Abstract
Background
There is increasing evidence for phenomenological, biological and genetic overlap between schizophrenia and bipolar disorder, bringing into question the traditional dichotomy between them. Neurobiological models linked to dimensional clinical data may provide a better foundation to represent diagnostic variation in neuropsychiatric disorders.
Method
To capture the interaction between psychosis and affective symptoms dimensionally, we devised a brief descriptive scale based on the type and relative proportions of psychotic and affective symptoms over the illness course. The scale was administered to a series of 762 patients with psychotic disorders, including schizophrenia, schizoaffective and psychotic bipolar disorder assessed as part of the Bipolar- Schizophrenia Network for Intermediate Phenotypes (B-SNIP) study.
Results
The resulting Schizo-Bipolar Scale scores across these disorders showed neither a clear dichotomy nor a simple continuous distribution. While the majority of cases had ratings close to prototypic schizophrenia or bipolar disorder, a large group (45% of cases) fell on the continuum between these two prototypes. .
Conclusions
Our data suggest a hybrid conceptualization model with a representation of cases with prototypic schizophrenia or bipolar disorder at the extremes, but a large group of patients on the continuum between them that traditionally would be considered schizoaffective. A dimensional approach, using the Schizo-Bipolar Scale, characterized patients across a spectrum of psychopathology. This scale may provide a valuable means to examine the relationships between schizophrenia and psychotic bipolar disorder.
Keywords: schizophrenia, bipolar disorder, schizoaffective disorder, continuum
Introduction
There is increasing evidence for phenomenological, biological and genetic overlap between schizophrenia and bipolar disorders (Potash & Bienvenu 2009; Potash 2006), bringing into question the traditional Kraepelinian dichotomy between these illnesses, and calling for conceptually new approaches to classification (Cheniaux et al 2008; Craddock et al 2009; Ivleva et al 2010). Ever since Kasanin (1933) originally proposed the term “schizoaffective psychosis”, this concept has remained a conundrum in psychiatric nosology and a diagnostic entity with poor reliability. This diagnosis has been variously thought to reflect: a) a variant of schizophrenia in which mood symptoms are unusually prominent but not unusual in type, b) a severe form of either major depressive or bipolar disorder in which episode-related psychotic symptoms fail to remit completely between mood episodes; c) a distinct disorder, and d) comorbid illness in which the individual is doubly unfortunate to have both disorders (Brockington and Meltzer 1983).
A categorical approach is limited by at least three key challenges. First, the heterogeneity of schizoaffective disorder reflects the possibility that this disorder may straddle the middle of a continuum between schizophrenia and bipolar disorder. In the 1980’s schizoaffective disorder was categorized into two types by research diagnostic criteria (RDC): prolonged non-affective psychosis and poor premorbid function was thought to characterize the mainly schizophrenia subtype of schizoaffective disorder; prolonged or recurrent affective syndromes and relatively brief psychotic periods were thought to characterize the mainly affective subtype of schizoaffective disorder (Spitzer et al 1978; Winokur et al 1996). The classification by DSM-IV (American Psychiatric Association, 1994) is into schizoaffective disorder, depressive type which tends to have outcomes similar to schizophrenia, while schizoaffective bipolar type tends to resemble bipolar disorder (Coryell et al 1987; Van Eerdewegh et al 1987; Keck et al 1996). The relative proportions of psychotic and affective symptoms as well as the type of the affective syndrome therefore are key components in its diagnosis and subtyping, generating a de-facto dimensional concept of schizoaffective disorder. Second, the reliability and stability of the DSM-IV schizoaffective diagnosis is poor (Forrester et al 2001; Kane 2010); in part because of its basic disease characteristics being poorly specified, and perhaps from confusion in applying criteria on episodic vs lifetime information (Salvatore et al 2011). . While criterion C for schizoaffective disorder in DSM-IV requires mood episode symptoms having been present for a “substantive” portion of the illness duration, no quantitative thresholds are set up for this judgment (Heckers, 2009). Third, the validity and the biological utility of categorical diagnoses in this situation depend on whether there exist natural distinctions between these psychotic and affective entities, distinctions which are expressed in a point or “zone” of rarity if adjacent disorders are examined on a continuum (Kendell and Jablensky 2003). There is controversy as to whether schizophrenia and psychotic bipolar disorders show such a point of rarity in the phenotype or their associated genotype (Bora et al 2010; Grozewa et al 2010). Because of these challenges, some clinicians have suggested abandoning schizoaffective disorder as an entity; alternatively, incorporating the two disorders onto one dimension may generate a more meaningful “serious mental illness” outcome (Gaebel and Zielasek 2009; Heckers 2009; Malhi et al 2008; Peralta and Cuesta 2008). If these disorders represent a true continuum, the relative admixture of psychotic and affective symptoms would show a continuous distribution between schizophrenia and psychotic bipolar disorder. To examine this phenomenological question, we constructed a simple scale to quantify salient characteristics of the psychotic and affective syndromal dimensions and administered it to a series of patients diagnosed categorically as having schizophrenia, schizoaffective or psychotic bipolar disorder..
