Abstract
Several recent studies have found that throwing athletes typically have lower humeral torsion (retroversion) and a greater range of external rotation at the shoulder than non-athletes. How these two parameters are related is debated. This study uses data from a sample of both throwers and non-throwers to test a new model that predicts torsion values from a range of motion data. The model proposes a series of predicted regressions which can help provide new insight into the factors affecting rotational range of motion at the shoulder. Humeral torsion angles were measured from computed tomography scans collected from 25 male subjects. These values are compared to predicted torsion values for the same subjects calculated from both kinematic and goniometric range-of-motion data. Results show that humeral torsion is negatively correlated (goniometric: r = −0.409, P = 0.047; kinematic: r = −0.442, P = 0.035) with external rotational range of motion and positively correlated (goniometric: r = 0.741, P < 0.001; kinematic: r = 0.559, P = 0.006) with internal rotational range of motion. The predicted torsion values are highly correlated (goniometric: r = 0.815, P < 0.001; kinematic: r = 0.617, P = 0.006) with actual torsion values. Deviations in the data away from predicted equations highlight significant differences between high torsion and low torsion individuals that may have significant functional consequences. The method described here may be useful for non-invasively assessing the degree of torsion in studies of the evolution and biomechanics of the shoulder and arm, and for testing hypotheses about the etiology of repetitive stress injuries among athletes and others who throw frequently.
Keywords: glenohumeral joint, humeral retroversion, humeral rotation, humeral torsion, throwing
Introduction
Humeral torsion describes the angular difference between the orientation of the proximal humeral head and the axis of the elbow at the distal humerus. This angle is measured at the intersection of two lines: one that evenly bisects the articular surface of the humeral head proximally, and the second being the transepicondylar line distally (Fig. 1). In the clinical literature, this angle is measured in the opposing direction and is referred to as humeral retroversion. Therefore, a measured increase in retroversion is the same as a decrease in torsion. These two terms simply represent different assumptions about the neutral position of this angle (Evans & Krahl, 1945; Krahl, 1947; Hill et al. 1989; Larson, 2007b; Rhodes, 2007). The use of alternative terms has led to some confusion in the literature (Larson, 2007b; Rhodes, 2007). For clarity, we will here use exclusively the term humeral torsion and have translated the results of previous studies cited as needed.
Fig. 1.
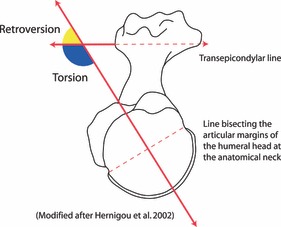
Humeral torsion (in blue) is determined by measuring the angle between the orientation of the humeral head and the distal condyle of the humerus. In the clinical literature, the same angle is referred to as humeral retroversion (in yellow) and is measured in the opposite direction.
In humans, humeral torsion is highly variable. Torsion values have been shown to differ between western and non-western populations (Broca, 1881; Martin, 1933; Evans & Krahl, 1945; Krahl & Evans, 1945), males and females (Broca, 1881; Martin, 1933; Krahl & Evans, 1945; Edelson, 1999), and by side of the body (Broca, 1881; Krahl & Evans, 1945; Kronberg et al. 1990). Torsion also varies ontogenetically, with younger individuals having less torsion, which then increases during postnatal growth (Krahl, 1947; Edelson, 2000; Scheuer & Black, 2000; Cowgill, 2007). During normal postnatal ontogeny, torsion steadily increases by an average of 23.4° until the completion of skeletal growth (Cowgill, 2007). Much of this change in torsion seems to occur at the proximal humerus, which is one of the last bones in the body to fuse: only 20% of individuals have achieved fusion by 18 years of age (McKern & Stewart, 1957).
Many previous functional studies of humeral torsion have focused on the relationship between torsion and habitual throwing activity (Pieper, 1998; Crockett et al. 2002; Osbahr et al. 2002; Reagan et al. 2002; Chant et al. 2007). Athletes who habitually throw tend to have 10–20° less torsion in their dominant, throwing arm compared to their non-dominant arm and the arms of non-throwing controls (King et al. 1969; Brown et al. 1988; Magnusson et al. 1994; Bigliani et al. 1997; Pieper, 1998; Crockett et al. 2002; Osbahr et al. 2002; Reagan et al. 2002; Borsa et al. 2005, 2006; Chant et al. 2007). No statistical difference has been found between arms in non-throwing controls (Pieper, 1998; Crockett et al. 2002; Chant et al. 2007). Furthermore, Pieper (1998) showed that when throwing athletes are subdivided into those with and without chronic pain, those reporting chronic pain did not show this reduction in dominant arm torsion. Other studies have sought to further clarify the relationship of torsion to injury by linking torsion to rotational range-of-motion (ROM) in the shoulder (Osbahr et al. 2002; Reagan et al. 2002; Chant et al. 2007).
Deficits to rotational ROM in the shoulder have long been suggested as a potential cause of shoulder injury in throwing athletes (Ellenbecker et al. 2002; Burkhart et al. 2003a,b; Dines et al. 2009; Torres & Gomes, 2009; Wilk et al. 2011). A recent study by Wilk et al. (2011) showed that a deficit to the total rotational ROM at the shoulder of as little as 5° led to a twofold increase in the likelihood of injury. Previous work has shown that, much like torsion, rotational ROM also differs between dominant and non-dominant arms in throwing athletes (Brown et al. 1988; Ellenbecker et al. 1996, 2002; Kibler et al. 1996; Bigliani et al. 1997; Crockett et al. 2002; Osbahr et al. 2002; Reagan et al. 2002; Chant et al. 2007). Throwing athletes typically have an externally shifted ROM arc in the throwing arm, with an increase in external rotational ROM of between 9° and 13° and a similar deficit to the internal rotational ROM (Crockett et al. 2002; Osbahr et al. 2002; Reagan et al. 2002; Chant et al. 2007).
