Abstract
Reoperation due to recurrence after tracheal resection and reconstruction still seems challenging. Although recurrence may lead to serious morbidity, an appropriate surgical technique plays a significant role in the cure of these patients. We report our experience of a patient who successfully underwent a third resection and anastomosis of the trachea. We believe that the number of previous operations is not a contraindication by itself against reoperating on a patient with restenosis. Also the success rate might be acceptably high if a sufficiently healthy tracheal length remains.
Keywords: Tracheal stenosis, Tracheal surgery, Restenosis, Reoperation
INTRODUCTION
Despite recognizing some risk factors and preventive methods, post-intubation tracheal stenosis (PITS) is still seen. The resection and anastomosis (RA) of the trachea is known as an effective treatment for PITS, and with the appropriate surgical technique the success rate is high [1].
Although recurrence is uncommon following RA, it may lead to severe morbidity [2]. In this situation, the second surgery is more difficult than the first.
In this case report, a patient with two previous failed tracheal resections underwent the third one successfully.
An emergent tracheostomy had been performed due to severe dyspnoea in a 28-year old female diagnosed with PITS. After 1 month, she underwent RA through a low cervical transverse incision, and the length of resection was reported to be 20 mm. In the next 2 weeks, she was referred to our centre. Using bronchoscopy, a lot of granulation tissue and unabsorbed sutures were detected at the anastomotic site, as well as 70% luminal stenosis. The length of the stenosis was 30 mm from 20 mm below vocal cords. The length of the normal trachea below the stenosis was 70 mm, which consisted of 16 rings. At first, frequent bronchoscopies and dilatations were carried out to relieve dyspnoea. Despite our recommendation, she did not accept a tracheostomy or T-tube; therefore, a second RA was performed and a fibrotic stenosis measuring 40 mm was resected only 2 months after the first operation. To mobilize the trachea, the anterior pretracheal space was released down to the carina. Also, the larynx was released up to above the hyoid bone by releasing insertions of strap muscles. However, 3 weeks later, she became dyspnoeaic, and, in bronchoscopy, granulation, tissue and malacia were detected. The function of the vocal cords as well as 85 mm of the airway were still normal (25 mm above the stenosis and 60 mm below that), and there were 12 normal rings below the stenosis. This showed that there was another chance of successful RA. A spiral CT scan of the trachea showed a ∼30 mm circumferential tracheal stenosis (Fig. 1). This time, a tracheostomy tube was inserted which was maintained for 6 months. After that, the third RA was performed and 40 mm of the trachea was resected. Because of high tension at the anastomotic site, the larynx was released with a Montgomery manoeuvre which led to additional downward movement of the superior part of the anastomosis and less tension subsequently. The anastomosis was not covered by any flaps. Neck flexion was achieved by a suture between the chin and presternal skin. One month later, the anastomosis looked good in bronchoscopy and the patient was asymptomatic; also the function of the vocal cords was normal. At present, 18 months after the last resection, the patient has no symptoms.
Figure 1:
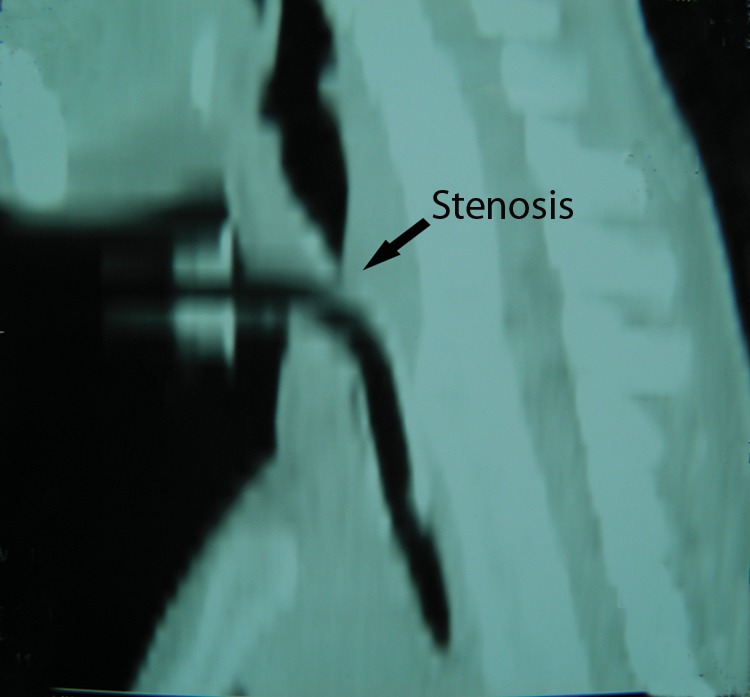
Spiral CT scan demonstrating tracheal stenosis.
