Abstract
Despite the material advancements and precise laboratory techniques, cement lines are inevitable in fixed prosthodontics which leads to increased dependence on the integrity of the cement to maintain the marginal seal. The material class of luting agent is known to influence microleakage. Studies of cement dissolution and disintegration have produced varying results. Hence, this study was done to evaluate marginal leakage under complete metal crowns using three adhesive cements, two resin cements (one self cure, one dual cure) and a glass ionomer cement. Metal crowns were prepared on sixty intact extracted premolars and were randomly divided into three groups of twenty each, with each group using a different cement for luting. All the samples were then subjected to thermocycling and were sectioned using a diamond saw. Reflected Binocular Stereomicroscope at 100× magnification was used to study the extent of microleakage at both metal cement (MC) and tooth cement (TC) interface, at two opposite margins of each sectioned specimen. Data was analyzed with a one way analysis of variance. For comparison among the groups multiple comparison Bonferroni test was done. Within group data was analysed with independent student t test. Between three groups, metal crowns cemented with multilink cement showed significantly less microleakage at both the interfaces. Glass ionomer cement recorded maximum combined microleakage amongst three cements irrespective of the interfaces. Within group, glass ionomer and multilink cement showed more microleakage at MC interfaces than at TC interface. A complex interaction between variables related to dental restoration, luting agent and tooth structure probably influence microleakage. In vitro studies must always be followed by in vivo studies before definite conclusion can be drawn.
Keywords: Adhesive luting cements, Microleakage, Thermocycling
Introduction
The ultimate goal of any prosthetic treatment is providing the patient with a precisely fabricated restoration which preserves the long term integrity of natural abutments of fixed partial dentures and their pulpal vitality [1]. An extracoronal restoration that has been completed precisely with attention to detail on a sound foundation has the best and most predictable prognosis [2].
Despite the material advancements and precise laboratory techniques, cement lines are inevitable in fixed prosthodontics and some degree of marginal discrepancy is always expected. Fusayama et al [3] discovered that marginal adaptation of cemented crowns is never perfect and the cast restorations usually display a marginal discrepancy [4]. This leads to increased dependence on the integrity of the cement to maintain the marginal seal [5].
At present, there is no luting cement with zero or complete insolubility in the oral environment and due to this solubility, luting cements in general have been described as the “weak link” in restoring teeth with cast restoration [4–7]. The cement therefore must have good mechanical properties, be as stable and insoluble as possible in the oral environment, should have a good adhesion to the tooth structure as well as to the restoration to resist bacterial penetration [8, 9]. Luting materials offering a high degree of bonding strength and relative insolubility in the oral environment have shown to have a negative impact on microleakeage around the restoration [10–13].
There is no universally accepted technique to determine marginal permeability at the interface between the tooth and the restoration. Use of dyes [1, 2, 6], radioactive isotopes [14], air pressure [15], bacteria [16], neutron activation analysis [17, 18], and artificial caries [19] has been documented. Modification of axial walls and alteration in configuration of the finish lines have been done to see the effect of tooth preparation variables on microleakage [20, 21]. Microleakage assessment has been done under complete coverage restorations by completing the wax pattern on spaced dies, using vents during cementation [22, 23], with different crown foundation materials [2, 10, 24] and luting with different cements [1, 2, 4–6, 8, 10, 11, 13, 14, 25, 26].
Studies of cement dissolution and disintegration have produced varying results. Hence, this study was done to evaluate marginal leakage under complete metal crowns using three adhesive cements, which included two resin cements (Self cure and Dual cure) and a glass ionomer cement.
Statement of Problem
The need to obtain an adequate thickness of the restoration that maintains dental anatomy causes exposure of millions of dentinal tubules. These tubules are potential channels for the diffusion and colonization of the bacteria to the pulp [27].
Normally, there is a balance between the rate of diffusion of bacterial products permeating dentin due to microleakage and the rate at which they are removed by the pulpal circulation. The exposure of more dentin surface during tooth preparation combined with decreased pulpal blood flow, increases the potential for greater microleakage and can permit the concentration of these products to increase, resulting in inflammation [28, 29].
In addition, marginal opening causing cement dissolution and microleakage allows saliva with its bacterial components to penetrate the gap and gain access to circumpulpal dentin from where bacteria and their products easily diffuse to the pulp [12]. This is a major cause of postoperative sensitivity, secondary caries and pulpal necrosis, ultimately leading to clinical failure of the treatment provided [29, 30].
Materials and Method
Preparation of the Samples
Sixty intact extracted human premolars of comparable coronal dimension were stored in water at room temperature till the time of their preparation for complete metal crowns. Teeth were mounted individually in the Typodont jaw (kavo, Charlotte, Germany) and were supported with putty (Flexi Time, Heraeus Kulzer, Germany). The coronal portion of each tooth was prepared with chamfer finish line and a flat occlusal surface. Parallel prep (Parallel-a-Prep, Dentatus, USA) was used for maintaining the uniform taper of the axial wall preparation.
