Abstract
Background
The burden of H1N1 among socially disadvantaged populations is unclear. We aimed to synthesize hospitalization, severe illness, and mortality data associated with pandemic A/H1N1/2009 among socially disadvantaged populations.
Methods/Principal Findings
Studies were identified through searching MEDLINE, EMBASE, scanning reference lists, and contacting experts. Studies reporting hospitalization, severe illness, and mortality attributable to laboratory-confirmed 2009 H1N1 pandemic among socially disadvantaged populations (e.g., ethnic minorities, low-income or lower-middle-income economy countries [LIC/LMIC]) were included. Two independent reviewers conducted screening, data abstraction, and quality appraisal (Newcastle Ottawa Scale). Random effects meta-analysis was conducted using SAS and Review Manager.
Conclusions/Significance
Sixty-two studies including 44,777 patients were included after screening 787 citations and 164 full-text articles. The prevalence of hospitalization for H1N1 ranged from 17–87% in high-income economy countries (HIC) and 11–45% in LIC/LMIC. Of those hospitalized, the prevalence of intensive care unit (ICU) admission and mortality was 6–76% and 1–25% in HIC; and 30% and 8–15%, in LIC/LMIC, respectively. There were significantly more hospitalizations among ethnic minorities versus non-ethnic minorities in two studies conducted in North America (1,313 patients, OR 2.26 [95% CI: 1.53–3.32]). There were no differences in ICU admissions (n = 8 studies, 15,352 patients, OR 0.84 [0.69–1.02]) or deaths (n = 6 studies, 14,757 patients, OR 0.85 [95% CI: 0.73–1.01]) among hospitalized patients in HIC. Sub-group analysis indicated that the meta-analysis results were not likely affected by confounding. Overall, the prevalence of hospitalization, severe illness, and mortality due to H1N1 was high for ethnic minorities in HIC and individuals from LIC/LMIC. However, our results suggest that there were little differences in the proportion of hospitalization, severe illness, and mortality between ethnic minorities and non-ethnic minorities living in HIC.
Introduction
In 2009, a novel H1N1 influenza virus strain circulated, which gave rise to the 2009 H1N1 pandemic (influenza A/Mexico/2009 (H1N1)). The H1N1 pandemic was associated with a high burden of illness in terms of hospitalizations, severe illness, absenteeism, and cost. For example, in the United States (US), over 43,677 laboratory-confirmed cases of pandemic H1N1 2009 were reported [1]. Using a mathematical model, it was estimated that between 1.8 million to 5.7 million cases occurred, including 9,000 to 21,000 hospitalizations in the US [1]. In Spain, the average work absenteeism due to the 2009 H1N1 pandemic ranged from 9 to 30.5 days [2]. The economic burden for those with confirmed influenza was estimated as €144,773,577 in Spain (95% confidence interval, CI: 13,753,043-383,467,535). In Italy, the estimated economic burden due to laboratory-confirmed H1N1 2009 pandemic ranged from €1.3 to €2.3 billion [3]. In Australia, the economic burden of treating H1N1-admitted patients to the intensive care unit (ICU) was over AU $65,000,000 [4]. These estimates indicate that a significant burden of illness was observed due to the 2009 H1N1 pandemic.
Previous reviews of the 2009 H1N1 pandemic reported that the majority of cases occurred among young to middle-aged adults often in those without comorbidity, followed by children and adolescents [5], [6]. Individuals with a greater burden of illness included the elderly, obese individuals, pregnant women, or those with comorbidity [5], [6]. In addition, it has been hypothesized that greater burden of illness was associated with poverty and individuals without access or disproportionate access to healthcare [7]. To examine this further, we aimed to synthesize hospitalization, severe illness, and mortality data associated with pandemic A/H1N1/2009 among socially disadvantaged populations, including low socioeconomic status, ethnic minorities, groups without access or disproportionate access to healthcare, and low-income economy countries or lower-middle-income economy countries [LIC/LMIC].
Methods
A systematic review protocol was used to guide the methods of our review, based on the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) Statement [8]. Our research question was: “what is the evidence that the burden of H1N1 was associated with social disadvantage?” At the time of study conduct, a similar systematic review protocol focusing on H1N1 burden among the socially disadvantaged did not exist.
Search
An experienced librarian (Perrier) developed the search strategy using medical subject headings (MeSH) and text words. The MEDLINE (OVID interface, 2009 to July 25, 2011) and EMBASE (OVID interface, 2009 to July 25, 2011) electronic databases were searched to identify potentially relevant material. The full search strategy for MEDLINE is presented in Appendix S1, which was modified for EMBASE (available upon request). Targeted searching for low-income and lower-middle-income economies was also conducted in PubMed using the terms “H1N1” and “country of interest”. The Eurosurveillance Journal and the Centers for Disease Control and Prevention (CDC) Morbidity and Mortality Weekly Report were hand-searched from January 2009 until August 1, 2011. The reference lists of included studies or relevant reviews [5], [6], [9] were scanned and a list of included studies was circulated to members of the World Health Organization (WHO) Influenza Programme to ensure all potentially relevant studies were identified.
Study Selection and Characteristics
Studies reporting the burden (prevalence of hospitalization, severe illness, and mortality) of influenza A/Mexico/2009 (H1N1) among socially disadvantaged populations (e.g., ethnic minorities, low socioeconomic status, groups without access or disproportionate access to healthcare, LIC/LMIC) were included. It was determined a priori in discussion with the World Health Organization (organization that commissioned this systematic review) that burden would include hospitalization, severe illness, and mortality. H1N1 had to be laboratory-confirmed through polymerase chain reaction, viral culture, or antibody assay [10], as each laboratory test has various advantages and limitations [11]. For example, antibody assay can detect infections missed by other laboratory methods but the diagnosis of influenza is retrospective and it takes weeks to retrieve the results [11]. According to the Center for Disease Control and Prevention (CDC), the preferred method of pandemic H1N1 2009 influenza ascertainment was polymerase chain reaction and viral culture [12]. Rapid influenza diagnostic tests were not recommended by the CDC (and hence, were excluded from this systematic review), as their sensitivity is low [10].
Ethnic minorities were classified as non-predominant races (e.g., non-Caucasians in predominant Caucasian continents, such as Europe and North America), as well as indigenous populations (i.e., first settlers in a particular territory [9]). LIC (gross national income ≤$1,005) and LMIC (gross national income $1,006–$3,975) were categorized according to the World Bank’s classification of countries [13]. We planned to classify low socioeconomic status as high-school education or less or below the particular country’s poverty line, but we did not identify articles relevant to this type of social disadvantage [14]. Inclusion was not limited by study design, publication status or language. Authors of conference proceedings were contacted to obtain the conference presentation or unpublished work. Two reviewers independently screened the titles and abstracts from the literature search and potentially relevant full-text articles for inclusion using the standardized eligibility criteria. Conflicts were resolved by discussion amongst the team.
Data Abstraction
A draft data abstraction form was developed, pilot-tested, and modified as necessary. Two reviewers abstracted all of the data independently. Conflicts were resolved by discussion amongst the review team. The following data were abstracted: study characteristics (e.g., study design, country of conduct, time period), patient characteristics (e.g., mean age, percent gender, type of social disadvantage examined) and outcomes (number of hospitalizations, severe illness, deaths). Authors were contacted for further information when the data were not clearly reported. In some instances, multiple studies reported H1N1 data from the same source (i.e., companion reports). When this occurred, the report with the most outcomes of interest or largest sample size was included and the other(s) was used for supplementary material only.
Validity Assessment
All relevant studies were assessed for risk of bias using the Newcastle Ottawa Scale (NOS) [15]. The NOS evaluates nonrandomized studies such as case-control and cohort studies and consists of 3 domains: selection, comparability, and exposure. A full explanation of the NOS can be found in Appendix S2.
Quantitative Data Synthesis
Random effects meta-analysis [16] was conducted to determine the prevalence of hospitalization, ICU admission, and mortality that occurred in high-income economy countries (HIC) and LIC/LMIC, separately, as well as for the proportion of ethnic minorities and non-ethnic minorities experiencing these outcomes in HIC. Confounding was examined through meta-analyses of the proportion of patients with comorbidity, pregnancy, and obesity for ethnic minorities versus non-ethnic minorities in HIC. Statistical heterogeneity was examined using the I2 and χ2 statistics [17]. Analyses were conducted in Review Manager Version 5 [18] and SAS (SAS 9.1 software, SAS Institute Inc., Cary, NC, USA).
