delusions-Symptoms-States Inventory (DSSI[24]) obtained at four time points from pregnancy to child’s age 5. Families were selected to include women with varying chronicity and severity of depressive symptoms including never symptomatic. Eight hundred and sixteen targeted families consented (82%), and did not differ from the original cohort with respect to family income, maternal education, and child’s gender. Further details of recruitment and selection are reported in Hammen and Brennan.[25]
Overall, the sample was 92% Caucasian, and median family income was in the lower middle class range. Women’s mean age was 41 years; 76.8% of women were married or cohabiting, and 64.8% were still married to the biological father of the child.
MEASURES
Interviews were conducted in the families’ homes after obtaining written informed consent. A team of two interviewers independently conducted diagnostic evaluations and assessments of life stress with the mother. Procedures were approved by institutional review committees at the University of Queensland, UCLA, and Emory University.
Diagnostic evaluation
Interviewers, who were blind to women’s previous DSSI scores, determined the presence of lifetime and current diagnoses using the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders—Fourth Edition.[26] Reliability ratings yielded weighted κ=.87 for diagnoses of current diagnoses of depression and weighted κ=.84 for past depressive disorders. Four hundred and fifty-nine women reported no lifetime history of depression; 357 reported a lifetime history of major depression or dysthymic disorder. Four women with possible bipolar disorder were excluded. Women with a history of recent or current dysthymic disorder (n=163) were also excluded to focus on the associations between recent acute and chronic stress and onset of MDE.
Chronic and acute life stress
Evaluations of life stress were conducted using a semi-structured interview designed to assess chronic and acute stressors (e.g., UCLA Life Stress Interview (LSI)[27]). Chronic stress was assessed by identifying typical conditions in at least the prior 6 months in each of eight domains: close friendships, intimate relationship, extended family relationships, relationships with children, work, finances, health (self), and health of family members. Unlike measures of functioning in major roles such as the SF36,[28] the Global Assessment of Functioning,[26] or the Social Adjustment Scale,[29] which conflate symptoms and functioning, the LSI attempts to obtain objective assessments of ongoing stressful circumstances that are independent of an individual’s symptomatology. Interviewers rated chronic stress for each domain on a five-point scale, with behaviorally specific anchors for each value; respondents’ subjective perceptions of stress are not scored. For example, for the domain of employment, a score of “2” represents good working conditions (workload, rewards, safety, stability, relations with boss and coworkers; or parallel if homemaker, retired), and “4” represents poor circumstances in three or four working conditions; if not working, two or more negative conditions among load, rewards, etc.; minimal steps taken or limited resources such as education, experience, or skills needed to resolve problems. Reliabilities based on independent raters yielded intraclass correlations of .82 for mother–child relationship, .88 for intimate relationship, .82 for close friend, and .77 for extended family relationships, .82 for work, .89 for finances, .81 for health/self, and .82 for health/family. Chronic stress scores were computed by summing ratings across all domains.
Two important characteristics of the chronic stress assessments are stability (they represent truly chronic, ongoing conditions) and convergent validity (they are not subjective and correspond to independent measures of similar constructs). Stability was demonstrated in a 5-year study of community young women in the transition to adulthood[16]; 1-year stability coefficients averaged over five 1-year periods ranged from .31 (work) to .68 (family relations), with a mean of .56 across domains. In an adult outpatient sample, similar stability over two 1-year periods was observed, with a mean correlation coefficient of .67 across domains. All values were highly statistically significant and indicate significant stability.
In the present sample convergent validity was supported by significant correlations between scores on the chronic stress domains and women’s reports on separate measures, and between women’s interviews and informant reports. For example, the financial chronic stress scale (interviewer rated based on funds available for necessities, savings, leisure and recreation, and extent of debt) correlated significantly with reported income, r=.51, P<.0001. Chronic stress in the intimate/marital relationship was significantly associated with modified Dyadic Adjustment Scale (DAS) marital satisfaction scores (r=−.70, P<.0001) and spouse report of DAS marital satisfaction (r=−.47, P<.0001). Chronic stress in the relationship with the 15-year-old child was significantly related to the child’s questionnaire reports of maternal warmth and hostility (rs=.43, −.39, respectively, Ps<.0001 in the expected direction.