Methods
This study sample included 762 probands recruited as part of the ongoing multi-site Bipolar- Schizophrenia Network for Intermediate Phenotypes (B-SNIP; Thaker 2008); the B-SNIP study recruits patients with ‘psychosis’ and, therefore, samples not only traditional diagnoses of schizophrenia or Bipolar Disorder 1, but also individuals with any combination of schizophrenia or psychotic bipolar disorder features, generating a more naturalistic recruitment of patients with the target diagnoses. Participants were aged 15–65 years, of both sexes, and had a DSM-IV diagnosis of schizophrenia, schizoaffective or psychotic bipolar disorder. Patients with current or recent substance use disorder (within the past month), mental retardation or psychoses secondary to medical illness or substance abuse were excluded. Diagnoses were based on site-specific consensus meetings after reviewing detailed medical and psychiatric history, chart reviews, and the Structured Clinical Interview for DSM Disorders (SCID; First et al 1991) carried out by trained and reliable clinicians at each site; complex cases were discussed by raters across all sites. Moreover, monthly cross-site diagnostic sessions were held, attended by all diagnosticians, where a variety of B-SNIP cases were presented, discussed and inter-rater reliability was evaluated. In addition we obtained symptom ratings using the Positive and Negative Symptom Scale (PANSS) (Kay et al 1987) and Young Mania rating Scale (Young et al 1978). The study sites included Baltimore (GT), Dallas (CT), Detroit and Boston (MSK), Hartford (GP) and Chicago (JS). All participants provided informed consent, and the study was approved by the respective Institutional Review Boards at each site. Using SCID- based DSM-IV-TR diagnoses, of the 762 probands, 341 were classified as having schizophrenia, 243 as bipolar disorder, 119 as schizoaffective disorder, bipolar type and 59 as schizoaffective disorder, depressed type.
The probands were rated by trained clinical raters on a new Schizo-Bipolar Scale (Table 1), a 10 point scale that rates three key elements of the schizophrenia- psychotic bipolar disorder continuum: (1) overall extent of non-affective psychosis as a proportion of the psychotic illness, (2) overall extent of manic syndrome as a proportion of the overall illness duration, and (3) the predominant type of mood symptoms (manic vs. depressive), when present. The first two items were designed, respectively, to quantify the relative proportions of nonaffective psychosis and the extent of the affective syndrome (weighted on mania since this is a Schizo-Bipolar, and not a schizoaffective scale) relative to the overall illness duration, which constitute the two key elements of the schizoaffective diagnosis in DSM-IV. Scoring is based on life-time history of active phases of illness (i.e. current and past episodes of psychosis and mood syndromes. The third item was included to determine the predominant polarity (over lifetime) of the affective syndrome (manic vs. depressive), in view of the literature suggesting that such polarity may be related to the diagnoses being closer to schizophrenia or bipolar disorder (Coryell et al 1987; Van Eerdewegh et al 1987; Keck et al 1996). In determining this item score, mood symptoms that have not reached episodic level (i.e. major depressive or mood syndromes) are also included. The sum of scores on these three items yields a total score between 0–9, with 0 representing the most bipolar-like and 9 representing the most schizophrenia-like disorder. Explicit guidelines are available for scoring, and are available upon request.