Results
Flow of Included Studies
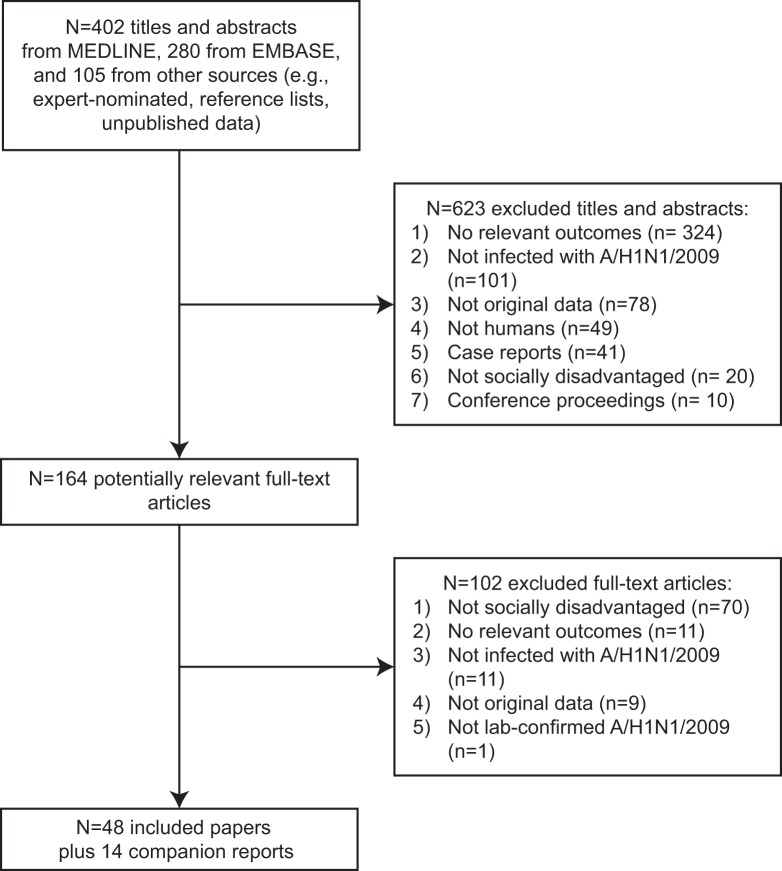
The literature search identified 787 titles and abstracts; 164 were potentially relevant (Figure 1, Flowchart S1, Checklist S1). From these, 62 articles fulfilled the eligibility criteria [19]–[80]. Of these, fourteen articles were companion reports and only supplementary data were obtained from them [23], [27], [31], [34], [36], [50], [54], [55], [57], [71], [75]–[78]. All of the studies were written in English and unpublished data were obtained for two studies identified by contacting authors of excluded studies [33], [35].
Figure 1. Study flow.
This is the flow of citations and articles that were screened for the systematic review.
Study Characteristics
The majority of the included studies were conducted in HIC, including the United States [20], [21], [24], [28]–[30], [32], [35], [37]–[40], [42], [45], [46], [48], [62], Australia or New Zealand [22], [43], [44], [49], [51], [53], [56], [59], [63], Canada [19], [25], [26], [33], [47], and the United Kingdom [41], [52], [58] (Table 1). Twelve studies were conducted in LIC/LMIC, including Guatemala [64], Morocco [65], [66], Pakistan [80], and India [67]–[78]. All of the included studies were cohort studies.
Table 1. Study characteristics.
| First author, Year | Time period | Region of conduct | Data source(s) | Number of lab-confirmed H1N1 [confirmation type] | Outcome(s) examined |
| ETHNIC MINORITIES | |||||
| Oluyomi-Obi 2010 [19] | March 1–August 31 2009 | Manitoba, Canada | St. Boniface Hospital & Health Sciences Centre ICU | 889 [PCR] | ICU admission |
| CDC Sept 2009 [20] | April-August 8 2009 | US | CDC influenza-associated pediatric mortality reporting system | 36 pediatric deaths [RT-PCR] | Mortality |
| Martin 2010 [21] | April 1–October 31 2009 | North Carolina, US | Duke University Medical Center | 123 hospitalizations [RT-PCR, viral culture] | Hospitalization |
| Paine 2010 [22]*(1) | April 1–November 1 2009 | New Zealand | EpiSurv | 3067 [PCR, viral culture, antibody assay] | Mortality |
| Baker 2009 [23] (1) | April 25–August 23 2009 | New Zealand | Surveillance data from notifiable disease, general practices, laboratories, Healthline, Ministry of Health ICU, population survey (Flutracker) | 3109 [PCR, viral culture, antibody assay] | Hospitalization |
| Wenger 2011 [24] | April 1– December 31 2009 | Alaska, US | Alaska ILI Surveillance Network, Medicaid, Indian Health Service Influenza Awareness System | 103 hospitalizations [PCR, viral culture] | Hospitalization, mortality |
| Zarychanski 2010 [25] | April 2–September 5 2009 | Manitoba, Canada | Manitoba Health and University of Manitoba Critical Care | 894 (location known for 795) [RT-PCR] | Hospitalization, ICU admission |
| Helferty 2010 [26]*(2) | April 12 2009– April 3 2010 | Canada | PHAC | 8678 hospitalizations [RT-PCR, viral culture, antibody assay] | Hospitalization, ICU admission, mortality |
| Campbell 2010 [27] (2) | April 26–September 26 2009 | Canada | PHAC | 1479 hospitalizations [RT-PCR, viral culture, antibody assay] | Hospitalization, ICU admission, mortality |
| Siston 2010 [28] | April 14 -August 21 2009 | US | CDC (Pregnancy Flu Line) | 788 pregnant women [rRT-PCR, antibody assay, rapid test, viral culture] | Hospitalization, ICU admission, mortality |
| CDC Dec 2009 [29] | April 15–November 13 2009 | US | Multidisciplinary workgroup from 12 state health departments | NR [rapid test, antibody assay, rRT-PCR, viral culture] | Mortality |
| Chitnis 2010 [30]*(3) | April 23–August 15 2009 | Wisconsin, US | Wisconsin Division of Public Health | 252 hospitalizations [rRT-PCR] | Hospitalization, ICU admission, mortality |
| Truelove 2011 [31] (3) | April 15 2009–January 2 2010 | Wisconsin, US | Wisconsin Division of Public Health | 1266 [rRT-PCR] | Hospitalization, mortality |
| Dee 2011 [32] | April 15 2009–January 26 2010 hospitalization (pediatric deaths: April 15 2009– March 23 2010) | US | Emerging Infections Program (CDC, 10 state and local health departments, academic institutions, medical providers), CDC Influenza-Associated Pediatric Mortality Surveillance System | 5793 hospitalizations [rapid test, RT-PCR, viral culture, documented in medical chart] | Hospitalization, mortality |
| Jung 2011 [33] *(4) unpublished data | April 16 2009–April 12 2010 | Canada | Canadian Critical Care Trials Group | 565 critically ill [rRT-PCR, viral culture] | ICU admission |
| Jouvet 2010 [34] (4) | April 16–August 15 2009 | Canada | Canadian Critical Care Trials Group | 49 pediatric ICU admissions [PCR, viral culture] | Pediatric ICU admission |
| Louie 2011 [35]*(5) unpublished data | April 1 2009–August 13 2010 | California, US | California Department of Public Health | 2476 hospitalizations [rRT-PCR] | Hospitalization, ICU admission, mortality |
| CDC May 2009 [36] (5) | April 20–May 17 2009 | California, US | California Department of Public Health | 333 hospitalizations [rRT-PCR] | Hospitalization |
| Lee 2010 [37] | April 24–July 1 2009 | New York City, US | New York City Department of Health and Mental Hygiene, New York City Office of Vital Statistics (death certificates) | 47 deaths [rRT-PCR] | Mortality |
| CDC Aug 2009 [38] | April 24–July 25 2009 | Illinois, US | Chicago Department of Public Health | 1557 [rRT-PCR] | Hospitalization |
| CDC Jan 2010 [39] | April 25–May 24 2009 | New York City, US | New York City Department of Health and Mental Hygiene (all hospitals) | 99 hospitalizations [PCR] | Hospitalization |
| Kwan-Gett 2009 [40] | April 25–August 7 2009 | Washington, US | Public Health–Seattle & King County | 565 [viral culture, PCR] | Mortality |
| Nguyen-Van-Tam 2010 [41] | April 27–Sept 30 2009 | UK | The Influenza Clinical Information Network (FluCAN) | 631 hospitalizations [rRT-PCR] | Hospitalization |
| Kumar 2010 [42] | April 28–August 31 2009 | Wisconsin, US | Children’s Hospital of Wisconsin | 81 hospitalizations [rRT-PCR] | Hospitalization, mortality |
| Harris 2010 [43] | April-August 2009 | Queensland, Australia | Townsville Hospital | 360 [rPCR] | Hospitalization, ICU admission, mortality |
| Kelly 2009 [44] | May-October 2009 | Australia | Australian Department of Health and Ageing | NR [lab-confirmed] | Hospitalization, ICU admission, mortality |
| Jain 2009 [45] | May 1–June 9 2009 | US | State health departments reports to the CDC | 272 hospitalizations [rRT-PCR] | Hospitalization |
| Creanga 2010 [46] | May 1–June 30 2009 | New York, US | New York City Department of Health and Mental Hygiene | 136 hospitalizations [rRT-PCR] | Hospitalization |
| Bettinger 2010 [47] | May 1–August 31 2009 | Canada | The Canadian Immunization Monitoring Program, Active (IMPACT) surveillance data | 324 hospitalizations [PCR, antibody assay, viral culture] | Hospitalization |
| Miller 2010 [48] | May 19–June 30 2009 | Utah, US | Four ICUs at three academic hospitals in Salt Lake County | 47 ICU admissions [PCR] | ICU admission |
| Flint 2010 [49]*(6) | June 1–August 31 2009 | Northern Territory, Australia | Northern Territory CDC, Royal Darwin Hospital | 161 acute care [PCR] | Hospitalization, ICU admission |
| Flint 2009 [50] (6) | May 29– June 18 2009 | Northern Territory, Australia | Northern Territory CDC, Royal Darwin Hospital | 81 [PCR] | Hospitalization |
| Cretikos 2009 [51] | May 15– September 4 2009 | New South Wales, Australia | NetEpi, laboratory notifications, hospital emergency department and ambulance dispatch surveillance system, death certificate surveillance | 5106 [PCR] | Hospitalization, ICU admission, mortality |
