The sudden unexpected death of an infant or child is one of the worst events to happen to any family. Bereaved parents expect and should receive appropriate, thorough, and sensitive investigations to identify the medical causes of such deaths. As a result, several parallel needs must be fulfilled. Firstly, the needs of the family must be recognised—including the need for information and support. Further, there is the need to identify any underlying medical causes of death that may have genetic or public health implications; the need for a thorough forensic investigation to exclude unnatural causes of death; and the need to protect siblings and subsequent children.1-5 Alongside this, families need to be protected from false or inappropriate accusations. Limitations in the present coronial system have led to delays or failures to detect deaths caused by relatives, carers, or health professionals.6 w1 w2 w3 Several recent, highly publicised trials have highlighted the possibilities of parents facing such accusations. As a result of this the whole process of death certification has come under intense scrutiny.7-9 w1 w2 w3
We review the medical, forensic, and sociological literature on the optimal investigation and care of families after the sudden death of a child. We describe the implementation in the former county of Avon of a structured multiagency approach and the potential benefits for families and professionals.
Methods
We conducted a literature search of Medline, the Social Science Citation Index, and the International Bibliography of the Social Sciences from 1966 to 2002, and CINAHL from 1982 to 2002, using the search terms “death scene” plus “sudden infant death syndrome,” and “child abuse” plus “sudden infant death or death, sudden.” We also searched the extensive database of relevant publications held in the Foundation for the Study of Infant Deaths research unit in the University of Bristol. We contacted investigating authorities in the United States, Australia, Canada, Scandinavia, and New Zealand. We conducted an extensive secondary search of references cited in publications identified in the above searches.
We reviewed all studies describing the processes of care of families and the investigation of the cause of sudden death in infancy or childhood. Most studies were anecdotal and descriptive, very few included appropriate controls, and none included long term outcome data for populations or individual families.
Summary points
In an optimal investigation after the sudden death of a child, the emphasis is on care and sensitivity throughout, and on continued sharing of information with the family and between agencies
A paediatrician and the police are involved immediately (with close consultation with social services) and visit the home and the scene of death
The primary healthcare team, in collaboration with the paediatrician, is also involved immediately
A full paediatric postmortem examination is carried out to an agreed protocol
The case is discussed at a multiagency case meeting, and all agencies offer continued support, care, and information to the family
The family is given full information orally and in writing, with the opportunity to ask questions
Professional responses to sudden unexpected deaths
The main purposes of professional responses are
To provide support and information for bereaved families
To investigate the circumstances of the death and identify potentially preventable factors or evidence of neglect or abuse
To collect and collate information on patterns of causes of death, and to identify potentially significant epidemiological or environmental factors
To modify current practices in medical or social care to reduce the risk of such deaths in the future.
The balance between these purposes varies widely between and within countries. The identification where possible of a cause of death may in itself be very important in the process of providing help to the bereaved family.1,2,10 w2 w3
Balance between care and investigation
In many countries the professional responses to sudden unexpected deaths in infancy are based on the investigation of the death and the identification of contributory factors, including abuse and neglect. Care of the bereaved family is commonly not a primary responsibility of the investigating agencies.1,5,11-14
In the United Kingdom a population based case-control study of sudden deaths in infants conducted in 1993-6 as part of the Confidential Enquiry into Stillbirths and Deaths in Infancy (CESDI) investigated a wide range of social, medical, economic, and environmental factors.2 w4 w5 w6 The study included a detailed semistructured interview with the parents of 456 infants who had died suddenly and similar interviews of the 1800 parents of age matched surviving control infants. Postmortem examinations were conducted to an agreed protocol and reviewed by independent paediatric pathologists. Each death was confidentially reviewed by a multiprofessional committee, which noted any contributory factors, and classified the “cause” of death according to an agreed protocol.2,15 This study showed that for 80% (363/456) of sudden deaths in infants no sufficient explanation of death was identified, and the death therefore met the definition of sudden infant death syndrome.2,16 Twenty one deaths (4.6% of the total sudden deaths of infants) were thought to be directly due to non-accidental injury. In the infants whose deaths were classified as sudden infant death syndrome, maltreatment (acts of commission or omission) was thought to be a contributory factor in a further 22 deaths (4.8% of the total sudden deaths of infants). Thus for more than 90% of the deaths no suspicion of maltreatment arose as a cause or important contributory factor. For such families the emphasis should be on care and support, and on the identification or exclusion of contributory medical factors. Thorough investigation of the circumstances of the death may be of great importance in protecting innocent families from later accusations, but an insensitive or inadequate approach to investigation can add to the distress experienced by families.9,17-19 Even where the death is a result of abuse or neglect the wider family, including any siblings and any non-abusing parent, will need support.
