Abstract
Objective The objective of this investigation was to examine how variation in adolescent physical activity is related to smoking and alternative tobacco use. Methods Adolescents (N = 1,384) completed a self-report survey every 6 months from ages 14- to 18-years old in a prospective study of health behaviors. The 8 waves of data were analyzed using General Growth Mixture Modeling (GGMM) Results GGMM identified five physical activity trajectories including stable higher (SHPA), decreased (DPA), stable regular (SRPA), curvilinear (CPA), and stable low (SLPA). Across 4 years, the likelihood of smoking was greater among adolescents in the DPA, SLPA and SRPA trajectories compared to adolescents belonging to the SHPA trajectory. Alternative tobacco use was greatest among adolescents in the DPA and SRPA trajectories. Conclusions Adolescents with decreasing physical activity and even adolescents averaging an hour of physical activity a day (SRPA) are important groups to target for tobacco use prevention and intervention efforts.
Keywords: adolescent, alternative tobacco, physical activity, smoking
Introduction
Tobacco use and physical inactivity are the leading preventable causes of morbidity and mortality in the United States, accounting for almost 30% of all deaths (Mokdad, Marks, Stroup, & Gerberding, 2004). About 20% of the adolescents are regular smokers (Centers for Disease Control, 2010) and 23% use an alternative form of tobacco (e.g., smokeless tobacco, cigars) with the prevalence of use increasing twofold across adolescence (Centers for Disease Control, 2010). Over 60% of the adolescents do not engage in 60 min of physical activity on five or more days each week and only 18% achieve the recommended 60 min of physical activity every day (Centers for Disease Control, 2011). Physical activity declines during adolescence and physical inactivity tracks into adulthood (Aaron, Storti, Robertson, Kriska, & LaPorte, 2002; Kimm et al., 2002; van Mechelen, Twisk, Post, Snel, & Kemper, 2000). Thus, on average, the prevalence of smoking tends to increase and physical activity tends to decrease across mid to late adolescence.
These epidemiologic trends are disconcerting as the available albeit limited, longitudinal research of smoking, and physical activity suggests that physical activity is protective against smoking uptake. Higher levels of physical activity have been shown to reduce the odds of smoking initiation and progression by almost 50% (Audrain-McGovern, Rodriguez, & Moss, 2003). Similarly, adolescents who are consistently involved in team sports are three times less likely to become regular smokers than adolescents with inconsistent participation (Rodriguez & Audrain-McGovern, 2004).
Researchers have speculated that regular physical activity might protect against smoking for social as well as biological reasons (Audrain-McGovern et al., 2003; Audrain-McGovern, Rodriguez, Wileyto, Schmitz, & Shields, 2006; Melnick, Miller, Sabo, Farrell, & Barnes, 2001). Smoking may be incompatible with physical activity or may provide greater social affiliation with nonsmokers, decreasing peer smoking influences. There also are behavioral norms for athletes (e.g., athletes do not smoke, smoking lessens athletic performance), which adolescents may conform to. However, while the athletic milieu eschews smoking, it may be less critical of smokeless tobacco use. Use of alternative forms of tobacco (e.g., smokeless tobacco) is more prevalent among team sport athletes (Castrucci, Gerlach, Kaufman, & Orleans, 2004; Soldz, Huyser, & Dorsey, 2003; Terry-McElrath, O'Malley, & Johnston, 2011). Biologically, physical activity and smoking are rewarding behaviors, associated with similar genes in the dopaminergic reward pathway and both impact mood (Audrain-McGovern, Rodriguez, & Kassel, 2009; Audrain-McGovern et al., 2006; Norris, Carroll, & Cochrane, 1992). Physical activity may provide an alternative source of reward to smoking as well as a means to manage mood, making smoking less likely. As physical activity declines, some adolescents may replace it with smoking as a reward and as a method to manage mood.
Whereas research has documented the importance of maintaining regular physical activity to lessen the odds of smoking, little is known about when the relationship between physical activity, smoking, and alternative tobacco use begins to unfold. While recent studies have focused on initial levels of physical activity and the average rate of physical activity decline (Duncan, Duncan, Strycker, & Chaumeton, 2007; Kahn et al., 2008; Raudsepp & Viira, 2008), there is likely significant variation in the timing, rate and magnitude of physical activity decline across mid to late adolescence. An investigation into this heterogeneity could highlight physical activity trajectories that are linked to a greater likelihood of smoking and alternative tobacco use. Indeed, approaches focused on individual variability rather than population averages are more likely to identify when, who and the circumstances under which smoking and alternative tobacco use develops (Dierker, Rose, Tan, & Li, 2010).
The present study sought to empirically identify variation in physical activity from mid to late adolescence and to longitudinally characterize these physical activity patterns with respect to smoking and alternative tobacco use. As the first study to empirically identify adolescent physical activity trajectories, we expected to find at least three trajectories: one representing a pattern of lower levels of physical activity, another pattern of higher levels of physical activity, and a pattern of declining physical activity. We anticipated that cigarette smoking would emerge out of low and declining physical activity patterns, while alternative tobacco use would more likely characterize a subgroup with higher levels of physical activity.
Despite the public health significance of tobacco use and physical inactivity among adolescents, our understanding of the relationship between these two behaviors is limited. The present study is novel in its examination of how variation in adolescent physical activity is related to the odds of regularly smoking and regularly using alternative forms of tobacco. As such, it has the potential to contribute to the literature in several important ways. The findings will help clarify the level and pattern of physical activity that is protective against tobacco use, rather than relying on less informative descriptions such as higher or lower levels of physical activity. The findings may also inform intervention timing and content by identifying key periods of risk for tobacco use based on the changes in physical activity and what type of intervention is necessary (i.e., smoking prevention, alternative tobacco use prevention, tobacco cessation, and/or physical activity promotion). Adolescence is a critical period for the development of health habits that are carried into adulthood (Chassin, Presson, Rose, & Sherman, 1996; Telama et al., 2005). Identifying the adolescents at risk for smoking uptake and for insufficient physical activity is critical for understanding, predicting, and intervening early to prevent behaviors that lead to premature morbidity and mortality.
Method
Participants and Procedures
Participants were high school students (50% female and 73% White) who participated in a longitudinal study of the relationship between adolescent physical activity and adolescent smoking adoption. Participants were enrolled in one of four public high schools in suburban Philadelphia, PA, USA. The four schools in the study ranged from 25% of the students to 65% of the students having a parent with a college education, which encompassed the national average for households (Crissey, 2009). Across the four schools, approximately 17–41% of the students reported receiving free or reduced cost lunch. This cohort was drawn from the 1,517 students identified through class rosters at the beginning of ninth grade. Students were ineligible to participate in this study if they had a special classroom placement (e.g., severe learning disability) or if they did not speak fluent English. Based on the selection criteria, a total of 1,487 (98%) ninth grade students were eligible to participate. Parents were mailed a study information letter (active information) with a telephone number to call to obtain answers to any questions and to decline consent for their adolescent to participate. Of these 1,487 eligible teens, 1,478 (99%) had a parent’s passive consent to participate. Thirty adolescents were absent on the assent/survey days and 19 adolescents did not provide assent due to lack of interest in the study. Thus, 1,429 of 1,478 teens with parental consent (97%) provided their assent to participate and completed a baseline survey. Adolescents who declined assent or who were absent on the baseline survey day did not differ on race and gender from those who provided assent and completed the baseline survey.
