Abstract
This clinical case report describes the oral rehabilitation of an adult female patient diagnosed with hypoplastic amelogenesis imperfecta with inadequate, deteriorated restorations of anterior teeth, inadequate clinical crown heights of posterior teeth due to severe attrition of hypoplastic enamel. Treatment included extraction of teeth with poor prognosis, root canal treatment and crown lengthening of severely worn out teeth & full coverage porcelain-fused-to metal fixed restoration of entire dentition. The main objectives of the selected treatment were to enhance the esthetics, restore masticatory function and eliminate the teeth sensitivity. These treatment objectives were successfully met by sequential fixed prosthodontics treatment using Pankey–Mann–Schuyler philosophy of complete occlusal rehabilitation. Treatment not only restored function and esthetic, but also showed a positive psychological impact and thereby improved perceived quality of life.
Keywords: Amelogenesis imperfect, Mutilated dentition, Faulty restoration, Fixed prosthodontics, Pankey–Mann–Schuyler philosophy
Introduction
Amelogenesis imperfecta (AI) encompasses a heterogeneous group of developmental disorders that demonstrates alterations in the enamel [1]. It is characterized by clinical and genetic heterogeneity in the absence of systemic abnormalities or diseases [1, 2]. AI is caused by mutations in genes that control amelogenesis and follows inheritance patterns of autosomal-dominant, autosomal recessive or X-linked modes of transmission [1–3]. There are also patients for whom a family history cannot be identified but where a mutation is present. An ideal classification of AI has not yet been established [3]. These anomalies can be classified as hypocalcified, hypoplastic, or hypomature based on clinical findings, radiographic findings and hereditary criteria [4, 5]. In the hypoplastic type, there is a deficiency in the quantity of enamel; the mineralization of enamel appears to be normal, hard and shiny, however it is malformed. In the hypocalcified type, the enamel is formed in relatively normal amounts but is poorly mineralized, soft, and friable and can be easily removed from the dentin. In the hypomaturation type, enamel appears mottled, opaque white to red-brown coloration, and is softer than normal and tends to chip from the underlying dentin. Other dental anomalies associated with amelogenesis imperfecta include, multiple impacted teeth, congenitally missing teeth, and taurodontism [6–8].