| Scriven 2009 [52] | June 1–July 21 2009 | Birmingham, UK | Heartlands Hospital | 3000 [PCR] | Hospitalization, severe illness |
| Webb 2009 [53]*(7) | June 1–August 31 2009 | New Zealand, Australia | Australian and New Zealand Intensive Care Research Centre | 722 ICU admissions [PCR, serology] | ICU admission |
| Knight 2010 [54] (7) | June 1–August 31 2009 | Australia, New Zealand | Australian and New Zealand Intensive Care Research Centre, Australasian Maternity Outcomes Surveillance System | 59 ICU pregnancy admissions [confirmed H1N1] | ICU admission |
| ANZIC Investigators 2010 [55] (7) | June 1–August 31 2009 | New Zealand, Australia | Australian and New Zealand Intensive Care Research Centre, Australasian Maternity Outcomes Surveillance System | 64 ICU pregnancy/postpartum admissions [PCR] | ICU admission |
| Verrall 2010 [56] *(8) | June 8–August 31 2009 | Wellington, New Zealand | Wellington Hospital and Hutt Valley Hospitals | 229 hospitalizations [rRT-PCR] | Hospitalization |
| Dee 2010 [57] (8) | June 17–July 20 2009 | Wellington, New Zealand | Hutt Valley Hospital | 54 hospitalizations [RT-PCR] | Hospitalization |
| Sachedina 2010 [58] | June 26 2009– March 22 2010 | England, UK | Department of Health, Regional Directors of Public Health, Health Protection Agency’s influenza reference centers | 70 deaths [lab-confirmed or H1N1 on death certificate] | Mortality |
| Kelly 2011 [59] | July 1–December 4 2009 | Australia | Influenza Complications Alert Network (FluCAN) sentinel hospitals | 465 hospitalizations [rRT-PCR] | Hospitalization, ICU admission |
| Chien 2010 [60] | July 2–August 29 2009 | Taiwan, Republic of China | Taiwan CDC | 149 severe illness[RT-PCR] | Pneumonia, respiratory failure |
| Subramony 2010 [61] | July 15–September 28 2009 | Singapore | Singapore General Hospital, Tan Tock Seng Hospital, Alexandra Hospital, National University Hospital, KK Women’s and Children’s Hospital and Changi General Hospital, Mount Elizabeth Hospital, Gleneagles Hospital, Mount Alvernia Hospital, East Shore Hospital, Thompson Medical Centre and Raffles Hospital | 1348 hospitalizations [RT-PCR] | Hospitalization, severe illness |
| Satterwhite 2010 [62] | August 1–October 31 2009 | Atlanta, Georgia, US | Emory University Hospital, Grady Memorial Hospital, Emory University Hospital Midtown/Crawford Long Hospital, Atlanta Veterans Affairs Medical Center | 109 hospitalizations [PCR] | Hospitalization, ICU admission |
| Bandaranayake 2011 [63] | January 1–Oct 24 2010 | New Zealand | Institute of Environmental Science and Research, Healthstat, Healthline, Episurv, National Minimum Data Set, Pandemic Influenza Mortality Review Committee | 1758 [nasopharyngeal swabs] | Hospitalization |
| LOW-INCOME ECONOMIES OR LOWER-MIDDLE-INCOME ECONOMIES | |||||
| Reyes 2010 [64] | May-December 2009 | Guatemala | National Hospital of Cuilapa, Western Regional Hospital, Health Center of Nueva Santa Rosa | 239 [rRT-PCR] | Hospitalization, ICU admission, pneumonia, mechanical ventilation, mortality |
| Louriz 2010 [65] | June-December 2009 | Rabat, Morocco | Ibn Sina University Hospital | 186 hospitalizations [RT-PCR] | Hospitalization, ICU admission, mechanical ventilation, mortality |
| Lahlou 2011 [66] | June 12–December 24 2009 | Rabat, Morocco | Mohammed V Military Teaching Hospital | 240 [rRT-PCR] | Hospitalization, severe illness, mortality |
| Jagannatha Rao 2011 [67] | August 2009–April 2010 | Karnataka, India | Tertiary care hospital | 20 hospitalizations [rRT-PCR] | Hospitalization, severe illness, mortality |
| Chacko 2010 [68] | August-October 2009 | Karnataka, India | Manipal Hospital multidisciplinary ICU | 66 hospitalizations [RT-PCR] | Hospitalization, ICU admission, mortality |
| Parakh 2010 [69] | August 2009–January 2010 | New Delhi, India | Kalawati Saran Children’s Hospital | 25 pediatric hospitalizations [PCR] | Hospitalization, ICU admission, severe illness, mortality |
| Ramakrishna 2011 [70]*(9) | August 2009–October 2010 | Tamil Nadu, India | Christian Medical College Hospital | 629 hospitalizations [rRT-PCR] | Hospitalization, ICU admission, severe illness mortality |
| Pramanick 2011 [71] (9) | August 5 2009–January 2010 | Tamil Nadu, India | Christian Medical College Hospital | 164 [rRT-PCR] | Hospitalization, ICU admission, mortality |
| Puvanalingam 2011 [72] | August 9 2009–January 2010 | Tamil Nadu, India | Madras Medical College and Government General Hospital records, Institute of Child Health, Egmore | 442 [RT-PCR] | Hospitalization, pneumonia, mortality |
| Sharma 2010 [73] | September 2009 to January 2010 | Delhi, India | GTB Hospital | 125 hospitalizations [RT-PCR] | Hospitalization, severe illness, mortality |
| Chudasama 2011 [74]* (10) | September 1, 2009–February 20, 2010 | Gujarat, India | Hospitals in Rajkot city of Saurashtra region | 274 hospitalizations [rRT-PCR] | Hospitalization, mortality |
| Chudasama 2010 [75] (10) | September 1, 2009–February 28, 2010 | Rajkot, India | Hospital records, Pediatric Department of Civil Hospital & two other pediatric hospitals of Rajkot city | 62 pediatric cases [rRT-PCR] | Hospitalization, mortality |
| Chudasama 2010 [76] (10) | September 1, 2009–February 20, 2010 | Rajkot, India | Hospitals in Rajkot city of Saurashtra region | 274 hospitalizations [rRT-PCR] | Hospitalization, mortality |
| Chudasama 2010 [77] (10) | September 1, 2009–February 20, 2010 | Rajkot, India | Hospitals in Rajkot city of Saurashtra region | 274 hospitalizations [rRT-PCR] | Hospitalization, mortality |
| Chudasama 2010 [78] (10) | September 1, 2009–January 31, 2010 | Rajkot, India | Hospitals in Rajkot city of Saurashtra region | 274 hospitalizations [rRT-PCR] | Hospitalization, mortality |
| Gupta 2011 [79] | November 2009–February 2010 | Rajasthan, India | Umaid Hospital for Women and Children | 62 pediatric hospitalizations [rPCR] | Hospitalization, ICU admission, mortality |
| Naseem 2011 [80] | December 1 2009–May 30 2010 | Rawalpindi, Pakistan | Department of Pulmonology and Critical Care, Military Hospital | 36 hospitalizations [RT-PCR] | Hospitalization, ICU admission, mechanical ventilation, mortality |
Notes: *major publication, () denotes companion reports.
Abbreviations: CDC Centers for Disease Control, ICU intensive care unit, ILI influenza-like illness, NR not reported, PCR polymerase chain reaction, rRT-PCR real-time reverse transcription-PCR, PH public health, PHAC Public Health Agency of Canada, SES socioeconomic status, UK United Kingdom.
Across the studies, the time period of examination ranged from March 1, 2009 to October 24, 2010. Most studies used PCR to confirm H1N1 infection (44/48); one study reported the use of nasopharyngeal swabs (type of lab-confirmation unspecified) [63], and two studies reported that H1N1 was lab-confirmed, without reporting the type of test used [44], [58]. The majority of studies examined ethnic minority status as the type of social disadvantage (36/48), except for 12 studies that examined H1N1 in LIC/LMIC [64]–[70], [72]–[74], [79], [80].
Patient Characteristics
Some studies examined differences in the number of hospitalizations, severe illness, and deaths between ethnic minorities and non-ethnic minorities, including Caucasian, European descent, and non-Indigenous populations, which were used as the reference group (Table 2). The number of H1N1-infected individuals ranged from 136 to 5,106 in the included studies (Tables 2 and 3). Few studies reported the percentage of female participants; in those that did report this, it ranged from 24% to 100% (Tables 2 and 3).