Beyond its relevance to understanding injury, rotational range of motion at the shoulder may also have significant performance consequences. Glenohumeral rotation is known to be a significant contributor to power generated during the throwing motion (Dillman, 1990; Fleisig et al. 1995, 1996; Bigliani et al. 1997; Hirashima et al. 2007). Reaching angular velocities in excess of 9000° per second, the rapid internal rotation of the humerus is the fastest motion produced by the human body and this rotation can generate very high torques (Fleisig et al. 1995, 1996; Bigliani et al. 1997; Pappas et al. 1985). Whether modifications to the rotational ROM allow additional acceleration of the arm and torque production at the shoulder is unknown and is an important avenue for future research.
What factors contribute to variations in the rotational ROM arc is unclear. Numerous authors have posited that these modifications result primarily from changes to the soft tissues of the shoulder capsule (King et al. 1969; Pappas et al. 1985; Brown et al. 1988; Kvitne & Jobe, 1993; Magnusson et al. 1994; Jobe et al. 1996; Bigliani et al. 1997; Burkhart et al. 2000; Meister, 2000a,b). These same studies note the high prevalence of severe laxity in the anterior glenohumeral capsule of throwing athletes. Burkhart and colleagues have further suggested that this anterior laxity is accompanied by tightening of the ligaments in the posterior portion of the capsule (Burkhart et al. 2000, 2003a). Still others have suggested that skeletal remodeling of the proximal humerus is the major cause of modifications to the rotational ROM at the shoulder (Pieper, 1998; Crockett et al. 2002; Osbahr et al. 2002; Reagan et al. 2002; Chant et al. 2007). Several studies investigating the relationship between humeral torsion and rotational ROM have found significant correlations between these two variables in professional and collegiate throwing athletes (Osbahr et al. 2002; Reagan et al. 2002; Chant et al. 2007). However, these correlations have not been consistent in either strength or directionality between studies.
Although the studies noted above have all found significant negative correlations between external rotational ROM and torsion, the relationship between internal rotational ROM and torsion is less clear. Osbahr et al. (2002) and Reagan et al. (2002) found no statistically significant relationship between internal rotational ROM and torsion in baseball pitchers. In contrast, Reagan et al. (2002) found these variables to be significantly, negatively correlated in baseball players playing field positions. This result contrasts with another study of baseball players of unspecified positions in which internal rotational ROM and torsion were significantly, positively correlated (Chant et al. 2007).
We sought to clarify and generalize the relationship between humeral torsion and rotational range of motion at the shoulder using a sample of both collegiate athletes and non-athletes. We propose a simple, new model to predict expected torsion values from ROM data collected using both standard goniometry and kinematics. Our method is then validated against observed (actual) torsion values derived from computed tomography (CT). This observed vs. expected framework allows us to generate testable predictions and move beyond simple strength of correlation results. Using this method, we can begin to address the complex interplay between how soft and hard tissues affect ROM at the shoulder joint, how this interplay may relate to injury, and the possible functional consequences of these tradeoffs. This method also provides a means to assess ranges of motion in the fossil record, allowing us to test some hypotheses about the evolution of throwing capabilities.
Model
We tested a model that uses ROM measures to predict torsion values and vice versa. Our model is based on a set of simple assumptions.
We begin with the assumption that the total rotational ROM (internal + external) is not correlated significantly with the degree of torsion, as shown by previous studies (Osbahr et al. 2002; Reagan et al. 2002; Chant et al. 2007). We therefore would expect any angular change at the external end of the ROM arc must be coupled with a commensurate, opposing angular change at the internal end of the ROM arc. Thus, whereas the values for internal and external rotational ROM will change, the sum of these to values will not. This requires a one-to-one tradeoff between internal and external rotational ROM, which accounts for the constant total ROM value, and leads to all regression predictions between torsion and any range of motion value in our analyses having an absolute slope of 1.0. This predicted slope allows for changes in torsion to affect changes in the position of the ROM arc relative to the body without affecting the total ROM. Furthermore, this assumption of a constant total ROM leads to the prediction that the regression relationships between external rotational ROM/torsion and internal rotational ROM/torsion should also be inversely related (as one increases, the other decreases).
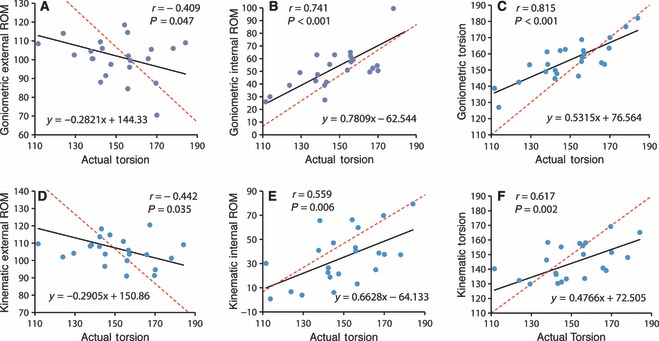
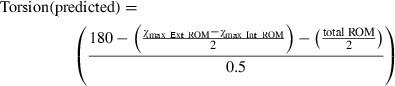
Predicting torsion values from ROM data further requires the assumption that the midpoint of the total ROM arc represents the neutral, resting position of the humerus in relation to the scapular glenoid. If this is correct, then the location of this neutral position should provide an indication of the degree of humeral torsion. Individuals with a total ROM midpoint that is internally shifted are predicted to have a higher torsion value than individuals with more externally shifted total ROM midpoints. Using the measured external and internal rotational ROM maxima, expected torsion values are generated using the formula below (see also Fig. 2). Note that the addition/subtraction of 180° in all formulas allows our results to be reported using a common convention for human torsion values (e.g. Martin, 1933; Larson, 1988):
Fig. 2.
