Abstract
Objective Data suggest parents’ preprocedural anxiety is related to children's acute procedural anxiety and pain. This study examined the temporal relations among these constructs to determine whether children's anxiety mediates the relation between parents' anticipatory anxiety and children's procedural pain. Methods A total of 90 preschoolers receiving immunizations, their parents, and the nurses rated children's procedural anxiety and pain. Parents provided ratings of their own preprocedural anxiety. Results Bootstrapping analyses revealed that children's procedural anxiety mediated the relation between parents' preprocedural anxiety and children's procedural pain according to parents' report and nurses’ report but not children's self-report of anxiety and pain. Conclusions Analyses suggest that children's procedural anxiety mediates the relation between parents' anticipatory anxiety and children's procedural pain. Thus, targeting parents’ preprocedural anxiety might be beneficial to the parents as well as the children undergoing a distressing medical procedure.
Keywords: anxiety, children, pain, parents
Children undergo numerous routine and unplanned medical procedures, many of which result in high distress (Blount et al., 2009; Cohen, MacLaren, & Lim, 2008). Although the umbrella term “distress” is often used to describe children's reactions to invasive medical events, it is likely that children experience a host of negative experiences including fear, anxiety, and sensory pain. Qualitative research suggests that preschoolers are able to describe fears separately from pain associated with painful events (Salmela, Aronen, & Salanterä, 2011; Salmela, Salanterä, & Aronen, 2009). In contrast, some data indicate that children under the age of 8 years may be unable to differentiate between sensory and affective components of painful experiences (Goodenough et al., 1999). If affective and sensory experiences associated with medical procedures can be differentiated, it follows that they could be separately targeted for intervention (Cohen, Blount, Cohen, & Johnson, 2004).
In terms of interventions to minimize children's medical distress, the most fruitful line of study has been into parents' behavior during the medical procedure (Blount et al., 2009; Cohen, Bernard, & Greco, 2002; Frank, Blount, Smith, Manimala, & Martin, 1995). The findings that specific parent behavior (e.g., excessive reassurance provision, giving too much control to the child, apologizing, criticizing) was associated with high child distress and that other parent behavior (e.g., distracting, coaching to cope) predicted low child distress led directly to parent training interventions to reduce children's medical anxiety and pain (e.g., Cohen, Blount, & Panopoulos, 1997; Cohen et al., 2002, 2006).
Closely related to parent behavior, parent anxiety is another influential predictor of child medical procedural distress. Although some studies have failed to find significant correlations between parent anxiety and child medical distress (Dahlquist, Power, Cox, & Fernbach, 1994; Frank et al., 1995; Wolff et al., 2009), a number of other studies have shown that parent anxiety predicts child anxiety and pain across a range of medical and nonmedical events (e.g., Bennett-Branson & Craig, 1993; Bernard & Cohen, 2006; Jacobsen, Manne, Gorfinkle, & Schorr, 1990; Jay, Ozolins, Elliott, & Caldwell, 1983; Lipani & Walker, 2006; Whaley, Pinto, & Sigman, 1999). Regarding a mechanism, research comparing the behavior of clinically anxious and nonanxious mothers suggests that mothers with high state anxiety are less emotionally sensitive and might communicate their anxiety to their children (e.g., Nicol-Harper, Harvey, & Stein, 2007; Woodruff-Borden, Morrow, Bourland, & Cambron, 2002). In addition to the relation between parent anxiety and child anxiety, associations have been demonstrated between parent anxiety and child pain (e.g., Bernard & Cohen, 2006; Jacobsen et al., 1990; Jay et al., 1983).
Researchers have implemented stress-inoculation (e.g., Jay & Elliott, 1990) and provided parents with coaching roles (e.g., Cohen et al., 1997) with hypotheses that lowering parent anxiety would result in lower child procedural anxiety and pain. Although this makes conceptual sense, there are no published data that support this directional hypothesis. Clearly, parents cannot be randomized to high and low state anxiety study conditions; however, careful inspection of the temporal relations among parent and child distress during a pediatric medical procedure might shed some light on directional relations.