Table 2. Patient characteristics and outcomes for ethnic minorities.
| First author, year | Number of H1N1 patients | Number of H1N1 patients by social disadvantage‡ | % female | Median age (range) in years | Number with medical conditions by social disadvantage | Number of hospitalizations | Number of severe illness/ICU | Number of deaths |
| Oluyomi-Obi 2010 [19] | 889 | Reports ICU admission by ethnicity | 100 | Mean 22.6 (16–29) | Pregnant: 5 I, 1 NI | NR | ICU 5 I, 1 NI | NR |
| CDC Sept 2009 [20] | NR | Reports mortality by ethnicity | 50 | 9 (2 months-17) | Obese:2 B Comorbidity: 1 B, 8 H, 2 A, 13 C [CLD, RAD, CP, seizure, ALL, MD, bronchospasm, htn, DS, pneumonia hx, autism] | NR | NR | 6 B, 12 H, 3 A, 15 C |
| Martin 2010 [21] | NR | Reports severe illness by ethnicity | NR | NR (23–51) | Pregnant: 2 B Comorbidity: 5 B, 1 C [asthma, htn, SLE, seizures, COPD, DM, CHD, CHF] | NR | Cardiac dysfunction: B 5, 1 C | NR |
| Paine 2010 [22]* Baker 2009 [23] | 3067 | Reports mortality by ethnicity | NR | All ages | NR | NR | NR | 7 I, 8 C, 2 O, 2 U |
| Wenger 2011 [24] | NR | Reports hospitalization by ethnicity | 49 | 17 (1 week-81) | Underlying disease: 23 I, 8 A/PI, 5 B, 24 C, 4 U | 39 I, 9 A/PI, 6 B, 42 C, 7 U | NR | 2 I, 4 C |
| Zarychanski 2010 [25] | 795 | 215 I, 373 NI | 52 | All ages 5.3(SD 18.8) | NR | 74 I, 62 NI | ICU 25 I, 17 NI | NR |
| Helferty 2010 [26]* Campbell 2010 [27] | NR | Reports hospitalization by ethnicity | 50 | All ages | NR | 607 I, 5484 NI | ICU 115 I, 989 NI | 30 I, 258 NI |
| Siston 2010 [28] | 788 pregnant women | 141 B, 242 H, 42 A/PI, 9 I, 4 MR, 167 C, 183 U | 100 | 25 (14–43) | Pregnant: 788 | 103 B, 175 H, 28 A/PI, 7 I, 2 MR, 89 C, 105 U | ICU 15 B, 39 H, 9 A/PI, 31 C, 21 U | 2 B, 8 H, 4 A/PI, 13 C, 3 U |
| CDC Dec 2009 [29] | NR | Reports mortality by ethnicity | NR | All ages | DM: 19 I, 92 NI Asthma: 13 I, 54 NI DM/asthma: 2 I, 238 NI | NR | NR | 42 (3.7/100,000) I, 384 (0.9/100,000) NI |
| Chitnis 2010 [30]* Truelove 2011 [31] | NR | Reports hospitalization by ethnicity | 57 | 28 (0.03–85) | Pregnant: 9 B, 2 H, 1 A, 3 C NMO: 22 B, 11 H, 4 A, 21 C MO: 21 B, 2 H, 6 C Comorbidity: CLD: 8 B, 4 H, 4 A, 13 C; DM: 15 B, 11 H, 4 A, 13 C; Cancer: 4 B, 4 H, 9 C; Hematologic: 14 B, 1 H, 1 A, 1 C | 120 (36/100,000) B, 19 (17/100,000) A, 39 H (14/100,000), 68 (1/100,000) C | ICU 19 B, 11 H, 6 A, 23 C | 4 B, 2 H, 1 A, 4 C |
| Dee 2011 [32] | NR | Reports hospitalization by ethnicity | NR | Hospitalizations (all ages), deaths (<18) | NR | 1569 (S/S 11/100,000, F/W 30/100,000) B, 1184 (S/S 8/100,000, F/W 31/100,000) H, 329 (S/S 8/100,000, F/W 13/100,000) A/PI, 53 (S/S 4/100,000, F/W 33/100,000) I, 2658 (S/S 3/100,000, F/W 16/100,000) C | NR | 45 B, 87 H, 14 A/PI, 6 I, 126 C (pediatric deaths only) |
| Jung 2011 [33]*† unpublished data; Jouvet 2010 [34] | NR | Reports critically ill by ethnicity | NR | NR | NR | NR | 66 I, 499 NI critically ill patients | NR |
| Louie 2011 [35] * unpublished data; CDC May 2009 [36] | NR | Reports hospitalization by ethnicity | NR | All ages | NR | 1024 H, 249 A/PI, 212 B, 16 I, 776 C, 126 U, 73 O | ICU 716 H, 156 A/PI, 132 B, 12 I, 587 C, 99 U, 53 O | 238 H, 42 A/PI, 38 B, 4 I, 192 C, 18 U, 7 O |
| Lee 2010 [37] | NR | Reports mortality by ethnicity | 53 | 43 (7 weeks-82) | NR | NR | NR | 17 B, 14 H, 5 A, 9 C, 2 U |
| CDC Aug 2009 [38] | 1557 | 308 B, 271 H, 47 A/PI, 99 C, 832 U | 50 | All ages | NR | 93 B, 64 H, 10 A/PI, 17 C, 21 U | NR | NR |
| CDC Jan 2010 [39] | NR | Reports hospitalization by ethnicity | 45 | All ages | NR | 26 B, 38 H, 5 A, 12 C, 18 U | NR | NR |
| Kwan-Gett 2010 [40] | 565 | 86 B, 127 A, 5 I, 41 other | 47 | All ages | Comorbidity: 1 A CLD, 1 H chemotherapy, 1 H DM MO: 1 H | NR | NR | 1 A, 2 H |
| Nguyen-Van-Tam 2010 [41] | NR | Reports hospitalization by ethnicity | 51 | 23 (0.25–90) | NR | 7 MR, 169 A, 100 B, 59 A/U, 202 C | NR | NR |
| Kumar 2010 [42] | NR | Reports hospitalization by ethnicity | 44 | 5 (0.1–19.2) | NR | 42 B, 17 H, 2 A, 13 C | NR | 1 B, 1 H |
| Harris 2010 [43] | 360 | 95 I, 86 NI | 52.5 | 21 (0.2–90) | Pregnant: 11 I, 80 NI Comorbidity: 71 I, 46 NI DM: 11 I, 3 NI | 23 (149/100,000) I, 38 (19/100,000) NI | ICU 2 (13/100,000) I, 7 (4/100,000) NI | 1 (7/100,000) I, 4 (2/100,000) NI |
| Kelly 2009 [44] | NR | Reports hospitalization by ethnicity | NR | NR | NR | 803 (150/100,000) I, 4030 NI | ICU 100 (19/100,000) I, 550 NI | 24 (5/100,000) I, 162 NI |
| Jain 2009 [45] | 272 | Reports hospitalization by ethnicity | 49 | 21 (0.06–86) | NR | 83 H, 53 B, 15 I/A/PI, 9 I, 73 C, 2 MR, 37 U | NR | NR |
| Creanga 2010 [46] | 136 | Reports hospitalization by ethnicity | 100 | NR (14–41) | Pregnant: 14 B, 30 H, 2 A, 9 C, 7 U | 38 B, 61 H, 6 A, 15 C, 16 U | NR | NR |
| Bettinger 2010 [47] | NR | Reports hospitalization by ethnicity | 45 | 4.8(0–16) | NR | 10 I | NR | NR |
| Miller 2010 [48] | NR | Reports ICU admission by ethnicity | 57 | 34 (15–62) | NR | NR | ICU 11 H, 1 A, 12 I, 1 B, 22 C | NR |
| Flint 2010 [49]* Flint 2009 [50] | NR | 116 I, 45 NI acute care | 52 | 39 (IQR 15.5–49) I 40 (IQR 19–15) overall | Pregnant: 8 I, 3 NI Obese: 8 I, 6 NI Comorbidity: Asthma: 16 I, 10 NI; COPD: 16 I, 9 NI; Bronchiectasis: 7 I, 2 NI; cardiac disease: 21 I, 8 NI, DM: 22 I, 8 I, Chronic liver disease: 10 I, 2 NI; CKD: 18 I, 2 NI; ND: 5 I, 4 NI; Immunosuppression: 3 I, 3 NI Smoker: 38 I, 5 NI Alcohol: 24 I, 3 NI | 92 (296/100,000) I, 39 (29/100,000) NI | 36/100,000 I, 7/100,000 NI | NR |
| Cretikos 2009 [51] | 5106 | Reports hospitalization by ethnicity | 47.8 | All ages | NR | 96 I, 1118 NI | ICU 14 I, 211 NI | 5 I, 43 NI |
| Scriven 2009 [52] | 3000 | Reports hospitalization by ethnicity | 69 | Adults 30.5 (NR) | NR | 35 A, 3 B, 14 C | Severe illness: 15 A, 3 B, 1 C | NR |
| Webb 2009 [53] *; Knight 2010 [54]; ANZIC Investigators 2010 [55] | NR | Reports ICU admission by ethnicity | 52.1 | 40 (IQR: 26–54) | NR | NR | ICU 129 I, 29 A, 483 C, 42 U | NR |
| Verrall 2010 [56]*; Dee 2010 [57] | NR | Reports hospitalization by ethnicity | NR | Mean 26 (range:0–82) | Chronic lung conditions: 47 I, 45 C/U | 134 I (PI 180/100,000; Maori 128/100,000), 74 NI, 21 U (C/U 26/100,000) | NR | NR |
| Sachedina 2010 [58] | NR | Reports mortality by ethnicity | 56 | 7 (0.25–17) | States “pre-existing health status did not differ between ethnic groups” | NR | NR | 27 A, 4 B, 37 C, 2 U |
| Kelly 2011 [59] | NR | Reports hospitalization by ethnicity | 53.8 | 46 (IQR: 29–58) hospitalizations | NR | 67 I, 386 NI | ICU 13 I, 86 NI | NR |
| Chien 2010 [60] | NR | Reports severe illness by ethnicity | 37 | RF: 33 (5–73) NRF: 13 (0–59) | NR | NR | 2 RF, 3 NRF | NR |
| Subramony 2010 [61] | NR | Reports hospitalization by ethnicity | 51 | 25 (IQR, 12–50) | NR | 599 Chinese [age-gender-adjusted hospitalization rate: 22.1/100,000], 390 Malay [76.3/100,000], 175 ID [53.2/100,000], 131 F [unadjusted: 10.4/100,000], 53 O [unadjusted: 44.2/100,000] | ICU 33 Chinese, 24 Malay, 9 ID, 6 F, 2 O | 10 Chinese, 2 Malay, 3 ID, 3 F, 3 U |
| Satterwhite 2010 [62] | NR | Reports hospitalization by ethnicity | 60 | 41.1 (95% CI: 38.0–44.2) | NR | 74 B, 28 C, 7 O/U | ICU admission: 15 B, 6 C, 2 O/U | NR |
| Bandaranayake 2011 [63] | 1758 | 51/100,000 I, 49/100,000 C, 25/100,000 U | NR | NR | NR | 33/100,000 I, 18/100,000 C, 26/100,000 other | NR | NR |
Notes: *major publication, ‡non-Indigenous and Caucasian are the reference groups unless it was a study conducted in another region (e.g., Chinese considered the reference group in China), Indigenous includes Aboriginals, First Nations, American Indians, Alaskan Natives, Maori, Native Hawaiians, Pacific Islanders, and Torres Strait Islanders, Blacks include African American, African, and Afro-Caribbean, † we obtained unpublished data from the authors of this study in the form of a poster presentation, Π we obtained unpublished data for the state of California from the authors.
