Abstract
Post-lobectomy bronchopleural fistula is a rare complication of lung resection surgery, and proper management is essential for its successful resolution. Most published papers deal with endoscopic and surgical treatment. We report our experience with conservative management. Data were collected by reviewing the clinical charts of patients diagnosed with post-lobectomy bronchopleural fistula at the University Hospitals Marqués de Valdecilla, Santander, and Puerta de Hierro, Majadahonda-Madrid, Spain, from June 2003 to December 2010. Bronchopleural fistula was diagnosed by means of endoscopic visualization. Treatment included the insertion of a thoracostomy drainage tube in the pleural cavity. In patients under mechanical ventilation, independent pulmonary ventilation was also applied. Seven cases of post-lobectomy bronchopleural fistula were collected. Three of them occurred within the first week, another three within the first month and the remaining case after 10 months. The fistula size ranged between 6 mm and complete suture dehiscence. Two patients died due to causes unrelated to the treatment. The period of time elapsed for the resolution of this complication varied between 5 and 36 days. We conclude that conservative treatment of post-lobectomy bronchopleural fistula is a safe and simple option that must be taken into account in the management of this problem.
Keywords: Bronchopleural fistula, Lobectomy, Conservative treatment
INTRODUCTION
One of the most feared complications in lung resection surgery is bronchopleural fistula due to the high associated mortality. Its incidence has considerably decreased during the last few decades, reaching figures of 4–20% in pneumonectomy and <1% in lobectomies [1–3]. Associated risk factors such as residual tumour on the bronchial stump, long bronchial stump, diabetes, steroids, neoadyuvant chemo or/and radiotherapy, infection, etc. are well known [2, 3], so prevention is in part possible. Once diagnosis is made, proper management is paramount to reduce the associated mortality, reported to be between 25 and 71% [1, 2], with aspiration pneumonia being the main cause of death [2].
Most papers in this area are related to post-pneumonectomy fistula. We describe our experience with the conservative treatment of post-lobectomy bronchopleural fistula.
METHODS
This was a retrospective and descriptive study. Data were collected by reviewing the clinical charts of patients diagnosed with post-lobectomy bronchopleural fistula at the University Hospitals Marqués de Valdecilla, Santander, and Puerta de Hierro, Majadahonda-Madrid, Spain, from June 2003 to December 2010. Bronchopleural fistulas were diagnosed by endoscopic visualization (Fig. 1a). The treatment applied was the insertion of a thoracostomy drainage tube in the pleural cavity, with either no aspiration or with the minimum aspiration necessary to get the lung expanded. Furthermore, in patients under mechanical ventilation, independent pulmonary ventilation was applied, optimally ventilating the healthy lung, with low pressure, short inspiratory period, low tidal volume, low respiratory rate and low pressure peak in the lung with the fistula. Whenever possible, thoracostomy tube was connected to a Heimlich valve and, in this case, outpatient follow-up was possible.
Figure 1:
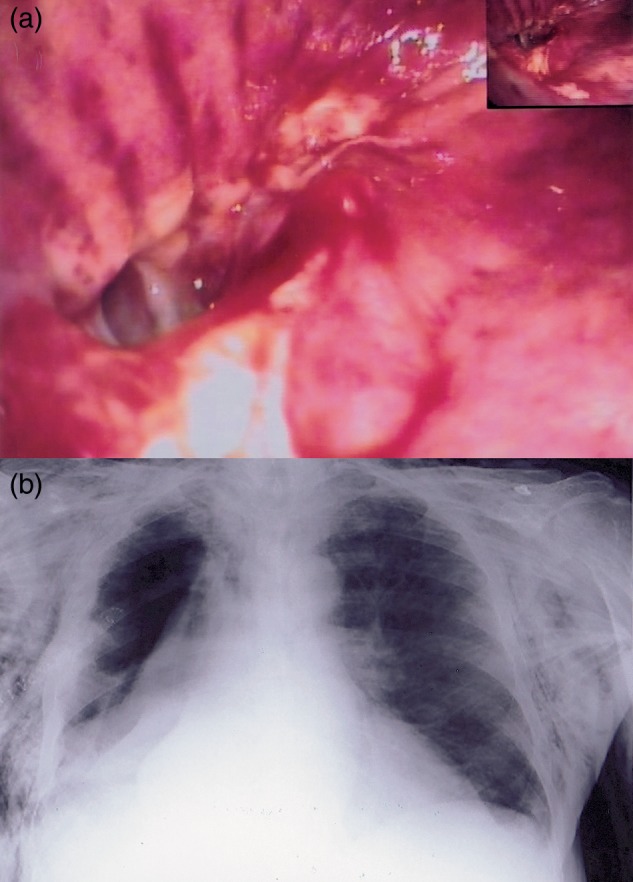
(a) Endoscopic view of a fistula. Dehiscence affects half of the suture. (b) Subcutaneous emphysema and pneumothorax in Patient 2.
