Whether a smoker succeeds in stopping smoking depends on the balance between that individual's motivation to stop smoking and his or her degree of dependence on cigarettes. Clinicians must be able to assess both of these characteristics. Motivation is important because “treatments” to assist with smoking cessation will not work in smokers who are not highly motivated. Dependence is especially important in smokers who do want to stop smoking, as it influences the choice of intervention. It is also important to bear in mind that:
Motivation to stop and dependence are often related to each other: heavy smokers may show low motivation because they lack confidence in their ability to quit; lighter smokers may show low motivation because they believe they can stop in the future if they wish
Motivation to stop can vary considerably with time and be strongly influenced by the immediate environment
What smokers say about their wish to stop, especially in a clinical interview, may not accurately reflect their genuine feelings.
Measuring dependence in smokers
Qualitative methods
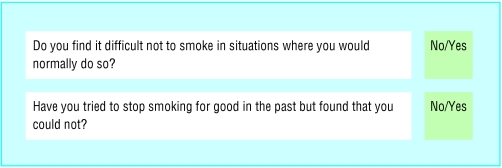
The simplest approach to measuring dependence on cigarettes is a basic qualitative approach that uses questions to find out whether the smoker has difficulty in refraining from smoking in circumstances when he or she would normally smoke or whether the smoker has made a serious attempt to stop in the past but failed.
Figure 1.
Clinical intervention goals for smoking according to dependence and motivation to quit
Quantitative methods
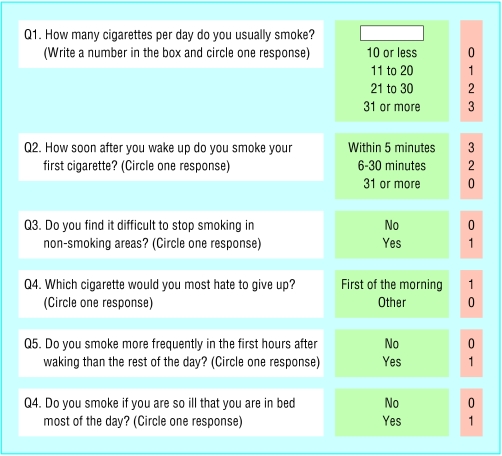
The most commonly used quantitative measure of dependence is the Fagerstrom test for nicotine dependence, which has proved successful in predicting the outcome of attempts to stop. The higher the score on this questionnaire, the higher the level of dependence: smokers in the general population score an average of about 4 on this scale. Of all the items in the questionnaire, cigarettes per day and time to first cigarette of the day seem to be the most important indicators of dependence.
Figure 2.
A “yes” response to either of these questions would suggest that the smoker might benefit from help with stopping
Objective methods
The concentration of nicotine or its metabolite, cotinine, in blood, urine, or saliva is often used in research as an objective index of dependence because it provides an accurate measure of the quantity of nicotine consumed, which is itself a marker of dependence. Carbon monoxide concentration of expired air is a measure of smoke intake over preceding hours; it is not as accurate an intake measure as nicotine based measures, but it is much less expensive and gives immediate feedback to the smoker.
Figure 3.
The Fagerstrom test for nicotine dependence: a quantitative index of dependence. The numbers in the pink shaded column corresponding to the smoker's responses are added together to produce a single score on scale of 0 (low dependence) to 10 (high dependence). Adapted from Heatherton et al. Br J Addict1991;86: 1119-27
How should dependence influence choice of treatment?
The main value of measuring dependence in tailoring cessation interventions to individual smokers is in the choice of pharmacotherapy. The manufacturers of smoking cessation drug products (principally nicotine replacement therapy and bupropion—see later chapters in this series) recommend that only smokers of 10 or more cigarettes a day should use their products. However, the UK National Institute for Clinical Excellence has recently recognised this cut off to be arbitrary and has not specified any particular lower limit for daily cigarette consumption.
This article reviews some simple methods to assess dependence and motivation in smokers
Measuring motivation to stop smoking
Survey evidence in the United Kingdom shows that about two thirds of smokers declare that they want to stop smoking and that in any year almost a third make an attempt to stop. Young smokers are widely believed to be less motivated to stop than older smokers, but in fact the reverse is true: older smokers are typically less motivated.
Table 2.