Abbreviations: A Asian, A/PI Asian/Pacific Islander, ALL acute lymphoblastic leukemia, B Black, C Caucasian, CHD coronary heart disease, CHF congestive heart failure, CI confidence interval, CLD chronic lung disease, COPD chronic obstructive pulmonary disease, CP cerebral palsy, DM diabetes mellitus, DS down syndrome, F foreigners, unspecified,F/W Fall/Winter, H Hispanic, htn hypertension, I Indigenous, ICU intensive care unit, ID Indian descent, MD muscular dystrophy, MO morbid obesity, ND neurological disease, NI non-Indigenous, NMO non-morbid obesity, NRF non-respiratory failure, RAD reactive airway disease, RF respiratory failure, SD standard deviation, SLE systemic lupus erthematosus, S/S Spring/Summer, U unspecified.
Table 3. Patient characteristics and outcomes for low-income and lower-middle-income economies.
| First author, year | #H1N1 patients | #H1N1 patients by social disadvantage | % female | Median age (range) in years | # medical history by social disadvantage | # hospitalizations | # severe illness/ICU | # deaths |
| Reyes 2010 [64] | 239 | 239 Guatemalan | 40.1 | 8.8 (0.05–82) | Comorbidity: 53 other respiratory virus, 21 htn, 12 asthma, 2 DM Pregnant: 49 | 76 Guatemalan | ICU 21 Gautemalan Pneumonia 76 Guatemalan Mechanical ventilation 8 Guatemalan | 11 Guatemalan |
| Louriz 2010 [65] | NR | Reports hospitalization by low-income/lower-middle income economy | 43 | 17.6 (0.08–57; SD 14.8) | Comorbidity: 48 asthma, 13 heart disease, 10 hematologic disease, 4 chronic nephritis, 2 DM Pregnant: 15 Obese 2 | 186 Moroccan | ICU 20 Moroccan Mechanical ventilation 10 Moroccan | 7 Moroccan |
| Lahlou 2011 [66] | 240 | 240 Morocco | 38 | All ages 23 (SD 14) | Hospitalization only: Comorbidity: 7 asthma, 5 DM Pregnant: 13 Obese: 2 | 27 Moroccan | 0 Moroccan | 0 Moroccan |
| Jagannatha Rao 2011 [67] | NR | Reports hospitalization by low-income/lower-middle income economy | 70 | NR (11–80) | Comorobidity: 6 htn | 20 ID | Acute respiratory distress syndrome 6 ID, bronchopneumonia 6 ID | 5 ID |
| Chacko 2010 [68] | NR | Reports hospitalization by low-income/lower-middle income economy | 42 | All ages 35 (IQR: 28.2–42.8) ICU admissions | Comorbidity: 4 htn, 3 DM, 2 asthma, 1 renal failure, 1 immunosuppression, 1 COPD, Obese: 9 Pregnant: 3 | 66 ID | ICU 38 ID | 6 ID |
| Parakh 2010 [69] | NR | Reports hospitalization by low-income/lower-middle income economy | 60 | 2.5 (0.25–10) | Comorbidity: 16 malnutrition, 1 TB, 1 heart disease | 25 ID | Pediatric ICU 7, mechanical ventilation 4 | 3 ID |
| Ramakrishna 2011 [70]*; Pramanick 2011 [71] | NR | Reports hospitalization by low-income/lower-middle income economy | ??ICU: 68% (wave 1), 51% (wave 2) | ICU: Mean 34.1 (SD 13) wave 1, 36.2 (SD 4.6) wave 2 | ICU: Comorbidity: 7 CVD, 8 immunosupressants, 3 DM, 2 respiratory disease MO: 2 Pregnant/postpartum: 15 | 629 ID | ICU 76 ID Mechanical ventilation 72 ID | 48 ID |
| Puvanalingam 2011 [72] | 442 | 442 ID | 44 | All ages | Comorbidity: 71 asthma, 39 TB, 32 HTN, 28 DM Alcoholism: 46 Smoking: 35 | 199 ID (12 pregnant women) | 9 ID pregnant women pneumonia | 3 ID pregnant women |
| Sharma 2010 [73] | NR | Reports hospitalization by low-income/lower-middle income economy | Deaths: 50 | Deaths: mean 38 (10–65, SD 15.3) | Deaths: Comorbidity: 3 COPD, 3 asthma, 3 asthma, 6 htn, 4 DM, 1 CAD Pregnant: 2 Obese: 3 Smoking: 1 Alcohol: 1 | 125 ID | Deaths: 12 acute respiratory distress syndrome ID | 16 ID |
| Chudasama 2011 [74]*; Chudasama 2010 [75]; Chudasama 2010 [76]; Chudasama 2010 [77]; Chudasama 2010 [78] | NR | Reports hospitalization by low-income/lower-middle income economy | 48.5 | 27 (0.38–68) | Comorbidity: 27 DM, 24 htn, 15 CLD, 13 CHD, 7 seizures, 2 chronic renal failure Pregnancy: 15 | 274 ID | NR | 71 ID |
| Gupta 2011 [79] | NR | Reports hospitalization by low-income/lower-middle income economy | 24 | Mean 5.7 (0.5–18, SD 4.1) | Comorbidity: 30 anemia, 30 malnourished | 62 ID | ICU 19 ID | 4 ID |
| Naseem 2011 [80] | NR | Reports hospitalization by low-income/lower-middle income economy | 61.1 | Adults only Mean 34.24 (SD 13.92) | Hospitalization only: Comorbidity: 2 COPD, 2 DM, 2 CHF Obese: 7 Pregnant: 3 Smoking: 9 | 36 Pakistani | ICU 10 Pakistani Mechanical ventilation 10 Pakistani | 6 Pakistani |
Abbreviations: CHD coronary heart disease, CHF congestive heart failure, CLD chronic lung disease, COPD chronic obstructive pulmonary disease, DM diabetes mellitus, htn hypertension, ID Indian descent, NR not reported, SD standard deviation.
Two studies included only pregnant women infected with H1N1 [19], [28] and 14 others reported on pregnancies among socially disadvantaged populations [21], [30], [43], [46], [49], [64]–[66], [68], [70], [72]–[74], [80]. No significant differences were observed between the proportion of pregnancies in ethnic minorities and non-ethnic minorities in HIC (n = 765 patients, OR 0.31, 95% CI: 0.03–3.64) [30], [43], [46], [49]. Six studies included only H1N1-infected children and adolescents [20], [42], [47], [58], [69], [79] and two studies reported deaths in pediatric patients (although the number of hospitalizations was for the entire population including all ages for one study) [20], [32]. Twenty-one studies reported comorbidities among the socially disadvantaged; including asthma, chronic lung conditions, heart conditions, and diabetes [20], [21], [24], [29], [30], [40], [43], [49], [56], [64]–[70], [72]–[74], [79], [80]; all studies conducted in LIC/LMIC reported this information. For HIC studies, there was no significant difference observed between ethnic minorities and non-ethnic minorities in terms of prevalent comorbidities (n = 1,203 patients, OR 1.14, 95% CI: 0.63–2.06; Appendix S3) [20], [24], [29], [30], [43], [49]. Ten studies reported on obesity [20], [30], [40], [49], [65], [66], [68], [70], [73], [80] and no significant differences were observed with respect to the prevalence of obesity between ethnic minorities and non-ethnic minorities in HIC studies (n = 500 patients, OR 0.76, 95% CI: 0.46–1.26) [20], [30], [49]. Four studies reported the proportion of patients who were pregnant and no differences were observed in the odds of being pregnant between ethnic minorities and non-ethnic minorities (n = 765 patients, OR 0.31, 95% CI: 0.03–3.64) [30], [43], [46], [49]. Four studies reported on smoking and alcohol use [49], [72], [73], [80]; meta-analysis was not possible because only one study reported on ethnic minorities in a HIC and the other three were conducted in LIC/LMIC.