Acute life events were assessed using methods similar to the contextual threat approach of Brown and Harris.[10] Covering the prior 12 months, interviewers obtained detailed information regarding the nature and date of each event, and the circumstances in which each event occurred. Interviewers presented narratives of each event to a rating team that was blind to diagnoses and to participants’ subjective reactions to the event. The team made objective ratings of how much impact the event would have on a typical person under similar circumstances, rating severity on a 1 (no impact) to 5 (extremely severe impact) scale. The team also rated the extent to which each event was dependent on the participant’s behavior or characteristics, using a 1 (entirely independent, “fateful”) to 5 (entirely dependent) scale. Independent judges’ ratings of women’s events yielded intraclass correlations of .85 for severity and .93 for dependence.
Given the 12-month time frame of the interview, all onsets of major depression within a 9-month period prior to the interview were noted, and scores of all events occurring in a 3-month period prior to the onset of the depressive episode were summed. For women who had no onset of major depression, events occurring during a randomly selected 3-month period during the prior year were summed.
RESULTS
Total acute stress in the 3-month period and total chronic stress scores were standardized, and entered as independent variables in a single logistic regression model to predict MDE onset. Where appropriate to the hypotheses, interaction terms (chronic × acute stress) were added to the model. Because depressed and nondepressed women did not differ significantly on socioeconomic factors, these variables were not included as covariates. The presence/absence of a prior history of depression was entered as a covariate in all analyses to control for its effects on MDE onset. Means and standard deviations of chronic and acute stress are presented in Table 1.
TABLE 1.
Stress scores for depressed and nondepressed women
| Group means ± standard deviations
|
|||
|---|---|---|---|
| Nondepressed women | MDD women | Cohen’s da | |
| Chronic stress scores (total across all domains) | 18.46 ± 2.41 | 20.46 ± 2.54 | .81 |
| Episodic stress scores (total severity of events) | 1.49 ± 1.94 | 3.27 ± 3.24 | .67 |
| Dependent event scores (total severity) | 0.64 ± 1.22 | 1.60 ± 1.99 | .58 |
MDD, major depressive disorder.
Effect size estimates reflect mean differences between participants with MDD and nondepressed participants.
INDEPENDENT EFFECTS OF CHRONIC AND ACUTE STRESS ON MDE
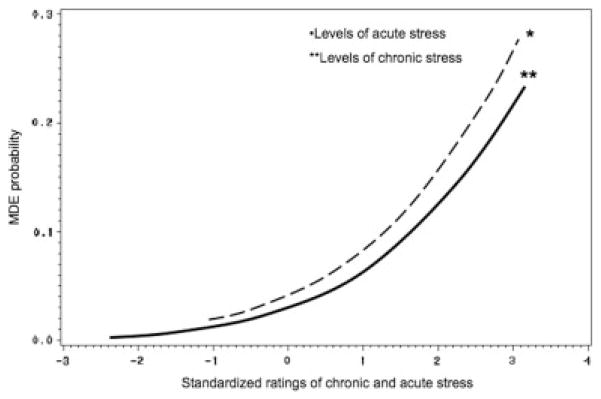
Logistic regression analyses of the association of stress variables with MDE onsets included a total of 24 depressed and 626 nondepressed women. Two women were excluded due to missing data. When examined simultaneously, higher levels of both chronic (Wald’s χ2(1, N=650)=3.63, OR=1.16, 95% CI: 1.00–1.36, P=.05) and acute stress (Wald’s χ2(1, N=650)= 29.28, OR=1.65, 95% CI: 1.35–1.90, P<.0001) were significantly associated with a higher probability of major depression. Figure 1 graphs the probabilities of MDE associated with varying levels of chronic and acute stress. The effects of acute stress on MDE onset were significantly greater than the effects of chronic stress (Wald’s χ2(1, N=650)=6.78, P=.01).
Figure 1.
Stress and probability of MDE. Probability of major depression is shown as a function of the level of prior acute and chronic stress. MDE, major depressive episode.
FUNCTIONAL RELATIONSHIPS BETWEEN CHRONIC AND ACUTE STRESS
Because chronic stress assessments covered the prior 6 months, only ratings of acute stress during the prior 6 months were used in multiple regression analyses. Events that occurred 6–12 months prior to assessment were not included to ensure that chronically negative conditions existed prior to the occurrence of acute stressors being examined. Multiple regression analyses indicated that higher levels of chronic stress were associated with higher levels of total acute stress during the same 6-month period, F(1, 650)=18.74, P<.0001. Chronic stress was also associated with “stress generation,”[26] occurrence of acute events that were judged to be dependent (those to which the person had contributed), F(1, 650)=9.04, P=.002, during the 6-month period, after controlling for the presence/absence of a history of depression.