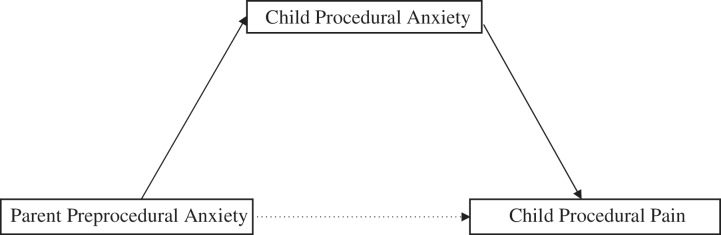
In summary, research suggests that children's procedural anxiety and pain are interwoven yet possibly distinct constructs (Cohen et al., 2004). In addition, there are ample data linking parents' state anxiety and children's procedural anxiety and pain (Jacobsen et al., 1990; Jay et al., 1983), although the temporal relation among these variables is unclear. The purpose of this study was to examine whether parents' state anxiety immediately preceding children's immunization injections predicted children's injection pain and whether this relation was mediated by children's injection anxiety. It has been acknowledged (Huguet, McGrath, & Pardos, 2011; McMurtry, Noel, Chambers, & McGrath, 2011) that fear and anxiety are distinct constructs, yet given the high inter-correlation, they are used interchangeably in the pediatric pain literature. In the current study, we describe children's affective reaction as “anxiety,” although we acknowledge that we might be measuring “fear.” Based on findings that the child, parent, and medical staff each have unique perspectives on the child's anxiety and pain, measures from multiple perspectives were employed in the current study (Cohen et al., 2008). It was hypothesized that parents' preprocedure anxiety would positively relate to children's anxiety, which in turn would predict children's pain during the injection (Figure 1). Given that prior studies have identified sex differences in children's anxiety and pain (e.g., Chambers, Craig, & Bennett, 2002; Tsao et al., 2006), it was hypothesized that girls would report higher levels of anxiety and pain than boys.
Figure 1.
Model of child procedural anxiety mediating the relation between parent preprocedural anxiety and child procedural pain.
Methods
Participants
The current study was part of a larger treatment outcome trial that involved training parents to coach in distraction to reduce child distress during routine immunizations. Preliminary analyses demonstrated no differences on children's distress by treatment condition; thus, all parents and children were included in the current study. To date, no other publications have resulted from this dataset. To be included in the study, children were required to be between 4- and 6-years old (M = 4.8 years, SD = 9.7 months), which is consistent with previous research examining associations between parent behavior and child immunization pain (e.g., Cohen, Blount, Cohen, Schaen, & Zaff, 1999; Manimala, Blount, & Cohen, 2000). In addition, this age range was selected because this is the age at which children receive their mandatory immunizations for entry into preschool. A total of 90 children were enrolled in the study, of whom 46 were females and 44 were males. Participants were Caucasian (81%), mixed race (7.8%), Asian/Pacific Islander (5.6%), Black (4.4%), and one parent failed to indicate race. Caregivers included 78 mothers and 12 fathers, with ages ranging from 28 to 50 (M = 38 years, SD = 4.3 years). Caregivers were Caucasian (83%), Asian/Pacific Islander (8.9%), Black (4.4%), or Mixed race (2.2%) and had education levels that varied from 12 to 25 years (M = 16.8, SD = 2.4). Annual household income ranged from $38,400 to $350,000 (M = $127,688, SD = $67,418).
Background Information
Demographic information for the parent (i.e., relation to child, age, sex, race, education level, total family income) and child (i.e., age, sex, and race) was assessed using a questionnaire.
Parent Anxiety, Child Anxiety, and Child Pain
Parent self-report of state anxiety was collected prior to the immunization procedure. Parent report, nurse report, and child self-report of child state procedural anxiety and pain were collected immediately following the procedure. The100-mm visual analog scales (VAS's) were used to collect parent and nurse ratings with anchors of “No Pain” to “Severe Pain” and “Not Anxious” to “Very Anxious.” VAS's are commonly used in pain studies and data indicate that they are psychometrically sound for measuring pediatric procedural distress (Cohen et al., 2008). Child self-reported procedural anxiety and pain were assessed using the Children's Anxiety and Pain Scales (CAPS; Kuttner & LePage, 1989). These scales include two sets of five drawings of children's faces. One group displays increasing expressions of anxiety and the other expressions of levels of pain. The CAPS was originally developed for use with children between 4- and 10-years old. Research indicates that the CAPS has good validity and reliability (e.g., Wright, Eisner, Stewart, & Finley, 2010) and discriminates between anxiety and pain (Kuttner & LePage, 1989). However, this measure is not widely used—likely because assessing only children's pain is the norm in this line of study—and thus there are not ample data on the psychometric properties of the CAPS (Stinson, Kavanaugh, Yamada, Gill, & Stevens, 2006).