Clinical problems of AI patients mainly include poor esthetics, sensitivity of teeth, chewing difficulties, loss of tooth substance due to chipping and attrition, higher risk for dental caries, open occlusal relationship and decreased occlusal vertical dimension. According to a survey, treating the AI patient is not only important from a functional standpoint, but from a psychosocial health standpoint also [9, 10]. Results of the survey reported that patients with AI experience higher levels of social avoidance combined with a reduced perceived quality of life compared to those without AI, and that treatment has a positive psychosocial impact [10].
This clinical report describes the sequenced treatment for an adult female patient with mutilated natural dentition associated with amelogenesis imperfecta using Pankey–Mann–Schuyler philosophy of complete occlusal rehabilitation.
Clinical Report
A 27-year old female patient, diagnosed with hypoplastic amelogenesis imperfect presented to the department of Prosthodontics, with chief complaint of difficulty in mastication, sensitivity and discoloration of teeth and unsatisfactory fractured crowns on some anterior teeth. Family history revealed that her brother is also suffering from similar condition. Medical history does not showed any systemic condition or disease that contraindicates dental treatment. Past dental history revealed that patient had undergone extraction of tooth 25 due to caries, endodontic treatment of 36 and fixed dental prosthetic treatment at the age of 20 years in the form of metal ceramic crowns on 14, 13, 12, 11, 21, 22, 23, 24 (as a single unit), 34, 33, 32, 31, 41, 42, 43, 44 (as a single unit).
On clinical examination (Figs. 1, 2), 25 was missing, PFM crowns were present on 12, 11, 21, 22, 33, 32, 31, 41, 42, and 43. Mandibular and maxillary molars showed severe attritional wear with very short clinical crown heights, resulting into loss of vertical dimension of occlusion. All teeth showed yellowish brown discoloration with rough irregular crowns. Deep caries lesions were seen on 15, 27, 37, and 46 with tenderness to percussion. There was generalized dentinal hypersensitivity and generalized interdental spacing with no proximal contacts between teeth. Patient’s oral hygiene was unsatisfactory with multiple carious teeth and gingivitis in mandibular and maxillary anterior region. On radiographic examination (Fig. 4), periapical radiolucent lesions were seen surrounding the roots of 15, 46 and endodontically treated 36. Diagnostic impressions were made with irreversible hydrocolloid impression material (Tropicalgin, Zhermack, Italy) and poured in type III dental stone (Kalabhai Karson, Mumbai) to obtain diagnostic casts. Diagnostic casts were mounted on a semi adjustable articulator using facebow (Fig. 3) and centric interocclusal records.
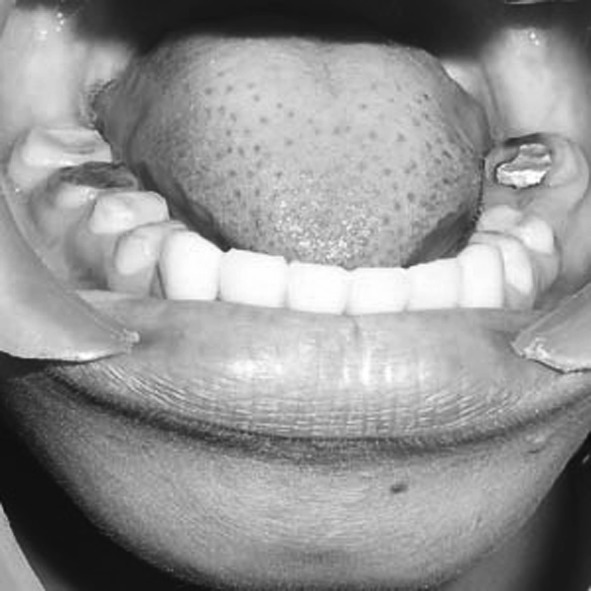
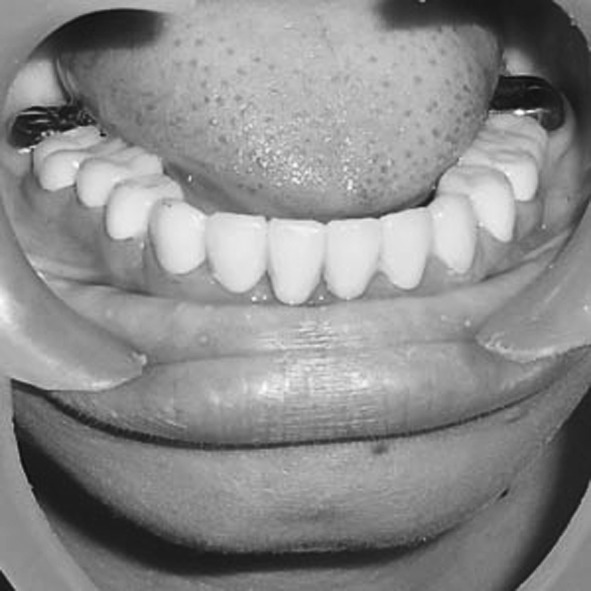
Fig. 1.
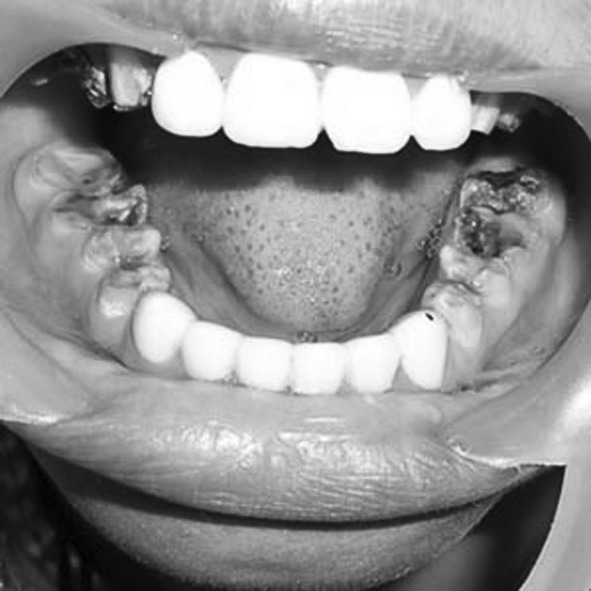
Preoperative mandibular dentition
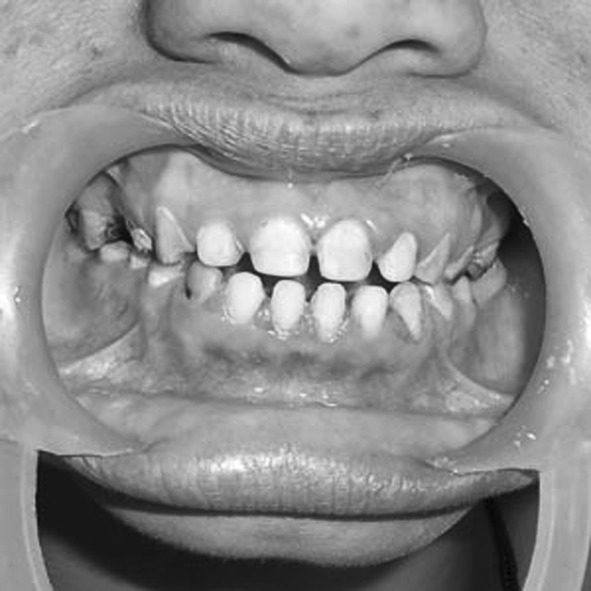
Fig. 2.

