Abstract
PURPOSE
The purpose of this clinical study was to evaluate the frequency and type of prosthetic complications in relation to type and properties of removable dentures and to investigate the influence of these complications and several data about the existing dentures on patient satisfaction.
MATERIALS AND METHODS
Ninety nine patients (44 males and 55 females) wearing removable dentures have been included in the study. The complications of the patients were recorded; patient satisfaction was determined with a Visual Analog Scale (VAS) and the relationship of complications and patient satisfaction with several data about the dentures such as denture age, type of denture, centric relation and vertical dimension was investigated. Kruskal Wallis, Mann Whitney U and Chi square tests were used for statistical analyses. The results were evaluated statistically at a significance level of P<.05.
RESULTS
Need for addition of artificial teeth for dentures with correct centric relations was found to be significantly lower than dentures with wrong centric relations (P<.01). Loss of retention, ulcerations and high vertical dimension affected the VAS chewing ability scores negatively and ulcerations affected the VAS phonation scores negatively (P<.05).
CONCLUSION
Considering the results of this study, it can be concluded that loss of retention, ulcerations and high vertical dimension caused patient dissatisfaction. Additionally, dentures with wrong centric relations caused need for addition of artificial teeth.
Keywords: Complete denture, Patient satisfaction, Partial denture
INTRODUCTION
The loss of teeth can impair function, esthetics and phonation and is restored most of the time with prosthesis. Although preventive dentistry helps protecting teeth, the demand for prosthodontic treatment is expected to rise even in developed countries as a result of a rapid increase in their elderly population.1-3 Many countries are facing an aging population, which will cause a ratio of individuals over 65 years of age up to 50% in the coming decades. The number of edentulous patients even in countries with a high standard of dental health care is significant.1,3 According to the World Health Organization (WHO) Global Oral Data Bank the prevalence of edentulism older than 65 years was shown as 58% in Canada, 41% in Finland and 46% in the United Kingdom.1
Removable dentures are an economic and easy treatment modality for edentulous or partially edentulous patients and are still widely used.4 However, these dentures can be associated with various complications. It is assumed that failures are consequences of destructive action of bad designed and manufactured dentures, since many clinicians delegate planning to technicians. Dental technicians may have a key role in the success of dentures, but it should be pointed out that they do not have adequate knowledge about biological structures and occlusion, which is needed for distribution of masticatory forces adequately. For this reason the final tooth setup is always checked clinically by dentists. There is not enough research about the data such as vertical dimension, centric relation, and position of the artificial teeth relative to the denture base underlying tissues and borders of dentures, giving information about the general trend of quality of dentures delivered in general practice.4
There are several textbooks pointing out the importance of precise denture base adaptation, setup of the artificial teeth in the right position, establishment of correct centric relation and vertical dimension for the maintenance of stability and retention of removable dentures.4-7 It could also be expected that the above mentioned factors could influence the emergence of complications. However, there are not enough clinical studies evaluating removable dentures.8
The quality of complete dentures assessed by clinicians does not always come to accordance with the subjective judgment of the patients. Although a number of studies failed to show statistically significant relations between the two variables,9-12 other studies could show weak or moderately significant associations.13-18
It can be assumed that the quality of the prosthetic treatment may also affect oral health, thus oral health is related to quality of life, since prosthodontic as well as surgical treatment is performed to improve patients' satisfaction.19-25 A previous denture quality assessment of 1306 removable partial dentures (RPDs) in the United States had found that 65% of the RPDs had various types of defects, indicating potential for quality improvement.26 Combined with the high prevalence of RPDs in the general US population,27 improvement of RPD quality could have a substantial effect on population oral health, assuming a causal association between denture quality and Oral Health Related Quality of Life (OHRQoL). On the other hand, a very recent study has reported that the quality of removable dentures had a minimal effect on OHRQoL.28
This clinical study was designed to collect information about the various complications such as fracture of denture base or other components, the need for relining, the need for repair of artificial teeth, and to evaluate their possible relation with denture type and several properties of the dentures. Additionally, the influence of these complications and several data about the existing dentures on patient satisfaction was evaluated.
MATERIALS AND METHODS
Patients from regular circulation at a University Clinic for Prosthetic Dentistry having applied for new dentures during a 3 month period have been examined and interviewed. The criteria of selection were that patients had worn conventional partial or complete removable dentures for at least 3 years. 99 patients (mean age: 63.26 ± 9.6 years; 44.4% male, 55.6% female) who had met these criteria were included in the present study. The study was approved by the institutional review board.
The removable dentures were divided into the following groups:
A maxillary complete denture vs. mandibular complete denture (CD/CD)
A maxillary complete denture vs. mandibular removable partial denture (CD/RPD)
A maxillary removable partial denture vs. mandibular complete denture (RPD/CD)
A maxillary removable partial denture vs. mandibular removable denture (RPD/RPD)
Subjects' age, gender and dental status including number of former dentures and age of the present dentures, period of edentulism, presence of prosthetic complications were recorded. Subsequently the dentures were examined by two experienced prosthodontists, blinded to the treatment, and data regarding retention, stability, the position of artificial teeth, condition of the dentures in terms of hygiene and coloring and technical problems have been collected.
