Abstract
To explore contemporary (from 1990) utilization and practice of electroconvulsive therapy (ECT) worldwide. Systematic search (limited to studies published 1990 and after) was undertaken in the databases Medline, Embase, PsycINFO, SveMed, and EBSCO/Cinahl. Primary data-based studies/surveys with reported ECT utilization and practice in psychiatric institutions internationally, nationally, and regionally; city were included. Two reviewers independently checked study titles and abstracts according to inclusion criteria, and extracted ECT utilization and practice data from those retrieved in full text. Seventy studies were included, seven from Australia and New Zealand, three Africa, 12 North and Latin America, 33 Europe, and 15 Asia. Worldwide ECT differences and trends were evident, average number ECTs administered per patient were eight; unmodified (without anesthesia) was used in Asia (over 90%), Africa, Latin America, Russia, Turkey, Spain. Worldwide preferred electrode placement was bilateral, except unilateral at some places (Europe and Australia/New Zealand). Although mainstream was brief-pulse wave, sine-wave devices were still used. Majority ECT treated were older women with depression in Western countries, versus younger men with schizophrenia in Asian countries. ECT under involuntary conditions (admissions), use of ambulatory-ECT, acute first line of treatment, as well as administered by other professions (geriatricians, nurses) were noted by some sites. General trends were only some institutions within the same country providing ECT, training inadequate, and guidelines not followed. Mandatory reporting and overall country ECT register data were sparse. Many patients are still treated with unmodified ECT today. Large global variation in ECT utilization, administration, and practice advocates a need for worldwide sharing of knowledge about ECT, reflection, and learning from each other's experiences.
Keywords: Electroconvulsive therapy, epidemiology, health care surveys, mental disorders, review, systematic
Introduction
Convulsive interventions have been used to treat mental disorders since the 16th century and even today in the form of electroconvulsive therapy (ECT). Ugo Cerletti and Luigi Bini demonstrated ECT in Rome for the first time in 1938 (Cerletti and Bini 1938). The ECT intervention per se, that is, the application of electrical current to the scalp in order to provoke a generalized epileptic seizure, for the purpose of alleviating psychotic and depressive symptoms, is still much the same today as it was in the beginning. Modifications of Cerletti and Bini's original bitemporal placement of electrodes to the scalp, administering 120 V sine-wave electrical current to the head (Cerletti and Bini 1938), include the development of newer brief-pulse electrical current wave devices and unilateral (UL) placement of electrodes.
ECT was originally used in the treatment of schizophrenia. ECTs effectiveness for patients with depression was established in 1941 (Hemphill and Walter 1941). The use of ECT declined in the 1970s and 1980s after the introduction of pharmacotherapy for severe mental disorders (McCall 2001). The main indication for ECT also transformed from first-line to last-resort treatment for medication-resistant and very severe life-threatening clinical conditions (McCall 2001; Eranti and McLoughlin 2003). However, in 2001, guidelines developed by the American Psychiatric Association (APA) advised that ECT should not only be used as a last resort (American Psychiatric Association 2001). Situations of increased risk that need special attention are mentioned by international guidelines, such as patients with disorders of the central nervous system, cardiovascular and respiratory system (American Psychiatric Association 2001; Royal College of Psychiatrists 2005; Enns et al. 2010). As a result of cognitive side effects (memory impairment) association with sine-wave current (The UK ECT Review Group 2003), it is now advised that brief-pulse wave be the standard treatment (American Psychiatric Association 2001; Royal College of Psychiatrists 2005; Enns et al. 2010). The use of sine-wave constant voltage and constant energy devices is currently not considered justified (APA guidelines) (American Psychiatric Association 2001).
ECT spread rapidly from Europe to other continents and to the United States, due to the Second World War's displacement of psychiatrists (Shorter 2009). In the beginning, ECT was administered without anesthesia (termed unmodified ECT) and later, under anesthesia together with muscle relaxant succinylcholine medication (termed modified ECT), in order to reduce side effects from the convulsions, such as bone fractures, teeth, tendon, and muscular damage. In the last decade, modified ECT has been recommended as the standard routine according to internationally established guidelines (American Psychiatric Association 2001; Royal College of Psychiatrists 2005; Enns et al. 2010).
ECT's mode of action has still not been clarified (Fink 2001). Despite documented efficacy for alleviating symptoms of depression (The UK ECT Review Group 2003), ECT still remains controversial and stigma-bound. Reported side effects, such as memory impairment (Rose et al. 2003), and whether ECT induces long-term permanent cognitive impairment remains yet obscure.
Worldwide, it has been estimated that about one million patients receive ECT annually (Prudic et al. 2001). ECT appears to have become a widely available treatment for mental disorders on all continents (Swartz 2009), in USA/Canada and Latin America (Magid and Rohland 2009; Rosa and Rosa 2009), Western Europe (Benbow and Bolwig 2009; Sienaert and van den Broek 2009) and Russia (Nelson and Giagou 2009), Africa and Asia (Chang 2009). Despite international guidelines (American Psychiatric Association 2001; Royal College of Psychiatrists 2005; Enns et al. 2010), large variations in clinical practice between countries and regions have been reported (Hermann et al. 1995; Glen and Scott 2000; Bertolin-Guillen et al. 2006; Gazdag et al. 2009a). Reports on ECT utilization also largely vary. There have been some international studies. A study by Van Waarde et al. (van Waarde et al. 2009) included data from nine other countries and another by Gazdag et al. (Gazdag et al. 2009a) presented an overview of 13 surveys undertaken on the use of ECT in the past 10 years. In the United States, the nationwide number of persons ECT treated per 10,000 resident population per year, was estimated to be 4.9 in 1995 (Hermann et al. 1995). On the whole, there seems to be a paucity of updated ECT utilization surveys, reviews, and data. There is, therefore, an imminent need for a systematic international review concerning contemporary use of ECT. Against this background, the main objective of this article is to give a systematic contemporary overview (from 1990) of the extent to which ECT is used worldwide.
Briefly the following aspects were considered. ECT utilization: ECT rates according to population, administration frequency, and inpatient prevalence rates; ECT parameters: the manner in which ECT is applied (modified or unmodified, brief-pulse or sine-wave current, device type, electrode placement bilateral [BL] or unilateral [UL]); and ECT practice: diagnoses, indications, gender, age, conditions (consent or involuntary), settings (ambulatory), under which ECT is applied.
Material and Methods
Data sources and search strategy
A systematic literature search was undertaken in the following databases. Medline, Embase, PsycINFO, SveMed and EBSCO/Cinahl, limited from 1990 to November 2010 (Appendix A, Table 1). Search terms intended for Medline were adapted as required for other databases. Terms used were “electroconvulsive therapy,”“electroshock,”“electroconvulsive,”“ECT,” combined with any of the following “use,”“utilization,”“practice,”“survey,”“statistical data,”“frequency,” limited to human studies and dating from 1990 to today. Relevant references, known to authors of this review published on governmental internet sites or from newly published text books (Swartz 2009) or reference lists in retrieved included papers, were also hand found.
Table 1.
Overview of included studies (N= 70) according to continent, country, region, city, or local hospital level.
| Country | Land (L)/Region (R)/City (C)/Hospital (H) | Publication year | First author (reference) |
|---|---|---|---|
| Australia and New Zealand (N= 7) | |||
| Australia | L | 2007 | Chanpattana W (Chanpattana 2007) |
| New Zealand | L | 2006 | Ministry of Health (Ministry of Health 2006) |
| New Zealand | L | 2005 | Ministry of Health (Ministry of Health 2005) |
| Australia and New Zealand | L | 1991 | O’Dea JF (O’Dea et al. 1991) |
| Victoria, Australia | R | 2003 | Wood DA (Wood and Burgess 2003) |
| Western Australia | R | 2005 | Teh SPC (Teh et al. 2005) |
| Sydney, New South Wales Australia | C | 2011 | Lamont S (Lamont et al. 2011) |
| Africa (N= 3) | |||
| Malawi | L | 2008 | Selis MA (Selis et al. 2008) |
| South Africa | H | 1991 | Mugisha RX (Mugisha and Ovuga 1991) |
| Nigeria | H | 1985 | Sijuwola OA (Sijuwola 1985) |
| North and Latin America (N= 12) | |||
| USA | L | 1995 | Hermann RC (Hermann et al. 1995) |
| USA, tri-state New York City Metropolitan region | L | 2001 | Prudic J (Prudic et al. 2001) |
| Latin America and the Caribbean | L | 1996 | Levav I (Levav and Gonzalez 1996) |
| California, USA | R | 1999 | Kramer BA (Kramer 1999) |
| Texas, USA | R | 2000 | Scarano VR (Scarano et al. 2000) |
| Texas, USA | R | 1998 | Reid WH (Reid et al. 1998) |
| USA (Medicare) | R | 1997 | Rosenbach ML (Rosenbach et al. 1997) |
| North Carolina, USA | R | 1995 | Creed P (Creed et al. 1995) |
| Louisiana, USA (Medicare) | C | 1997 | Westphal JR (Westphal,et al. 1997) |
| North Carolina, USA | H | 1992 | McCall WV (McCall et al. 1992) |
| South West Pennsylvania, State Hospital, USA | H | 2000 | Sylvester AP (Sylvester et al. 2000) |
| Rio de Janeiro, Brazil | H | 2008 | Pastore DL (Pastore et al. 2008) |
| Europe (N= 33) | |||
| Belgium | L | 2006 | Sienaert P (Sienaert et al. 2006) |
| England | L | 2007 | Department of Health (http://www.dh.gov.uk) (Department of Health 2007) |
| Hungary | L | 2004 | Gazdag G (Gazdag et al. 2004a) |
| Poland | L | 2009 | Gazdag G (Gazdag et al. 2009a) |
| Germany | L | 1998 | Muller U (Muller et al. 1998) |
| Spain | L | 2006 | Bertolin-Guillen JM (Bertolin-Guillen,et al. 2006) |
| Russia | L | 2005 | Nelson AI (Nelson 2005) |
| Netherlands | L | 2009 | van Waarde JA (van Waarde et al. 2009) |
| France | L | 2001 | Benadhira R (Benadhira and Teles 2001) |
| Denmark | L | 2002 | Andersson JE (Andersson and Bolwig 2002) |
| Denmark | L | 2010 | Sundhedsstyrelsen (Sundhedsstyrelsen 2011) |
| Norway | L | 2011 | Schweder LJ (Schweder et al. 2011a) |
| Norway | L | 2011 | Schweder LJ (Schweder et al. 2011b) |
| Sweden | L | 2010 | Socialstyrelsen (http://www.socialstyrelse.se) (Socialstyrelsen 2010) |
| Belgium | R | 2005 | Sienaert P (Sienaert et al. 2005a) |
| Wales | R | 1999 | Duffett R (Duffett et al. 1999) |
| England | R | 1998 | Duffett R (Duffett and Lelliott 1998) |
| England | R | 1992 | Pippard J (Pippard 1992) |
| Ireland | R | 2010 | Enriquez S (Enriquez et al. 2010) |
| Chuvash republic, Russia | R | 2010 | Golenkov A (Golenkov et al. 2010) |
| Vienna, Austria | C | 1997 | Tauscher J (Tauscher et al. 1997) |
| Barcelona, Spain | C | 1996 | Bernardo M (Bernardo et al. 1996) |
| London (UK) and Bengaluru, India | C | 2011 | Eranti SV (Eranti et al. 2011) |
| Edinburgh, Scotland | C | 1999 | Glen T (Glen and Scott 1999) |
| Edinburgh, Scotland | C | 2008 | Okagbue N (Okagbue et al. 2008) |
| Munich, Germany | C | 2005 | Baghai TC (Baghai et al. 2005) |
| Dikemark Hospital, Oslo, Norway | H | 2010 | Moksnes KM (Moksnes and Ilner 2010) |
| Ullevaal University Hospital, Oslo, Norway | H | 2006 | Moksnes KM (Moksnes et al. 2006) |
| Hospital Innland, Norway | H | 2010 | Eiring O (Eiring 2010) |
| Pitkaniemi Hospital, Finland | H | 2000 | Huuhka MJ (Huuhka et al. 2000) |
| Hospital, Turkey | H | 2008 | Saatcioglu O (Saatcioglu and Tomruk 2008) |
| Scotland | H | 2004 | Fergusson GM (Fergusson et al. 2004) |
| Cukurova University Psychiatry Service, Turkey | H | 2003 | Zeren T (Zeren et al. 2003) |
| Asia (N= 15) | |||
| Japan | L | 2004 | Motohashi N (Motohashi et al. 2004) |
| Japan | L | 2005 | Chanpattana W (Chanpattana et al. 2005a) |
| Thailand | L | 2004 | Chanpattana W (Chanpattana and Kramer 2004) |
| Asia | L | 2003 | Little JD (Little 2003) |
| Asia | L | 2010 | Chanpattana W (Chanpattana et al. 2010) |
| Katmandu, Nepal | C | 2008 | Ahikari SR (Ahikari et al. 2008) |
| Hong Kong | C | 2003 | Chung KF (Chung 2003) |
| Hong Kong | C | 2003 | Chung KF (Chung et al. 2003) |
| India | H | 2005 | Chanpattana W (Chanpattana et al. 2005b) |
| Chulalongkorn Memorial Hospital, Thailand | H | 2005 | Lalitanatpong D (Lalitanatpong 2005) |
| Local psychiatric unit, Hong Kong | H | 2009 | Chung JPY (Chung et al. 2009) |
| Tokushima, University Hospital, Japan | H | 2000 | Ishimoto Y (Ishimoto et al. 2000) |
| Hospital, Saudi Arabia | H | 1999 | Alhamad AM (Alhamad 1999) |
| Hospital, Karachi, Pakistan | H | 2005 | Naqvi H (Naqvi and Khan 2005) |
| Al Ain, United Arab Emirates | H | 1998 | Tewfik KD (Tewfik et al. 1998) |
Inclusion and exclusion criteria
Inclusion criteria: Data-based observational studies or surveys with reported ECT utilization, frequency, or prevalence rates, by data collected from 1990 and above, for patients in psychiatric establishments (inpatients or outpatients) in well-defined continents, countries, regions, cities, or local hospitals. Also included were relevant studies published near the date limits for this study (from 1990), for geographical areas that had few pertinent publications.
Studies in the following languages were included: English, Scandinavian (Norwegian, Swedish, Danish), and European (German, French, Spanish, Portuguese, Turkish). In addition to authors’ European language fluency, the online Google translation tool (http://translate.google.com/) was used when needed (e.g., for Portuguese and Turkish).
Following exclusion criteria were included. Not data-based study or survey, no or unclear report of ECT utilization, frequency, prevalence rate, practice, in unclearly defined populations. All report of utilization frequency, prevalence rates of ECT in selected samples or subgroups (e.g., young/adolescent, elderly) or special populations (such as pregnancy, disability, mental retardation), and qualitative studies about clinician or physician subjective experience (views or opinions) on ECT.
Screening of literature
Two reviewers (KAL, BH) independently checked the titles, and where available, the abstracts of the studies identified by the electronic database searches. All references appearing to meet inclusion criteria, including those with insufficient details, were requested in full text. All reviewers (KAL, LJVS, BH) consisting of two pairs independently extracted data from the retrieved full-text articles according to a premade data extraction scheme. All discrepancies were resolved by consensus meeting/discussion, and the final decision was made by the first author (KAL).
Data extraction and data analyses
Where possible, utilization data have been presented as either (1) number of persons ECT treated per 10,000 resident population per year, that is, treated person rate (TPR), (2) number of ECT administrations per 10,000 resident population per year, that is, ECT administration rate (EAR), (3) the proportion in percent (%) of ECT-treated patients among the inpatient (psychiatric ward, hospital admitted) population, that is, inpatient prevalence (iP%), and (4) average number of ECTs administered per patient (in a series or course), that is, average ECT number (AvE). Information about ECT parameters, diagnoses and main indications, gender and age is also presented. Other information such as ethnicity, education, side effects, mortality, adverse events, use of written consent, involuntary conditions has also been noted.
Results
Study selection
The study selection process, databases searched and total numbers of references identified (N= 1403), title and abstract screened (N= 851), full-text screened (N= 101), included for data extraction (N= 70) and full text excluded (N= 31) references are given in Figure 1.
Figure 1.
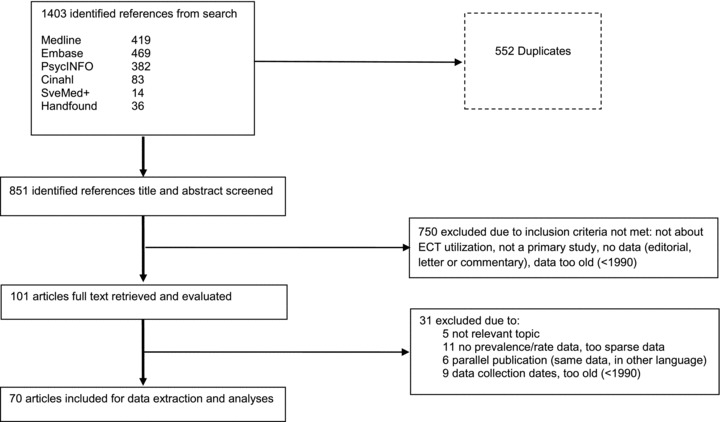
Flow chart of study-selection process.
Description of studies
Overview of included studies (N= 70) and data extracted is given in Table 1, sorted according to the continents: Australia and New Zealand (N= 7), Africa (N= 3), North and Latin America (N= 12), Europe (N= 33), and Asia (N= 15). Each reference was categorized according to the data presented, whether it represented the Land (n= 27), Region (n= 13), City (n= 11), or Hospital (n= 19).
Overview of full text excluded references (N= 31) and reasons for exclusion are given in Appendix B. Five references were found not relevant in topic, 10 had no rate or prevalence data or insufficient/too sparse data, six were parallelly published in other languages than English or not possible to find/full-text retrieve, and the data in nine were evaluated too old, collected before 1990.
Detailed summery of findings tables of included full-text studies are presented in Appendix C, Tables C1–C5 according to the five continents: (1) Australia and New Zealand, (2) Africa, (3) North and Latin America, (4) Europe and (5) Asia.
Seven studies were included from Australia and New Zealand, including a recent one from Sydney (Lamont et al. 2011). Only three of six studies from Africa were included, representing Malawi, Nigeria, and South Africa. The three excluded (Appendix B) were two from Nigeria and one from Egypt, due to data being too old (before 1990), insufficient, and sparse. One of the two included studies from Latin America, claimed representation of 17 Latin American and four Caribbean countries, but with unstated names except for Haiti being excluded (Levav and Gonzalez 1996). Two of the 10 studies from North America represented Medicare populations (Rosenbach et al. 1997; Westphal et al. 1997) leaving many of all USA's 50 States not represented. A study by the National Institute of Mental Health (NIMH) was found too old (Thompson et al. 1994). Altogether, 33 studies were included from Europe and nine were from the Nordic countries. Twelve identified European studies, including one study from Italy (Lucca et al. 2010), did not meet inclusion criteria (Appendix B). Surveys including a number of countries were identified from Asia (Little 2003; Chanpattana and Kramer 2004; Chanpattana et al. 2010) and 15 studies from this continent were included. ECT practice was verified from 27 Asian countries: Bangladesh, China, Hong Kong, India, Indonesia, Iran, Iraq, Israel, Japan, Jordan, South Korea, Malaysia, Myanmar, Nepal, Oman, Pakistan, Philippines, Singapore, Sri Lanka, Thailand, Turkey, United Arab Emirates, Vietnam (Chanpattana et al. 2010), Fiji, Kiribati, Solomon Islands (Little 2003), and Saudi Arabia (Alhamad 1999). ECT was reported not available in all countries, such as Bhutan, Brunei, Cambodia, Georgia, Laos, and Lebanon (Chanpattana et al. 2010), Micronesia and Palau (Little 2003). The countries Cyprus, Macoa, Qatar, and Maldives had also been excluded by a survey (Chanpattana et al. 2010).
Overall, the included studies displayed a large heterogeneity in the presentation of rate and prevalence data and practice of ECT worldwide. On a global basis, a crude estimate (from numbers given in Appendix C, Tables C1–C5) of worldwide contemporary TPR (SD) (age < 65 years) was 2.34 (1.56); EAR (SD), 11.2 (9.0); iP (SD) 6.1 (6.9); and AvE (SD) 8 (1.4). Globally, under half of all psychiatric institutions within the same country provided ECT. Main findings of ECT utilization, parameters, and practice from the five continents are presented below.
ECT Utilization
Treated person rate
Overview of TPR from all countries providing such data is illustrated in Figure 2.
Figure 2.
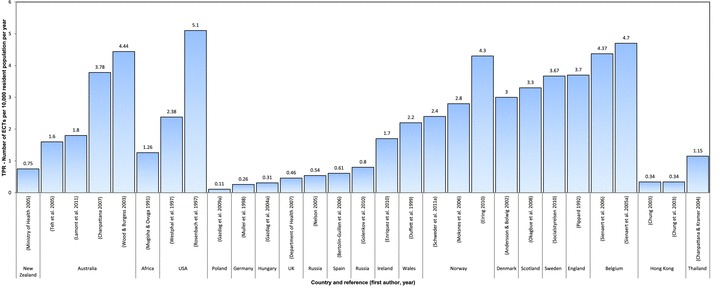
Worldwide Treated Person Rates (TPR)—number of ECTs per 10,000 resident population per year. [Correction added after first online publication on 20 March 2012: The TPR column for UK (Department of Health 2007) has been changed to 1.84.]
TPR (Fig. 2) varied from 0.75 in New Zealand (Ministry of Health 2005) to 4.4 in Victoria, Australia (Teh et al. 2005). TPR in the USA Medicare population was 5.1 (5.7 women; 3.6 men) (Rosenbach et al. 1997). TPR by age groups (and therefore not included in Fig. 2) ranged from 0.0001 (<18 years) to 3.8 (>65 years) in California (Kramer 1999). TPR for the elderly (>65 years) in the Medicare population was from 2.4 to 4.2, (Rosenbach et al. 1997; Westphal et al. 1997) and varied from 3.8 West USA to 6.1 in the Northeast, as well as between rural (TPR 3.2) to large urban areas (TPR 6.0) (Rosenbach et al. 1997). TPR variations within the same State were reported from Louisiana, TPR (>65 years): 2.8 urban parishes versus 1.9 rural parishes (Westphal et al. 1997).
TPR in Europe varied between countries and regions and between individual centers (Fig. 2), with the lowest TPR 0.11 in Poland (Gazdag et al. 2009a). The within-country regional variation in Belgium (TPR 2.6–10.6) was reported as significant (Sienaert et al. 2006), which was also the case for Norway (TPR 1.83–3.44) (Schweder et al. 2011a). In South Africa, TPR was 1.26 (Mugisha and Ovuga 1991). In Asia, TPR was only reported from Thailand 1.15 (Chanpattana and Kramer 2004) and Hong Kong ranging 0.27–0.34 (Chung 2003; Chung et al. 2003; Chanpattana et al. 2010).
Inpatient prevalence
Overview of iP from all countries providing such data is illustrated in Figure 3.
Figure 3.