RESULTS
A total of 1627 lung resections were performed: 252 pneumonectomies and 1373 lobectomies. We found 18 post-pneumonectomy (7.14%) and 7 post-lobectomy (0.46%) fistulas. Regarding this latter group, we collected five cases at the Marques de Valdecilla and two at the Puerta de Hierro University Hospitals (details shown in Table 1). The case which occurred after 10 months was a patient who underwent thoracic wall resection, suffered a respiratory complication and needed aggressive mechanical ventilation.
Table 1:
Patients, general characteristics
| Patient | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| Gender | Male | Male | Male | Male | Male | Male | Male |
| Age | 68 | 70 | 63 | 55 | 72 | 69 | 68 |
| Pathology and TNM | SqCC, T3N0 | SqCC, T1N0 | ADC, T2N1 | ADC, T1N0 | LCC, T2N0 | ADC, T1N0 | SqCC, T2N0 |
| Risk factors | MV | Pneumonia, steroids | Alcoholic, malnutrition | Diabetes | Alcoholic, malnutrition | None | None |
| Suture | Mch | Mch | Mch | Mch | Mch | Mn | Mch |
| Resection | RUL VATS | RUL | RUL | RLL | RUL | RLL | RLL VATS |
| Symptoms | air leak | ScE pneumothorax Fig. 1b | Empyema | Air leak | Pneumonia empyema | Pneumonia empyema | Air leak |
| Size | 6 mm | Half stump | Complete | 6 mm | 10 mm | Complete | Half stump |
| Time from surgery | 10 m | 7 d | 20 d | 4 d | 25 d | 1 m | 3 d |
| MV | Yes | No | No | No | Yes | Yes | No |
| Treatment | Cons. | Cons. | Cons. | Cons. | Cons. | Stent, cons. | Cons. |
| Time to close | 17 d dead | 5d | 36 d | 23 d | dead | 28 d | 16 d |
| Follow-up (m) | 12 | 15 | 40 | 80 | 1 | 51 | 32 |
SqCC: squamous cell carcinoma; ADC: adenocarcinoma; LCC: large cell carcinoma; MV: mechanical ventilation; Mch: mechanical; Mn: manual; RUL: right upper lobectomy; RLL: right lower lobetomy; VATS: video-assisted thoracic surgery; ScE: subcutaneous emphysema; Cons.: conservative.
All the patients underwent conservative treatment, except for one who initially underwent bronchoscopic stent placement to facilitate mechanical ventilation, with no success. In this patient, due to his dismal general condition, surgical re-intervention was inadvisable, so conservative treatment was applied successfully.
One of the patients died as a result of the severe aspiration pneumonia that was already present when he attended the emergency department where the fistula diagnosis was made; another died as a result of causes other than the fistula, which was completely resolved several weeks previously; and the remaining patients were discharged without consequences.
The period of time elapsed for the resolution of this complication was considered from diagnosis to thoracostomy tube removal.
DISCUSSION
Post-resection bronchopleural fistula remains an important complication due to its associated mortality. It is more prevalent after pneumonectomy, particularly on the right side [2]. Post-lobectomy fistula is extremely unusual [1, 3] and we see it more often after a lower lobectomy or lower and middle bi-lobectomy [1]. It usually appears in patients with some risk factors for fistula [3].
Treatment must be applied early and properly to reduce mortality. In general, the treatment options reported include: bronchoscopy with fistula occlusion using different kinds of stents or the application of different biological glues [4–7]. Also, the addition of a combined pneumoperitoneum and autologous blood patch can reduce air leak duration [8]. Surgical techniques with muscle or epiplon transposition to close the fistula and obliterate the emphyema cavity, once sterilized [9], or completion of pneumonectomy in the case of previous lobectomy [2]. Conservative management, allowing for an easier spontaneous closure of the fistula in lobectomies and segmentectomies [3]. Randomized studies comparing these options are lacking and nearly all reports showed only isolated cases, which prevented the reaching of definitive conclusions.