Procedure
The study was approved by an institutional review board. Researchers approached families after they entered a pediatric healthcare clinic. At this time, informed consent/assent was obtained and background information was collected. Parents completed ratings of their state anxiety prior to the procedure. Immediately following the immunization procedure, children, parents, and nurses completed independent ratings of children's procedural anxiety and pain. Researchers separately administered these scales to minimize participants influencing each others' ratings.
Results
Preliminary Analyses
Preliminary statistics were used to evaluate relations between variables of interest and demographic factors. Specifically, family income, age of child, and ethnicity were analyzed for relations with parent self-report of preprocedural state anxiety, as well as parent report, nurse report, and child self-report of child procedural anxiety and pain. Pearson product moment correlations (PPMCs) were used to assess child age and family income. Analysis of variance (ANOVA) was used to analyze ethnicity. PPMCs revealed a significant negative relation between child age and parent report of child procedural pain (r = −.275, p = .009). No other demographic variables were found to be associated with variables of interest.
Correlation analyses conducted across raters revealed significant relations among reports. Specifically, child self-report of procedural anxiety was correlated with both parent report (r = .31, p = .003) and nurse report (r = .36, p < .001) of child procedural anxiety. Similarly, child self-report of procedural pain exhibited a significant relation to parent (r = .45, p < .001) and nurse (r = .46, p < .001) reports of child procedural pain. Additionally, parent and nurse agreements of child procedural anxiety (r = .66, p < .001) and pain (r = .48, p < .001) were correlated. Descriptive and correlational analyses are provided in Tables I and II.
Mediation Analyses
It was hypothesized that parent preprocedural anxiety would affect child procedural anxiety, which would, in turn, affect child's procedural pain. To test this hypothesis, three mediation analyses were conducted. The first mediation analysis included parent self-reported preprocedural anxiety, parent-reported child procedural anxiety, and parent-reported child procedural pain. The second mediation analysis included parent self-report preprocedural anxiety and nurse-report of child procedural anxiety and pain. The third mediation analysis included parent self-reported preprocedural anxiety and child self-reported procedural anxiety and pain. We utilized the Preacher and Hayes (2008) mediation macro, which develops estimates of indirect effects with bias-corrected bootstrap confidence intervals. Bootstrap method has been validated in the literature and is preferred over other methods in assessing the existence of mediation among variables (Preacher & Hayes, 2008), especially when working with small samples. Preference is based on the fact that other methods for testing for indirect effects assume a standard normal distribution when calculating the p-value for the indirect effect, whereas bootstrapping does not assume normality of the sampling distribution. In addition, bootstrap method repeatedly samples from the data set, estimating the indirect effect with each resampled data set. This process is repeated thousands of times, producing confidence intervals for the indirect effect.
Analyses utilizing the bootstrap method (5,000 bootstrap samples were used) confirmed the existence of a mediation effect of parent preprocedural anxiety on child procedural pain via child procedural anxiety according to parent report and nurse report (Table III). Specifically, the absence of zero in the confidence interval for the indirect pathways indicated that the indirect effect was significantly different from zero at p < .05, two tailed. Confidence intervals for the third mediation analysis, which included child self-reported procedural anxiety and pain overlapped with zero and did not suggest mediation at p < .05, two tailed.
Table I.
Means and Standard Deviations of Anxiety and Pain Measures
| M (SD) | Range | |
|---|---|---|
| Parent Preprocedural Anxiety (n = 90) | 19.81 (23.941) | 0–95 |
| Parent Reported Child Procedural Anxiety (n = 90) | 73.83 (26.533) | 3–100 |
| Parent Reported Child Procedural Pain (n = 90) | 54.94 (24.701) | 0–97 |
| Nurse Reported Child Procedural Anxiety (n = 90) | 62.99 (31.238) | 1–100 |
| Nurse Reported Child Procedural Pain (n = 90) | 47.66 (22.184) | 0–93 |
| Child Self-Reported Procedural Anxiety (n = 88) | 3.44 (1.611) | 0–4 |
| Child Self-Reported Procedural Pain (n = 88) | 3.51 (1.597) | 0–4 |
Note. Parent and nurse report measures range for 0–100 mm; child self-report measures range from 0 to 4.