Following prosthetic complications have been recorded as present or not present:
Loss of retention
Existence of any denture irritation or ulceration
Existence of any debonded/fractured artificial teeth
Existence of any fracture in the denture base
Existence of fractured retaining clasps
Existence of denture stomatitis
Existence of epulis fissuratum
Existence of inflammatory papillary hyperplasia
The borders of the existing dentures which influence the peripheral seal as well as the denture stability have been evaluated and classified as long, normal and short for each maxillary and mandibular denture separately.
Vertical dimension of all patients was determined as correct, high or low, whereas the overlapping of centric occlusion with centric relation evaluated as wrong or right. For the determination of the vertical dimension the closest speaking space was used as usually in the department. In order to be able to prevent confusion, 3 patients with upper and lower partial dentures and natural occlusion where a centric occlusion could not be established, have been excluded from the study group. The patients in the study group wearing upper and lower partial dentures (RPD/RPD) had no natural occlusion (tooth to tooth contact).
Conditions of the denture were evaluated in two categories:
a) Hygiene (good/bad),
b) Wear of the artificial teeth and coloring (present/absent).
A 100 mm Visual Analog Scale (VAS)29 was signed out by the patients to assess their personal opinion based on three main factors including esthetics, phonetics and mastication.
Statistical analyses were used in this study to evaluate the influence of various parameters on denture complications. For the statistical analysis of the results the NCSS (Number Cruncher Statistical System) 2007 & PASS 2008 Statistical Software (Kaysville, UT, USA) was used. Demographic parameters (age and gender), denture types and complications were evaluated. Beside descriptive statistics (means and standard deviations), Mann Whitney U test was used for the comparison of the parameters of two groups and Kruskal Wallis test was used for the comparison of quantitative data of more than two groups. For the determination of the group engendering the difference, the Mann Whitney U test was used. The comparison of qualitative data was performed using a Chi square test. The results were assessed at 95% confidence interval, at a significance level of .05.
RESULTS
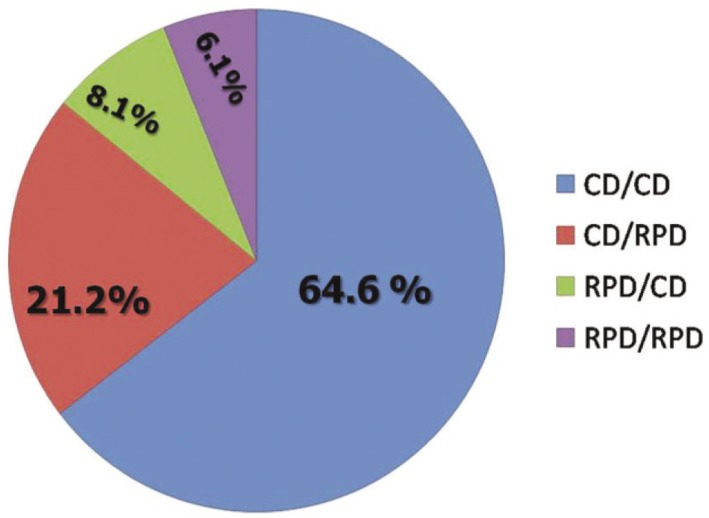
99 patients with removable dentures were evaluated in the present study. The distribution of the dentures is shown in Fig. 1.
Fig. 1.
Distribution of denture types (n = 64 for CD/CD, n = 21 for CD/RPD, n = 8 for RPD/CD, and n = 6 for RPD/RPD).
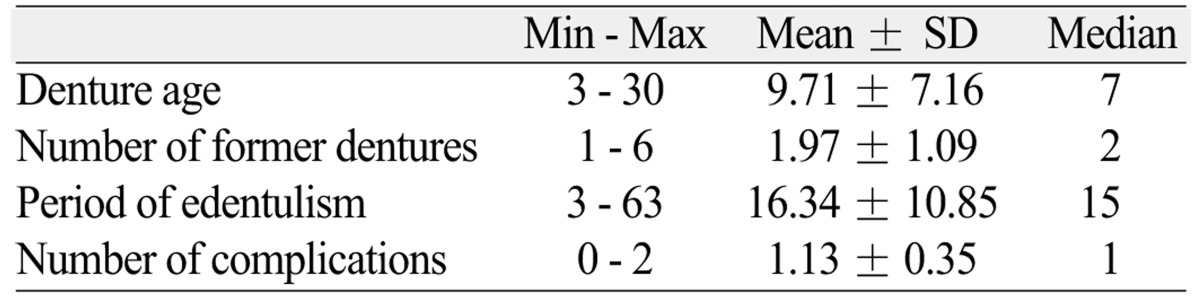
Patient's denture ages, the number of former dentures, the period of edentulism are shown in Table 1. The number of complications per denture varied between 0 and 2 (Table 1).
Table 1.