Wax pattern was made (Crown wax: hard blue, Bego, Germany) after applying 2 layers of die spacer on all the surfaces, except around 1 mm of the prepared margin for the crown. Sprue (Bego, Germany) was attached while the pattern was still on the die and then was invested in phosphate bonded investment (Star glow, Starvest, Germany). Casting was completed using base metal alloy (Bellabond Plus, Bego, Germany) in an induction casting machine and were adjusted on their respective dies, polished and fitted on the prepared teeth. All sixty samples were randomly divided into three groups of twenty teeth each, with each group using a different cement for luting.
Group 1 self cure resin luting cement (Multilink cement, Ivoclar Vivadent, Leichenstein, Germany).
Group 2 dual cure resin luting cement (Adhesive bridge cement, Ivoclar Vivadent, Leichenstein, Germany).
Group 3 glass ionomer luting cement (GC Fuji, GC Corporation, Japan). Manufacturer’s instructions were followed to mix the cements.
Thermocycling Procedure
One hour after cementation of the crowns, all the samples in each group were mounted in the plaster base and were stored for 24 h in water at room temperature (31°C, 74% relative humidity) before thermocycling. Each thermal cycle consisted of immersing the samples alternatively in water bath (Metzer Biomedical and Electronics Ltd, Mumbai, India) maintained at 5 and 55°C. 1,000 cycles were done in each water bath with 30 s dwell time and 5 s of transition time.
Microleakage Assessment
After thermocycling was completed, the samples with only their exposed portion were immersed in 5% solution of Indigo carmine dye for 72 h. Samples were then washed in the running water to remove the superficial stains.
Each group was then randomly divided into two subgroups of ten samples each, which were sectioned using diamond wheel (Model 650, South Bay Technology, CA). Reflected Binocular Stereomicroscope (SZX-12, Olympus, Tokyo, Japan) at 100× magnifications was used to study the extent of microleakage, which was indicated by the dye penetration recorded at both metal cement (MC) and tooth cement (TC) interface, at two opposite margins of each sectioned specimen (Fig. 1).
Fig. 1.
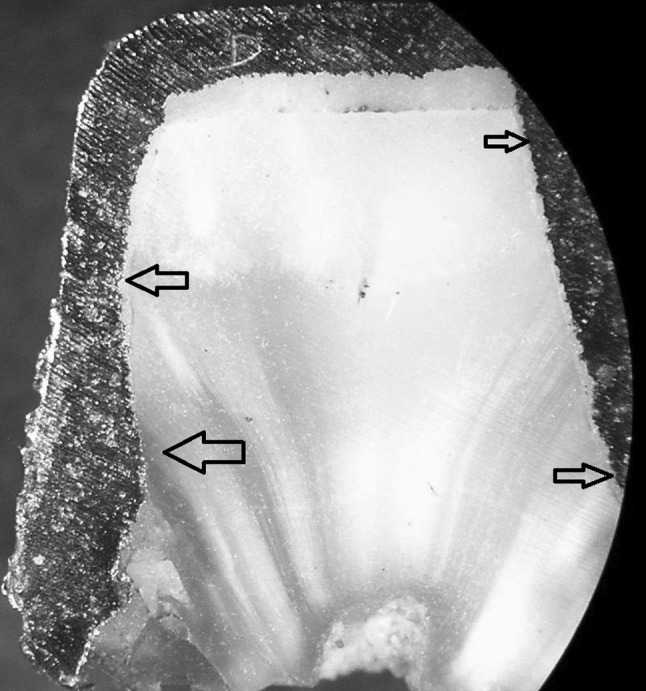
Arrows showing microleakage (dye penetration) more than 2/3rd the axial wall length on left side and on the occlusal surface on the right side
Qualitative assessment of microleakage was done according to the criteria proposed by Tjan et al. [31];
0—No microleakage.
1—Microleakage less than 1/3rd the axial wall length.
2—Microleakage more than 1/3rd but less than 2/3rd the axial wall length.
3—Microleakage all along the axial wall length.
4—Microleakage on the occlusal surface.
The marginal leakage of each sample was the average of the scores of dye penetration recorded at the opposite margins of each sectioned specimen, both at MC and TC interface. The data of all the three groups was analyzed with a one way analysis of variance. For comparison among the groups multiple comparison Bonferroni test was done and student t test was used to compare the microleakage scores within the group at both the interfaces. The statistical analysis was done with a software package (SPSS/PC+, SPSS, version 7.50, Chicago).