Table II.
Intercorrelations for Anxiety and Pain Measures
| 1. | 2. | 3. | 4. | 5. | 6. | |
|---|---|---|---|---|---|---|
| 1. Parent Preprocedural Anxiety (n = 90) | – | |||||
| 2. Parent Reported Child Procedural Anxiety (n = 90) | .273** | – | ||||
| 3. Parent Reported Child Procedural Pain (n = 90) | .222** | .359** | – | |||
| 4. Nurse Reported Child Procedural Anxiety (n = 90) | .194 | .656** | .357** | – | ||
| 5. Nurse Reported Child Procedural Pain (n = 90) | .198 | .483** | .478** | .618** | – | |
| 6. Child Self-Reported Procedural Anxiety (n = 88) | .202 | .314** | .244* | .359** | .337** | – |
| 7. Child Self-Reported Procedural Pain (n = 88) | .228* | .241* | .446* | .315** | .458** | .639** |
*p ≤ 0.05, **p ≤ 0.01.
Table III.
Parent, Nurse, and Child Report of Indirect Effect of Parent Preprocedural Anxiety on Child Procedural Pain as Mediated by Child Procedural Anxiety
| Bootstrap 95% CIs | ||
|---|---|---|
| Point estimate (SE) | Lower to Upper | |
| Parent Report | 0.091 (0.044) | 0.0200 to 0.1948 |
| Nurse Report | 0.107 (0.054) | 0.0103 to 0.2270 |
| Child Self-Report | 0.009 (0.004) | −0.0009 to 0.0165 |
Note. Confidence intervals (CIs) are bias corrected; 5,000 bootstrap samples.
Based on previous findings (e.g., Chambers et al., 2002; Tsao et al., 2006), we examined child sex as a potential moderator of the relation between parent preprocedural anxiety and child procedural anxiety. To explore this relation, an analysis of moderated mediation was conducted in accordance with Preacher, Rucker, and Hayes (2007). This analysis revealed no significant findings, suggesting that sex did not impact children's anxiety level during the medical procedure.
Discussion
Our data suggest that parents' preprocedural anxiety might result in increasing children's procedural anxiety, which in turn heightens children's procedural pain. This mediation was found based on parent and nurse ratings—but not self-reported—of child procedural anxiety and pain. In explaining these findings, it could be that parents with high state anxiety communicate this emotional state or behave in ways that increase their child's anxiety. There are ample data suggesting that children are sensitive to parents' state anxiety (e.g., Caldwell-Andrews, Kain, Mayes, Kerns, & Ng, 2005; Nicol-Harper et al., 2007; Woodruff-Borden et al., 2002). Although not examined in the current study, genetics would also explain high correlations between parents' and children's anxiety. Regarding the second part of the mediation, there are ample data linking children's anxiety and their procedural pain (e.g., Blount, Piira, & Cohen, 2003; Cohen et al., 2004; McGrath, 1994). It could be that children's anxiety heightens their physiological awareness and sensitivity to painful stimuli. Melzack and Wall's Gate Control Theory (1965) posits that anxiety may enhance pain by opening sensory “gates” that allow more input into the central nervous system. Consistent with this theory, studies in neuroscience have revealed exacerbation of pain due to anxiety based on regions of brain activation (Ploghaus et al., 2001).
The most likely reason that child-self report data did not reveal mediation may be that preschoolers are simply not able to differentiate their own anxiety and pain during an immunization injection. Data suggest that children younger than 8 years have difficulty making this distinction (Goodenough et al., 1999; Huguet et al., 2011). The high correlation between children's anxiety and pain ratings with our sample provide additional support of this explanation. Whether children are truly unable to identify the affective and sensory aspects of the experience or whether our measure was insufficient for the task remains unclear.