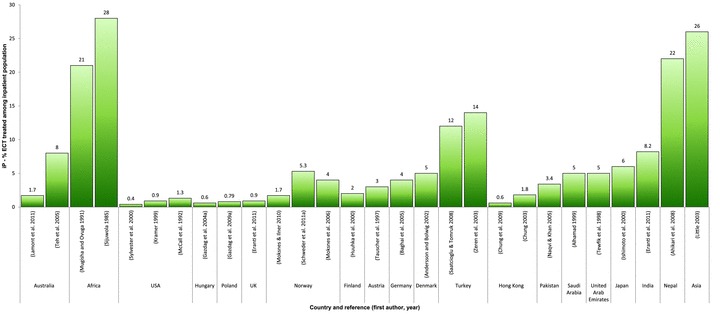
Inpatient prevalence rate (iP%)—percent of ECT-treated patients among inpatient population.
The iP was highest in Africa 21–28% (Mugisha and Ovuga 1991; Selis et al. 2008), Nepal 22%, (Ahikari et al. 2008), and overall in Asia estimated between <9% and 26% (Little 2003). In the United States, iP was lowest, from 0.4% to 1.3% (McCall et al. 1992; Sylvester et al. 2000), similar to Hong Kong was 0.6–1.8% (Chung 2003; Chung et al. 2009). In Australia, iP ranged from 1% to 8% (Wood and Burgess 2003; Teh et al. 2005), and in Europe from 0.6% (Hungary) (Gazdag et al. 2004a) to 14% (Turkey) (Zeren et al. 2003).
Average ECT number
The AvE in New Zealand and Australia ranged from seven to 12 (O’Dea et al. 1991; Ministry of Health 2006; Chanpattana 2007), in Africa from one to 10, (Sijuwola 1985; Selis et al. 2008), in USA from five (Reid et al. 1998; Kramer 1999) to 12 (Sylvester et al. 2000), USA overall seven to eight (Rosenbach et al. 1997; Scarano et al. 2000; Prudic et al. 2001), and in Brazil eight (Pastore et al. 2008) (Appendix C, Tables C1–C5). AvE in Europe ranged from five (Glen and Scott 1999) to 11 (Sundhedsstyrelsen 2011a), except Sweden where it was one to 22 (Socialstyrelsen 2010). AvE in Pakistan was one to 20 (Naqvi and Khan 2005), in Nepal two to 16 (Ahikari et al. 2008), and generally in Asia between six and eight.
ECT Parameters
Unmodified and modified
All parameter report in Australia and New Zealand indicated modified ECT (O’Dea et al. 1991; Ministry of Health 2005; Chanpattana 2007; Lamont et al. 2011), similarly in the United States (Reid et al. 1998; Scarano et al. 2000; Prudic et al. 2001). ECT in Africa was generally administered unmodified and in Malawi modified after 2007 (Mugisha and Ovuga 1991; Selis et al. 2008). A study excluded from Nigeria reported modified ECT administered in 1979, but found too expensive (Odejide et al. 1987).
In Europe, all parameter report indicated modified ECT, except for Russia (in contrast to Hungary [Gazdag et al. 2004a], with obligatory anesthesia) where >80% was unmodified (Nelson 2005). In the Chuvash Republic, ECT was modified, but 40% without use of muscle relaxants (and administered mainly to women with schizophrenia) (Golenkov et al. 2010). In Spain, 0.6% received unmodified ECT, and 2.3% without muscle relaxants (Bertolin-Guillen et al. 2006).
A large survey in Asia with 23 countries investigated reported 129,906 unmodified ECTs administered to 22,194 patients (55.7%) at 141 (54.9%) institutions in 14 countries (61%) (Chanpattana et al. 2010). Two-thirds of patients were treated unmodified in Japan (1997–1999) (Motohashi et al. 2004), and 20% of all institutions administered only unmodified, with only sine-wave approved devices. In a later survey from Japan (2001–2003), unmodified comprised 57% of all administered ECTs (Chanpattana et al. 2005a). Patients selected for modified (with anesthesia) in Japan were mainly elderly or with medical conditions (Motohashi et al. 2004). In Thailand, almost all (94%) ECT administration was unmodified (Chanpattana and Kramer 2004). In India, both modified and unmodified ECT was administered (Chanpattana et al. 2005b), 52% of patients received unmodified at 50% of all institutions, and 30% of institutions administered only unmodified.
Overall in Asia, only 45% of facilities used modified ECT exclusively (Chanpattana et al. 2010), in Hong Kong 87% modified (Chung et al. 2003), and the Asian Pacific Region (Little 2003) and Katmandu, Nepal, used only modified (Ahikari et al. 2008). Eight facilities in Asia reported succinylcholine muscle relaxant used routinely without anesthesia (Chanpattana et al. 2010). Anesthesia was also used without muscle relaxants in Japan, and extreme motion from the convulsions held down with aid of assistants restraining patient's shoulders, arms, and thighs (Ishimoto et al. 2000).
Overall, 26% Latin American countries used unmodified ECT (Levav and Gonzalez 1996), except for all modified in Rio de Janeiro, Brazil and one country in the Caribbean (Levav and Gonzalez 1996; Pastore et al. 2008).
Placement and devices
On a worldwide scale, BL placement was the preferred electrode placement. However, UL placement was the first main choice in Australia and New Zealand (O’Dea et al. 1991; Ministry of Health 2005; Chanpattana 2007; Lamont et al. 2011), likewise to several European countries such as Vienna (Tauscher et al. 1997), Munich (Baghai et al. 2005), Netherlands (van Waarde et al. 2009), and Norway (Schweder et al. 2011b).
In the United States, there was some sine wave (2%) (Prudic et al. 2001) and some UL (16–21%) (Reid et al. 1998; Scarano et al. 2000; Prudic et al. 2001) report, but BL placement (73–79%) and brief-pulse wave current (Reid et al. 1998; Scarano et al. 2000; Prudic et al. 2001) was mainstream. Similarly, brief-pulse wave current devices were dominant in Europe, except sine-wave current still used in Spain 14% (Bertolin-Guillen et al. 2006), Russia 26% (Nelson 2005), Belgium 34% (Sienaert et al. 2006), Poland 30% (Gazdag et al. 2009a), Germany 39% (Muller et al. 1998), and Hungary 52% (Gazdag et al. 2004a).
Overall electrode placement in Asia was BL (77%) (Chanpattana et al. 2010). Thailand (Chanpattana and Kramer 2004) and Japan (Motohashi et al. 2004) reported only the use of BL and India always reported the use of BL in 82% (Chanpattana et al. 2005b). In Asia, 58% of institutions used brief-pulse devices and 42% sine wave (Chanpattana et al. 2010). In Japan, the device type was often Japanese-produced Sakai C1, but also some had Thymatron® DGx devices (Somatics, Inc., http://www.thymatron.com) (Chanpattana et al. 2005a). In India, a diversity of devices was in use, including locally made (Chanpattana et al. 2005b). In Katmandu, Nepal, device type was only brief pulse (Ahikari et al. 2008).
ECT Practice
Provision of ECT and training
In Australia, ECT was provided by 66% institutions and ECT training by 73% (Chanpattana 2007).
In the tri-state New York City metropolitan region, 55% of institutions provided ECT (Prudic et al. 2001), 33% in Texas (Reid et al. 1998), and 44% of all psychiatric hospitals in North Carolina (Creed et al. 1995). A decrease from 1990 to 1994 in provision of ECT was reported in California and ECT provided by public institutions to be very low, <6% (Kramer 1999).
In Europe, ECT provision in the Netherlands was 23% (van Waarde et al. 2009), Belgium nationwide 22% (Sienaert et al. 2006), Flanders and Brussels capital region 26% (Sienaert et al. 2005a), Poland 34% (Gazdag et al. 2009a), Spain and Russia 46% (Nelson 2005; Bertolin-Guillen et al. 2006), France 51% (Benadhira and Teles 2001), Hungary 57% (Gazdag et al. 2004a), Germany 59% (Muller et al. 1998), Norway 72% (Schweder et al. 2011a), and in Denmark 100% (Andersson and Bolwig 2002). In Norway, patients had to wait up to eight weeks for treatment due to a low capacity in administrating ECT (Schweder et al. 2011b).
ECT was mainly performed by junior doctors in Denmark (Andersson and Bolwig 2002), England (Duffett and Lelliott 1998), and Norway (Schweder et al. 2011b). In Norway, 6% of ECTs were administered by nurses (Schweder et al. 2011b) and in the Netherlands sometimes by geriatricians or physicians (van Waarde et al. 2009). About one-third of clinics in England had developed clear policies to help guide junior doctors in administering ECT effectively (Duffett and Lelliott 1998). ECT teaching programs were found at 59% of institutions in India (Chanpattana et al. 2005b), and 78% in Japan, but rated in 10% as fair to poor (Chanpattana et al. 2005a). Acceptable ECT training in Thailand was only found for five hospitals (Chanpattana and Kramer 2004). In Saudi Arabia, a two-lecture course on ECT was given every year for junior doctors, as well as practical demonstration and training (Alhamad 1999).
Diagnoses and diagnostic indication
Main diagnoses, diagnostic indication for ECT in Australia, New Zealand, USA, South America, and Africa, are illustrated in Figure 4.
Figure 4.
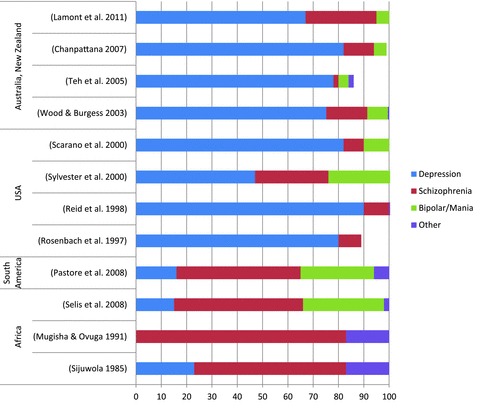
Diagnoses and ECT in Australia, New Zealand, USA, South America, Africa.
Affective disorder (unipolar/bipolar depression) was the main diagnoses in Australia and New Zealand (O’Dea et al. 1991; Wood and Burgess 2003; Teh et al. 2005; Chanpattana 2007; Lamont et al. 2011), but other main indications for administering ECT were also noted (Lamont et al. 2011), such as being too distressed to await drug response, patient preference, previous response, life saving, and medication resistance. Affective disorders (unipolar/bipolar depression) were also the main diagnoses in USA (72–92%), and schizophrenia and/or schizoaffective disorders were much less (8–29%) (McCall et al. 1992; Hermann et al. 1995; Rosenbach et al. 1997; Reid et al. 1998; Scarano et al. 2000; Sylvester et al. 2000; Prudic et al. 2001). However in Africa, the main diagnoses were schizophrenia and psychotic conditions (60–83%) (Sijuwola 1985; Mugisha and Ovuga 1991; Selis et al. 2008), and in Brazil 49% of cases reported same conditions (Pastore et al. 2008).
Main diagnoses, diagnostic indication for ECT in Europe, are illustrated in Figure 5.
Figure 5.
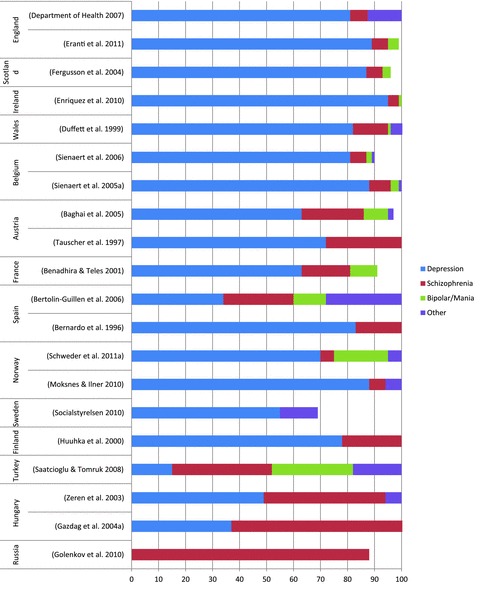
Diagnoses and ECT in Europe.
Although affective disorders (unipolar and/or bipolar depression with or without psychosis) were the most prominent in Europe (Fig. 5), schizophrenia and/or schizoaffective disorder were major in Hungary 64%, Chuvash Republic 88%, and Turkey 37% (Gazdag et al. 2004a; Saatcioglu and Tomruk 2008; Golenkov et al. 2010).
Schizophrenia and/or schizoaffective disorder were much less common in Belgium 5% (Sienaert et al. 2006), Norway 5% (Schweder et al. 2011a), Ireland 4% (Enriquez et al. 2010), and Scotland 5% (Fergusson et al. 2004). ECT for mania varied from 0.2% (Munich) (Baghai et al. 2005) to 12% (Spain) (Bertolin-Guillen et al. 2006). The main indication for ECT was medication resistance, but also life saving, catatonia, previous good response, and patient preference (Muller et al. 1998; Duffett et al. 1999; Zeren et al. 2003; Schweder et al. 2011a). ECT administered under pregnancy was noted at 10 Polish sites (Gazdag et al. 2009a) and in Spain (Bertolin-Guillen et al. 2006).
Main diagnoses, diagnostic indication for ECT in Asia, are illustrated in Figure 6.
Figure 6.

Diagnoses and ECT in Asia.
Main diagnostic indication in Asia overall (Little 2003; Chanpattana and Kramer 2004; Chanpattana et al. 2005b, 2010) was schizophrenia (Ishimoto et al. 2000; Motohashi et al. 2004; Chanpattana et al. 2005a). However, in Saudi Arabia (Alhamad 1999), Pakistan (Naqvi and Khan 2005), and Hong Kong (Chung et al. 2009), depressive illness was the main indication (over 60%). Reasons for giving ECT to patients with schizophrenia (74%) in Thailand was small budget for mental health care and no antipsychotics included in the essential drug list from the Ministry of Health (Chanpattana and Kramer 2004). In India, ECT was prescribed to other diagnoses, including drug abuse (Chanpattana et al. 2005b). Indication for ECT in Asia was also severe violence, suicide and refractory treatment (Lalitanatpong 2005), need of rapid improvement (Ishimoto et al. 2000), drug resistance, or life-threatening situation (Naqvi and Khan 2005), and in Saudi Arabia 35% as first-choice emergency treatment (Alhamad 1999).
Gender, age, and ethnicity
An overview of studies presenting gender and age data is given in Table 2.
Table 2.
Overview of ECT treatment worldwide by gender and age.
| Age in years | |||||
|---|---|---|---|---|---|
| Country | First author (reference) | Percent of ECT-treated women | %N >65 (%) | Mean | Range |
| Australia and New Zealand | |||||
| Sydney, Australia | Lamont (Lamont et al. 2011) | 71 | 28 | ||
| New Zealand | Ministry of Health (Ministry of Health 2006) | 69 | 40 (2004/2005) | ||
| Western Australia | Teh (Teh et al. 2005) | 65 | |||
| Australia | Chanpattana (Chanpattana 2007) | 63 | 38 | ||
| Victoria, Australia | Wood (Wood and Burgess 2003) | 63 | 33 | ||
| Africa | |||||
| Malawi | Selis (Selis et al. 2008) | 49 | 17–35 | ||
| South Africa | Mugisha (Mugisha and Ovuga 1991) | 29 | 30.7 | ||
| North America | |||||
| Louisiana | Westphal (Westphal et al. 1997) | 79 | 100 | ||
| Pennsylvania | Sylvester (Sylvester et al. 2000) | 71 | 59 (>60) | ||
| Texas | Reid (Reid et al. 1998) | 70 | 48 | ||
| Texas | Scarano (Scarano et al. 2000) | 69 | |||
| California | Kramer (Kramer 1999) | 69 | |||
| USA | Rosenbach (Rosenbach et al. 1997) | 66 | |||
| USA | Prudic (Prudic et al. 2001) | 55 (>60) | |||
| North Carolina | McCall (McCall et al. 1992) | 44.3 | 19–75 | ||
| South America | |||||
| Brazil | Pastore (Pastore et al. 2008) | 71 | 41.3 | ||
| Europe | |||||
| Austria | Tauscher (Tauscher et al. 1997) | 81 | 49 | 23–69 | |
| Finland | Huuhka (Huuhka et al. 2000) | 76 | 58.9 | 18–83 | |
| Norway | Moksnes (Moksnes and Ilner 2010) | 74 | 64 | 29–87 | |
| UK | Department of Health (Department of Health 2007) | 71 | 46 | ||
| Wales | Duffett (Duffett et al. 1999) | 71 | 56.9 (women) | ||
| 55.5 (men) | |||||
| Scotland | Glen (Glen and Scott 1999) | 71 | |||
| London, UK | Eranti (Eranti et al. 2011) | 70 | 62.8 | ||
| Scotland | Fergusson (Fergusson et al. 2004) | 70 | 26 | ||
| Norway | Moksnes (Moksnes et al. 2006) | 69 | 67 (women) | 23–91 | |
| 65 (men) | |||||
| Ireland | Enriquez (Enriquez et al. 2010) | 66 | 50.6 | 18–87 | |
| Munich | Baghai (Baghai et al. 2005) | 66 | 51.2 | ||
| Poland | Gazdag (Gazdag et al. 2009a) | 65 | |||
| Norway | Schweder (Schweder et al. 2011a) | 65 | 55 | ||
| UK | Duffett (Duffett and Lelliott 1998) | 64 | |||
| Sweden | Socialstyrelsen (Socialstyrelsen 2010) | 59 | 54.5 | 15–92 | |
| Hungary | Gazdag (Gazdag et al. 2004a) | 59 | |||
| Russia | Golenkov (Golenkov et al. 2010) | 56 | 34.4 | 15–64 | |
| Turkey | Zeren (Zeren et al. 2003) | 52 | 3(>64) | 33.1 | |
| Turkey | Saatcioglu (Saatcioglu and Tomruk 2008) | 44 | 1(>64) | 35.1 | |
| Asia | |||||
| Hong Kong | Chung (Chung et al. 2009) | 88 | 60 | 62 | 21–87 |
| Hong Kong | Chung (Chung 2003) | 68 | 15 | ||
| Thailand | Lalitanatpong (Lalitanatpong 2005) | 63 | |||
| Saudi Arabia | Alhamad (Alhamad 1999) | 60 | 27.9 | 15–60 | |
| Pakistan | Naqvi (Naqvi and Khan 2005) | 56 | 7 (>60) | ||
| Japan | Chanpattana (Chanpattana et al. 2005a) | 54 | 39 (>64) | ||
| Japan | Ishimoto (Ishimoto et al. 2000) | 51 | 27.5 | 13–59 | |
| Bengaluru, India | Eranti (Eranti et al. 2011) | 51 | 30.3 | ||
| India | Chanpattana (Chanpattana et al. 2005b) | 39 | 15 | ||
| Asia | Chanpattana (Chanpattana et al. 2010) | 38 | 4 (>64) | ||
| United Arab Emirates | Tewvik (Tewfik et al. 1998) | 33 | 30.1 | ||
| Thailand | Chanpattana (Chanpattana and Kramer 2004) | 28 | |||
| Nepal | Ahikari (Ahikari et al. 2008) | 28 | |||
ECT-treated patients in Australia and New Zealand were mainly women (63–71%) (O’Dea et al. 1991; Wood and Burgess 2003; Teh et al. 2005; Ministry of Health 2006; Chanpattana 2007; Lamont et al. 2011), and one-third of patients were above 65 years (O’Dea et al. 1991; Wood and Burgess 2003; Teh et al. 2005; Ministry of Health 2006; Chanpattana 2007; Lamont et al. 2011). Similarly in the United States, 66–79% of patients were women (Rosenbach et al. 1997; Westphal et al. 1997; Reid et al. 1998; Kramer 1999; Scarano et al. 2000; Sylvester et al. 2000), and 48–59% were elderly (over 60 years) (Reid et al. 1998; Sylvester et al. 2000; Prudic et al. 2001). In New Zealand, >80% were of European ethnicity (Ministry of Health 2006) and in USA Caucasian white ethnicity was dominant (87% to >90%) (Rosenbach et al. 1997; Westphal et al. 1997; Reid et al. 1998; Kramer 1999; Scarano et al. 2000). A typical ECT patient in the United States was said to be an elderly white female paying for treatment with insurance or private funds (Kramer 1999).
In Europe, not all studies reported gender and age, such as Russia (Nelson 2005) and Denmark (Andersson and Bolwig 2002). The percent of ECT-treated European women ranged from 44% to 81%. Mean age for ECT in Europe was overall high (49–66 years) (Tauscher et al. 1997; Duffett et al. 1999; Huuhka et al. 2000; Baghai et al. 2005; Moksnes et al. 2006; Moksnes and Ilner 2010; Socialstyrelsen 2010; Eranti et al. 2011), except 33.1–35.1 years in Turkey (Zeren et al. 2003; Saatcioglu and Tomruk 2008) and 34.4 years in the Chuvash Republic (Golenkov et al. 2010). Patients above 64 years seldom received ECT in Turkey (1–3%) (Zeren et al. 2003; Saatcioglu and Tomruk 2008), in the Chuvash Republic none (Golenkov et al. 2010). UK's National Health Service data revealed 0.2% ECT-given young patients (16–18, but none <16 years) in 2007 (Department of Health 2007). The highest treatment rates in the United Kingdom were found among those with Caucasian white ethnicity (Department of Health 2007).
In Africa, men were treated with ECT more often than women (29% women), and mean age was young (30.7 [Mugisha and Ovuga 1991], range 17–37 years [Selis et al. 2008]). Similarly, percent of ECT-treated female patients in Asia was generally low, for example, 28% Katmandu (Ahikari et al. 2008) 33% Emirates (Tewfik et al. 1998), 39% India (Chanpattana et al. 2005b), 28–63% Thailand (Chanpattana and Kramer 2004; Lalitanatpong 2005), and overall estimated to be 38% (Chanpattana et al. 2010). In some places, the female proportion was higher, for example, 51% Japan (Ishimoto et al. 2000), 56% Pakistan (Naqvi and Khan 2005), 60% Saudi Arabia (Alhamad 1999), and 68–88% Hong Kong (Chung et al. 2003, 2009). In Saudi Arabia, the typical ECT patient was described to be a Saudi married woman, with medium level of education, living in the City, not employed outside the home, and with affective disorder (Alhamad 1999). Proportion of young (<18 years) ECT-treated patients in Asia was overall 6% (Chanpattana et al. 2010), 5% Hong Kong (Chung 2003), 1% India (Chanpattana et al. 2005b), and 11% (<19 years) Katmandu (Ahikari et al. 2008). In Thailand, ECT-treated patients with schizophrenia were younger than those with depression (Lalitanatpong 2005).
Other data—conditions, adverse events, side effects, training, guidelines, legal regulations conditions
In Australia and New Zealand, consent by Mental Health Review Tribunal varied from 21% to 60% (Teh et al. 2005; Lamont et al. 2011). In the United States, use of informed consent was noted as 37% always and 26% never (Levav and Gonzalez 1996), involuntary conditions and use of guardian consent ranged from 1–2% in Texas (Reid et al. 1998; Scarano et al. 2000), 3% California (Kramer 1999) to 29% North Carolina (McCall et al. 1992). From 1993, mandatory report of ECT use to health authorities was initiated in Texas and ECT use was prohibited for patients <16 years of age (Reid et al. 1998).
Report of involuntary ECT conditions varied in Europe from 1% in Spain (Bertolin-Guillen et al. 2006), 3.2% Denmark (2009) (Sundhedsstyrelsen 2011a), to 20% Germany (Muller et al. 1998), 24% Scotland (Fergusson et al. 2004), and 26% in Finland (Huuhka et al. 2000). In Scotland, 18% of patients received ECT under the safeguards of the Scottish Mental Health Act of 1984 (Fergusson et al. 2004), and in England 60%, of those formally detained, did not consent to ECT treatment (Department of Health 2007).