Results
Raw data of marginal leakage for the three cements at both the interfaces (Table 1) and mean, standard deviation, standard error and minimum and maximum of the microleakage scores at TC and MC interface (Table 2) is shown.
Table 1.
Raw data of marginal leakage at both metal cement and tooth cement interface
| Cement | Multilink | Adhesive bridge | Glass ionomer | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number | TC | MC | TC | MC | TC | MC | ||||||
| BL | MD | BL | MD | BL | MD | BL | MD | BL | MD | BL | MD | |
| 1 | 0.5 | 0 | 0 | 0 | 1.5 | 1 | 0.5 | 0 | 1 | 1 | 4 | 2 |
| 2 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0.5 | 1 | 0 | 1 | 4 |
| 3 | 0.5 | 0 | 0 | 0 | 1 | 0.5 | 2.5 | 0.5 | 0.5 | 1.5 | 1.5 | 3 |
| 4 | 0.5 | 0 | 0.5 | 1.5 | 0.5 | 1 | 2 | 0 | 0.5 | 3.5 | 0 | 3 |
| 5 | 0 | 0 | 0 | 0 | 0.5 | 1.5 | 2 | 2 | 0.5 | 0 | 1 | 0 |
| 6 | 0 | 0.5 | 0 | 0 | 1 | 1 | 2 | 0 | 1 | 0.5 | 1.5 | 1 |
| 7 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 2.5 | 0 | 1 | 3 | 0 |
| 8 | 0.5 | 0 | 0.5 | 0 | 0.5 | 0.5 | 3.5 | 0.5 | 3 | 1 | 0 | 2.5 |
| 9 | 0 | 0 | 0 | 0 | 1 | 1.5 | 0 | 0.5 | 2.5 | 0 | 4 | 1 |
| 10 | 0 | 0 | 0 | 1.5 | 0.5 | 0 | 2.5 | 0 | 0.5 | 1 | 1 | 2 |
| Mean | 0.125 | 0.2 | 1.1 | 1.075 | 1 | 1.775 | ||||||
Table 2.
Mean standard deviation, standard error and minimum and maximum of the microleakage scores at tooth cement and metal cement interface
| Interface | Cement | N | Mean | Std. deviation | Std. error | Min. | Max |
|---|---|---|---|---|---|---|---|
| TC | Multilink | 20 | 0.125 | 0.2221 | 0.0497 | 0 | 0.5 |
| Glass ionomer | 20 | 1 | 0.9733 | 0.2176 | 0 | 3.5 | |
| Adhesive bridge | 20 | 1.1 | 1.0463 | 0.2340 | 0 | 2.0 | |
| Total | 60 | 0.74166 | 0.9320 | 0.1203 | 0 | 3.5 | |
| MC | Multilink | 20 | 0.2 | 0.4702 | 0.1051 | 0 | 1.5 |
| Glass ionomer | 20 | 1.775 | 1.3715 | 0.3067 | 0 | 4 | |
| Adhesive bridge | 20 | 1.075 | 1.1502 | 0.2572 | 0 | 3.5 | |
| Total | 60 | 1.01666 | 1.2350 | 0.1594 | 0 | 4 |
One way analysis of variance revealed highly significant association between the cement type and microleakage at TC interface and MC interface (Table 3). Therefore, the multiple comparison Bonferroni test was conducted to find out difference between various pair of cements (Table 4).
Table 3.
One-way analysis of variance at tooth cement and metal cement interface
| DF | Sum of squares | Mean square | F ratio | Significance | ||
|---|---|---|---|---|---|---|
| TC | Between groups | 2.0000 | 11.5083 | 5.7542 | 8.2539 | 0.00 |
| Within groups | 57.0000 | 39.7375 | 0.6971 | |||
| Total | 59.0000 | 51.2458 | ||||
| MC | Between groups | 2.0000 | 24.9083 | 12.4542 | 10.9088 | 0.00 |
| Within groups | 57.0000 | 65.0750 | 1.1417 | |||
| Total | 59.0000 | 89.9833 |
Table 4.