Inconsistent with some prior data (Chambers et al., 2002; Tsao et al., 2006), no sex differences were found. However, the Chambers and Tsao studies examined laboratory-induced pain and it is possible that “real-world” pain is experienced or expressed more consistently across sexes. In fact, many medical procedure pain studies have not detected differences in pain between young boys and girls (e.g., Fillingim, King, Ribeiro-Dasilva, Rahim-Williams, & Riley, 2009; Fuller, 2002; Rosmus, Johnston, Chan-Yip, & Yang, 2000).
Results from the current study provide further support for the need to increase parent awareness regarding how their anxiety can impact their children's experience during painful medical experiences. For example, teaching parents optimal ways to manage their own anxiety prior to their children's painful medical procedures might result in lower child procedural anxiety and pain. To evaluate this hypothesis, experimental studies might examine whether parent anxiety-management interventions (e.g., relaxation, deep breathing) result in lower child procedural anxiety and pain. Although there are few studies of this sort, Jay and Elliott's (1990) parent stress-inoculation provide preliminary data that this line of study might be fruitful.
Limitations of the current study include its homogenous sample. Participants were primarily Caucasian, middle to upper-middle class, and were mostly college educated. It is possible that other samples of parents might not reveal the same relations. Along these lines, given that most caregivers were mothers, future studies might examine whether fathers' anticipatory anxiety has a similar relation with children's anxiety and pain. Additional measures of parent anxiety (e.g., observer report, physiological, anxious behavior) and child affective and sensory distress (e.g., observational scale) might provide additional information about the relations between parent anxiety, child anxiety, and child pain. In conclusion, findings suggest a pathway from parents' anticipatory anxiety through child's procedural anxiety leading to child's procedural pain, which highlights several avenues for interventions to improve the medical experience for the whole family.
Funding
The National Institute of Child Health and Human Development (grant 5R21HD047263-02 to Lindsey L. Cohen, PhD).
Conflicts of interest: None declared.
References
- Bennett-Branson S M, Craig K D. Postoperative pain in children: Developmental and family influences on spontaneous coping strategies. Canadian Journal of Behavioural Sciences. 1993;25:355–383. [Google Scholar]
- Bernard R, Cohen L L. Parent anxiety and infant pain during pediatric immunizations. Journal of Clinical Psychology in Medical Settings. 2006;13:285–290. [Google Scholar]
- Blount R L, Piira T, Cohen L L. Management of pediatric pain and distress due to painful medical procedures. In: Roberts M C, editor. Handbook of pediatric psychology. 3rd ed. New York: Guilford Press; 2003. pp. 216–233. [Google Scholar]
- Blount R L, Zempsky W T, Jaaniste T, Evans S, Cohen L L, Devine K A, Zeltzer L K. Management of pain and distress due to medical procedures. In: Roberts M C, Steele R, editors. Handbook of pediatric psychology. 4th ed. New York: Guilford Press; 2009. pp. 171–188. [Google Scholar]
- Caldwell-Andrews A, Kain Z, Mayers L, Kerns R, Ng D. Motivation and maternal presence during induction of anesthesia. Anesthesiology. 2005;103:478–483. doi: 10.1097/00000542-200509000-00008. [DOI] [PubMed] [Google Scholar]
- Chambers C T, Craig K D, Bennett S M. The impact of maternal behavior on children's pain experiences: An experimental analysis. Journal of Pediatric Psychology. 2002;27:293–301. doi: 10.1093/jpepsy/27.3.293. [DOI] [PubMed] [Google Scholar]
- Cohen L L, Bernard R S, Greco L A. A child-focused intervention for coping with procedural pain: Are parent and nurse coaches necessary? Journal of Pediatric Psychology. 2002;27:749–757. doi: 10.1093/jpepsy/27.8.749. [DOI] [PubMed] [Google Scholar]