Table 1.
Schizo-Bipolar Scale and Psychopathology Characteristics Among Patients with Bipolar Disorder, Schizoaffective Disorder, and Schizophrenia (N = 762).
| Variable | Group | Analysis | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| (1) | (2) | (3) | (4) | Fa | Direction | |
| Bipolar N= 243 |
Schizoaffective (Bipolar) N= 119 |
Schizoaffective (Depressed) N= 59 |
Schizophrenia N= 341 |
|||
| Schizo- Bipolar Scale | 1.06 (1.11) | 4.35 (1.04) | 6.15 (1.28) | 7.94 (1.15) | 1786.82** | 1 < 2 < 3 < 4 |
| PANSS | ||||||
| Positive | 13.25 (4.44) | 18.56 (4.69) | 16.88 (5.31) | 16.64 (5.70) | 34.28** | 1 < 2, 3, 4; 2 > 4 |
| Negative | 12.19 (3.94) | 15.59 (5.01) | 16.40 (5.27) | 16.61 (5.96) | 35.45** | 1 < 2, 3, 4 |
| General | 29.31 (7.94) | 35.32 (8.38) | 33.93 (8.89) | 31.73 (8.94) | 14.52** | 1 < 2, 3, 4; 2 > 4 |
| Manic Symptoms | 1.33 (.65) | 1.53 (.79) | 1.38 (.67) | 1.57 (.91) | 4.51* | 1 < 4 |
| Depressive Symptoms | 2.78 (1.44) | 3.31 (1.55) | 3.50 (1.38) | 2.37 (1.35) | 19.32** | 1, 4 < 2, 3; 1 > 4 |
Numerator df = 3, denominator df ranges from 730 to 758
Schizo-Bipolar Scale scores were first examined for their differences between the diagnostic categories using analyses of variance (ANOVAs), and the distribution of these scores was examined across the psychosis spectrum using descriptive statistics and distributions of normality. We evaluated inter-rater reliability within and across sites in 17 cases which were rated independently by 10 raters in 6 sites. A two-way mixed (Judges fixed) effect model was used to compute Intraclass Correlation Coefficient (ICC)(Shrout and Fleiss, 1979).
Results
We first examined the characteristics of the Schizo-Bipolar Scale by investigating its distributional properties across patients diagnosed with DSM IV TR bipolar disorder, schizoaffective disorder, and schizophrenia. Inter-rater reliability yielded a Intra-class Correlation Coefficient (ICC) single measure (3,1) equal to 0.94 and ICC(3,10) average measure of 0.99. ICCs between sites were 0.95 for single items [ICC(3,1)] and 0.99 for total scores [ICC(3,5)]. The within site ICCs for the 3 multi-rater sites (n=2, n=3, n=3) ranged from 0.94 to 0.98 for single measures [ICC(3,1)] and from 0.97 to 0.99 for average measures [ICC(3,2/3)]. The scale had high internal consistency among the three items (Cronbach’s alpha= 0.84).
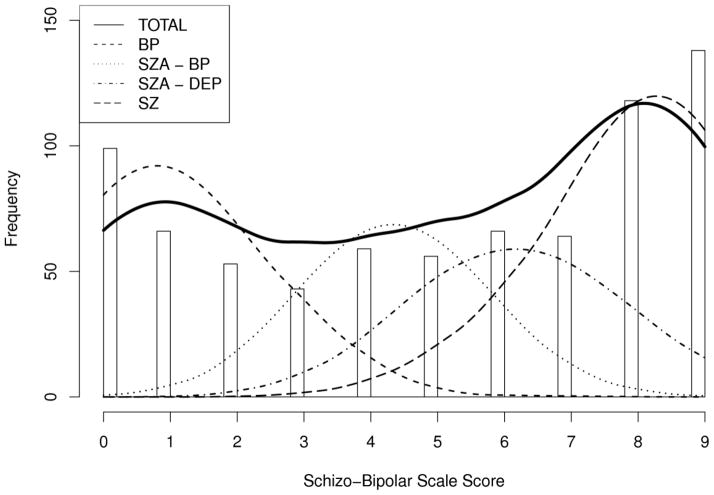
Figure 1 shows the distribution of the total Schizo-Bipolar scores. A larger number of cases were seen at either end of the distribution (scores 0–1: n= 165; 8–9: n= 256), but there were 341 subjects (45% of the sample) in the middle ranges. When conducting statistical analysis of the degree to which this distribution exhibited multimodal characteristics using Hartigan’s (1985) dip statistic, results revealed significant departure from unimodality (dip = 0.08, p < 0.001). An overlay of Co-sine curves for different diagnostic groups as defined by DSM across the distribution of Schizo-Bipolar Scale scores demonstrated marked distributional differences (see Figure 1). As expected, there was little overlap in scores between patients with bipolar disorder and those with schizophrenia, who tended to score at the extreme of the distribution on the scale, whereas individuals with schizoaffective disorder scored intermediately and overlapped with both bipolar disorder and schizophrenia score ranges.
