Abstract
Objective
Fathers, in general, have been underrepresented in studies of parent training outcome for children with ADHD, and the present study aimed to investigate the efficacy of a behavioral parent training program developed expressly for fathers.
Method
The present investigation randomly assigned 55 fathers of children ages 6–12 with ADHD to the Coaching Our Acting-out Children: Heightening Essential Skills (COACHES) program or a waitlist control group. Outcomes for the study included objective observations of parent behaviors and parent ratings of child behavior.
Results
Results indicated that fathers in the COACHES group reduced their rates of negative talk and increased rates of praise as measured in parent-child observations, and father ratings of the intensity of problem behaviors were reduced, relative to the waitlist condition. Groups did not differ on observations of use of commands or father ratings of child behavior problems. Untreated mothers did not significantly improve on observational measures or behavioral ratings.
Conclusions
This study provides preliminary evidence for the efficacy of the COACHES parenting program for fathers of children with ADHD. Results are cast in light of the larger literature on behavioral parent training for ADHD as well as how to best work with fathers of children with ADHD in treatment contexts.
Keywords: Behavioral parent training, fathers, parenting, ADHD
Fathers are underrepresented in studies of treatment outcome for parent training groups (Cassano, Adrian, Veits, & Zeman, 2006; Fabiano, 2007; Phares, 1996; Tiano & McNeil, 2005). For instance, although behavioral parent training (BPT) is a well-established, evidence-based intervention for children with ADHD (Fabiano, Pelham et al., 2009; Lundahl, Risser, & Lovejoy, 2006; Pelham & Fabiano, 2008), only a minority of studies have included fathers and/or father-focused outcomes (Fabiano, 2007; Tiano & McNeil, 2005). The lack of father participation in parent training is concerning, given that fathers contribute to many aspects of a child’s development, including the development of emotion regulation, social cognition, focused attention, and peer relationships (Parke et al., 2002), appropriate social behavior (Amato & Rivera, 1999), and academic achievement and academic sense of competence (Forehand, Long, Brody, & Fauber, 1986). Fathers also have primary responsibility for children in recreational play times (Russell & Russell, 1987), which may make these contexts important for intervention efforts for fathers (Chronis, Chacko, Fabiano, Wymbs, & Pelham, 2004).
The research on father-related outcomes for BPT for ADHD presents mixed results. Studies have shown fathers and their children benefit from BPT on measures of parenting and child behavioral outcomes when they attend BPT with the child’s mother (Danforth, Harvey, Ulaszek, & McKee, 2006; Schuhmann, Foote, Eyberg, Boggs, & Algina, 1998; Webster-Stratton, Reid, & Hammond, 2004) or alone (Fabiano, Chacko et al., 2009). Yet, in some studies fathers improve on only a portion of the outcome measures on which mothers improved (Danforth et al., 2006), or intervention effects do not maintain at follow-up (Barkley, Edwards, Laneri, Fletcher, & Metevia, 2001). There are also some studies that have suggested father involvement in BPT programs with mothers did not result in incremental improvements relative to mothers who attended BPT alone (Firestone, Kelley, & Fike, 1980; Martin, 1977). Firestone et al. (1980) speculated that it may only be necessary for one parent to attend BPT; thus there is a question whether mothers would improve in families where only fathers attended BPT.
A recent study compared a BPT intervention specifically aimed at fathers, the Coaching Our Acting-out Children: Heightening Essential Skills (COACHES) program, to a classroom-based BPT approach (Fabiano, Chacko et al., 2009). COACHES includes group BPT for fathers followed by a parent-child recreational activity (i.e., soccer game) during which fathers practice the parenting strategies in the context of the sport while coaching the game. Results included increased engagement and attendance for fathers and children in the COACHES program, and fathers in the COACHES program also rated their children as more improved relative to a BPT program without the recreational component (Fabiano, Chacko et al., 2009). However, the study was limited because it compared two active interventions and it did not include a control condition. The efficacy of the program and estimates of effect size were not obtained.
The present study was conducted to investigate the efficacy of the COACHES program for fathers of children with ADHD relative to a waitlist condition. It was hypothesized that the COACHES program would result in superior outcomes to a waitlist control group on measures of parenting and child behavior. It was further hypothesized that these effects would be maintained one-month later. Exploratory aims were to investigate whether the intervention generalized to untreated parents (e.g., mothers).
Method
Participants
Fifty-five male caregivers (hereafter referred to as “fathers”) and their 6–12 year-old child enrolled. The families were recruited through radio advertisements, mailings, and school/pediatrician referrals. Fathers and mothers who participated signed an informed consent and children signed an informed assent, and all procedures were approved by the Institutional Review Board.
Children were diagnosed with ADHD through mother, father, and teacher Disruptive Behavior Disorder (DBD) rating scales and a semi-structured DBD interview with the child’s parents (Pelham, Gnagy, Greenslade, & Milich, 1992). Mothers and fathers completed DBD ratings independently, and ratings were combined by taking the maximum symptom rating across parents. Cross-situational impairment was assessed through parent and teacher ratings on the Impairment Rating Scale (IRS; Fabiano et al., 2006). Children were diagnosed with ADHD if they met symptom criteria for ADHD between the home and school (i.e., at least six symptoms of inattentive and/or hyperactive/impulsive behavior rated as occurring “pretty much” or more), and impairment ratings indicated at least one impairment domain at home and at school rated at a score greater than three. The presence of oppositional defiant disorder and conduct disorder were also diagnosed using the DBD rating scale and interview. Participants were excluded from the study if the child had an estimated IQ below 80, psychosis, or pervasive developmental disorder. The child and parent also had to be able to speak and understand English. Families that participated in the study were asked to keep their child’s medication status steady during the 12-week study.1 Demographic information is listed in Table 1.
