Abstract
Objective To estimate the very early stroke risk after a transient ischaemic attack (TIA) or minor stroke and thereby inform the planning of effective stroke prevention services.
Design Population based prospective cohort study of patients with TIA or stroke.
Setting Nine general practices in Oxfordshire, England, from April 2002 to April 2003.
Participants All patients who had a TIA (n = 87) or minor stroke (n = 87) during the study period and who presented to medical attention.
Main outcome measures Risk of recurrent stroke at seven days, one month, and three months after TIAs and minor strokes.
Results The estimated risk of recurrent stroke was 8.0% (95% confidence interval 2.3% to 13.7%) at seven days, 11.5% (4.8% to 18.2%) at one month, and 17.3% (9.3% to 25.3%) at three months after a TIA. The risks at these three time periods after a minor stroke were 11.5% (4.8% to 11.2%), 15.0% (7.5% to 22.5%), and 18.5% (10.3% to 26.7%).
Conclusions The early risks of stroke after a TIA or minor stroke are much higher than commonly quoted. More research is needed to determine whether these risks can be reduced by more rapid instigation of preventive treatment.
Introduction
Approximately 15% of ischaemic strokes are preceded by a transient ischaemic attack (TIA).1 This “warning” event provides an opportunity to prevent stroke, and guidelines highlight the need for rapid access clinics.2-4 However, although much work has been done on the causes and dangers of delayed assessment after acute major stroke,5,6 few studies of TIA or minor stroke have been done, and we do not know how urgently patients must be seen for these clinics to be effective. North American guidelines recommend that assessment and investigation should be completed within one week of a TIA or minor stroke,7,8 and British guidelines recommend assessment within two weeks,2,3 but routine practice varies widely.9 In the United Kingdom, the national service framework for older people requires that rapid access stroke prevention services are in place by April 2004.4 However, no guidance is given for how rapidly patients should be seen.
The danger of delaying investigation and treatment after a TIA or minor stroke depends on the early risk of subsequent stroke. Commonly quoted risks, of 1-2% at seven days and 4% at one month,1,8,10-13 are underestimates because patients were usually recruited several weeks after the TIA and any patients who had a major stroke during this period were excluded. A study of patients presenting to an emergency department within 24 hours of a TIA reported a risk of stroke of 5.3% at two days,14 but no recent data from population based studies exist, and no data are available on the risk of recurrence after a minor stroke, which is also usually investigated in “TIA” clinics.
We have studied the early risk of stroke after a TIA or minor stroke in a prospective population based study (the Oxford vascular study), in which patients are enrolled as soon as possible after their symptoms and detailed information is collected on the timing of onset of symptoms and early recurrent events.
Methods
The Oxford vascular study is a population based study of the incidence and prognosis of TIA and stroke.15 The methods and population are similar to those of the Oxfordshire community stroke project (1981-6).16 The study covers a population of 90 542, registered with 63 general practitioners in nine family health centres in Oxfordshire, England. Registration of patients into the study began on 1 April 2002 and continued until 31 March 2003.
Collaborating general practitioners were encouraged to notify the study physician immediately by telephone, pager, or facsimile of any patient whom they thought might have had a TIA or stroke. We made regular checks to ensure that all relevant patients were referred, by means of a liaison general practitioner in each practice, a bimonthly visit to each practice from the study research nurse, frequent personal contact between the study physicians and the general practitioners, and searches of practice diagnostic codes. We ascertained patients presenting to hospital by daily review of hospital admission registers, emergency department attendance records, and admission to the John Radcliffe Hospital stroke unit and other relevant wards and by regularly checking all requests for brain and carotid imaging. Patients not needing hospital admission were seen as soon as possible by a study physician in a daily (Monday to Friday) clinic or assessed in the community. We recorded the date and time of onset of each vascular event and the date and time that each patient first sought medical attention. In addition to standard ascertainment, a study nurse did follow up by face to face interview at one month and three months. If the nurse suspected a recurrent event a study neurologist (PMR) re-examined the patient.