The adolescent cohort was formed in the ninth grade and followed until the end of 12th grade. A self-report 40-min survey was administered every 6 months (fall and spring) on-site during compulsory classes each year of high school for a total of eight surveys. In order to characterize the variation in physical activity across time with respect to smoking and alternative tobacco use, we estimated the effects of smoking and alternative tobacco use at Wave 1 (ninth grade fall, baseline) and at Wave 4 (10th grade spring), and treated smoking and alternative tobacco use as distal outcomes at Wave 8 (12th grade spring). As such, participants were 1,384 adolescents, 1,087 adolescents, and 1,094 adolescents, with complete data on these variables and repeated measures of the outcome variable, hours of physical activity per week at Waves 1, 4, and 8. University Institutional Review Board approval of the study was obtained.
Measures
Hours of Physical Activity per Week
Physical activity, the dependent variable, was assessed using a past 6 month recall instrument designed for adolescent epidemiologic studies (Aaron et al., 1993; Aaron, Kriska et al., 1995). The questionnaire asked respondents to check physical activities they did at least 10 times in the past 6 months using a list of common activities, and add activities not prelisted. Next, they were asked to identify months in which they practiced those activities and the estimated time (days per week and minutes per day) spent in each activity. Metabolic equivalents (METs) were computed for each activity (Ainsworth, 2000). Hours per week in activities ≥3.0 METS were summed for an indicator of weekly moderate-to-vigorous physical activity. Research supports the validity and reliability of the recall measure at 1-year intervals (Aaron et al., 1993; Aaron, Kriska et al., 1995), and its validity predicting smoking and other high-risk behaviors in adolescents (Aaron, Dearwater et al., 1995). The physical activity recall measure correlates significantly and negatively with time to complete a one mile run (Aaron et al., 1993; Aaron, Kriska et al., 1995). Test–retest reliability estimates for past year recall measured one year apart was .66 and .72 for hours per week for all leisure time and vigorous activity, respectively (Aaron et al., 1993; Aaron, Kriska et al., 1995). Correlations of past year recall with past week recall ranged from .63 to .76 for hours of leisure-time physical activity per week, and .76 to .84 for hours of vigorous physical activity per week.
Covariates
Gender, race, and parental education were included in the model as covariates. In addition, smoking and alternative tobacco use were used to discriminate among the physical activity trajectories at Wave 1 and at Wave 4, and then treated as a binary distal outcome for the final wave (Wave 8).
Smoking was derived from evaluating smoking practices with a series of standard epidemiological questions regarding smoking such as, “Have you ever tried or experimented with cigarette smoking, even a few puffs?”, and “Have you smoked a cigarette in the past 30 days?” (Audrain-McGovern, Rodriguez, Epstein et al., 2009; Eaton et al., 2006). The six-category ordered categorical smoking variable used to discriminate among the physical activity trajectories was coded as 0 = never smoked, 1 = puffed but did not smoke a whole cigarette, 2 = smoked a whole cigarette but not in the past month, 3 = smoked in the last month, 4 = smokes weekly and 5 = smokes daily. For the binary distal outcome, the two category smoking variable was coded as 0 = did not smoke in the past 30 days, and 1 = smoked in the past 30 days. Current use (past 30 days) of alternative tobacco products (e.g., cigars, snuff, chewing tobacco) was measured with items from the Youth Risk Behavior Survey (Tercyak & Audrain, 2002). The binary alternative tobacco use variable used to discriminate among physical activity trajectories and as a binary distal outcome was coded 0 = did not use alternative tobacco products in the past 30 days, and 1 = used alternative tobacco products in the past 30 days.
Overview of Analyses
Growth Mixture Modeling
Growth Mixture Modeling (GMM) is a factor mixture modeling method that extends beyond a single average developmental trajectory in latent growth curve modeling (LGCM) to explore developmental heterogeneity among trajectories of a repeated measure like hours of physical activity per week measured every 6 months for 4 years (Jung & Wickerama, 2008; Muthén, 2004; Nylund, Asparouhov, & Muthén, 2006). GMM seeks to identify whether two or more developmental trajectories each with a unique average initial level and average rate of change exists. GMM permits the assessment of predictors of class membership relative to a comparison class using multinomial logistic regression. General GMM (GGMM) extends GMM by adding binary distal outcomes and permitting for the assessment of the effects of trajectory membership on outcomes like smoking and alternative tobacco use at last follow-up (Muthén, 2002, 2004; Muthén & Shedden, 1999). We used smoking and alternative tobacco use to characterize the trajectories at Waves 1 and 4, re-centering the baseline from ninth grade (Wave 1) to 10th grade spring (Wave 4). This allowed us to examine differences in tobacco use among the physical activity trajectories at the beginning (age of 14 years) and at the midpoint (Wave 4, age of 16 years) of the study in order to provide data on if, how, and when smoking and alternative tobacco use emerges among the distinct physical activity trajectories. Furthermore, we included binary distal outcome measures of smoking and alternative tobacco use to assess whether there were overall differences in the odds of regular smoking and regular alternative tobacco use for the physical activity trajectories across the 4 years. These analyses were conducted using Mplus, version 6, software (Muthén & Muthén, 1998–2007).
To determine the optimal number of subpopulations (trajectory, classes), we used the most widely accepted empirical criteria (Muthén, 2004). Empirical criteria used were the Bayesian Information Criterion (BIC), the sample size adjusted BIC (SSABIC), average classification probability (Entropy), and the Bootstrap Likelihood ratio test (BLRT) (Boscardin, Muthén, Francis, & Baker, 2008; Jung & Wickerama, 2008; Nylund et al., 2006). For modeling stability and generalizability, we did not accept trajectories representing less than 5% of the entire sample size.