Table 1.
Demographic Information for Participants in the COACHES and Waitlist Group.
| COACHES (N=28) | Waitlist (N=27) | |
|---|---|---|
| Child age in years | 8.36 (SD=1.81) | 8.67 (SD=1.78) |
| Child sex | 89% male | 85% male |
| Father age in years | 40.52 (SD=7.37) | 41.63 (SD=7.26) |
| Father education | 48% High School/GED | 19% High School/GED |
| 8% Some college | 4% Some college | |
| 16% Associate’s degree | 19% Associate’s degree | |
| 8% Bachelor’s degree | 33% Bachelor’s degree | |
| 20% Graduate degree | 26% Graduate degree | |
| Child race | 88% Caucasian | 85% Caucasian |
| 13% AA | 11% AA | |
| 0% Biracial | 4% Biracial | |
| Child ethnicity | 0% Hispanic/Latino | 11% Hispanic/Latino |
| Father race | 89% Caucasian | 82% Caucasian |
| 11% AA | 11% AA | |
| 8% Biracial | ||
| Father ethnicity | 4% Hispanic/Latino | 4% Hispanic/Latino |
| Marital status | 84% Married/Co-habitating | 84% Married/ Co-habitating |
| 12% Separated/ Divorced | 12% Separated/Divorced | |
| 4% Single | 4% Single | |
| Caretaking responsibility | 41% Primarily Mother | 52% Primarily Mother |
| 7% Primarily Father | 0% Primarily Father | |
| 52% Split evenly | 48% Split evenly | |
| Discipline Responsibility | 44% Primarily Mother | 56% Primarily Mother |
| 11% Primarily Father | 4% Primarily Father | |
| 44% Split evenly | 41% Split evenly | |
| Percent of childrentaking medication for ADHD |
54% | 54% |
| Child Comorbidity | 61% ODD | 78% ODD |
| 4% CD | 7% CD | |
| Mother DBD-I | 2.05 (SD=0.51) | 2.05 (SD=0.45) |
| Mother DBD-H/I | 1.77 (SD=0.53) | 1.71 (SD=0.42) |
| Mother DBD-ODD | 1.58 (SD=0.82) | 1.52 (SD=0.66) |
| Mother IRS – Overall | 5.00 (SD=1.12) | 4.74 (SD=1.10) |
| Father DBD-I | 1.68 (SD=0.45) | 1.80 (SD=0.63) |
| Father DBD-H/I | 1.80 (SD=0.51) | 1.76 (SD=0.55) |
| Father DBD-ODD | 1.48 (SD=0.66) | 1.34 (SD=0.63) |
| Father IRS – Overall | 4.29 (SD=1.41) | 4.78 (SD=1.28) |
| Teacher DBD-I | 1.59 (SD=0.65) | 1.52 (SD=0.89) |
| Teacher DBD-H/I | 1.41 (SD=0.79) | 1.36 (SD=0.91) |
| Teacher DBD-ODD | 0.89 (SD=0.77) | 0.90 (SD=1.00) |
| Teacher IRS – Overall | 3.78 (SD=1.91) | 3.52 (SD=1.90) |
Notes: SD= Standard Deviation. COACHES=Coaching Our ADHD Children: Heightening Essential Skills. AA=African-American. ODD=Oppositional Defiant Disorder. CD=Conduct Disorder. I/O = Inattentive/Overactive factor. O/D = Oppositional defiant factor. DBD-I = Disruptive Behavior Disorders rating scale, Inattentive factor. DBD-H/I = Disruptive Behavior Disorders rating scale, Hyperactive-Impulsive factor. DBD-ODD = Disruptive Behavior Disorders rating scale, Oppositional Defiant Disorder factor. IRS = Impairment Rating Scale.
There were no significant differences between groups on any variables in the table using Chi-square tests for percentages or t-tests for mean scores (p > .05). Some percentages do not sum to 100% due to rounding.
Procedures
Families eligible for the study were randomly assigned to the COACHES program or a waitlist group. To prevent unbalanced groups on the medication status variable, children were block randomized by medication status, to ensure an equal number of medicated and unmedicated children in both groups.