COMMENT
Although recurrence after RA is uncommon, due to the high morbidity of it, the surgeon always has a serious challenge. The surgeon's judicious judgement is of great importance in understanding the cause of a recurrence. Appropriate techniques result in a high success rate, which include complete resection of the stenosis, minimal tension on the anastomosis and preservation of laryngeal nerves [1,3].
Excessive granulation tissue formation at the site of the anastomosis used to be the main cause of the stenosis, while nowadays it is not considered a major concern due to the use of absorbable sutures [1,4].
Tension or infection at the anastomosis, ischaemia and insufficient resection of the stenosis are some of the factors which lead to recurrence [4,5]. The length of resection is also closely related to the amount of tension and if resection is >40 mm, tension will be excessive [2,5]. Longer resections necessitate more laryngeal release, including the Montgomery technique of the supra hyoid muscle division. It is hard to say whether the measured resected part of the trachea (in repeated RA) is completely related to the destroyed trachea, or fibrosis at the site of dehiscence might be a portion of it. Actually, we do not know how many rings and how much of the real trachea have been resected. We just measured the distance between upper and lower ends of stenotic segment. This length is probably less than a real portion of the trachea which has been destructed by process of scar and stenosis.
Therefore, it seems that the number of intact remaining tracheal rings at the preoperative bronchoscopy is a more reliable criterion for the estimation of the treatment plan and the possibility of another RA.
The presence of too much scar tissue around the trachea limits the mobilization of it, which results in more tension at the anastomosis.
Additionally, most surgeons attempt to avoid preoperation tracheostomy and try to maintain the patient's airway by other means such as bronchoscopy and dilatation. Similarly, we do not use laser therapy before surgery, since we believe that it is to some extent as harmful as tracheostomy.
Last but not the least is the necessity of postponing the second RA surgery for some months after the first one.
Grillo and his colleagues [4] have emphasized a 4- to 6-month delay to ensure the relief of any inflammation and for better defining and healing of the diseased trachea. In the present case, it seems that the short elapsed time after the first surgery was the probable cause of the unsuccessful second surgery.
If preservation of airways is not possible by dilatation, it might be better to insert a tracheostomy tube or T-tube through the stenosis rather than doing a premature resection.
Although the length of the resected part in previous surgeries, as well as the number of surgeries, is very indicative of the difficulty of future operations, they are not the only determining factors for depriving the patient of another RA. We believe that the length of the remaining normal trachea, rather than the resected parts is the most important factor by which we can predict the feasibility of reoperation.
CONCLUSION
Repeated tracheal RA, even though difficult and challenging, is the best way to avoid tracheostomy or stents in patients with recurrent stenosis after previous RA. In the future, an alternative method could be tracheal transplant.
Conflict of interest: none declared.
REFERENCES
- 1.Grillo HC, Donahue DM, Mathisen DJ, Wain JC, Wright CD. Postintubation tracheal stenosis: treatment and results. Thorac Cardiovasc Surg. 1995;109:486–93. doi: 10.1016/S0022-5223(95)70279-2. [DOI] [PubMed] [Google Scholar]
- 2.Wright CD, Grillo HC, Wain JC, Wrong DR, Donahue DM, Gaissert HA, et al. Anastomotic complications after tracheal resection: prognostic factors and management. J Thorac Cardiovasc Surg. 2004;128:731–9. doi: 10.1016/j.jtcvs.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 3.Pearson FG, Cooper JD, Nelems JM, Van Nostrand AW. Primary tracheal anastomosis after resection of cricoid cartilage with preservation of recurrent laryngeal nerves. J Thorac Cardiovascular Surg. 1975;70:806–16. [PubMed] [Google Scholar]
- 4.Donahue DM, Grillo HC, Wain JC, Wright CD, Mathisen DJ. Reoperative tracheal resection and reconstruction for unsuccessful repair of post intubation stenosis. J Thorac Cardiovasc Surg. 1997;114:934–9. doi: 10.1016/S0022-5223(97)70007-2. [DOI] [PubMed] [Google Scholar]
- 5.Abbasidezfuli A, Akbarian E., Shadmehr MB, Arab M, Javaherzadeh M, Pejhan S, et al. The etiological factors of recurrence after tracheal resection and reconstruction in post-intubation stenosis. Interact CardioVasc Thorac Surg. 2009;9:446–9. doi: 10.1510/icvts.2009.202978. [DOI] [PubMed] [Google Scholar]