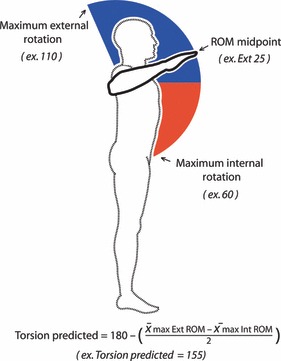
Torsion is predicted from mean ROM maxima data. The difference between external and internal rotation (in the example –25°) is equal to the ROM midpoint. The use of the 180° term allows the torsion value to be reported according to prior convention. Note: Following clinical definition, external rotational ROM is illustrated in blue and internal rotational ROM is illustrated in red.
 |
1 |
To test our assumptions, these expected values are regressed against actual torsion values. If our model is accurate, the predicted torsion values will closely match the actual values. Thus, for the predicted torsion (y)/actual torsion (x) regression we predict a regression equation of y = x.
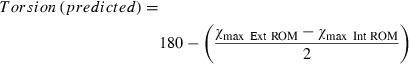
Although predicting torsion values from ROM data is useful, when the actual regressions differ from our predictions it becomes important to address the discrepancy accurately. By running our model in the reverse direction and predicting external and internal rotational ROM from actual torsion values we can better identify the source of the discrepancy. These reverse predictions again rely on the assumption that the midpoint of the total rotational ROM reflects the underlying torsion. Given this assumption, a predicted ROM midpoint can be generated from actual torsion values. By adding/subtracting half of the mean total ROM from this midpoint, external and internal ROM maxima can be generated. The formula used to generate predicted external ROM values is:
 |
2 |
The regression equation derived from this formula is y = −x + (180 + ½ total ROM); with (y) as predicted external ROM and (x) as actual torsion. For our calculations, we use the mean total ROM value across all subjects (reported below). According to our model, as torsion increases there should be a commensurate decrease in external ROM maxima (hence the slope of −1.0). This prediction is tested against the actual, external rotational ROM maxima/torsion regression. The formula used to generate predicted internal ROM values is:
 |
3 |
The regression equation derived from this formula is y = x− (180 −½ total ROM); with (y) as predicted internal ROM and (x) as actual torsion. Accordingly, as torsion increases, so should the internal ROM maxima (hence the slope of 1.0). This prediction is tested against the actual internal rotational ROM maxima/torsion regression.
Materials and methods
Subjects
Twenty-five adult male subjects (ages 18–35 years) were recruited to participate in the study. Thirteen of the subjects were collegiate athletes (six baseball players from a variety of positions, seven athletes from non-throwing sports) and the remaining 12 subjects were non-athletes. The proportions of the study sample were chosen to maximize the variance in torsion values surveyed and to reduce the effects of pathological ROM often found in throwing athletes (Burkhart et al. 2000; Dines et al. 2009; Wilk et al. 2011). Institutional review board approval was obtained from both Massachusetts General Hospital and Harvard University. Subjects provided written consent and completed an injury history and physical activity questionnaire prior to participation in the study.
Computed tomography (CT) imaging
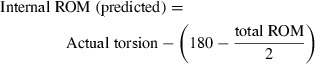
All subjects were CT scanned at the Massachusetts General Hospital Imaging Center using a GE 8-slice Lightspeed Computed Tomography Imager. A low dose scanning technique was used to minimize radiation exposure to the subjects. Subjects were positioned on the scanner examination table with their dominant arm fully adducted at their side and their elbow flexed 90° with their forearm resting on their abdomen. The arm was then immobilized by wedging a stiff pillow between the arm and the examination table. Two separate scans were targeted and collected at the shoulder and the elbow. Each scan covered approximately 5 cm of the arm, capturing each end of the humerus with 5-mm-thick image slices. The images were processed using image j software and the humeral torsion angle calculated (following Hernigou et al. 2002) by subtracting the angle of the transepicondylar line from the axis of the humeral head (Fig. 3). The humeral torsion angle was calculated using the mean of the three best superior and inferior scans. The measurement reliability was calculated (see Supporting Information) and the mean torsion angle was used in the analysis as the actual, CT-derived torsion value.
Fig. 3.
Humeral torsion was measured in image j by creating transects between the inflection points marking the anatomical neck proximally (A) and along the distal transepicondylar line (B).
Range of motion (ROM) measures
Active ROM was measured using both standard goniometry and three-dimensional kinematic imaging. Active ROM, where subjects rotate their arm to the limits of their ROM using their own muscular power, was used instead of passive ROM because it most closely approximates the functional ROM available for actions such as throwing and also reduces the effects of any anisotropy in the capsular ligaments. The two different methods for collecting ROM data were used to maximize the utility of our method for a variety of research and clinical contexts.
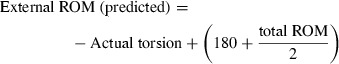
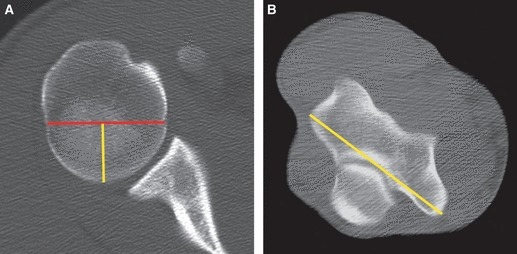
For goniometric ROM measurements, subjects were positioned on an examination table with their dominant arm off the side of the table (Fig. 4). The arm was positioned in line with both shoulders in a neutral shoulder flexion/extension posture. The shoulder was abducted 90° and the elbow flexed 90°. The subject was instructed to keep their shoulder pressed to the examination table to prevent scapular movement. The subject then rotated his arm to both its maximal external and internal rotation position and held this position for 5 s for goniometric measurement taken along the length of the forearm. The measurements were taken using a Jamar 12½″ goniometer, which was modified to include a weighted plumb line to serve as a vertical arm. The rotational motion and measurements were repeated twice. Measurement repeatability was calculated using the interclass correlation (see Supporting Information). The means of both external and internal ROM maxima measures were taken and the predicted, goniometry-derived torsion value was calculated using Eqn 1.