Multiple comparison Bonferroni test
| Dependent variable | (I) Cement | (J) Cement | Mean diff (I−J) | Std. error | Sig. P value |
|---|---|---|---|---|---|
| TC | Multilink | Glass ionomer | −0.875 | 0.264035816 | 0.004808 |
| Adhesive bridge | −0.975 | 0.264035816 | 0.001496 | ||
| Glass ionomer | Multilink | 0.875 | 0.264035816 | 0.004808 | |
| Adhesive bridge | −0.1 | 0.264035816 | 1 | ||
| Adhesive bridge | Multilink | 0.975 | 0.264035816 | 0.001496 | |
| Glass ionomer | 0.1 | 0.264035816 | 1 | ||
| MC | Multilink cement | Glass ionomer | −1.575 | 0.337885582 | 0.00 |
| Adhesive bridge | −0.875 | 0.337885582 | 0.04 | ||
| Glass ionomer | Multilink | 1.575 | 0.337885582 | 0.00 | |
| Adhesive bridge | 0.7 | 0.337885582 | 0.13 | ||
| Adhesive bridge | Multilink | 0.875 | 0.337885582 | 0.04 | |
| Glass ionomer | −0.7 | 0.337885582 | 0.13 |
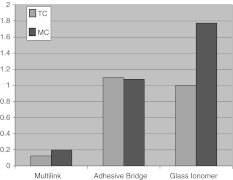
The Bonferroni test at both the interfaces revealed that there was a highly significant difference in mean microleakage values between multilink cement and both the other cements. Difference in mean microleakage between glass ionomer and adhesive bridge cement was not statistically significant (Fig. 2).
Fig. 2.
Multiple bar diagram showing mean microleakage of the three cements at metal cement (MC) and at tooth cement (TC) interface
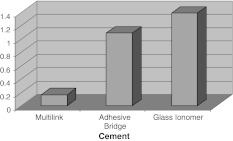
The combined microleakage (TC + MC) was maximum for glass ionomer cement however the difference was statistically significant only between multilink cement and the other two cements (Fig. 3).
Fig. 3.
Simple bar diagram showing combined mean microleakage of the three cements. Maximum for glass ionomer cement and minimum for self cure resin cement
Table 5 shows the group statistics for multilink cement for the comparison of microleakage within each group at both the interface. This was done by independent samples student t test (Table 6).
Table 5.
Group statistics for Multilink cement
| Group | N | Mean | Std. deviation | Std. error mean |
|---|---|---|---|---|
| TC | 20 | 0.125 | 0.222130829 | 0.04967 |
| MC | 20 | 0.2 | 0.470162346 | 0.105131 |
Table 6.
Independent samples student t test
| T | DF | Sig. (2-tailed) |
|---|---|---|
| −0.64502589 | 38 | 0.52278592 |
Discussion
Multiple factors ranging from non retentive tooth preparation, poor casting fit, poor cementing technique, weak cement, to malocclusion, excessive forces of mastication and improper prosthesis usage influence microleakage [1–14, 22].
In addition to the inevitable errors at the margin of restorations, the type of luting agent and its mechanical properties has significant effect on microleakage [32, 33]. Compressive strength may be critical to retention [34], tensile strength to retention and marginal seal [35–37]. Cement with high modulus of elasticity is important to prevent microleakage [38–44]. Water soluble cements (zinc phosphate, glass ionomer, polycarboxylate) are susceptible to tensile failure while resin cements (with higher tensile strength) are prone to fail through cyclic fatigue stresses [39–44].
Glass ionomer cement has shown maximum combined microleakage amongst the three cements evaluated. This may be attributed to its susceptibility to disintegration due to early water contact before maturation and relative weak bond with both dentin and metal superstructure. Powers and Sakaguchi [40] suggested protection for 24 h at the margin and use of acid conditioner followed by aqueous solution of ferric chloride on dentin, while sandblasting and tin plating the castings have been advocated by Graver, Vallittu, Hotz and Hondrum [25, 45–47] to improve glass ionomers bond strength with both the tooth and restoration.
Glass ionomer cement is most susceptible to dissolution during and immediately after initial set due to its prolonged setting reaction in progressive, multiple and overlapping stages. Its modulus of elasticity increases over time and the cement might mature over a period of 24 h to 1 year [40, 42, 44].
In the present study, the glass ionomer cement samples were stored in water after 1 h of the cementation. The effect is dramatically shown in the results by the relatively high leakage with glass ionomer cement due to the presence of excess water during the growth of the hydrated silica phase [48, 49].
Improved bonding to both teeth and the restoration is an advantage with resin cements. However, inherent polymerization shrinkage and high coefficient of thermal expansion are potential concerns with resin based luting agents [41]. These stresses may exceed the adhesive and cohesive strength of the material itself resulting in the formation of the marginal gap at the point of weakest bond leading to marginal leakage at the interface. Davidson et al. [50] highlighted the importance of establishing early bond formation between the resin cements and the two interfaces and hygroscopic expansion to counteract stresses of polymerization shrinkage and decreasing the marginal gap. However, polymerization shrinkage occurs immediately while adequate compensatory hygroscopic expansion would require hours or days. Therefore, the immediate bond strength to dentin is crucial to resist the combined forces of polymerization shrinkage, pattern of contraction and coefficient of thermal expansion mismatch. If adhesion to dentin is lost at the time of resin polymerization, any compensatory hygroscopic expansion cannot completely seal this interface [50–53].