- Cohen L L, Blount R L, Cohen R J, Johnson V C. Dimensions of pediatric procedural distress: Children's anxiety and pain during immunizations. Journal of Clinical Psychology in Medical Settings. 2004;11:41–47. [Google Scholar]
- Cohen L L, Blount R L, Cohen R J, Schaen E R, Zaff J F. Comparative study of distraction versus topical anesthesia for pediatric pain management during immunizations. Health Psychology. 1999;18:591–598. doi: 10.1037//0278-6133.18.6.591. [DOI] [PubMed] [Google Scholar]
- Cohen L L, Blount R L, Panopoulos G. Nurse coaching and cartoon distraction: An effective and practical intervention to reduce child, parent, and nurse distress during immunizations. Journal of Pediatric Psychology. 1997;22:355–370. doi: 10.1093/jpepsy/22.3.355. [DOI] [PubMed] [Google Scholar]
- Cohen L L, MacLaren J E, Lim C S. Pain and pain management. In: Steele R G, Elkin T D, Roberts M C, editors. Handbook of evidence based therapies for children and adolescents: Bridging science and practice. New York: Springer Publishers; 2008. pp. 283–296. [Google Scholar]
- Dahlquist L M, Power T G, Cox C N, Fernbach D J. Parenting and child distress during cancer procedures: A multidimensional assessment. Children's Health Care. 1994;23:149–166. doi: 10.1207/s15326888chc2303_1. [DOI] [PubMed] [Google Scholar]
- Fillingim R B, King CD, Ribeiro-Dasilva M C, Rahim-Williams B, Riley Iii J L. Sex, gender, and pain: A review of recent clinical and experimental findings. Journal of Pain. 2009;10:447–485. doi: 10.1016/j.jpain.2008.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank N C, Blount R L, Smith A J, Manimala M R, Martin J K. Parent and staff behavior, previous child medical experience, and maternal anxiety as they relate to child procedural distress and coping. Journal of Pediatric Psychology. 1995;20:277–289. doi: 10.1093/jpepsy/20.3.277. [DOI] [PubMed] [Google Scholar]
- Fuller B F. Infant sex differences regarding acute established pain. Clinical Nursing Research. 2002;11:190–203. doi: 10.1177/105477380201100207. [DOI] [PubMed] [Google Scholar]
- Goodenough B, Thomas W, Champion G G, Perrott D, Taplin J E, von Baeyer C L, Ziegler J B. Unraveling age effects and sex differences in needle pain: Ratings of sensory intensity and unpleasantness of venipuncture pain by children and their parents. Pain. 1999;80:179–190. doi: 10.1016/s0304-3959(98)00201-2. [DOI] [PubMed] [Google Scholar]
- Huguet A, McGrath P J, Pardos J. Development and preliminary testing of a scale to assess pain-related fear in children and adolescents. The Journal of Pain. 2011;12:840–848. doi: 10.1016/j.jpain.2011.01.005. [DOI] [PubMed] [Google Scholar]
- Jacobsen P B, Manne S L, Gorfinkle K, Schorr O. Analysis of child and parent behavior during painful medical procedures. Health Psychology. 1990;9:559–576. doi: 10.1037//0278-6133.9.5.559. [DOI] [PubMed] [Google Scholar]
- Jay S M, Elliott C H. A stress inoculation program for parents whose children are undergoing painful medical procedures. Journal of Consulting and Clinical Psychology. 1990;58:799–804. doi: 10.1037//0022-006x.58.6.799. [DOI] [PubMed] [Google Scholar]
- Jay S M, Ozolins M, Elliott C H, Caldwell S. Assessment of children's distress during painful medical procedures. Health Psychology. 1983;2:133–147. [Google Scholar]
- Katz E R, Kellerman J, Siegel S E. Behavioral distress in children with cancer undergoing medical procedures: Developmental considerations. Journal of Consulting and Clinical Psychology. 1980;48:356–365. doi: 10.1037//0022-006x.48.3.356. [DOI] [PubMed] [Google Scholar]
- Kuttner L, LePage T. Face scales for the assessment of pediatric pain: A critical review. Canadian Journal of Behavioural Science. 1989;21:198–209. [Google Scholar]