Missing Data
To account for missing data, multivariate modeling used all available data. Mplus allows modeling with missing data using maximum likelihood estimation of the mean, variance, and covariance parameters, when requested, employing the expectation maximization (EM) algorithm, assuming data are missing at random (MAR) (Muthén, 1998–2004). However, this only accounted for missing data on the repeated measure of physical activity, not the covariates (gender, race, parental education) or tobacco use. Thus, cases with missing data on these variables were not included in the analysis. As such, the analyses were based on 1384 participants at Wave 1 (ninth grade, fall), 1087 participants at Wave 4 (10th grade spring), and 1094 participants at Wave 8 (12th grade spring). An analysis comparing adolescents who were retained versus lost to follow-up (n = 327) indicated that those lost to follow-up engaged in less weekly physical activity per week (M = 7.50, SD = 7.91 vs. M = 9.30, SD = 8.19, p = .001) at baseline than those retained. As such, data were not Missing Completely at Random (MCAR), but rather MAR. MAR means that missing data can be related to prior instances of the dependent variable (i.e., baseline physical activity) as long as it is not the reason for the missing data (Missing Not at Random; MNAR). We can conclude MAR since there was no evidence that lost participants failed to complete subsequent surveys because of issues with reporting physical activity. Instead they did not complete subsequent surveys because they moved or changed schools. As there is no evidence of systematic missingness (nonignorable missing data; missing not at random) (Little & Rubin, 2002), we concluded that our data were MAR, permitting modeling with all available data in Mplus (Little & Rubin, 2002; Muthén & Muthén, 2001).
Results
Model Building
LGCM
We began by identifying the best fitting LGCM to represent average baseline level and rate of change from baseline in physical activity. The best fitting LGCM representing the average trajectory of physical activity across the eight waves of data was a quadratic model,  = 121.54, p < .0001, CFI = .97, RMSEA = .05 (95% CI = 0.04–0.06), which fit significantly better than a LGCM without a quadratic trend based on a chi-square difference test,
= 121.54, p < .0001, CFI = .97, RMSEA = .05 (95% CI = 0.04–0.06), which fit significantly better than a LGCM without a quadratic trend based on a chi-square difference test,  = 29.51, p < .0001. The quadratic LGCM served as the general population model from which we tested for developmental heterogeneity in the GGMM.
= 29.51, p < .0001. The quadratic LGCM served as the general population model from which we tested for developmental heterogeneity in the GGMM.
GGMM
Table I presents the model specification results. We determined the optimal number of classes without and then with the covariates (gender, race, parental education) and smoking and alternative tobacco use. The model was designed to include a trajectory class of stable physical activity by fixing the mean linear and quadratic trend factors to equal zero, along with residual variances for baseline level and linear trend, representing a class of adolescents with a consistently low physical activity. However, when the results of our modeling supported the presence of greater than three trajectory classes, including one very large low physical activity class, we extended these constraints to two classes in order to divide the large low physical activity class. Thus, the final model included two classes with the linear and quadratic trend factor means constrained to equal zero, along with their baseline and linear trend factor residual variances constrained to equal zero. As the quadratic term variance was not significantly different from zero, we also fixed its variance to equal zero for all classes (Rodriguez, Moss, & Audrain-McGovern, 2005).
Table I.
Model Specification
| Model | Classes | Predictors | Log likelihood | BIC | SSABIC | Entropy | SCS % | BLRT, p-value |
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | No | −30,752.43 | 61,650.15 | 61,586.62 | .63 | 47 | |
| 2 | 3 | No | −30,718.28 | 61,610.92 | 61,534.68 | .62 | 13 | |
| 3 | 4 | No | −30,564.03 | 61,346.00 | 61,250.70 | .69 | 9 | |
| 4 | 5 | No | −30,521.22 | 61,303.98 | 61,189.62 | .68 | 6 | <.0001 |
| 5 | 6 | No | −30,495.00 | 61,295.12 | 61,161.70 | .68 | 5a | <.0001 |
| 6 | 7 | No | −30,462.62 | 61,273.94 | 61,121.47 | .75 | 1 | <.0001 |
| 7 | 5 | Yes | −29,539.48 | 59,484.00 | 59,306.11 | .71 | 5 |
Note. BIC = Bayesian Information Criterion; SSABIC = the sample size adjusted BIC; average classification probability (Entropy); SCS = smallest class size %; BLRT = Bootstrap Likelihood Ratio Test.
aTwo trajectories had 5% of the participants.
The BIC and SSABIC decreased through Model 6 (7 class model). Furthermore, the BLRT continued to be significant, favoring each subsequent model tested. However, with Model 6, the smallest class size decreased below our 5% threshold. Thus, we selected the six class model at this stage which included two classes with 5% of the participants. We next added the ninth grade covariates to the six class model. However, this model proved to be very unstable and could not solve with the inclusion of these variables due to the small class sizes. Therefore, based on empirical and class size criteria, we selected the five class model (Model 4) as the best representation of physical activity and tobacco use for the data.
Descriptive Statistics
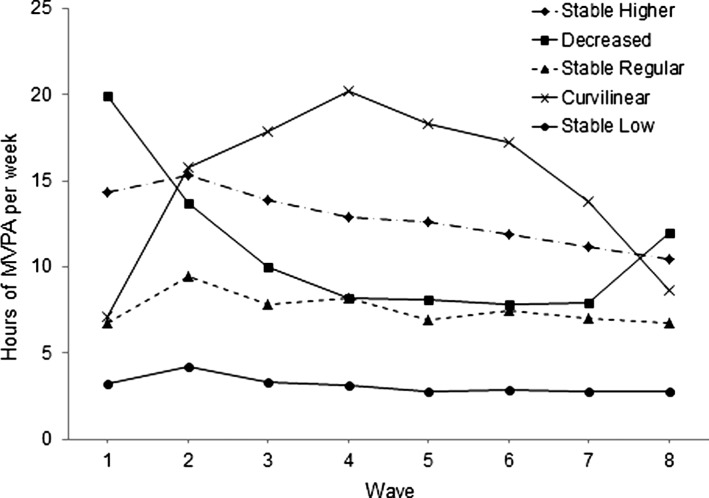
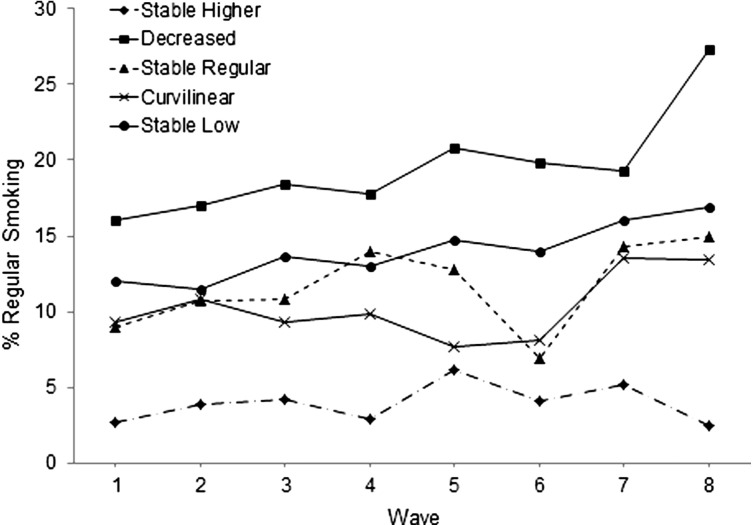
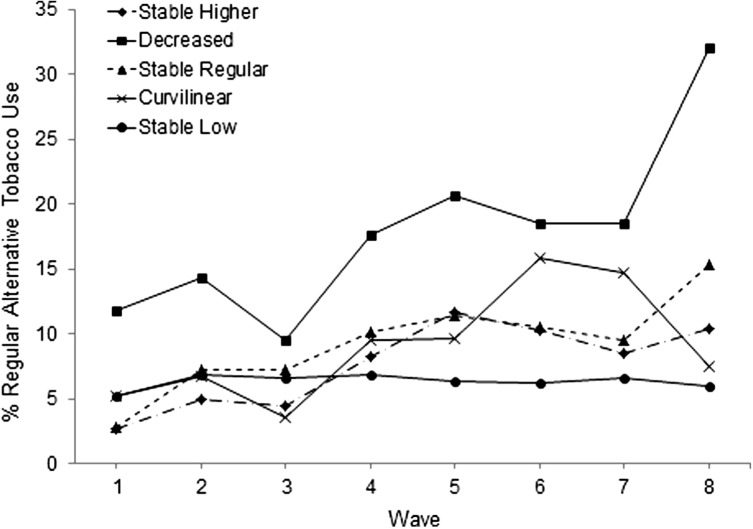
Frequency distributions for the demographic and tobacco use variables for each of the five trajectories at baseline, Waves 4 and 8 are presented in Table II. Across the five trajectories, the average hours of physical activity per week declined across the eight waves from a mean of 8.72 (SD = 8.42) hours per week at baseline to 7.03 (SD = 6.71) hours per week at Wave 8. Figure 1 represents the average hours of weekly physical activity for each class across 4 years. Ten percent of the sample regularly smoked at Wave 1 with 26% progressing along the smoking uptake continuum across 4 years. Overall, 5% of the sample used alternative tobacco products at baseline increasing to 12% across 4 years. Figures 2 and 3 depict the regular use of cigarettes and alternative tobacco, respectively, across time for the groups.
