Abstract
Dengue fever (DF) is endemic in tropical and subtropical zones and the prevalence is increasing across South-east Asia, Africa, the Western Pacific and the Americas. In recent years, the spread of unplanned urbanisation, with associated substandard housing, overcrowding and deterioration in water, sewage and waste management systems, has created ideal conditions for increased transmission of the dengue virus in tropical urban centres. While dengue infection has traditionally been considered a paediatric disease, the age distribution of dengue has been rising and more cases have been observed in adolescents and adults. Furthermore, the development of tourism in the tropics has led to an increase in the number of tourists who become infected, most of whom are adults. Symptoms and risk factors for dengue haemorrhagic fever (DHF) and severe dengue differ between children and adults, with co-morbidities and incidence in more elderly patients associated with greater risk of mortality. Treatment options for DF and DHF in adults, as for children, centre round fluid replacement (either orally or intravenously, depending on severity) and antipyretics. Further data are needed on the optimal treatment of adult patients.
Keywords: Dengue, Adults, Adolescents, DHF, Dengue haemorrhagic fever, Age
Background
In hyperendemic areas in Asia, dengue fever (DF) and dengue haemorrhagic fever (DHF) affect mainly children under 15 years of age.1 The age distribution is different in the Americas where these syndromes occur in all age groups, although the majority of fatalities during epidemics occur in children.2 This article discusses the impact of dengue in adolescents and adults.
Dengue in Different Age Groups
Data from several South-east Asian countries have shown that the average/mean age of reported dengue cases has increased from 5–9 years to older children and adults.3–7 In Thailand, affected adults over 15 years of age comprise 30–40% of dengue cases. At present, the morbidity rate of DHF is declining in Thailand, while the average age of patients with dengue infection is increasing.8,9 Dengue infection in adolescents and adults is also a potential hazard in international travellers returning from endemic areas, especially South-east Asia,10–13 a topic covered in more detail in the Wilder-Smith article ‘Dengue infections in travellers’ in this supplement.14
Dengue virus infection produces a spectrum of clinical illness ranging through undifferentiated fever, DF and self-limiting febrile illness associated with headache, myalgia and thrombocytopenia. DHF and dengue shock syndrome (DSS) are more serious and can be fatal.15,16 The classification of dengue fever severity is explored in the Hadinegoro article ‘The revised WHO dengue case classification: does the new system need to be modified?’, also in this supplement.17
Several factors may influence disease severity, including host factors, virus serotype or genotype, sequence of virus infection, differences in dengue cross-reactive antibody, and T-cell responses.18 DF is usually self-limiting, and death is uncommon. However, age-related differences in dengue severity are poorly understood and data on clinical features in adult patients are limited.3–5 Older age has previously been reported to be a risk factor for mortality in patients with DF or DHF as the co-morbidities associated with ageing and waning immunity pose a substantial risk for fatality in elderly patients with active infection.19,20 Although shock and plasma leakage seem to be more prevalent in younger patients, the frequency of internal haemorrhage augments as age increases.21 Furthermore, complications of dengue infection observed in adults, including DF with unusual bleeding and DHF, have been increasing.22–24
Clinical Manifestations
The clinical characteristics in 140 adults infected with dengue virus during the Bangkok dengue epidemic in 1997–1998 are summarised in Table 1.
Table 1. The clinical manifestations of DF in 140 adults during the Bangkok epidemic in 1997–1998.