The use of written informed consent documents was obligatory in Poland (Gazdag et al. 2009a), and reported as 15% in Germany (Muller et al. 1998), 44% in Belgium (Sienaert et al. 2006), and 50% in Norway (Schweder et al. 2011b). Written informed consent was mainly obtained from family members in Japan (Motohashi et al. 2004; Chanpattana et al. 2005a), Thailand (Chanpattana and Kramer 2004), and Pakistan (Naqvi and Khan 2005), and countersigning by a near relative practiced in Saudi Arabia (Alhamad 1999). In Hong Kong, 13% were judged incapable of giving informed consent (Chung 2003).
Adverse events and side effects
Adverse events (within two weeks after ECT) in Texas, in 1998 (Reid et al. 1998), were eight deaths (two were noted as possibly anesthesia-related complications) and in 2000, 25 deaths (Scarano et al. 2000), with mortality rate (within two weeks after ECT) estimated at 14 deaths per 100,000 treatments (Scarano et al. 2000). Side effects were noted in 37% in Japan, including one case of compression fractures of vertebrae (Ishimoto et al. 2000). Side effects from unmodified ECT in India were fractures, dislocations, teeth injury, and one death in the one-year study period (Chanpattana et al. 2005b). Mortality rate was estimated 0.08% in Thailand (Chanpattana and Kramer 2004), although there were no ECT-related deaths in the survey period.
Maintenance, continuation, and ambulatory ECT
Maintenance ECT was practiced in Texas (Reid et al. 1998), and continuation ECT (C-ECT) in Australia (Chanpattana 2007). Ambulatory ECT (A-ECT) was lacking in the Chuvash Republic (Golenkov et al. 2010), rarely used in Belgium (Sienaert et al. 2006), and not performed in Polish outpatients clinics (Gazdag et al. 2009a). A-ECT was reported available in 2% of Russian institutions (Nelson 2005) and 63% of Norwegian (Schweder et al. 2011b). Proportion of A-ECT-treated patients was 15% in Norway (Schweder et al. 2011b), 16% Wales (Duffett et al. 1999), 18% Ireland (Enriquez et al. 2010), and 19% UK (Department of Health 2007). A-ECT was also practiced in Thailand (Lalitanatpong 2005) but A-ECT and C-ECT rarely were used in Hong Kong (Chung 2003). In India, C-ECT report varied from given to 1–10% to 60% of patients (Chanpattana et al. 2005b).
Legislation and guidelines
In Victoria, Australia legislation requires mandatory monthly reports (Teh et al. 2005). In Poland (Gazdag et al. 2009a) and the Chuvash Republic (Golenkov et al. 2010), the presence of an anesthetist under ECT was mandatory.
Locally developed guidelines were described in Norway (Moksnes et al. 2006; Schweder et al. 2011b) and Vienna (Tauscher et al. 1997), and in Belgium less than 44% of departments did not follow guidelines (Sienaert et al. 2005a). Guidelines were used only by 28% of Japanese institutions (Motohashi et al. 2004). In Hong Kong, a hospital policy of patient assessment every one to two treatments during an ECT course was practiced only sometimes (Chung et al. 2003).
Other—funding and attitudes
Over half (57%) funding of ECT in the United States was financed by public third party payment source (including Medicare) (Reid et al. 1998). Attitudes of psychiatrists toward ECT were generally favorable in Europe, for example, in Spain (Bertolin-Guillen et al. 2006), Germany (Muller et al. 1998), Russia (Nelson 2005), and Norway (Schweder et al. 2011a). Reasons for not prescribing ECT in Europe were attributed to lack of equipment, economy, and difficulties in recruiting anesthetist (Muller et al. 1998; Nelson 2005; Bertolin-Guillen et al. 2006; Schweder et al. 2011b).
Main findings of this review are summarized as follows:
There is a large variation in ECT utilization and practice worldwide today. Global crude estimates of TPR (age < 65 years) is 2.34, EAR 11.2, iP 6.1, and AvE eight. Only some (usually under half) of all institutions within the same country provide ECT. Mandatory report of ECT use and monitoring by governmental agents is overall scant. Reporting of side effects, adverse events, and mortality is sparse. The results reflect that the guidelines by APA and Royal College of Psychiatrists are not internationally acknowledged, except in Western countries, and therefore the lack of implementation may be rational in these regions of the world.
Overall, there is a considerable variation in ECT administration and parameters worldwide. Unmodified ECT is substantially used today, not only in Asia (over 90%), Africa, Latin America, but also occurs in Europe (Russia, Turkey, and Spain). The most common electrode placement is BL, but a few places in Europe and Australia/New Zealand adhere to UL as first choice. Brief-pulse wave current devices are used worldwide, but old sine-wave stimulus and apparatus still in use.
In Western countries (Europe, USA, Australia, and New Zealand), ECT is at large administered to elderly female patients with depressive disorders. In those areas of the world (Asia, Africa, Latin America, Russia), where ECT is still often administered unmodified, it is predominantly prescribed to younger patients (often more male) with schizophrenia. ECT is administered worldwide under involuntary and guardian consent conditions (ranging from a few percent up to nearly two-thirds). (Involuntary conditions, implying also ECT administered under involuntary admission, are though in the extracted data but not always directly equivalent or indicative of involuntary [against wish] treatment.)
New trends are revealed. ECT is used as first-line acute treatment and not only last resort for medication resistant conditions in many countries. Other professions than psychiatrists (geriatricians and nurses) are administering ECT. ECT use among outpatients (ambulatory setting) is increasing.
Discussion
ECT utilization and practice are presented from all continents of the world in this review, representing a widespread use of ECT in the today's world. Two continents, Africa and Latin America, have sparse ECT country data, which might indicate a trend away from ECT (Levav and Gonzalez 1996), but this does not at all seem to be the case in the rest of the world. Although the report of ECT seems abundant in Europe, Asia, and America, the data do not cover all countries known to have ECT practice. For example, no “up to date” 1990 and after ECT studies are identified from either Iceland or Canada.
Large variations between continents, countries, and regions in ECT utilization, rates, and clinical practice are displayed, despite international guidelines (American Psychiatric Association 2001; Royal College of Psychiatrists 2005; Enns et al. 2010). Due to no uniform standard of reporting ECT utilization, rates are computed in the data extraction to TPR per 10,000, to make it comparable. This revealed a large worldwide TPR variation, from 0.11 (Gazdag et al. 2009a) to 5.1 (Rosenbach et al. 1997). Likewise worldwide iPs varied greatly. Although the large worldwide differences in ECT utilization have been pointed out previously (Hermann et al. 1995; Glen and Scott 2000; Bertolin-Guillen et al. 2006; Gazdag et al. 2009a), and the differences between countries on the basis of practice reports are not so easy to compare (Little 2003), overall variations in contemporary practice between the continents (Asia and Africa vs. USA, Australia and New Zealand, Europe) revealed by this review are immense. Explanations of these variations are complex, encompassing not only the diversity in organization of psychiatric services, but no doubt also grounded in professional beliefs concerning the efficacy and safety of ECT (The UK ECT Review Group 2003). On a worldwide scale, the number of patients receiving unmodified ECT is large, nearly 20,000 of patients in India (Chanpattana et al. 2005b), over 6000 in Thailand (Chanpattana and Kramer 2004), and overall in Asia estimated at 11.2 patients treated with unmodified ECT per 100,000 (Chanpattana 2010).
Diverse reasons for this high use of unmodified ECT have been put forth, such as lack of equipment, personnel and anesthesiologists, contraindication for anesthesia, convenience, emergency, and economic purposes (Chanpattana et al. 2005b). Whether these arguments are acceptable in this modern era and in light of knowledge about benefits and harms of ECT is another question. In spite of attempts to ban it (Mudur 2002), the debate defending unmodified ECT practice (Andrade et al. 2010), and voices claiming this practice to be unjustified and unethical (Grunhaus 2010) is ongoing today. Unmodified ECT is still practiced in some parts of Russia, Turkey, and Spain (Zeren et al. 2003; Nelson 2005; Bertolin-Guillen et al. 2006), and international guidelines (American Psychiatric Association 2001; Royal College of Psychiatrists 2005; Enns et al. 2010) appear to have failed (Strachan 2001) in influencing important aspects of today's ECT practice.
The practice in many countries of Asia (Chanpattana and Kramer 2004; Chanpattana et al. 2005a, b, 2010), Latin America (Levav and Gonzalez 1996), and Africa (Odejide et al. 1987; Mugisha and Ovuga 1991; Selis et al. 2008; James et al. 2010) bear a resemblance to the beginning of ECTs medical history in Europe (Cerletti and Bini 1938). The Asian practice of today resembles practice that was used in Finland in 1944 and 1964 (Huuhka et al. 2000), where the majority of ECT-treated patients were diagnosed with schizophrenia (75–78%) and treated unmodified. Likewise, in 1944 in Finland, ECT was (Huuhka et al. 2000) more often given to men than women (36% women). In 1997 in Finland, a major shift occurred toward majority of patients (78%) having affective disorders (unipolar/bipolar depression) and treated modified (Huuhka et al. 2000). This shift in Western world practice and the increasing use of ECT among women is also found both in USA and Australia, in the 1980s to 1990s (Galletly et al. 1991; Rosenbach et al. 1997). Similar changes seem to be occurring in some areas of Asia (Alhamad 1999; Naqvi and Khan 2005; Ahikari et al. 2008; Chanpattana et al. 2010). One reason for the lingering ECT use among patients with schizophrenia might be availability of antipsychotic medication, such as in Thailand, where the essential drug list from the Ministry of Health does not include antipsychotics (Chanpattana and Kramer 2004). Also, shortage of anesthesiologist and negative images is another explanation that is given for having hindered Japanese psychiatrists from reforming ECT practice for a long time (Motohashi et al. 2004).
Another explanation of practice differences, diagnostic and gender disparities between Asia and Europe, Australia and New Zealand, and USA might be the historical use of ECT, being much longer in Europe where it originated in 1938 (Cerletti and Bini 1938) and its early spreading to the United States (Cerletti and Bini 1938; Hemphill and Walter 1941; Shorter 2009). In Thailand, ECT was first administered unmodified in 1950, modified in 1974, and brief-pulse wave first applied in 1992 (Chanpattana 2010). Whereas, in Japan, ECT was first administered unmodified in 1939 and modified 1958 (Chanpattana et al. 2005a), but even so the practice of unmodified ECT in Japan in the 1990s is still profuse (Motohashi et al. 2004; Chanpattana et al. 2005a).
In Europe, USA, and Australia/New Zealand, practice was almost entirely modified ECT and even in Hungary (Gazdag et al. 2004a) anesthesia was obligatory. In several countries, Chuvash Republic, Russia, Spain, and Japan, the practice of modified ECT was sometimes without muscle relaxants (Ishimoto et al. 2000; Bertolin-Guillen et al. 2006; Golenkov et al. 2010), and even assistants were used to restrain extreme motion from the convulsions in Japan (Ishimoto et al. 2000). The unusual practice of muscle relaxants without anesthesia is also undertaken in a few Asian institutions (Chanpattana et al. 2010), and availability and recruitment of anesthesiologists pointed out as a problem both in Asia and Europe (Duffett and Lelliott 1998; Motohashi et al. 2004; Schweder et al. 2011b). On the other hand, Wales has no shortage of anesthesiologists (Duffett et al. 1999).
Preferred placement of electrodes worldwide (approximately 80%) is BL, as it was from the very beginning (Cerletti and Bini 1938), except for Australia, New Zealand (O’Dea et al. 1991), Norway (Schweder et al. 2011b), Vienna (Tauscher et al. 1997), Munich (Baghai et al. 2005), and the Netherlands (van Waarde et al. 2009) where UL is the first choice, but they also use both types. Brief-pulse wave current devices appear widespread world widely. Many countries (Scandinavia, Australia, and New Zealand) adhere to brief-pulse wave and UL electrode placement as first choice (Fink 2001; Rose et al. 2003; Shorter 2009), no doubt due to the reported trade-off effect between effectiveness and memory impairment (The UK ECT Review Group 2003), but switch to BL when the clinical response is judged as too poor. In spite of sine-wave current being declared unjustified by guidelines today (American Psychiatric Association 2001), it still occurs in Europe (14–52%) (Muller et al. 1998; Gazdag et al. 2004a, 2009a; Nelson 2005; Bertolin-Guillen et al. 2006; Sienaert et al. 2006), Asia (30–58%) (Chanpattana et al. 2005a, b, 2010), and USA (2%) (Prudic et al. 2001).
Previous literature indicates a predominance of patients receiving ECT in Western countries to be elderly female with affective disorder (unipolar/bipolar depression) (Reid et al. 1998; Glen and Scott 1999; Fergusson et al. 2003; Baghai et al. 2005; Moksnes et al. 2006), as is also confirmed by this review, and also in Hong Kong (Chung et al. 2009). Except for age being younger, female and depression predominance was also the case for Saudi Arabia (Alhamad 1999) and Pakistan (Naqvi and Khan 2005). In some European sites (Brussels and Wallonia in Belgium), ECT is regarded as an “antidepressant,” since it is used exclusively for the treatment of depressive disorder (Sienaert et al. 2006). In contrast, ECT in Asia it is regarded as an “antipsychotic” agent (Little 2003; Chanpattana et al. 2005a, b, 2010; Chanpattana and Kramer 2004; Ahikari et al. 2008). Discrepancies in indication could be due to differences in diagnostic practice, a lower recognition, and under treatment of depressive disorder, and also lower mental health care budgets (Chanpattana and Kramer 2004). In contrast to Asia, the typical ECT patient in the United States is said to be an elderly white female paying for treatment with insurance or private funds (Kramer 1999). Higher ECT treatment rates are found among Caucasian white ethnicity in Pennsylvania (Sylvester et al. 2000), England (Department of Health 2007), and Western Australia (Teh et al. 2005), which might imply discriminatory factors in treatment selection.
Worldwide, there is a general tendency toward a low, within-country, ECT provision by psychiatric institutions, varying from below 6% in USA (Kramer 1999), to 23–51% in Europe (Benadhira and Teles 2001; Sienaert et al. 2005a, 2006; Bertolin-Guillen et al. 2006; van Waarde et al. 2009; Schweder et al. 2011a), 66% in Australia (Chanpattana 2007), and 59–78% in Asia (Chanpattana et al. 2005a, b). In Norway, institutions even have waiting lists for ECT treatment (Schweder et al. 2011b). Altogether, this might indicate a trend toward ECT being provided by specialized units, but could also be a result of worldwide paucity in ECT training (Duffett and Lelliott 1998; Chanpattana et al. 2005a, b; Chanpattana and Kramer 2004), and even changing treatment trends.
ECT has for a long time been over held as a last-resort treatment for medication-resistant and very severe life-threatening clinical conditions (McCall 2001; Eranti and McLoughlin 2003), as reported from USA (Prudic et al. 2001). However, a transformation in ECT indication into first-line acute treatment (life saving, catatonia, previous good response, and patient preference) is apparent not only in Europe (Muller et al. 1998; Duffett et al. 1999; Zeren et al. 2003; Schweder et al. 2011a), but also in Saudi Arabia (Alhamad 1999) and Australia (Lamont et al. 2011). Although world widely ECT is mainly administered by psychiatrists and trainee psychiatrists, another change is that of other professions than psychiatrists (geriatricians and nurses) administering ECT in Europe (van Waarde et al. 2009; Schweder et al. 2011b). The trend toward increasing ambulatory ECT and ECT use among outpatients in Europe (15–19%) (Duffett et al. 1999; Department of Health 2007; Enriquez et al. 2010; Schweder et al. 2011b) is conceivably, parallel to other ambulatory treatment tendencies, out of the best interest to the recovering patient and his caregivers.
Overall, the report of side effects, adverse events, and mortality rates is sparse. Although mortality rate is reported from Thailand (0.08%) (Chanpattana and Kramer 2004) and Texas (14 deaths per 100,000 treatments within two weeks after ECT) (Scarano et al. 2000), it is not clear if the ECT-related deaths are due to lethal side effects (e.g., cardiac arrhythmia) or comorbid somatic illnesses or anesthetic complications.
ECT is administered worldwide under involuntary and guardian consent conditions, ranging from a few percent in USA and Europe 1–3% (Reid et al. 1998; Kramer 1999; Scarano et al. 2000; Bertolin-Guillen et al. 2006; Sundhedsstyrelsen 2011a) to 20–29% (McCall et al. 1992; Muller et al. 1998; Huuhka et al. 2000; Fergusson et al. 2004). Involuntary conditions in the extracted data though cannot be taken as directly equivalent to or directly indicative of involuntary (against wish) treatment. In Asia, written informed consent is mainly obtained directly or counter signed by family members (Alhamad 1999; Chanpattana and Kramer 2004; Chanpattana et al. 2005a; Naqvi and Khan 2005). Consent given by legal bodies varies from 18% in Scotland (under the Scottish Mental Health Act) (Fergusson et al. 2004) to 60% in Sydney, Australia (by the Mental Health Review Tribunal) (Lamont et al. 2011). Mandatory ECT data reporting is almost nonexistent and found only in a few places (Texas, USA, and Australia) (Reid et al. 1998; Scarano et al. 2000; Wood and Burgess 2003). Likewise legislature regulating practice, such as obligatory anesthesia (Gazdag et al. 2004a), obligatory written informed patient consent (Schweder et al. 2011b), ECT licensed facilities (Wood and Burgess 2003), prohibited administered to persons under 16 years of age (Reid et al. 1998), involuntary by order of court or legal body (Fergusson et al. 2004; Lamont et al. 2011), is also nonexistent.
Implications of findings
Worldwide improvement of ECT utilization and practice is needed, alongside development of an international minimal dataset standard applied in all countries. Continuous and mandatory monitoring and use of ECT health registrar reporting systems, taking into account patient confidentiality, would also ultimately reduce our knowledge gaps. This would again contribute to more uniform worldwide ECT practice, to the best for the patient.
Strengths and limitations
Strengths of this study are the extensive search strategy, high number of included studies, methodological transparency, and summary of findings table, providing an overview of contemporary worldwide use of ECT, which has not been undertaken in such detail previously. Limitations of this review are the inclusion of nonrandomized survey/questionnaire studies, based on practitioner accounts of ECT use, influencing the precision of the estimated rates, either to be overestimated or underestimated depending on the accuracy of the source. Seemingly, more accurate are direct reports from individual hospitals studies or national registers. The overall diversity in practice data reporting unclear representativeness of region or land as a whole and large heterogeneity in reported ECT utilization rates did not lend the data to meta-analyses. National overviews of ECT data published by regulatory bodies or governmental agencies on the internet are not so easily accessed, despite such internet sites being hand searched. National government overviews do not usually appear in the databases where systematic literature search of published journal articles and studies is undertaken.
Conclusion
Today utilization rates, practice, and ECT parameters vary greatly throughout continents and countries. Unmodified ECT is still in use (Asia, Africa, Latin America, and even in Europe). In spite of existing guidelines, there is no uniform worldwide practice. Large global variation in ECT utilization, administration, and practice advocates a need for worldwide sharing of knowledge about ECT, reflection, and learning from each other's experiences.
Acknowledgments
This study has been possible because of research commissioning on the topic “ECT for depression” from the Norwegian Directorate of Health to the Norwegian Knowledge Centre. We thank the Norwegian Knowledge Centre's research librarian K. T. Hammerstrøm (KTH) for designing and undertaking the literature search in collaboration with the authors. We also extend our gratitude to M. J. Cooke, Bergen University Psychiatric Hospital Psychosis Unit, for all her helpful English language correction. This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Appendices
Appendix A.
Search strategy
| Ovid MEDLINE(R) 1950 to November 2010 Week 2 | EMBASE 1980 to 2010 Week 45 | PsycINFO 1806 to November 2010 Week 3 | SveMed+ | EBSCO; Cinahl | |
|---|---|---|---|---|---|
| 1 | Electroconvulsive Therapy/ | Electroconvulsive Therapy/ | Electroconvulsive exp Shock/ | Explodesökning på Electroconvulsive-Therapy | S7 or S14 |
| 2 | (electroconvulsive$ or electr$ convulsive$).tw. | (electroconvulsive$ or electr$ convulsive$).tw. | (electroconvulsive$ or electr$ convulsive$).tw. | (electroconvulsive$ or electr$ convulsive$) | S8 or S9 or S10 or S11 or S12 or S13 |
| 3 | (electroshock$ or electr$ shock$).tw. | (electroshock$ or electr$ shock$).tw. | (electroshock$ or electr$ shock$).tw. | (electroshock$ or electr$ shock$) | TI ((practice of electroconvulsive*) or (practice of electr* convulsive*) or (practice of electroshock*) or (practice of electr* shock*) or (practice of ect)) or AB ((practice of electroconvulsive*) or (practice of electr* convulsive*) or (practice of electroshock*) or (practice of electr* shock*) or (practice of ect)) |
| 4 | ect.tw. | ect.tw. | ect.tw. | ect | TI ((ect n1 “use of”) or (ect n1 used) or (ect n1 frequen* of) or (ect n1 analys* of)) or AB ((ect n1 “use of”) or (ect n1 used) or (ect n1 frequen* of) or (ect n1 analys* of)) |
| 5 | or/1–4 | or/1–4 | or/1–4 | elterapi or elektrokonvulsiv$ or elektrosjokk$ or elektrochok$ or elchok$ or eletrochock$ or elchock$ or elektrostim$ | TI ((electroshock* n1 “use of”) or (electroshock* n1 used) or (electroshock* n1 frequen* of) or (electroshock* n1 analys* of)) or AB ((electroshock* n1 “use of”) or (electroshock* n1 used) or (electroshock* n1 frequen* of) or (electroshock* n1 analys* of)) |
| 6 | (utiliz$ or survey$).tw. | (utiliz$ or survey$).tw. | (utiliz$ or survey$).tw. | S1 OR S2 OR S3 OR S4 OR S5 | TI ((electr* shock* n1 “use of”) or (electr* shock* n1 used) or (electr* shock* n1 frequen* of) or (electr* shock* n1 analys* of)) or AB ((electr* shock* n1 “use of”) or (electr* shock* n1 used) or (electr* shock* n1 frequen* of) or (electr* shock* n1 analys* of)) |
| 7 | 5 and 6 | 5 and 6 | 5 and 6 | utiliz$ or survey$ or bruk$ or anvend$ or använd$ or benytt$ | TI ((electro convulsive* n1 “use of”) or (electro convulsive* n1 used) or (electro convulsive* n1 frequen* of) or (electro convulsive* n1 analys* of)) or AB ((electro convulsive* n1 “use of”) or (electro convulsive* n1 used) or (electro convulsive* n1 frequen* of) or (electro convulsive* n1 analys* of)) |
| 8 | Electroconvulsive Therapy/sn, ut [Statistics & Numerical Data, Utilization] | ((electroconvulsive$ or electr$ convulsive$ or electroshock$ or electr$ shock$ or ect) adj1 (“use of” or used)).tw. | ((electroconvulsive$ or electr$ convulsive$ or electroshock$ or electr$ shock$ or ect) adj1 (“use of” or used)).tw. | praksis$ or prakti$ or frekven$ | TI ((electroconvulsive* n1 “use of”) or (electroconvulsive* n1 used) or (electroconvulsive* n1 frequen* of) or (electroconvulsive* n1 analys* of)) or AB ((electroconvulsive* n1 “use of”) or (electroconvulsive* n1 used) or (electroconvulsive* n1 frequen* of) or (electroconvulsive* n1 analys* of)) |
| 9 | ((electroconvulsive$ or electr$ convulsive$ or electroshock$ or electr$ shock$ or ect) adj1 (“use of” or used)).tw. | (practice of electroconvulsive$ or practice of electr$ convulsive$ or practice of electroshock$ or practice of electr$ shock$ or practice of ect).tw. | (practice of electroconvulsive$ or practice of electr$ convulsive$ or practice of electroshock$ or practice of electr$ shock$ or practice of ect).tw. | S7 OR S8 | S5 and S6 |
| 10 | (practice of electroconvulsive$ or practice of electr$ convulsive$ or practice of electroshock$ or practice of electr$ shock$ or practice of ect).tw. | (((frequen$ adj of) or (analys$ adj of)) adj1 (electroconvulsive$ or electr$ convulsive$ or electroshock$ or electr$ shock$ or ect)).tw. | (((frequen$ adj of) or (analys$ adj of)) adj1 (electroconvulsive$ or electr$ convulsive$ or electroshock$ or electr$ shock$ or ect)).tw. | s6 and s9 | S1 or S2 or S3 or S4 |
| 11 | (((frequen$ adj of) or (analys$ adj of)) adj1 (electroconvulsive$ or electr$ convulsive$ or electroshock$ or electr$ shock$ or ect)).tw. | or/8–10 | or/8–10 | TI (utiliz* or survey*) or AB (utiliz* or survey*) | |
| 12 | 8 or 9 or 10 or 11 | 7 or 11 | 7 or 11 | AB ect or TI ect | |
| 13 | 7 or 12 | human/ | limit 12 to yr =“1990 -Current” | AB ((electroshock* or electr* shock*)) or TI ((electroshock* or electr* shock*)) | |
| 14 | humans.sh. | 12 and 13 | AB ((electroconvulsive* or electr* convulsive*)) or TI ((electroconvulsive* or electr* convulsive*)) | ||
| 15 | 13 and 14 | limit 14 to yr =“1990 -Current” | (MH “Electroconvulsive Therapy”) | ||
| 16 | limit 15 to yr =“1990 -Current” |
Appendix B.