Table II.
Descriptive Statistics for the Physical Activity Trajectories
| Total (n = 1429) | CPA (n = 77) | SHPA (n = 299) | DPA (n = 170) | SRPA (n = 213) | SLPA (n = 670) | |
|---|---|---|---|---|---|---|
| Female | 50 (716) | 39 (30) | 40 (119) | 33 (56) | 46 (98) | 62 (413) |
| White | 73 (1038) | 74 (57) | 78 (232) | 82 (139) | 72 (152) | 68 (458) |
| Both parents have a high school education or less | 17 (236) | 22 (16) | 18 (52) | 15 (26) | 14 (30) | 17 (112) |
| Physical activity, Wave 1 (Mean, SD) | 8.72 (8.42) | 6.47 (5.78) | 15.52 (7.67) | 21.48 (7.17) | 6.84 (3.84) | 3.30 (3.21) |
| Physical activity, Wave 4 (Mean, SD) | 7.81 (7.48) | 20.70 (7.40) | 13.92 (7.10) | 7.74 (6.35) | 8.38 (5.29) | 3.12 (3.54) |
| Physical activity, Wave 8 (Mean, SD) | 7.03 (6.71) | 8.07 (6.25) | 11.24 (7.67) | 12.02 (9.01) | 7.07 (2.97) | 2.73 (1.95) |
| Smoked in the past 30 days, Wave 1 | 3 (44) | 4 (3) | 2 (5) | 5 (9) | 2 (5) | 3 (22) |
| Smoked in the past 30 days, Wave 4 | 2 (27) | 2 (1) | 0.42 (1) | 2 (3) | 3 (6) | 3 (16) |
| Smoked in the past 30 days, Wave 8 | 3 (34) | 3 (2) | 1 (2) | 7 (10) | 4 (6) | 3 (14) |
| Smokes weekly, Wave 1 | 7 (97) | 5 (4) | 1 (3) | 11 (18) | 7 (14) | 9 (58) |
| Smokes weekly, Wave 4 | 9 (99) | 8 (5) | 2 (6) | 16 (21) | 10 (18) | 10 (49) |
| Smokes weekly, Wave 8 | 12 (129) | 10 (7) | 2 (4) | 20 (28) | 11 (19) | 14 (71) |
| Used alternative tobacco in the past month, Wave 1 | 5 (73) | 5 (4) | 3 (8) | 12 (20) | 3 (6) | 5 (35) |
| Used alternative tobacco in the past month, Wave 4 | 9 (103) | 9 (6) | 8 (20) | 18 (24) | 10 (18) | 7 (35) |
| Used alternative tobacco in the past month, Wave 8 | 12 (131) | 7 (5) | 10 (25) | 32 (45) | 15 (26) | 6 (30) |
Note. CPA = Curvilinear physical activity; SHPA = stable higher physical activity; DPA = decreased physical activity; SRPA = stable regular physical activity; SLAP = stable low physical activity. Values are expressed as % (n) unless otherwise specified.
Figure 1.
Physical activity patterns across mid to late adolescence. MVPA = moderate and vigorous physical activity.
Figure 2.
Regular smoking across time for the physical activity trajectories.
Figure 3.
Regular alternative tobacco use across time for the physical activity trajectories.
Identifying the Physical Activity Trajectories
We identified five distinct physical activity trajectories. Based on the mean level changes observed across the eight data waves, we labeled these trajectories: stable higher physical activity (n = 299); decreased physical activity (n = 170), stable regular physical activity (n = 213), curvilinear physical activity (n = 77) and stable low physical activity (n = 670). The physical activity trajectories are depicted based on their observed means in Figure 1. For the stable higher physical activity trajectory class, physical activity changed from an average of 15.52 (SD = 7.67) hours per week at baseline to 11.24 (SD = 7.67) hours per week at the last follow-up (Wave 8). This higher physical activity trajectory contrasted with the steady lower physical activity trajectory, which averaged low levels of weekly physical activity from baseline (M = 3.30, SD = 3.21) to the last follow-up (M = 2.73, SD = 1.95). The steady regular physical activity trajectory class maintained recommended levels of physical activity per week across the eight study waves averaging 6.84 (SD = 3.84) hours per week at baseline and 7.07 (SD = 2.97) hours at last follow-up (Wave 8). The decreased physical activity trajectory started high with an average of 21.84 (SD = 7.17) hours of weekly physical activity at baseline, decreasing significantly to 7.74 (SD = 6.35) hours per week at Wave 4 before rebounding to 12.02 (SD = 9.01) hours per week at Wave 8. The curvilinear physical activity trajectory class showed an inverted-U pattern starting with a weekly average of 6.47 (SD = 5.78) hours of physical activity, rising to an average of 20.70 (SD = 7.40) hours of physical activity per week, before falling back down to 8.07 (SD = 6.25) hours at last follow-up.