Fig. 4.
For the ROM calculations, each subject was measured using a standard goniometer (A) and a kinematic imaging system (B). For the goniometric measurement, the subject was in a supine position on an examining table. For the kinematic measurement, the subject was seated in an armless chair. External rotational ROM is illustrated in blue and internal rotational ROM in red.
For the kinematic ROM measurements, data was collected using an eight-camera Qualisys Motion Capture 3D Infrared Oqus camera system collecting at 500 Hz. All subjects were fitted with nine 25-cm passive reflective markers. The markers were placed on C7 prominens, both hips (at the greater trochanter of the femora), both scapular acromion, the lateral and medial epicondyles of the dominant side distal humerus and both ulnar and radial styloid processes in the dominant side wrist. The subject was then seated in an armless, high-backed office chair in an upright posture with the back firmly against the chair back. The subject was again instructed to position his arm out to the side of his body, in line with both shoulders. The shoulder was abducted 90° and the elbow flexed 90°. The subject was then instructed to again rotate their arm to both its maximal external and internal rotation position with as little scapular motion as possible (to limit scapular protraction or retraction). The motion was repeated between four and six times during 30 s of data capture. Raw 3D marker positional data were processed using qualisys task manager software and exported for analysis to matlab 7.6. Custom-written matlab code was used to calculate external and internal ROM maxima while correcting for minor deviations in elbow and shoulder position. Measurement reliability was calculated and the means of both external and internal rotational maxima were used to generate predicted, kinematics-derived torsion values using Eqn 1.
Statistical analysis
Pearson correlation coefficients were calculated and the presence of outliers tested (using Mahalanobis distances at a 95% confidence interval) with jmp version 5 software. Intraclass correlations were calculated to assess measurement reliability using spss version 19 software.
Results
Total rotational ROM was calculated first as an initial test of the validity of our model. Total ROM values, calculated as the external ROM maxima plus the internal ROM maxima, ranged from 108.5 to 205.5° (goniometric: mean 153.4, SD 18.2; kinematic: mean 142.3, SD 21.5). As hypothesized, no statistically significant correlation was found between actual torsion and the total rotational ROM (goniometric: r = 0.229, P = 0.293; kinematic: r = 0.328, P = 0.127). This lack of a significant relationship between torsion and total rotational ROM is consistent with previous studies (Osbahr et al. 2002; Reagan et al. 2002; Chant et al. 2007) and provides support for our model's initial assumption.
The measured values of both internal and external rotation ROM were then regressed against actual, CT-derived torsion values. These regressions were compared to the predicted regression relationship derived from the model to assess any potential skew in our model.
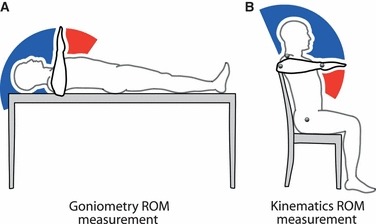
Measured external ROM values ranged from 70.5 to 120.5° (goniometric: mean 100.7, SD 10.9; kinematic: mean 105.4, SD 7.9). In keeping with previous work (Osbahr et al. 2002; Reagan et al. 2002; Chant et al. 2007) and our model's predictions, external rotational ROM is significantly negatively correlated with actual torsion using both goniometric (r = −0.409) and kinematic (r = −0.442) measures. However, the slope of the measured external ROM/torsion regression is significantly lower than our predicted slope of −1.0 (Fig. 5A,D). This deviation from the predicted equation appears to be driven primarily by lower than predicted external ROM values in low torsion individuals.
Fig. 5.
Regression relationships, Pearson's correlation coefficients (r) and significance values (P) are shown for all statistically significant parameters. The red dashed line illustrates the expected regression equations for each parameter. Please note: The number of subjects (n) represented in each graph is variable. For graphs A and C; n = 24 as goniometry data were not collected for one subject. For graph B; n = 23 due to the same lack of data from one subject and the exclusion of a significant outlier. For graphs D, E and F; n = 23 as maker occlusion prevents calculation for two subjects.
Measured internal ROM values ranged from 1 to 99.5° (goniometric: mean 51.5, SD 15.5; kinematic: mean 34.8, SD 22.4). As hypothesized, internal rotational ROM is significantly positively correlated with actual torsion using both goniometric (r = 0.741) and kinematic (r = 0.559) measures. The internal ROM/actual torsion regression equations are not significantly different from the predicted equation and the predicted slope of 1.0 (Fig. 5B,E).
Finally, predicted torsion values were calculated from both ROM data sets and regressed against actual torsion. The actual (CT-derived) torsion values ranged from 111.6 to 184.1° (mean – 141.1, SD – 18.3). Both predicted torsion measures are significantly correlated with actual torsion (Fig. 5C,F). Goniometric predictions are more highly correlated (r = 0.815) with actual values than are the kinematic predictions (r = 0.617). Beyond the strength of the correlations, it is worth noting that neither predicted vs. actual torsion regressions has the slope of 1.0 expected in our model. Both predicted/actual torsion regressions show significantly higher predicted values in individuals with low actual torsion. This is in keeping with the deviation from expected values found in the external ROM maxima in low torsion individuals. While the strength of the correlations varies between the ROM collection methods, the regression equations for both predicted/actual torsion regressions are statistically indistinguishable from each other.
