Lung cancer is the leading cause of cancer-related death and, even with detection and curative resection of early-stage non-small-cell lung cancer, 30–50% of patients will die of the disease.1,2 Determination of prognosis is not optimal with available clinical pathological characteristics, so many attempts have been made to develop biomarkers that could provide prognostic information.3,4
Lung cancers with different prognoses should have different biological properties, which in turn should be reflected in different gene expression profiles. In the best of all scenarios, these differentially expressed genes would also be functionally relevant and potential therapeutic targets. If such tumours could be identified when patients have only microscopic disease, curative treatment should be most effective. Yet in practice this approach has been very challenging—many studies have yielded prognostic signatures, but these seldom overlap with other signatures. Prognostic signatures are usually tested and validated in small samples, with methods that might not be transferable to real-life clinical situations. Thus, the report by Johannes Kratz and colleagues5 in The Lancet is important, providing a lung cancer molecular prognostic signature that seems ready for widespread use.
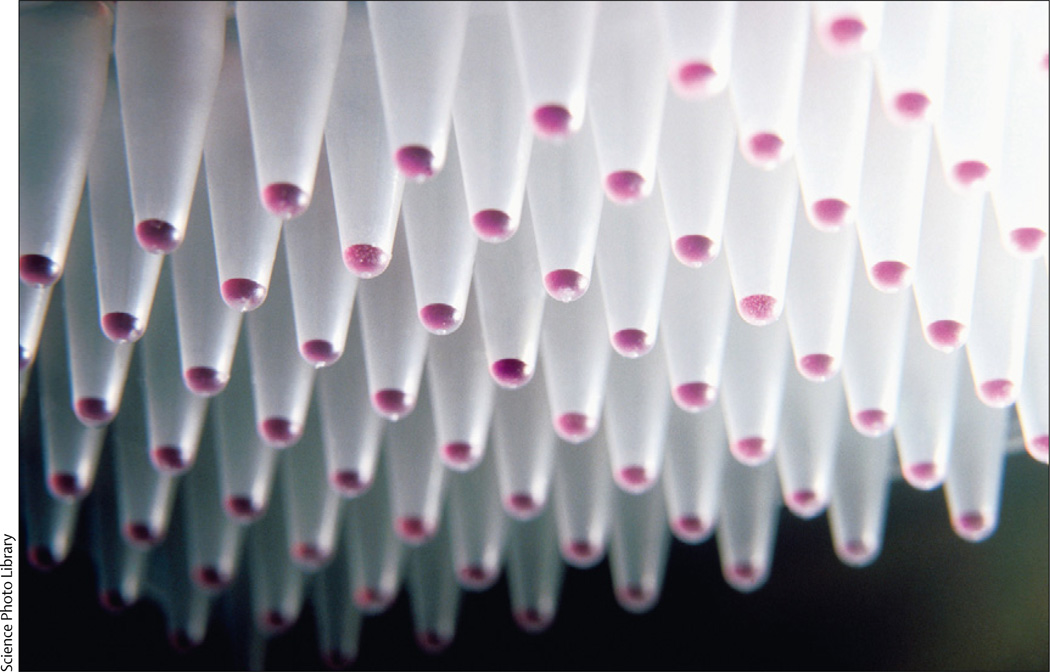
A 14-gene mRNA expression assay (including 11 target genes and three reference genes) for prognosis in early-stage non-squamous non-small-cell lung cancer (NSCLC) was developed and run with rigorous technical validation guidelines. The assay uses quantitative PCR and runs on widely available formalin-fixed paraffin-embedded tissue samples, with collection and processing techniques common in clinical practice. The assay improved prognostic accuracy through rigorous independent and blinded validation in a US cohort (433 patients) and a separate Chinese cohort (1006 patients). The analysis identified those at high, intermediate, and low risk of lung-cancer-related death, and the hazard ratio of the high risk compared with the low risk was 2·04 in one validation cohort after adjusting for routine clinical-pathological variables in multivariate analysis.
Rigorous validation in independent datasets or cohorts is essential, and full documentation is needed to allow independent scrutiny, which is essential particularly after problems with some prognostic signatures.6,7 Although statistical methods can deal with a large number of genes in such signatures, the number of genes plays an important part in the feasibility and cost of assay development, and use in practice. Therefore, good feature-selection approaches—which reduce the number of genes in a signature while achieving similar prediction performance—are crucial in development of a practical assay.8 Kratz and colleagues used a variety of such methods to select 11 target genes from more than 200. A commonly-used feature selection approach ranks the performance of individual genes and selects the top-ranked features. However, this approach does not consider the relation between genes, nor redundancy of information, so the combination of top-ranked individual features might not be optimum. A feature selection approach that could take account of interactions between genes and select a set of genes with high information content might enable the further development of such assays.
Although we believe that Kratz and colleagues’ assay is ready for widespread clinical testing, there are cautions to be considered. First, the signature works for non-squamous lung cancers, meaning that a squamous-cell lung cancer and other non-adenocarcinoma variants must first be ruled out by pathology. However, errors can be made, and many such NSCLCs are scored by pathologists as NSCLC not otherwise specified, and additional immunohistochemical studies are needed.9,10 Thus, an important aspect in the success of this assay is whether or not the signature works in squamous-cell lung cancer and all NSCLCs, irrespective of histological subtype. If not, other signatures will need to be developed.