| DF/DHF | DF | DHF | |
| n = 140 | n = 89 | n = 51 | |
| Age, y, mean, [range] | 26·9 [15–67] | 28·6 [15–67] | 23·4 [15–44] |
| Total duration of fever, d, mean, [range] | 5·2 [2–8] | 5·2 [2–8] | 5·2 [3–8] |
| Fever, % | 100 | 100 | 100 |
| Nausea/vomiting, % | 47·1 | 40·4 | 58·8 |
| Headache, % | 37·8 | 38·2 | 37·3 |
| Diarrhoea, % | 25·0 | 33·3 | 21·2 |
| Myalgia, % | 25·7 | 25·8 | 25·6 |
| Abdominal pain, % | 23·6 | 12·3 | 43·1 |
| Haemorrhagic manifestations, % | 35·7 | 24·7 | 54·9 |
| Petechiae | 22·1 | 14·6 | 35·2 |
| Epistaxis | 7·8 | 4·4 | 14·3 |
| Gum bleeding | 7·1 | 5·5 | 10·2 |
| Haematemesis | 2·1 | 0 | 5·9 |
| Vaginal bleeding | 24·6 | 21 | 31·6 |
| Bleeding >2 sites | 27 | 6·7 | 19·6 |
| Rash (occurring in convalescence), % | 27·8 (5) | 31·5 | 21·6 |
| Hypotension/pulse pressure <20 mmHg, % | 2·1 | 0 | 5·8 |
| Jaundice, % | 0·7 | 0 | 1·9 |
| Epigastric or RUQ tenderness, % | 18·6 | 10·1 | 29·4 |
| Hepatomegaly, % | 21·4 | 11·2 | 39·2 |
| Splenomegaly (by ultrasonography), % | 2·1 | 0 | 5·9 |
| Ascites (by ultrasonography), % | 3·6 | 0 | 9·8 |
| Pleural effusion (by chest radiograph), % | 10·7 | 0 | 29·4 |
RUQ, right upper quadrant
Manifestations of Dengue Fever
During the acute febrile phase of DF, usually lasting 3–8 days, many of the clinical symptoms resemble those of DHF, including fever, nausea/vomiting, headache, rash and myalgia; abdominal pain and severe or widespread bleeding are less frequent in DF.25 Minor haemorrhagic manifestations such as petechiae, epistaxis and gingival bleeding do sometimes occur in DF, although they are rarely associated with severe haemorrhage leading to shock.26
Manifestations of Dengue Haemorrhagic Fever
Owing to differences in capillary permeability, adults may be at lower risk than children of developing DHF.27 DHF can be distinguished from DF by the presence of increased vascular permeability (plasma leakage syndrome) and marked thrombocytopenia (<100,000/μl) associated with bleeding, hepatomegaly and/or abnormal liver function. Acute respiratory failure, although a rare complication in adults, has a high mortality rate.28 Although children are more likely to develop hypovolaemic shock characterised by increased microvascular permeability in DHF, a high mortality rate has been observed in adult patients.29 The outcome of DHF and DSS depends largely on early diagnosis and the immediate replacement of fluid.
Haemorrhage contributes to dengue morbidity and mortality, especially during the severe thrombocytopenia and toxic haemorrhagic stage (3–5 days after illness onset).30 In Thailand, bleeding manifestations including petechiae, epistaxis and menorrhagia have been observed frequently in adults with DF or DHF (own data, Table 1), although upper gastro-intestinal (GI) bleeding is the most common type of severe haemorrhage.30 In reports of endoscopic examination of dengue patients with upper GI tract bleeding, haemorrhagic gastritis was the most common finding (40·9–58·5%).31–33 However, massive haematemesis may occur in adults with DF or DHF owing to peptic ulcers, which is not associated with profound shock, as in previous reports in children.33 In patients with pre-existing peptic ulcers, severe or even fatal bleeding can be precipitated by dengue infection, though in most cases supportive therapy and blood transfusions are adequate to manage this complication.33 Subcapsular splenic bleeding and rupture have also been reported in adults with dengue infection.34,35 However, splenic rupture in patients with haemorrhagic dengue is uncommon and can happen spontaneously or as a result of trauma, which may be minor or unnoticed.34,35