Discussion
As predicted, the above results show that the ROM available for internal rotation increases with humeral torsion. Further, this increase is accompanied by a decrease in the ROM available for external rotation. This finding supports the inverse tradeoff between internal and external rotation and humeral torsion found by Chant et al. (2007). The strength of the correlations reported here between ROM and torsion are equivalent to previous published values for external rotation ROM and significantly higher than previously published values for internal rotation ROM (Osbahr et al. 2002; Reagan et al. 2002; Chant et al. 2007). This improved correlation coefficient for the relationship between internal rotational ROM and torsion may partly result from increasing the variance in the sample by including non-throwers in the study population.
As in previous studies, no significant relationship was found between total rotational ROM and humeral torsion (Osbahr et al. 2002; Reagan et al. 2002; Chant et al. 2007). This result supports the validity of our model's assumptions. It should be noted that there is a non-significant trend in this relationship towards a slight increase in total rotational ROM with increased torsion from both ROM datasets. A power test indicates that significantly larger samples would be required to test the statistical validity of this trend (needed sample, goniometric: 197; kinematic: 92). If this trend were supported, it would seem to defy clinical expectations that low torsion throwing athletes might be expected to extend their total rotational ROM with increased laxity of the anterior shoulder capsule. However, in the light of its current non-significance this trend should be interpreted with caution until a larger, balanced sample of throwers and non-throwers is available.
The strength of the correlation coefficients reported here suggests that the hard tissue contributions to rotational ROM are significant and that soft tissue contributions are likely of secondary importance and are possibly quite minimal. The differences in capsular laxity reported in previous studies (Burkhart et al. 2000; Dines et al. 2009; Torres & Gomes, 2009) may in fact be the result of other shoulder motions and have very little to do with humeral rotation. Given the near spherical shape of the articular surface of the humeral head and the rotational nature of the motion investigated here, it seems likely that, in a neutral shoulder flexion/extension posture, the anterior and posterior ligaments of the glenohumeral capsule would be stretched roughly equally. Only when these humeral rotations are accompanied by deviations from this neutral flexion/extension posture, such as during the maximal shoulder extension seen in the windup of a pitch, would we expect the asymmetrical stretching of the capsular ligaments and the resulting laxity.
The strength of the predicted torsion values reported here strongly validate our method of estimating torsion using simple kinematic measures and without the use of costly radioactive imaging. Although the goniometric predictions were significantly stronger in this analysis than the kinematic method, this difference in strength may very well be due to small scapular protraction/retraction that occurred during the kinematic imaging trials. Whereas scapular movement was limited by contact with the table during goniometric data collection, this was not possible during the kinematic trials. Although our marker setup allowed us to identify protraction and retraction of the scapula, without additional markers collecting scapular movement data it was not possible to correct for the minor scapular rotations that accompanied these movements. Another potential factor affecting the strength of our regressions could result from not providing external support for the weight of the arm. Minor deviations in humeral position could introduce noise into our data. However, due to the short duration of data collection, fatigue effects are unlikely and humeral movements are thought to be quite minimal and evenly applied to both datasets. Although these small movements apparently reduced the strength of the regressions (more noticeably in the kinematic data), they did not significantly alter the slope of the regression equations. The consistency of the slope between both ROM datasets provides further confidence in the predictive model.
A key result is that the predicted torsion values deviate from the predicted regression equation (y = x), especially in the low torsion individuals. These low torsion individuals showed more internal rotation than expected and lower external rotation. In the kinematic ROM measures the high torsion individuals also deviate from the predicted regression with higher than expected external ROM and lower internal ROM. What factors are responsible for these residuals is unclear. Covarying changes in the carrying angle of the elbow (Hernigou et al. 2002) could be responsible for these differences, as might some non-ligamentous soft tissue constraint such as differences in muscle mass. Further research is needed to resolve this problem.
Based on our empirical data (reported in Fig. 5C,F), we propose that a better linear regression for predicting torsion would be (y = 5x + ½ total ROM). This regression equation represents a simplification of the empirically derived slopes (0.4766x, 0.5315x) to a slope of 0.5x and the empirical intercepts (72.505, 76.564) to an intercept equal to half of the total ROM (for our data – 71.2, 76.7 respectively). Using this modified regression equation to predicting torsion from ROM maxima, we derive:
 |
4 |
This predictive equation is useful in kinematic studies and when imaging of subjects is not possible. It could also be a useful clinical tool for quickly identifying throwing athletes with high torsion values who might be at increased risk of shoulder and elbow injury.
This non-invasive assessment of torsion may be particularly important for juvenile athletes. Little League players (especially pitchers) have been shown to have high rates of injury both to the shoulder and elbow (Adams, 1966; Gugenheim et al. 1976; Larson et al. 1976; Axe et al. 1996; Klingele & Kocher, 2002; Ricci & Mason, 2004; Olsen et al. 2006; Keeley et al. 2008; Stein & Micheli, 2011). It has been suggested that these injuries are the result of overuse of the shoulder and arm during the throwing motion (Jobe et al. 1996; Burkhart et al. 2000; Lyman et al. 2002; Fleisig et al. 2011). It is also possible that the risk of injury in juveniles is further increased due to the incomplete torsion of their throwing arm. Such incomplete torsion could lead to compensations in the throwing motion, which in turn could put additional stresses on downstream joint such as the elbow, leading to injury.