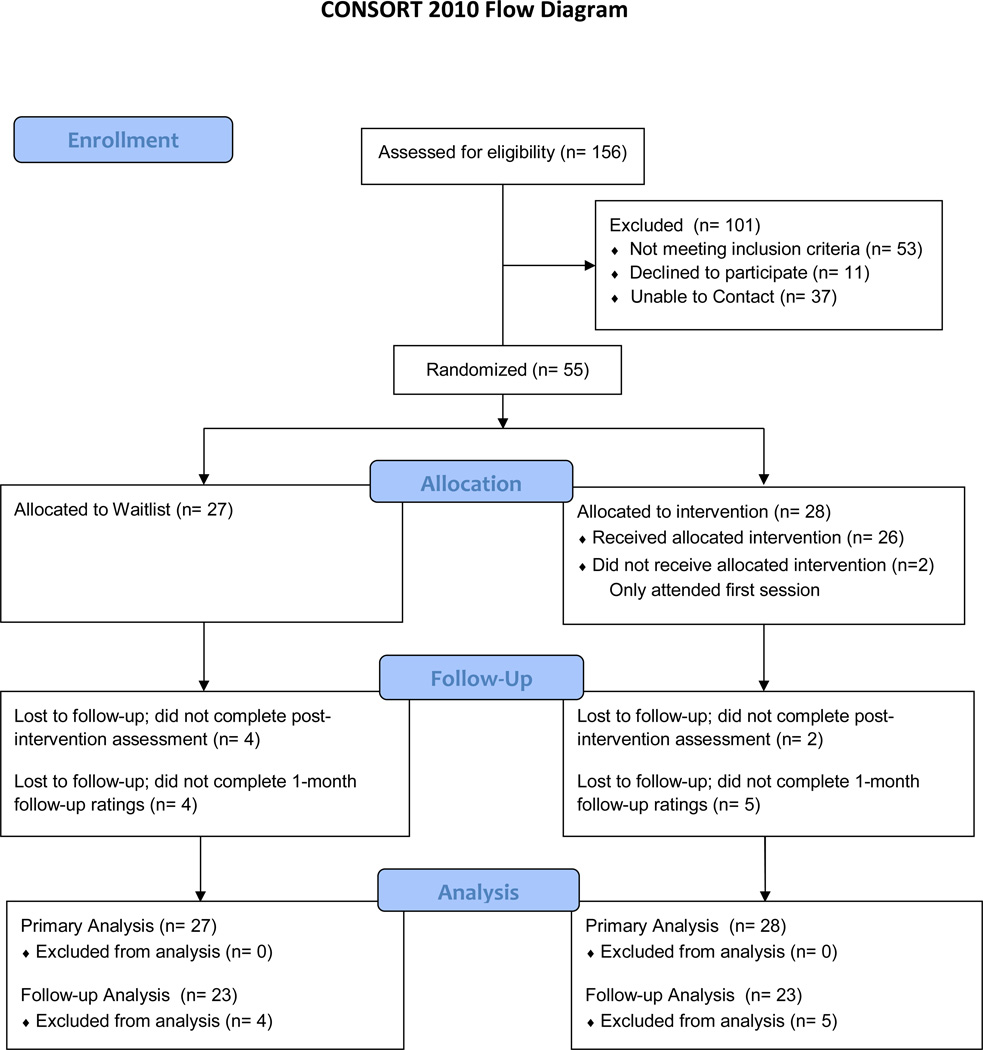
At the end of the 8-week program, mothers and fathers completed ratings and participated in clinic-based observations to measure treatment outcome. One month later, mothers and fathers completed a follow-up rating of functioning. Parents were paid $50.00 for completing ratings at the end of treatment and at follow-up. Figure 1 illustrates the recruitment and allocation plan for the study.
Figure 1.
CONSORT diagram to illustrate study recruitment, screening, random assignment and data analysis.
Study Conditions
COACHES
The COACHES program is an eight-week, two-hour behavioral parent training program. This study includes results from three cohorts of fathers. The COACHES program was inspired by components of two manualized treatment approaches: the Summer Treatment Program (STP; Pelham, Fabiano, Gnagy, Greiner, & Hoza, 2005) and the Community Parent Education Program (COPE; Cunningham, Bremner & Boyle, 1995). The COACHES program integrates program components from these two approaches into an intervention aimed at improving the parenting of fathers of children with ADHD.
During the first hour, fathers learned how to implement effective parenting strategies in a group setting through homework review, viewing videotapes of parenting errors, discussing and identifing the errors, and generating solutions (Cunningham et al., 1993; Cunningham, 1996; Cunningham, Bremner, & Boyle, 1995; Cunningham, Bremner, & Secord, 1998). Further, the group facilitator (a clinical psychologist) modeled the use of the parenting strategy consistent with the COPE manual (see Cunningham et al., 1998). Parent training topics included: (1) Constructing a home-based daily report card and reward system; (2) Attending to positive behavior; (3) Ignoring minor inappropriate behavior; (4) Issuing effective commands; (5) Using “When-Then” contingencies and transitional warnings; (6) Using time out; (7) Problem-solving; and (8) Planning for maintenance. Concurrently, children practiced soccer skill drills with undergraduate counselors using procedures for teaching sport skill competencies combined with a contingency management approach for appropriate behavior (e.g., Pelham et al., 2005).
Then, during the second hour, the parent and child groups joined together for a soccer game. The soccer game provided a context for the fathers to interact with their children and practice the parenting strategies taught in the classroom (e.g., praise, using effective commands), and for clinicians to provide feedback to the fathers. For example, during the week emphasizing attending to positive behavior, a father was asked to issue at least five, labeled praise statements to his child each quarter of the game. Following each quarter, fathers and the group facilitator met to review progress. Fathers were assigned weekly homework assignments to review the week’s material with their partner (if present) and practice the techniques with their child during the week. During week 8, the structure of the second hour was modified to include a father versus child soccer game followed by a trophy presentation.
Waitlist
Fathers assigned to the waitlist group were evaluated eight weeks later and again for a one-month follow-up. Following the one-month follow-up evaluation, families assigned to the waitlist condition enrolled in the COACHES program.
Treatment Integrity
A manual explicitly outlined all procedures to be used in the intervention. All sessions were audiotaped and treatment integrity was assessed by independent review through a checklist review of a sample of audiotapes. A review of 10% of these audiotapes distributed across sessions and cohorts indicated that program content was implemented as prescribed.