Figure 1.
Schizo-Bipolar Scale scores across diagnostic groups, showing the distributions respresented by co-sine curves..
After finding evidence for multimodal distributions for the Schizo-Bipolar Scale across conventional diagnoses, we conducted a series of ANOVAs to examine Schizo-Bipolar and psychopathology score differences between patients with DSM IV TR-diagnosed bipolar disorder, schizoaffective disorder (bipolar and depressive types), and schizophrenia. As shown in Table 1, ANOVA models confirmed distributional analyses indicating that bipolar disorder patients scored lowest on the Schizo-Bipolar scale, with schizoaffective disorder patients scoring intermediate, and schizophrenia patients scoring highest. Further, as expected, patients with schizoaffective disorder, bipolar type scored closer to bipolar disorder patients, where those with the depressed type of schizoaffective disorder scored closer to the middle of the continuum; thus, the two types of schizoaffective disorder were not symmetrically positioned relative to schizophrenia and bipolar disorder. Psychopathology assessments generally confirmed these findings, with schizophrenia and schizoaffective disorder patients scoring higher on measures of positive and negative symptoms. In general, patients with schizoaffective disorder tended to demonstrate the greatest level of general psychopathology and depression.
Discussion
When DSM IV TR schizophrenia and bipolar disorders are examined phenomenologically on a Schizo-Bipolar dimension, their distribution overlapped significantly. While disorders at the extreme end of the psychosis spectrum differed predictably across the Schizo-Bipolar dimension to reflect prototypic classifications of schizophrenia and bipolar disorder, no clear-cut discontinuity was evident between the adjacent categories. This suggests a non-categorical distribution of psychotic and affective elements among a population of seriously mentally ill research volunteers with a history of psychosis. Because the pathophysiology of psychosis remains obscure, and thus lacks biomarkers, genetic research into the disorder has usually taken clinical, phenomenologically defined entities as its starting point (Allen et al, 2009). In considering disease risk, rather than overt illness categories, a dimensional approach to analyze schizo-bipolarity is therefore more likely to be very fruitful when examining endophenotypes and the genome. This conceptual approach is also consonant with the recently proposed NIMH Research Domain Criteria project (RDoCs; http://www.nimh.nih.gov/research-funding/rdoc.shtml), that seeks new ways of classifying psychopathology cutting across disorders as traditionally defined, based on dimensions of observable behavior and neurobiological measures to be studied across multiple levels of analysis, from genes to neural circuits to behaviors. In fact, the Schizo-Bipolar scale was explicitly developed for use in the BSNIP study (Thaker 2008), a multi-site study of psychotic disorders that gathers multiple biological measures in order to detect relationships between neurobiological and clinical variables.