Excluded studies (N= 31)
| First author (reference) | Country or continent and reason for exclusion: (1) not relevant topic (2) no rate or prevalence data, very sparse data, review without primary data (3) parallel other language publication, not possible to find or full-text retrieve (4) too old, <1990 | Comments |
|---|---|---|
| O’Dea JF (O’Dea et al. 1991) | Australia and New Zealand (1) | Questionnaire survey of ECT practice and attitudes to medical superintendents at hospitals. Frequency of unilateral versus bilateral electrode placement main aim. Sparse ECT utilization data |
| Galletly CA (Galletly et al. 1991) | South Australia (4) | Too old, use of ECT data at hospital in Adelaide from 1981 to 1985 (five years). [Decline in use over period due to reduction of ECT for patients with schizophrenia] |
| Gassy JE (Gassy and Rey 1990) | NSW, Australia (4) | Too old, a general hospital psychiatry unit use of ECT from April 1982 to December 1987 |
| Ikeji OC (Ikeji et al. 1999) | Nigeria (2) | A prospective open-label study of 70 unmodified ECT treated patients without rate or prevalence data |
| Odejide AO (Odejide et al. 1987) | Nigeria (4) | Sparse data from <1990, records from 1982 and1984 examined. Unmodified bilateral ECT. Modified ECT was tried in 1979, but found too expensive. Thirty percent of patients ECT treated in 1984 and average no. of ECTs six, range 1–19 |
| Okasha TA (Okasha 2007) | Egypt (2) | General article about ECT use, economic aspects, problems of training, ethical issues, and discrepancies between developed and developing countries in its application. No ECT utilization data |
| Alhamad AM (Alhamad and,al–Haidar 1999) | Saudi Arabia (3) | Parallel publication, same data presented as in other included reference by same author (Alhamad 1999) |
| Hermann RC (Hermann et al. 1999) | USA (1) | Retrospective study of ECT use among beneficiaries of a New England insurance company in 1994 and 1995 |
| Olfson M (Olfson et al. 1998) | USA, New York (1) | ECT use for general hospital in patients with only recurrent major depression diagnoses and estimate of effect on prompt ECT on the length of stay and cost of inpatient care |
| Fink M (Fink and Kellner 2007) | USA (1) | General about ECT practice, no primary data |
| Eranti SV (Eranti and McLoughlin 2003) | UK, USA (2) | Editorial article state of the art, no primary data |
| Thompson JW (Thompson et al. 1994) | USA (4) | Too old, National Institute of Mental Health (NIMH) data, ECT-treated patients in 1975, 1980, and 1986, focusing on data from 1980 and 1986 |
| Levav I (Levav and Gonzalez 1998) | Latin America (3) | Parallel publication in English, replication of primary data presented in earlier study/ publication in 1996 (Levav and Gonzalez 1996) |
| Glen T (Glen and Scott 2000) | Edinburgh, Scotland, UK (1) | Calculated annual and aggregate rates of ECT use by consultant teams, not relevant |
| Fergusson G (Fergusson et al. 2003) | Scotland (3) | Parallel publication, same data presented in included 2004 publication (Fergusson et al. 2004), by same first author |
| Berg JE (Berg 2009) | Diverse countries in three continents (2) | Report from visiting 14 diverse hospitals in three continents about ECT practice. ECT data unclear, insufficient and no overall ECT utilization country-specific data |
| Gazdag G (Gazdag et al. 2009b) | Hungary (2) | To analyze the referral practice of patients for ECT, no rate or prevalence data |
| Lucca AM (Lucca et al. 2010) | Milan, Italy (2) | Letter to editor about 33 patients receiving ECT, insufficient ECT utilization data |
| Stromgren LS (Stromgren 1991) | Nordic countries: Denmark, Norway Sweden, Iceland (4) | Too old, use of ECT survey in the Nordic countries, from1977–1987 |
| Frederiksen SO (Frederiksen and d’Elia 1979) | Sweden (4) | Too old, ECT survey data in 1975 |
| Kornhuber J (Kornhuber and Weller 1995) | Germany (3) | Not possible to full-text retrieve |
| Sienaert P (Sienaert et al. 2005b) | Flanders and Brussels Capital Region (3) | Parallel publication in Dutch language to already included study (Sienaert et al. 2005a) |
| Gazdag G (Gazdag et al. 2004b) | Hungary (3) | Parallel publication in Hungarian language to already included study (Gazdag et al. 2004a) |
| Palinska D (Palinska et al. 2008) | Poland (3) | Polish language and ECT utilization in Poland of later date by Gazdag G (Gazdag et al. 2009a) included |
| Latey RH (Latey and Fahy 1985) | Ireland (4) | Too old, ECT survey data from 1982 |
| Baudis P (Baudis 1992) | Czech Republic (4) | Too old, ECT survey data from 1981 to 1989 |
| Agarwal AK (Agarwal et al. 1992) | India (2) | About issues relating to administration of ECT, no ECT utilization data |
| Andrade C (Andrade et al. 1993) | India (2) | About practical administration of ECT, no ECT utilization data |
| Chanpattana WM (Chanpattana 2010) | Thailand (2) | Review article, not a primary study with data |
| Takebayashi M (Takebayashi 2010) | Japan (2) | Review article about history of the practice and guidelines of ECT in Japan |
| Kramer BA (Kramer, Hsin-Tung 1990) | Asia (China, Hong Kong, India, Indonesia, Japan, Korea, Malaysia, Pakistan, Singapore, Sri Lanka, Thailand) (4) | Too old survey of ECT use in 28 institutions from 11 Asian countries, unclear time period before 1990. (Unmodified ECT always used at 12 institutions) |
Appendix C. Summary of findings tables of included studies (N= 70) according to five continents
Table C1.
Australia and New Zealand (N= 7).
| Country | Reference | Study | Demographics | Other data | Rates | Technical parameters |
|---|---|---|---|---|---|---|
| Land (L) | First autdor (reference) | Study design | Diagnoses | Side effects | TRP* | Modified/Unmodified |
| Region (R) | N | Indication | Outcome | EAR* | Anesthesia | |
| City (C) | Date | Gender | Conditions | iP* | Devices | |
| Hospital (H) | Time span | Age | Training | AvE* | Current type | |
| Ethnicity | Guidelines | Electrode placement | ||||
| Legal regulations | C-ECT** | Dosage | ||||
| Other | A-ECT** | (Monitoring) | ||||
| Australia (L) | Chanpattana W (Chanpattana 2007) | Study: Questionnaire survey (29 items) to hospitals providing psychiatric care. N= 136 hospitals (83% response rate) with N= 90 (66%) providing ECT Date: October 2002 to February 2004 Time span: One year and five months | Diagnoses: 82% major depression 10% schizophrenia 5% mania 2% catatonia Gender: 63% women Age, year groups: 0.2%, <18 7%, 18–24 26%, 25–44 28%, 45–64 38%, >65 | Side effects: 96% memory problems 77% headache 51% muscle pain 7% post-ECT delirium 2% teeth injuries 1% concentration difficulty 3% no side effects ECT training provided by: 73% institutions Guidelines not mentioned | TPR: 3.78 AvE: 8 C-ECT practiced | Modified Devices: Thymatron or MECTA device 2% old brief-pulse constant current device Type: Brief pulse Placement: 46% UL 24% BL 22% UL and BL 3% BL only Dosage: 70% stimulus titration 28% age based 2% fixed dose |
| New Zealand (L) | Ministry of Health, New Zealand (Ministry of Health 2006) | Study: National health data from 21 district health boards in two periods (2003/04 and 2004/05). Time span: Two periods of one year | Gender: 69% women (both periods) Age >65: 40% (2004/05) 38% (2003/04) Ethnicity (2004/05; 2003/04) Asian: 2%; 1% European: 85%; 84% Maori: 6%; 5% Pacific people: 7%; 2% Other: 17%; 8% | Legal regulations not consented: 22% (2004/05) 24% (2003/04) | TPR: 0.75 (both periods) AvE: 7 | |
| New Zealand (L) | Ministry of Health, New Zealand (Ministry of Health 2005) | Study: Audit of technical aspects and quality of ECT delivered by site visit. N= 20 (district health boards) sites visited, and 19 (95%) sites providing ECT N= 414 (approximately) patients and 3506 ECT administrations Date: September to November 2002 Time span: Two months | Training: 10 (50%) had advanced training program Guidelines: All had some forms of ECT policy, but variations Other: All had ECT teams All ECT prescribed only by senior medical officer All sites administered by consultant psychiatrists or trained/supervised registrar All anesthesia by consulting anesthesiologist or trained/supervised anesthetic registrar All sites had recovery ECT nurse, four sites with specially employed ECT co-ordinating nurse | Rate: 92 ECT treatments per 100,000 people (in 2001–2002) AvE: 8 | Modified Type: Brief-pulse wave Devices and monitoring: 18 brief pulse with EEG One without EEG monitoring | |
| Australia & New Zealand (L) | O’Dea JF (O’Dea et al. 1991) | Study: Questionnaire survey (11 items) to N= 130 psychiatric hospitals and units. N= 96 responded (74% response rate) and 20 of 96 (21%) did not provide ECT and two insufficient N= 74 institutions providing ECT N= 915 patients ECT treated in survey period Date: 1989 Time span: Six months | Diagnoses: Mentioned according to preference of choice of electrode placement, with depression as main indication. N= 577 patients (63%) commenced treatment with unilateral ECT. Most institutions (66%) began the majority of their courses with unilateral ECT | Attitudes: 50% considered BL ECT to be more effective for the treatment of depression in general and 39% believed BL and UL ECT to be equally effective | AvE: 12 [Estimated 2500 ECT-treated patients per year in Australia and New Zealand] | Modified Devices: Kabtronics Konvulsator Duopulse Ectonus and other Type: Brief-pulse wave according to devices, but 19% reported as sine wave Placement: 63% UL 16% BL |
| Victoria, Australia (R) | Wood DA (Wood and Burgess 2003) | Study: Descriptive analysis from aggregated statutory data N= 1526 patients ECT treated N= 14,116 ECT administrations. Date: 1998–1999 Time span: One year | Diagnoses: 75% depression 10% schizophrenia 6% schizoaffective 8% bipolar 0.5% residual Gender: 63% women Age, year groups: 6%, 15–24 32%, 25–44 28%, 45–64 33%, >65 | Licensing: All facilities providing ECT must be licensed Mandatory: Monthly reports Other: High use in age group >65 years | TPR: 3.99–4.44 EAR: 33.03–36.26 iP: 8% | No information |
| Western Australia (R) | Teh SPC (Teh et al. 2005) | Study: Register data from Mental Health Information System of Western Australia and records from state psychiatric hospitals N= 1175 estimated ECT treated in five-year period. N= 622 ECT treated within State psychiatric facilities from 1988 to 2001. Date: 1997–2001 Time span: Five years | Diagnoses: 43% affective psychoses 35% depression 4% bipolar 2% schizophrenia 2% other Gender: 65% women Age, year groups: 2%, 0–18 71%, 19–64 27%, >65 Ethnicity: 1% aboriginality 99% nonaboriginality | Involuntary: 21% treated involuntary at least once (within State facilities) Other: Upward trend in TPR and number of ECT recipients in five-year period | TPR: 0.8 (1997) 1.3 (1998) 1.2 (1999) 1.6 (2000) 1.4 (2001) iP: 1.0–1.7% | No information |
| Australia, Sydney, New South Wales (C) | Lamont S (Lamont et al. 2011) | Study: Audit of ECT service provision at metropolitan teaching hospital in Sydney with 28 inpatients bed, serving a population of 260,000. N= 43 ECT-treated patients Date: November 2007– November 2008 Time span: One year | Diagnoses: 67% depression 9% schizoaffective 14% schizophrenia 5% bipolar 5% schizophrenia catatonic type, neuroleptic malignant syndrome Indication: 25% resistant to antidepressants: 21% resistant to antipsychotics/lithium: 21% suicidal 9% previous response 7% life-saving intervention 5% severe retardation 5% too distressed to wait drug response 5% patient preference 2% psychosis Gender: 71% women Age, year groups: 5%, 15–24 37%, 25–44 30%, 45–64 14%, 65–74 14%, >75 | Condition: 40% voluntary 60% involuntary (Mental Health Review Tribunal consent) | TRP: 1.8 AvE, women: 10.2 AvE, men: 8 | Modified Anesthesia: Propofol Sucxamethonium Device: Thymatron System IV Type: Brief pulse Placement: 35% RUL 40% BL 23% Both RUL and BL |
TPR: treated person rate = persons ECT treated per 10,000 resident population per year.
EAR: ECT administration rate = no. of ECTs administered per 10,000 resident population.
iP: inpatient prevalence = proportion (percent, %) ECT treated among inpatient population.
AvE: average number of ECTs administered per patient (in a session or course).
C-ECT: continuation-ECT.
A-ECT: ambulatory-ECT.
Table C2.
Africa (N= 3).
| Country | Reference | Study | Demographics | Other data | Rate | Technical parameters |
|---|---|---|---|---|---|---|
| Land (L) | First autdor (reference) | Study design | Diagnoses | Side effects | TRP* | Modified/Unmodified |
| Region (R) | N | Indication | Outcome | EAR* | Anesthesia | |
| City (C) | Date | Gender | Conditions | iP* | Devices | |
| Hospital (H) | Time span | Age | Training | AvE* | Current type | |
| Ethnicity | Guidelines | Electrode placement | ||||
| Legal regulations | C-ECT** | Dosage | ||||
| Other | A-ECT** | (Monitoring) | ||||
| Malawi (L) | Selis MA (Selis et al. 2008) | Study: Naturalistic descriptive cohort N= 47 patients ECT treated in study period [N= 780 patients estimated ECT treated in one year] [N= 1 national mental hospital with N= 333 beds] Date: March to April 2006 Time span: One month | Diagnoses: 32% mania 30% psychosis 21% postpartum psychosis 15% depression 2% no diagnoses Indication (main): Postpartum depression and psychosis Gender: 49% women Age, years: Range 17–37 | Guidelines and conditions: Use of protocols and consent. Side effects: For unmodified: 39% confusion, amnesia, headache, muscle aches, oral lacerations | EAR: 0.6 [Calculated rate: 780 ECT treatments per year, 13 million population] AvE: Range 1–10 | Unmodified until September 2007 then modified. N= 3 patients underwent both unmodified and modified Anesthesia: None before 2007 Placement: BT (bitemporal) |
| South Africa (H) | Mugisha RX (Mugisha and Ovuga 1991) | Study: Survey of case notes at hospital Total: N= 1816 case notes N= 378 patients ECT treated Date: 1976–1982 Time span: Seven years | Diagnoses: 83% schizophrenia 17% other diagnoses, including depression, epilepsy, alcoholism or cannabis abuse, dementia, and unknown Gender: 29% women, among subgroup with schizophrenia Age, mean (SD) years: 30.7 (9.9) [women 30.2, men 31.9] | Drop in use of ECT from 1976 to 1982. ECT discontinued after 1982. Data from before 1990, but published in 1991. Mainly young adult men (<35 years) treated with ECT. Main indication schizophrenia, not depression | TPR: 1.26 [Calculated rate: 378 patients ECT treated, 3 million population] iP: 21% (in seven-year period) | Unmodified No anesthesia Device and type: No information Placement: No information |
| Nigeria (H) | Sijuwola OA (Sijuwola 1985) | Study: Survey of psychiatric hospital with 500 beds, covering also neighbor countries. N= 278 patients N= 1529 ECT administrations Time span: Four weeks [Data from 1985 (<1990), but included due to paucity of studies from Africa] | Diagnoses: 60% schizophrenia 23% affective disorders 17% other | iP: 28% AvE: 5 Range 4–6 | No information | |
TPR: treated person rate = persons ECT treated per 10,000 resident population per year.
EAR: ECT administration rate = no. of ECTs administered per 10,000 resident population.
iP: inpatient prevalence = proportion (percent,%) ECT treated among inpatient population.
AvE: average number of ECTs administered per patient (in a session or course).
C-ECT: continuation-ECT.
A-ECT: ambulatory-ECT.
Table C3.
North and Latin America, N= 12.