It is also noteworthy that there are some significant differences between the correlation values reported in this and other studies (Osbahr et al. 2002; Reagan et al. 2002; Chant et al. 2007). These may in fact represent important differences in functional constraints between differing study populations. Our study found correlation coefficients for external rotation ROM and torsion that were equal to or slightly lower than previous studies. Conversely, we found significantly higher correlation values for the relationship between internal rotation ROM and torsion. This may be due to the fact that our study surveyed a wide variety of torsion values and included many non-throwers, whereas previous work has largely focused on throwing athletes. It is possible that these groups have different functional requirements when it comes to humeral rotation. Non-throwers may require more internal rotational movement for manipulative tasks and power generation for actions such as pounding and prying. Conversely, throwing athletes, for whom high projectile velocity is imperative, may benefit greatly from increased external rotational ROM. An increase in external rotational ROM could allow throwers to achieve a much greater range of rotational motion prior to the release of the projectile and still maintain accuracy. Given that humeral rotation is known to occur very quickly and is a significant contributor to projectile velocity at release, a change in rotational ROM could have significant performance effects during throwing. These potential differences in functional constraint may explain some important differences in the literature and are a relevant avenue of future study.
In short, humeral torsion significantly affects rotational ROM at the shoulder. Low torsion (high retroversion) is strongly associated with reduced internal rotational ROM and a greater range of external rotational ROM. We present a simple metric for assessing humeral torsion using non-invasive, easily obtained ROM data which can be helpful clinically in diagnosing individuals with high risk of shoulder and elbow injuries and useful for kinematic studies of shoulder motion. This method also allows for the assessment of rotational ROM at the shoulder from the skeleton itself. Assessing ROM using skeletal material allows for estimates of ROM at the shoulder in fossil hominins, which show considerable variability in this feature. For example, two recently published Homo erectus skeletons have been shown to have low degrees of humeral torsion (Larson, 2007a; Lordkipanidze et al. 2007). These values are similar to or lower than those found in the dominant arm in elite throwing athletes, suggesting a comparable or even more externally shifted ROM in these hominin shoulders. If it is the case, as we propose, that greater external rotational ROM at the shoulder increases throwing velocity, then it is possible that the uniquely human capacity for high performance throwing may have evolved by 2 million years ago. Testing this hypothesis, however, requires additional data on how rotational ROM at the shoulder relates to throwing velocity, as well as how other anatomical changes in the upper body that occur in H. erectus affect the ability to throw with power and accuracy.
Acknowledgments
The authors would like to thank the subjects who volunteered their time, the staff at the MGH Imaging Service, Michelle Cardillo, Louise Borda and Isabella Suzarte for their help making this study possible. The authors would also like to thank the two reviewers for their helpful comments and criticisms. Generous funding for the Qualisys Oqus camera system was provided by the Hintze Family Charitable Trust and the American School for Prehistoric Research. External funding was provided by the National Science Foundation (BCS 0961943).
Author contributions
N.R. designed the experiment, collected and analyzed the data and wrote the manuscript. D.L. provided critical feedback on the experimental design and manuscript. T.G. IV and W.P. provided material support. T.G. III helped with human subjects’ approval and provided critical feedback on the experimental design and manuscript.
Supporting Information
Table S1. Measurement reliability using intra-class correlation coefficients (ICC).
As a service to our authors and readers, this journal provides supporting information supplied by the authors. Such materials are peer-reviewed and may be re-organized for online delivery, but are not copy-edited or typeset. Technical support issues arising from supporting information (other than missing files) should be addressed to the authors.
As a service to our authors and readers, this journal provides supporting information supplied by the authors. Such materials are peer-reviewed and may be re-organized for online delivery, but are not copy-edited or typeset. Technical support issues arising from supporting information (other than missing files) should be addressed to the authors.
References
- Adams JE. Little League shoulder: osteochondrosis of the proximal humeral epiphysis in boy baseball pitchers. Calif Med. 1966;105:22–25. [PMC free article] [PubMed] [Google Scholar]
- Axe MJ, Snyder-Mackler L, Konin JG, et al. Development of a distance-based interval throwing program for little league-aged athletes. Am J Sports Med. 1996;24:594–602. doi: 10.1177/036354659602400506. [DOI] [PubMed] [Google Scholar]
- Bigliani LU, Codd TP, Connor PM, et al. Shoulder motion and laxity in the professional baseball player. Am J Sports Med. 1997;25:609–613. doi: 10.1177/036354659702500504. [DOI] [PubMed] [Google Scholar]