Preoperative maxillary dentition
Fig. 4.

Preoperative OPG radiograph
Fig. 3.
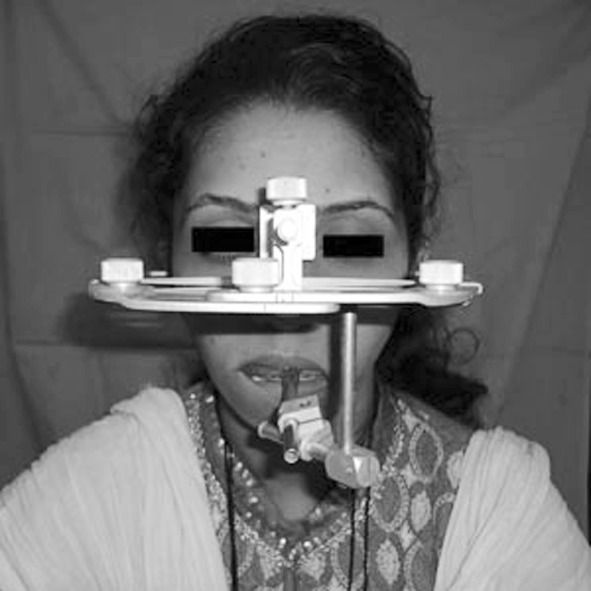
Facebow transfer
Using mounted diagnostic models, along with clinical and radiographic findings, the treatment plan was formulated. The patient was informed about the surgical, periodontal, endodontic and restorative procedures required and all other treatment alternatives including the differences in costs, the levels of tooth structure removal, the expected clinical longevity, the time period necessary to conclude the treatment, and the possible esthetic result. Treatment plan included removal of faulty prostheses on anterior teeth, scaling and root planning, extraction of root piece of 15 and endodontically treated 36 (as repeat endodontic treatment was not possible because it has broken instrument in mesiobuccal canal during previous endodontic treatment), endodontic treatment of 27, 37, and 46 followed by crown lengthening of posterior teeth with very short clinical crown heights and finally full mouth rehabilitation by metal ceramic crowns following Pankey–Mann–Schuyler philosophy of complete occlusal rehabilitation.
According to treatment plan extraction of 25 and 36 was done followed by endodontic treatment of 27, 37 and 46. 0.12% chlorhexidine gluconate mouthwash twice a day was prescribed to the patient and instructions regarding proper oral hygiene maintenance were given. Crown lengthening of required teeth was completed using surgical stent as a guide. After 2 weeks of healing, patient was recalled and faulty prostheses on anterior teeth were removed (Fig. 5). Mandibular and maxillary anterior teeth were prepared (Figs. 6, 7) and full arch irreversible hydrocolloid impressions were made and poured in type III dental stone. Diagnostic casts were mounted on semi-adjustable articulator (#8500, Whip mix corp. Kentucky) using facebow (Quickmount facebow, Whip mix corp.) and centric interocclusal record (Aluwax). Vertical dimension of occlusion was raised by 2 mm and diagnostic wax up of anterior teeth was completed (Fig. 8). Heat cured acrylic temporaries (DPI dental products, Mumbai.) were fabricated from diagnostic wax up and tried intraorally to evaluate esthetic, phonetics and to harmonize anterior guidance. After the anterior temporary crowns were found to be satisfactory, they were cemented in place with temporary cement (Templute, Prime dental products, Mumbai). Mandibular and maxillary posterior teeth were prepared (Figs. 9, 10) and full arch impressions were made with irreversible hydrocolloid. Resultant casts were mounted on semi-adjustable articulator using facebow record and centric interocclusal record. Customized anterior guidance table was fabricated in cold cure acrylic resin. A Customized Broadrick’s occlusal plane analyzer was used to develop posterior occlusal scheme and posterior diagnostic wax up was completed. After ensuring posterior disclusion on protrusion and lateral excursion (Fig. 11), temporaries for posterior teeth were fabricated in heat cure using diagnostic wax up. Temporaries were checked intraorally for proper contacts in centric relation and disclusion on protrusion and lateral excursion. Temporaries were cemented in place using temporary cement after they were found to be satisfactory (Figs. 12, 13, and 14). Patient was kept under observation for a period of 3 months. At 3 months recall visit on examination and questioning patient did not reported any discomfort and she was very happy with esthetic and function with temporaries at increased vertical dimension of occlusion. As patient was comfortable with raised vertical dimension of occlusion, it was decided to proceed with permanent restorations.
Fig. 5.
Intraoral view after removal of defective restorations and completion of crown lengthening
Fig. 6.