Characterizing the Physical Activity Trajectories
Table III presents the odds ratios comparing members of the decreased, curvilinear, stable regular, and stable low physical activity trajectories to members of the stable higher physical activity trajectory on smoking and alternative tobacco use at baseline and at Wave 4. We divided the α-level of .05 by 16 comparisons. Therefore, each comparison is judged at .003 in order to maintain an overall .05 Type I error rate. Compared to adolescents in the stable higher physical activity trajectory, adolescents belonging to the decreased (OR = 2.17, 95% CI 1.45–3.25) and curvilinear (OR = 2.22, 95% CI 1.38–3.57) physical activity trajectories had a twofold increased risk of smoking at a higher level at baseline than adolescents with stable higher physical activity, while adolescents in the stable regular physical activity trajectory had a greater than three and a half fold odds (OR = 3.65, 95% CI 2.61–5.10) of smoking at a higher level at baseline. At Wave 4, adolescents with higher levels of smoking were over three times more likely (OR = 3.33, 95% CI 1.84–6.04) to belong to the decreased physical activity trajectory and over four times more likely (OR = 4.15, 95% CI 2.99–5.77) to belong to the stable regular physical activity trajectory than the stable higher physical activity trajectory.
Table III.
Smoking and Alternative Tobacco Use Among the Physical Activity Trajectories at Baseline (n =1384) and Wave 4 (n = 1087).
| Decreased versus stable higher, OR (95% CI) | Curvilinear versus stable higher, OR (95% CI) | Stable regular vs. stable higher, OR (95% CI) | Stable low versus stable higher, OR (95% CI) | |
|---|---|---|---|---|
| Baseline | ||||
| Gender | 0.41 (0.21–0.79 | 0.56 (0.20–1.56) | 1.60 (0.81–3.15) | 2.64 (1.78–3.90) |
| Race | 2.70 (0.85–8.51) | 1.12 (0.50–2.51) | 2.70 (1.07–6.81) | 0.50 (0.33–0.74) |
| Parental education | 1.14 (0.75–1.72) | 1.22 (0.75–1.96) | 1.02 (0.67–1.55) | 1.14 (0.90–1.46) |
| Smoking | 2.17 (1.45–3.25) | 2.22 (1.38–3.57) | 3.65 (2.61–5.10) | 0.88 (0.56–1.38) |
| Alternative tobacco use | 4.67 (0.64–34.38) | 1.21 (0.11–13.36) | 1.94 (0.28–13.30) | 1.96 (0.27–14.23) |
| Wave 4 | ||||
| Smoking | 3.33 (1.84–6.04) | 2.38 (0.96–5.93) | 4.15 (2.99–5.77) | 1.22 (0.83–1.79) |
| Alternative tobacco use | 1.33 (0.03–54.97) | 1.11 (0.00–254.50) | 1.18 (0.03–49.43) | 0.44 (0.04–5.08) |
Note. Gender (1 = Female, 0 = Male); Race (1 = White, 0 = other); Parental education (0 = both parents have greater than high school education, 1 = at least one parent has a high school education or less; 2 = both parents have a high school education or less); Smoking (0 = never smoked, not even a puff of a cigarette, 1 = smoked a puff but never a whole cigarette, 2 = smoked a whole cigarette but not in the past 30 days, 3 = smoked in the past 30 days, 4 = smokes weekly; 5 = smokes daily); Alternative tobacco use (1 = used alternative tobacco products in the past 30 days, 0 = did not use alternative tobacco products in the past 30 days). OR = odds ratio; ci = confidence interval; bolded odds ratios are significant at p < .001. All odds ratios are adjusted odds ratios (adjusted for sex, race, parental education, and tobacco use).
Treating Wave 8 smoking and alternative tobacco use as distal outcomes, the results revealed that the relationships between physical activity trajectory, smoking, and alternative tobacco were significant, p < .0001. This indicated that these two tobacco use behaviors are affected by the pattern of physical activity across the eight time points. Only 3% of the adolescents belonging to the stable higher physical activity were regular smokers at last follow up, whereas 17% of adolescents belonging to the stable low physical activity smoked regularly at last follow-up. Furthermore, 13% of the adolescents belonging to the curvilinear trajectory, and 27% of the adolescents belonging to the decreasing pattern of physical activity were regular smokers at the last follow-up. Finally, 15% of the adolescents belonging to the stable regular physical activity were regular smokers at the last follow-up.
Regarding alternative tobacco use, 10% of the adolescents in the stable higher physical activity trajectory used alternative tobacco products in the past 30 days compared to 6% of adolescents in the stable low physical activity trajectory. Furthermore, 7% of the adolescents in the curvilinear group and 15% of the adolescents belonging to the stable regular physical activity used alternative tobacco products at Wave 8. The greatest use was seen among adolescents belonging to the decreasing physical activity trajectory (32% at Wave 8).
Discussion
The present study is the first to provide empirical evidence for five distinct adolescent physical activity trajectories and to examine the relationship between these trajectories and the emergence of regular tobacco use. Across 4 years, the likelihood of smoking was at least twice as great among adolescents in the decreasing, stable low and stable regular physical activity trajectories compared to adolescents belonging to the stable high physical activity trajectory. Between-trajectory differences in smoking were apparent at the age of 14 years and increased across time with 27% of the adolescents in the decreasing, 17% of the adolescents in the stable low, and 15% of the adolescents in the stable regular physical activity trajectories smoking regularly 4 years later. In contrast, between-trajectory differences in alternative tobacco use did not emerge until later in adolescence. One-third of the adolescents belonging to the decreasing and 15% of the adolescents belonging to the stable regular physical activity trajectory were using alternative tobacco regularly at the age of 18 years. These findings offer new insights into the relationship between physical activity and tobacco use across mid to late adolescence and highlight which adolescents to target, when to intervene, and with what type of intervention (e.g., physical activity promotion, adolescent smoking, and/or alternative tobacco use prevention).
Adolescents who have a pattern of physical activity marked by significant declines (40–70% of their level at the age of 14 years) are an important group to target for tobacco use prevention and intervention efforts. The declining physical activity trajectory comprised 12% of the sample, yet had the greatest proportion of regular smoking and alternative tobacco use. While some of these adolescents were already smoking and using alternative tobacco regularly at the age of 14 years, there was a salient increase in the percentage regularly using both forms of tobacco across time as physical activity declined, with the most significant increase occurring in the last 6 months of high school. This emphasizes that tobacco use prevention efforts should not only occur before the age of 14 years to capture those with early onset, but also that prevention and intervention efforts need to occur during high school, before 12th grade, to prevent later onset and escalation in use.