- Borsa PA, Wilk KE, Jacobson JA, et al. Correlation of range of motion and glenohumeral translation in professional baseball pitchers. Am J Sports Med. 2005;33:1392–1399. doi: 10.1177/0363546504273490. [DOI] [PubMed] [Google Scholar]
- Borsa PA, Dover GC, Wilk KE, et al. Glenohumeral range of motion and stiffness in professional baseball pitchers. Med Sci Sports Exerc. 2006;38:21–26. doi: 10.1249/01.mss.0000180890.69932.15. [DOI] [PubMed] [Google Scholar]
- Broca P. Le torsion de l'humerus et le tropometre. Rev Anthropol. 1881;4:193–210. 385–423. [Google Scholar]
- Brown LP, Niehues SL, Harrah A, et al. Upper extremity range of motion and isokinetic strength of the internal and external shoulder rotators in major league baseball players. Am J Sports Med. 1988;16:577–585. doi: 10.1177/036354658801600604. [DOI] [PubMed] [Google Scholar]
- Burkhart SS, Morgan CD, Kibler WB. Shoulder injuries in overhead athletes. The ‘dead arm’ revisited. Clin Sports Med. 2000;19:125–158. doi: 10.1016/s0278-5919(05)70300-8. [DOI] [PubMed] [Google Scholar]
- Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology part I: pathoanatomy and biomechanics. Arthroscopy. 2003a;19:404–420. doi: 10.1053/jars.2003.50128. [DOI] [PubMed] [Google Scholar]
- Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology part III: The SICK scapula, scapular dyskinesis, the kinetic chain, and rehabilitation. Arthroscopy. 2003b;19:641–661. doi: 10.1016/s0749-8063(03)00389-x. [DOI] [PubMed] [Google Scholar]
- Chant CB, Litchfield R, Griffin S, et al. Humeral head retroversion in competitive baseball players and its relationship to glenohumeral rotation range of motion. J Orthop Sports Phys Ther. 2007;37:514–520. doi: 10.2519/jospt.2007.2449. [DOI] [PubMed] [Google Scholar]
- Cowgill LW. Humeral torsion revisited: a functional and ontogenetic model for populational variation. Am J Phys Anthropol. 2007;134:472–480. doi: 10.1002/ajpa.20689. [DOI] [PubMed] [Google Scholar]
- Crockett HC, Gross LB, Wilk KE, et al. Osseous adaptation and range of motion at the glenohumeral joint in professional baseball pitchers. Am J Sports Med. 2002;30:20–26. doi: 10.1177/03635465020300011701. [DOI] [PubMed] [Google Scholar]
- Dillman CJ. Proper mechanics of pitching. Sports Med Update. 1990;5:15–20. [Google Scholar]
- Dines JS, Frank JB, Akerman M, et al. Glenohumeral internal rotation deficits in baseball players with ulnar collateral ligament insufficiency. Am J Sports Med. 2009;37:566–570. doi: 10.1177/0363546508326712. [DOI] [PubMed] [Google Scholar]
- Edelson G. Variations in the retroversion of the humeral head. J Shoulder Elbow Surg. 1999;8:142–145. doi: 10.1016/s1058-2746(99)90007-1. [DOI] [PubMed] [Google Scholar]
- Edelson G. The development of humeral head retroversion. J Shoulder Elbow Surg. 2000;9:316–318. doi: 10.1067/mse.2000.106085. [DOI] [PubMed] [Google Scholar]
- Ellenbecker TS, Roetert EP, Piorkowski PA, et al. Glenohumeral joint internal and external rotation range of motion in elite junior tennis players. J Orthop Sports Phys Ther. 1996;24:336–341. doi: 10.2519/jospt.1996.24.6.336. [DOI] [PubMed] [Google Scholar]
- Ellenbecker TS, Roetert EP, Bailie DS, et al. Glenohumeral joint total rotation range of motion in elite tennis players and baseball pitchers. Med Sci Sports Exerc. 2002;34:2052–2056. doi: 10.1097/00005768-200212000-00028. [DOI] [PubMed] [Google Scholar]
- Evans FG, Krahl VE. The torsion of the humerus: a phylogenetic study from fish to man. Am J Anat. 1945;76:303–307. [Google Scholar]
- Fleisig GS, Andrews JR, Dillman CJ, et al. Kinetics of baseball pitching with implications about injury mechanisms. Am J Sports Med. 1995;23:233–239. doi: 10.1177/036354659502300218. [DOI] [PubMed] [Google Scholar]
- Fleisig GS, Barrentine SW, Escamilla RF, et al. Biomechanics of overhand throwing with implications for injuries. Sports Med. 1996;21:421–437. doi: 10.2165/00007256-199621060-00004. [DOI] [PubMed] [Google Scholar]
- Fleisig GS, Andrews JR, Cutter GR, et al. Risk of serious injury for young baseball pitchers: a 10-year prospective study. Am J Sports Med. 2011;39:253–257. doi: 10.1177/0363546510384224. [DOI] [PubMed] [Google Scholar]
- Gugenheim JJ, Jr, Stanley RF, Woods GW, et al. Little League survey: the Houston study. Am J Sports Med. 1976;4:189–200. doi: 10.1177/036354657600400501. [DOI] [PubMed] [Google Scholar]
- Hernigou P, Duparc F, Hernigou A. Determining humeral retroversion with computed tomography. J Bone Joint Surg Am. 2002;84-A:1753–1762. doi: 10.2106/00004623-200210000-00003. [DOI] [PubMed] [Google Scholar]
- Hill JA, Tkach L, Hendrix RW. A study of glenohumeral orientation in patients with anterior recurrent shoulder dislocations using computerized axial tomography. Orthop Rev. 1989;18:84–91. [PubMed] [Google Scholar]
- Hirashima M, Kudo K, Watarai K, et al. Control of 3D limb dynamics in unconstrained overarm throws of different speeds performed by skilled baseball players. J Neurophysiol. 2007;97:680–691. doi: 10.1152/jn.00348.2006. [DOI] [PubMed] [Google Scholar]
- Jobe CM, Pink MM, Jobe FW, et al. Anterior shoulder instability, impingement, and rotator cuff tear: theories and concepts. In: Jobe FW, editor. Operative Techniques in Upper Extremity Sports Injuries. St. Louis: Mosby; 1996. [Google Scholar]
- Keeley DW, Hackett T, Keirns M, et al. A biomechanical analysis of youth pitching mechanics. J Pediatr Orthop. 2008;28:452–459. doi: 10.1097/BPO.0b013e31816d7258. [DOI] [PubMed] [Google Scholar]