Mandibular anterior tooth preparation
Fig. 7.

Maxillary anterior tooth preparation
Fig. 8.

Anterior diagnostic wax up
Fig. 9.
Mandibular posterior tooth preparation
Fig. 10.

Maxillary posterior tooth preparation
Fig. 11.

Posterior disclusion on protrusion
Fig. 12.

Full mouth temporization
Fig. 13.

Posterior disclusion on protrusion (right side)
Fig. 14.

Posterior disclusion on protrusion (left side)
Mandibular and maxillary anterior temporaries were removed, gingival tissue was retracted using pre-impregnated retraction cord (PD dental products) and final impressions were made in vinyl polysiloxane impression material (Aquasil soft putty and light body, Dentsply). Impressions were poured in type IV dental stone (Kalabhai Karson, Mumbai) to obtain working casts. Working casts were mounted on the semi-adjustable articulator using facebow record and centric interocclusal record. Metal copings (KeraN, Germany) were fabricated and tried intraorally to check marginal accuracy and fit (Figs. 15, 16). Ceramic (d-Sign, Ivoclar Vident, Liechtenstein) build up was carried out followed by bisque trial. After minor adjustments metal ceramic crowns were glazed, polished and cemented in place using GIC (Ketac Cem, 3M ESPE, Germany). Next the mandibular and maxillary posterior temporaries were removed, gingival tissue was retracted using retraction cord and final impressions were made in vinyl polysiloxane impression material. Impressions were poured in type IV dental stone to obtain working casts, which were mounted on same articulator using facebow and centric interocclusal records. Customized anterior guidance table was fabricated in cold cure acrylic resin. Wax up for metal copings on 14, 15, 16 (3 unit bridge), 24, 25, 26 (3 unit bridge), 34, 35, 36 and full metal crowns on 17, 27, 37, and 47 were completed. Posterior occlusal scheme was developed using custom made Broadrick’s occlusal plane analyzer (Fig. 17). Wax up was evaluated for centric contacts and disclusion in eccentric movements followed by casting, coping trial (Figs. 18, 19), ceramic build up and bisque trial. After minor adjustments in bisque trial, metal ceramic crowns were glazed and polished and finally cemented in place (Figs. 20, 21, and 22).
Fig. 15.

Mandibular anterior coping try-in
Fig. 16.

Maxillary anterior coping try-in
Fig. 17.

Customized Broadrick’s occlusal plane analyzer used to cutback the wax patterns
Fig. 18.

Mandibular posterior coping try in
Fig. 19.

Maxillary posterior coping try in
Fig. 20.
Postoperative mandibular dentition
Fig. 21.