In this study, the samples were stored in water for 24 h. This is a brief period compared to the life expectancy of the cast restorations, but this early storage may have allowed some relaxation of internal stresses caused by polymerization shrinkage of the resin materials. Hygroscopic expansion coupled with their high flexural strength, high modulus of elasticity and adhesive potential might have led to their low microleakage values in comparison to glass ionomer cement [54, 55].
Both resin based cements recorded less microleakage as compared to glass ionomer cement which can be related to their better adhesion to conditioned metal and tooth, their high mechanical strength and inherent relative insolubility.
Between the two resin cements multilink has recorded less microleakage. This better result may be related to its self-curing nature with low curing rate, rapid and superior adhesion to both dentin and restoration and better mechanical properties [56].
A poor interfacial seal and more leakage for adhesive bridge cement as compared to multilink cement may be attributed to the mechanical insufficiency of the bond (between the cement and both the interfaces), combined with its high viscosity, decreased flow, high cement film thickness (Fig. 4), greater polymerization shrinkage due to the bulk of the cement, and inadequate degree of cure through metal restoration (DC%) [39, 57, 58].
Fig. 4.
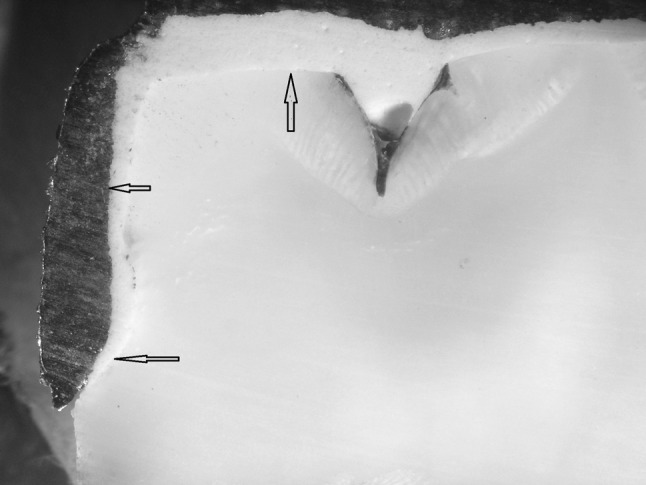
Arrows showing microleakage (dye penetration) more than 2/3rd the axial wall length with adhesive bridge cement. Also showing is the excessive cement layer thickness
In addition to its inherent advantages of the resin cements in inhibiting microleakage, use of metal primers has been advocated to improve the bond strength between the cement and the metal surface which further reduces the microleakage and hence improve clinical durability [58–61].
In vitro microleakage tests carried out with dyes are considered stricter than those carried out in the oral cavity. Therefore, it may be suggested that if a material responds positively to the dye test, it is likely to respond even better on a clinical level.
Conclusion
Between three groups, metal crowns cemented with Multilink cement showed least microleakage. The result was statistically significant both at tooth cement and metal cement interface in comparison to the other two cements.
Glass ionomer cement recorded maximum combined microleakage amongst three cements irrespective of the interfaces.
Within group, glass ionomer and multilink cement showed more microleakage at MC interfaces than at tooth cement interface. Result was statistically significant only for glass ionomer cement. Adhesive bridge cement showed almost equal amount of leakage at both the interface.
A complex interaction between variables related to dental restoration, luting agent and tooth structure influence microleakage. Therefore, precaution has to be taken to standardize these variables and in vitro studies must always be followed by in vivo studies before definite conclusion can be drawn.
Acknowledgments
My sincere gratitude to; Ivoclar Vivadent, Leichenstein, Germany for providing Multilink cement for the study. Dr R.K. Sharma, National Physics Laboratory, New Delhi for helping in sectioning the samples.