Menorrhagia is common in female adults with DF/DHF (up to 25%).7 Uterine haemorrhage resulting in spontaneous abortion, premature labour and severe postpartum bleeding has been observed in women with DF/DHF.36–38 In patients with dengue during onset of labour, blood or platelet transfusion may be required in cases with severe bleeding or where caesarean section is required.38,39
Increased liver enzymes [alanine aminotransferase (ALT) and aspartate aminotransferase (AST)] have been found in children and adults during dengue infection, indicating liver involvement.40–42 Unlike conventional viral hepatitis, AST level is higher than ALT in dengue infection,41 with levels increasing to a maximum 7–9 days after onset of symptoms, decreasing to normal within 2 weeks.41 Pre-existing liver disease such as chronic hepatitis and haemoglobinopathies are more likely to be present in adults than in children with dengue and may aggravate the liver impairment.19,43 Liver injury is often self-limiting, but fulminant hepatitis and death have been reported.42,44 The association between severe liver disease and encephalopathy is well described in children and adults with DF/DHF, and high mortality has been reported in dengue patients with hepatitis and encephalopathy.45
More unusual manifestations of dengue infection in adults include severe internal haemorrhage, cardiomyopathy, cardiac arrhythmias, adult respiratory distress syndrome (ARDS), rhabdomyolysis, pancreatitis, appendicitis, co-infection with other tropical diseases, and neurological phenomena such as altered consciousness, seizures and coma owing to encephalitis and encephalopathy.46–53 Neurological manifestations secondary to dengue infection were ascribed to non-specific complications such as myelitis, optic neuritis, polyradiculopathy or neuropathy.54,55 Possible causes of dengue encephalopathy include hypotension, cerebral oedema, focal haemorrhage, hyponatraemia and fulminant hepatic failure.51,55,56 However, a recently documented possibility is dengue invasion of the nervous system.57,58 Furthermore, some studies have indicated that 5·5% of patients with DHF have dual infections such as urinary tract infection, diarrhoea or bacteraemia.19 Failure to correctly diagnose any concurrent infection in patients with DHF may lead to greater morbidity or mortality, which would otherwise be preventable. Prolonged fever and acute renal failure are independent predictive factors for dual infection.19
Treatment of Dengue Infection in Adults
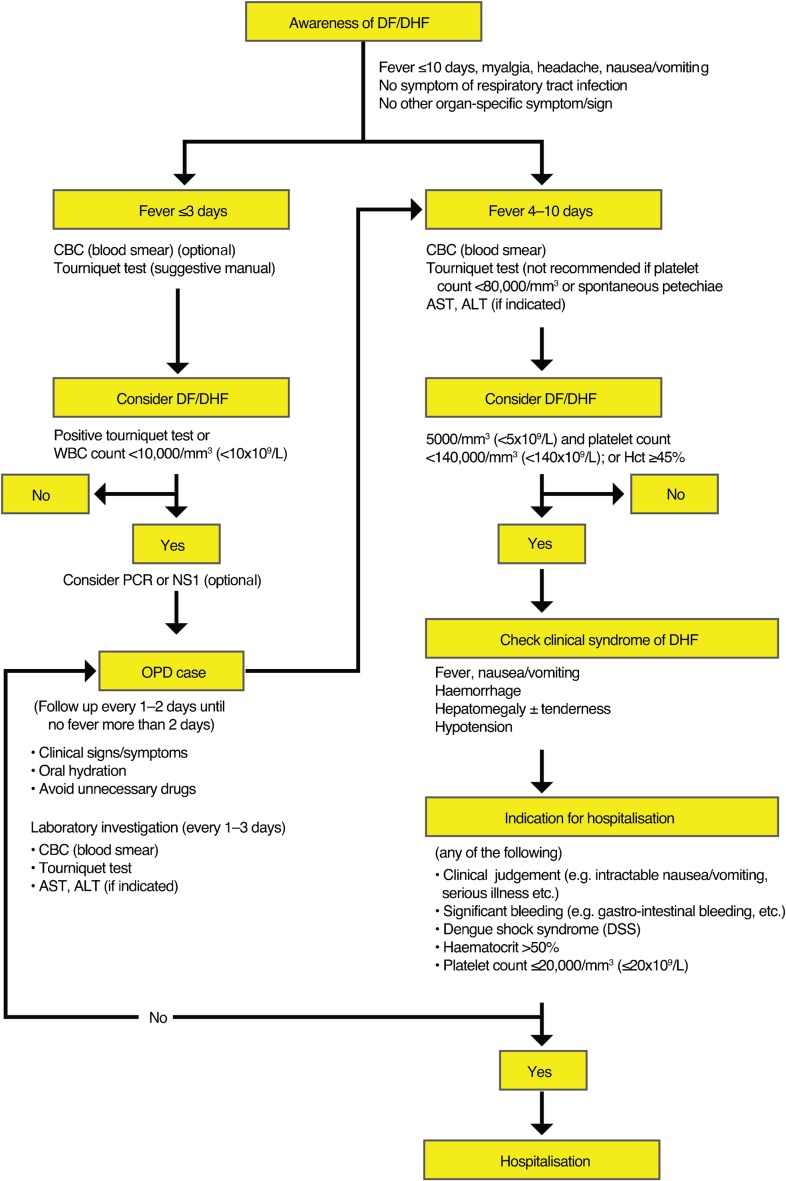
Currently, there are no specific therapeutic agents for dengue. In adults, early recognition of dengue infection, bleeding and signs of circulatory collapse reduces mortality with dengue (Figs 1 and 2).