Postoperative maxillary dentition
Fig. 22.
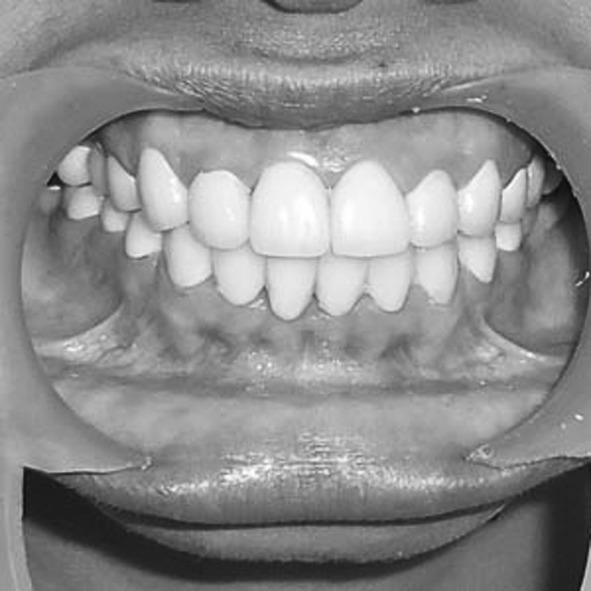
Postoperative intraoral view
Instructions regarding maintenance of proper oral hygiene were given to the patient and patient was recalled for evaluation at an interval of a month for 3 months. At recall visits, patient was very happy with improved esthetic and function by oral rehabilitation (Fig. 23). On clinical examination soft tissues were healthy and restorations in satisfactory function without any complications.
Fig. 23.