References
- 1.Baldissara P, Comin G, Martone F, Scotti R. Comparative study of the marginal leakage of six cements in fixed provisional crowns. J Prosthet Dent. 1998;80:417–422. doi: 10.1016/S0022-3913(98)70005-8. [DOI] [PubMed] [Google Scholar]
- 2.Lindquist TJ, Connolly J. In vitro microleakage of luting cements and crown foundation materials. J Prosthet Dent. 2001;85:292–298. doi: 10.1067/mpr.2001.113705. [DOI] [PubMed] [Google Scholar]
- 3.Fusayama T, Ide K, Hosoda H. Cement thickness between cast restorations and preparation walls. J Prosthet Dent. 1963;13:35–64. doi: 10.1016/0022-3913(63)90181-1. [DOI] [Google Scholar]
- 4.Jacobs MS, Windeler AS. An investigation of dental luting cements solubility as a function of marginal gap. J Prosthet Dent. 1991;65:436–442. doi: 10.1016/0022-3913(91)90239-S. [DOI] [PubMed] [Google Scholar]
- 5.Myers ML, Staffanou RS, Hembree JH, Jr, Wiseman WB. Marginal leakage of contemporary cementing agents. J Prosthet Dent. 1983;50:513–516. doi: 10.1016/0022-3913(83)90571-1. [DOI] [PubMed] [Google Scholar]
- 6.Kydd WL, Nicholls JI, Harrington G, Freeman M. Marginal leakage of cast gold crowns luted with zinc phosphate cement: an in vitro study. J Prosthet Dent. 1996;75:9–13. doi: 10.1016/S0022-3913(96)90411-4. [DOI] [PubMed] [Google Scholar]
- 7.Shen C (2003) Dental cements. In: Anusavice KJ (ed) Phillips’science of dental materials. 11th ed. Saunders, Missouri, p. 456
- 8.Mondelli J, Ishikiriama A, Galan J., Jr Marginal microleakage in cemented complete crowns. J Prosthet Dent. 1978;40:632–636. doi: 10.1016/0022-3913(78)90060-4. [DOI] [PubMed] [Google Scholar]
- 9.Shortall AC. Microleakage, marginal adaptation and composite resin restoration. Br Dent J. 1982;153:223–226. doi: 10.1038/sj.bdj.4804895. [DOI] [PubMed] [Google Scholar]
- 10.Tjan AH, Chiu J. Microleakage of core materials for complete cast gold crowns. J Prosthet Dent. 1989;61:659–664. doi: 10.1016/S0022-3913(89)80037-X. [DOI] [PubMed] [Google Scholar]
- 11.White SN, Sorensen JA, Kang SK, Caputo AA. Microleakage of new crown and fixed partial denture luting agents. J Prosthet Dent. 1992;67:156–161. doi: 10.1016/0022-3913(92)90447-I. [DOI] [PubMed] [Google Scholar]
- 12.Kidd EA. Microleakage: a review. J Dent. 1976;4:199–206. doi: 10.1016/0300-5712(76)90048-8. [DOI] [PubMed] [Google Scholar]
- 13.Ferrari M. Cement thickness and microleakage under dicor crowns: an in vivo study. Int J Prosthodont. 1991;4:126–131. [PubMed] [Google Scholar]
- 14.Mash LK, Beninger CK, Bullard JT, Staffanou RS. Leakage of various types of luting agents. J Prosthet Dent. 1991;66:763–766. doi: 10.1016/0022-3913(91)90411-O. [DOI] [PubMed] [Google Scholar]
- 15.Pickard HM, Gayford JJ. Leakage at the margins of the amalgam restorations. Br Dent J. 1965;119:69–77. [PubMed] [Google Scholar]
- 16.Mortesen DW, Boucher NE, Ryge G. A method of testing for marginal leakage of dental restorations with bacteria. J Dent Res. 1965;4:58–63. doi: 10.1177/00220345650440013101. [DOI] [PubMed] [Google Scholar]
- 17.Going RE, Myers HM, Prussin SG. Quantitative method of studying microleakage in vivo and invitro. J Dent Res. 1968;47:1128–1132. doi: 10.1177/00220345680470061901. [DOI] [PubMed] [Google Scholar]
- 18.Douglas WH, Chen CJ, Craig RG. Improved neutron activation analysis of microleakage around a hydrophobic composite restorative. J Dent Res. 1980;59:1507–1510. doi: 10.1177/00220345800590090901. [DOI] [PubMed] [Google Scholar]
- 19.Grieve JR, Jones JC. An in vitro study of marginal leakage associated with composite restorations using an acidified gas technique. J Oral Rehab. 1980;7:215–233. doi: 10.1111/j.1365-2842.1980.tb00438.x. [DOI] [PubMed] [Google Scholar]
- 20.Gardner FM. Margins of full crowns. J Prosthet Dent. 1982;48:396. doi: 10.1016/0022-3913(82)90072-5. [DOI] [PubMed] [Google Scholar]