To our knowledge no similar prior effort exists in representing the key diagnostic characteristics of psychotic disorders on a dimensional continuum between schizophrenia and psychotic bipolar disorders. The strengths of our approach lies in the assessment of cross-sectional and life-time information of bipolar and psychotic symptomatology in a large sample of these subjects in the same study. In our experience, the Schizo-Bipolar Scale is reliable, easy to use, and can be completed relatively quickly after a diagnostic interview complemented by informant interviews and chart reviews as needed. Limitations include the fact that comprehensive information about life-time affective and psychotic symptoms is at best an approximation, as it relies on autobiographical memory, and availability of adequate collateral and medical record information. However, it should be noted that our SBS ratings were based not only on SCID interviews, but often by reports from relatives also recruited into the study and reviews of chart notes when they were available. Also, all of this information was reviewed at a consensus diagnosis meeting where SBS scores were determined. Second, it is to be noted that this scale addressed the schizophrenia-bipolar continuum, and not the full psychotic disorder spectrum (by not including the psychotic depression patients); further work is needed to examine the spectrum from schizophrenia to major depression with psychosis as well as organic psychotic disorders more fully. Third, as currently developed, this scale uses only the psychosis and affective dimensions. Psychopathological dimensions such as symptomatology, such as mood congruent vs non- congruent delusions may also be relevant to the schizophrenia vs psychotic bipolar disorder distinction (ref); another aspect of symptomatology considered to be sufficient for dagnosis in DSM-IV criteria is bizarreness of delusions. We will consider incorporating these measures in the next iteration of the schizobipolar scale. However, the reliability of assessing these measures is debatable especially when reviewing past episodes of the iillness (Cermolacce et al 2010; Kumazaki, 2011).
More data are needed to examine the reliability and longitudinal stability of Schizo-Bipolar Scale ratings, and the extent to which scores on this scale might inform the etiopathological similarities and distinctions that may exist across the spectrum of psychotic disorders. Further work is likely to offer a useful clinical tool for the practicing clinician as the field moves toward a judicious combination of categorical and dimensional approaches to psychiatric classificatory systems.
Our results suggest that the depressive and bipolar subtypes of schizoaffective disorder may represent categorical captures of a continuous reality, supporting the case for schizoaffective disorder as an intermediate category, not weakening. A major question for the field is whether psychotic disorders should be categorized at all or whether a continuous dimensional representation is more appropriate. It may well be that like with blood pressures or resting blood sugars, we need to impose cutoffs on the dimensional realities to be able to address diagnosis and treatment.
Clearly, as in many aspects of psychiatric diagnosis, those favoring categorical and dimensional models (the lumpers and the splitters) have had differing views of psychotic disorders; this debate is a critical component of current thinking in DSM5 (www.dsm5.org). Some recent studies suggest dimensional approaches do not necessarily offer better predictive power than categorical diagnoses (Moller et al 2011). The results of the present study rather suggest in the words of Lewis Carroll that “all have won and all shall have prizes”. Many patients conformed to prototypic categorical diagnoses of schizophrenia or bipolar disorder, yet the percent of patients that did not fit neatly into those categories was also quite considerable. Thus, a hybrid conceptualization model is indicated with a high representation of cases with prototypic schizophrenia or bipolar disorder together with a large group of patients on the continuum between them. In this situation, forcing patients into one of the diagnoses of schizophrenia or bipolar disorder may often not be appropriate. Placing these non-prototypic patients on a continuum between the disorders may be appropriate using a strategy such as the Schizo-Bipolar Scale, indicating a need for studies addressing questions about treatment implications and about the neurobiological similarities of intermediate cases with those of the prototype disorders.
Acknowledgments
Role of Funding Source Role of Funding Source
This study was supported in part by NIMH grants MH 78113 (MSK); R01 MH077945 (Pearlson) MH 77852 (Thaker), MH 77851 (CT), MH077862 (JS) and KL2 RR024154 (SME)
We are grateful for our collaborators Drs. David Schretten, James Gold, Hilary Blumberg, Trisha Suppes, Elliot Gershon, Melvin McKinnis and Nashaat Boutros for their contributions to this study. We also thank Julie Paavola and Tejas Bhojraj for their very thoughtful contributions to the data analyses.
Footnotes
Contributors
Matcheri Keshavan wrote the first draft of the manuscript. All authors contributed to and have approved the final manuscript.
