Abstract
The primary objectives of successful prosthetic rehabilitation are to provide function, esthetics and comfort to the patient. Combination prosthesis is one which is supported by both natural teeth and implant. The periodontal ligament and osseointegrated interface distribute force differently to the supporting bone. Therefore problems can develop when tooth and implants are combined in the same prosthesis. However, clinicians can apply biomechanical principles, to negate the deleterious leverages exerted by the fixed prosthesis by using non rigid components and to equalize the stress applied by the prosthesis on implant and teeth. A case of partially edentulous situation was rehabilitated successfully with a combination of prostheses. Maxillary arch was restored to function with crowns, fixed dental prosthesis and with an extra coronal castable attachment prosthesis and the mandibular arch with a combination of tooth and implant supported attachment prosthesis. The clinical and laboratory steps for the fabrication of these prostheses are explained in this report.
Keywords: Implant, Attachment, Combination prosthesis, Implant overdenture
Introduction
Dental implants have been used increasingly in recent years as an adjunct for the rehabilitation of partially or completely edentulous patients. The superstructure fabricated over osseointegrated implants can be of two types: a removable overdenture or a fully anchored fixed prosthesis. Overdenture for implant supported prosthesis varies from a simple ball overdenture to a parallel milled bar attachment [1].
As an alternative to implant supported fixed prosthesis, an implant overdenture offers certain advantages. They are often clinically simpler and economically viable treatment option for the patient. An overdenture unlike a fixed prosthesis, replaces the missing teeth, along with the supporting structures. Moreover, overdenture enables the occlusal forces to be transmitted to the implant and alveolar bone, which provides a better stress distribution. By being removable, an overdenture affords easy access to the implant structures and better maintenance of oral hygiene [1–3].
Ideally, natural teeth should not be linked to implants due to difference in mobility [4]. In particular, it is not advisable for a tooth to be linked into a bridge that is supported by several implants [5, 6]. Overdentures can be designed to incorporate natural teeth along with implants by placing primary copings with or without attachments. The added implants in the edentulous site result in more retentive units in the restoration, and less stress to the supporting bone. As a result, complications are minimized and implant and prosthesis longevity are increased at a reduced treatment cost.
Case Report
A 52 year old female reported for correction of proclination and spacing of upper and lower anterior teeth. On examination, there was generalized gingival recession and spacing. However, the periodontal condition of maxillary teeth was good except for 16, 22, and 26–28. 22 was distally migrated and 26 and 27 were supraerupted. There was grade 1 mobility of teeth 16, 22, and 26–28. 13 was labially placed outside the arch. The mandibular arch had poor periodontal status except for teeth 43–45 which had acceptable periodontal support. Patient’s medical history was non contributory (Figs. 1, 2). She was having proclination of teeth since childhood; however spacing has increased in recent years. She had been undergoing regular oral prophylactic measures, annually.
Fig. 1.

Pre-operative photograph shows proclination and spacing of upper and lower anteriors
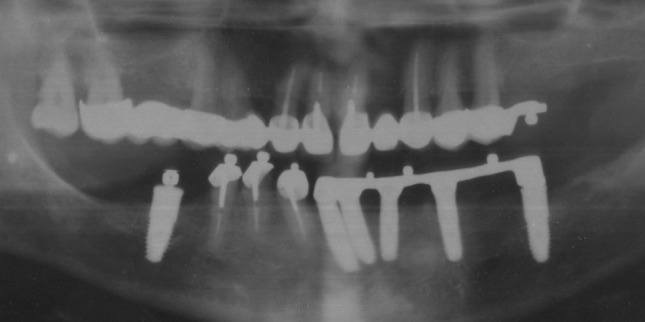
Fig. 2.