We included patients in this analysis if they presented with a first or recurrent TIA or minor stroke, diagnosed according to standard criteria, during the study period.16,17 We defined minor stroke as ≤ 3 on the National Institutes of Health stroke scale at the time of initial assessment.18 We excluded patients if they did not give informed consent or if assent from the nearest relative was unavailable. We calculated actuarial survival free of stroke from the time of onset of the first TIA or the first minor stroke during the study period.
Results
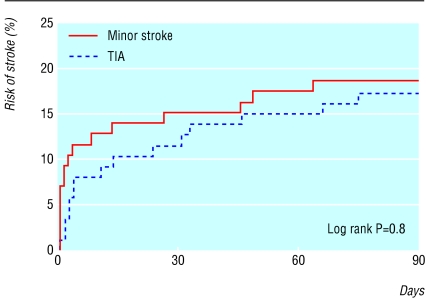
We recruited 87 patients with a TIA and 87 patients with a minor stroke (table). We excluded 83 patients with major stroke (National Institutes of Health score > 3). All patients were followed up for 3 months. During this time 15 patients with TIA had a subsequent stroke, two of which were fatal and three of which resulted in an increased Rankin score at three months' follow up.19 The remaining 10 cases were minor strokes, and we therefore entered them into the minor stroke analysis from the date of the minor stroke onwards. Sixteen patients with minor stroke had a subsequent stroke, of which four were fatal and two resulted in increased disability at three months. The estimated stroke risks after a TIA were 8.0% (95% confidence interval 2.3% to 13.7%) at seven days, 11.5% (4.8% to 18.2%) at one month, and 17.3% (9.3% to 25.3%) at three months. The risks at the three time points were similar (log rank P = 0.8; figure) after a minor stroke: 11.5% (4.8% to 11.2%), 15.0% (7.5% to 22.5%), and 18.5% (10.3% to 26.7%).
Table 1.
Characteristics of patients included in the analyses. Values are numbers (percentages) unless stated otherwise
| Characteristics | TIA patients (n=87) | Minor stroke patients (n=87) |
|---|---|---|
| Mean (SD) age (years) | 75.0 (10.8) | 73.0 (12.5) |
| Male sex | 38 (44) | 41 (47) |
| Previous TIA or stroke | 36 (41) | 19 (22) |
| Treated hypertension | 48 (55) | 47 (54) |
| Current smoking | 5 (6) | 19 (22) |
| Treated diabetes mellitus | 10 (12) | 10 (12) |
| Angina | 18 (21) | 16 (18) |
| Previous myocardial infarction | 16 (18) | 16 (18) |
| History of treated hyperlipidaemia | 28 (32) | 21 (24) |
| Antiplatelet treatment before event | 44 (51) | 36 (41) |
| Anticoagulated before event | 6 (7) | 1 (1) |
TIA=transient ischaemic attack.
Figure 1.
Cumulative risk of stroke after a transient ischaemic attack (TIA) or minor stroke
Five TIA patients and three minor stroke patients had their subsequent stroke before seeking medical attention after the initial event. If we exclude these patients to produce more conservative estimates, the seven day, one month, and three month stroke risks are 7.2% (1.7% to 12.8%), 8.4% (2.4% to 14.4%), and 13.3% (6.0% to 20.6%) after a TIA and 7.2% (1.7% to 12.8%), 10.9% (4.2% to 17.6%), and 14.6% (7.0% to 22.2%) after a minor stroke.
Discussion
Our results support the findings of a recent reanalysis of the data from the Oxford community stroke project, which showed similarly high risks of stroke after a first ever TIA.20 However, this analysis was based on data collected 20 years ago, when fewer patients were likely to be taking stroke prevention treatments, and it did not include patients with minor stroke. Our more recent data have important clinical implications. If patients present to medical attention very soon after a TIA or minor stroke, either in general practice or in the emergency department, the risk of stroke is high and urgent preventive treatment is needed. This is particularly important for patients in whom specific treatments are indicated, such as those with cardiac embolism or carotid stenosis. Patients with atrial fibrillation need anticoagulation,21 and benefit from carotid endarterectomy falls rapidly with time after a TIA or non-disabling stroke.22 British guidelines recommend that patients with TIA and minor stroke should be seen in clinics within two weeks,2,3 but our data show that a substantial number of patients will have a stroke before being seen in such clinics. For stroke prevention to be most effective, patients will need to be seen within the first few hours or days.