| Country | Reference | Study | Demographics | Other data | Rate* | Technical parameters |
|---|---|---|---|---|---|---|
| Land (L) | First autdor (reference) | Study design | Diagnoses | Side effects | TRP* | Modified/Unmodified |
| Region (R) | N | Indication | Outcome | EAR* | Anesthesia | |
| City (C) | Date | Gender | Conditions | iP* | Devices | |
| Hospital (H) | Time span | Age | Training | AvE* | Current type | |
| Ethnicity | Guidelines | Electrode placement | ||||
| Legal regulations | C-ECT** | Dosage | ||||
| Other | A-ECT** | (Monitoring) | ||||
| USA (L) | Hermann RC (Hermann et al. 1995) | Study: Survey data, American Psychiatric association (APA)'s Professional Activities Survey Date: 1988–1989 Time span: One year | Indication (main): depression Gender: No information Age: Not reported, except proportion of residents >60 years stated not significantly related to utilization rate | Other: 6% of psychiatrists administered ECT to at least one patient during the last month Large variability. ECT use higher in middle and upper classes | TPR: 0.4–81.2 TPR Nationwide: 4.9 | No information |
| USA (L) | Prudic J (Prudic et al. 2001) | Study: Postal questionnaire survey in tri-state New York City metropolitan region to all Directors of Psychiatric Services with inpatient mental health beds. N= 156 facilities N= 86 of 156 (55%) provided ECT N= 59 of 86 responded (response rate 69%). No. of patients annually receiving ECT: Range 1–288 No. of patients ECT treated per year census reported by facilities: <15 patients by 21 facilities >100 patients by nine facilities Date:1997 Time span: One year | Indication (main): >85% medication resistant depression (major depression) then mania and schizophrenia next most common Gender: No information Age, year groups: 45%, 18–60 55%, >60 (0%, <13) | Side effects: 46% post ECT cognitive impairment and cognitive evaluation usually undertaken in 80% Treatment setting: 85% inpatient 14% outpatients Outcome: 23% relapse rate of illness Guidelines: APA guidelines not entirely followed | AvE: 8 | Modified Anesthetic agents: 59% methohexital 36% sodium pentothal 31% propofol Type: 2% sine wave Placement: 79% BL 21% UL Dose: 18% dosing strategy 30% fixed (formula-based) 55% titration Monitoring: All used EKG, pulse oximetry and vital sign monitoring. 14% EEG monitoring not used. 53% cuff technique not used |
| Latin America and the Caribbean (L) | Levav I (Levav and Gonzalez 1996) | Study: Postal questionnaire survey to directors responsible for mental health programs and/or psychiatric hospitals N= 19 Latin America countries, 17 (89%) responded and two partially. N= 12 Caribbean, only four (30%) provided ECT Date: 1995 Time span: One year | No information | Comment: Haiti not included among the Caribbean territories Unknown country names of included in Latin America. Public hospitals use ECT more frequent than private Trend away from use of ECT reported in eight Latin American countries and in two most populated English-speaking Caribbean Guidelines: In four Caribbean countries, but only in 10 out of 19 Latin American Conditions: Informed consent (Latin America): 37% always 26% sometimes 26% never 11% no data | No information | Unmodified and modified: 26% Latin America unmodified One of four Caribbean used modified |
| California, USA (R) | Kramer BA (Kramer 1999) | Study: Retrospective chart review of ECT required reports by Welfare and Institutions Code, from state department of health ECT-treated patients: N= 2671 (1990) N= 2251 (1991) N= 2356 (1992) N= 2636 (1993) N= 2529 (1994) ECT facilities providing ECT: N= 81 (1990) N= 80 (1991) N= 71 (1992) N= 70 (1993) N= 69 (1994) Date: 1984–1994 Time span: 11 years | Diagnoses: No information Gender (1994): 69% women Ethnicity (1994): 91% Anglo-American 4% Hispanic 2% African-American | Adverse events: 0.2 deaths/10,000 11 cardiac arrests nine fractures Conditions: 2.4–3.4% involuntary (in period 1990–1994) Other: Mandatory report of death if within 24 h after ECT treatment Increased ECT use with age Decrease in facilities providing ECT. Less than 6% ECT treatment in public hospitals | TPR: 0.9 (1990) 0.7 (1991) 0.8 (1992) 0.8 (1993) 0.8 (1994) TPR by age in years (1994): 0.001 <18 0.1 18–24 0.5 25–44 1.2 45–65 3.8 >65 AvE: 5. | No information |
| Texas, USA (R) | Scarano VR (Scarano et al. 2000) | Study: Retrospective chart review. N= approximately 5971 ECT-treated patients N= 41,660 ECT administrations Date: 1993–1997 Time span: Four years | Diagnoses: 82% depression 6% schizoaffective 10% bipolar/mania 2% schizophrenia Gender: 69% women 31% male Ethnicity: 87% Anglo-American 9% Hispanic 3% African American Age, year groups*: 0.7%, 16–20 37.4%, 21–50 53.7%, 51–80 8.2%, >80 | Conditions: 98% voluntary 2% consent by legal guardian. Adverse events (within two weeks after ECT): Five unexpected apnea, one fracture, 25 deaths [two week mortality rate 14 deaths per 100,000 treatments] Outcome: 61% completed ECT treatment series Other: Report of memory impairment by physicians, no rating instruments | AvE: 7 | Placement: 76% BL 16% UL 8% mixed |
| *[Correction added after first online publication on 20 March 2012: The “Age, year groups” for Texas, USA (R) was earlier missing from the article.] | ||||||
| Texas, USA (R) | Reid WH (Reid et al. 1998) | Study: Retrospective chart review. N= 2583 mandatory reports (describing a patient treatment with an index series), approximately. N= 15,240 ECT treatments administered in 50 hospitals (Representing 33% of all psychiatric units in Texas). Date: September 1993 to April 1995 Time span: One year + seven months (19 months) | Diagnoses (approximately): 90% severe mood disorder (some manic), 10% schizoaffective, schizophrenia, or related diagnoses 2% organic affective syndrome, mood disorder due to a general medical condition, or dementia Gender: 70% women Age, year groups: 0.2%, 16–17 2%, 18–24 24%, 25–44 25%, 45–64 48%, >64 Ethnicity: 88% Caucasian 8% Hispanic 3% Black 1% Other | Conditions: 1% involuntary guardian consent Adverse events (within two weeks after ECT): Eight deaths (two possibly anesthesia related complications) Other: 6% of institutions performed ECT during the study period Legal regulations: Since 1993 mandatory ECT reporting to Department of Mental Health and Mental Retardation in Texas. ECT not allowed to persons <16 years. Funding: 57% public third party payment source (including Medicare) | AvE: 5 [excluding maintenance ECT] | Placement: 73% BL 19% UL 8% Mixed |
| USA (Medicare) (R) | Rosenbach ML (Rosenbach et al. 1997) | Study: Retrospective chart review of ECT-treated Medicare enrollees. N= 15,560 (1992) [N= 12,000 (1987)] Date: 1987–1989 and 1990–1992 Time span: Two, one-year time periods | Diagnoses (1992): 80% affective disorder 9% schizophrenia Gender (1992): 66% women Ethnicity (1992): >90% Caucasian | Treatment setting (1992): 75% inpatients 11% outpatients 14% both Other: Mean no. of ECT treatment length of stay days: 57.1 Comments: Increase in rate of ECT use 1987–1992. Increasing use among women, Caucasian, and disabled. Substantial geographic treatment variation from West to Northeast in United States, an increase in outpatient ECT use | TPR (TPR in Medicare population): 5.1 (1992) [4.2 (1987)] TPR (1992) by gender: 5.7 women 3.6 men TPR (1992) by age, year groups: 16.2, <45 6.4, 45–65 4.2, >65 TPR (1992) for disabled <65 years: 9.2 TPR (1992) by region: 6.1, Northeast 4.1, South 5.4, North Central 3.8, West TPR (1992) by location: 3.2, rural 4.8, small urban 6.0, large urban AvE: 8 AvE (in both inpatient and outpatient setting): 13 | No information |
| North Carolina, USA (R) | Creed P (Creed et al. 1995) | Study: Postal and telephone survey to all 169 hospitals in region, with 54 having psychiatric units. Structured questionnaire to those providing ECT N= 24 (14%, out of 169 hospitals and 44% out of 54 psychiatric units) Date: September 1992 to August 1993 Time span: One years | Patient demographic data: No information | Training: 55% provided on-the-job training for ECT nursing staff Other: No. of physicians at each facility administering ECT, Range 1–6 Resident physicians administering ECT in 25% of facilities | Estimated rate data: No. of combined inpatient and outpatient ECT treatments per year: Range <100 to >1,300 | Devices: Unclear, report of only use of recommended ECT machines Monitoring: 75% use combination of EEG and cuffed distal limb |
| Louisiana, USA (Medicare) (C) | Westphal JR (Westphal et al. 1997) | Study: Retrospective chart review of elderly (≥65 years) ECT treated in Louisiana Medicare population. N= 218 ECT administrations in ≥65 years Medicare population Date: 1993 and 1994 Time span: Two years | Age, age groups ≥65 years: 54%, 65–74 37%, 75–84 8%, ≥85 Gender: 79% women Ethnicity: 89% Caucasian 7% Black 4% Other | Comment: Within Louisiana variability in rates between urban parishes, TPR 2.8 versus rural TPR 1.9 was nonsignificant—but significant nonrandom variation found when comparing treatment for major depression and inpatient ECT | TPR (Medicare population ≥65 years): 2.38 [TPR rural parishes: 1.9 TPR urban parishes: 2.8] | No information |
| North Carolina, USA (H) | McCall WV (McCall et al. 1992) | Study: State hospital survey of all patients referred for ECT N= 82 ECT-treated patients Date: 1989 to 1991 Time span: Two years | Diagnoses: 73% of depressed patients receiving ECT were women, constituted 52% of all patients with severe depression Gender: Percent women among ECT patients by diagnoses: 73% major depression 58% bipolar, manic 68% schizoaffective 16% schizophrenia Percent men among ECT patients by diagnoses: 27% major depression 42% bipolar, manic 32% schizoaffective 84% schizophrenia Age mean (SD) years: 44.3 (15) Range 19–75 50.9 (15.1) for depression 38.4 (13.2) for mania, schizophrenia, and schizoaffective | Conditions: 29% treatment by guardian consent Other: ECT given to patients with schizophrenia, mania, or schizoaffective disorder younger than those with depression | iP: 1.3% C-ECT: 5% (Given to four patients: three women, one man) | Modified Device: MECTA SR1 constant current device. Placement: No information |
| South West Pennsylvania, State Hospital, USA (H) | Sylvester AP (Sylvester et al. 2000) | Study: Retrospective chart review of all receiving ECT, in one state hospital giving psychiatric services to South West Pennsylvania. N= 21 ECT-treated patients in 10 year period (charts available for 17 patients) Date: 1986–1995 Time span: 10 years | Diagnoses: 47% major depression 25% bipolar 29% schizoaffective, schizophrenia Indications: Suicidal ideation or passive death wish Refusal of oral food intake Weight loss, daily life disability, and poor hygiene. Disorganized psychotic, aggressive behavior Gender: 71% women Age, 59% >60 years Range: 28–78 years Ethnicity: 94% Caucasian | Conditions: All on civil commitment and nine (53%) patients judged incompetent of consent Other: 59% of ECT treated >60 years and only 46% of all admitted patients female. Ten (58%) patients had documented previous ECT | iP: 0.4% AvE: 12 | Devices: Until 1991, MECTA-D After 1991 MECTA-SRI Type and dosage: Brief pulse, square wave, and constant current stimuli dose |
| Rio de Janeiro, Brazil (H) | Pastore DL (Pastore et al. 2008) | Study: Medical record survey of ECT-treated patients at federal psychiatric university hospital. N= 69 ECT-treated patients Date: June 2005 to June 2007 Time span: Two years | Diagnoses: 49% schizophrenia 29% bipolar/mania 16% depression 6% other Indication: Violence, suicidal attempts, self injury Gender: 71% women Age, mean 41.3 years | Side effects: Most common (reported as mild and transient): Anterograde amnesia, disorientation, headache. Rare: Myalgia, nausea, fatigue. No deaths. Other: Clonidine given to hypertensive patients | AvE: 8 | Modified Anesthesia: Alfentanil or propofol and succinylcholine muscle relaxant Device: EMAI trademark Placement: BL |
TPR: treated person rate = persons ECT treated per 10,000 resident population per year.
EAR: ECT administration rate = no. of ECTs administered per 10,000 resident population.
iP: inpatient prevalence = proportion (percent,%) ECT treated among inpatient population.
AvE: average number of ECTs administered per patient (in a session or course).
C-ECT: continuation-ECT.
A-ECT: ambulatory-ECT.
Table C4.
Europe N= 33.
| Country | Reference | Study | Demographics | Other data | Rate* | Technical parameters |
|---|---|---|---|---|---|---|
| Land (L) | First autdor (reference) | Study design | Diagnoses | Side effects | TRP* | Modified/Unmodified |
| Region (R) | N | Indication | Outcome | EAR* | Anesthesia | |
| City (C) | Date | Gender | Conditions | iP* | Devices | |
| Hospital (H) | Time span | Age | Training | AvE* | Current type | |
| Ethnicity | Guidelines | Electrode placement | ||||
| Legal regulations | C-ECT** | Dosage | ||||
| Other | A-ECT** | (Monitoring) | ||||
| Belgium (L) | Sienaert P (Sienaert et al. 2006) | Study: Questionnaire (30 items) survey to psychiatric hospitals and wards of general hospitals N= 149 (Response rate 100%), only 32 (21.5%) provided ECT Date: 2003–2004 Time span: One year | Diagnoses: 81% depressive episode 6% psychoses 2% mania 0.9% other Gender and age: No information | Conditions: 44% written informed consent 65% patient information Training: 34% Other: 53% of the hospitals administered <10 ECT sessions per month Within-country significant difference in TPR utilization rates Attitudes psychiatrists: ECT is not used enough: 84.3% | TPR, Flanders: 2.6 TPR, Wallonia: 5.5 TPR, Brussels Capital Region: 10.6 TPR, Belgium total: 4.37 C-ECT: Rarely used (none (44%), 0–5 (47%)) A-ECT: Rarely used (none (44%), 0–5 (44%)) | Modified Anesthesia: 75% Propofol Current type: 34% sine wave Electrode placement & dose: BT: 66% UL: not used 37% combined BT and fixed high stimulus dose |
| England (L) | Department of Health (http://www.dh.gov.uk) (Department of Health 2007) | Study: National survey data (for governmental and private institutions) N= 12,800 ECT administrations N= 2,272 patients Date: January to March 2002 Time span: Three months | Diagnoses (ICD-10): 81% mood disorders 6.5% schizophrenia, schizotypal, delusional disorder 12.5% other Gender: 71% Women Age, year groups: 0%, <16 0.2%, 16–18 2%, 19–24 23%, 25–44 29%, 45–64 24%, 65–74 22%, >75 | Conditions: 16% Involuntary (Of the 600 patients formally detained while receiving ECT treatment, 60% did not consent to treatment) Other: No patients under 16 years, but 0.2% young patients age 16–18 years Decrease in use of ECT since 1999 | TPR: 1.84* (TPR, women: 2.56 TPR, men: 1.12) AvE: 5.6 (range 4.8–6.2) A-ECT: 19% | No parameters |
| *[Correction added after first online publication on 20 March 2012: The Rate Data for England (L) has been changed.] | ||||||
| Ethnicity: (patients per 100,000 ethnic origin) 4.2 White 1.8 Asian or Asian British 1.2 Black or Black British 1.0 Mixed 2.1 other | ||||||
| Hungary (L) | Gazdag G (Gazdag et al. 2004a) | Study: Semi structured (13 item) questionnaire survey to psychiatric departments. N= 76 departments, 43 answered (Response 57%, ECT not used in 43%) Date: 2002 Time span: One year | Diagnoses: 64% schizophrenia, schizoaffective 32% affective disorder (including mania, organic affective) 4% other Gender: 59% women Age: No information | Legal: Anesthesia obligatory Other: Within-country variability, ECT administered in little over one-half of all departments | TPR: 0.31 iP: 0.6% (up to 2.6%) AvE: 6. (range 3–17) | Modified ECT Anesthesia: 57% propofol 36% thiopental 7% etomidate Devices and type: 52% (sine wave) ICOMAT devices, 38% (brief pulse, square wave, constant currant) Siemans 10% (brief pulse) Thymatron Electrode placement: Mainly bitemporal (BL), also bifrontal (BF) in 2 units and UL in 1 unit |
| Poland (L) | Gazdag G (Gazdag et al. 2009a) | Study: Semistructured questionnaire (20 items) survey to all Polish psychiatric inpatient facilities N= 58 responded facilities (100% response rate) N= 25 confirmed use of ECT, but only N= 20 (34%) facilities administered ECT during study period N= 435 ECT-treated patients in period Date: 2005 Time span: One year | Diagnoses: Depression, mania, schizophrenia and schizoaffective, and other disorders Gender: 65% women Age: >18 years (but six units offered to patients <18 years) | Conditions: Written informed consent obligatory For involuntary approval from court necessary Legal: Requires specialist in anesthesiologist Other: Only one-third of facilities treated patients with ECT during study period. ECT administered under pregnancy in 10 settings | TPR: 0.11 iP: 0.79% (up to 6.46%) AvE: 9 C-ECT: 25% A-ECT: ECT not performed in Polish outpatient clinics | Modified Anesthesia: 58% thiopenthal 23% propofol 15% etomidate 4% midazolam Devices: Mecta JR-1, Mecta SR-1 & Spectrum 5000, Thymatron IV, Pabel ES and Siemens E2077 Type: 30% sine wave 70% brief pulse Placement: All BL Two facilities used UL or BF as second choice |
| Germany (L) | Muller U (Muller et al. 1998) | Study: Questionnaire survey to psychiatric hospitals and university clinics. N= 451 clinics (Response rate 64%) N= 1050 patients ECT treated Clinics (59%) providing ECT were: 82% university clinics 74% state hospitals 48% special hospitals 68% psychiatric wards Date: April to October 1995 Time span: Seven months | Diagnoses (diagnostic indication for ECT given by clinics): 79% catatonia 58% depression 24% malignant neuroleptic syndrome 2% neurological disorders Gender: No information Age: 18–64 years, seldom elderly patients | Side effects reported (common to rare): amnesia, headache, cognitive problems, organic psychoses, dental injuries, neurologic disease Conditions: 20% involuntary (nonconsent) Patient information: 43% oral 42% oral and written 15% written Other: Reasons for not providing ECT: No equipment and not enough knowledge or for political reasons Attitudes: 96% positive | TPR, East Germany: 0.15 TPR, West Germany: 0.36 (between 1992 &1994) TPR total: 0.26 C-ECT:14% | Modified Anesthesia: 64% barbiturate 38% etomidate 20% propofol Devices: 21%Thymatron DG 39% Siemens konvulsator 2077S 2% other machines Type: 21% brief pulse 39% sine wave Dose: 39% titration 18% fixed Placement: 21% UL 19% BL 18% both BL & UL 39% no data |
| Spain (L) | Bertolin-Guillen JM (Bertolin-Guillen et al. 2006) | Study: Questionnaire survey to all hospitals with psychiatric unit in Spain. N= 233 hospitals (response rate 100%) N= 108 (46%) provided ECT (28% prescribed and 25% neither prescribed nor applied ECT) Date: January to June 2001 Time span: Six months | Diagnoses: 34% depression 26% schizophrenia 12% mania 11% psychoses 8% other not diagnostic (including pregnancy, suicide risk) 3% OCD 3% organic 3% other (anxiety, neurotic, personality disorder) No age, gender, or diagnostic information | Conditions: 98.7% informed consent (1.3% involuntary) Training: 92% ECT given of psychiatrist or resident Other: Variety of diagnostic indication. 59 (25%) hospitals neither applied nor prescribed ECT Reasons for not providing ECT: 49% lack of technical means 27% no ECT type of patients | TPR: 0.61 (range 0.03–1.7) AvE: 9 C-ECT:16% of patients C-ECT practice: 35% of institutions using monthly or decreasing frequency regimes | Modified mainly 0.6% unmodified 2.3% without muscle relaxants Type: 65% brief pulse 14% sine wave 3% both 18% unknown Placement: 90% BL |
| Other reasons: therapeutic inefficacy; inexperience; ethical or moral concerns; side effects; bureaucratic problems; lack of protocols; attitudes. | ||||||
| Russia (L) | Nelson AI (Nelson 2005) | Study: Questionnaire survey to 1468 hospitals representing 54 of the 89 Russian states, which represents 80% of the population N= 114 responded hospitals (out of 1468, 8% response rate) N= 52 (out of 114, 46%) provided ECT Date: November 2003 to June 2004 Time span: eight months | Diagnoses: No information No age, gender, or diagnostic information Indication: 71% equivalent to drug therapy 29% last resort 27% medication resistance 25% as first-line treatment 12% as lifesaving | Other: No specific license, credentials or privileging required for provision of ECT Reasons for not prescribing ECT: Lack of equipment or space Unfamiliarity with ECT Absence of consideration Attitudes: 57% positive physician attitudes toward ECT | TPR: 0.54 iP: 1.4% AvE: 8 A-ECT: 2% of institutions C-ECT: 26% of institutions (Although no mention of m-ECT in official Russian ECT guidelines) | Modified and unmodified Unmodified ECT>80% Device: Modern elikon-01 (from Ukraine) EKT-01 FILAT Siemens-400 Siemens konvulsator 2077 Type: 39% brief pulse 26% sine wave Placement: 94% BL 13% UL 4% BF |
| Netherlands (L) | van Waarde JA (van Waarde et al. 2009) | Study: Questionnaire survey sent to 35 University, psychiatric and general hospitals providing ECT. Total N= 142 university, general, psychiatric hospitals 35/142 (25% providing ECT) N= 35 (Response rate 94%, 33 responded) Date: February 2008 Time span: Questionnaire period to psychiatrists, six weeks | Diagnoses: sparse information, ECT administered to patients with comorbid physical diseases, patients with malignant neuroleptic syndrome or other catatonic disorders | Training: 20 of 33 (61%) of institutions trained psychiatrists to administer ECT 50% of psychiatrists had attended certified course in ECT treatment ECT sometimes administered by other profession (geriatrician and physician) Used international guidelines (APA, RCP, DAP) Other: Most institutions had long experience, used ECT five to 25 years (median 18 years) | AvE: 8.5 (per 10,000) C-ECT: Many could manage C-ECT on an outpatient (ambulatory) basis. | Modified Type: Brief pulse and constant current device used according to guidelines 88%. (91% had local protocols) Placement (more than one answer allowed): 55% BL (25% BL only) 2% BF 40% RUL 2% RFT 2% not described Mainly UL first, then change to BL |
| France (L) | Benadhira R (Benadhira and Teles 2001) | Study: Questionnaire survey to all 815 French Psychiatric Public Hospital services N= 391 (response rate 48%) 51% of, responded hospitals administered ECT Period: 1996–1997 Time span: One year | Diagnoses: 63% medication resistant depression 18% schizophrenia 10% mania Gender and age: not reported | Other: Only half of all hospitals in France administer ECT | No rate/prevalence data | Modified Anesthesia: 65% Propofol 24% Thiopenthal Device: 55% Thymatron DG/Mecta SRI 44%Lapipe et Rondepierre Type: brief pulse and sine wave Placement: 18% UL |
