Abstract
Primary calcified tumours of major central veins are extremely rare. Epithelioid haemangioendotheliomas (EHs) are malignant tumours of vascular origin with very limited reports in the literature. The aetiology is unknown. Immunohistochemically, tumours are often positive for at least one endothelial marker. We present a unique presentation of an EA in the superior vena cava.
Keywords: Epithelioid haemangioendothelioma, Endothelial marker, Calcified tumour
CASE REPORT
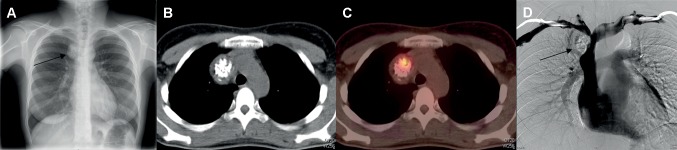
A 29-year old woman, a radiology technician, was referred to our surgical department for a widened superior mediastinum noticed on a routine chest radiograph (Fig. 1). Her medical history and physical examination were unremarkable (normal performance status, no fever, no superior cava syndrome) and the tumour markers (AFP, ACE, LDH, βHCG) were normal. A review of the chest radiograph confirmed the finding of a mediastinal mass that seemed to project into the right hemithorax. There was no elevated hemidiaphragm. A CT scan with intravenous contrast demonstrated an intraluminal non-enhancing calcified tumour (43 by 34 mm) in the superior vena cava (SVC), at the confluence of the brachiocephalic veins. An angiogram confirmed the invasion of the SVC at the confluence of the left and right bachiocephalic veins. A positron emission tomographic (PET)-CT revealed an avid uptake by the mass (SUVMax = 7.4).
Figure 1:
Chest radiography showing an enlargement of the right superior mediastinum (A); CT scan (B) and PET-CT (C) showing the intense glucose avidity of the tumour; superior phlebography showing the reduced lumen of the SVC (D).
After a multidisciplinary discussion, we chose to resect this endovascular SVC tumour without preoperative histology (Fig. 2). The tumour was approached via a median sternotomy allowing control of the SVC, the left and right brachiocephalic veins and the azygos vein without a pericardial opening. The tumour was endoluminal, located at the confluence of the left and right brachiocephalic veins and appeared to make contact with the right phrenic nerve.
Figure 2:
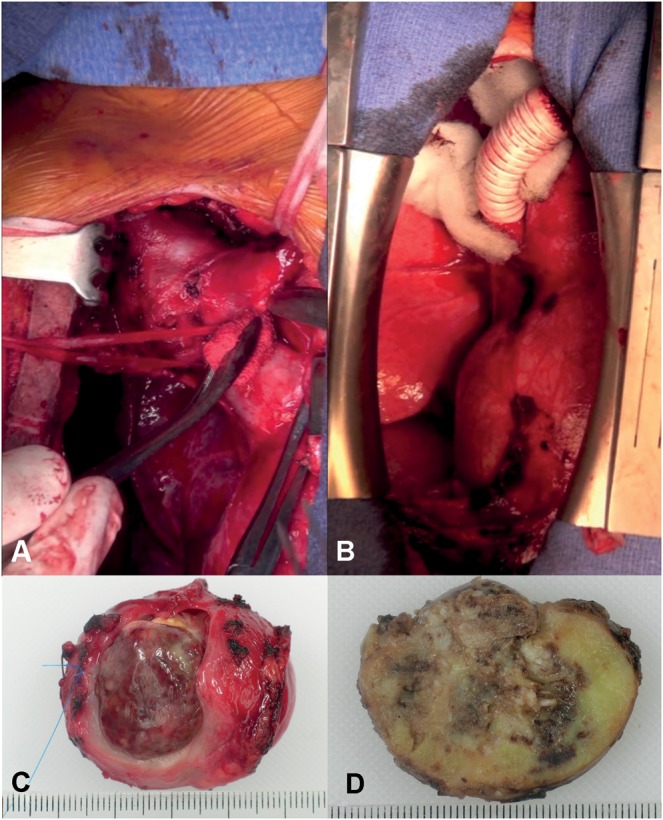
Perioperative view of the tumour at the confluence of the brachiocephalic veins (A); final view of the PTFE graft between the left brachiocephalic vein and the SVC; (B) macroscopical views of the 43 mm by 34 mm tumour (C).
After heparin injection, the SVC was cross-clamped during the procedure of resection and reconstruction.
A transverse section of the right and left brachiocephalic veins and the SVC were made to safely isolate the encased vessel and tumour.
An en bloc resection was performed that encompassed the tumour and its attachments to the mediastinum were dissected out without sacrificing the right phrenic nerve. The right brachiocephalic vein was divided with a mechanical stapler. An end-to-end anastomosis was performed between the left innominate vein and the SVC with a 16-mm PTFE graft. On gross anatomic inspection, the tumour measured 45 by 35 mm.
A final histological examination reported a complete resection of an epithelioid haemangioendothelioma (EH) of the SVC. After an uneventful postoperative course, our patient left the hospital on postoperative day 9. Ten months after surgery, the PTFE tube graft of the innominate vein is still patent.