What investigations are needed?
Arnestad et al reviewed investigations into sudden deaths of infants carried out in Oslo and assessed their relative values in the identification of specific causes of deaths.13 Of 309 sudden deaths of infants, 73 (24%) were found to be due to specific identifiable causes, (infections, accidents, or non-accidental injuries). In the identification of these causes, the case history was a major factor for 10% (30) of deaths, the examination of the circumstances of the death for 42% (130), and the gross postmortem examination for 44% (136). For many the combination of two or more investigations was necessary to make the diagnosis. In a similar study in Australia Mitchell et al found that the assessment of the scene of death was less often informative.20
The nature and complexity of the postmortem examination after the sudden death of an infant should also be clearly related to the probability of finding an explanation for the death. Various complex protocols have been described.3,13,16,20-22 The public reaction to the past practices of tissue or organ retention has led to a marked reduction in the investigations carried out at postmortem examination by some pathologists, with a consequent lack of potentially important information on conditions (such as metabolic disorders) that may have major genetic implications for other members of the family. Berry et al have defined an evidence based postmortem protocol for such infants, which balances the probability of obtaining useful information against the needs of parents for the examination to be completed quickly, with a minimum of tissue retention.2 This protocol, based on the large UK CESDI study, shows that with a minimum number of tissue samples taken for histological examination, combined with radiological, microbiological, and biochemical investigations and a thorough clinical history, virtually all of the deaths for which a cause could be ascertained will be identified correctly.
Interpretation of findings at the scene of death
One difficulty with investigations at the scene of death is that they are commonly conducted by professionals who visit homes only after an infant has died, and findings that may be social, cultural, or economic markers of normal patterns of child care may be misinterpreted as being causally related to the death. Conversely, without good “control” information, factors (for example, sleeping position) of great importance in the aetiology of the deaths may not be recognised.
Although some hazardous sleeping environments can be identified by investigations of the death scene, it is dangerous to overinterpret more subtle findings in the absence of appropriate controls that are matched for age, social group, ethnic origin, and culture.2,23 w4 w6 w7 w8
Medical or forensic investigation of sudden deaths in infancy
In the assessment of the possibility of abuse or neglect as a cause of injury or illness in childhood the emphasis over the past 10 years has increasingly been on multiagency cooperation and joint working practices.18,19,24 w7 w9 w10 In the United Kingdom, police child protection teams, social services departments, and medical carers have developed joint protocols to ensure prompt recognition of child abuse or neglect and early investigation and action where appropriate. In most areas the police child protection team consists of experienced crime investigators, with training and experience in the care of children and families in difficult circumstances.
Given the requirement by most coroners that all sudden unexpected deaths are investigated by the police, such investigations are best conducted by child protection officers working as part of a multiagency team including medical and social services staff.
Avon's multiagency approach
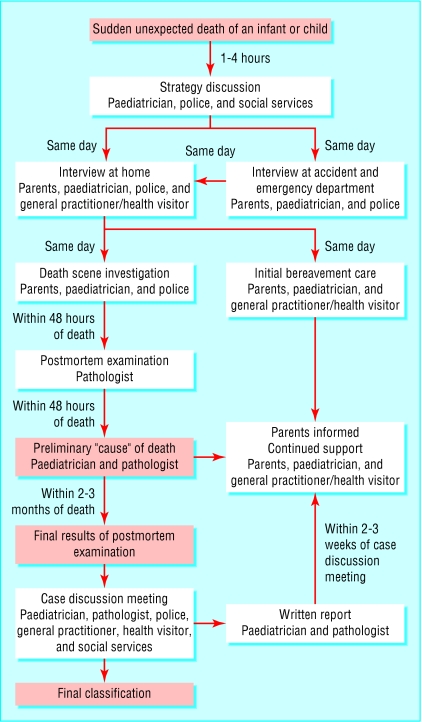
The approach that has been adopted in Avon is based on the practices recommended in the report of the CESDI study, and endorsed by the Foundation for the Study of Infant Deaths (fig 1).2 w3 w11
Fig 1.
Avon's multiagency approach to sudden unexpected deaths in infancy and childhood
Early strategy discussion
As soon as possible after every sudden unexpected death of an infant a strategy discussion is held that includes the paediatrician, the police child protection team, and the social services duty team. The purpose of the discussion is to plan how best to investigate the death and support the family.