Conflict of Interest
There are no other conflicts relevant to this work.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Allen AJ, Griss ME, Folley BS, Hawkins KA, Pearlson GD. Endophenotypes in schizophrenia: a selective review. Schizophr Res. 2009;109(1–3):24–37. doi: 10.1016/j.schres.2009.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American psychiatric association. Diagnostic and statistical manual of mental Disorders. 4. American Psychiatric Association; Washington DC: 1994. [Google Scholar]
- Bora E, Yücel M, Pantelis C. Cognitive impairment in schizophrenia and affective psychoses: implications for DSM-V criteria and beyond. Schizophr Bull. 2010;36(1):36–42. doi: 10.1093/schbul/sbp094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brockington IF, Meltzer HY. The nosology of schizoaffective psychosis. Psychiatr Dev. 1983;1(4):317–38. [PubMed] [Google Scholar]
- Cheniaux E, Landeira-Fernandez J, Lessa Telles L, Lessa JL, Dias A, Duncan T, Versiani M. Does schizoaffective disorder really exist? A systematic review of the studies that compared schizoaffective disorder with schizophrenia or mood disorders. J Affect Disord. 2008;106(3):209–17. doi: 10.1016/j.jad.2007.07.009. [DOI] [PubMed] [Google Scholar]
- Cermolacce M, Sass L, Parnas J. What is bizarre in bizarre delusions? A critical review. Schizophr Bull. 2010;36(4):667–79. doi: 10.1093/schbul/sbq001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coryell W, Grove W, vanEerdewegh M, Keller M, Endicott J. Outcome in RDC schizo-affective depression: the importance of diagnostic subtyping. J Affect Disord. 1987;12(1):47–56. doi: 10.1016/0165-0327(87)90060-7. [DOI] [PubMed] [Google Scholar]
- Craddock N, O’Donovan MC, Owen MJ. Psychosis genetics: modeling the relationship between schizophrenia, bipolar disorder, and mixed (or “schizoaffective”) psychoses. Schizophr Bull. 2009;35(3):482–90. doi: 10.1093/schbul/sbp020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, Williams JB, Gibbon M, First MB. The Structured Clinical Interview for DSM-III-R (SCID). I: History, rationale, and description. Arch Gen Psychiatry. 1992;49(8):624–9. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- Forrester A, Owens DG, Johnstone EC. Diagnostic stability in subjects with multiple admissions for psychotic illness. Psychol Med. 2001;31(1):151–8. doi: 10.1017/s0033291799003116. [DOI] [PubMed] [Google Scholar]
- Gaebel W, Zielasek J. Future classification of psychotic disorders. Eur Arch Psychiatry Clin Neurosci. 2009;259(Suppl 2):S213–8. doi: 10.1007/s00406-009-0049-6. [DOI] [PubMed] [Google Scholar]
- Grozeva D, Kirov G, Ivanov D, Jones IR, Jones L, Green EK, St Clair DM, Young AH, Ferrier N, Farmer AE, McGuffin P, Holmans PA, Owen MJ, O’Donovan MC, Craddock N. Wellcome Trust Case Control Consortium. Rare copy number variants: a point of rarity in genetic risk for bipolar disorder and schizophrenia. Arch Gen Psychiatry. 2010;67(4):318–27. doi: 10.1001/archgenpsychiatry.2010.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckers S. Is schizoaffective disorder a useful diagnosis? Curr Psychiatry Rep. 2009;11(4):332–7. doi: 10.1007/s11920-009-0048-3. [DOI] [PubMed] [Google Scholar]
- Ivleva EI, Morris DW, Moates AF, Suppes T, Thaker GK, Tamminga CA. Genetics and intermediate phenotypes of the schizophrenia--bipolar disorder boundary. Neurosci Biobehav Rev. 2009;34(6):897–921. doi: 10.1016/j.neubiorev.2009.11.022. [DOI] [PubMed] [Google Scholar]
- Kane JM. Strategies for making an accurate differential diagnosis of schizoaffective disorder. J Clin Psychiatry. 2010;71(Suppl 2):4–7. doi: 10.4088/JCP.9096su1cc.01. [DOI] [PubMed] [Google Scholar]