Descriptive data about denture age, period of edentulism, number of former dentures and number of complications
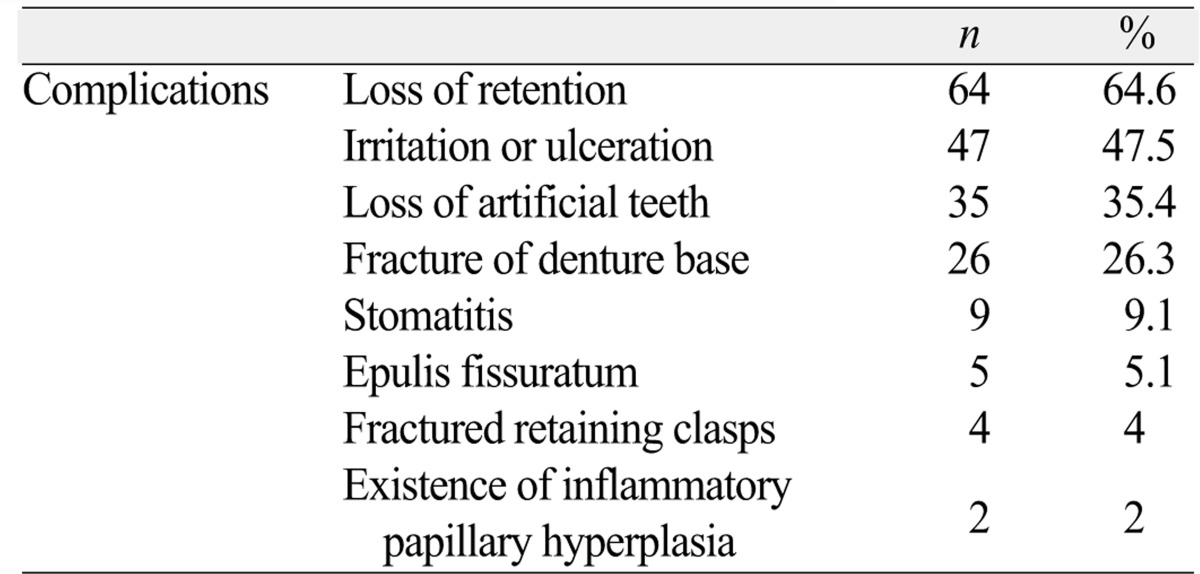
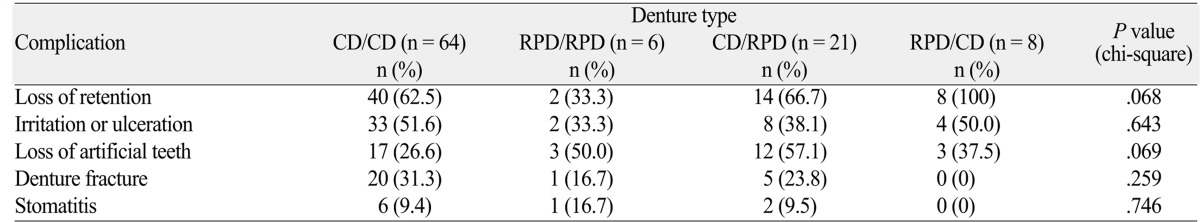
The type and occurrence frequency of complications are shown in Table 2. No significance was noted between the complication frequency and type of the prosthesis (P>.05).
Table 2.
The incidence of complications
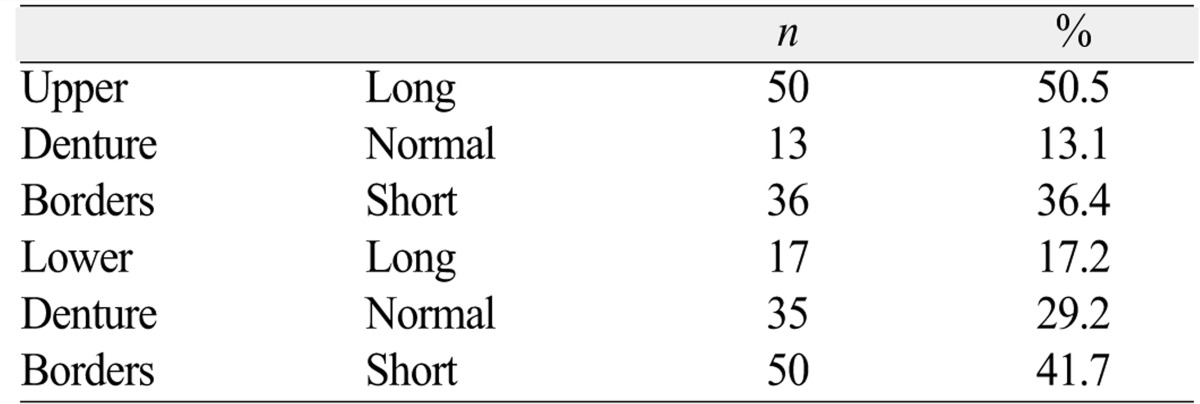
Distribution of the assessed border lengths of the dentures are listed in Table 3.
Table 3.
The evaluation of the borders of the denture bases
The evaluation of the centric relation of the patients' dentures revealed that in 61.6% of the subjects the centric occlusion was correct, whereas in 38.4% of the cases there was a discrepancy between habitual intercuspal position and centric relation.
It was determined that only 2% of the dentures' vertical dimension was correct. 26.3% of the patients had a denture with a high vertical dimension where as 71.7% of the patients had a denture with a low vertical dimension.
The hygiene of dentures was found inadequate for 51.5% of the subjects. 53.5% dentures had worn artificial teeth and 67.7% showed coloration.