Methodological Quality
The majority of the studies used a sample truly representative of the average individual infected with H1N1 in the community (e.g., population-based sample of an entire province or state) or somewhat representative sample of the average individual infected with H1N1 in the community (e.g., pregnant woman from an entire state or province). Ten studies did not use a representative sample; one included volunteers [45], one included only those with severe illness [33], four included individuals with severe illness who died [20], [29], [37], [58], two included pediatric cases in India [69], [79], and two obtained data from one local hospital [43], [49] (Table 4). All of the studies selected the non-exposed cohort from the same community as the exposed cohort and used a structured interview (i.e., self-report) to assess exposure (e.g., social disadvantage), except for studies conducted in LIC/LMIC, for which the data were obtained from hospital records. All of the studies ensured that the patients were not severely ill, hospitalized or dead at the start of the study, except for four studies [20], [29], [37], [58]. All studies assessed the outcomes using record linkage, and the duration of follow-up was deemed appropriate in all of the studies. Most studies did not control for important factors, such as comorbidity (13 studies controlled for comorbidities [22], [29], [32], [33], [41], [43], [48], [49], [56], [58], [60], [61], [63]) and 18 studies had greater than 10% of the patients lost to follow-up or did not describe the follow-up rate [21], [22], [29], [45], [48], [56], [58], [60], [62], [63], [65], [67]–[69], [72], [73], [79], [80].
Table 4. Methodological quality.
| Study | Representative exposed cohort | Selection of non- exposed cohort | Ascertainment of exposure | Outcome of interest not present at study start | Comparability of cohorts | Assessment of outcome | Long enough follow-up for outcomes to occur | Loss to follow-up |
| Oluyomi-Obi 2010 [19] | b | a | b | a | c | b | a | a |
| CDC Sept 2009 [20] | c | a | b | b | c | b | a | a |
| Martin 2010 [21] | a | a | b | a | c | b | a | d |
| Paine 2010 [22] | a | a | b | a | a | b | a | d |
| Wenger 2011 [24] | b | a | b | a | c | b | a | a |
| Zarychanski 2010 [25] | a | a | b | a | c | b | a | c |
| Helferty 2010 [26] | a | a | b | a | c | b | a | c |
| Siston 2010 [28] | b | a | b | a | c | b | a | a |
| CDC Dec 2009 [29] | c | a | b | c | a | b | a | d |
| Chitnis 2010 [30] | a | a | b | a | c | b | a | a |
| Dee 2011 [32] | a | a | b | a | a | b | a | c |
| Jung 2011 [33] unpub. | c | a | b | a | a | b | a | a |
| Louie 2011 [35] unpub. | a | a | b | a | c | b | a | a |
| Lee 2010 [37] | c | a | b | a | c | b | a | a |
| CDC Aug 2009 [38] | a | a | b | a | c | b | a | a |
| CDC Jan 2010 [39] | a | a | b | a | c | b | a | a |
| Kwan-Gett 2010 [40] | a | a | b | a | c | b | a | a |
| Nguyen-Van-Tam 2010 [41] | a | a | b | a | a | b | a | b |
| Kumar 2010 [42] | b | a | b | a | c | b | a | a |
| Harris 2010 [43] | c | a | b | a | a | b | a | c |
| Kelly 2009 [44] | a | a | b | a | c | b | a | a |
| Jain 2009 [45] | c | a | b | b | c | b | a | d |
| Creanga 2010 [46] | b | a | b | a | c | b | a | a |
| Bettinger 2010 [47] | b | a | b | a | c | b | a | c |
| Miller 2010 [48] | a | a | b | a | a | b | a | d |
| Flint 2010 [49] | c | a | b | a | a | b | a | a |
| Cretikos 2009 [51] | a | a | b | a | c | b | a | a |
| Scriven 2009 [52] | a | a | b | a | c | b | a | a |
| Webb 2009 [53] | a | a | b | a | c | b | a | b |
| Verrall 2010 [56] | b | a | b | a | a | b | a | d |
| Sachedina 2010 [58] | c | a | b | b | a | b | a | d |
| Kelly 2011 [59] | a | a | b | a | c | b | a | b |
| Chien 2010 [60] | b | a | b | a | a | b | a | d |
| Subramony 2010 [61] | a | a | a | a | a | b | a | b |
| Satterwhite 2010 [62] | a | a | a | a | c | b | a | d |
| Bandaranayake 2011 [63] | a | a | a | a | a | b | a | d |
| Reyes 2010 [64] | b | a | a | a | c | b | a | b |
| Louriz 2010 [65] | b | a | a | a | c | b | a | d |
| Lahlou 2011 [66] | b | a | a | a | c | b | a | a |
| Jagannatha Rao 2011 [67] | b | a | a | a | c | b | a | d |
| Chacko 2010 [68] | b | a | a | a | c | b | a | d |
| Parakh 2010 [69] | c | a | a | a | c | b | a | d |
| Ramakrishna 2011 [70] | b | a | a | a | c | b | a | a |
| Puvanalingam 2011 [72] | b | a | a | a | c | b | a | d |
| Sharma 2010 [73] | b | a | a | a | c | b | a | d |
| Chudasama 2011 [74] | b | a | a | a | c | b | a | a |
| Gupta 2011 [79] | c | a | a | a | c | b | a | d |
| Naseem 2011 [80] | b | a | a | a | c | b | a | d |
Note: Please see Appendix S2 for an explanation of each methodological quality component. Briefly, each item was appraised as follows:
1) Representativeness: a) truly representative, b) somewhat representative, c) selected group of users, d) no description of the derivation of the cohort.
2) Selection: a) drawn from the same community as exposed cohort, b) drawn from a different source, c) no description.
3) Ascertainment: a) secure record, b) structured interview, c) written self report, d) no description.
4) Demonstration: a) yes, b) no.
5) Comparability: a) study controls for age or gender, b) study controls for any additional factor, c) no control.
6) Assessment: a) independent blind assessment, b) record linkage, c) self report, d) no description.
7) Follow-up: a) yes, b) no.
8) Adequacy: a) complete follow up, b) subjects lost to follow up unlikely to introduce bias, c) large loss to follow-up, d) no statement.
Hospitalization
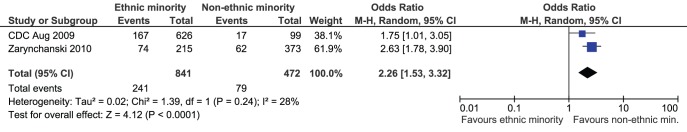
Twenty-four studies reported hospitalization data broken down by ethnicity (Table 2) [24]–[26], [28], [30], [32], [35], [38], [39], [41]–[47], [49], [51], [52], [56], [59], [61]–[63]. Four studies reported the number of H1N1-infected individuals by ethnicity and the prevalence hospitalization among those with H1N1 ranged from 24–27% among ethnic minorities and 17–87% among non-ethnic minorities in HIC [25], [38], [43], [49]. Two studies were not included in the meta-analysis due to concerns about confounding and inclusion of a non-representative sample [43], [49]. Once these studies were excluded, there was a significantly greater proportion of ethnic minority versus non-ethnic minority hospitalizations (n = 1,313 patients, OR 2.26, 95% CI: 1.53–3.32, I2 = 28%; Figure 2) [25], [36]. Similarly, a study including pregnant women infected with H1N1 reported a significantly higher proportion of hospitalizations among ethnic minorities (72%) versus non-ethnic minorities (53%; OR based on this study: 2.27, 95% CI: 1.57–3.28) [28].
Figure 2. Meta-analysis of hospitalizations among ethnic minorities versus non-ethnic minorities in North America.
Favours ethnic minority means that ethnic minorities experienced a lower proportion of H1N1 hospitalizations compared to non-ethnic minorities. Favours non-ethnic minorities means that non-ethnic minorities experienced a lower proportion of H1N1 hospitalizations compared to ethnic minorities.
All of the studies conducted in LIC/LMIC reported hospitalization data for individuals with H1N1 (Table 3). The prevalence of hospitalization among those infected with H1N1 was 32% in Guatemala [64], 11% in Morocco [66], and 45% in India [72]. Prevalence meta-analysis was not possible because only one study was conducted in each country.
Severe Illness
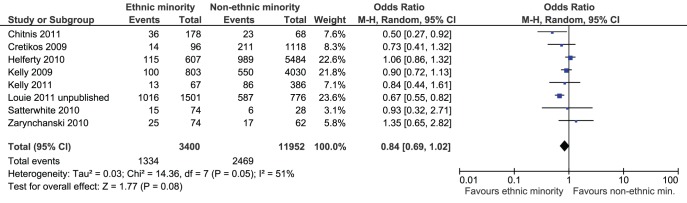
Nineteen of the included studies reported the number of H1N1 patients experiencing severe illness broken down by ethnicity, including intensive care unit (ICU) admission [19], [21], [25], [26], [28], [30], [33], [35], [43], [44], [48], [49], [51]–[53], [59], [62], severe illness unspecified [61], and pneumonia or respiratory failure [60]. One study of H1N1-infected pregnant women observed similar proportions of ICU admissions between ethnic minorities (15%) and non-ethnic minorities (19%; OR based on this study: 0.74, 95% CI: 0.46–1.20) [28]. One study observed a similar relationship for patients admitted to the ICU among all H1N1-infected patients in Australia (OR 0.24, 95% CI: 0.05–1.20) [43], while another study observed a greater proportion of ICU admissions among ethnic minorities in Manitoba (OR 2.76, 95% CI: 1.45–5.23) [25]. Meta-analysis was not conducted because the Australian study was affected by confounding and did not use a representative sample [43]. In LIC/LMIC, the proportion of ICU admissions among H1N1-infected was 9% in Guatemala [64] and 0% in Morocco [66].