Figure 1.
Management of adult dengue in Thailand (clinical practice guidelines by the Infectious Diseases Society of Thailand, 2006)
Figure 2.
Management of adult dengue in Thailand, continued (clinical practice guidelines by the Infectious Diseases Society of Thailand, 2006)
Mild dengue infection may be treated with oral hydration and antipyretics.59 Agents such as salicylates, non-steroidal anti-inflammatory drugs and traditional medicines that may have hepatotoxic effects must be avoided.16 Attentive clinical monitoring of patients with suspected DHF, along with anticipatory and supportive care, are life-saving and reduce fatality rates. To identify the need for intravenous fluid therapy, circulation and vascular leakage must be monitored by serial clinical assessments of pulse, blood pressure, skin perfusion, urine output and haematocrit.16 Patients with DHF need to be monitored closely for signs of shock for at least 24 hours after defervescence.29 Prompt fluid resuscitation remains the mainstay of treatment to counteract massive plasma leakage. In most adult cases, timely and effective intravenous crystalloid replacement of plasma losses results in a favourable outcome. If shock persists, immediate volume replacement with Ringer’s lactate, Ringer’s acetate or physiological saline should be followed by plasma or colloid solutions.60 Recently, three randomised controlled trials evaluated therapeutic responses to colloid and crystalloid solutions.61–63 Results indicate that Ringer’s lactate performed least well.61–63 Patients with a narrow pulse pressure (⩽10 mmHg), indicating more severe DSS, should benefit from initial resuscitation with colloid solution rather than crystalloid solution.61–63 Preventive transfusions may be harmful and should be avoided, and invasive procedures should be minimised to avoid haemorrhagic complications.
Conclusion
Dengue infection is generally considered to be a paediatric disease but is currently a growing problem in adults throughout the tropics. Furthermore, dengue infection can be more severe in adults in whom early recognition of dengue infection, bleeding tendencies and signs of circulatory collapse would reduce mortality. Fluid replacement is the gold-standard therapeutic option for adults with dengue fever, as it is for children. However, further studies in adults are required to establish the best therapeutic approaches and determine whether any specific factors should be considered in terms of warning signs and risk factors.
Acknowledgments
Editorial support was provided by Eleanor Steele of Interlace Global and funded by Sanofi Pasteur.