Pre-operative panoramic radiograph shows poor bone support of 16, 22, 26–28, 31–35, 38, 41, 42, 47, and 48
The case was diagnosed as pathologic migration due to periodontal disease. As there was no periodontal pocket or active periodontal disease, periodontal treatment was not indicated.
Patient was informed about the need for extraction and replacement of some of the teeth. Various treatment options like implant supported removable, and implant supported fixed prosthesis were explained to the patient and the advantages and disadvantages were discussed. Patient opted for a removable prosthesis.
For the maxillary arch, extraction of 16, 13, 22, and 26–28, followed by esthetic correction of remaining teeth with crowns and fixed dental prosthesis along with the replacement of 26 and 27, with an attachment supported partial removable dental prosthesis was planned. In the mandibular arch, extraction of mobile teeth and fabrication of a tooth and implant supported combined over denture was planned. Considering the clinical findings six implants were planned to be placed.
31, 32, 34, 35, 38, 41, 42, 47, and 48 were extracted, followed by immediate placement of implant fixtures (UniTi, Equinox, Holland) in 32, 35, 37, 41, 42, and 46 regions. 33 was retained temporarily for the placement of provisional crowns. Endodontic treatment was initiated for 12, 11, 21, 23, and 43–45, 2 weeks after implant placement.
Maxillary teeth were prepared to receive porcelain fused to metal crowns and fixed partial dentures (Fig. 3). During the fabrication, at wax pattern stage, castable attachments (OT cap, Rhein 83 srl, Italy) were placed in a parallel manner on 16 and 25 with the help of a milling machine (S3 Junior, Schick, Germany) (Fig. 4). An attachment supported removable partial denture replacing 26, and 27 was fabricated (Figs. 5, 6, 7).
Fig. 3.

Photograph shows prepared maxillary teeth
Fig. 4.

Upper fixed prosthesis with the attachments on 16 and 25
Fig. 5.

Wax pattern of upper removable prosthesis on refractory cast
Fig. 6.

Upper removable prosthesis replacing 26 and 27
Fig. 7.

Intaglio surface of upper removable prosthesis
After 4 months, second stage surgery was performed for the mandibular implants and gingival formers were placed. Two weeks later, 43–45. were sectioned 1 mm above the gingiva and root canals were prepared to a depth of 5–8-mm with a Mooser bur (Rhein 83 srl, Italy). The external surface was prepared to receive over denture copings (Fig. 8). Gingival formers were replaced with impression posts. Polyether impression material was injected in and around the root canal with the help of a syringe. Plastic pivots (Rhein 83 srl, Italy) (Fig. 9), coated with tray adhesive were inserted into the root canals and a full mouth impression, was made with polyether impression material (Impregum, 3M ESPE), with an acrylic custom made tray using closed tray impression technique. After placement of implant analogue, impression was poured with type IV gypsum and cast was prepared.
Fig. 8.

Tooth preparation of 43–45
Fig. 9.
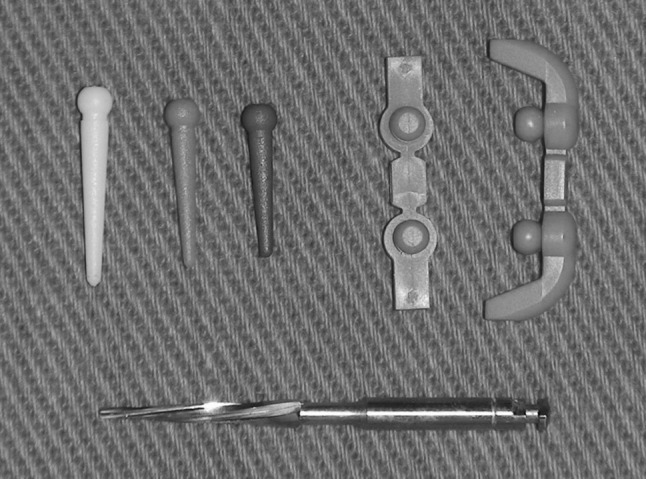
Photograph shows plastic pivots, mooser bur, castable attachments, Rhein 83 srl, Italy
On the cast, impression posts were replaced with abutments. After securing the cast on the milling table, of the milling machine (S3 Junior, Schick, Germany), an appropriate path of insertion was selected and the milling table was locked in that position. The height of the abutments was reduced with a diamond disc attached to the milling unit, to bring it to the same level. Then the disc was replaced with a milling bur and the abutments were milled to get 3° taper. Abutment screw holes were blocked with block-out wax and two coats of die spacers were applied on the abutments.
Individual wax copings were fabricated over the abutments and prepared natural teeth. Wax copings on implant abutments were joined with milling wax to form a bar which was milled to 6° taper with a wax milling bur. Castable ball attachments (rhein 83 srl, Italy) were placed in a parallel manner on the bar and on the copings made on the natural teeth, with the help of the milling machine (Figs. 10, 11). Normal sized (Rhein83 srl.) attachments were placed on 36, 34, 44, 45 regions and micro sized (Rhein83 srl.) on 31 and 43 region.
Fig. 10.