One study of H1N1-infected pregnant women observed a significantly greater proportion of ICU admissions among non-ethnic minority hospitalizations (35%) versus ethnic minority hospitalizations (35%; OR based on this study: 0.47, 95% CI: 0.28–0.79) [28]. Eight studies reported ethnicity data on the proportion of patients admitted to the ICU among those hospitalized in HIC and were meta-analyzed [25], [26], [30], [35], [44], [51], [59], [62]. The prevalence ranged from 6–68% among ethnic minorities and 7–76% among non-ethnic minorities. One study was not included in the meta-analysis due to concerns about confounding and inclusion of a non-representative sample [43]. Excluding this study, there were no differences in ICU admissions among hospitalized non-ethnic minorities compared to ethnic minorities (n = 15,352 patients, OR 0.84, 95% CI: 0.69, 1.02, I2 = 51%, Figure 3).
Figure 3. Meta-analysis of ICU admissions among ethnic minorities versus non-ethnic minorities.
Favours ethnic minority means that ethnic minorities experienced a lower proportion of intensive care unit (ICU) admissions due to H1N1 compared to non-ethnic minorities. Favours non-ethnic minorities means that non-ethnic minorities experienced a lower proportion of ICU admissions due to H1N1 compared to ethnic minorities.
All of the studies conducted in LIC/LMIC reported data on severe illness (Table 3). Two studies conducted in India reported ICU admission among hospitalized adults and the pooled prevalence was 34% (95% CI: 0–79%) [68], [70]. Two studies reported this information among Indian children and the pooled prevalence was 30% (95% CI: 20–40%) [69], [79].
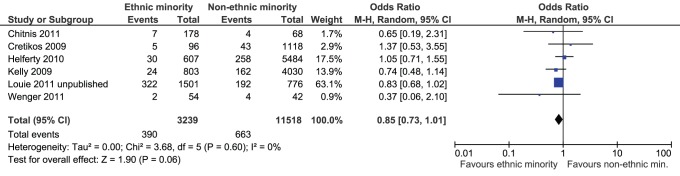
Mortality
Fifteen studies reported the number of deaths by ethnicity [20], [22], [24], [26], [29], [30], [32], [33], [35], [37], [40], [43], [44], [51], [58]. One study of pregnant women infected with H1N1 observed a significantly lower proportion of deaths among H1N1-infected pregnant ethnic minorities (3%) versus pregnant non-ethnic minorities (15%; OR based on this study: 0.19, 95% CI: 0.09–0.43) [28]. None of the others reported the proportion of deaths among H1N1-infected individuals. This study also observed a significantly lower death rate among pregnant ethnic minority hospitalizations (4%) versus pregnant non-ethnic minority hospitalizations (15%; OR 0.27, 95% CI: 0.12–0.61) [28]. Mortality ranged from 1–21% among ethnic minorities and 4–25% among non-ethnic minorities in HIC. Six studies reported the proportion of deaths among hospitalized patients and were meta-analyzed [24], [26], [30], [35], [44], [51]. One study was not included in the meta-analysis due to confounding and inclusion of a non-representative sample [43]. Excluding this study, there were no differences in the proportion of deaths among hospitalized non-ethnic minorities compared to ethnic minorities (n = 14,757 patients, OR 0.85, 95% CI: 0.73–1.01, I2 = 0%, Figure 4).
Figure 4. Meta-analysis of mortality among hospitalized ethnic minorities versus hospitalized non-ethnic minorities.
Favours ethnic minority means that ethnic minorities experienced a lower proportion of deaths due to H1N1 among hospitalized patients compared to non-ethnic minorities. Favours non-ethnic minorities means that non-ethnic minorities experienced a lower proportion of deaths due to H1N1 among hospitalized patients compared to ethnic minorities.
All of the studies conducted in LIC/LMIC reported mortality (Table 3). Five studies conducted in India reported the number of deaths among hospitalized adults and the pooled prevalence was 15% (95% CI: 7–23%) [67], [68], [70], [73], [74]. Two reported this information among Indian children and the pooled prevalence was 8% (95% CI: 2–13%) [69], [79].
Discussion
We conducted a systematic review on the occurrence of hospitalization, severe illness, and mortality among socially disadvantaged groups of the population. The prevalence of hospitalization among those with H1N1 ranged from 24–27% among ethnic minorities and 17–87% among non-ethnic minorities in HIC and was 11–45% in LIC/LMIC. The proportion of patients admitted to the ICU among those with H1N1 ranged from 2–12% among ethnic minorities and 5–8% among non-ethnic minorities in HIC and was 0–9% in LIC/LMIC. The proportion of ICU admissions among hospitalized patients ranged from 6–68% among ethnic minorities and 7–76% among non-ethnic minorities in HIC. The pooled prevalence of ICU admission among hospitalizations in India was approximately 30%. The prevalence of mortality ranged from 1–21% among ethnic minorities and 4–25% among non-ethnic minorities in HIC and the pooled prevalence of deaths among hospitalizations ranged from 8–15% in India. These estimates suggest that the burden of H1N1 was significant across LIC/LMIC and HIC.
Our results are similar to previous reviews on the global burden of H1N1. In a systematic review of H1N1 in the Southern Hemisphere, 17–45% of laboratory-confirmed H1N1 cases were hospitalized, of which 8–26% were admitted to ICUs and 14–22% died [5]. A similar burden was observed in the Northern Hemisphere, with 94% of patients hospitalized, 36% of patients admitted to ICU, and 39% died [6]. The current review is more comprehensive, with a scope encompassing all regions of the world and comparisons drawn across ethnic minorities in HIC and individuals from LIC/LMIC.
Another study pooled data on risk factors for acquiring H1N1 pandemic and included data from governmental surveillance programs across 19 countries [81]. In this study, ethnic minorities had a higher risk of hospitalization and fatality compared to the general population in Canada, Australia, and New Zealand. For severe H1N1 pandemic, ethnic minorities were under-represented among cases in Thailand and Mexico [81]. Meta-analysis results were not reported due to the small number of countries reporting data.
Some of the included studies compared the burden of H1N1 for ethnic minorities versus non-ethnic minorities in HIC, allowing comparisons between these groups. In two large North American studies, there were significantly more hospitalizations among ethnic minorities versus non-ethnic minorities [25], [38]. However, there were no differences in ICU admissions or deaths among patients hospitalized with H1N1 for ethnic minorities and non-ethnic minorities among studies conducted in North America and Australia. It is possible that non-ethnic minorities had a greater proportion of comorbidities, pregnancy or obesity – known risk factors for pandemic H1N1 (i.e., confounding variables) [5], [6]. However, we did not find any differences in these factors between ethnic minorities and non-ethnic minorities in HIC across some of the studies that were included in the meta-analyses.
Pregnancy is a recognized risk factor for seasonal influenza and pandemic influenza [5], [6], [82]. One of the studies included pregnant women infected with H1N1 and the results were inconsistent across the outcomes examined [28]. For example, significantly higher hospitalizations were observed for pregnant ethnic minorities versus pregnant non-ethnic minorities, yet a significantly higher proportion of deaths occurred among pregnant non-ethnic minorities versus pregnant ethnic minorities [28]. These results could be because non-ethnic minorities had a greater proportion of comorbidity, but this information was not reported. Only one study reported this data so we were unable to examine pregnancy further through meta-analysis.
A small number of seniors were infected with the pandemic A/H1N1/2009 virus, which is inconsistent with previous influenza pandemics [5]. This is likely because seniors were previously exposed to a similar H1N1 strain [83], affording some protection against the 2009 pandemic. However, the elderly still experienced high hospitalization and death rates [5], [6]. We were unable to examine this as none of the included studies reported data specific to elderly socially disadvantaged individuals.
There are limitations associated with the conduct of our systematic review. First, we were unable to include some studies if they did not provide a breakdown for the outcomes of interest by ethnicity. Furthermore, we found that because the classification of ethnicity varies by region, drawing comparisons across countries was difficult [84]. Second, some potentially relevant studies were excluded if they did not isolate confirmed cases from suspected cases in their analysis. Third, some of the included studies did not report details, such as total number of individuals with H1N1, record of potential confounding variables or number lost to follow-up. For these reasons, the systematic review conduct was challenging.
It is possible that relevant unpublished studies were omitted, although efforts were made to contact authors and request access to data that had been presented at conferences. Through these efforts, we successfully obtained the results from two unpublished studies [33], [35]. As well, it’s worth noting that due to the small number of studies included in the meta-analysis of HIC, we were unable to assess the impact of publication bias on our results (i.e., through the use of a funnel plot). Finally, our results are generalizable only to ethnic-minorities in HIC and individuals in LIC/LMIC, as none of the identified studies reported data for other types of social disadvantage (e.g., groups without access or disproportionate access to healthcare or individuals of low socioeconomic status).
To conclude, the prevalence of hospitalization, severe illness, and mortality due to H1N1 was high for ethnic minorities in HIC and individuals from LIC/LMIC. In addition, there was an increased proportion of hospitalization among ethnic minorities compared to non-ethnic minorities in two studies conducted in North America. However, a similar risk of ICU admission and death was observed among ethnic minorities and non-ethnic minorities in studies conducted in Canada, the United States, and Australia. These results suggest that there was little difference in H1N1 burden between ethnic minorities and non-ethnic minorities living in HIC.