An important issue regarding the conservative option is the type of resection performed: if it is pneumonectomy, only 30% of fistulas close after drainage with a thoracic window, while after lobectomy all close after the drainage of the pleural space [10]. It is very important to avoid aspiration pneumonia by draining the empyema, if present. The surgical option has the advantage of potentially closing the fistula immediately, but has the disadvantage of being an invasive alternative. Bronchoscopic procedures and surgical options share the advantage of potential immediate fistula closure, although with a greater percentage of failures [2], but it is a much less invasive technique. The success of biological glues depends enormously on the fistula size. Stents have the disadvantage of frequent migration, and have a deleterious effect on the airway mucous membrane. The conservative option has the advantage of being a completely non-invasive treatment, which is safe if we drain the empyema as soon as it is diagnosed. Two of our patients died, but not in relation to the treatment applied. It has the disadvantage of needing a long period of time for the closure of the fistula and of the difficult management in cases requiring mechanical ventilation. The long time required for the closure does not imply an increase in expenditure, because if the patient does not suffer any complications apart from the fistula, the drainage tube can be connected to a Heimlich valve and the patient can be discharged. In our patients, we initially chose this option in all cases except in one, because it is simple, safe and non-invasive. Once the pleural cavity is drained, all we have to do is wait patiently for nature to do its work. In patients who need mechanical ventilation this can be simplified if we seal the fistula as soon as possible, and the least invasive option is endoscopic stent placement. A limitation of this study is that it is a descriptive, retrospective series, preventing comparison with other treatment strategies.
In conclusion, there have been several techniques reported for the closure of a post-lung resection bronchopleural fistula, although most of the papers dealt with post-pneumonectomy fistula. In post-lobectomy fistula, the option of conservative treatment must be taken into account, as well as endoscopic and surgical treatments.
Conflict of interest: none declared.
REFERENCES
- 1.Nagahiro I, Aoe M, Sano Y, Date H, Andou A, Shimizu N. Bronchopleural fistula after lobectomy for lung cancer. Asian Cardiovasc Thorac Ann. 2007;15:45–8. doi: 10.1177/021849230701500110. [DOI] [PubMed] [Google Scholar]
- 2.Sirbu H, Busch T, Aleksic I, Schreiner W, Oster O, Dalichau H. Bronchopleural fistula in the surgery of non-small cell lung cancer: incidence, risk factors, and management. Ann Thorac Cardiovasc Surg. 2001;7:330–6. [PubMed] [Google Scholar]
- 3.Cooper WA, Miller JI., Jr Management of bronchopleural fistula after lobectomy. Semin Thorac Cardiovasc Surg. 2001;13:8–12. doi: 10.1053/stcs.2001.22494. [DOI] [PubMed] [Google Scholar]
- 4.Bellato V, Ferraroli GM, De Caria D, Infante MV, Cariboni U, Spoto MR, et al. Management of postoperative bronchopleural fistula with a tracheobronchial stent in a patient requiring mechanical ventilation. Intensive Care Med. 2010;36:721–2. doi: 10.1007/s00134-010-1757-0. [DOI] [PubMed] [Google Scholar]
- 5.Takanami I. Closure of a bronchopleural fistula using a fibrin-glue coated collagen patch. Interact CardioVasc Thorac Surg. 2003;2:387–8. doi: 10.1016/S1569-9293(03)00109-9. [DOI] [PubMed] [Google Scholar]
- 6.Mora G, de Pablo A, García-Gallo CL, Laporta R, Ussetti P, Gámez P, et al. Is endoscopic treatment of bronchopleural fistula useful? Arch Bronconeumol. 2006;42:394–8. doi: 10.1016/s1579-2129(06)60553-3. [DOI] [PubMed] [Google Scholar]
- 7.Fernández-Díaz JA, García-Gallo C, Goicolea-Ruigómez J, Varela-de Ugarte A. Use of Amplatzer(®) device for closure of bronchopleural fistulas, a hybrid procedure using bronchoscopy and radiology. Rev Esp Cardiol. 2011;64:1065–6. doi: 10.1016/j.recesp.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 8.Korasidis S, Adreetti C, D'Andrilli A, Ibrahim M, Ciccone A, Poggi C, et al. Management of residual pleural space and air leaks after major pulmonary resection. Interact CardioVasc Thorac Surg. 2010;10:925–6. doi: 10.1510/icvts.2009.231241. [DOI] [PubMed] [Google Scholar]
- 9.Ridgway E, DeCamp M, Morris D. Bronchopleural fistula repair using combined breast parenchymal and pectoralis major musculocutaneous flap. Ann Thorac Surg. 2008;86:1022–5. doi: 10.1016/j.athoracsur.2008.02.052. [DOI] [PubMed] [Google Scholar]
- 10.Shamji FM, Ginsberg RJ, Cooper JD. Open window thoracostomy in the management of postpneumonectomy empyema with or without bronchopleural fistula. J Thorac Cardiovasc Surg. 1983;86:818. [PubMed] [Google Scholar]