Measures
Observational measures and parent ratings were collected from mothers and fathers immediately preceding the COACHES and waitlist group and again eight-weeks later following the last COACHES session. Fathers and mothers additionally completed the Eyberg Child Behavior Inventory (ECBI) one-month later as a measure of maintenance. A post-treatment measure of satisfaction was completed by fathers in the COACHES group.
Eyberg Child Behavior Inventory (ECBI)
Child-based impairment in behavior was assessed using the ECBI (Eyberg & Pincus, 1999). The ECBI is a 36-item rating scale for children between 2- to 16- years that rates the frequency and intensity of common child behavior problems. The ECBI is wellvalidated. For the present study, the ECBI problem and intensity factors (t-scores) were evaluated.
Behavioral observations
Father-child and mother-child interactions were measured using the Dyadic Parent-Child Interaction Coding System II (DPICS-II; Eyberg, Bessmer, Newcomb, Edwards, & Robinson, 1994). The DPICS-II is an observational system used to measure child and parent behavior. The DPICS-II measures the behavior in child-directed, parent-directed, and clean-up interactions. The DPICS-II has demonstrated sensitivity to measuring outcomes for fathers (Schuhmann et al., 1998). Observations were collected in a laboratory room outfitted with a table, chairs, and materials.
For the present study, unblinded observer codes of frequency counts of Total Commands, Total Praise, and Total Negative Talk across the child-directed, parent-directed, and clean-up segments were used. Inter-rater reliability was assessed by blinded observers on 19% of videos distributed across time-points, cohorts, and parents, and the correlations were .92 for Total Commands, .93 for Total Praise, and .81 for Negative Talk.
Therapy Attitude Inventory (TAI)
The TAI (Brestan, Jacobs, Rayfield, & Eyberg, 1999) is a 10-item measure that asks respondents to rate satisfaction with intervention on a scale of 1 (very dissatisfied) to 5 (very satisfied). Factor analytic studies of the TAI in a BPT context yield two factors, a satisfaction with outcome factor and a satisfaction with treatment process factor. It was administered to fathers in the COACHES program at post-treatment.
Results
To investigate primary measures of outcome a Mixed Model analysis (SPSS v. 16) with Maximum Likelihood estimation was used. In these analyses, time was a repeated measure (Pretreatment, Post-treatment) and group was a between subjects fixed factor (COACHES, Waitlist). Child inappropriate behavior was entered as a covariate for observational analyses and the main effect of child inappropriate behavior and the Child behavior×Group×time interaction was entered in all models. Measures with non-normal distributions were transformed to increase normality. Means, standard deviations, F values, p values, and effect size estimates for father-related measures are presented in Table 2. Effect sizes were estimated from the parameter estimates of the group by time interaction (Cohen, 1992). Attrition in the study was modest for primary outcomes, with 93% of fathers assigned to the COACHES program completing post-treatment assessments (82% completed follow-up) compared to 85% of fathers assigned to the waitlist condition (85% completed follow-up).
Table 2.
Descriptive statistics and analysis results for father measures of primary outcome.
| Measure | COACHES Pre- treatment M (SD) |
COACHES Post- treatment M (SD) |
WL Pre- treatment M (SD) |
WL Post- treatment M (SD) |
F (Group × Time interaction) |
p | Effect size |
|---|---|---|---|---|---|---|---|
| DPICS | |||||||
| Total Commands | 26.04 (17.02) | 19.67 (10.13) | 21.05 (12.34) | 16.08 (9.09) | 0.14 | .707 | −.10 |
| Total Praise | 4.58 (4.70) | 6.28 (8.07) | 4.28 (9.3) | 4.16 (9.89) | 4.05 | .047 | .54 |
| Total NT | 5.43 (4.29) | 2.83 (3.26) | 3.01 (3.37) | 3.16 (2.37) | 4.44 | .038 | .57 |
| ECBI | |||||||
| Problem rating | 66.25 (10.41) | 62.08 (8.57) | 65.48 (12.24) | 63.17 (11.21) | .208 | .649 | .12 |
| Intensity rating | 63.96 (9.08) | 56.96 (6.93) | 60.78 (9.80) | 60.65 (9.33) | 4.13 | .045 | .55 |
Notes: COACHES=Coaching Our Acting-Out Children: Heightening Essential Skills. DPICS= Dyadic Parent-Child Interaction System. WL=Waitlist. NT=Negative Talk. M=Mean. SD=Standard Deviation. Means and standard deviations in the table reflect untransformed descriptive statistics. Effect sizes were calculated using the t-statistic from the assessment point by group parameter estimate.
Measures of Primary Outcome
The proximal outcome of this study was parenting behavior as measured by the DPICS-II. Analysis of the DPICS-II results for the Total Praise variable yielded a significant Group×Time interaction, F (1,92) = 4.05, p=.047. Fathers in COACHES increased their use of praise relative to fathers in the waitlist group. The variable of Negative Talk yielded a significant Group×Time interaction, F (1,98) = 4.44, p=.038. Negative Talk was reduced at post-treatment for the COACHES group relative to the waitlist group. The interactions for the Total Commands variable were not significant (p > .05).
On measures of father ratings of child behavior, a distal outcome of the intervention, there was a significant Group×Time interaction for ratings of the intensity of problematic behaviors on the ECBI, F (1,100) = 4.13, p=.045. Direction of means favored families in the COACHES group. At post-treatment, there was no significant difference between groups on ECBI intensity scores less than 60, which indicated no differences in normalization of functioning across groups, Chi-square (1) = .93, p > .05 (62% below 60 for COACHES vs. 48% for the waitlist). Father ratings of the number of problems on the ECBI did not result in a significant group by time interaction (p > .05). Descriptive statistics and effect sizes for all primary outcome measures are listed in Table 2.