References
- 1.Gubler DJ. Epidemic dengue/dengue hemorrhagic fever as a public health, social and economic problem in the 21st century. Trends Microbiol. 2002;10:100–3. doi: 10.1016/s0966-842x(01)02288-0. [DOI] [PubMed] [Google Scholar]
- 2.Guzman MG, Kouri G. Dengue and dengue hemorrhagic fever in the Americas: lessons and challenges. J Clin Virol. 2003;27:1–13. doi: 10.1016/s1386-6532(03)00010-6. [DOI] [PubMed] [Google Scholar]
- 3.Chareonsook O, Foy HM, Teeraratkul A, Silarug N. Changing epidemiology of dengue hemorrhagic fever in Thailand. Epidemiol Infect. 1999;122:161–6. doi: 10.1017/s0950268898001617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pongsumpun P, Yoksan S, Tan IM. A comparison of the age distributions in the dengue hemorrhagic fever epidemics in Santiago de Cuba (1997) and Thailand (1998). Southeast Asian J Trop Med Public Health. 2002;33:255–8. [PubMed] [Google Scholar]
- 5.Kularatne SA, Gawarammana IB, Kumarasiri PR. Epidemiology, clinical features, laboratory investigations and early diagnosis of dengue fever in adults: a descriptive study in Sri Lanka. Southeast Asian J Trop Med Public Health. 2005;36:686–92. [PubMed] [Google Scholar]
- 6.Annual Epidemiological Surveillance Report: Thailand [cited February 2012]Available from: http://epid.moph.go.th [Google Scholar]
- 7.Tantawichien T, Thisyakorn U, Pisarnpong A, Israsena S, Suwangool P. Dengue fever and dengue hemorrhagic fever in adults. The First International Conference on Dengue and Dengue Hemorrhagic fever, Chiang Mai, Thailand, 20–24 November 2000. Abstract pp 16–17 [unpublished data] [Google Scholar]
- 8.Patumanond J, Tawichasri C, Nopparat S. Dengue hemorrhagic fever, Uttaradit, Thailand. Emerg Infect Dis. 2003;9:1348–50. doi: 10.3201/eid0910.020681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Simmons M, Burgess T, Lynch J, Putnak R. Protection against dengue virus by non-replicating and live attenuated vaccines used together in a prime boost vaccination strategy. Virology. 2010;396:280–8. doi: 10.1016/j.virol.2009.10.023. [DOI] [PubMed] [Google Scholar]
- 10.Jelinek T. Dengue fever in international travelers. Clin Infect Dis. 2000;31:144–7. doi: 10.1086/313889. [DOI] [PubMed] [Google Scholar]
- 11.O'Brien D, Tobin S, Brown GV, Torresi J. Fever in returned travelers: review of hospital admissions for a 3-year period. Clin Infect Dis. 2001;33:603–9. doi: 10.1086/322602. [DOI] [PubMed] [Google Scholar]
- 12.Pongsumpun P, Patanarapelert K, Sriprom M, Varamit S, Tang IM. Infection risk to travelers going to dengue fever endemic regions. Southeast Asian J Trop Med Public Health. 2004;35:155–9. [PubMed] [Google Scholar]
- 13.Stephan C, Allwinn R, Brodt HR, Knupp B, Preiser W, Just-Nubling G. Travel-acquired dengue infection: clinical spectrum and diagnostic aspects. Infection. 2002;30:225–8. doi: 10.1007/s15010-002-3052-7. [DOI] [PubMed] [Google Scholar]
- 14.Wilder-Smith A. Dengue infections in travellers. Paediatr Int Child Health. 2012;32:28–32. doi: 10.1179/2046904712Z.00000000050. (suppl. 1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pancharoen C, Kulwichit W, Tantawichien T, Thisyakorn U, Thisyakorn C. Dengue infection: a global concern. J Med Assoc Thai. 2002;85((suppl 1)):S25–33. [PubMed] [Google Scholar]
- 16.World Health Organization. Geneva, Switzerland: WHO; 2009. Dengue: Guidelines for Diagnosis, Treatment, Prevention and Control. [PubMed] [Google Scholar]