- 21.Gavelis JR, Morency JD, Riley Ed, Sozio RB. The effect of various finish line preparations on the marginal seal and occlusal seat of full crown preparations. J Prosthet Dent. 1981;45:138–145. doi: 10.1016/0022-3913(81)90330-9. [DOI] [PubMed] [Google Scholar]
- 22.Eames WB, O’Neal SJ, Monteiro J, Roan JD, Cohen KS. Techniques to improve the seating of the castings. J Am Dent Assoc. 1987;96:432–437. doi: 10.14219/jada.archive.1978.0090. [DOI] [PubMed] [Google Scholar]
- 23.Wang CJ, Millstein PL, Nathanson D. Effects of cement, cement space, marginal design, seating aid materials, and seating force on crown cementation. J Prosthet Dent. 1992;67:786–790. doi: 10.1016/0022-3913(92)90583-V. [DOI] [PubMed] [Google Scholar]
- 24.Larson TD, Jensen JR. Microleakage of composite resin and amalgam core material under complete cast crowns. J Prosthet Dent. 1980;44:40–44. doi: 10.1016/0022-3913(80)90044-X. [DOI] [PubMed] [Google Scholar]
- 25.Graver H, Trowbridge H, Alperstein K. Microleakage of castings cemented with glass ionomer cements. Oper Dent. 1990;15:2–9. [PubMed] [Google Scholar]
- 26.Shortall AC, Fayyad MA, Williams JD. Marginal seal of injection molded ceramic crowns cemented with three adhesive systems. J Prosthet dent. 1989;61:24–27. doi: 10.1016/0022-3913(89)90102-9. [DOI] [PubMed] [Google Scholar]
- 27.Goldman M, Laosonthorn P, White RR. Microleakage-full crowns and the dental pulp. J Endod. 1992;18(10):473–475. doi: 10.1016/S0099-2399(06)81345-2. [DOI] [PubMed] [Google Scholar]
- 28.Pashley DH. Clinical considerations of microleakage. J Endod. 1990;16:70–77. doi: 10.1016/S0099-2399(06)81567-0. [DOI] [PubMed] [Google Scholar]
- 29.Pashley DH. Clinical correlation of dentin structure and function. J Prosthet Dent. 1991;66:777–781. doi: 10.1016/0022-3913(91)90414-R. [DOI] [PubMed] [Google Scholar]
- 30.Nelsen RJ, Wolcott RB, Paffenbarger GC. Fluid exchange at the margins of the restorations. J Am Dent Assoc. 1952;44:288–295. doi: 10.1016/s0002-8177(52)43006-8. [DOI] [PubMed] [Google Scholar]
- 31.Tjan AH, Dunn JR, Grant BE. Marginal leakage of cast gold crowns luted with an adhesive luting cement. J Prosthet Dent. 1992;67:11–15. doi: 10.1016/0022-3913(92)90039-D. [DOI] [PubMed] [Google Scholar]
- 32.Gu XH, Kern M. Marginal discrepancies and leakage of all ceramic crowns: influence of luting agents and aging conditions. Int J Prosthodont. 2003;16:109–116. [PubMed] [Google Scholar]
- 33.White SN, Ingles S, Kipnis V. Influence of marginal opening on microleakage of cemented artificial crowns. J Prosthet Dent. 1994;71:257–264. doi: 10.1016/0022-3913(94)90464-2. [DOI] [PubMed] [Google Scholar]
- 34.Jorgensen KD, Holst K. The relationship between the retention of cemented veneer crowns and casting strength of the cement. Acta Odontol Scand. 1967;25:355–359. doi: 10.3109/00016356709043644. [DOI] [PubMed] [Google Scholar]
- 35.Nicolls JL. Effect of convergence angle variation on the computed stresses in the luting agent. J Prosthet dent. 1974;3:651–657. doi: 10.1016/0022-3913(74)90120-6. [DOI] [PubMed] [Google Scholar]
- 36.Farah JW, Craig RG. Finite element analysis of a restored axisymmetric first molar. J Dent Res. 1974;53:859–866. doi: 10.1177/00220345740530041701. [DOI] [PubMed] [Google Scholar]
- 37.Farah JW, Craig RG. Distribution of stresses in porcelain-fused-to-metal and porcelain jacket crowns. J Dent Res. 1975;54:255–261. [PubMed] [Google Scholar]
- 38.White SN, Yu Z, Tom JF, Sangsurasak S. In vivo microleakage of luting cement for cast crowns. J Prosthet Dent. 1994;71:333–338. doi: 10.1016/0022-3913(94)90090-6. [DOI] [PubMed] [Google Scholar]
- 39.White SN, Yu Z. Physical properties of fixed prosthodontic resin composite luting agents. Int J Prosthodont. 1993;6:384–389. [PubMed] [Google Scholar]
- 40.Powers JM, Sakaguchi RL (2006) Cements. In: Powers JM, Sakaguchi RL (eds) Craig’s restorative dental materials 12th edn. Mosby, Missouri, p 485