Measures of Generalization and Maintenance
Mothers (i.e., other parents) were asked to complete the same assessments as the fathers in the study as a measure of generalization. At baseline and end of treatment assessments, mothers’ parenting behavior was measured by the DPICS. The Group×Time interactions for the Total Commands, Negative Talk, and Total Praise variables were not significant (p > .05). On measures of mother ratings of child behavior, a distal outcome of the intervention, there were no significant differences between groups. Descriptive statistics for mother-related measures are listed in Table 3.
Table 3.
Descriptive statistics and analysis results for mother measures of primary outcome.
| Measure | COACHES Pre- treatment M (SD) |
COACHES Post- treatment M (SD) |
WL Pre- treatment M (SD) |
WL Post- treatment M (SD) |
F (Group × Time interaction) |
p | Effect size |
|---|---|---|---|---|---|---|---|
| DPICS | |||||||
| Total Commands | 23.64 (13.12) | 19.78 (10.70) | 22.37 (12.44) | 21.86 (11.18) | 0.53 | .468 | .20 |
| Total Praise | 4.28 (3.96) | 4.78 (5.90) | 4.37 (4.68) | 3.81 (2.71) | 1.23 | .270 | .31 |
| Total NT | 7.48 (7.38) | 3.26 (3.37) | 4.37 (4.09) | 6.38 (6.07) | 1.69 | .197 | .36 |
| ECBI | |||||||
| Problem rating | 65.16 (9.15) | 59.50 (9.85) | 65.54 (9.17) | 64.40 (9.46) | 1.41 | .238 | .36 |
| Intensity rating | 64.84 (8.83) | 56.75 (8.42) | 63.69 (8.70) | 61.80 (8.92) | 3.11 | .081 | .53 |
Notes: COACHES=Coaching Our Acting-Out Children: Heightening Essential Skills. DPICS= Dyadic Parent-Child Interaction System. WL=Waitlist. NT=Negative Talk. N=25 Mothers in the COACHES group and N=27 Mothers in the waitlist group. Means and standard deviations in the table reflect untransformed descriptive statistics. M=Mean. SD=Standard Deviation. Means and standard deviations in the table reflect untransformed descriptive statistics. Effect sizes were calculated using the t-statistic from the assessment point by group parameter estimate.
To measure the maintenance of treatment effects, the ECBI was re-administered to all COACHES and waitlist families one month later. Independent samples t-tests yielded no significant differences between groups for mothers or fathers (p > .05; See Table 4).
Table 4.
Father and Mother ratings on the Eyberg Child Behavior Inventory Follow-up Rating Scale.
| COACHES (N=23 Fathers and 22 Mothers) |
Waitlist (N=23 Fathers and 20 Mothers) |
|
|---|---|---|
| M (SD) | M (SD) | |
| Father Rating | ||
| ECBI-Problem rating | 59.09 (9.04) | 58.91 (8.84) |
| ECBI-Intensity rating | 62.09 (11.35) | 63.35 (11.61) |
| Mother Rating | ||
| ECBI-Problem rating | 62.05 (9.57) | 64.20 (10.70) |
| ECBI- Intensity rating | 57.50 (9.56) | 63.00 (9.53) |
ECBI=Eyberg Child Behavior Inventory. M=Mean. SD=Standard deviation
Treatment Process
Fathers attended an average of 6.75 COACHES sessions (SD=1.81; Range = 1–8; Median = 7). For sessions attended, fathers were late for 1.18 (SD=1.77; Range = 0–8; Median = 1). Thus, fathers generally attended the majority of sessions and arrived on time for most, variables that demonstrate engagement (e.g., Cunningham et al., 1993). Acceptability was also measured by ratings on the TAI at post-treatment, available for 26 fathers in the COACHES group. The mean score on the satisfaction with outcome factor was 4.04 (SD=.36; Range = 4–5). The mean score on the satisfaction with process factor was 4.01 (SD=.35; Range = 3–4.5). Fathers reported they were “Satisfied” or “Very Satisfied” with outcomes and process (100% and 89%, respectively).
Discussion
The present study reported results of a randomized trial of the COACHES intervention for fathers of children with ADHD. Outcomes suggested the COACHES program resulted in reductions in father verbalizations that were negative or disapproving, increases in praise during a laboratory interaction, and on father ratings of problem behavior intensity. Measures of father-rated behavior problem frequency and observations of the use of commands were unchanged following the eight-week intervention. Intervention effects did not generalize to untreated mothers. Intervention effects appeared to recede once the COACHES program ended. The intervention was rated as acceptable by fathers and it was well-attended. Each of these major results will be discussed in turn.
Fathers in the COACHES group were observed to exhibit fewer negative, disapproving, sarcastic, or critical verbal behaviors toward their children at post-treatment relative to the waitlist group and their pre–test scores. This replicates a finding of another parent training study that demonstrated fathers were less critical following a parent training program using the same laboratory-based measure (Schuhmann et al., 1998). However, when Danforth et al. (2006) used in-home recordings, fathers did not improve on a measure of negative tone at post-treatment. These discrepant findings may be explained by differences in the methods, definitions of the dependent variable, and/or the settings (see Roberts, 2001 for an expanded discussion).