Stress moderation effects were examined by entering interactions between chronic and acute stress in their association with depression onset in logistic regression analyses. The interaction term approached significance (Wald’s χ2(1, N=650)=3.57, OR=1.34, 95% CI: 0.99–1.82, P=.06), and indicated that, with increases in chronic stress, the effects of acute stress on the probability of major depression also increased. For women with lower levels of chronic stress, increases in acute stressors were less associated with the likelihood of a depressive episode.
DISCUSSION
This study explored the often-neglected issue of chronic stress, defined as ongoing conditions in multiple domains of daily roles, in depression. The study also examined whether chronic stress has an independent or interactive association with acute life events in their association with onset of major depression. The results confirmed the importance of chronic stress in three ways. First, chronic stress was independently associated with MDE onset, along with acute life events, although the latter had a stronger association with depression, similar to earlier findings reported by Brown and Harris.[1] Second, higher levels of chronic stress predicted higher levels of acute stress, including both total life events and stress generation—events that were dependent on the person. Third, there was a trend, consistent with a sensitizing effect, for chronic stress to moderate the effects of acute events on major depression such that high levels of chronic stress amplified the impact of acute events (see also References [19,20]); in contrast, the association between acute stress and depression was lower among women with lower levels of chronic stress.
The results confirm the importance of taking into account the effects of chronic stress in the stress–depression relationship. They suggest that the full extent of the role of stress on depression may not be detected if only acute life events are assessed. Further, chronic stress appears to contribute to stress occurrence, consistent with the “stress generation” patterns associated with major depression.[4,7] Although the results fell slightly short of statistical significance, the effects of chronic negative conditions appeared to amplify the association between acute life events and depression. Several implications are noteworthy. First, knowledge of both chronic and episodic stress conditions increases the predictability of major depression. Second, acute life events are more likely to occur in the context of greater ongoing chronic stress, and may suggest focus on such conditions in treatment to reduce likelihood of recurrent episodes. Third, if replicated in further studies, the interaction between chronic and episodic stress in predicting depression may have implications for mechanisms by which episodic stressors provoke depression, suggesting that elevated chronic stress may increase vulnerability to the precipitating effects of episodic events on depression. It is likely that psychological and neurobiological stress mechanisms differ for acute and chronic stressors, and their effects warrant separation and analysis.
Several limitations and directions for further clarification are noted. Although the study argues that the chronic and acute stress temporally preceded and contributed to the onset of MDEs, issues in the timing of associations among depression, acute stress, and chronic stress are noted. Depression and stress experiences were assessed retrospectively. However, the dates of MDE onset and acute event occurrence were obtained in separate interviews by different interviewers to maximize independence, and a wealth of data from numerous studies using similar methods has supported a triggering role for acute negative events.[1,3] It is possible that subclinical symptoms of depression occurring before MDE onset contributed to stress occurrence. Indeed, it is the nature of stress that its relationship to depression is bidirectional.[4] To address this issue, our analyses controlled for prior history of major depression, which itself may be a source of residual symptoms. A related issue is that although the study argues that chronic stress contributes to depressive episodes, a small number of depressive episodes (n=6) commenced before the chronic stress assessment period. However, chronic stress is relatively stable over a 1-year period, and the study obtained the same pattern of results when it only examined depressive episodes occurring during the 6-month period for which chronic stress was assessed. These factors increase confidence that the chronic stress was a contributor to, rather than a consequence of, major depression.
The current sample was limited to adult women, but stress–depression associations in male and youth populations also should be pursued. Other models of stress–depression links that include more distal stressors such as childhood adversity or that measure cumulative burden of childhood and adult stress exposure[19,30,31] should also be pursued. Further, this study employed a chronic stress measure that assesses major life roles across multiple content areas and attempted to evaluate them objectively and as separately as feasible from functioning due to symptoms, but other measures of chronic stressful conditions using different definitions and contents[32,33] may yield different results. This study did not investigate whether some chronic stress content domains are more likely associated with depression outcomes than others, but future research might fruitfully pursue such issues. It is also acknowledged that only a relatively small number of women experienced major depression in the 1-year window of the stress assessment, and larger samples would be desirable. These women differed in their histories of depression, and further studies should explore stress–depression associations at different points in the course of disorder.[34] However, an advantage of the current sample was that it is community based, and therefore widely generalizable to the most common experiences of major depression.