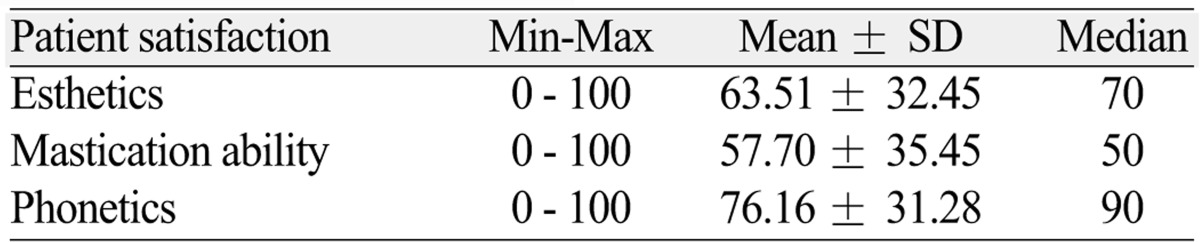
The esthetic, phonetic and masticatory performance VAS scores are shown in Table 4.
Table 4.
The VAS scores
No statistically significant difference was found between denture and complication types (P>.05; Table 5).
Table 5.
Distribution of different denture types and complications
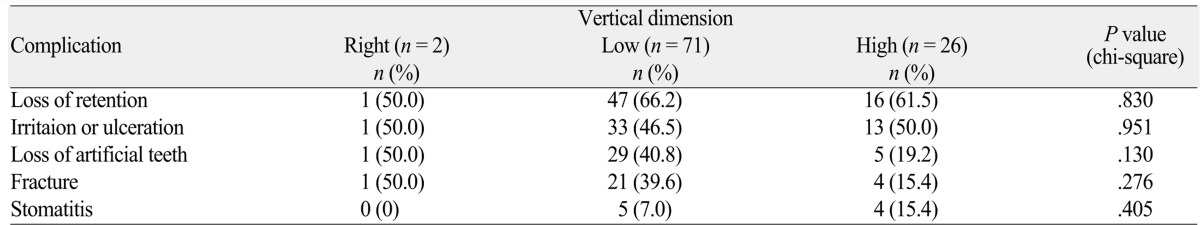
No statistically significant difference was observed between denture type and vertical dimension results (P>.05; Table 6).
Table 6.
Distribution of complications in relation to vertical dimension
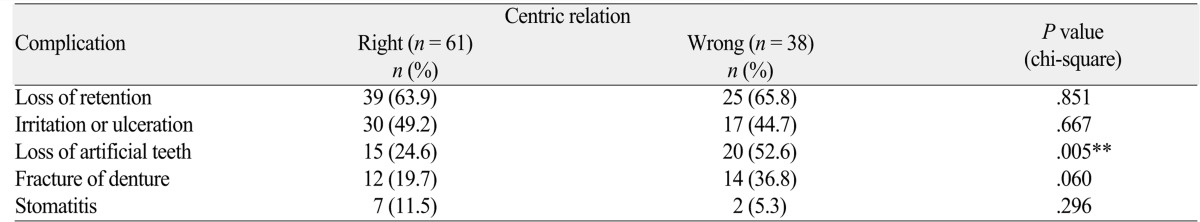
Statistically significant difference was found between centric relation and need for addition of artificial teeth (P<.01). Need for addition of artificial teeth for dentures which had a correct centric relation was found to be significantly lower than dentures having a wrong centric relation (Table 7). No statistically significant difference was found between centric relation and loss of retention, mucosal irritation/ulceration, denture fracture and stomatitis (P>.05; Table 7).
Table 7.
Distribution of complications in relation to accuracy of the centric relation
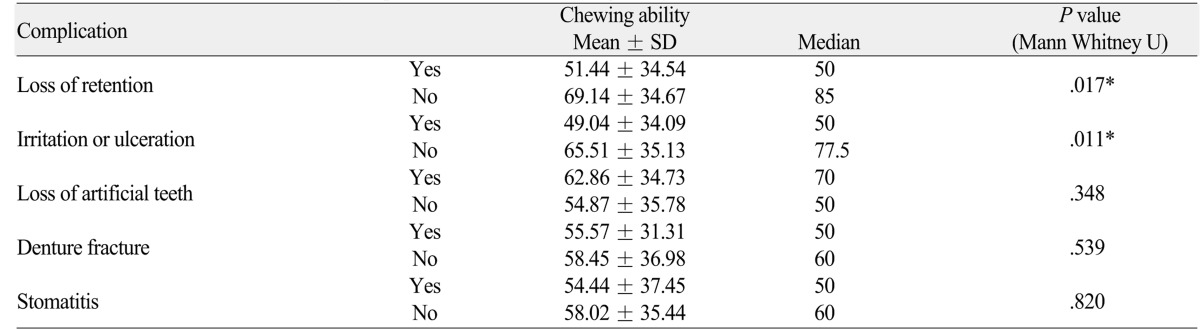
Significant difference was found between VAS esthetic scores and complication types (P>.05). The relationship between VAS chewing ability scores and complication types are shown in Table 8. Loss of retention and ulcerations affected the VAS chewing ability scores negatively (P<.05; Table 8)
Table 8.