Of note, adolescents in this group did not fall below the recommended amount of adolescent physical activity (i.e., averaged an hour a day) at any time point. This raises several important questions. Are the activities that these adolescents engage in associated with smoking and alternative tobacco use? All physical activity may not be protective (Peretti-Watel, Beck, & Legleye, 2002). Although not well delineated, there is some evidence to suggest that sports with more risk (e.g., snowboarding, skateboarding, skiing) are linked to tobacco use (Peretti-Watel et al., 2002). Involvement in these types of sports and tobacco use may reflect an overall sensation-seeking behavioral style (Zuckerman, 1994). The types of activities as well as the sharp decline in physical activity levels may be more predictive of tobacco use than the amount of physical activity per week. As physical activity levels decline, a reward deficit may be addressed by nicotine, perpetuating subsequent tobacco use. Once an adolescent begins smoking more regularly, smoking may influence further declines in physical activity (Audrain-McGovern et al., 2003; Kimm et al., 2002). Research is warranted to characterize the heterogeneity in physical activity to determine what precipitates a significant decline in physical activity and the uptake of tobacco use. Factors associated with both of these behaviors (e.g., depression, substance use) may decrease involvement in physical activity and increase involvement in tobacco use (Audrain-McGovern et al., 2009; Audrain-McGovern et al., 2006; Norris et al., 1992).
About 15% of the sample was comprised of adolescents with stable regular physical activity. Adolescents in this group averaged an hour of physical activity a day, yet 15% were smoking regularly and 15% were using alternative tobacco at the age of 18 years. As with the decreasing physical activity trajectory, it is possible that adolescents in this trajectory engaged in certain types of physical activity that were associated with tobacco use (Peretti-Watel et al., 2002). As public health messages are aimed at increasing overall physical activity, discerning which activities are associated with tobacco use is warranted to prevent further involvement in activities linked to smoking and alternative tobacco use. In addition, certain motives for engaging in physical activity, such as self-esteem and weight loss show an association with tobacco use motives (Rockafellow & Saules, 2006; Verkooijen, Nielsen, & Kremers, 2009). Likewise, smoking may be used to manage weight in sports that rely on weight cutoffs, such as wrestling.
Similar to the decreasing physical activity trajectory, adolescents in the stable regular physical activity trajectory had a significant increase in alternative tobacco use across the 4 years; 3% of the adolescents used alternative tobacco at the age of 14 years increasing to 15% at the age of 18 years. The curvilinear physical activity trajectory was small (5%) and exhibited a different pattern of activity, but had similar smoking rates as the stable regular trajectory and half of the alternative tobacco use. Until, there is a better understanding of the types of physical activity that are and are not associated with smoking and tobacco use, it appears that addressing smoking prevention prior to and during high school and alternative tobacco use during high school even in adolescents who have regular physical activity is warranted.
Adolescents in the stable low physical activity trajectory (47% of the sample) were below the recommended level of physical activity at the age of 14 years and remained at suboptimal levels in the subsequent 4 years (about 3 hr a week). This trajectory was composed of more females than any other trajectory. As such, alternative tobacco use was the lowest in this group; however, 17% of the adolescents belonging to this trajectory were smoking regularly at the age of 18 years. Adolescents in this trajectory may lack features important to the regular involvement in physical activity (e.g., physical activity support, enjoyment and competence beliefs, less screen time) (Marsh, 1996; Sallis, Prochaska, & Taylor, 2000). Lower levels of physical activity along with other smoking risk factors may increase the likelihood of regular smoking for these adolescents. Research has shown that persistent inactivity in adolescence predicts adult smoking, even after familial factors are taken into account (Kujala, Kaprio, & Rose, 2007). These adolescents may benefit from an intervention that targets both the promotion of physical activity and the prevention of smoking. Given that these adolescents were not obtaining sufficient levels of physical activity at mid adolescence and 12% were regularly smoking at baseline, physical activity promotion, and smoking prevention should begin in early adolescence.
The current findings also emphasize that the adolescents who maintain higher levels of physical activity (21% of the sample) are the least likely to smoke and fewer use alternative tobacco products compared to adolescents in the decreasing or stable regular physical activity trajectories. Adolescents in this stable higher physical activity trajectory consistently averaged at least 90 min of physical activity a day from mid adolescence to late adolescence. Although physically active adolescents are less likely to smoke possibly because of the negative impact on athletic performance, research has found that the use of alternative forms of tobacco is more prevalent among team sport athletes (Castrucci et al., 2004; Soldz et al., 2003) and may be perceived as more acceptable than smoking. While we did not specifically assess team sport involvement, our findings indicate that the adolescents with higher levels of physical activity (e.g., averaging more than an hour a day), are least likely to smoke (3%), but that 10% do use alternative tobacco regularly by the age of 18 years. Contrary to our hypothesis, this group did not have the highest alternative tobacco use, although their prevalence of use tripled from the age of 14 to 18 years. Thus, alternative tobacco prevention messages at the beginning of high school may lessen the number the athletes that become regular users.
As the first study to examine the heterogeneity in adolescent physical activity and its link to smoking, the study has several strengths. These strengths include a large sample of the adolescents and eight measurement waves across 4 years. There are several potential limitations. As in previous epidemiological investigations of physical activity (e.g. Kahn et al., 2008), the outcome variable of physical activity was based on self-report. Assessing physical activity using objective measures such as accelerometry would have been difficult given the large sample size. The current public health recommendations for physical activity are based on decades of research linking self-reported physical activity with health outcomes (USDHHS, 1996). Smoking was also based on self-report. Biochemical verification of smoking status is not typically implemented in epidemiological studies since (a) adolescent self-reports have been determined to be valid when confidentiality is assured (Society for Research on Nicotine and Tobacco, 2002; Wills & Cleary, 1997) and (b) the standard cotinine cutoff of 15 ng/ml cannot validate definitions of an adolescent current smoker (e.g., 1 cigarette in the past 30 days) (Dolcini, Adler, Lee, & Bauman, 2003; Society for Research on Nicotine and Tobacco, 2002). Finally, the results showed that by the age of 14 years, the relationship between physical activity and smoking may have already begun to unfold for some adolescents and future investigations of this relationship may need to begin in early adolescence.
In conclusion, there are unique physical activity patterns across adolescence. Certain patterns of physical activity are linked to a greater likelihood of smoking and alternative tobacco use. The results of the present study indicate that the link between physical activity and smoking is not as clear as previously thought. Further research is warranted to determine the profile or characteristics of the adolescents who belong to these distinct physical activity trajectories. This will help to better define adolescents who need a specific type on intervention. In addition, discerning the types of physical activity that are associated with tobacco use and those that are protective may further delineate adolescents at risk for tobacco use despite achieving recommended levels of physical activity. Finally, determining the mechanisms that underlie the relationship between physical activity and smoking may elucidate variables to target to prevent tobacco use and promote physical activity. As physical activity and smoking influence each other, adolescent health behavior interventions should consider both the maintenance of physical activity and the prevention of smoking as well as alternative tobacco use. Targeting multiple and related risk factors may have a greater impact on adolescent health than targeting single health behaviors.
Funding
This study was supported by National Cancer Institute (RO1 CA126958 to J.A-M.).
Conflicts of interest: None declared.