- 41.Kumbuloglu O, Lassila LV, User A, Vallittu PK. A study of the physical and chemical properties of four resin composite luting agents. Int J Prosthodont. 2004;17:357–363. [PubMed] [Google Scholar]
- 42.Attar N, Tam LE, McComb D. Mechanical and physical properties of contemporary dental luting agents. J Prosthet Dent. 2003;89:127–134. doi: 10.1067/mpr.2003.20. [DOI] [PubMed] [Google Scholar]
- 43.Knobloch LA, Kerby RE, Seghi R, Berlin JS, Lee JS. Fracture toughness of resin based luting cements. J Prosthet Dent. 2000;83:204–209. doi: 10.1016/S0022-3913(00)80013-X. [DOI] [PubMed] [Google Scholar]
- 44.Li ZC, White SN. Mechanical properties of dental luting cements. J Prosthet Dent. 1999;81:597–609. doi: 10.1016/S0022-3913(99)70216-7. [DOI] [PubMed] [Google Scholar]
- 45.Vallittu PK, Forss H. Adhesion of glass ionomer cement to ceramometal alloy. J Prosthet Dent. 1997;77:12–16. doi: 10.1016/S0022-3913(97)70200-2. [DOI] [PubMed] [Google Scholar]
- 46.Hotz P, Mclean JW, Sced I, Wilson AD. The bonding of glass ionomer cements to metal and tooth substrates. Br Dent J. 1977;142:41–47. doi: 10.1038/sj.bdj.4803864. [DOI] [PubMed] [Google Scholar]
- 47.Hondrum SO. Storage stability of dental luting agents. J Prosthet Dent. 1999;81:464–468. doi: 10.1016/S0022-3913(99)80015-8. [DOI] [PubMed] [Google Scholar]
- 48.Earl MS, Ibbetson RJ. The clinical disintegration of glass ionomer cement. Br Dent J. 1986;161:287–291. doi: 10.1038/sj.bdj.4805953. [DOI] [PubMed] [Google Scholar]
- 49.Gemalmaz D, Yoruc B, Ozcan M, Alkumru HN. Effect of early water contact on solubility of glass ionomer luting cements. J Prosthet Dent. 1998;80:474–478. doi: 10.1016/S0022-3913(98)70014-9. [DOI] [PubMed] [Google Scholar]
- 50.Davidson CL, Zeghbroeck L, Feilzer AJ. Destructive stresses in adhesive luting cements. J Dent Res. 1991;70:880–882. doi: 10.1177/00220345910700050301. [DOI] [PubMed] [Google Scholar]
- 51.Torstenson B, Brännström M. Contraction gap under composite resin restorations: effect of hygroscopic expansion and thermal stress. Oper Dent. 1988;13:24–31. [PubMed] [Google Scholar]
- 52.Feilzer AJ, Gee AJ, Davidson CL. Relaxation of polymerization contraction shear stress by hygroscopic expansion. J Dent Res. 1990;69:36–39. doi: 10.1177/00220345900690010501. [DOI] [PubMed] [Google Scholar]
- 53.Sorensen JA, Dixit NV, White SN, Avera SP. In vitro microleakage of dentin adhesives. Int J Prosthodont. 1991;4:213–218. [PubMed] [Google Scholar]
- 54.Bullard RH, Leinfelder KF, Russell CM. Effect of coefficient of thermal expansion on microleakage. J Am Dent Assoc. 1988;116:871–874. doi: 10.14219/jada.archive.1988.0291. [DOI] [PubMed] [Google Scholar]
- 55.Crim GA, Garcia-Godoy F. Microleakage: the effect of storage and cycling duration. J Prosthet dent. 1987;57:574–576. doi: 10.1016/0022-3913(87)90339-8. [DOI] [PubMed] [Google Scholar]
- 56.Meerbeek B, Lambrechts P, Inokoshi S, Braem M, Vanherle G. Factors affecting adhesion to mineralized tissue. Oper Dent. 1992;5:111–124. [PubMed] [Google Scholar]
- 57.White SN, Yu Z. Film thickness of new adhesive luting agents. J Prosthet Dent. 1992;67:782–785. doi: 10.1016/0022-3913(92)90582-U. [DOI] [PubMed] [Google Scholar]
- 58.Ishijima T, Caputo AA, Mito R. Adhesion of resin to casting alloys. J Prosthet Dent. 1992;67:445–449. doi: 10.1016/0022-3913(92)90070-Q. [DOI] [PubMed] [Google Scholar]
- 59.Breeding LC, Dixon DL. The effect of metal surface treatment on the shear bond strengths of base and noble metals bonded to enamel. J Prosthet Dent. 1996;76:390–393. doi: 10.1016/S0022-3913(96)90544-2. [DOI] [PubMed] [Google Scholar]
- 60.Imbery TA, Burgess JO, Naylor WP. Tensile strength of three resin cements following two alloy surface treatments. Int J Prosthodont. 1992;5:59–67. [PubMed] [Google Scholar]
- 61.Cotert HS, Ozturk B. Tensile bond of enamel-resin-metal joints. J Prosthet Dent. 1996;75:609–616. doi: 10.1016/S0022-3913(96)90245-0. [DOI] [PubMed] [Google Scholar]