- 17.Hadinegoro SR.The revised WHO dengue case classification: does the system need to be modified? Paediatr Int Child Health. 201232(suppl. 1)33–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Green S, Rothman A. Immunopathological mechanisms in dengue and dengue hemorrhagic fever. Curr Opin Infect Dis. 2006;19:429–36. doi: 10.1097/01.qco.0000244047.31135.fa. [DOI] [PubMed] [Google Scholar]
- 19.Lee IK, Liu JW, Yang KD. Clinical characteristics and risk factors for concurrent bacteremia in adults with dengue hemorrhagic fever. Am J Trop Med Hyg. 2005;72:221–6. [PubMed] [Google Scholar]
- 20.Rigau-Perez JG, Laufer MK. Dengue-related deaths in Puerto Rico, 1992–1996: diagnosis and clinical alarm signals. Clin Infect Dis. 2006;42:1241–6. doi: 10.1086/501355. [DOI] [PubMed] [Google Scholar]
- 21.Hammond SN, Balmaseda A, Perez L, Tellez Y, Saborio SI, Mercado JC, et al. Differences in dengue severity in infants, children, and adults in a 3-year hospital-based study in Nicaragua. Am J Trop Med Hyg. 2005;73:1063–70. [PubMed] [Google Scholar]
- 22.Agarwal R, Kapoor S, Nagar R, Misra A, Tandon R, Mathur A, et al. A clinical study of the patients with dengue hemorrhagic fever during the epidemic of 1996 at Lucknow, India. Southeast Asian J Trop Med Public Health. 1999;30:735–40. [PubMed] [Google Scholar]
- 23.Anuradha S, Singh NP, Rizvi SN, Agarwal SK, Gur R, Mathur MD. The 1996 outbreak of dengue hemorrhagic fever in Delhi, India. Southeast Asian J Trop Med Public Health. 1998;29:503–6. [PubMed] [Google Scholar]
- 24.Rongrungruang Y, Leelarasamee A. Characteristics and outcomes of adult patients with symptomatic dengue virus infections. J Infect Dis Antimicrob Agents. 2001;18:19–23. [Google Scholar]
- 25.Lee VJ, Lye DC, Sun Y, Fernandez G, Ong A, Leo YS. Predictive value of simple clinical and laboratory variables for dengue hemorrhagic fever in adults. J Clin Virol. 2008;42:34–9. doi: 10.1016/j.jcv.2007.12.017. [DOI] [PubMed] [Google Scholar]
- 26.Seet RCS, Ooi E, Wong HB, Paton NI. An outbreak of primary dengue infection among migrant Chinese workers in Singapore characterized by prominent gastrointestinal symptoms and a high proportion of symptomatic cases. J Clin Virol. 2005;33:336–40. doi: 10.1016/j.jcv.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 27.Wichmann O, Hongsiriwon S, C B, Chotivanich K, Sukthana Y, Pukrittayakamee S. Risk factors and clinical features associated with severe dengue infection in adults and children during the 2001 epidemic in Chonburi, Thailand. Trop Med Int Health. 2004;9:1022–9. doi: 10.1111/j.1365-3156.2004.01295.x. [DOI] [PubMed] [Google Scholar]
- 28.Wang CC, Liu SF, Liao SC, Lee IK, Liu JW, Lin AS, et al. Acute respiratory failure in adult patients with dengue virus infection. Am J Trop Med Hyg. 2007;77:151–8. [PubMed] [Google Scholar]
- 29.Thomas L, Moravie V, Besnier F, Valentino R, Kaidomar S, Coquet LV, et al. Clinical presentation of dengue among patients admitted to the adult emergency department of a tertiary care hospital in Martinique: implications for triage, management, and reporting. Ann Emerg Med. 2012;59:42–50. doi: 10.1016/j.annemergmed.2011.08.010. [DOI] [PubMed] [Google Scholar]
- 30.Srikiatkhachorn A, Krautrachue A, Ratanaprakarn W, Wongtapradit L, Nithipanya N, Kalayanarooj S, et al. Natural history of plasma leakage in dengue hemorrhagic fever: a serial ultrasonographic study. Pediatr Infect Dis J. 2007;26:283–90. doi: 10.1097/01.inf.0000258612.26743.10. [DOI] [PubMed] [Google Scholar]