In conclusion, this study highlights the importance of chronic stress, defined as ongoing conditions in multiple domains of daily life, along with acute life events, in a fuller understanding of the stress–depression process, using a large community sample. It is hoped that the findings contribute to further studies of the mechanisms of stress in depression.
Acknowledgments
This study was supported by R01 MH52239 (NIMH) awarded to Constance Hammen and Patricia Brennan and by National Research Service Award postdoctoral fellowships (NIMH Grant 5-T32-MH14584) awarded to Eunice Kim and Nicole Eberhart. We thank Professor Jake Najman of the University of Queensland and MUSP colleagues William Bor, M.D., and Gail Williams, Ph.D. Special thanks to project coordinators Robyne LeBrocque and Cheri Dalton Comber. The authors have no financial interests to declare.
Footnotes
This article is a US Government work and, as such, is in the public domain in the United States of America.
References
- 1.Brown GW, Harris T. Depression. In: Brown GW, Harris TO, editors. Life Events and Illness. New York: Guilford Press; 1989. pp. 49–93. [Google Scholar]
- 2.Kessler RC. The effects of stressful life events on depression. Annu Rev Psychol. 1997;48:191–214. doi: 10.1146/annurev.psych.48.1.191. [DOI] [PubMed] [Google Scholar]
- 3.Mazure CM. Life stressors as risk factors in depression. Clin Psychol: Sci Pract. 1998;5:291–313. [Google Scholar]
- 4.Hammen C. Stress and depression. Annu Rev Clin Psychol. 2005;1:293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938. [DOI] [PubMed] [Google Scholar]
- 5.Caspi A, Sugden K, Moffitt TE, et al. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science. 2003;301:386–389. doi: 10.1126/science.1083968. [DOI] [PubMed] [Google Scholar]
- 6.de Kloet ER, Joels M, Holsboer F. Stress and the brain: from adaptation to disease. Nat Rev Neurosci. 2005;6:463–475. doi: 10.1038/nrn1683. [DOI] [PubMed] [Google Scholar]
- 7.Hammen C. Generation of stress in the course of unipolar depression. J Abnorm Psychol. 1991;100:555–561. doi: 10.1037//0021-843x.100.4.555. [DOI] [PubMed] [Google Scholar]
- 8.McEwen BS. Allostasis and allostatic load: implications for neuropsychopharmacology. Neuropsychopharmacology. 2000;22:108–124. doi: 10.1016/S0893-133X(99)00129-3. [DOI] [PubMed] [Google Scholar]
- 9.Post RM. Transduction of psychosocial stress into the neurobiology of recurrent affective disorder. Am J Psychiatry. 1992;149:999–1010. doi: 10.1176/ajp.149.8.999. [DOI] [PubMed] [Google Scholar]
- 10.Brown GW, Harris T. Social Origins of Depression. London: Free Press; 1978. [DOI] [PubMed] [Google Scholar]
- 11.Afifi TO, Cox BJ, Enns MW. Mental health profiles among married, never-married, and separated/divorced mothers in a nationally representative sample. Soc Psychiatry Psychiatr Epidemiol. 2006;41:122–129. doi: 10.1007/s00127-005-0005-3. [DOI] [PubMed] [Google Scholar]
- 12.Evans DL, Charney DS, Lewis L, et al. Mood disorders in the medically ill: scientific review and recommendations. Biol Psychiatry. 2005;58:175–189. doi: 10.1016/j.biopsych.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 13.Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder: results from the national epidemiologic survey on alcoholism and related conditions. Arch Gen Psychiatry. 2005;62:1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- 14.Latkin CA, Curry AD. Stressful neighborhoods and depression: a prospective study of the impact of neighborhood disorder. J Health Soc Behav. 2003;44:34–44. [PubMed] [Google Scholar]
- 15.Pearlin LI, Lieberman MA, Menaghan EG, Mullan JT. The stress process. J Health Soc Behav. 1981;22:337–356. [PubMed] [Google Scholar]
- 16.Daley SE, Hammen C, Rao U. Predictors of first onset and recurrence of major depression in young women during the 5 years following high school graduation. J Abnorm Psychol. 2000;109:525–533. [PubMed] [Google Scholar]