References
- Aaron D J, Dearwater S R, Anderson R, Olsen T, Kriska A M, Laporte R E. Physical activity and the initiation of high-risk health behaviors in adolescents. Medicine and Science in Sports and Exercise. 1995;27:1639–1645. [PubMed] [Google Scholar]
- Aaron D J, Kriska A M, Dearwater S R, Anderson R L, Olsen T L, Cauley J A, Laporte R E. The epidemiology of leisure physical activity in an adolescent population. Medicine and Science in Sports and Exercise. 1993;25(7):847–853. doi: 10.1249/00005768-199307000-00014. [DOI] [PubMed] [Google Scholar]
- Aaron D J, Kriska A M, Dearwater S R, Cauley J A, Metz K F, LaPorte R E. Reproducibility and validity of an epidemiologic questionnaire to assess past year physical activity in adolescents. American Journal of Epidemiology. 1995;142(2):191–201. doi: 10.1093/oxfordjournals.aje.a117618. [DOI] [PubMed] [Google Scholar]
- Aaron D J, Storti K L, Robertson R J, Kriska A M, LaPorte R E. Longitudinal study of the number and choice of leisure time physical activities from mid to late adolescence: Implications for school curricula and community recreation programs. Archives of Pediatrics & Adolescent Medicine. 2002;156(11):1075–1080. doi: 10.1001/archpedi.156.11.1075. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=12413332. [DOI] [PubMed] [Google Scholar]
- Ainsworth B E, Haskell W L, Whitt M C, Irwin M L, Swartz A M, Strath S J, O'Brien W L, Bassett D R, Schmitz K H, Emplaincourt P O, Jacobs D R, Leon A S. Compendium of physical activities: An update of activity codes and MET intensities. Medicine and Science in Sports and Exercise. 2000;32(9 Suppl):S498–S504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- Audrain-McGovern J, Rodriguez D, Epstein L H, Cuevas J, Rodgers K, Wileyto E P. Does delay discounting play an etiological role in smoking or is it a consequence of smoking? Drug & Alcohol Dependence. 2009;103(3):99–106. doi: 10.1016/j.drugalcdep.2008.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Audrain-McGovern J, Rodriguez D, Kassel J D. Adolescent smoking and depression: Evidence for self-medication and peer smoking mediation. Addiction. 2009;104(10):1743–1756. doi: 10.1111/j.1360-0443.2009.02617.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Audrain-McGovern J, Rodriguez D, Moss H B. Smoking progression and physical activity. Cancer Epidemiol Biomarkers Prev. 2003;12(11 Pt 1):1121–1129.. Retrieved from http://cebp.aacrjournals.org/content/12/11/1121.full. [PubMed] [Google Scholar]
- Audrain-McGovern J, Rodriguez D, Wileyto E P, Schmitz K H, Shields P G. Effect of team sport participation on genetic predisposition to adolescent smoking progression. Archives of General Psychiatry. 2006;63(4):433–441. doi: 10.1001/archpsyc.63.4.433. [DOI] [PubMed] [Google Scholar]
- Boscardin C K, Muthén B O, Francis D J, Baker E L. Early identification of reading difficulties using heterogeneous developmental trajectories. Journal of Educational Psychology. 2008;100(1):192–208. [Google Scholar]
- Castrucci B C, Gerlach K K, Kaufman N J, Orleans C T. Tobacco use and cessation behavior among adolescents participating in organized sports. American Journal of Health Behavior. 2004;28(1):63–71. doi: 10.5993/ajhb.28.1.7. [DOI] [PubMed] [Google Scholar]
- CDC. Cigarette use among high school students - United States, 1991-2009. Morbidity and Mortality Weekly Report. 2010;59(26):797–801.. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5926a1.htm. [PubMed] [Google Scholar]
- CDC. Physical Activity Levels of High School Students—United States, 2010. MMWR. 2011;60(23):773–777.. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6023a1.htm. [PubMed] [Google Scholar]
- Chassin L, Presson C C, Rose J S, Sherman S J. The natural history of cigarette smoking from adolescence to adulthood: Demographic predictors of continuity and change. Health Psychology. 1996;15(6):478–484. doi: 10.1037//0278-6133.15.6.478. [DOI] [PubMed] [Google Scholar]
- Crissey S R. Educational Attainment in the United States: 2007. U.S. Census Bureau: 2009. Retrieved from www.census.gov/population/www/socdemo/educattn.html. [Google Scholar]
- Dierker L, Rose J, Tan X, Li R. Uncovering multiple pathways to substance use: A comparison of methods for identifying population subgroups. Journal of Primary Prevention. 2010;31(5–6):333–348. doi: 10.1007/s10935-010-0224-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolcini M M, Adler N E, Lee P, Bauman K E. An assessment of the validity of adolescent self-reported smoking using three biological indicators. Nicotine & Tobacco Research. 2003;5(4):473–483. [PubMed] [Google Scholar]
- Duncan S C, Duncan T E, Strycker L A, Chaumeton N R. A cohort-sequential latent growth model of physical activity from ages 12 to 17 years. Annals of Behavioral Medicine. 2007;33(1):80–89. doi: 10.1207/s15324796abm3301_9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton D K, Kann L, Kinchen S, Ross J, Hawkins J, Harris W A, Lowry R, McManus T, Chyen D, Shanklin S, Lim C, Grunbaum J A, Wechsler H. Youth risk behavior surveillance–United States, 2005. Morbidity and Mortality Weekly Report Surveillance Summaries. 2006;55(5):1–108. [PubMed] [Google Scholar]
- Jung T, Wickerama K A S. An introduction to latent class growth analysis and growth mixture modeling. Social and Personality Psychology Compass. 2008;1:302–317. [Google Scholar]
- Kahn J A, Huang B, Gillman M W, Field A E, Austin S B, Colditz G A, Frazier A L. Patterns and determinants of physical activity in U.S. adolescents. Journal of Adolescent Health. 2008;42(4):369–377. doi: 10.1016/j.jadohealth.2007.11.143. [DOI] [PubMed] [Google Scholar]
- Kimm S Y, Glynn N W, Kriska A M, Barton B A, Kronsberg S S, Daniels S R, Crawford P B, Sabry Z I, Liu K. Decline in physical activity in black girls and white girls during adolescence. The New England Journal of Medicine. 2002;347(10):709–715. doi: 10.1056/NEJMoa003277. [DOI] [PubMed] [Google Scholar]
- Kujala U M, Kaprio J, Rose R J. Physical activity in adolescence and smoking in young adulthood: A prospective twin cohort study. Addiction. 2007;102(7):1151–1157. doi: 10.1111/j.1360-0443.2007.01858.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little R J A, Rubin D B. Statistical analysis with missing data. 2nd ed. Hoboken, NJ: Wiley Interscience; 2002. [Google Scholar]