The relation between occurring complications and VAS chewing ability scores
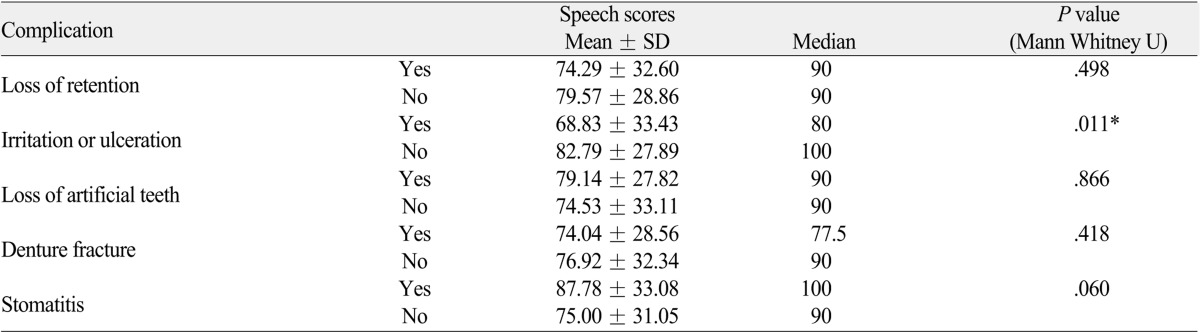
The relationship between VAS phonetic scores and complication types are shown in Table 9. Only ulcerations affected the scores negatively (P=.011); whereas the other complications had no significant effect (P>.05; Table 9).
Table 9.
The relation between occurring complications and VAS speech scores
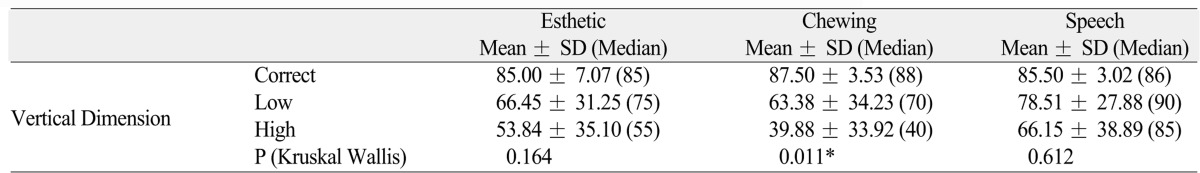
Significant difference was found between VAS esthetic, phonetic and chewing ability scores and centric relation (P>.05). Vertical dimension didn't affect the VAS esthetic and phonetic scores (P>.05); whereas VAS scores for chewing ability of dentures were found to be statistically significantly different according to vertical dimension (P<.05). VAS chewing ability scores with higher vertical dimension were found to be significantly lower than the dentures with lower (P=.012) and correct vertical dimensions (P=.042; Table 10).
Table 10.
The relation between vertical dimension and VAS esthetic, chewing ability and speech scores
DISCUSSION
Although a major part of the population in many countries has an incomplete dentition, a substantial number of patients remain either not prosthetically restored30 or functioning with a shortened dental arch without any need for treatment.31 Nevertheless, the restoration of oral function and esthetics especially in higher economic groups is preferred. The replacement of missing teeth can be achieved by fixed or removable appliances, but generally it is accepted that removable dentures deteriorate in a shorter time period,32 even though there are studies indicating more favorable results by careful planning, regular recall appointments, patient instruction and prosthetic adjustments.33-35
Although conventional metal frame removable partial or complete dentures are not the ideal solution, this option is widely used for the treatment of partial or complete edentulism. The number of studies evaluating the success, complication rate and patient satisfaction related to removable prosthesis is relatively scarce. There are rather studies dealing with the fate of the abutment teeth,36,37 periodontal status of the remaining teeth38 or the comparison of the influence of different denture types on patient satisfaction and patients' quality of life.39
Lack of stability and retention of the mandibular dentures, increasing in time with ongoing residual bone resorption, the impaired chewing ability are the main complaints of complete denture wearers.40 These handicaps combined with the consequential pain and impairment of patients' ability to communicate may cause dissatisfaction.
The most frequent complication in the present study was the loss of retention which is in agreement with previous reports.1,41,42 Most of the patients in the present study complained about the looseness and misfitting of their dentures. This complication is the main reason of need for replacement of their dentures. Additionally, loss of retention caused dissatisfaction of patients related to function. The loss of retention of the dentures may have impaired the patients' ability to chew. A denture sore spot which is the second frequent encountered complication might also be related to the misfitting of the dentures. Sheppard et al.43 revealed denture looseness as the main cause of complaints of denture wearers, followed by pain which corroborates the results of our study. Furthermore, with the presence of denture sore spots, patients reported lower phonetic and chewing satisfaction scores. The low phonetic VAS scores may be due to the overextension of the upper dentures onto the soft palate which generally results in speech difficulties and the low chewing VAS scores may be the reason of the sore spots in buccal surfaces of the maxillary tuberosities, buccal and lingual surfaces of mandibular crest because of instability or frenulum impingements. An interesting finding of this study was the insignificant difference between the complication number, complication type and type of the prosthesis. It is usually estimated for the removable partial dentures to show fewer complications than complete dentures due to the presence of teeth which consequently result in more retentive dentures. This finding may be because of the unequal distributions of patients into denture groups which can be regarded as a limitation of this study.