- 17.McGonagle KA, Kessler RC. Chronic stress, acute stress, and depressive symptoms. Am J Community Psychol. 1990;18:681–706. doi: 10.1007/BF00931237. [DOI] [PubMed] [Google Scholar]
- 18.Rojo-Moreno L, Livianos-Aldana L, Cervera-Martinez G, et al. The role of stress in the onset of depressive disorders: a controlled study in a Spanish clinical sample. Soc Psychiatry Psychiatr Epidemiol. 2002;37:592–598. doi: 10.1007/s00127-002-0595-y. [DOI] [PubMed] [Google Scholar]
- 19.Turner HA, Turner RJ. Understanding variations in exposure to social stress. Health: an interdisciplinary. J Soc Stud Health Illn Med. 2005;9:209–240. doi: 10.1177/1363459305050586. [DOI] [PubMed] [Google Scholar]
- 20.Ormel J, Oldehinkel AJ, Brilman EI. The interplay and etiological continuity of neuroticism, difficulties, and life events in the etiology of major and subsyndromal, first and recurrent depressive episodes in later life. Am J Psychiatry. 2001;158:885–891. doi: 10.1176/appi.ajp.158.6.885. [DOI] [PubMed] [Google Scholar]
- 21.Cairney J, Boyle M, Offord DR, Racine Y. Stress, social support and depression in single and married mothers. Soc Psychiatry Psychiatr Epidemiol. 2003;38:442–449. doi: 10.1007/s00127-003-0661-0. [DOI] [PubMed] [Google Scholar]
- 22.Dougherty LR, Klein DN, Davila J. A growth curve analysis of the course of dysthymic disorder: the effects of chronic stress and moderation by adverse parent–child relationships and family history. J Consult Clin Psychol. 2004;72:1012–1021. doi: 10.1037/0022-006X.72.6.1012. [DOI] [PubMed] [Google Scholar]
- 23.Keeping JD, Najman JM, Morrison J, et al. A prospective longitudinal study of social, psychological, and obstetrical factors in pregnancy: response rates and demographic characteristics of the 8,556 respondents. Br J Obstet Gynaecol. 1989;96:289–297. doi: 10.1111/j.1471-0528.1989.tb02388.x. [DOI] [PubMed] [Google Scholar]
- 24.Bedford A, Foulds GA. Delusions-Symptoms-States Inventory of Anxiety and Depression. Windsor, UK: NFER; 1978. [Google Scholar]
- 25.Hammen C, Brennan PA. Interpersonal dysfunction in depressed women: impairments independent of depressive symptoms. J Affect Disord. 2002;72:145–156. doi: 10.1016/s0165-0327(01)00455-4. [DOI] [PubMed] [Google Scholar]
- 26.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders. Washington, DC: American Psychiatric Press; 1995. [Google Scholar]
- 27.Hammen C, Adrian C, Gordon D, et al. Children of depressed mothers: maternal strain and symptom predictors of dysfunction. J Abnorm Psychol. 1987;96:190–198. doi: 10.1037//0021-843x.96.3.190. [DOI] [PubMed] [Google Scholar]
- 28.Stewart AL, Hays RD, Ware JE. The MOS short-form general health survey. Reliability and validity in a patient population. Med Care. 1988;26:724–735. doi: 10.1097/00005650-198807000-00007. [DOI] [PubMed] [Google Scholar]
- 29.Weissman MM, Bothwell S. Assessment of social adjustment by patient self-report. Arch Gen Psychiatry. 1976;33:1111–1115. doi: 10.1001/archpsyc.1976.01770090101010. [DOI] [PubMed] [Google Scholar]
- 30.Turner RJ, Wheaton B, Lloyd DA. The epidemiology of social stress. Am Sociol Rev. 1995;60:104–125. [Google Scholar]
- 31.Ensel WM, Lin N. Distal stressors and the life stress process. J Community Psychol. 1996;24:66–82. [Google Scholar]
- 32.Wheaton B. Stress and mental health: contemporary issues and prospects for the future. In: Avison WR, Gotlib IH, editors. The Plenum Series on Stress and Coping. New York, NY: Plenum Press; 1994. pp. 77–114. [Google Scholar]
- 33.Steptoe A, Marmot M. Burden of psychosocial adversity and vulnerability in middle age: associations with biobehavioral risk factors and quality of life. Psychosom Med. 2003;65:1029–1037. doi: 10.1097/01.psy.0000097347.57237.2d. [DOI] [PubMed] [Google Scholar]
- 34.Monroe SM, Harkness KL. Life stress, the “kindling” hypothesis, and the recurrence of depression: considerations from a life stress perspective. Psychol Rev. 2005;112:417–445. doi: 10.1037/0033-295X.112.2.417. [DOI] [PubMed] [Google Scholar]