Praise statements issued by fathers increased by 27% in the COACHES group at the post-treatment assessment whereas the waitlist group rate of praise was unchanged (See descriptive statistics in Table 2). If these results are generalizable to the home setting, fathers exhibited two more praise statements per half-hour following the COACHES program. This translates to potentially 18–27 more positive statements per day as it is estimated fathers are available to their child 3–4.5 hours daily on average (Hoffreth, Steuve, Pleck, Bianchi, & Sayer, 2002). Coupled with the reduced rate of negative talk, fathers in the COACHES program appear to be having more positive, and less negative, interactions with their child. This may be a critically important outcome of the study, as positive parenting has been shown to predict longitudinal outcomes for children with ADHD (Chronis, et al., 2007).
Fathers also rated the intensity of child behavior problems as being less severe following the COACHES program, though they continued to indicate the child was exhibiting problematic behaviors (see Schuhmann et al., 1998 for a similar pattern of results on the ECBI for fathers). This pattern of results is perhaps not surprising when one considers ADHD is a chronic condition. It is unlikely an eight-week intervention attended by only one parent will result in large changes in important functional domains. For instance, even the intensive and protracted Multi-modal Treatment Study for ADHD (MTA Cooperative Group, 1999) produced modest outcomes on an important functional domain like peer relationships. Thus, it is encouraging that this short-term study did result in reductions in problem intensity following the active intervention period, but future studies will likely require interventions be implemented for longer periods of time with all family members to promote any maintenance of gains.
Although the positive outcomes are encouraging, it is also remarkable that these gains did not appear to be maintained one month later and there was little evidence that the gains generalized to untreated mothers. There are some speculative explanations for these results. For example, a previous study indicated fathers did not routinely complete assigned homework as part of a behavioral parent training group (Fabiano, Chacko et al., 2009). It may be that while the program is ongoing, fathers implement and attend to behavior modification procedures, but outside of the structured program it is more difficult for them to maintain gains. An alternative explanation is that because mothers were not involved in the intervention, maintenance of gains was harder to obtain within families. This explanation is supported by studies that have suggested the opposite is the case; there is a lack of maintenance for mothers when fathers were not involved in intervention (Bagner & Eyberg, 2003; Webster-Stratton, 1980).
The acceptability of the COACHES intervention was assessed in this project. A previous study indicated that fathers were more engaged in intervention activities, parents and children attended more regularly, and the fathers rated the intervention process as more acceptable relative to a classroom-based parenting program (Fabiano, Chacko et al., 2009). The present COACHES intervention, which included the coping-modeling-problem-solving approach pioneered in the COPE program (and previously found to be acceptable and engaging; Cunningham et al., 1993) coupled with the recreational sports activities as a forum for practicing parenting strategies (e.g., Pelham et al., 2005) was also rated as well-liked and as resulting in improvement in this study.
The small sample size (the study was powered to detect at least moderate effect sizes, not small effects), short duration of intervention, lack of information on comorbid internalizing or learning problems, and relative homogeneity of demographics are limitations of the current report. Approximately half the children in the study were taking medication for ADHD, which may further limit the generalizability of these results. The results related to maintenance are limited in that we did not collect follow-up observations of parenting. An additional limitation is related to the somewhat contrived nature of the clinical situation. It would be unlikely the majority of enrollees in a behavioral parent training program would be solely fathers. Therefore, although studies such as this are important to isolate outcomes for fathers in behavioral parent training, the next generation of studies are needed to determine the best approach for integrating father-specific interventions into a comprehensive treatment approach (see also Phares, Fields, & Binitie, 2006).
Future Directions
The goal of this study was to investigate the efficacy of COACHES. Future studies now need to determine the best manner of applying these procedures into routine family-based interventions. For example, the COACHES program may be useful as a maintenance program following a course of BPT or other intervention to maintain engagement given potential concerns about attrition and long-term treatment compliance (Eyberg, Edwards, Boggs, & Foote, 1998; Marcus, Wan, Kemner, & Olfson, 2005), as an adjunctive intervention when a father’s parenting is impaired, or as part of a multi-modal intervention. The COACHES program, may also be studied with mothers or co-parents. These avenues may help realize the ideal of consistent and complimentary parenting between mothers and fathers of children with ADHD.
Acknowledgments
This project was funded by a grant from the National Institute of Mental Health 1R34MH078051. Dr. Pelham is now at Florida International University. We would like to express our gratitude to the parents, children, and staff who worked together in this program.
Footnotes
There were medication changes during the eight week trial. Three participants in the COACHES group changed medication during the trial (one discontinued all medication, one began Concerta 36 mg, and one began Daytrana 15 mg/9hr). In the waitlist condition, one participant modified medication from 5 mg of Adderall b.i.d to 20 mg of Adderall XR, one increased the dose of Adderall from 5 mg to 10 mg, one began taking methylphenidate 5 mg b.i.d., and one discontinued Risperdal but continued concurrent stimulant medication. There were no significant differences between groups in medication changes.
Contributor Information
Gregory A. Fabiano, University at Buffalo, State University of New York
William E. Pelham, University at Buffalo, State University of New York
Charles E. Cunningham, McMaster University
Jihnhee Yu, University at Buffalo, State University of New York.
Brian Gangloff, University at Buffalo, State University of New York.
Melina Buck, University at Buffalo, State University of New York.
Stuart Linke, University at Buffalo, State University of New York.
Matthew Gormley, University at Buffalo, State University of New York.