- Kibler WB, Chandler TJ, Livingston BP, et al. Shoulder range of motion in elite tennis players. Effect of age and years of tournament play. Am J Sports Med. 1996;24:279–285. doi: 10.1177/036354659602400306. [DOI] [PubMed] [Google Scholar]
- King J, Brelsford HJ, Tullos HS. Analysis of the pitching arm of the professional baseball pitcher. Clin Orthop Relat Res. 1969;67:116–123. [PubMed] [Google Scholar]
- Klingele KE, Kocher MS. Little League elbow: valgus overload injury in the paediatric athlete. Sports Med. 2002;32:1005–1015. doi: 10.2165/00007256-200232150-00004. [DOI] [PubMed] [Google Scholar]
- Krahl VE. The torsion of the humerus; its localization, cause and duration in man. Am J Anat. 1947;80:275–319. doi: 10.1002/aja.1000800302. [DOI] [PubMed] [Google Scholar]
- Krahl VE, Evans FG. Humeral torsion in man. Am J Phys Anthropol. 1945;3:229–253. [Google Scholar]
- Kronberg M, Brostrom LA, Soderlund V. Retroversion of the humeral head in the normal shoulder and its relationship to the normal range of motion. Clin Orthop Relat Res. 1990;253:113–117. [PubMed] [Google Scholar]
- Kvitne RS, Jobe FW. The diagnosis and treatment of anterior instability in the throwing athlete. Clin Orthop Relat Res. 1993;291:107–123. [PubMed] [Google Scholar]
- Larson SG. Subscapularis function in gibbons and chimpanzees: implications for interpretation of humeral head torsion in hominoids. Am J Phys Anthropol. 1988;76:449–462. [Google Scholar]
- Larson SG. Evolutionary transformation of the hominin shoulder. Evol Anthropol. 2007a;16:172–187. [Google Scholar]
- Larson SG. The definition of humeral torsion: a comment on Rhodes (2006) Am J Phys Anthropol. 2007b;133:819–820. doi: 10.1002/ajpa.20505. discussion 820–1. [DOI] [PubMed] [Google Scholar]
- Larson RL, Singer KM, Bergstrom R, et al. Little League survey: the Eugene study. Am J Sports Med. 1976;4:201–209. doi: 10.1177/036354657600400502. [DOI] [PubMed] [Google Scholar]
- Lordkipanidze D, Jashashvili T, Vekua A, et al. Postcranial evidence from early Homo from Dmanisi, Georgia. Nature. 2007;449:305–310. doi: 10.1038/nature06134. [DOI] [PubMed] [Google Scholar]
- Lyman S, Fleisig GS, Andrews JR, et al. Effect of pitch type, pitch count, and pitching mechanics on risk of elbow and shoulder pain in youth baseball pitchers. Am J Sports Med. 2002;30:463–468. doi: 10.1177/03635465020300040201. [DOI] [PubMed] [Google Scholar]
- Magnusson SP, Gleim GW, Nicholas JA. Shoulder weakness in professional baseball pitchers. Med Sci Sports Exerc. 1994;26:5–9. [PubMed] [Google Scholar]
- Martin CP. The cause of torsion of the humerus and of the notch on the anterior edge of the glenoid cavity of the scapula. J Anat. 1933;67:573–582. [PMC free article] [PubMed] [Google Scholar]
- McKern TW, Stewart TD. 1957. Skeletal age changes in young American males. Natick, MA: US Army Quartermaster Research & Development Command.
- Meister K. Injuries to the shoulder in the throwing athlete. Part one: Biomechanics/pathophysiology/classification of injury. Am J Sports Med. 2000a;28:265–275. doi: 10.1177/03635465000280022301. [DOI] [PubMed] [Google Scholar]
- Meister K. Injuries to the shoulder in the throwing athlete. Part two: evaluation/treatment. Am J Sports Med. 2000b;28:587–601. doi: 10.1177/03635465000280042701. [DOI] [PubMed] [Google Scholar]
- Olsen SJ, II, Fleisig GS, Dun S, et al. Risk factors for shoulder and elbow injuries in adolescent baseball pitchers. Am J Sports Med. 2006;34:905–912. doi: 10.1177/0363546505284188. [DOI] [PubMed] [Google Scholar]
- Osbahr DC, Cannon DL, Speer KP. Retroversion of the humerus in the throwing shoulder of college baseball pitchers. Am J Sports Med. 2002;30:347–353. doi: 10.1177/03635465020300030801. [DOI] [PubMed] [Google Scholar]
- Pappas AM, Zawacki RM, McCarthy CF. Rehabilitation of the pitching shoulder. Am J Sports Med. 1985;13:223–235. doi: 10.1177/036354658501300403. [DOI] [PubMed] [Google Scholar]
- Pappas AM, Zawacki RM, Sullivan TJ. Biomechanics of baseball pitching: A preliminary report. Am J Sports Med. 1985;13:216–222. doi: 10.1177/036354658501300402. [DOI] [PubMed] [Google Scholar]
- Pieper HG. Humeral torsion in the throwing arm of handball players. Am J Sports Med. 1998;26:247–253. doi: 10.1177/03635465980260021501. [DOI] [PubMed] [Google Scholar]
- Reagan KM, Meister K, Horodyski MB, et al. Humeral retroversion and its relationship to glenohumeral rotation in the shoulder of college baseball players. Am J Sports Med. 2002;30:354–360. doi: 10.1177/03635465020300030901. [DOI] [PubMed] [Google Scholar]
- Rhodes JA. Humeral torsion and retroversion in the literature: a reply to Larson. Am J Phys Anthropol. 2007;133:819–821. doi: 10.1002/ajpa.20505. [DOI] [PubMed] [Google Scholar]
- Ricci AR, Mason DE. Little League shoulder: case report and literature review. Del Med J. 2004;76:11–14. [PubMed] [Google Scholar]
- Scheuer L, Black S. Developmental Juvenile Osteology. New York: Elsevier Academic Press; 2000. [Google Scholar]
- Stein CJ, Micheli LJ. Overuse injuries in youth sports. Phys Sportsmed. 2011;38:102–108. doi: 10.3810/psm.2010.06.1787. [DOI] [PubMed] [Google Scholar]
- Torres RR, Gomes JL. Measurement of glenohumeral internal rotation in asymptomatic tennis players and swimmers. Am J Sports Med. 2009;37:1017–1023. doi: 10.1177/0363546508329544. [DOI] [PubMed] [Google Scholar]
- Wilk KE, Macrina LC, Fleisig GS, et al. Correlation of glenohumeral internal rotation deficit and total rotational motion to shoulder injuries in professional baseball pitchers. Am J Sports Med. 2011;39:329–335. doi: 10.1177/0363546510384223. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