Dependence and dose of nicotine in treatment
| • The nicotine dose should be guided by measures of dependence |
| • The higher strength forms of nicotine replacement are particularly recommended for high dependence smokers |
| • For nicotine therapy, high dependence smoking is typically considered to be at least 15-20 cigarettes a day and/or smoking within 30 minutes of waking |
| Nicotine therapy will be covered in a later article in this series |
However, only a minority of smokers attempting to stop currently use smoking cessation medications or attend a specialist cessation service. This may reflect a lack of confidence among smokers that these treatments will help.
Table 3.
Estimated prevalence of selected indices of motivation to stop smoking
| Index | % of smokers |
|---|---|
| Would like to stop smoking for good |
70 |
| Intend to stop smoking in next 12 months |
46 |
| Made an attempt to stop in a given year |
30 |
| Used medication to aid cessation in a given year* |
8 |
| Attended smokers clinic or followed behavioural support programme† | 2 |
Based on surveys showing that 30% of smokers make a quit attempt each year and that in 25% of quit attempts medication is used.
Based on figures from attendance in 2001 at NHS cessation clinics.
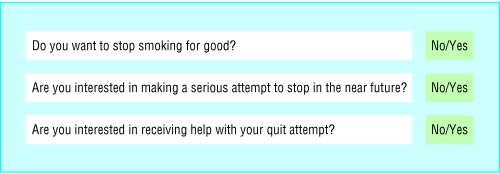
Direct questioning
Motivation to stop can be assessed qualitatively by means of simple direct questions about their interest and intentions to quit. This simple approach is probably sufficient for most clinical practice, although slightly more complex, semiquantitative measures (asking the smoker to rate degree of desire to stop on a scale from “not at all” to “very much”) can also be used.
Stages of change
One model of the process of behaviour change has become popular: the “transtheoretical model.” In this model, smokers are assigned to one of five stages of motivation: precontemplation (not wishing to stop), contemplation (thinking about stopping but not in the near future), preparation (planning to stop in the near future), action (trying to stop), and maintenance (have stopped for some time). Smokers may cycle through the contemplation to action stages many times before stopping for good. This model has been widely adopted, though no evidence exists that the rather elaborate questionnaires for assigning smokers to particular stages predict smoking cessation better than the simple direct questions outlined above.
Figure 4.
Simple qualitative test of motivation to stop smoking. A “yes” response to all questions suggests that behavioural support and/or medication should be offered
Some clinicians use a smoker's degree of motivation to stop as a prognostic indicator of likely success once the quit attempt has been decided. In fact, degree of motivation seems to play a fairly small role in success; once a quit attempt is made, markers of dependence are far stronger determinants of success. The ultimate practical objective of assessing motivation is therefore to identify smokers who are ready to make a quit attempt. After that, it is the success of the intervention in overcoming dependence that matters.
Figure 5.
Stages of change in process of stopping smoking. Adapted from Prochaska et al. Clin Chest Med 1991;12: 727-35
Table 1.
Key points
| • Motivation to stop smoking can be assessed with simple questions |
| • Once a decision to quit is made, success is determined more by the degree of dependence than the level of motivation |
| • Simple questions can identify heavily dependent smokers |
| • For high dependence, higher strength nicotine products may help |
The ABC of smoking cessation is edited by John Britton, professor of epidemiology at the University of Nottingham in the division of epidemiology and public health at City Hospital, Nottingham. The series will be published as a book in the late spring.
Competing interests: RW has done paid research and consultancy for, and received travel funds and hospitality from, manufacturers of smoking cessation products, including nicotine replacement therapies and Zyban. See first article in this series (24 January 2004) for the series editor's competing interests.
References
- • Kozlowski LT, Porter CQ, Orleans CT, Pope MA, Heatherton T. Predicting smoking cessation with self-reported measures of nicotine dependence: FTQ, FTND, and HSI. Drug Alcohol Depend 1994;34: 211-6. [DOI] [PubMed] [Google Scholar]
- • National Institute for Clinical Excellence. Technology appraisal guidance No 38. Nicotine replacement therapy (NRT) and bupropion for smoking cessation. London: NICE, 2002.
- • Sutton S. Back to the drawing board? A review of applications of the transtheoretical model to substance use. Addiction 2001;96: 175-86. [DOI] [PubMed] [Google Scholar]