| Denmark (L) | Andersson JE (Andersson and Bolwig 2002) | Study: Questionnaire survey to hospitals in Denmark, Greenland, and Faroe Islands N= 35 clinics, (100% response) All provided ECT N= 1556 patients received ECT Period: 1999 Time span: One year | Diagnostic indication from 35 units (%): 35 (100%) depression 28 (80%) delirium 22 (63%) mania 12 (34%) schizophrenia 5 (14%) other | Training: Provided by 49% (17 of 35) institutions. Psychiatrist administering ECT. In most institutions, junior doctors performed ECT. | TPR: 3.0 iP: 5% (1.8–10.0%) AvE: 9 (range 6–18) | Anesthesia, 33 units (%): 28 (85%) Barbiturate 3 (9%) propofol 2 (6%) unknown Devices and Type: Thymatron or Mecta (brief-pulse wave) one Siemens konvulsator device (sine wave) |
| Denmark (L) | Sundhedsstyrelsen (Sundhedsstyrelsen 2011a) | Study: National register data, 2000–2007 N= 17 psychiatric units, hospitals No. of ECT-treated patients/ECT administrations per year: 260/2336 (2000) 313/3237 (2001) 460/4686 (2002) 1399/15,174 (2003) 1563/16,606 (2004) 1786/19,173 (2005) 1774/19,389 (2006) 1772/19,127 (2007) | Main indication: Elderly depressed patients | Side effects: No. of deaths 24 h after ECT in study period = 6 and evaluated as not ECT-related Conditions: Prevalence of involuntary ECT treated patients (supplementary ECT data from same online source (http://www.sst.dk) in Use of coercion in Mental Health Care, 2009 (Sundhedsstyrelsen 2011b): 2.8%[722/25,199] (2002) | AvE per year: 11.1 (2000) 9.2 (2001) 9.8 (2002) 9.2 (2003) 9.5 (2004) 9.3 (2005) 9.1 (2006) 9.2 (2007) | No information |
| Period: 2000–2007 Time span: Seven years | 2.6%[667/25,291] (2003) 2.8%[714/24,872] (2004) 2.9%[734/24,501] (2005) 3.1%[765/24,308] (2006) 3.1%[736/24,129] (2007) 3.3%[821/24,311] (2008) 3.2%[848/26,014] (2009) Guidelines: Not all institutions followed all instructions, developed by Sunhedsstyrelsen guidelines no. 9001, 20 November 2000. Other: High increase in no. of ECT-treated patients from 2000 to 2007. | |||||
| Norway (L) | Schweder, LJ (Schweder et al. 2011a) | Study: Questionnaire survey to psychiatric hospitals, mental health care community centers, including child and adolescent psychiatry about ECT practice. N= 125 (Response rate 54%, but 69% from hospitals) ECT was performed in 72% of the hospitals Date: 2004 Time span: One year | Diagnoses: 70% unipolar depression 19% bipolar depression 1% mania 4% schizoaffective disorders 1% schizophrenia, polymorphic psychoses 3% mixed episodes 1% Parkinson disease 1% other Indication (main): 60% lack of psychopharmacological effect Gender: 65% Women Age, year groups: 0%, <18 8%, 18–24 13%, 25–44 30%, 45–64 55%, >65 | Other: 63% wished to offer more ECT, but unable to due to low capacity Approximately eight weeks waiting list for ECT treatment Reasons for not providing were mostly lack of equipment or anesthesiologist and not large enough institution Attitudes: 96% psychiatrists positive attitudes toward ECT | TPR: 2.4 (significant TPR Regional variation 1.83 to 3.44) iP: 5.3% (range 4.2–6.9%) | |
| Norway (L) | Schweder LJ (Schweder et al. 2011b) | Study: Questionnaire survey about ECT practice to psychiatric hospitals, mental health care community centers, including child and adolescent psychiatry. N= 125 (total response rate 54% and 69% from hospitals) Date: 2004 Time span: One year | No information | Side effects according to much/very much impaired: 26% memory impairment: 5% headache Outcome: 78% very much/much improved 21% minimal/no change 1% worse Conditions: 100% provided information about ECT 50% written informed consent Training/administration: Administration of ECT by 96% junior doctors, with or without psychiatrist present and 6% by nurses Other: Local guidelines, pretreatment examination, equipment, facilities, drugs during ECT also reported | No. of ECTs: 1-3 (7%), 4-6 (23%), 7-9 (30%), 10-12 (24%), >12 (15%) C-ECT practice: 88% of the units C-ECT: 14% of patients A-ECT practice: 63% of the units A-ECT: 15% of patients | Modified Anesthetics: 94% thiopental 6% propofol Device and Type: Thymaton or Mecta device (brief pulse) Placement: 94% UL 63% BL 2% BF |
| Sweden (R) | Socialstyrelsen (http://www.socialstyrelse.se) (Socialstyrelsen 2010) | Study: Pilot study of ECT use in hospitals, in middle region of Sweden Middle Sweden: N= 7 hospitals N= 441 ECT-treated patients, in total population 1.2 mill Skellefteå: One psychiatric unit N= 1029 ECTs N= 109 patients, population 57,530 Date: 2009 Time span: One year | Diagnoses: 55% depression 5% mania or schizophrenia 9% unknown diagnoses Gender: 59% women, Mean age in years: 54.5 (range 15–92) | Other: No national data | TPR Middle Sweden: 3.67 TPR Skellefteå: 1.89 AvE Middle Sweden: 8 (range 1–22) AvE, Skellefteå: 10 | No information |
| Belgium (R) | Sienaert P (Sienaert et al. 2005a) | Study: Questionnaire survey (30 item) sent to all psychiatric hospitals and psychiatric wards, in Flanders and Brussels Capital Region N= 88 (hospitals and wards) N= 23 (100% response rate) 26% providing ECT Date: 2003–2004 Time span: One year | Diagnoses (main indication): 88% major depression 8% schizophrenia 3% mania 1% other Gender and age: Not reported | Training/administration: Administration performed by: 57% psychiatrist 43% trainee psychiatrist without supervision 9% trainee psychiatrist with supervision Guidelines: 44% followed guidelines Other: 75% of psychiatrist had attended a specific ECT course Psycotropic drug use also reported Attitude: 96% expressed a concern of ECT under use | TPR: 4.7 | Modified ECT Anesthesia: 74% propofol 17% thiopental 13% etomidate 4% methohexital 4% ketamine 4% sevoflurane 13% others Device and type: 52% Mecta or Ectron (brief pulse) 30% Siemens konvulsator (sine wave) Dosage: 48% fixed high dose 48% dose titration strategy Placement (more than 1 answer allowed): 65% bitemporal 22% bifrontal 8.6% unilateral 13% used more than one electrode placement |
| Wales, UK (R) | Duffett R (Duffett et al. 1999) | Study: Survey questionnaire and visits to all clinics in Wales. N= 17 hospitals by phone N= 321 patients received ECT Period: first six months in 1996 Time span: Six months | Diagnoses: 82% depression 7% schizoaffective 5% schizophrenia 5% mixed affective disorder 1% mania 1% puerperal psychosis Indication: 80% Failure to respond 13% Life-saving procedure 5% patient choice Gender: 71% women Mean age: 56.9 years women 55.5 years men | Outcome: 59% much or very much impaired 31% improved 1.5% worse Conditions: 9% were given ECT against their consent 20% detained under Mental Health Act Information about pharmacotherapy | TPR: 2.2 AvE: 6.7 (range 1–8) A-ECT: 16% of patients | No information about ECT parameters |
| England (R) | Duffett R (Duffett and Lelliott 1998) | Study: Survey, questionnaire, visits, and telephoning ECT clinics (ECT practice audit) N= 215 clinics (Response rate 84%) N= 130 observed ECT-treated patients Period:1995–1996 Time span: One year | Diagnoses, age: No information Gender: 64% women | Training: 42% had attended an ECT course Usually junior doctors give ECT Guidelines: 36% followed guidelines Other: 7% used old not more recommended device 15% difficulties in obtaining anesthesiologist | No rate data | Modified Anesthesia: 17% propofol Devices: 18% Thymatron 11% Mecta 5% Neurotronics 24% Ectron 5a/b 34% Ectron 5 Type: Brief pulse and sine wave Placement: Mainly BL 7% UL |
| England (R) | Pippard J (Pippard 1992) | Study: Survey, visits by first author to hospitals in North–East Thames (NET) and East Anglian (EA). NET covered 16 health authority districts where ECT was provided in 22 NHS hospitals and three private hospitals (N= 25) EA covered eight health authority districts, where ECT was provided in 13 NHS hospitals and two private nursing homes (N= 15) Date of audit: 1991 Data from:1988–1989 Time span: One year | Other: A practical description of ECT use in the units visited Replacement of old sine-wave devices began in 1982. Guidelines: By Royal college of psychiatrist, 1989 used. Training/administration: Training programs for ECT inadequate and in one-third of hospitals there was almost none. ECT performed by: 25% patients own doctor 74% by duty doctor in training on call | [TPR (NET): 1.47] [TPR (EA): 3.7] [TPRs <1990] | Modified ECT Type: sine wave [Devices in use before 1990: Ecton Mark 4 Series 2+ and 3+ (updated models) Series 5 (1987)] | |
| Ireland (R) | Enriquez S (Enriquez et al. 2010) | Study: Survey of annual reports from Limeric mental health services Data-gathering process N= 126 ECT-treated patients with N= 153 series/courses Period: 2003 to 2008 Time span: Five years | Diagnoses: 95% depression 4% nonaffective psychosis 1% mania Gender: 66% women Age, mean (SD) years: 50.6 (16.7) (range 18–87) | Adverse events: 0.7% cardiac arrests 3% cardiac arrhythmias 0% prolonged seizure 21% cognitive impairment 1.3% respiratory difficulties 0.7% oro-pharyngeal bleeding 1.3% hypotension Conditions: 7% involuntary 14% not able to written consent Other: Annual reports from 2005 to 2007,but with limited information | TPR: 1.7 (variation in use) AvE: 6.5 (range 1–13) A-ECT: 18% | Device: Mecta spectrum 5000M Placement: 85% BL |
| Chuvash republic, Russia (R) | Golenkov A (Golenkov et al. 2010) | Study: Annual statistical hospital reports Date: 1998–2007 | Diagnoses: 88% schizophrenia Gender: 56% women Age, mean (SD) years: 34.4 (10.6) (range 15–64) | Outcome: 10.6% significant improvement 48.9% moderate improvement Consideration: Qualified anesthetist is mandatory Other: 61% of inpatients diagnosed with schizophrenia. Also about attitudes: Authors say answers revealed a high level of false beliefs and markedly negative attitudes | TPR (for 2006 & 2007): 0.8 AvE: 10.3 (SD 2.0) (range 2–20) A-ECT: are lacking | Modified, but only 40% used muscle relaxants Device: Elicon-01 machine Type: Square wave (brief pulse) Placement: BL only |
| Vienna, Austria (C) | Tauscher J (Tauscher et al. 1997) | Study: Prospective study in a hospital. N= 21 ECT-treated patients Date: September 1994 to August 1995. Time span: One year | Diagnoses: 72% Depression 14% schizoaffective psychoses 14% catatonic schizophrenia Gender: 81% women Age, mean years: 49 (range 23–69) | Side effects: 33% headache 14% reversible disorientation or amnesia Outcome: mean CGI: –3.7 Guidelines: Local guidelines as well as by American Psychiatric Association | iP: 3% AvE: 8.9 (range 5–15) | Modified Anesthesia: Propofol or methohexital Device: Thymatron Placement: mainly UL, switch to BL if no effect after 6 ECTs |
| Barcelona (C) | Bernardo M (Bernardo et al. 1996) | Study: Descriptive, interview of hospitals. N= 20 hospitals Date: August 1993 | Diagnoses: 83% depression 17% schizophrenia | No rate data | Type: Mainly sine wave | |
| London, United Kingdom and Bengaluru, India (C) | Eranti SV (Eranti et al. 2011) | Study: Retrospective case note study of all patients referred for ECT and comparison between centers (teaching hospitals) in UK and India N= 46 hospitals, London (Lo) N= 345 hospitals Bengaluru (Be) Date: 2001, London and 2002, Bengaluru Time span: One year | Diagnoses: Depression 89% Lo, 40% Be Manic episodes 4% Lo, 7% Be Schizophrenia & other psychosis 2% Lo, 41% Be Schizoaffective disorder 4% Lo, 4% Be Organic psychosis 0 Lo, 1% Be Catatonia: 0 Lo, 7% Be Indications: Not eating and drinking: 21% Lo, 6% Be Stupor 6% 1 Lo, 10% Be Suicide: 14% Lo, 33% Be Previous good response 18% Lo, 12% Be Treatment resistance 38% Lo, 12% Be Gender (women): 69.6% Lo, 51.2% B Age, mean (SD) years: 62.8 (16.0) Lo 30.3 (10.4) Be | Treatment response Complete recovery: 10% Lo, 26% Be Major improvement: 50% Lo, 55% Be Minor improvement or no change 40% Lo, 19% Be Side effects: Confusion/amnesia: 29% Lo, 12% Be Anesthetic complication 6% Lo, 13% Be Headache 1% Lo, 37% Be Injuries 0 Lo, 2% Be Other: ECT-treated patients were much younger and, more often men in Bengaluru compared to London | IP%: 0.9% Lo 8.2% Be AvE: 8.75 (6.02) Lo 6.67 (2.83) Be | Modified (Lo and Be) Anesthesia: Methohexitone, Propofol, etomidate (Lo) Thiopentone (Be) Type: Brief-pulse wave (Lo and Be) Device: Thymatron DGx (Lo) NIVIQURE (Technonivilac, Bangalore, India) Be Dosage: Half-age method (Lo) Determined by motor seizure threshold (Be) |
| Ethnicity (among depressed patients): Caucasian: 88% Lo, 0 Be Afro Caribbean. 8% Lo, 0 Be South Asian: 4% Lo, 100% Be | ||||||
| Edinburgh, Scotland (C) | Glen T (Glen and Scott 1999) | Study: Register database survey of ECT records at Royal Edinburgh Hospital Total no. of ECT treated patients, by year: N= 145, 1992–1993 N= 138, 1993–1994 N= 93, 1994–1995 N= 94, 1995–1996 N= 78, 1996–1997 Total no. of ECTs, by year: N= 1189, 1992–1993 N= 1013, 1993–1994 N= 774, 1994–1995 N= 557, 1995–1996 N= 696, 1996–1997 Date: 1992 to1997 Time span: Five years | Gender: 71% women Gender age group 18–64: 67% women Gender age group >65: 83% women | The rate of ECT use was on average three times higher for population of age >65 years than in the general adult population “rate of ECT use fell progressively and significantly (p,0.01) from 2.9 to 1.4 treatments” ECT-treated patients in 1997 were 58% less than the number treated in 1992. As measured by the number of treatments per thousand population—there was an overall 53% reduction in rate of ECT use | TPR in age groups 18–64 and >65, by year: 3.4 and 10.3, 1992–93 3.2 and 8.6, 1993–1994 2.3 and 6.1, 1994–1995 2.5 and 4.5, 1995–1996 1.7 and 6.1, 1996–1997 EAR for age groups 18–64 and >65, by year: 2.9 and 7.9, 1992–1993 2.3 and 8.0, 1993–1994 1.9 and 5.1, 1994–1995 1.6 and 2.3, 1995–1996 1.4 and 6.6, 1996–1997 AvE in age group 18–64: Range 6–8 AvE in age group >65: Range 5–10 | Placement: all BL |
| Edinburgh (C) | Okagbue N (Okagbue et al. 2008) | Study: Survey data from computerized ECT treatment records at Royal Edinburgh Hospital No. of patients ECT treated by year: N= 146 (1993) | No information | Other: Four patients younger than 18 years treated before 1998, none after Usage diminished significantly (P < 0.01) over time, for both adult 18–64 and >64 years age groups | TPR by year: 3.3 (1993) 2.9 (1994) 2.1 (1995) 2.1 (1996) 1.8 (1997) 1.6 (1998) 1.4 (1999) | No information |
| N= 130 (1994) N= 94 (1995) N= 95 (1996) N= 78 (1997) N= 73 (1998) N= 62 (1999) N= 71 (2000) N= 76 (2001) N= 64 (2002) N= 60 (2003) N= 61 (2004) N= 61 (2005) Total N= 1071 Periode: 1993 to 2005 Time span:13 years | Some overlapping rate data (1992–1997) to previous reference, Glen T (Glen and Scott 1999) | 1.6 (2000) 1.7 (2001) 1.4 (2002) 1.3 (2003) 1.3 (2004) 1.3 (2005) | ||||
| Munich (C) | Baghai TC (Baghai et al. 2005) | Study: Survey of ECT treated patients at university hospital N= 445 ECT-treated patients N= 4803 ECT administrations Date: 1995 to 2002 Time span: Eight years | Diagnoses: 63% depression 17% schizophrenia 9% bipolar 6% schizoaffective 0.2% mania 2% other Gender: 66% women Mean age: 51.2 ± 15.4 years Side effects: 61% no amnesia 32% mild amnesia 6% severe amnesia 0.3% severe cardiac | iP: 4% | Modified Device and Type: Thymatron (brief pulse) Placement from 2000: 60% UL 35% BL | |
| Dikemark Hospital, Norway (H) | Moksnes KM (Moksnes and Ilner 2010) | Study: Retrospective survey of medical records from three units at Dikemark psychiatric hospital N= 141 ECT-treated patients N= 1960 ECT administrations Period: 1960–1995 Time span: 35 years | Diagnoses: 88% affective disorder 6% organic 6% schizophrenia, schizoaffective Gender: 74% women Age, mean (SD) years: 64 (10.9) (range 29–87) (16%, 29–59 years) | Other: ECT mainly given to elderly population only 16% under 59 years, none under 18 | Prevalence among inpatients: 1990–1995: 1.7% [1980–1989: 1.0%] [1960–1979: 0.3%] AvE: 8 (Average no. of courses 1.7) | Modified Devices: 80% Siemens konvulsator After 1992, the new Thymatron apparatus with brief-pulse wave stimulation |
| Ullevaal University Hospital, Oslo (H) | Moksnes KM (Moksnes et al. 2006) | Study: Retrospective survey of medical records at Dikemark and Ullevaal hospital. N= 383 ECT-treated patients (1988–2002) Date: 1988–2002 Time span: 15 years | Diagnoses: No information Gender: 69% women Age in years: mean women: 67 mean men: 65 (range 23–91) (58% > 65) | Guidelines: Local developed by author, Dikemark Hospital in accordance with International by APA and Royal College of Physician Data for [1988: 0.5–1.7%] [1989: 0.7–2.8%] | TPR 2002: 2.8 iP and EAR, by year: 0.8% and 2.8, 1990 1.5% and 4.8, 1991 2.1% and 9.2, 1992 2.1% and 10.7, 1993 1.9% and 7.4, 1994 2.4% and 11.1, 1995 3.8% and 16.5, 1996 3.2% and 15.0, 1997 5.2% and 19.3, 1998 5.7% and 24.9, 1999 3.3% and 15.1, 2000 4.0% and 20.3, 2001 2.9% and 14.5, 2002 AvE: 8.8 | Modified Devices: Until 1995 Siemens konvulasor After 1995 Thymatron Type: sine wave until 1995 and brief pulse >1995 Placement: UL |
| Hospital Innland, Norway (H) | Eiring O (Eiring 2010) | Study: Health region “Innlandet” psychiatric hospital ward survey, three local hospitals N= 162 ECT-treated patients Date: 2008 Time span: One year | Diagnoses: No information | No information about diagnoses | TPR: 4.3 (Calculated by authors according to national resident population data from http://www.ssb.no. Population “Innlandet” 2006: 371714 (162/371714) AvE: Range 6–8 | Modified Dosage: Age-dose or stimulus-titration method Placement: RUL or BL |
| Pitkaniemi Hospital, Finland (H) | Huuhka MJ (Huuhka et al. 2000) | Study: Clinical record survey of all ECT-treated patients at hospital in 1944, 1964, and 1997. N= 46 patients (1997) N= 2289 ECT treatments (1997) Dates: [1994, 1964] 1997 Time span: One year | Diagnoses (1997): 78% Affective disorders 22% Schizophrenia Gender (1997): 76% women Age, mean years (1997): 58.9 (range 18–83) | Side effects (1997): 24% some problems during the treatment, none serious 13% amnesia 9% headache 2% minor cardiac complication Conditions (1997): 26% Involuntary | iP (1997): 2.0% AvE (1997): 8 (range 3–12). | (1997) Modified Anesthesia: Propofol or methohexital, and succinylcholine muscle relaxant 100% oxygenation Device: Siemens konvulsator 2077 Placement: BL only |
| Other: Drop in iP over time from 14.4%, 1944 to 2.2% in 1964 and 2.0% in 1997. In 1944 and 1964, main indication schizophrenia, whereas in 1997 >75% had affective disorders. ECT was administered unmodified in 1944 and 1965. ECT administered more often to young men with schizophrenia in 1944 and 1964. Use of psychotropic drug treatment during ECT | Monitoring: Oxymetry and EEG monitored Cuff method used Other: Treatment frequency, 3 times weekly | |||||
| Hospital, Istanbul, Turkey (H) | Saatcioglu O (Saatcioglu and Tomruk 2008) | Study: Retrospective case review study of ECT-treated patients admitted to Bakirkoy Research and Training Hospital for Psychiatric and Neurological Diseases, Istabul N= 1531 patients and N= 13,618 ECT administrations Date: 1 January 2006 to 30 June 2007 Time span: One and half year | Diagnoses: 37% schizophrenia, schizoaffective 30% bipolar 15% depressive disorder 14% nonorganic Psychotic disorder 4% Other (OCD, substance abuse) Gender: 44% women Age, mean (SD) years: 35.1 (10.9) Age, year groups: 1%, <18 15%, 18–24 65%, 25–44 17%, 45–64 1%, >64 Side effects: 79.7% Memory problems 34.5% Headache 27.8% Muscle pain | Outcome: Improvement: 79% completely 19% partially 2% minimum | iP: 12% AvE: 9 (range 1–18) | Modified Anesthesia Propofol & succinylcholine (muscle relaxant) & oxygenation Device: Thymatron IV Type: Brief pulse Placement: Bifrontotemporal (BL) standard |
| Scotland (H) | Fergusson GM (Fergusson et al. 2004) | Study: Audit of clinics from 1997 to 1999 N= 36 sites providing ECT ECT-treated patients: N= 794 (1997) N= 717 (1999) Date: February 1997 to July 1999 Time span: Two years and five months | Diagnoses: 87% depressive episode 6% schizophrenia/ schizoaffective 3% manic episode Indications for ECT: 55% resistant to antidepressants 39% previous good response Gender: 70% women Age (ECT among depressed inpatients), year groups: 3.4%, 15–24 4.8%, 25–44 11.6%, 45–64 13.6%, 65–74 12.7%, >75 Ethnicity: Mainly (99%) to white adult patients suffering from a depressive disorder | Conditions: 18% receiving treatment under the safeguards of the Mental Health (Scotland) Act 1984 Gender comment: Ratio of women to men, approximately: 2:1. Age comment: ECT not given disproportionately to the elderly Legal status: 76% voluntary (involuntary 24%) 82% consent given 18% under Mental Health (Scotland) Act of 1984 Training and supervision: Initial training of junior doctors evaluated good, but difficulties in providing continued supervision. Clinical global index scale (CGI): 61% of the 29 patients with schizophrenia and 68% of the 13 patients with manic-episode were rated as at least “much improved” and none as worse | EAR (1997): 15.5 EAR (1999): 13.0 AvE (1997): 6.8 AvE (1999): 6.6 AvE (total): 7 (range 1–19) | 95% BL (in accordance with advice in the Royal college of psychiatrists handbook, 1995) Equipment evaluated as: All, up to date |
| Cukurova University Psychiatry Service, Turkey (H) | Zeren T (Zeren et al. 2003) | Study: Retrospective chart review of hospital ECT-treated patients at Cukurova University, Department of psychiatry. University, Dept. of psychiatry. N= 384 ECT-treated patients Date: 1990–2001 Time span: 12 years | Diagnoses: 45% psychotic 49% affective 6% other (including postpartum psychoses, dissociative, personality disorders, obsessive compulsive) Gender: 52% women Age, year groups: 5%, <18 92%, 18–64 3%, >64 Mean age 33.1 years Education: Average no. of education years: 8.7. 54% of patients undergoing ECT had high school and higher education | iP: 14% AvE: 8 Side effects: 53% for unmodified 41% for modified (memory impairment, muscle pain, headache, confusion, prolonged seizure, cardiovascular, ECT induced mania/hypomania, bone fracture) Outcome: 82% moderate to marked improvement | Unmodified N= 179 (47%) Modified N= 205 (53%) Since 1996 all ECT performed under anesthesia. Until 1996 use of anesthesia judged according to age (<40 years) or medical condition. Device constant current brief pulse Siemens Placement: all BL (bitemporal) Frequency: 3 times week | |
TPR: treated person rate = persons ECT treated per 10,000 resident population per year.
EAR: ECT administration rate = no. of ECTs administered per 10,000 resident population.
iP: inpatient prevalence = proportion (percent,%) ECT treated among inpatient population.
AvE: average number of ECTs administered per patient (in a session or course).
C-ECT: continuation-ECT.
A-ECT: ambulatory-ECT.
Table C5.