- Lipani T A, Walker L S. Children's appraisal and coping with pain: Relation to maternal ratings of worry and restriction in family activities. Journal of Pediatric Psychology. 2006;31:667–673. doi: 10.1093/jpepsy/jsj038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manimala M R, Blount R L, Cohen L L. The effects of parental reassurance versus distraction on child distress and coping during immunizations. Child Health Care. 2000;29:161–177. [Google Scholar]
- McGrath P A. Psychological aspects of pain perception. Archives of Oral Biology. 1994;39:55S–62S. doi: 10.1016/0003-9969(94)90189-9. [DOI] [PubMed] [Google Scholar]
- McMurtry C, Noel M, Chambers C T, McGrath P J. Children's fear during procedural pain: Preliminary investigation of the Children's Fear Scale. Health Psychology. 2011;30:780–788. doi: 10.1037/a0024817. [DOI] [PubMed] [Google Scholar]
- Melzack R, Wall P D. Pain mechanisms: A new theory. Science. 1965;150:971–979. doi: 10.1126/science.150.3699.971. [DOI] [PubMed] [Google Scholar]
- Nicol-Harper R, Harvey A G, Stein A. Interactions between mothers and infants: Impact of maternal anxiety. Infant Behavior & Development. 2007;30:161–167. doi: 10.1016/j.infbeh.2006.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ploghaus A, Narain C, Beckmann C F, Clare S, Bantick S, Wise R, Matthews P M, Rawlins J N, Tracey I. Exacerbation of pain by anxiety is associated with activity in a hippocampal network. The Journal of Neuroscience. 2001;21:9896–9903. doi: 10.1523/JNEUROSCI.21-24-09896.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher K J, Hayes A F. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Preacher K J, Rucker D D, Hayes A F. Assessing moderated mediation hypotheses: Theory, methods, and prescriptions. Multivariate Behavioral Research. 2007;42:185–227. doi: 10.1080/00273170701341316. [DOI] [PubMed] [Google Scholar]
- Rosmus C, Johnston C C, Chan-Yip A, Yang F. Pain response in Chinese and non-Chinese Canadian infants: Is there a difference? Social Science & Medicine. 2000;51:175–184. doi: 10.1016/s0277-9536(99)00447-5. [DOI] [PubMed] [Google Scholar]
- Salmela M M, Aronen E T, Salanterä S S. The experience of hospital-related fears of 4- to 6-year-old children. Child: Care, Health and Development. 2011;37:719–726. doi: 10.1111/j.1365-2214.2010.01171.x. [DOI] [PubMed] [Google Scholar]
- Salmela M, Salanterä S, Aronen E T. Child-reported hospital fears of 4 to 6 year-old children. Pediatric Nursing. 2009;5:269–276. [PubMed] [Google Scholar]
- Stinson J N, Kavanagh T, Yamada J, Gill N, Stevens B. Systematic review of the psychometric properties, interpretability and feasibility of self-report pain intensity measures for use in clinical trials in children and adolescents. Pain. 2006;125:143–157. doi: 10.1016/j.pain.2006.05.006. [DOI] [PubMed] [Google Scholar]
- Tsao J C, Lui Q, Myers C D, Kim S C, Turk N, Zeltzer L K. Parent and child anxiety sensitivity: Relationships to children's experimental pain responsivity. The Journal of Pain. 2006;7:319–326. doi: 10.1016/j.jpain.2005.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whaley S E, Pinto A, Sigman M. Characterizing interactions between anxious mothers and their children. Journal of Consulting and Clinical Psychology. 1999;67:826–836. doi: 10.1037//0022-006x.67.6.826. [DOI] [PubMed] [Google Scholar]
- Wolff N J, Darlington A S, Hunfeld J A, Verhulst F C, Jaddoe W V, Moll H A, Hofman A, Passchier J, Teimeier H. The association of parent behaviors, chronic pain, and psychological problems with venipuncture distress in infants: The Generation R study. Health Psychology. 2009;28:605–613. doi: 10.1037/a0015202. [DOI] [PubMed] [Google Scholar]
- Wright K D, Eisner A, Stewart S H, Finley G A. Measurement of preoperative anxiety in young children: Self-report versus observer-rated. Journal of Psychopathology and Behavioral Assessment. 2010;32:416–427. [Google Scholar]
- Woodruff–Borden J, Morrow C, Bourland S, Cambron S. The behavior of anxious parents: Examining mechanisms of transmission of anxiety from parent to child. Journal of Clinical Child and Adolescent Psychology. 2002;31:364–374. doi: 10.1207/S15374424JCCP3103_08. [DOI] [PubMed] [Google Scholar]