castable attachment and paralleling mandrel
Fig. 11.

positioning of castable attachments with milling machine
The milled bar and copings were cast in Chrome–Cobalt alloy (Wironium plus, Bego, Germany) and positioned back on the milling table and the bar was milled with 6° metal milling bur. Bar and copings were polished to a high gloss (Fig. 12). An individual ball attachment (UniTi, Equinox), was placed on 46. After verifying the fit intra-orally (Fig. 13), a pickup impression was made with additional silicone using putty-wash single impression technique using stock tray and a cast was poured in type IV gypsum.
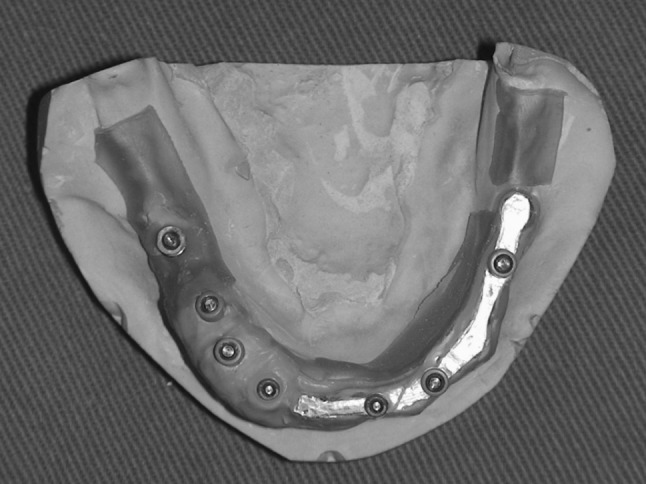
Fig. 12.

Bar and copings with attachments
Fig. 13.

Mandibular primary copings with attachments
A secondary framework was fabricated with castable housings and connectors (Rhein83 srl, Italy) (Fig. 14). After blocking the undercuts on the master cast, positional rings were placed on the ball attachments (Fig. 15). Castable housings were secured over the positional rings and joined to plastic connectors with the help of a pattern resin (GC, Japan) (Fig. 16). Pattern was removed, invested and cast in Chrome–cobalt alloy. Fit of the secondary framework was tried on the cast and a record base was fabricated in auto polymerizing acrylic resin over the framework. Bite registration was recorded and denture was fabricated with group function occlusion following try-in (Fig. 17). At the time of denture insertion, yellow nylon retention caps(medium) were placed in the housing corresponding to the ball head over the natural teeth and green nylon caps (soft) were placed in the housing corresponding to the ball heads over the implants to equalize the resiliency of the tooth and implant (Figs. 18, 19, 20, 21).
Fig. 14.
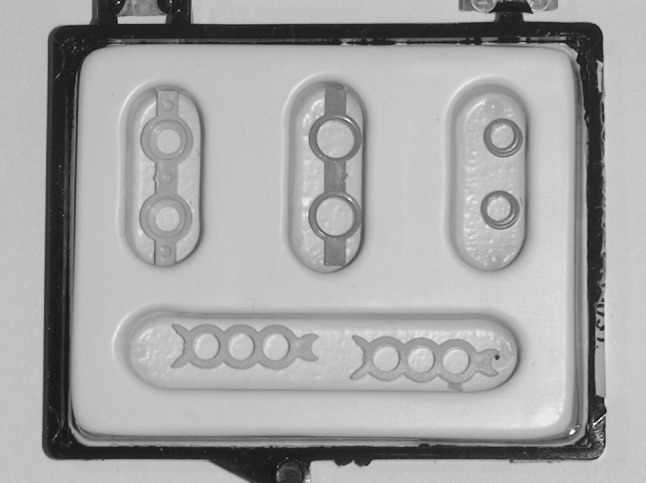
Castable housing, positional rings, and connectors
Fig. 15.
Positional rings were placed on ball attachments
Fig. 16.
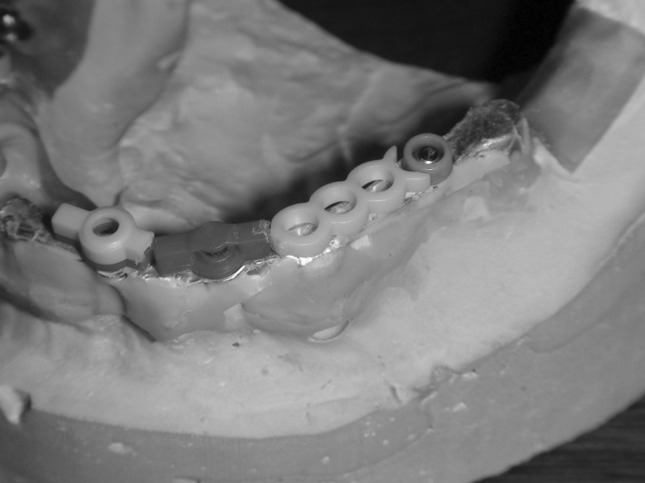
Castable housing and connectors ready to join
Fig. 17.