Asia N= 15.
| Country | Reference id | Reference | Study | Demographics | Other data | Rates | Technical parameters |
|---|---|---|---|---|---|---|---|
| Land (L) | Ref. id | First autdor (reference) | Study design | Diagnoses | Side effects | TRP* | Modified/Unmodified |
| Region (R) | N | Indication | Outcome | EAR* | Anesthesia | ||
| City (C) | Date | Gender | Conditions | iP* | Devices | ||
| Hospital (H) | Time span | Age | Training | AvE* | Current type | ||
| Ethnicity | Guidelines | Electrode placement | |||||
| Legal regulations | C-ECT** | Dosage | |||||
| Other | A-ECT** | (Monitoring) | |||||
| Japan (L) | 295 | Motohashi N (Motohashi et al. 2004) | Study: Questionnaire survey to university and national hospitals N= 121 hospitals (71% response rate) N= 56 providing ECT (65%) and given a new questionnaire (82% response rate) Date: Between 1997 and 1999 Time span: Three years | Diagnoses (no numbers): Depression Schizophrenia Schizoaffective disorder Indications: Stupor, catatonic, or manic excitement, and suicide risk Other: Elderly or patients with medical conditions received most modified ECT | Side effects (major of modified): amnesia, delirium, headache Side effects (major of unmodified): amnesia, bone fracture, delirium, prolonged apnea Conditions: Consent obtained at least from families Guidelines used in 28% of institutions Other: Number of ECTs administered per year varied from 0.5 to 120 | AvE: Range 5–10 | 33% modified 20% (N= 9) facilities used only unmodified ECT Anesthetic agents: amobarbital, thiamylal, thiopental and propofol Devices: Constant voltage sine-wave current approved ECT devices Type: Sine wave Placement: 100% BL UL only sometimes used at one unit |
| Japan (L) | 1954 | Chanpattana W (Chanpattana et al. 2005a) | Study: Questionnaire (29 item) survey sent to head of the psychiatry department of university hospitals, director of psychiatric, and general hospitals. N= 248 hospitals contacted N= 100 (33 university, 33 psychiatric, 34 general) (40% response rate) | Diagnoses: 50% schizophrenia 37% major depression 7% catatonia 4% mania 2% other (dysthymia, neuroleptic malignant syndrome, personality disorder, Parkinson, other) | Psychiatrist administered ECT unassisted at one hospital. Practice of continuation and maintenance-ECT (M-ECT) in 18 hospitals. M-ECT given to 20% to 1% of ECT patients. Training programs for psychiatry residents in 65 (78%) hospitals, rated as | AvE: 9 | 55% unmodified: (670 patients received 6364 unmodified ECTs, 57% of total number of treatments at 60 (72%) institutions (14 university, 23 psychiatric and 23 general hospitals) |
| N= 83 (83%) provided ECT N= 1210 patients treated N= 11,146 ECTs Date: 2001–2003 | Gender: women 54% Age, year groups: 2%, <18 3%, 18–24 15%, 25–44 40%, 45–64 39%, >64 | inadequate/fair to nonexistent/poor in seven hospitals. Consent: Written informed consent from family member in 48 hospitals, informal consent in three hospitals | Devices: Mainly Sakai-C1 (Japanese built sine-wave ECT device) and some Thymatron DGx Type: 58% sine wave 19% brief pulse 6% both 17% did not know | ||||
| Thailand (L) | 2139 | Chanpattana W (Chanpattana and Kramer 2004) | Study: Questionnaire survey sent to 67 hospitals/psychiatric units/institutions in Thailand. N= 53 responded (response rate 79%) ECT provided by: N= 26 (49%) hospitals N= 6,914 (approximately) patients received N= 51,565 ECT treatments Date: September 2001 to August 2002 Time span: One year | Diagnoses: 74% schizophrenia 16% mania or major depression 7% catatonia 2% drug abuse 1% other (psychotic, dysthymia, personality disorder, obsessive compulsive disorder) Gender: 28% women Age, year groups: 4%, <18 24%, 18–24 53%, 25–44 16%, 45–64 3%, >64 | Side effects: Memory loss, headache, muscle pain, teeth injury, fracture but no deaths in survey period Conditions: Written informed consent mainly obtained from family members Training: Five of 26 (19%) institutions with acceptable training Other: 94% received treatments in psychiatric hospitals Mortality rate estimated: 0.08% (no ECT-related death in survey period) Reasons for not providing ECT: Facility too small and is an unnecessary treatment Reasons for unmodified ECT: lack of anesthesiologist, convenience, lack of personnel, lack of equipment, economy, risk of anesthesia | TPR: 1.15 AvE: 7 C-ECT practice: 42% (11 of 26) institutions given for six to nine months to prevent relapse A-ECT and C-ECT are practiced | 94% unmodified Devices: 46% MECTA Spectrum, MECTA SR-1, or Thymatron DGxn, 8% two brands 35% Ectonus 5A, Ectonustim, Ectron, Medcraft B-25, and Siemens konvulasor 11% unknown Type: 42% brief pulse 12% sine wave 46% unknown Placement: All BL |
| Asia, Pacific Region (L) | 3715 | Little JD (Little 2003) | Study: Survey by mail to practitioners attending first Asian pacific ECT conference and 3361 brochures sent out by automatic mailing system to countries in Asia Pacific Region. Contact addresses for 23 of 34 countries identified. N= 12 responses from practitioners having practiced in 12 countries N= approximately 668 patients ECT treated N= approximately 2257 inpatients Date: 2000 Time span: One year | Diagnoses: 68% schizophrenia 18% mania 4% depression Other: Data from countries Fiji Kiribati, Malaysia (USM), Malaysia (Sabah), Nepal Palau, Philippines, Solomon Island, and Thailand. ECT not available: Brunei, Cambodia, Micronesia, Palau | Side effects: (reported not common), memory impairment most commonly reported Outcome: Response rate to ECT approximately 86% Other: No ECT services in Brunei, Cambodia, Micronesia and Palau Other: Indicates large variation in practice in Asia Pacific Region. Attitudes: Cultural attitude generally negative, except for the Philippines where ECT was generally well accepted | iP: Varied from 1% to 9%, except for Nepal 26% | Modified Devices: Thymatron in Malaysia and Thailand Mecta in Nepal and Thailand Ectonus series 5B in Sabah (a state of Malaysia) Type: All brief-pulse wave, except sine wave in Kiribati and Solomon Islands Placement: BL preferred |
| Asia (L) | 561 | Chanpattana W (Chanpattana et al. 2010) | Study: Survey (29 item) questionnaire of ECT-treated patients to psychiatric treatment facilities and countries in Asia N= 977 psychiatric facilities (334 responded, response rate 34%), N= 45 countries in Asia (Russia excluded) (29 responded, response rate 64%) N= 23 of 29 (79%) countries provided ECT in 257 institutions N= 39,875 patients who received N= 240,314 ECTs | Diagnoses: 42% schizophrenia 32% major depression 14% mania 7% catatonia 2% drug abuse 2% dysthymia 1% other Gender: 38% women Age, year groups: 6%, <18 29%, 18–24 44%, 25–44 17%, 45–64 4%, >64 | Countries (N= 23) in survey with ECT practice: Bangladesh, China, Hong Kong, India, Indonesia, Iran, Iraq, Israel, Japan, Jordan, South Korea, Malaysia, Myanmar, Nepal, Oman, Pakistan, Philippines, Singapore, Sri Lanka Thailand, Turkey, United Arab Emirates, Vietnam Countries (N= 6) in survey without ECT practice: Bhutan, Brunei, Cambodia, Georgia, Laos, and Lebanon | AvE: 7 [N= 129,906 unmodified ECTs administered to N= 22,194 patients (55.7%) at N= 141 (54.9%) institutions in N= 14 (61%) of the 23 countries] | Unmodified: 36% unmodified always 19% unmodified, ranging from 1–98% of the time Modified: 45% always modified Anesthesia: 30% institutions used anesthetic agents (thiopental, propofol, sevoflurane, diazepam, thiamylal, flunitrazepam, methohexital) without muscle relaxant |
| Date: 2001–2003 | Other: Large variation in Asian countries Unmodified in 36% and sine wave in 42% of institutions Only 45% always modified, that is,. never unmodified | N= 8 of 141 (5.7%) institutions (four Japan, three Malaysia, one South Korea used routinely succinylcholine muscle relaxant without anesthesia Devices: 58% (115/197) institutions brief-pulse ECT devices Placement: 77% BL Monitoring: 23% of institutions used EEG | |||||
| Katmandu, Nepal (C) | 114 | Ahikari SR (Ahikari et al. 2008) | Study: Naturalistic prospective hospital (Kathmandu Medical College Teaching Hospital) study. N= 210 hospital admitted patients N= 47 ECT treated Date: May 2005 to April 2006 Time span: One year | Diagnoses: 34% schizophrenia, psychotic disorder 23% severe (major) depression 28% bipolar depression 15% other Gender: 28% women Age, years in groups: 11%, 10–19 57%, 20–29 19%, 30–39 6%, 40–49 6%, 50–59 | Other: Psychotropic drugs used concurrently | iP: 22% AvE: 6 (range 2–16) | Modified Anesthesia: Propofol or Sodium Thiopental plus Succinylcholine muscle relaxant Device: ECTON constant current brief-pulse ECT device, manufactured by RMS, Chandigarh, India. Type: All brief pulse in study |
| Hong Kong (C) | 2296 | Chung KF (Chung 2003) | Study: Prospective questionnaire survey of treated patients to all public hospitals with ECT treatment facilities 40 public hospitals in Hong Kong, and nine of 13 inpatient psychiatric services with ECT treatment facilities N= 167 ECT-treated patients | Diagnoses (for N= 164): 40% depression 23% schizophrenia 19% bipolar, manic or mixed 10% bipolar, depressed 9% schizoaffective 1% acute or transient psychotic disorder Indications: Mainly failure to respond to alternative treatment, | Side effects: Memory outcome: 1% much worse 24% worse 71% no change 4% improved Outcome: 83% Much or very much improved 13% minimally improved 2% no change 3% worse | TPR: 0.27–0.34 iP: 1.3–1.8% AvE: 7.7 Range 5–8 A-ECT and C-ECT: Rarely used | No information about anesthesia Devices: All Mecta US domestic version SR1 except one facility using Mecta Spectrum 5000M. Placement: 77% BL 119 22% UL 34 1% mixed |
| Date: April 2001 to March 2002 Time span: One year | Gender: 68% women Age, year groups: 3%, <16 2%, 16–7 11%, 18–24 44%, 25–44 25%, 45–64 14%, 65–80 1%, >80 (total 15% >65 years) | Conditions: 13% Involuntary (judged incapable of giving informed consent) | |||||
| Hong Kong (C) | 441 | Chung KF (Chung et al. 2003) | Study: Survey, (postal questionnaire and site visit) to public inpatient psychiatric units in Hong Kong. (Response rate 100% from public ECT units and 91% from private psychiatric service) N= 13 psychiatric units, and 8 (62%) providing ECT Date: October 1999 to August 2000 Time span: One year | No information | Training: Junior doctors given informal ECT briefing and at least one supervised ECT administration before treatment on their own Other: Hospital policy required patient assessment every one to two treatments during ECT course, but only practiced in four of nine patients observed | TPR (1998): 0.34 | Modified and unmodified. Anesthesia: 87% provided anesthesia Devices: Seven Mecta US domestic version SR1. One Mecta spECTrum 5000M. Three of four private units had Ectron Mark 4. Dose: 63% used preselected stimulus dosing Placement: BL |
| India (H) | 218 | Chanpattana W (Chung et al. 2003) | Study: Survey questionnaire (29 items) about ECT practice during the last year, to all medical colleges and psychiatric hospitals in India. N= 188 contacted institutions N= 74 responded (Response rate 39%) | Diagnoses: 37% schizophrenia 34% major depression 18% mania 6% catatonia 3% dysthymia 2% personality disorder, Parkinson's disease, neuroleptic malignant syndrome, other | Side effects: headache, muscle pains, memory problems, and with unmodified fractures, dislocations, teeth injury, one death Training: reported ECT teaching program 89% to medical students 59% psychiatry residents | AvE: 6 C-ECT: Variation from 1–10% to 60% of patients | Unmodified and modified. N= 20 (30%) institutions always unmodified Anesthetic agents in use sometimes (and not always together): Thiopental, diazepam, methohexital. Succinylcholine and atropine |
| N= 66 of 74 (89%) administered ECT N= 19,632 patients received 114,111 ECTs in survey period N= 10,234 (52%) patients received 52,459 unmodified ECTs in 33 (50%) institutions Date: September 2001 to August 2002 Time span: One year | Gender: women 39% Age, year groups: 1%, <18 6%, 18–24 34%, 25–44 44%, 45–64 15%, >65 | Other: Reasons for unmodified ECT: MemoryLack of anesthesiologist, lack of equipment, lack of personnel, contraindication for anesthesia, emergency, convenience, and economic purpose | Devices: 30% Indian built ECT devices 66% no report of device name [only one MECTA-JR2 or Thymatron DGx] Type: 50% brief pulse 30% sine wave 9% both wave types 11% unknown Placement: 82% BL always 15% BL mainly | ||||
| Chulalongkorn Memorial Hospital, Thailand (H) | 173 | Lalitanatpong D (Lalitanatpong 2005) | Study: Medical hospital record survey of patients admitted to psychiatric ward. N= 51 ECT treated Date: August to September 2004 Time span: One month | Diagnosis and (mean age in years): 49% schizophrenia—(35.5) 23% bipolar—(38.1) 8% acute psychosis—(24.0) 6% depression—(47.7) 4% dementia—(75.5) 10% other—(27.6) ECT indication: severe violence, suicide, refractory treatment Gender: 63% women Age, mean years: 36.7 | Side effects (most common): headache, transient amnesia, dental complications Mean length of stay in days for ECT treated 25.9 ± 15.8 compared to non-ECT treated 17.8 ± 12.7 (difference not significant) | No prevalence or rate data A-ECT: Practiced | Modified Type: Multiple ECT types stated, otherwise no information |
| Pamela Youde Nethersole Eastern Hospital, Chai Wan, Hong Kong (H) | 527 | Chung JPY (Chung et al. 2009) | Study: A retrospective review of case records at hospital in Hong Kong serving 0.8 million. N= 34 ECT-treated patients Date: June 2006 to April 2009 Time span: Three years | Diagnoses: 65% depression 23% bipolar 6% schizophrenia 6% schizoaffective Gender: 88% women Age, mean (SD) years: 62 (19) (range, 21–87) 60% >65 years or older | Side effects: 71% headache, postictal confusion, nausea, dizziness, memory loss (most common)—dental injury, transient bradycardia, oxygen desaturation bronchospasm (less common) | iP: 0.6% AvE: 6 (range 3–10) | Modified Device: MECTA Spectrum 5000Q constant current stimulus Type: Brief-pulse wave Placement: BL |
| Tokushima, University Hospital, Japan (H) | 7782 | Ishimoto Y (Ishimoto et al. 2000) | Study: Retrospective review of patient charts at university hospital N= 185 ECT-treated patients N= 3067 admitted patients Date: Between 1975 and 1997 Time span: 23 years | Diagnoses: 71% schizophrenia 6% manic depressive psychosis 5% atypical psychosis 14% psychogenic reactions 4%other Indication: Drug resistance or need of rapid improvement Gender: 51% women Age, mean (SD) years: 27.5 (8.8) (range 13–59) | Side effects: 37% of patients—amnesia, headache, pyrexia. One case of compression fractures of vertebrae Other: Assistants restrained patients shoulders, arms and thighs to prevent extreme motion | iP: 6% AvE: 10 (range 1–43) | Modified, but without muscle relaxant Anesthesia: Thiamylal sodium (short-acting barbiturate) Device: C-1 Sakai Medical, Tokyo, Japan. Type: Sine wave (according to device type) Placement: BL Monitoring: Pulse and blood pressure check |
| Hospital, Saudi Arabia (H) | 2640 | Alhamad AM (Alhamad 1999) | Study: Retrospective clinical review of all ECT-treated inpatients at King Khalid University hospital N= 127 ECT-treated patients Date: 1985 to 1994 Time span: 10 years | Diagnoses: 61% major depressive illness (unipolar, bipolar, postpartum, and atypical depression) 13% manic episode (bipolar mixed state, postpartum) 9% schizoaffective 11% schizophrenia 3% brief reactive, organic psychoses 2% other Indication: 69% no response to medication 35% as a first-choice emergency treatment Gender: 60% women Age, mean (SD) years: 27.9 (9.23) (range 15–60) Ethnicity: 82% Saudi Arabian Other: 94% living in urban area 52% married 52% secondary, university, or higher education level | Side effects: 3.6% amnesia or disorientation Outcome: 76% good response 79% of nonresponders were schizophrenic patients 59% maintained long term improvement Training/administering A two-lecture course on ECT every year for junior doctors and practical demonstration and training ECT given by junior doctors Consent: Patients have to sign informed consent, counter-signed by a near relative | iP: 5% AvE: 8 | Modified Muscle relaxant mainly suxamethonium Device: Siemens konvulsator 2077S Type: Brief pulse Placement: BL |
| Hospital, Karachi, Pakistan (H) | 3515 | Naqvi H (Naqvi and Khan 2005) | Study: Retrospective study N= 136 ECT treated of total 4013 admitted patients N= 126 (Data available for only 126 [93%[ECT-treated patients) Date: January 1990 to January 2003 Time span: Three years | Diagnoses: 69% major depressive disorder 10% bipolar 5% schizophrenia 4% postpartum depression 2% schizoaffective 2% paranoid psychosis 3% brief psychotic disorder 5% others Indications: Drug resistance, life-threatening situation Gender: 56% women Age%, year groups: 48%, 20–40 38%, 41–50 7%, >60 | Side effects: Tongue biting, loosening of dentures, postictal malaise, confusion, headache. One case of arrhythmia and ECT terminated Consent: Written informed consent when family agree | iP: 3.4% AvE: 6 (range 1–20) | Modified Device and type: Brief pulse, constant-current device Placement: BL Monitoring: Observation of seizures, no EEG |
| Al Ain, United Arab Emirates (H) | 4055 | Tewvik KD (Tewfik et al. 1998) 1998 | Study: Computerized psychiatric inpatient register N= 51 ECT treated Date: 1995 and 1996 Time span: Two years | Diagnoses: 43% depression 43% schizophrenia 8% schizoaffective 6% other Age, mean (SD) years: 30.1 (10.5) Gender: 33% women | iP women: 6% iP men: 4% [total iP (approximately): 5%] AvE: 6. | Modified No anesthesia or device type information Placement: BL | |
TPR: treated person rate = persons ECT treated per 10,000 resident population per year.
EAR: ECT administration rate = no. of ECTs administered per 10,000 resident population.
iP: inpatient prevalence = proportion (percent,%) ECT treated among inpatient population.
AvE: average number of ECTs administered per patient (in a session or course).
C-ECT: continuation-ECT.
A-ECT: ambulatory-ECT.
References
- Agarwal AK, Andrade C, Venkataswamy Reddy M. The practice of ECT in India: issues relating to the administration of ECT. Indian J. Psychiatry. 1992;34:285–297. [PMC free article] [PubMed] [Google Scholar]
- Ahikari SR, Pradhan SN, Sharma SC, Shrestha BR, Shrestha S, Tabedar S. Diagnostic variability and therapeutic efficacy of ECT in Nepalese sample. Kathmandu Univ. 2008;6:41–48. [PubMed] [Google Scholar]
- Alhamad AM, al-Haidar F. A retrospective audit of electroconvulsive therapy at King Khalid University Hospital, Saudi Arabia. East Mediterr. Health J. 1999;5:255–261. [PubMed] [Google Scholar]
- Alhamad AM. The use of ECT in the treatment of psychiatric disorders in a teaching hospital in Saudi Arabia. Bahrain Med. Bull. 1999;21:52–55. [Google Scholar]
- Weiner RD, editor. American Psychiatric Association. The Practice of electroconvulsive therapy: recommendations for treatment, training, and privileging: a task force report of the American Psychiatric Association. VII. Washington, DC: The American Psychiatric Association; 2001. p. 355. [Google Scholar]
- Andersson JE, Bolwig TG. Electroconvulsive therapy in Denmark 1999. A nation-wide questionnaire study [Danish] Ugeskr Laeger. 2002;164:3449–3452. [PubMed] [Google Scholar]
- Andrade C, Agarwal AK, Venkataswamy Reddy M. The practice of ECT in India: II. The practical administration of ECT. Indian J. Psychiatry. 1993;35:81–86. [PMC free article] [PubMed] [Google Scholar]
- Andrade C, Chanpattana W, Kramer B, Kunigiri G, Gangadhar B, Kitphati R. The practice of electroconvulsive therapy in Asia: variations and deviations from the guidelines—a response to Dr Grunhaus. J. ECT. 2010;26:34–36. doi: 10.1097/YCT.0b013e3181d03773. [DOI] [PubMed] [Google Scholar]
- Baghai TC, Marcuse A, ller HJ, Rupprecht R. Electroconvulsive therapy at the Department of Psychiatry and Psychotherapy, University of Munich. Development during the years 1995–2002 [German]. Nervenarzt. 2005;76:597–612. doi: 10.1007/s00115-004-1813-5. [DOI] [PubMed] [Google Scholar]
- Baudis P. Electroconvulsive therapy in the Czech Republic 1981–1989 [Czech] Cesk Psychiatr. 1992;88:41–47. [PubMed] [Google Scholar]
- Benadhira R, Teles A. Current status of electroconvulsive therapy in adult psychiatric care in France [French] Encephale. 2001;27:129–136. [PubMed] [Google Scholar]
- Benbow SM, Bolwig TG. Electroconvulsive therapy in Scandinavia and the United Kingdom. In: Swartz CM, editor. Electroconvulsive and neuromodulation therapies. New York: Cambridge Univ. Press; 2009. pp. 236–245. [Google Scholar]
- Berg JE. Electroconvulsive treatment-more than electricity?: an Odyssey of facilities. J. ECT. 2009;25:250–255. doi: 10.1097/YCT.0b013e3181a2f23e. [DOI] [PubMed] [Google Scholar]
- Bernardo M, Arrufat F, Pintor L, Catarineu S, Buisan E, Ballus C. Patterns of the use of electroconvulsive therapy in Barcelona [Spanish] Med. Clin. (Barc) 1996;106:201–204. [PubMed] [Google Scholar]
- Bertolin-Guillen JM, Peiro-Moreno S, Hernandez-de-Pablo ME. Patterns of electroconvulsive therapy use in Spain. Eur. Psychiatry. 2006;21:463–470. doi: 10.1016/j.eurpsy.2004.11.005. [DOI] [PubMed] [Google Scholar]
- Cerletti U, Bini L. Un nuovo metodo di shockterapie: ‘l’ elettroshock’ (riassunto) Rome: Reale Accademia Medica (Communicazione alla seduta del 28 maggio 1938-XVI della Reale Accademia Medica di Roma.); 1938. [Google Scholar]
- Chang SS. Electroconvulsive therapy in Asia. In: Swartz CM, editor. Electroconvulsive and neuromodulation therapies. New York: Cambridge Univ. Press; 2009. pp. 256–265. [Google Scholar]