Postoperative extraoral view
Discussion
The prosthetic rehabilitation of Al patients has been previously presented in several case reports [11–14]. Historically, patients with AI have been treated with extractions or with the construction of complete removable dentures. These options are psychologically harsh when the problem must be addressed in adolescent patients. Currently the different materials and methods for restorative procedures are available and have made it both exciting and confusing for dental practitioners. It should be pointed out that, limitations exist, and the application of techniques are not universal [15]. The treatment for patients with amelogenesis imperfecta is related to many factors including the age of patients, the socio-economic status, the type and severity of the disorder, its intra oral manifestation and aesthetic and functional demands. Treatment plan should have common goals i.e., functional, aesthetic and longevity of restoration, yet the approaches being slightly different. Adhesive restorative techniques, over-dentures, porcelain-fused-to metal crowns, fixed partial dentures, full porcelain crowns, and inlay/onlay restorations are all used for the prosthodontic treatment of AI patients [11, 15, 16].
In the present case porcelain fused to a metal alloy approach was utilized except for second molars. Both the marginal fit and the color acceptability of the restorations were satisfactory. The option of using porcelain laminate veneers for anterior teeth was eliminated as all anterior teeth were previously prepared for full crowns. Pankey–Mann–Schuyler’s philosophy of full mouth rehabilitation was used for the restoration of all teeth, which is the simplest and effective means of achieving treatment objectives in stepwise manner [17]. The anterior guidance was established first with the diagnostic wax up and it was incorporated in the temporary restorations. This was followed by developing posterior occlusal scheme using Broadrick’s occlusal plane analyzer. Ultimately, the occlusion with stable contacts in centric and no interference in eccentric movements was developed.
Summary
Case report is presented to describe the functional and esthetic rehabilitation of amelogenesis imperfecta with porcelain-fused-to metal and full metal crowns using Pankey–Mann–Schuyler philosophy of occlusal rehabilitation. Treatment objectives were achieved by accurate diagnosis, meticulous treatment planning together with a dedicated team approach involving different disciplines in dentistry.
Contributor Information
Jitendra J. Mete, Email: jeetendra1685@gmail.com
Shankar P. Dange, Email: drdange4@gmail.com
Arun N. Khalikar, Email: drkhalikar@yahoo.com
Smita P. Vaidya, Email: smitakhalikar@yahoo.com
References
- 1.Aren G, Ozdemir D, Firatli S, Uygur C, Sepet E, Firatli E. Evaluation of oral, systemic manifestations in an amelogenesis imperfecta population. J Dent. 2003;31(8):585–591. doi: 10.1016/S0300-5712(03)00116-7. [DOI] [PubMed] [Google Scholar]
- 2.Stephanopoulos G, Garefalaki ME, Lyroudia K. Genes and related proteins involved in amelogenesis imperfecta. J Dent Res. 2005;84(12):1117–1126. doi: 10.1177/154405910508401206. [DOI] [PubMed] [Google Scholar]
- 3.Aldred MJ, Savarirayan R, Crawford PJ. Amelogenesis imperfecta: a classification, catalogue for the 21st century. Oral Dis. 2003;9(1):19–23. doi: 10.1034/j.1601-0825.2003.00843.x. [DOI] [PubMed] [Google Scholar]
- 4.Soares CJ, Fonseca RB, Martins LR, Giannini M. Esthetic rehabilitation of anterior teeth affected by enamel hypoplasia: a case report. J Esthet Restor Dent. 2002;14(6):340–348. doi: 10.1111/j.1708-8240.2002.tb00176.x. [DOI] [PubMed] [Google Scholar]
- 5.Wright TJ, Robinson C, Shore R. Characterization of the enamel ultrastructure and mineral content in hypoplastic amelogenesis imperfecta. Oral Surg Oral Med Oral Pathol. 1991;72(5):594–601. doi: 10.1016/0030-4220(91)90499-3. [DOI] [PubMed] [Google Scholar]
- 6.Witkop CJ, Rao SR. Inherited defects in tooth structure. Birth Defects Orig Artic Ser. 1971;7:153–184. [PubMed] [Google Scholar]
- 7.Aldred MJ, Crawford PJM. Variable expression in amelogenesis imperfecta with taurodontism. J Oral Pathol Med. 1988;17:327–333. doi: 10.1111/j.1600-0714.1988.tb01545.x. [DOI] [PubMed] [Google Scholar]
- 8.Ayers KMS, Drummond BK, Harding WJ, Salis SG, Liston PN. Amelogenesis imperfecta-multidisciplinary management from eruption to adulthood. Review and case report. N Z Dent J. 2004;100:101–104. [PubMed] [Google Scholar]
- 9.Seow WK. Clinical diagnosis and management strategies of amelogenesis imperfecta variants. Pediatr Dent. 1993;15(6):384–393. [PubMed] [Google Scholar]
- 10.Coffield KD, Phillips C, Brady M, Roberts MW, Strauss RP, Wright JT. The psychosocial impact of developmental dental defects in people with hereditary amelogenesis imperfecta. J Am Dent Assoc. 2005;136(5):620–630. doi: 10.14219/jada.archive.2005.0233. [DOI] [PubMed] [Google Scholar]
- 11.Nel JC, Pretorius JA, Weber A, Marais JT. Restoring function and esthetics in a patient with amelogenesis imperfecta. Int J Periodontics Restor Dent. 1997;17:478–483. [PubMed] [Google Scholar]
- 12.Bouvier D, Duprez JP, Pirel C, Vincent B. Amelogenesis imperfecta-a prosthetic rehabilitation: a clinical report. J Prosthet Dent. 1999;82:130–131. doi: 10.1016/S0022-3913(99)70144-7. [DOI] [PubMed] [Google Scholar]
- 13.Encias RP, Garcia-Espona I, Mondela JMNR. Amelogenesis imperfecta: diagnosis and resolution of a case with hypoplasia and hypocalcification of enamel, dental agenesis, and skeletal open bite. Quintessence Int. 2001;32:183–189. [PubMed] [Google Scholar]
- 14.Greenfield R, Iacono V, Zove S. Periodontal and prosthodontic treatment of amelogenesis imperfecta: a clinical report. J Prosthet Dent. 1992;68:572–574. doi: 10.1016/0022-3913(92)90367-J. [DOI] [PubMed] [Google Scholar]
- 15.Li RWK. Adhesive solutions: report of a case using multiple adhesive techniques in the management of enamel hypoplasia. Dent Update. 1999;26:277–287. doi: 10.12968/denu.1999.26.7.277. [DOI] [PubMed] [Google Scholar]
- 16.Williams WP, Becker LH. Amelogenesis imperfecta: functional and esthetic restoration of a severely compromised dentition. Quintessence Int. 2000;31:397–403. [PubMed] [Google Scholar]
- 17.Mann A, Pankey L, Part I. Use of the P-M instrument in treatment planning and in restoring the lower posterior teeth. J Prosthet Dent. 1960;10:135–150. doi: 10.1016/0022-3913(60)90098-6. [DOI] [Google Scholar]