- 31.Wang JY, Tseng CC, Lee CS, Cheng KP. Clinical and upper gastroendoscopic features of patients with dengue virus infection. J Gastroenterol Hepatol. 1990;5:664–8. doi: 10.1111/j.1440-1746.1990.tb01122.x. [DOI] [PubMed] [Google Scholar]
- 32.Chiu YC, Wu KL, Kuo CH, Hu TH, Chou YP, Chuah SK, et al. Endoscopic findings and management of dengue patients with upper gastrointestinal bleeding. Am J Trop Med Hyg. 2005;73:441–4. [PubMed] [Google Scholar]
- 33.Tsai CJ, Kuo CH, Chen PC, Changcheng CS. Upper gastrointestinal bleeding in dengue fever. Am J Gastroenterol. 1991;86:33–5. [PubMed] [Google Scholar]
- 34.Imbert P, Sordet D, Hovette P, Touze JE. Spleen rupture in a patient with dengue fever. Trop Med Parasitol. 1993;44:327–8. [PubMed] [Google Scholar]
- 35.Pungjitprapai A, Tantawichien T. A fatal case of spontaneous rupture of the spleen due to dengue virus infection: case report and review. Southeast Asian J Trop Med Public Health. 2008;39:383–6. [PubMed] [Google Scholar]
- 36.Basurko C, Carles G, Youssef M, Guindi WE. Maternal and fetal consequences of dengue fever during pregnancy. Eur J Obstet Gynecol Reprod Biol. 2009;147:29–32. doi: 10.1016/j.ejogrb.2009.06.028. [DOI] [PubMed] [Google Scholar]
- 37.Carles G, Peiffer H, Talarmin A. Effects of dengue fever during pregnancy in French Guiana. Clin Infect Dis. 1999;28:637–40. doi: 10.1086/515144. [DOI] [PubMed] [Google Scholar]
- 38.Thaithumyanon P, Thisyakorn U, Deerojnawong J, Innis BL. Dengue infection complicated by severe hemorrhage and vertical transmission in a parturient woman. Clin Infect Dis. 1994;18:248–9. doi: 10.1093/clinids/18.2.248. [DOI] [PubMed] [Google Scholar]
- 39.Chitra TV, Panicker S. Maternal and fetal outcome of dengue fever in pregnancy. J Vector Borne Dis. 2011;48:210–13. [PubMed] [Google Scholar]
- 40.Kalayanarooj S, Rimal HS, Andjaparidze A, Vatcharasaevee V, Nisalak A, Jarman RG, et al. Clinical intervention and molecular characteristics of a dengue hemorrhagic fever outbreak in Timor Leste, 2005. Am J Trop Med Hyg. 2007;77:534–7. [PubMed] [Google Scholar]
- 41.Kuo CH, Tai DI, Chang-Chien CS, Lan CK, Chiou SS, Liaw YF. Liver biochemical tests and dengue fever. Am J Trop Med Hyg. 1992;47:265–70. doi: 10.4269/ajtmh.1992.47.265. [DOI] [PubMed] [Google Scholar]
- 42.Kurane I, Innis BL, Nimmannitya S, Nisalak A, Rothman AL, Livingston PG, et al. Human immune responses to dengue viruses. Southeast Asian J Trop Med Public Health. 1990;21:658–62. [PubMed] [Google Scholar]
- 43.Trung DT, Thao le TT, Hien TT, Hung NT, Vinh NN, Hien PT, et al. Liver involvement associated with dengue infection in adults in Vietnam. Am J Trop Med Hyg. 2010;83:774–80. doi: 10.4269/ajtmh.2010.10-0090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ling LM, Wilder-Smith A, Leo YS. Fulminant hepatitis in dengue haemorrhagic fever. J Clin Virol. 2007;38:265–8. doi: 10.1016/j.jcv.2006.12.011. [DOI] [PubMed] [Google Scholar]
- 45.Parkash O, Almas A, Jafri SM, Hamid S, Akhtar J, Alishah H. Severity of acute hepatitis and its outcome in patients with dengue fever in a tertiary care hospital Karachi, Pakistan (South Asia). BMC Gastroenterol. 2010;10:43. doi: 10.1186/1471-230X-10-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Thakare J, Walhekar B, Banerjee K. Hemorrhagic manifestations and encephalopathy in cases of dengue in India. Southeast Asian J Trop Med Public Health. 1996;27:471–5. [PubMed] [Google Scholar]
- 47.Nimmannitya S, Thisyakorn U, Hemsrichart V. Dengue haemorrhagic fever with unusual manifestations. Southeast Asian J Trop Med Public Health. 1987;18:398–406. [PubMed] [Google Scholar]