Delays before patients are included into studies lead to underestimation of the risk, because strokes occurring during this time are excluded. We minimised these delays in our study by prompt evaluation of patients in a daily clinic. Nevertheless, a short delay is unavoidable, and a few patients in our study who had a recurrent stroke before seeking medical attention for the initial TIA or minor stroke were therefore included retrospectively. This can result in an overestimation of the risk, because an unknown number of patients who had no recurrent event and who never presented to the study are excluded. However, only eight patients were ascertained retrospectively, and exclusion of these cases did not significantly alter our results.
In conclusion, the estimated risk of stroke after a TIA or minor stroke is 8-12% at seven days and 11-15% at one month. For stroke prevention to be effective, the public would need to be educated to seek medical attention urgently and services would need to be organised such that all patients with TIA or minor stroke are seen immediately. Further research is needed to determine the most effective strategy to prevent early recurrent stroke.
What is already known on this topic
How urgently patients with transient ischaemic attack and minor stroke should be seen for effective stroke prevention is uncertain
The commonly quoted risks of early stroke after a TIA of 1-2% at seven days and 2-4% at one month are probably underestimates
Recent reports based on 20 year old data suggest that the early risks of stroke after a TIA are much higher than previously quoted; no equivalent data exist for minor stroke
What this study adds
The early risks of stroke after either a TIA or a minor stroke are much higher than usually quoted: 8-12% at seven days and 11-15% at one month
Public education about the symptoms of TIA or stroke are needed so that patients seek medical attention quickly
Patients who present soon after their symptoms need urgent investigation and stroke prevention treatment
We thank everyone who helped with this project, particularly M Giles (study physician), P Edwards (study administrator), and L Silver and L Bull (study nurses). We especially thank the participating general practitioners. The participating general practices were (name of liaison partner from each practice only): M Raine (19 Beaumont Road, Oxford), T Nicholson-Lailey (East Oxford Health Centre, Oxford), H Hoy (Health Centre, Berinsfield), D Otterburn (Malthouse Surgery, Abingdon), S Street (Exeter Surgery, Kidlington), D Evans (Kidlington and Yarnton Medical Group, Kidlington), M Drury (Church Street, Wantage), M Robertson (Marcham Road Family Health Centre, Abingdon), and P Buttar (Abingdon Surgery, Abingdon).
AJC collected the data, assisted in the study design and data analysis, and drafted the paper. JKL analysed the data, assisted with data collection, and drafted the paper. PMR had the original idea, designed the study, assisted with data collection and in drafting the manuscript, and is the guarantor. As guarantor, PMR accepts full responsibility for the conduct of the study, has access to the data, and controlled the decision to publish.
Funding: The first year of the Oxford vascular study was supported by grants from the Medical Research Council and the Stroke Association.
Competing interests: None declared
Ethical approval: The study was approved by the Oxfordshire clinical research ethics committee (C0.043).
References
- 1.Hankey GJ. Impact of treatment of people with transient ischaemic attack on stroke incidence and public health. Cerebrovasc Dis 1996;6(suppl 1): 26-33. [Google Scholar]
- 2.Intercollegiate Working Party for Stroke. National clinical guidelines for stroke. London: Royal College of Physicians, 2000.
- 3.Scottish Intercollegiate Guidelines Network. SIGN guidelines: management of patients with stroke. Edinburgh: SIGN, 1997.
- 4.Department of Health. National service framework for older people. London: Department of Health, 2001.