Secondary frame incorporated in mandibular prosthesis
Fig. 18.

Mandibular prosthesis
Fig. 19.

Nylon caps placed in the denture
Fig. 20.

Immediate post-operative photograph
Fig. 21.
Post-operative radiograph
Patient was given oral hygiene instructions and asked to report after 1 week. Recall visits were done after 1, 2 months, followed by every 6 months. During each subsequent visit, retention of the prosthesis, oral hygiene maintenance and periodontal health were checked. Patient was happy with the function, esthetics and comfort provided by the treatment. Retention caps were replaced over a period of time and the case was followed up to 4 years (Figs. 22, 23).
Fig. 22.

Post-operative photograph after 4 years
Fig. 23.
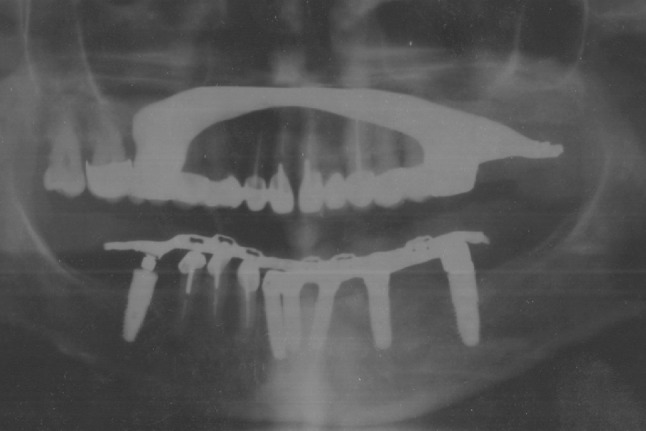
Post-operative radiograph after 4 years
Discussion
Tooth supported or implant supported overdentures are common treatment options for rehabilitation of edentulous situations. In a potentially edentulous situation, the distribution of the remaining natural teeth at times may not provide a favourable stress distribution for an overdenture. In such situations, the placement of implants in certain areas, not only provide better stability and support, but also will improve the prognosis and prevent ridge resorption.
Advantages of overdentures over fixed prosthesis are lower cost, high esthetics, improved access for oral hygiene, and better distribution of occlusal forces. The implants or tooth will not be overloaded as some of the occlusal load will be transmitted to the residual alveolar ridge. Splinting of the implants was done as splinted implants exhibit better load sharing than non-splinted implants [7]. Moreover, the leverage on implant will be reduced as the rotational axis is shifted closer to the implant fixture contrary to fixed prosthesis, where leverage starts from the occlusal contact point.
The character of force distributed to bone by tooth and implant is different. The periodontal ligament of a tooth distributes the forces to all the surrounding bone [8, 9], whereas the osseointegrated interface concentrates the force at the crestal bone [10, 11]. A combined prosthesis is one which is supported by both the natural tooth and implant. The method of attachments between the segments can be flexible (overdenture) or stiff (fixed prosthesis). When a lateral force is applied to the implant side of the combined rigid prosthesis, no force is distributed to the opposite side. When lateral force is applied to the tooth side of the rigid prosthesis, the force is not distributed to the tooth side, but rather is concentrated at the implant side as destructive long lever arm [12].
In a combined overdenture, where there is a flexible connection between the overdenture and primary structures, the force applied to the tooth side will not be transmitted to the implant side in a deleterious manner as there is a stress breakage at the attachment level. For this, overdentures should be designed in such a way that prosthesis should be able to rotate at attachment level without torquing on the primary bar. A parallel milling with close fit in such cases can transmit these deleterious forces to the implants, hence should be avoided. In addition to this, the stress equalization between the natural tooth and implant can be done by placement of nylon caps with different degrees of resiliencies. As there is stress breaking between the final prosthesis and both implant and tooth and the implants being splinted together, there will be even stress distribution among them.