Shradha Gera, University at Buffalo, State University of New York.
References
- Amato PR, Rivera F. Paternal involvement and children’s behavior problems. Journal of Marriage and the Family. 1999;61:375–384. [Google Scholar]
- Bagner DM, Eyberg SM. Father involvement in parent training: When does it matter? Journal of Clinical Child and Adolescent Psychology. 2003;32:599–605. doi: 10.1207/S15374424JCCP3204_13. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Edwards G, Laneri M, Fletcher K, Metevia L. The efficacy of problem-solving communication training alone, behavior management training alone, and their combination for parent-adolescent conflict in teenagers with ADHD and ODD. Journal of Consulting and Clinical Psychology. 2001;69:926–941. [PubMed] [Google Scholar]
- Brestan EV, Jacobs JR, Rayfield AD, Eyberg SM. A consumer satisfaction measure for parent-child treatments and its relation to measures of child behavior change. Behavior Therapy. 1999;30:17–30. [Google Scholar]
- Cassano M, Adrian M, Veits G, Zeman J. The inclusion of fathers in the empirical investigation of child psychopathology: An update. Journal of Clinical Child and Adolescent Psychology. 2006;35:583–589. doi: 10.1207/s15374424jccp3504_10. [DOI] [PubMed] [Google Scholar]
- Chronis AM, Chacko A, Fabiano GA, Wymbs BT, Pelham WE. Enhancements to the behavioral parent training paradigm for families of children with ADHD: Review and future directions. Clinical Child and Family Psychology Review. 2004;7:1–27. doi: 10.1023/b:ccfp.0000020190.60808.a4. [DOI] [PubMed] [Google Scholar]
- Chronis AM, Lahey BB, Pelham WE, Williams SH, Baumann BB, Kipp H, Rathouz PJ. Maternal depression and early positive parenting predict future conduct problems in young children with attention-deficit/hyperactivity disorder. Developmental Psychology. 2007;43:70–82. doi: 10.1037/0012-1649.43.1.70. [DOI] [PubMed] [Google Scholar]
- Cohen J. A power primer. Psychological Bulletin. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Cunningham CE. Improving availability, utilization, and cost efficacy of parent training programs for children with disruptive behavior disorders. In: Peters RD, McMahon RJ, editors. Preventing Childhood Disorders, Substance, Abuse, and Delinquency. Thousand Oaks, CA: Sage Publications; 1996. pp. 144–160. [Google Scholar]
- Cunningham CE, Bremner R, Boyle M. Large group community parenting programs for families of preschoolers at risk for disruptive behaviour disorders: Utilization, cost effectiveness, and outcome. Journal of Consulting and Clinical Psychology. 1995;36:1141–1159. doi: 10.1111/j.1469-7610.1995.tb01362.x. [DOI] [PubMed] [Google Scholar]
- Cunningham CE, Bremner R, Secord M. The Community Parent Education Program: A School-Based Family Systems Oriented Workshop for Parents of Children with Disruptive Behavior Disorders. 1998. Unpublished Treatment Manual. [Google Scholar]
- Cunningham CE, Davis JR, Bremner R, Dunn KW, Rzasa T. Coping modeling problem solving versus mastery modeling: Effects on adherence, in-session process, and skill acquisition in a residential parent-training program. Journal of Consulting and Clinical Psychology. 1993;61:871–877. doi: 10.1037//0022-006x.61.5.871. [DOI] [PubMed] [Google Scholar]
- Danforth JS, Harvey E, Ulaszek WR, McKee TE. The outcome of group parent training for families of children with attention-deficit/hyperactivity disorder and defiant/aggressive behavior. Journal of Behavior Therapy and Experimental Psychiatry. 2006;37:188–205. doi: 10.1016/j.jbtep.2005.05.009. [DOI] [PubMed] [Google Scholar]
- Eyberg SM, Pincus D. Eyberg Child Behavior Inventory and Sutter-Eyberg Student Behavior Inventory-Revised Professional Manual. Lutz, FL: Psychological Assessment Resources, Inc.; 1999. [Google Scholar]
- Eyberg SM, Bessmer JL, Newcomb K, Edwards DL, Robinson EA. Dyadic Parent-Child Interaction Coding System-II: A Manual. San Rafael, CA: Select Press; 1994. [Google Scholar]
- Eyberg SM, Edwards D, Boggs S, Foote R. Maintaining the treatment effects of parent training: The role of booster sessions and other maintenance strategies. Clinical Psychology: Science and Practice. 1998;5:544–554. [Google Scholar]
- Fabiano GA. Father participation in behavioral parent training for ADHD: Review and recommendations for increasing inclusion and engagement. Journal of Family Psychology. 2007;21:683–693. doi: 10.1037/0893-3200.21.4.683. [DOI] [PubMed] [Google Scholar]
- Fabiano GA, Chacko A, Pelham WE, Robb JA, Walker KS, Wienke AL, Schulman S. A comparison of behavioral parent training programs for fathers of children with attention-deficit/hyperactivity disorder. Behavior Therapy. 2009;40:190–204. doi: 10.1016/j.beth.2008.05.002. [DOI] [PubMed] [Google Scholar]