Joint home visit by police and paediatrician
The paediatrician and police officer usually see the family together in the accident and emergency department, followed by a joint home visit, usually with the family doctor or health visitor. A full medical and social history is taken, with particular emphasis on recent events and a careful review of the circumstances and scene of the death.
Historically, the scene of the death of a baby was approached by police officers as a “scene of crime,” and the same rules with regard to preservation of evidence were applied as at any suspected homicide. In developing the Avon protocol, police were reassured that evidence for any potential criminal inquiry was not at risk of being compromised.
By visiting the home and seeing where the baby died, both the police and the paediatrician can gain further information, and family members are given the opportunity to talk through what happened in detail. Both police and paediatrician, in conjunction with the primary healthcare team, provide further support to the family. Families have expressed great appreciation of this coordinated approach, recognising the need for police involvement but feeling that the joint visits have been helpful rather than intrusive.
Postmortem examination
Information is passed to the pathologist by the paediatrician, to ensure that appropriate and relevant postmortem investigations are carried out. A full postmortem examination is conducted to an agreed protocol.2 Preliminary information on the postmortem is fed back to the family as it becomes available. When major concerns are raised about child protection issues the police or social services may become the “lead” agency, but the paediatrician and primary healthcare team continue their involvement with the family.
Multiagency meeting to discuss the case
Finally, two to three months after the death a meeting is held to discuss the case, which includes all professionals who were involved with the family. This gives an opportunity to review the classification of the death, identify any contributory factors (fig 2), debrief all parties participating in the care of the family, and plan for continuing support of the family, including informing them of the assessment of the cause of the infant's death. The family is given a written explanation in plain English of what is understood of the cause of death and the results of the pathology investigations, and a meeting is arranged for the family with the paediatrician and general practitioner to answer their questions and identify continuing needs for support.
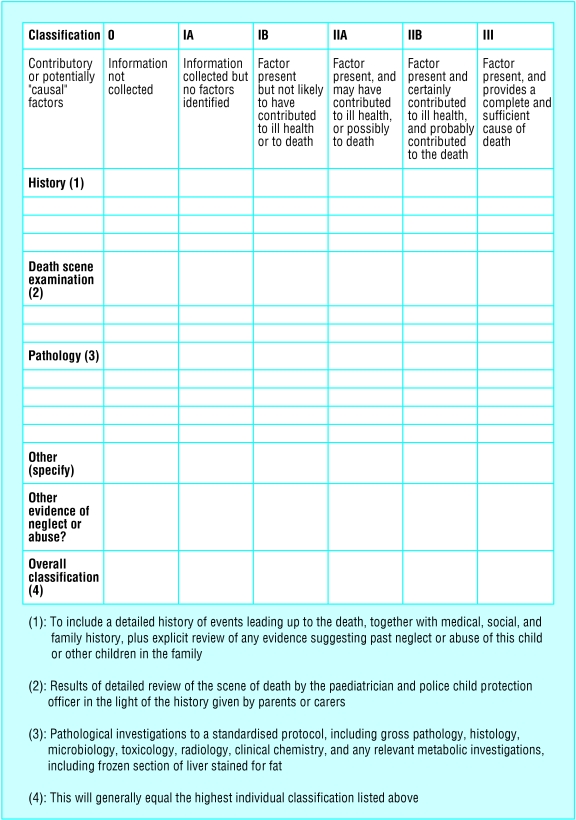
Fig 2.
Grid for completion at multidisciplinary case meeting. Entry is made for each heading and score (0-III) agreed for each line. Overall score is generally equal to the highest score in the grid; III=complete and sufficient cause of death, I-IIB=sudden infant death syndrome
This joint approach ensures that all necessary information is collected sensitively and promptly, with a minimum of repetition. The broad experience of normal childcare practices in the community that is brought by the paediatrician and child protection team reduces the risk of attributing death or injury to normal variants in patterns of child care. The continuing participation of the paediatricians in research into current childcare practices in the community further helps to inform their interpretation of information obtained after infant deaths.
Summary
The sudden unexpected death of an infant or young child warrants careful, evidence based investigation involving child protection teams, healthcare staff, and social services, to include a careful review of the history, examination of the scene of the death, postmortem examination to an evidence based protocol, and a multiagency review meeting. The aim is to provide help and support for the bereaved family, to identify where possible the cause of the death, to help prevent further such deaths if possible, and to ensure that future children are protected from avoidable environmental hazards, medical conditions (for example, metabolic conditions), and abuse.
Supplementary Material
 References w1-w11 are on bmj.com
References w1-w11 are on bmj.com
Contributors: PS, PJF, and PSB jointly conducted the literature review. PS, PJF, and TH jointly developed the multiagency protocol.