Conclusion
A combined prosthesis is one which is supported by both natural teeth and implants. The periodontal ligament and osseointegrated interface distribute force differently to the supporting bone. Therefore problems develop when teeth and implants are combined in the same prosthesis. The biomechanics of a removable prosthesis differ from a fixed prosthesis and clinicians can apply biomechanical principles to equalize loading on implant and tooth. A combined overdenture can successfully utilize both tooth and implant for its retention, support and stability without jeopardizing the life of the osseointegrated implant or tooth, at a lower cost.
References
- 1.Inan O, Aykent F, Alptekin N. Implant supported overdenture therapy: a 3- to 8-year prospective study. Implant Dent. 2000;9(369):373. doi: 10.1097/00008505-200009040-00015. [DOI] [PubMed] [Google Scholar]
- 2.Hobo S, Ichida E, Gacia LT. Osseointegration and occlusal rehabilitation. Tokyo: Quintessence Publishing; 1990. pp. 187–208. [Google Scholar]
- 3.Watson CJ, Ogden AR, Tinsley D, et al. A 3-to 6- year study of over dentures supported by hydroxyapatite coated endosseous dental implants. Int J Prosthodont. 1998;11:610–619. [PubMed] [Google Scholar]
- 4.Davies SJ, Gray RJ, Young MPJ. Good occlusal practice in the provision of implant borne prostheses. Br Dental J. 2002;192:79–88. doi: 10.1038/sj.bdj.4801298. [DOI] [PubMed] [Google Scholar]
- 5.Palmer RM, Howe LC, et al. Implant dentistry—prosthodontics: a prospective 3-year study of fixed bridges linking Astra Tech ST implants to natural teeth. Clin Oral Implants Res. 2005;16:302–307. doi: 10.1111/j.1600-0501.2005.01110.x. [DOI] [PubMed] [Google Scholar]
- 6.Charkawi Hussein G, Zekry Khaled A, Mohammed T. El wakad stress analysis of different osseointegrated implants supporting a distal extension prosthesis . J Prosthet Dent. 1994;72:614–622. doi: 10.1016/0022-3913(94)90294-1. [DOI] [PubMed] [Google Scholar]
- 7.Guichet DL, Yoshinobu D. Caputo AA effect of splinting and interproximal contact tightness on load transfer by implant restorations. J Prosthet Dent. 2002;87:528–535. doi: 10.1067/mpr.2002.124589. [DOI] [PubMed] [Google Scholar]
- 8.Weinberg LA, Kruger B. Biomechanical considerations when combining tooth-supported and imlant-supported prosthesis. Oral Surg Oral Med Oral Pathol. 1994;78:22–27. doi: 10.1016/0030-4220(94)90112-0. [DOI] [PubMed] [Google Scholar]
- 9.Weinberg LA. Biomechanics of force distribution in implant-supported prosthesis. Int J Oral Maxillofac Implants. 1993;8:19–31. [PubMed] [Google Scholar]
- 10.Reiger MR, Mayberry M, Brose MO. Finite element analysis of a six endosseous implants. J Prosthet Dent. 1990;63:671–676. doi: 10.1016/0022-3913(90)90325-7. [DOI] [PubMed] [Google Scholar]
- 11.Clelland NL, Ismail YH, Zaki HS, Pipko D. Three-dimensional finite element stress analysis in and around the screw and implant. Int J Oral Maxillifac Implants. 1991;6:391–398. [PubMed] [Google Scholar]
- 12.Weinberg LA (2003) Atlas of tooth- and implant-supported prosthodontics. Quintessence Publishing Company, pp 51–52