- Fabiano GA, Pelham WE, Coles EK, Gnagy EM, Chronis AM, O’Connor BC. A meta-analysis of behavioral treatments for attention-deficit/hyperactivity disorder. Clinical Psychology Review. 2009;29:129–140. doi: 10.1016/j.cpr.2008.11.001. [DOI] [PubMed] [Google Scholar]
- Fabiano GA, Pelham WE, Waschbusch DA, Gnagy EM, Lahey BB, Chronis AM, Burrows-MacLean L. A practical measure of impairment for children with ADHD: Psychometric properties in samples of children with ADHD and two school samples. Journal of Clinical Child and Adolescent Psychology. 2006;35:369–385. doi: 10.1207/s15374424jccp3503_3. [DOI] [PubMed] [Google Scholar]
- Firestone P, Kelley MJ, Fike S. Are fathers necessary in parent training groups? Journal of Clinical Child Psychology. 1980:44–47. [Google Scholar]
- Forehand R, Long N, Brody GH, Fauber R. Home predictors of young adolescents’ school behavior and academic performance. Child Development. 1986;57:1528–1533. doi: 10.1111/j.1467-8624.1986.tb00477.x. [DOI] [PubMed] [Google Scholar]
- Hoffreth SL, Steuve JL, Pleck J, Bianchi S, Sayer L. The demography of fathers: What fathers do. In: Tamis-LeMonda CS, Cabrera N, editors. Handbook of Father Involvement: Multidisciplinary Perspectives. Mahwah, NJ: Lawrence Erlbaum & Associates, Publishers; 2002. pp. 63–90. [Google Scholar]
- Lundahl B, Risser HJ, Lovejoy MC. A meta-analysis of parent training: Moderators and follow-up effects. Clinical Psychology Review. 2006;26:86–104. doi: 10.1016/j.cpr.2005.07.004. [DOI] [PubMed] [Google Scholar]
- Marcus SC, Wan GJ, Kemner JE, Olfson M. Continuity of methylphenidate treatment for attention-deficit/hyperactivity disorder. Archives of Pediatric and Adolescent Medicine. 2005;159:572–578. doi: 10.1001/archpedi.159.6.572. [DOI] [PubMed] [Google Scholar]
- Martin B. Brief family intervention: Effectiveness and the importance of including the father. Journal of Consulting and Clinical Psychology. 1977;45:1002–1010. doi: 10.1037//0022-006x.45.6.1002. [DOI] [PubMed] [Google Scholar]
- MTA Cooperative Group. 14-Month Randomized Clinical Trial of Treatment Strategies for Attention Deficit Hyperactivity Disorder. Archives of General Psychiatry. 1999;56:1073–1086. doi: 10.1001/archpsyc.56.12.1073. [DOI] [PubMed] [Google Scholar]
- Parke RD, McDowell DJ, Kim M, Killian C, Dennis J, Wild MN. Fathers’ contributions to children’s peer relationships. In: Tamis-LeMonda CS, Carbrera N, editors. Handbook of Father Involvement: Interdisciplinary Perspectives. Mahwah, NJ: Lawrence Erlbaum, Publishers; 2002. pp. 141–167. [Google Scholar]
- Pelham WE, Fabiano GA. Evidence-based psychosocial treatment for attention-deficit/hyperactivity disorder: An update. Journal of Clinical Child and Adolescent Psychology. 2008;37:184–214. doi: 10.1080/15374410701818681. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Fabiano GA, Gnagy EM, Greiner AR, Hoza B. Comprehensive psychosocial treatment for ADHD. In: Hibbs E, Jensen P, editors. Psychosocial Treatments for Child and Adolescent Disorders: Empirically Based Strategies for Clinical Practice. Second Edition. Washington, DC: American Psychological Association; 2005. pp. 377–409. [Google Scholar]
- Pelham WE, Gnagy EM, Greenslade KE, Milich R. Teacher ratings of DSM-III-R symptoms of the disruptive behavior disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31:210–218. doi: 10.1097/00004583-199203000-00006. [DOI] [PubMed] [Google Scholar]
- Phares V. Fathers and Developmental Psychopathology. New York: John Wiley and Sons, Inc.; 1996. [Google Scholar]
- Phares V, Fields S, Binitie I. Getting fathers involved in child-related therapy. Cognitive and Behavioral Practice. 2006;13:42–52. [Google Scholar]
- Roberts MW. Clinic observations of structured parent-child interaction designed to evaluate externalizing disorders. Psychological Assessment. 2001;13:46–58. [PubMed] [Google Scholar]
- Russell G, Russell A. Mother-child and father-child relationships in middle childhood. Child Development. 1987;58:1573–1585. [Google Scholar]
- Schuhmann EM, Foote RC, Eyberg SM, Boggs SR, Algina J. Efficacy of parent-child interaction therapy: Interim report of a randomized trial with short-term maintenance. Journal of Clinical Child Psychology. 1998;27:34–45. doi: 10.1207/s15374424jccp2701_4. [DOI] [PubMed] [Google Scholar]
- Tiano JD, McNeil CB. The inclusion of fathers in behavioral parent training: A critical evaluation. Child and Family Behavior Therapy. 2005;27:1–28. [Google Scholar]
- Webster-Stratton C. The effects of father involvement in parent training for conduct problem children. Journal of Child Psychology and Psychiatry. 1980;26:801–810. doi: 10.1111/j.1469-7610.1985.tb00593.x. [DOI] [PubMed] [Google Scholar]
- Webster-Stratton C, Reid MJ, Hammond M. Treating children with early-onset conduct problems: Intervention outcomes for parent, child, and teacher training. Journal of Clinical Child and Adolescent Psychology. 2004;33:105–124. doi: 10.1207/S15374424JCCP3301_11. [DOI] [PubMed] [Google Scholar]