In the first year following tooth extraction a loss of bone width by 25% and a loss in bone height of 4 mm can be expected.44 With the use of removable dentures, bone loss continues over the years. It was observed that half of the evaluated dentures had long borders in the present study. This might be explained as the ongoing process of bone resorption with removable denture use of the patients and inability of the present dentures to compensate this resorption as well as the overextended impressions taken often by inexperienced clinicians.
The establishment of a correct centric occlusion is very important for the success of removable dentures; especially when the removable denture is a complete denture.45 Dawson had defined centric relation as the relationship of mandible to the maxilla when the properly aligned condyle/disc assemblies are in the most superior positions against the eminence irrespective of tooth positions or vertical dimension,45 which is the best repeatable position of the mandible. In the present study it was found that need for addition of artificial teeth for dentures which had a correct centric relation was significantly lower than dentures having a wrong centric relation. This might be explained as the result of an occlusal disharmony with the presence of a wrong centric occlusion. The artificial teeth may have encountered unequal forces and therefore been broken.
Vertical dimension of occlusion is defined as "the distance measured between two points when the occluding members are in contact".46 Actually vertical dimension can be accurately determined in the clinic with various methods and its value has diagnostic validity.47 In all circumstances, an adequate interocclusal rest space must be developed in the range of 2 to 4 mm. Faults in the development of the appropriate individualized dimension can result either an increased or decreased vertical dimension of occlusion.48 It was reported that improper vertical dimension of occlusion with inadequate interocclusal clearance as the most common error found in patients with removable dentures.49 However, the results of the present study were not in agreement with a previous study.49 Only 26.3% of the patients with existing dentures had a high vertical dimension; whereas a majority (71.7%) dentures with low vertical dimension. This result is in accordance with the findings of Carlsson and Persson44 and caused a significantly lower patient satisfaction. It has been shown that removable denture wearers with high vertical dimension generally complain of uncertain pains involving both maxilla and mandible and a feeling of tiredness of the jaws.48 This may be the reason of low VAS chewing ability scores in patients with high vertical dimension. The trend between clinicians during denture fabrication though seems to be towards establishment of low vertical dimension, since dentures with low vertical dimensions are expected to cause less dissatisfaction.
The major limitation of this study is that the sample group consists of patients having sought prosthodontic treatment or repair service at a university prosthodontic clinic. The results may vary in the general population wearing removable dentures. To be able to generalize the results, more studies in different centers with higher case numbers which would provide valuable information should be accomplished. The evaluation of recently delivered dentures in various clinics would additionally elicit valuable data.
CONCLUSION
Within the limitations of the present study following conclusions may be drawn:
The most frequently encountered complication in association with removable dentures is the loss of retention, followed by ulcerations.
Complications do not affect the esthetic patient satisfaction scores, whereas loss of retention causes dissatisfaction of patients related to chewing ability.
Complications do not affect the esthetic patient satisfaction scores, whereas loss of retention causes dissatisfaction of patients related to chewing ability.
It was seen that a vast majority of the dentures had a wrong vertical dimension and especially the high vertical dimension caused a significant decrease in patient satisfaction concerning chewing ability.
References
- 1.Petersen PE, Yamamoto T. Improving the oral health of older people: the approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol. 2005;33:81–92. doi: 10.1111/j.1600-0528.2004.00219.x. [DOI] [PubMed] [Google Scholar]
- 2.Felton DA. Edentulism and comorbid factors. J Prosthodont. 2009;18:88–96. doi: 10.1111/j.1532-849X.2009.00437.x. [DOI] [PubMed] [Google Scholar]
- 3.Turkyilmaz I, Company AM, McGlumphy EA. Should edentulous patients be constrained to removable complete dentures? The use of dental implants to improve the quality of life for edentulous patients. Gerodontology. 2010;27:3–10. doi: 10.1111/j.1741-2358.2009.00294.x. [DOI] [PubMed] [Google Scholar]