- Marsh H W. Construct validity of physical self-description questionnaire responses: Relations to external criteria. Journal of Sport and Exercise Psychology. 1996;18:111–131. [Google Scholar]
- Melnick M J, Miller K E, Sabo D F, Farrell M P, Barnes G M. Tobacco use among high school athletes and nonatieletes: Results of the 1997 youth risk behavior survey. Adolescence. 2001;36(144):727–747. [PubMed] [Google Scholar]
- Mokdad A H, Marks J S, Stroup D F, Gerberding J L. Actual causes of death in the United States, 2000. The Journal of the American Medical Association. 2004;291(10):1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- Muthén B O. Mplus technical appendices. Los Angeles, CA: Muthén & Muthén; 1998-2004. [Google Scholar]
- Muthén B O. Beyond SEM: General latent variable modeling. Behaviormetrika. 2002;29:81–117. [Google Scholar]
- Muthén B O. Latent variable analysis: Growth mixture modeling and related techniques for longitudinal data. In: Kaplan D, editor. Handbook of quantitative methodology for the social sciences. Nebury Park, CA: Sage Publications; 2004. pp. 345–368. [Google Scholar]
- Muthén B O, Muthén L K. Mplus user's guide. 2nd ed. Los Angeles, CA: Muthen & Muthen; 2001. [Google Scholar]
- Muthén B O, Shedden K. Finite mixture modeling with mixture outcomes using the EM algorithm. Biometrics. 1999;55:463–469. doi: 10.1111/j.0006-341x.1999.00463.x. [DOI] [PubMed] [Google Scholar]
- Muthén L K, Muthén B O. Mplus user’s guide. Los Angeles, CA: Muthén & Muthén; 1998-2007. [Google Scholar]
- Norris R, Carroll D, Cochrane R. The effects of physical activity and exercise training on psychological stress and well-being in an adolescent population. Journal of Psychosomatic Research. 1992;36(1):55–65. doi: 10.1016/0022-3999(92)90114-h. [DOI] [PubMed] [Google Scholar]
- Nylund K L, Asparouhov T, Muthén B O. Deciding on the number of classes in latent class analysis and growth mixture modeling. A Monte Carlo simulation study. Los Angeles: University of California.; 2006. Retrieved from http://www.statmodel.com/download/LCA_tech11_nylund_v83.pdf. [Google Scholar]
- Peretti-Watel P, Beck F, Legleye S. Beyond the U-curve: The relationship between sport and alcohol, cigarette and cannabis use in adolescents. Addiction. 2002;97:707–716. doi: 10.1046/j.1360-0443.2002.00116.x. [DOI] [PubMed] [Google Scholar]
- Raudsepp L, Viira R. Changes in physical activity in adolescent girls: A latent growth modelling approach. Acta Paediatrica. 2008;97(5):647–652. doi: 10.1111/j.1651-2227.2008.00748.x. [DOI] [PubMed] [Google Scholar]
- Rockafellow B D, Saules K K. Substance use by college students: The role of intrinsic versus extrinsic motivation for athletic involvement. Psychology of Addictive Behaviors. 2006;20(3):279–287. doi: 10.1037/0893-164X.20.3.279. [DOI] [PubMed] [Google Scholar]
- Rodriguez D, Audrain-McGovern J. Team sport participation and smoking: Analysis with general growth mixture modeling. Journal of Pediatric Psychology. 2004;29(4):299–308. doi: 10.1093/jpepsy/jsh031. [DOI] [PubMed] [Google Scholar]
- Rodriguez D, Moss H B, Audrain-McGovern J. Developmental heterogeneity in adolescent depressive symptoms: Associations with smoking behavior. Psychosomatic Medicine. 2005;67(2):200–210. doi: 10.1097/01.psy.0000156929.83810.01. [DOI] [PubMed] [Google Scholar]
- Sallis J F, Prochaska J J, Taylor W C. A review of correlates of physical activity of children and adolescents. Medicine & Science in Sports & Exercise. 2000;32(5):963–975.. doi: 10.1097/00005768-200005000-00014. Retrieved from http://ovidsp.tx.ovid.com/sp-3.4.2a/ovidweb.cgi?&S=AFIFFPGCFPDDKGJKNCBLGGJCFEAEAA00&Link+Set=S.sh.15.16.20.24|14|sl_10. [DOI] [PubMed] [Google Scholar]
- Soldz S, Huyser D J, Dorsey E. Characteristics of users of cigars, bidis, and kreteks and the relationship to cigarette use. Preventive Medicine. 2003;37(3):250–258. doi: 10.1016/s0091-7435(03)00121-x. [DOI] [PubMed] [Google Scholar]
- SRNT. Biochemical verification of tobacco use and cessation. Nicotine & Tobacco Research. 2002;4(2):149–159. doi: 10.1080/14622200210123581. [DOI] [PubMed] [Google Scholar]
- Telama R, Yang X, Viikari J, Valimaki I, Wanne O, Raitakari O. Physical activity from childhood to adulthood: A 21-year tracking study. American Journal of Preventive Medicine. 2005;28(3):267–273. doi: 10.1016/j.amepre.2004.12.003. [DOI] [PubMed] [Google Scholar]
- Tercyak K P, Audrain J. Psychosocial correlates of alternate tobacco product use during early adolescence. Preventive Medicine. 2002;35(2):193–198. doi: 10.1006/pmed.2002.1060. [DOI] [PubMed] [Google Scholar]
- Terry-McElrath Y M, O'Malley P M, Johnston L D. Exercise and substance use among American youth, 1991-2009. American Journal of Preventive Medicine. 2011;40(5):530–540. doi: 10.1016/j.amepre.2010.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- USDHHS. Physical activity and health: A report of the surgeon general: Centers of Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion. 1996. Retrieved from http://www.cdc.gov/nccdphp/sgr/sgr.htm.
- van Mechelen W, Twisk J W, Post G B, Snel J, Kemper H C. Physical activity of young people: The Amsterdam Longitudinal Growth and Health Study. Medicine & Science in Sports & Exercise. 2000;32(9):1610–1616.. doi: 10.1097/00005768-200009000-00014. Retrieved from http://ovidsp.tx.ovid.com/sp-3.4.2a/ovidweb.cgi?&S=FJGJFPECAKDDKGLKNCBLCAOBAFGCAA00&Link+Set=S.sh.15.16.20.24|14|sl_10. [DOI] [PubMed] [Google Scholar]
- Verkooijen K T, Nielsen G A, Kremers S P J. Leisure time physical activity motives and smoking in adolescence. Psychology of Sport and Exercise. 2009;10(5):559–564. [Google Scholar]
- Wills T A, Cleary S D. The validity of self-reports of smoking: Analyses by race/ethnicity in a school sample of urban adolescents. American Journal of Public Health. 1997;87(1):56–61. doi: 10.2105/ajph.87.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuckerman M. Behavioural expressions and biosocial bases of sensation seeking. Cambridge: Cambridge University Press; 1994. [Google Scholar]