Kratz and colleagues selected tumour samples that had different amounts of tumour cells, all substantial compared with the associated tumour microenvironment. Some previous signatures implicated immune-response genes (probably coming from the microenvironment), and so future studies will need to establish if such genes are also of prognostic value.11 Evidence suggests that a subpopulation of cells within the tumour (so-called cancer stem cells) plays an important part in metastasis and treatment resistance, and that lung cancers with increased numbers of such cells have a worse prognosis.12,13 Thus, whether or not Kratz and colleagues’ signature will need to take into account lung cancers with different amounts of cancer stem cells will be of great interest.
Although most studies focus on the prediction performance of molecular signatures, the biological relevance of genes in the signature is important. For example, one study showed that nuclear receptors can define prognosis markers for lung cancer that are probably of functional relevance and might be potential therapeutic targets.14 A related example is whether the expression of genes that are synthetic lethals with oncogenotype or chemotherapy (eg, their continued expression is required for tumour cell survival in the presence of a specific mutation such as KRAS, or administered chemotherapy like a taxane) could be of prognostic and therapeutic importance15
In addition to the identification of patients with poor prognosis who need additional treatment, the availability of biomarker signatures that will be predictive of better survival when coupled with specific therapy will be important.16 Together, prognostic and predictive markers will allow personalised medicine for each lung cancer patient—determining who needs additional therapy and what specific type of therapy to use.16,17 Further studies will tell whether the genes in the Kratz and colleagues’ signature are of functional relevance, and whether they will provide predictive information about how a patient with lung cancer responds to adjuvant treatment.
Acknowledgments
JDM is supported by a research grant from Geron and is an adviser to AMGEN.
Footnotes
YX declares that she has no conflicts of interest.
References
- 1.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62:10–29. doi: 10.3322/caac.20138. [DOI] [PubMed] [Google Scholar]
- 2.Team TNLSTR. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365:395–409. doi: 10.1056/NEJMoa1102873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shedden K, Taylor JM, Enkemann SA, et al. Gene expression-based survival prediction in lung adenocarcinoma: a multi-site, blinded validation study. Nat Med. 2008;14:822–827. doi: 10.1038/nm.1790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xie Y, Minna JD. Predicting the future for people with lung cancer. Nat Med. 2008;14:812–813. doi: 10.1038/nm0808-812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kratz JR, He J, Van Den Eeden SK, et al. A practical molecular assay to predict survival in resected non-squamous, non-small-cell lung cancer: development and international validation studies. Lancet. 2012;379:823–832. doi: 10.1016/S0140-6736(11)61941-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coombes KR, Wang J, Baggerly KA. Microarrays: retracing steps. Nat Med. 2007;13:1276–1277. doi: 10.1038/nm1107-1276b. [DOI] [PubMed] [Google Scholar]
- 7.Subramanian J, Simon R. Gene expression-based prognostic signatures in lung cancer: ready for clinical use? J Natl Cancer Inst. 2010;102:464–474. doi: 10.1093/jnci/djq025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Minna JD, Girard L, Xie Y. Tumor mRNA expression profiles predict responses to chemotherapy. J Clin Oncol. 2007;25:4329–4336. doi: 10.1200/JCO.2007.12.3968. [DOI] [PubMed] [Google Scholar]
- 9.Rekhtman N, Ang DC, Sima CS, Travis WD, Moreira AL. Immunohistochemical algorithm for differentiation of lung adenocarcinoma and squamous cell carcinoma based on large series of whole-tissue sections with validation in small specimens. Mod Pathol. 2011;24:1348–1359. doi: 10.1038/modpathol.2011.92. [DOI] [PubMed] [Google Scholar]
- 10.Travis WD, Rekhtman N. Pathological diagnosis and classification of lung cancer in small biopsies and cytology: strategic management of tissue for molecular testing. Semin Respir Crit Care Med. 2011;32:22–31. doi: 10.1055/s-0031-1272866. [DOI] [PubMed] [Google Scholar]
- 11.Roepman P, Jassem J, Smit EF, et al. An immune response enriched 72-gene prognostic profile for early-stage non-small-cell lung cancer. Clin Cancer Res. 2009;15:284–290. doi: 10.1158/1078-0432.CCR-08-1258. [DOI] [PubMed] [Google Scholar]
- 12.Sullivan JP, Spinola M, Dodge M, et al. Aldehyde dehydrogenase activity selects for lung adenocarcinoma stem cells dependent on notch signaling. Cancer Res. 2010;70:9937–9948. doi: 10.1158/0008-5472.CAN-10-0881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ooi AT, Mah V, Nickerson DW, et al. Presence of a putative tumor-initiating progenitor cell population predicts poor prognosis in smokers with non-small cell lung cancer. Cancer Res. 2010;70:6639–6648. doi: 10.1158/0008-5472.CAN-10-0455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jeong Y, Xie Y, Xiao G, et al. Nuclear receptor expression defines a set of prognostic biomarkers for lung cancer. PLoS Med. 2010;7:e1000378. doi: 10.1371/journal.pmed.1000378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Whitehurst AW, Bodemann BO, Cardenas J, et al. Synthetic lethal screen identification of chemosensitizer loci in cancer cells. Nature. 2007;446:815–819. doi: 10.1038/nature05697. [DOI] [PubMed] [Google Scholar]
- 16.Xie Y, Minna JD. Non-small-cell lung cancer mRNA expression signature predicting response to adjuvant chemotherapy. J Clin Oncol. 2010;28:4404–4407. doi: 10.1200/JCO.2010.31.0144. [DOI] [PubMed] [Google Scholar]
- 17.Zhu CQ, Ding K, Strumpf D, et al. Prognostic and predictive gene signature for adjuvant chemotherapy in resected non-small-cell lung cancer. J Clin Oncol. 2010;28:4417–4424. doi: 10.1200/JCO.2009.26.4325. [DOI] [PMC free article] [PubMed] [Google Scholar]