- Chanpattana W, Kramer BA. Electroconvulsive therapy practice in Thailand. J. ECT. 2004;20:94–98. doi: 10.1097/00124509-200406000-00004. [DOI] [PubMed] [Google Scholar]
- Chanpattana W, Kramer BA, Kunigiri G, Gangadhar BN, Kitphati R, Andrade C. A survey of the practice of electroconvulsive therapy in Asia. J. ECT. 2010;26:5–10. doi: 10.1097/YCT.0b013e3181a74368. [DOI] [PubMed] [Google Scholar]
- Chanpattana W, Kunigiri G, Kramer BA, Gangadhar BN. Survey of the practice of electroconvulsive therapy in teaching hospitals in India. J. ECT. 2005b;21:100–104. doi: 10.1097/01.yct.0000166634.73555.e6. [DOI] [PubMed] [Google Scholar]
- Chanpattana W, Kojima K, Kramer BA, Intakorn A, Sasaki S, Kitphati R. ECT practice in Japan. J. ECT. 2005a;21:139–144. doi: 10.1097/01.yct.0000169503.80981.c9. [DOI] [PubMed] [Google Scholar]
- Chanpattana W. A questionnaire survey of ECT practice in Australia. J. ECT. 2007;23:89–92. doi: 10.1097/YCT.0b013e318031bc50. [DOI] [PubMed] [Google Scholar]
- Chanpattana W. One hundred twenty years of mental health care in Thailand and the development of electroconvulsive therapy. J. ECT. 2010;26:11–13. doi: 10.1097/YCT.0b013e3181c185f9. [DOI] [PubMed] [Google Scholar]
- Chung JPY, Yim PHW, Dunn ELW. Clinical and treatment characteristics of Chinese patients undergoing electroconvulsive therapy in an acute psychiatric unit in Hong Kong. Hong Kong J. Psychiatr. 2009;19:150–154. [Google Scholar]
- Chung K-F, Ng Y-K, Yiu G-C, Cheung H-K. Electroconvulsive therapy in Hong Kong. Psychiatr. Bull. 2003;27:102–104. [Google Scholar]
- Chung KF. Electroconvulsive therapy in Hong Kong: rates of use, indications, and outcome. J. ECT. 2003;19:98–102. doi: 10.1097/00124509-200306000-00008. [DOI] [PubMed] [Google Scholar]
- Creed P, Froimson L, Mathew L. Survey of the practice of electroconvulsive therapy in North Carolina. Convuls. Ther. 1995;11:182–187. [PubMed] [Google Scholar]
- Department of Health. Electro convulsive therapy: survey covering the period from January 2002 to March 2002. 2007. Available at http://www.dh.gov.uk/en/Publicationsandstatistics/Statistics/StatisticalWorkAreas/Statisticalhealthcare/DH_4000216. Updated 8 Feb 2007 (accessed January 6, 2011) [Google Scholar]
- Duffett R, Lelliott P. Auditing electroconvulsive therapy. The third cycle. Br. J. Psychiatry. 1998;172:401–405. doi: 10.1192/bjp.172.5.401. [DOI] [PubMed] [Google Scholar]
- Duffett R, Siegert DR, Lelliott P. Electroconvulsive therapy in Wales. Psychiatr. Bull. 1999;23:597–601. [Google Scholar]
- Eiring O. First in Norway with treatment flow chart for ECT [Norwegian] PsykNytt [serial on the Internet] 2010;8:3–5. http://www.helsebiblioteket.no (accessed 1 December 1, 2010) [Google Scholar]
- Enns MW, Reiss JP, Chan P. Electroconvulsive therapy. [Position Paper 1992–27-R1] Can. J. Psychiatry. 2010;55:1–12. doi: 10.1177/070674379203701001. Available at http://publications.cpa-apc.org/media.php?mid 978 (accessed January 13, 2011) [DOI] [PubMed] [Google Scholar]
- Enriquez S, Tighe S, Fitzgibbon N. Five years of ECT: the relationship between consent status and treatment experiences. Ir. J. Psychol. Med. 2010;27:117–122. doi: 10.1017/S0790966700001270. [DOI] [PubMed] [Google Scholar]
- Eranti SV, McLoughlin DM. Electroconvulsive therapy—state of the art. Br. J. Psychiatry. 2003;182:8–9. doi: 10.1192/bjp.182.1.8. [DOI] [PubMed] [Google Scholar]
- Eranti SV, Thirthalli J, Pattan V, Mogg A, Pluck G, Velayudhan L, Chan J, Gangadhar BN, McLoughlin DM. Comparison of electroconvulsive therapy practice between London and Bengaluru. J. ECT. 2011;27:275–280. doi: 10.1097/YCT.0b013e31820f8f7c. [DOI] [PubMed] [Google Scholar]
- Fergusson G, Hendry J, Freeman C. Do patients who receive electroconvulsive therapy in Scotland get better? Results of a national audit. Psychiatr. Bull. 2003;27:137–140. [Google Scholar]
- Fergusson GM, Cullen LA, Freeman CPL, Hendry JD. Electroconvulsive therapy in Scottish clinical practice: A national audit of demographics, standards, and outcome. J. ECT. 2004;20:166–173. doi: 10.1097/00124509-200409000-00008. [DOI] [PubMed] [Google Scholar]
- Fink M, Kellner CH. Belling the cat: ECT practice standards in the United States. J. ECT. 2007;23:3–5. doi: 10.1097/01.yct.0000263250.91173.08. [DOI] [PubMed] [Google Scholar]
- Fink M. Convulsive therapy: a review of the first 55 years. J. Affect. Disord. 2001;63:1–15. doi: 10.1016/s0165-0327(00)00367-0. [DOI] [PubMed] [Google Scholar]
- Frederiksen SO, d’Elia G. Electroconvulsive therapy in Sweden. Br. J. Psychiatry. 1979;134:583–587. doi: 10.1192/bjp.134.3.583. [DOI] [PubMed] [Google Scholar]
- Galletly CA, Field CD, Ormond CL. Changing patterns of electroconvulsive therapy use: results of a five-year survey. Aust. NZ J. Psychiatry. 1991;25:535–540. doi: 10.3109/00048679109064447. [DOI] [PubMed] [Google Scholar]
- Gassy JE, Rey JM. A survey of ECT in a general hospital psychiatry unit. Aust. NZ J. Psychiatry. 1990;24:385–390. doi: 10.3109/00048679009077707. [DOI] [PubMed] [Google Scholar]
- Gazdag G, Palinska D, Kloszewska I, Sobow T. Electroconvulsive therapy practice in Poland. J. ECT. 2009a;25:34–38. doi: 10.1097/YCT.0b013e3181794690. [DOI] [PubMed] [Google Scholar]
- Gazdag G, Sebestyen G, Zsargo E, J Survey of referrals to electroconvulsive therapy in Hungary. World J. Biol. Psychiatry. 2009b;10:900–904. doi: 10.1080/15622970802256180. [DOI] [PubMed] [Google Scholar]
- Gazdag G, Kocsis N, Lipcsey A. Changes in the use of electroconvulsive treatment in Hungarian psychiatry between 1992 and 2002. [Hungarian] Psychiatr. Hung. 2004a;19:53–60. [Google Scholar]
- Gazdag G, Kocsis N, Lipcsey A. Rates of electroconvulsive therapy use in Hungary in 2002. J. ECT. 2004b;20:42–44. doi: 10.1097/00124509-200403000-00009. [DOI] [PubMed] [Google Scholar]
- Glen T, Scott AIF. Rates of electroconvulsive therapy use in Edinburgh (1992–1997) J. Affect. Disord. 1999;54:81–85. doi: 10.1016/s0165-0327(98)00144-x. [DOI] [PubMed] [Google Scholar]
- Glen T, Scott AIF. Variation in rates of electroconvulsive therapy use among consultant teams in Edinburgh (1993–1996) J. Affect. Disord. 2000;58:75–78. doi: 10.1016/s0165-0327(99)00095-6. [DOI] [PubMed] [Google Scholar]
- Golenkov A, Ungvari GS, Gazdag G. ECT practice and psychiatrists’ attitudes towards ECT in the Chuvash Republic of the Russian Federation. Eur. Psychiatry. 2010;25:126–128. doi: 10.1016/j.eurpsy.2009.02.011. [DOI] [PubMed] [Google Scholar]
- Grunhaus L. A call for action-my own personal views. J. ECT. 2010;26:32–33. doi: 10.1097/YCT.0b013e3181a74381. [DOI] [PubMed] [Google Scholar]
- Hemphill KE, Walter WG. The treatment of mental disorders by electrically induced convulsions. J. Ment. Sci. 1941;87:256–275. [Google Scholar]
- Hermann RC, Dorwart RA, Hoover CW, Brody J. Variation in ECT use in the United States. Am. J. Psychiatry. 1995;152:869–875. doi: 10.1176/ajp.152.6.869. [DOI] [PubMed] [Google Scholar]
- Hermann RC, Ettner SL, Dorwart RA, Langman-Dorwart N, Kleinman S. Diagnoses of patients treated with ECT: a comparison of evidence-based standards with reported use. Psychiatr. Serv. 1999;50:1059–1065. doi: 10.1176/ps.50.8.1059. [DOI] [PubMed] [Google Scholar]
- Huuhka MJ, Korpisammal LA, Leinonen EVJ. Historical perspective on electroconvulsive therapy in Pitkaniemi Hospital: a comparison of practice in 1940s, 1960s, and 1990s. Psychiatria Fennica. 2000;31:55–64. [Google Scholar]
- Ikeji OC, Ohaeri JU, Osahon RO, Agidee RO. Naturalistic comparative study of outcome and cognitive effects of unmodified electro-convulsive therapy in schizophrenia, mania and severe depression in Nigeria. East Afr. Med. J. 1999;76:644–650. [PubMed] [Google Scholar]
- Ishimoto Y, Imakura A, Nakayama H. Practice of electroconvulsive therapy at University Hospital, the University of Tokushima School of Medicine from 1975 to 1997. J. Med. Invest. 2000;47:123–127. [PubMed] [Google Scholar]
- James BO, Morakinyo O, Lawani AO, Omoaregba JO, Olotu OS. Unmodified electroconvulsive therapy: the perspective of patients from a developing country. J. ECT. 2010;26:218–222. doi: 10.1097/YCT.0b013e3181c30494. [DOI] [PubMed] [Google Scholar]
- Kornhuber J, Weller M. Patient selection and remission rates with the current practice of electroconvulsive therapy in Germany. Convuls. Ther. 1995;11:104–109. [PubMed] [Google Scholar]
- Kramer BA, Hsin-Tung PE. A survey of ECT use in Asia. Convuls. Ther. 1990;6:26–31. [PubMed] [Google Scholar]
- Kramer BA. Use of ECT in California, revisited: 1984–1994. J. ECT. 1999;15:245–251. [PubMed] [Google Scholar]
- Lalitanatpong D. The use of electroconvulsive therapy and the length of stay of psychiatric inpatients at King Chulalongkorn Memorial Hospital, Thai Red Cross Society. J. Med. Assoc. Thai. 2005;88:S142–S148. [PubMed] [Google Scholar]
- Lamont S, Brunero S, Barclay C, et al. Evaluation of an electroconvulsive therapy service in a general hospital. Int. J. Ment. Health Nurs. 2011;20:223–9. doi: 10.1111/j.1447-0349.2010.00725.x. doi: 10.1111/j.1447-0349.2010.00725.x [Published first online February 18, 2011] [DOI] [PubMed] [Google Scholar]
- Latey RH, Fahy TJ. Electroconvulsive therapy in the Republic of Ireland 1982: a summary of findings. Br. J. Psychiatry. 1985;147:438–439. doi: 10.1192/bjp.147.4.438. [DOI] [PubMed] [Google Scholar]
- Levav I, Gonzalez UR. The use of electroconvulsive therapy in Latin America and the Caribbean [Spanish] Acta Psiquiatr. Psicol. Am. Lat. 1996;42:137–141. [Google Scholar]
- Levav I, Gonzalez UR. The use of electroconvulsive therapy in Latin America and the Caribbean. Rev. Panam. Salud. Publica [serial on the Internet] 1998;3:120–123. Available at http://www.scielosp.org/scielo.php?script=sci_arttext&pid=S1020-49891998000200013&lng=en. doi: 10.1590/S1020-49891998000200013 (accessed July 12, 2011) [Google Scholar]
- Little JD. ECT in the Asia Pacific region: what do we know? J. ECT. 2003;19:93–97. doi: 10.1097/00124509-200306000-00007. [DOI] [PubMed] [Google Scholar]
- Lucca AM, Rossini DM, Malaguti AM, Zanardi RM, Magri LP, Smeraldi EM. Use of electroconvulsive therapy in the city of Milan: a naturalistic study. J. ECT. 2010;26:148. doi: 10.1097/YCT.0b013e3181c18834. [DOI] [PubMed] [Google Scholar]
- Magid M, Rohland BM. Electroconvulsive therapy availability in the United States. In: Swartz CM, editor. Electroconvulsive and neuromodulation therapies. New York: Cambridge Univ. Press; 2009. pp. 227–35. [Google Scholar]
- McCall WV, Weiner RD, Shelp FE, Austin S. ECT in a state hospital setting. Convuls. Ther. 1992;8:12–18. [PubMed] [Google Scholar]
- McCall WV. Electroconvulsive therapy in the era of modern psychopharmacology. Int. J. Neuropsychop. 2001;4:315–324. doi: 10.1017/S1461145701002437. [DOI] [PubMed] [Google Scholar]
- Ministry of Health. Elevtroconvulsive therapy audit report. 2005. New Zealand. Available at http://www.moh.govt.nz (accessed October 3, 2011) [Google Scholar]
- Ministry of Health. Electroconvulsive therapy annual statistics: for the period 1 July 2003 to 30 June 2005. 2006. New Zealand. Available at http://www.moh.govt.nz (accessed October 28, 2011) [Google Scholar]
- Moksnes KM, Ilner SO. Electroconvulsive therapy—efficacy and side-effects. Tidsskr. Nor. Laegeforen. 2010;130:2460–2464. doi: 10.4045/tidsskr.09.1102. [DOI] [PubMed] [Google Scholar]
- Moksnes KM, Vatnaland T, Eri B, Torvik NH. Electroconvulsive therapy in the Ullevaal region of Oslo 1988–2002 [Norwegian] Tidsskr. Nor. Laegeforen. 2006;126:1750–1753. [PubMed] [Google Scholar]
- Motohashi N, Awata S, Higuchi T. A questionnaire survey of ECT practice in university hospitals and national hospitals in Japan. J. ECT. 2004;20:21–23. doi: 10.1097/00124509-200403000-00005. [DOI] [PubMed] [Google Scholar]
- Mudur G. Indian group seeks ban on use of electroconvulsive therapy without anaesthesia. Br. Med. J. 2002;324:806. doi: 10.1136/bmj.324.7341.806/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mugisha RX, Ovuga EB. The use of electroconvulsive therapy in the treatment of psychiatric illness at Umzimkulu Hospital in Transkei. A retrospective study. South Afr. Med. J. 1991;79:391–393. [PubMed] [Google Scholar]
- Muller U, Klimke A, Janner M, Gaebel W. Electroconvulsive therapy in psychiatric clinics in Germany in 1995 [German] Nervenarzt. 1998;69:15–26. doi: 10.1007/s001150050234. [DOI] [PubMed] [Google Scholar]
- Naqvi H, Khan MM. Use of electroconvulsive therapy at a university hospital in Karachi, Pakistan: a 13-year naturalistic review. J. ECT. 2005;21:158–161. doi: 10.1097/01.yct.0000177962.76163.44. [DOI] [PubMed] [Google Scholar]
- Nelson AI, Giagou N. History of electroconvulsive therapy in the Russian Federation. In: Swartz CM, editor. Electroconvulsive and neuromodulation therapies. New York: Cambridge Univ. Press; 2009. pp. 266–275. [Google Scholar]
- Nelson AI. A national survey of electroconvulsive therapy use in the Russian Federation. J. ECT. 2005;21:151–157. doi: 10.1097/01.yct.0000172569.44675.53. [DOI] [PubMed] [Google Scholar]
- Odejide AO, Ohaeri JU, Ikuesan BA. Electroconvulsive therapy in Nigeria. Convuls. Ther. 1987;3:31–39. [PubMed] [Google Scholar]
- Okagbue N, McIntosh A, Gardner M, Scott AI. The rate of usage of electroconvulsive therapy in the city of Edinburgh, 1993–2005. J. ECT. 2008;24:229–231. doi: 10.1097/YCT.0b013e31815dd4a2. [DOI] [PubMed] [Google Scholar]
- Okasha TA. Electro-convulsive therapy (ECT): an Egyptian perspective. Afr. J. Psychiatry. 2007;10:22–24. [Google Scholar]
- Olfson M, Marcus S, Sackeim HA, Thompson J, Pincus HA. Use of ECT for the inpatient treatment of recurrent major depression. Am. J. Psychiatry. 1998;155:22–29. doi: 10.1176/ajp.155.1.22. [DOI] [PubMed] [Google Scholar]
- O’Dea JFJ, Mitchell PB, Hickie IB. Unilateral or bilateral electroconvulsive therapy for depression? A survey of practice and attitudes in Australia and New Zealand. Med. J. Aust. 1991;155:9–11. doi: 10.5694/j.1326-5377.1991.tb116367.x. [DOI] [PubMed] [Google Scholar]
- Palinska D, Gazdag G, Sobow T, Hese RT, Kloszewska I. Electroconvulsive therapy in Poland in 2005—a nationwide questionnaire study performed in Polish psychiatric clinics [Polish] Psychiatr. Pol. 2008;42:825–839. [PubMed] [Google Scholar]
- Pastore DL, Bruno LM, Nardi AE, Dias AG. Use of electroconvulsive therapy at Instituto de Psiquiatria, Universidade Federal do Rio de Janeiro, from 2005 to 2007. Revista de Psiquiatria do Rio Grande do Sul. 2008;30:175–181. [Google Scholar]
- Pippard J. Audit of electroconvulsive treatment in two National Health Service regions. Br. J. Psychiatry. 1992;160:621–637. doi: 10.1192/bjp.160.5.621. [DOI] [PubMed] [Google Scholar]
- Prudic J, Olfson M, Sackeim HA. Electro-convulsive therapy practices in the community. Psychol. Med. 2001;31:929–934. doi: 10.1017/s0033291701003750. [DOI] [PubMed] [Google Scholar]
- Reid WH, Keller S, Leatherman M, Mason M. ECT in Texas: 19 months of mandatory reporting. J. Clin. Psychiatry. 1998;59:8–13. [PubMed] [Google Scholar]
- Rosa MA, Rosa MO. Electroconvulsive therapy in Latin America. In: Swartz CM, editor. Electroconvulsive and neuromodulation therapies. New York: Cambridge Univ. Press; 2009. pp. 276–284. [Google Scholar]
- Rose D, Fleischmann P, Wykes T, Leese M, Bindman J. Patients’ perspectives on electroconvulsive therapy: systematic review. Br. Med. J. 2003;326:1363–1368. doi: 10.1136/bmj.326.7403.1363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenbach ML, Hermann RC, Dorwart RA. Use of electroconvulsive therapy in the Medicare population between 1987 and 1992. Psychiatr. Serv. 1997;48:1537–1542. doi: 10.1176/ps.48.12.1537. [DOI] [PubMed] [Google Scholar]
- Royal College of Psychiatrists. The ECT handbook: the third report of the Royal College of Psychiatrist's Special Committee on ECT. xii. London: Royal College of Psychiatrists; 2005. p. 243. [Google Scholar]
- Saatcioglu O, Tomruk NB. Practice of electroconvulsive therapy at the research and training hospital in Turkey. Soc. Psychiatry Psychiatr. Epidemiol. 2008;43:673–677. doi: 10.1007/s00127-008-0351-z. [DOI] [PubMed] [Google Scholar]
- Scarano VR, Felthous AR, Early TS. The state of electroconvulsive therapy in Texas. Part I: reported data on 41,660 ECT treatments in 5971 patients. J. Forensic Sci. 2000;45:1197–1202. [PubMed] [Google Scholar]
- Schweder LJ, Wahlund B, Bergsholm P, Linaker OM. Questionnaire study about the practice of electroconvulsive therapy in Norway. J. ECT. 2011b;27:296–299. doi: 10.1097/YCT.0b013e31821ff3bd. [DOI] [PubMed] [Google Scholar]
- Schweder LJ, Lydersen S, Wahlund B, Bergsholm P, Linaker OM. Electroconvulsive therapy in Norway: rates of use, clinical characteristics, diagnoses and attitude. J. ECT. 2011a;27:292–295. doi: 10.1097/YCT.0b013e318208e24b. [DOI] [PubMed] [Google Scholar]
- Selis MA, Kauye F, Leentjens AF. Leentjens. The practice of electroconvulsive therapy in Malawi. J. ECT. 2008;24:137–140. doi: 10.1097/YCT.0b013e31815dcfd7. [DOI] [PubMed] [Google Scholar]
- Shorter E. History of electroconvulsive therapy. In: Swartz CM, editor. Electroconvulsive and neuromodulation therapies. New York: Cambridge Univ. Press; 2009. pp. 167–79. [Google Scholar]
- Sienaert P, van den Broek WW. Electroconvulsive therapy in continental Western Europe: a litterature review. In: Swartz CM, editor. Electroconvulsive and neuromodulation therapies. New York: Cambridge Univ. Press; 2009. pp. 246–255. [Google Scholar]
- Sienaert P, Filip B, Willy M, Joseph P. Electroconvulsive therapy in Belgium: a questionnaire study on the practice of electroconvulsive therapy in Flanders and the Brussels Capital region. J. ECT. 2005b;21:3–6. doi: 10.1097/01.yct.0000148622.26223.56. [DOI] [PubMed] [Google Scholar]
- Sienaert P, Bouckaert F, Milo W, Peuskens J. The practice of electroconvulsive therapy in Flanders and the Brussels Capital region. A survey [Dutch] Tijdschr. Psychiatr. 2005a;47:279–287. doi: 10.1097/01.yct.0000148622.26223.56. [DOI] [PubMed] [Google Scholar]
- Sienaert P, Dierick M, Degraeve G, Peuskens J. Electroconvulsive therapy in Belgium: a nationwide survey on the practice of electroconvulsive therapy. J. Affect. Disord. 2006;90:67–71. doi: 10.1016/j.jad.2005.09.016. [DOI] [PubMed] [Google Scholar]
- Sijuwola OA. Use of electroconvulsive therapy in a Nigerian hospital. East Afr. Med. J. 1985;62:60–64. [PubMed] [Google Scholar]
- Socialstyrelsen. 2010. ECT-treatment, a pilot study [Swedish]. Socialstyrelsen (Artikkel nr. 2010–4-3). Available at http://www.socialstyrelsen.se/publikationer2010/2010-4-3 (accessed December 1, 2010)
- Strachan JA. Electroconvulsive therapy—attitudes and practice in New Zealand. Psychiatr. Bull. 2001;25:467–470. [Google Scholar]
- Stromgren LS. Electroconvulsive therapy in the Nordic countries, 1977–1987. Acta Psychiatr. Scand. 1991;84:428–434. doi: 10.1111/j.1600-0447.1991.tb03173.x. [DOI] [PubMed] [Google Scholar]
- Sundhedsstyrelsen. Electroconvulsive therapy (ECT-therapy) and deaths—report. Version 1.0 [Danish] 2011a. Sundhedsstyrelsen. Available at http://www.sst.dk (accessed July 11, 2011)
- Sundhedsstyrelsen. Use of coercion in mental health care 2009 [Danish] 2011b. Sundhedsstyrelsen. Available at http://www.sst.dk/publ/Publ2011/DAF/Sundhedsdata/TvangIPsykiatrien.pdf (accessed July 11, 2011)
- Swartz CM. Electroconvulsive and neuromodulation therapies. New York: Cambridge Univ. Press; 2009. [Google Scholar]
- Sylvester AP, Mulsant BH, Chengappa KN, Sandman AR, Haskett RF. Use of electroconvulsive therapy in a state hospital: a 10-year review. J. Clin. Psychiatry. 2000;61:534–539. doi: 10.4088/jcp.v61n0714. [DOI] [PubMed] [Google Scholar]
- Takebayashi M. The development of electroconvulsive therapy in Japan. J. ECT. 2010;26:14–15. doi: 10.1097/YCT.0b013e3181c18a79. [DOI] [PubMed] [Google Scholar]
- Tauscher J, Neumeister A, Fischer P, Frey R, Kasper S. Electroconvulsive therapy in clinical practice [German] Nervenarzt. 1997;68:410–416. doi: 10.1007/s001150050143. [DOI] [PubMed] [Google Scholar]
- Teh SPC, Xiao AJG, Helmes E, Drake DG. Electroconvulsive therapy practice in Western Australia. J. ECT. 2005;21:145–150. doi: 10.1097/01.yct.0000171611.86728.70. [DOI] [PubMed] [Google Scholar]
- Tewfik KD, Saad A, Younis Y. Contemporary status of electroconvulsive therapy in a teaching psychiatric unit in Al Ain, United Arab Emirates. Nord. J. Psychiatry. 1998;52:481–485. [Google Scholar]
- The UK ECT Review Group. Efficacy and safety of electroconvulsive therapy in depressive disorders: a systematic review and meta-analysis. Lancet. 2003;361:799–808. doi: 10.1016/S0140-6736(03)12705-5. [DOI] [PubMed] [Google Scholar]
- Thompson JW, Weiner RD, Myers CP. Use of ECT in the United States in 1975, 1980, and 1986. J. ECT. 1994;151:1657–1661. doi: 10.1176/ajp.151.11.1657. [DOI] [PubMed] [Google Scholar]
- van Waarde JA, Verwey B, van den Broek WW, van der Mast RC. Electroconvulsive therapy in the Netherlands: a questionnaire survey on contemporary practice. J. ECT. 2009;25:190–194. doi: 10.1097/YCT.0b013e31819190b5. [DOI] [PubMed] [Google Scholar]
- Westphal JR, Horswell R, Kumar S, Rush J. Quantifying utilization and practice variation of electroconvulsive therapy. Convuls. Ther. 1997;13:242–252. [PubMed] [Google Scholar]
- Wood DA, Burgess PM. Epidemiological analysis of electroconvulsive therapy in Victoria, Australia. Aust. NZ J. Psychiatry. 2003;37:307–311. doi: 10.1046/j.1440-1614.2003.01182.x. [DOI] [PubMed] [Google Scholar]
- Zeren T, Tamam L, Evlice YE. Electroconvulsive therapy: assesment of practice of 12 years’ period [Turkish] Yeni Symposium: psikiyatri, noroloji ve davranis bilimleri dergisi. 2003;41:54–63. [Google Scholar]