DISCUSSION
EHs are rare malignant tumours of vascular origin that often involve soft tissues and visceral organs and, less commonly, large veins [1, 2]. The term ‘EH’ was defined first by Weiss and Enzinger [3] in 1982 as a soft tissue vascular tumour of endothelial origin with a clinical course between that of a benign haemangioma and angiosarcoma. An EH is a neoplasm composed of epithelioid endothelial cells characterized by their round or polygonal shape, abundant eosinophilic hyaline cytoplasm and the presence of cytoplasmic vacuoles and vesicular nuclei.
There is a wide histological spectrum between the benign epithelioid haemangioma and the malignant epithelioid angiosarcoma; the EH seems to lie in the middle of this spectrum.
Only 35 cases of vascular EHs are described in the literature. Most of them are hepatic EH that spread into the inferior vena cava [4, 5]; according to Ferretti's review of the literature [6], among the 16 cases of mediastinal EH, there were two innominate vein cases, two azygos vein cases and two SVC cases.
Tumour histology has not been reliable in predicting the clinical outcome. In the largest study of 137 cases of hepatic EH, the histology of the tumour, including nuclear polymorphism and mitotic count, was of no value in predicting the clinical outcome [1]. Immunohistochemically, tumours are often positive for at least one endothelial marker (factor VIII-related antigen [FVIII-RAg], CD34, CD31); in our case, the tumour was CD34 positive and factor VIII-Rag positive [1].
Patients are often asymptomatic despite the evidence of occlusive disease confirmed on venography; tumours are often incidentally discovered after an abnormal chest radiograph [2]. The tumours have ranged from discrete nodules to a mass of coalesced nodules. Radiographically, contrast-enhanced CT reveals a well-defined rounded mass of fat attenuation occluding the lumen of the SVC [6]. Superior vena cavography typically shows a reduced lumen of the SVC and a large lobulated filling defect. Only surgical therapy for EH has proved beneficial, with an ambiguous role for adjuvant chemotherapy and none for radiation therapy for liver EH [1, 2, 4]. An en bloc resection is needed to control all the major thoracic veins.
The reconstruction of only one brachiocephalic vein facilitates better blood flow in the prosthesis and also long-term patency of the SVC bypass. Anaesthetic techniques prevent complications of SVC clamping: through a femoral central venous access, continuous arterial and venous pressures are increased to maintain the physiological arterial–venous brain parenchymal gradient. After clamping, the level of the central venous pressure increases, while a level of the mean arterial pressure (stabilized with fluid administration and intravenous vasopressors) is maintained. The period of SVC clamping should typically last no longer than 30 min, without the use of the cardiopulmonary bypass or shunt.
CONCLUSION
An EH of the SVC is a very rare and often asymptomatic vascular malignant tumour. This diagnosis must be considered when a calcified tumour of a major central vein is discovered. Contrast-enhanced CT, superior cavography and PET-CT are useful for the diagnosis and guiding surgery. A safe and complete surgical resection is the optimal approach. No adjuvant treatment is recommended.
Conflict of interest: none declared.
References
- 1.Makhlouf HR, Ishak KG, Goodman ZD. Epithelioid hemangioendothelioma of the liver: a clinicopathologic study of 137 cases. Cancer. 1999;85:562–82. doi: 10.1002/(sici)1097-0142(19990201)85:3<562::aid-cncr7>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 2.Mehrabi A, Kashfi A, Fonouni H, Schemmer P, Schmied BM, Hallscheidt P, et al. Primary malignant hepatic epithelioid hemangioendothelioma: a comprehensive review of the literature with emphasis on the surgical therapy. Cancer. 2006;107:2108–21. doi: 10.1002/cncr.22225. [DOI] [PubMed] [Google Scholar]
- 3.Weiss SW, Enzinger FM. Epithelioid hemangioendothelioma: a vascular tumor often mistaken for a carcinoma. Cancer. 1982;50:970–81. doi: 10.1002/1097-0142(19820901)50:5<970::aid-cncr2820500527>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 4.De Verbizier G, Gasquet C, Barret D, Drouineau J, Poncin E, Touchard G, et al. Epithelioid hemangioendothelioma of the liver and superior vena cava. Radiological results apropos of a case in an adult. J Radiol. 1987;68:55–9. [PubMed] [Google Scholar]
- 5.Scordi-Bello IA, Snyder A, Schwartz M, Fallon JT. Intravascular epithelioid hemangioendothelioma of the inferior vena cava: case report of an unusual and unpredictable vascular tumor. Cardiovasc Pathol. 2009;18:243–6. doi: 10.1016/j.carpath.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 6.Ferretti GR, Chiles C, Woodruff RD, Choplin RH. Epithelioid hemangioendothelioma of the superior vena cava: computed tomography demonstration and review of the literature. J Thorac Imaging. 1998;13:45–8. doi: 10.1097/00005382-199801000-00011. [DOI] [PubMed] [Google Scholar]