- Kasanin J. The acute schizoaffective psychoses. Am J Psychiatry. 1994;151(6 Suppl):144–54. doi: 10.1176/ajp.151.6.144. [DOI] [PubMed] [Google Scholar]
- Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261–76. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- Keck PE, Jr, McElroy SL, Strakowski SM. New developments in the pharmacologic treatment of schizoaffective disorder. J Clin Psychiatry. 1996;57(Suppl 9):41–8. [PubMed] [Google Scholar]
- Kendell R, Jablensky A. Distinguishing between the validity and utility of psychiatric diagnoses. Am J Psychiatry. 2003;160(1):4–12. doi: 10.1176/appi.ajp.160.1.4. [DOI] [PubMed] [Google Scholar]
- Kumazaki T. What is a ‘mood-congruent’ delusion? History and conceptual problems. History of Psychiatry. 2011;22(3):315–331. doi: 10.1177/0957154X10390438. [DOI] [PubMed] [Google Scholar]
- Malhi GS, Green M, Fagiolini A, Peselow ED, Kumari V. Schizoaffective disorder: diagnostic issues and future recommendations. Bipolar Disord. 2008;10(1 Pt 2):215–30. doi: 10.1111/j.1399-5618.2007.00564.x. [DOI] [PubMed] [Google Scholar]
- Möller HJ, Jäger M, Riedel M, Obermeier M, Strauss A, Bottlender R. The Munich 15-year follow-up study (MUFUSSAD) on first-hospitalized patients with schizophrenic or affective disorders: assessing courses, types and time stability of diagnostic classification. Eur Psychiatry. 2011;26(4):231–43. doi: 10.1016/j.eurpsy.2010.04.012. [DOI] [PubMed] [Google Scholar]
- Peralta V, Cuesta MJ. Exploring the borders of the schizoaffective spectrum: a categorical and dimensional approach. J Affect Disord. 2008;108(1–2):71–86. doi: 10.1016/j.jad.2007.09.009. [DOI] [PubMed] [Google Scholar]
- Potash JB, Bienvenu OJ. Neuropsychiatric disorders: Shared genetics of bipolar disorder and schizophrenia. Nat Rev Neurol. 2009;5(6):299–300. doi: 10.1038/nrneurol.2009.71. [DOI] [PubMed] [Google Scholar]
- Potash JB. Carving chaos: genetics and the classification of mood and psychotic syndromes. Harv Rev Psychiatry. 2006;14(2):47–63. doi: 10.1080/10673220600655780. [DOI] [PubMed] [Google Scholar]
- Salvatore P, Baldessarini RJ, Tohen M, Khalsa HM, Sanchez-Toledo JP, Zarate CA, Jr, Vieta E, Maggini C. McLean-Harvard International First-Episode Project: two-year stability of ICD-10 diagnoses in 500 first-episode psychotic disorder patients. J Clin Psychiatry. 2011;72(2):183–93. doi: 10.4088/JCP.09m05311yel. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrout PE, Fleiss JL. Intraclass Correlations: Uses in Assessing Rater Reliability. Psychological Bulletin. 1979;86(2):420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Endicott J, Robins E. Research diagnostic criteria: rationale and reliability. Arch Gen Psychiatry. 1978;35(6):773–82. doi: 10.1001/archpsyc.1978.01770300115013. [DOI] [PubMed] [Google Scholar]
- Thaker G. Psychosis endophenotypes in schizophrenia and bipolar disorder. Schizophr Bull. 2008;34(4):720–721. doi: 10.1093/schbul/sbn055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Eerdewegh MM, Van Eerdewegh P, Coryell W, Clayton PJ, Endicott J, Koepke J, Rochberg N. Schizo-affective disorders: bipolar-unipolar subtyping. Natural history variables: a discriminant analysis approach. J Affect Disord. 1987 May-Jun;12(3):223–32. doi: 10.1016/0165-0327(87)90031-0. [DOI] [PubMed] [Google Scholar]
- Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry. 1978;133:429–35. doi: 10.1192/bjp.133.5.429. [DOI] [PubMed] [Google Scholar]
- Winokur G, Monahan P, Coryell W, Zimmerman M. Schizophrenia and affective disorder--distinct entities or continuum?: an analysis based on a prospective 6-year follow-up. Compr Psychiatry. 1996 Mar-Apr;37(2):77–87. doi: 10.1016/s0010-440x(96)90566-0. [DOI] [PubMed] [Google Scholar]