- 4.Grant AA, Heath JR, McCord JF. Complete prosthodontics: problems, diagnosis and management. 1st ed. Manchester: Mosby Inc.; 1994. pp. 33–115. [Google Scholar]
- 5.Basker RM, Davenport JC. Prosthetic treatment of the edentulous patient. 4th ed. Berlin: Wiley-Blackwell; 2002. pp. 71–80. [Google Scholar]
- 6.Zarb GA, Bolender CL, Eckert SE, Fenton AH, Jacob RF, Mericske-Stern R. Prosthodontic treatment for Edentulous Patients: Complete Dentures and Implant-supported Prosthesis. 12th ed. St. Louis: Mosby; 2004. pp. 268–329. [Google Scholar]
- 7.Devlin H. Complete dentures: A clinical manual for the general dental practitioner. Berlin: Springer; 2002. pp. 33–59. [Google Scholar]
- 8.Dorner S, Zeman F, Koller M, Lang R, Handel G, Behr M. Clinical performance of complete dentures: a retrospective study. Int J Prosthodont. 2010;23:410–417. [PubMed] [Google Scholar]
- 9.Langer A, Michman J, Seifert I. Factors influencing satisfaction with complete dentures in geriatric patients. J Prosthet Dent. 1961;11:1019–1031. [Google Scholar]
- 10.Smith M. Measurement of personality traits and their relation to patient satisfaction with complete dentures. J Prosthet Dent. 1976;35:492–503. doi: 10.1016/0022-3913(76)90043-3. [DOI] [PubMed] [Google Scholar]
- 11.Manne S, Mehra R. Accuracy of perceived treatment needs among geriatric denture wearers. Gerodontology. 1983;2:67–71. [Google Scholar]
- 12.Magnusson T. Clinical judgement and patients' evaluation of complete dentures five years after treatment. A follow-up study. Swed Dent J. 1986;10:29–35. [PubMed] [Google Scholar]
- 13.Salonen MA. Assessment of states of dentures and interest in implant-retained prosthetic treatment in 55-year-old edentulous Finns. Community Dent Oral Epidemiol. 1994;22:130–135. doi: 10.1111/j.1600-0528.1994.tb01588.x. [DOI] [PubMed] [Google Scholar]
- 14.Bergman B, Carlsson GE. Review of 54 complete denture wearers. Patients' opinions 1 year after treatment. Acta Odontol Scand. 1972;30:399–414. doi: 10.3109/00016357209002493. [DOI] [PubMed] [Google Scholar]
- 15.Heyink J, Heezen J, Schaub R. Dentist and patient appraisal of complete dentures in a Dutch elderly population. Community Dent Oral Epidemiol. 1986;14:323–326. doi: 10.1111/j.1600-0528.1986.tb01083.x. [DOI] [PubMed] [Google Scholar]
- 16.van Waas MA. The influence of clinical variables on patients' satisfaction with complete dentures. J Prosthet Dent. 1990;63:307–310. doi: 10.1016/0022-3913(90)90202-n. [DOI] [PubMed] [Google Scholar]
- 17.van Waas MA. Determinants of dissatisfaction with dentures: a multiple regression analysis. J Prosthet Dent. 1990;64:569–572. doi: 10.1016/0022-3913(90)90130-5. [DOI] [PubMed] [Google Scholar]
- 18.Kalk W, de Baat C, Kaandorp A. Comparison of patients views and dentists evaluations 5 years after complete denture treatment. Community Dent Oral Epidemiol. 1991;19:213–216. doi: 10.1111/j.1600-0528.1991.tb00148.x. [DOI] [PubMed] [Google Scholar]
- 19.Firtell DN, Finzen FC, Holmes JB. The effect of clinical remount procedures on the comfort and success of complete dentures. J Prosthet Dent. 1987;57:53–57. doi: 10.1016/0022-3913(87)90116-8. [DOI] [PubMed] [Google Scholar]
- 20.Jennings DE. Treatment of the mandibular compromised ridge: a literature review. J Prosthet Dent. 1989;61:575–579. doi: 10.1016/0022-3913(89)90279-5. [DOI] [PubMed] [Google Scholar]
- 21.Jooste CH, Thomas CJ. The influence of the retromylohyoid extension on mandibular complete denture stability. Int J Prosthodont. 1992;5:34–38. [PubMed] [Google Scholar]
- 22.Kalk W, van Waas MA, Engels SE. A comparison of different treatment strategies in patients with atrophic mandibles: a clinical evaluation after 6.5 years. Int J Prosthodont. 1992;5:277–283. [PubMed] [Google Scholar]
- 23.Harper GW. Posterior base repair to maximize complete denture retention. Compendium. 1993;14:454, 456, 458. [PubMed] [Google Scholar]
- 24.Sykora O, Sutow EJ. Posterior palatal seal adaptation: influence of processing technique, palate shape and immersion. J Oral Rehabil. 1993;20:19–31. doi: 10.1111/j.1365-2842.1993.tb01511.x. [DOI] [PubMed] [Google Scholar]
- 25.Garrett NR, Kapur KK, Perez P. Effects of improvements of poorly fitting dentures and new dentures on patient satisfaction. J Prosthet Dent. 1996;76:403–413. doi: 10.1016/s0022-3913(96)90546-6. [DOI] [PubMed] [Google Scholar]
- 26.Hummel SK, Wilson MA, Marker VA, Nunn ME. Quality of removable partial dentures worn by the adult U.S. population. J Prosthet Dent. 2002;88:37–43. [PubMed] [Google Scholar]
- 27.Douglass CW, Watson AJ. Future needs for fixed and removable partial dentures in the United States. J Prosthet Dent. 2002;87:9–14. doi: 10.1067/mpr.2002.121204. [DOI] [PubMed] [Google Scholar]