- 5.Evenson KR, Rosamond WD, Morris DL. Prehospital and in-hospital delays in acute stroke care. Neuroepidemiology 2001;20: 65-76. [DOI] [PubMed] [Google Scholar]
- 6.Proceedings of a national symposium on rapid identification and treatment of acute stroke. Washington: National Institute of Neurological Disorders and Stroke, 1997.
- 7.Feinberg WM, Albers GW, Barnett HJ, Biller J, Caplan LR, Carter LP, et al. Guidelines for the management of transient ischemic attacks. Circulation 1994;89: 2950-65. [DOI] [PubMed] [Google Scholar]
- 8.Wolf PA, Clagett GP, Easton JD, Goldstein LB, Gorelick PB, Kelly-Hayes M, et al. Preventing ischemic stroke in patients with prior stroke and transient ischemic attack: a statement for healthcare professionals from the Stroke Council of the American Heart Association. Stroke 1999;30: 1991-4. [DOI] [PubMed] [Google Scholar]
- 9.Johnston SC, Smith WS. Practice variability in management of transient ischemic attacks. Eur Neurol 1999;42: 105-8. [DOI] [PubMed] [Google Scholar]
- 10.Gubitz G, Phillips S, Dwyer V. What is the cost of admitting patients with transient ischaemic attacks to hospital? Cerebrovasc Dis 1999;9: 210-4. [DOI] [PubMed] [Google Scholar]
- 11.Warlow CP, Dennis MS, van Gijn J, Sandercock PAG, Bamford JM, Wardlaw JM. Preventing recurrent stroke and other serious vascular events. In: Stroke: a practical guide to management. Oxford: Blackwell Science, 2001.
- 12.Gubitz G, Sandercock P. Prevention of ischaemic stroke. BMJ 2000;321: 1455-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hankey GJ, Dennis MS, Slattery JM, Warlow CP. Why is the outcome of transient ischaemic attacks different in different groups of patients? BMJ 1993;306: 1107-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Johnston SC, Gress DR, Browner WS, Sidney S. Short-term prognosis after emergency department diagnosis of TIA. JAMA 2000;284: 2901-6. [DOI] [PubMed] [Google Scholar]
- 15.Schulz UG, Rothwell PM. Differences in vascular risk factors between etiological subtypes of ischemic stroke: importance of population-based studies. Stroke 2003;34: 2050-9. [DOI] [PubMed] [Google Scholar]
- 16.Bamford J, Sandercock P, Dennis M, Burn J, Warlow C. A prospective study of acute cerebrovascular disease in the community: the Oxfordshire Community Stroke Project—1981-86. 2: incidence, case fatality rates and overall outcome at one year of cerebral infarction, primary intracerebral and subarachnoid haemorrhage. J Neurol Neurosurg Psychiatry 1990;53: 16-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dennis MS, Bamford JM, Sandercock PA, Warlow CP. Incidence of transient ischemic attacks in Oxfordshire, England. Stroke 1989;20: 333-9. [DOI] [PubMed] [Google Scholar]
- 18.Goldstein LB, Bertels C, Davis JN. Interrater reliability of the NIH stroke scale. Arch Neurol 1989;46: 660-2. [DOI] [PubMed] [Google Scholar]
- 19.Van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke 1988;19: 604-7. [DOI] [PubMed] [Google Scholar]
- 20.Lovett JK, Dennis MS, Sandercock PAG, Bamford J, Warlow CP, Rothwell PM. The very early risk of stroke after a transient ischaemic attack. Stroke 2003; 138-40e. [DOI] [PubMed]
- 21.EAFT (European Atrial Fibrillation Trial) Study Group. Secondary prevention in non-rheumatic atrial fibrillation after transient ischaemic attack or minor stroke. Lancet 1993;342: 1255-62. [PubMed] [Google Scholar]
- 22.Rothwell PM, Eliasziw M, Gutnikov SA, Warlow CP, Barnett HJM, for the Carotid Endarterectomy Trialists' Collaboration. Effect of endarterectomy for symptomatic carotid stenosis in relation to clinical subgroups and to the timing of surgery. Lancet 2004. (in press). [DOI] [PubMed]