Competing interests: PJF has given expert evidence in both civil and criminal court proceedings on the subject of the investigation of unexpected deaths of infants.
References
- 1.Byard RW, Cohle SD. Sudden death in infancy, childhood and adolescence. Cambridge: Cambridge University Press, 1994.
- 2.Fleming PJ, Blair P, Bacon C, Berry PJ. Sudden unexpected deaths in infancy. The CESDI SUDI studies 1993-1996. London: Stationery Office, 2000.
- 3.Centers for Disease Control and Prevention. Guidelines for death scene investigation of sudden unexplained infant deaths: recommendations of the interagency panel on sudden infant death syndrome. Morb Mortal Wkly Rep MMWR 1996;45(RR-10): 1-22. [Google Scholar]
- 4.Bass M, Kavath RE, Glass L. Death-scene investigation in sudden infant death. N Engl J Med 1986;315: 100-5. [DOI] [PubMed] [Google Scholar]
- 5.American Academy of Pediatrics. Committee on Child Abuse and Neglect. Distinguishing sudden infant death syndrome from child abuse fatalities. Pediatrics 2001;107: 437-41 [PubMed] [Google Scholar]
- 6.Stanton J, Simpson A. Murder misdiagnosed as SIDS: a perpetrator's perspective. Arch Dis Child 2001;85: 454-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dyer C. Group to review babies' deaths. BMJ 2003;327: 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Walkins SJ. Conviction by mathematical error? BMJ 2000;320: 2-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Meadow R. A case of murder and the BMJ. BMJ 2002;324: 41-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dent A, Condon L, Blair P, Fleming PJ. A study of bereavement care after a sudden and unexpected death. Arch Dis Child 1996;74: 522-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morentin B, Aguilera B, Garamendi PM, Suarez-Mier MP. Sudden unexpected non-violent death between 1 & 19 years in north Spain. Arch Dis Child 2000;82: 456-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Durfee M, Tilton-Durfee D. Multiagency child death review teams: experiences in the United States. Child Abuse Rev 1995:4: 377-81. [Google Scholar]
- 13.Arnestad M, Vege A, Rognum TO. Evaluation of diagnostic tools applied in the examination of sudden unexpected deaths in infancy and early childhood. Forensic Sci Int 2002;125: 262-8. [DOI] [PubMed] [Google Scholar]
- 14.Rognum T, Lier L. Police investigation and SIDS: an improved system of co-operation between health personnel, forensic pathologists and the police. In: Rognum T, ed. Sudden infant death syndrome: new trends in the nineties. Oslo: Scandinavian University Press, 1995: 289-92.
- 15.Gilbert RE, Rudd PT, Berry PJ, Fleming PJ, Hall E, White DG, et al. Combined effect of infection and heavy wrapping on the risk of sudden infant death. Arch Dis Child 1992;67: 272-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Willinger M, James S, Catz C. Defining the SIDS: deliberations of an expert panel convened by the National Institute of Child Health and Human Development. Pediatr Pathol 1991;11: 677-84. [DOI] [PubMed] [Google Scholar]
- 17.Dyer C. Paediatricians did not have duty of care to patient's mother. BMJ 2002;325: 1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Working Party of the Royal College of Paediatrics and Child Health. Fabricated or induced illness by carers. Report of the working party of the Royal College of Paediatrics and Child Health. London: RCPCH, 2002.
- 19.Department of Health. Safeguarding children in whom illness is fabricated or induced. London: DoH, 2002.
- 20.Mitchell E, Krous HF, Donald T, Byard RW. An analysis of the usefulness of specific stages in the pathologic investigation of sudden infant death. Am J Forensic Med Pathol 2000;21: 395-400. [DOI] [PubMed] [Google Scholar]
- 21.Krous HF. The international standardised autopsy protocol for sudden unexpected infant death. In: Rognum T, ed. Sudden infant death syndrome: new trends in the nineties. Oslo: Scandinavian University Press, 1995: 81-98.
- 22.Wigglesworth JS, Keeling JW, Rushton DI, Berry PJ. Pathological investigations in cases of sudden infant death. J Clin Pathol 1987;40: 1481-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mitchell EA, Stewart AW, Scragg R, Ford RPK, Taylor BJ, Becroft DMO, et al. Ethnic differences in mortality from sudden infant death syndrome in New Zealand. BMJ 1993;306: 13-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Creighton SJ. Fatal child abuse—how preventable is it? Child Abuse Rev 1995;4: 318-28. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.