- 28.Inoue M, John MT, Tsukasaki H, Furuyama C, Baba K. Denture quality has a minimal effect on health-related quality of life in patients with removable dentures. J Oral Rehabil. 2011;38:818–826. doi: 10.1111/j.1365-2842.2011.02222.x. [DOI] [PubMed] [Google Scholar]
- 29.de Grandmont P, Feine JS, Tache′R, Boudrias P, Donohue WB, Tanguay R, Lund JP. Within-subject comparisons of implant-supported mandibular prostheses: psychometric evaluation. J Dent Res. 1994;73:1096–1104. doi: 10.1177/00220345940730051201. [DOI] [PubMed] [Google Scholar]
- 30.Battistuzzi P, Ka¨yser A, Kanters N. Partial edentulism, prosthetic treatment and oral function in a Dutch population. J Oral Rehabil. 1987;14:549–555. doi: 10.1111/j.1365-2842.1987.tb00751.x. [DOI] [PubMed] [Google Scholar]
- 31.Witter DJ, van Elteren P, Ka¨yser AF. Signs and symptoms of mandibular dysfunction in shortened dental arches. J Oral Rehabil. 1988;15:413–420. doi: 10.1111/j.1365-2842.1988.tb00177.x. [DOI] [PubMed] [Google Scholar]
- 32.Wetherell JD, Smales RJ. Partial denture failures: a long-term clinical survey. J Dent. 1980;8:333–340. doi: 10.1016/0300-5712(80)90049-4. [DOI] [PubMed] [Google Scholar]
- 33.Bergman B, Hugoson A, Olsson CO. Caries, periodontal and prosthetic findings in patients with removable partial dentures: a ten-year longitudinal study. J Prosthet Dent. 1982;48:506–514. doi: 10.1016/0022-3913(82)90352-3. [DOI] [PubMed] [Google Scholar]
- 34.Rissin L, Feldman RS, Kapur KK, Chauncey HH. Six-year report of the periodontal health of fixed and removable partial denture abutment teeth. J Prosthet Dent. 1985;54:461–467. doi: 10.1016/0022-3913(85)90413-5. [DOI] [PubMed] [Google Scholar]
- 35.Drake CW, Beck JD. The oral status of elderly removable partial denture wearers. J Oral Rehabil. 1993;20:53–60. doi: 10.1111/j.1365-2842.1993.tb01514.x. [DOI] [PubMed] [Google Scholar]
- 36.Saito M, Notani K, Miura Y, Kawasaki T. Complications and failures in removable partial dentures: a clinical evaluation. J Oral Rehabil. 2002;29:627–633. doi: 10.1046/j.1365-2842.2002.00898.x. [DOI] [PubMed] [Google Scholar]
- 37.Vermeulen AH, Keltjens HM, van't Hof MA, Kayser AF. Ten-year evaluation of removable partial dentures: survival rates based on retreatment, not wearing and replacement. J Prosthet Dent. 1996;76:267–272. doi: 10.1016/s0022-3913(96)90170-5. [DOI] [PubMed] [Google Scholar]
- 38.Wagner B, Kern M. Clinical evaluation of removable partial dentures 10 years after insertion: success rates, hygienic problems, and technical failures. Clin Oral Investig. 2000;4:74–80. doi: 10.1007/s007840050119. [DOI] [PubMed] [Google Scholar]
- 39.Geckili O, Bilhan H, Bilgin T. Impact of mandibular two-implant retained overdentures on life quality in a group of elderly Turkish edentulous patients. Arch Gerontol Geriatr. 2011;53:233–236. doi: 10.1016/j.archger.2010.11.027. [DOI] [PubMed] [Google Scholar]
- 40.van Waas MA. The influence of psychologic factors on patient satisfaction with complete dentures. J Prosthet Dent. 1990;63:545–548. doi: 10.1016/0022-3913(90)90073-l. [DOI] [PubMed] [Google Scholar]
- 41.Hobkirk JA, Abdel-Latif HH, Howlett J, Welfare R, Moles DR. Prosthetic treatment time and satisfaction of edentulous patients treated with conventional or implant-supported complete mandibular dentures: a case-control study (part 1) Int J Prosthodont. 2008;21:489–495. [PubMed] [Google Scholar]
- 42.Hobkirk JA, Abdel-Latif HH, Howlett J, Welfare R, Moles DR. Prosthetic treatment time and satisfaction of edentulous patients treated with conventional or implant-stabilized complete mandibular dentures: a case-control study (part 2) Int J Prosthodont. 2009;22:13–19. [PubMed] [Google Scholar]
- 43.Sheppard IM, Schwartz LR, Sheppard SM. Oral status of edentulous and complete denture-wearing patients. J Am Dent Assoc. 1971;83:614–620. doi: 10.14219/jada.archive.1971.0376. [DOI] [PubMed] [Google Scholar]
- 44.Carlsson GE, Persson G. Morphologic changes of the mandible after extraction and wearing of dentures. A longitudinal, clinical, and x-ray cephalometric study covering 5 years. Odontol Revy. 1967;18:27–54. [PubMed] [Google Scholar]
- 45.Dawson PE. Evaluation, diagnosis and treatment of occlusal problems. 2nd ed. St. Louis: Mosby; 1989. pp. 41–46. [Google Scholar]
- 46.The glossary of prosthodontic terms. J Prosthet Dent. 2005;94:10–92. doi: 10.1016/j.prosdent.2005.03.013. [DOI] [PubMed] [Google Scholar]
- 47.Hobkirk JA. Loss of the vertical dimension of occlusion and its management implications. Int J Prosthodont. 2009;22:520–521. [PubMed] [Google Scholar]
- 48.Jeganathan S, Payne JA. Common faults in complete dentures: a review. Quintessence Int. 1993;24:483–487. [PubMed] [Google Scholar]
- 49.Yemm R. Analysis of patients referred over a period of five years to a teaching hospital consultant service in dental prosthetics. Br Dent J. 1985;159:304–306. doi: 10.1038/sj.bdj.4805715. [DOI] [PubMed] [Google Scholar]