- 48.Jusuf H, Sudjana P, Djumhana A, Abdurachman SA. DHF with complication of acute pancreatitis related hyperglycemia: a case report. Southeast Asian J Trop Med Public Health. 1998;29:367–9. [PubMed] [Google Scholar]
- 49.Pancharoen C, Thisyakorn U. Coinfections in dengue patients. Pediatr Infect Dis J. 1998;17:81–2. doi: 10.1097/00006454-199801000-00019. [DOI] [PubMed] [Google Scholar]
- 50.Thisyakorn U, Thisyakorn C, Limpitikul W, Nisalak A. Dengue infection with central nervous system manifestations. Southeast Asian J Trop Med Public Health. 1999;30:504–6. [PubMed] [Google Scholar]
- 51.Solomon T, Dung NM, Vaughn DW, Kneen R, Thao LT, Raengsakulrach B, et al. Neurological manifestations of dengue infection. Lancet. 2000;355:1053–9. doi: 10.1016/S0140-6736(00)02036-5. [DOI] [PubMed] [Google Scholar]
- 52.Davis JS, Bourke P. Rhabdomyolysis associated with dengue virus infection. Clin Infect Dis. 2004;38:e109–11. doi: 10.1086/392510. [DOI] [PubMed] [Google Scholar]
- 53.Promphan W, Sopontammarak S, Pruekprasert P, Kajornwattanakul W, Kongpattanayothin A. Dengue myocarditis. Southeast Asian J Trop Med Public Health. 2004;35:611–13. [PubMed] [Google Scholar]
- 54.Chanthamat N, Sathirapanya P. Acute transverse myelitis associated with dengue viral infection. J Spinal Cord Med. 2010;33:425–7. doi: 10.1080/10790268.2010.11689722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Misra UK, Kalita J, Syam UK, Dhole TN. Neurological manifestations of dengue virus infection. J Neurol Sci. 2006;244:117–22. doi: 10.1016/j.jns.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 56.Garcia-Rivera EJ, Rigau-Perez JG. Encephalitis and dengue. Lancet. 2002;360:261. doi: 10.1016/S0140-6736(02)09481-3. [DOI] [PubMed] [Google Scholar]
- 57.Chokephaibulkit K, Kankirawatana P, Apintanapong S, Pongthapisit V, Yoksan S, Kositanont U, et al. Viral etiologies of encephalitis in Thai children. Pediatr Infect Dis J. 2001;20:216–18. doi: 10.1097/00006454-200102000-00020. [DOI] [PubMed] [Google Scholar]
- 58.Lum LC, Lam SK, Choy YS, George R, Harun F. Dengue encephalitis: a true entity? Am J Trop Med Hyg. 1996;54:256–9. doi: 10.4269/ajtmh.1996.54.256. [DOI] [PubMed] [Google Scholar]
- 59.Harris E, Perez L, Phares CR, Perez Mde L, Idiaquez W, Rocha J, et al. Fluid intake and decreased risk for hospitalization for dengue fever, Nicaragua. Emerg Infect Dis. 2003;9:1003–6. doi: 10.3201/eid0908.020456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Molyneux EM, Maitland K. Intravenous fluids – getting the balance right. N Engl J Med. 2005;353:941–4. doi: 10.1056/NEJMe058135. [DOI] [PubMed] [Google Scholar]
- 61.Dung NM, Day NP, Tam DT, Loan HT, Chau HT, Minh LN, et al. Fluid replacement in dengue shock syndrome: a randomized, double-blind comparison of four intravenous-fluid regimens. Clin Infect Dis. 1999;29:787–94. doi: 10.1086/520435. [DOI] [PubMed] [Google Scholar]
- 62.Ngo NT, Cao XT, Kneen R, Wills B, Nguyen VM, Nguyen TQ, et al. Acute management of dengue shock syndrome: a randomized double-blind comparison of 4 intravenous fluid regimens in the first hour. Clin Infect Dis. 2001;32:204–13. doi: 10.1086/318479. [DOI] [PubMed] [Google Scholar]
- 63.Wills BA, Oragui EE, Dung NM, Loan HT, Chau NV, Farrar JJ, et al. Size and charge characteristics of the protein leak in dengue shock syndrome. J Infect Dis. 2004;190:810–18. doi: 10.1086/422754. [DOI] [PubMed] [Google Scholar]