Supporting Information
Medline search strategy.
(DOCX)
Methodological quality.
(DOCX)
Confounding variables and meta-analysis results.
(DOCX)
(DOCX)
(DOCX)
Acknowledgments
We thank Nahoko Shindo of the WHO and Tanya Horsley for providing us with potentially relevant articles. We also thank Janice Louie and Samuel Yang for providing unpublished data from the state of California and Anand Kumar for sharing their poster presentation. We thank Maggie Chen for her statistical consultation and for meta-analyzing the prevalence estimates from India.
Footnotes
Competing Interests: The authors have the following interests: ACT has been a paid consultant to examine cross-protection of non-influenza vaccine types for GlaxoSmithKline. This does not alter the authors' adherence to all the PLoS ONE policies on sharing data and materials. The other authors have nothing to declare.
Funding: This systematic review was partially funded by the World Health Organization (WHO), Global Influenza Programme (http://www.who.int/influenza/about/en/). The funders had no role in study design, data collection and analysis, decision to publish, or the preparation of the manuscript. Sharon E. Straus is funded by a Tier 1 Canada Research Chair through the Canadian Institutes for Health Research.
References
- 1.Reed C, Angulo FJ, Swerdlow DL, Lipsitch M, Meltzer MI. Estimates of the prevalence of pandemic (H1N1) 2009, United States, April-July 2009. Emerg Infect Dis. 2009;15:2007. doi: 10.3201/eid1512.091413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Galante M, Garin O, Sicuri E, Cots F, Garcia-Altes A. Health Services Utilization, Work Absenteeism and Costs of Pandemic Influenza A (H1N1) 2009 in Spain: A Multicenter-Longitudinal Study. PLoS One. 2012;7:e31696. doi: 10.1371/journal.pone.0031696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lai PL, Panatto D, Ansaldi F, Canepa P, Amicizia D. Burden of the 1999–2008 seasonal influenza epidemics in Italy: comparison with the H1N1v (A/California/07/09) pandemic. Hum Vaccin. 2011;7 doi: 10.4161/hv.7.0.14607. [DOI] [PubMed] [Google Scholar]
- 4.Higgins AM, Pettila V, Harris AH, Bailey M, Lipman J. The critical care costs of the influenza A/H1N1 2009 pandemic in Australia and New Zealand. Anaesth Intensive Care. 2011;39:391. doi: 10.1177/0310057X1103900308. [DOI] [PubMed] [Google Scholar]
- 5.Falagas ME, Koletsi PK, Baskouta E, Rafailidis PI, Dimopoulos G. Pandemic A(H1N1) 2009 influenza: review of the Southern Hemisphere experience. Epidemiol Infect. 2011;139:40. doi: 10.1017/S0950268810002037. [DOI] [PubMed] [Google Scholar]
- 6.Falagas ME, Cholevas NV, Kapaskelis AM, Vouloumanou EK, Michalopoulos A. Epidemiological aspects of 2009 H1N1 influenza: the accumulating experience from the Northern Hemisphere. Eur J Clin Microbiol Infect Dis. 2010;29:1347. doi: 10.1007/s10096-010-1002-3. [DOI] [PubMed] [Google Scholar]
- 7.Larussa P. Pandemic Novel 2009 H1N1 Influenza: What Have We Learned? Semin Respir Crit Care Med. 2011;32:399. doi: 10.1055/s-0031-1283279. [DOI] [PubMed] [Google Scholar]
- 8.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.La Ruche G, Tarantola A, Barboza P, Vaillant L, Gueguen J. The 2009 pandemic H1N1 influenza and indigenous populations of the Americas and the Pacific. Euro Surveill 14. 2009. [DOI] [PubMed]
- 10.Center for Disease Control and Prevention (CDC) Evaluation of rapid influenza diagnostic tests for detection of novel influenza A (H1N1) Virus - United States. MMWR Morb Mortal Wkly Rep. 2009;58:829. [PubMed] [Google Scholar]
- 11.Landry ML. Diagnostic tests for influenza infection. Curr Opin Pediatr. 2011;23:97. doi: 10.1097/MOP.0b013e328341ebd9. [DOI] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention (CDC) Influenza Diagnostic Testing Algorithm. 2011. Available: http://www.cdc.gov/flu/professionals/diagnosis/testing_algorithm.htm. Accessed Sept 14, 2011.
- 13.World Bank. World Bank Classification. 2011. Available: http://data.worldbank.org/about/country-classification/country-and-lending-groups. Accessed Sept 14, 2011.
- 14.Galarce EM, Minsky S, Viswanath K. Socioeconomic status, demographics, beliefs and A(H1N1) vaccine uptake in the United States. Vaccine. 2011;29:5289. doi: 10.1016/j.vaccine.2011.05.014. [DOI] [PubMed] [Google Scholar]
- 15.Wells G, Shea BJ, O'Connell D, Peterson J, Welch V. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2011. Available: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed Sept 14, 2011.
- 16.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 17.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 18.Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.2. [updated September 2009]. The Cochrane Collaboration. 2009. Available: www.cochrane-handbook.org. Accessed Sept 14, 2011.
- 19.Oluyomi-Obi T, Avery L, Schneider C, Kumar A, Lapinsky S. Perinatal and maternal outcomes in critically ill obstetrics patients with pandemic H1N1 Influenza A. J Obstet Gynaecol Can. 2010;32:447. doi: 10.1016/S1701-2163(16)34497-8. [DOI] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention (CDC) Surveillance for Pediatric Deaths Associated with 2009 Pandemic Influenza A (H1N1) Virus Infection –- United States, April–August 2009. MMWR Morb Mortal Wkly Rep. 2009;58:947. [PubMed] [Google Scholar]
- 21.Martin SS, Hollingsworth CL, Norfolk SG, Wolfe CR, Hollingsworth JW. Reversible cardiac dysfunction associated with pandemic 2009 influenza A(H1N1). Chest. 2010;137:1197. doi: 10.1378/chest.10-0032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Paine S, Mercer GN, Kelly PM, Bandaranayake D, Baker MG. Transmissibility of 2009 pandemic influenza A(H1N1) in New Zealand: effective reproduction number and influence of age, ethnicity and importations. Euro Surveill 15. 2010. [PubMed]
- 23.Baker MG, Wilson N, Huang QS, Paine S, Lopez L. Pandemic influenza A(H1N1)v in New Zealand: the experience from April to August 2009. Euro Surveillance: Bulletin Europeen sur les Maladies Transmissibles = European Communicable Disease Bulletin 14. 2009. [DOI] [PubMed]
- 24.Wenger JD, Castrodale LJ, Bruden DL, Keck JW, Zulz T. 2009 Pandemic influenza A H1N1 in Alaska: temporal and geographic characteristics of spread and increased risk of hospitalization among Alaska Native and Asian/Pacific Islander people. Clin Infect Dis. 2011;52:S197. doi: 10.1093/cid/ciq037. [DOI] [PubMed] [Google Scholar]
- 25.Zarychanski R, Stuart TL, Kumar A, Doucette S, Elliott L. Correlates of severe disease in patients with 2009 pandemic influenza (H1N1) virus infection. CMAJ. 2010;182:264. doi: 10.1503/cmaj.091884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Helferty M, Vachon J, Tarasuk J, Rodin R, Spika J. Incidence of hospital admissions and severe outcomes during the first and second waves of pandemic (H1N1) 2009. CMAJ. 2010;182:1987. doi: 10.1503/cmaj.100746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Campbell A, Rodin R, Kropp R, Mao Y, Hong Z. Risk of severe outcomes among patients admitted to hospital with pandemic (H1N1) influenza. CMAJ. 2010;182:355. doi: 10.1503/cmaj.091823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Siston AM, Rasmussen SA, Honein MA, Fry AM, Seib K. Pandemic 2009 influenza A(H1N1) virus illness among pregnant women in the United States. JAMA. 2010;303:1525. doi: 10.1001/jama.2010.479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention (CDC) Deaths related to 2009 pandemic influenza A (H1N1) among American Indian/Alaska Natives - 12 states, 2009. MMWR Morb Mortal Wkly Rep. 2009;58:1344. [PubMed] [Google Scholar]
- 30.Chitnis AS, Truelove SA, Druckenmiller JK, Heffernan RT, Davis JP. Epidemiologic and clinical features among patients hospitalized in Wisconsin with 2009 H1N1 influenza A virus infections, april to august 2009. Wis Med J. 2010;109:208. [PubMed] [Google Scholar]
- 31.Truelove SA, Chitnis AS, Heffernan RT, Karon AE, Haupt TE. Comparison of patients hospitalized with pandemic 2009 influenza A (H1N1) virus infection during the first two pandemic waves in Wisconsin. J Infect Dis. 2011;203:837. doi: 10.1093/infdis/jiq117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dee DL, Bensyl DM, Gindler J, Truman BI, Allen BG. Racial and Ethnic Disparities in Hospitalizations and Deaths Associated with 2009 Pandemic Influenza A (H1N1) Virus Infections in the United States. Ann Epidemiol. 2011;21:630. doi: 10.1016/j.annepidem.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 33.Jung J, Fowler R, Long J, Zarychanski R, Rodin R. 2009–2010 H1N1–related critical illness among Aboriginal and Non-Aboriginal Canadians. Unpublished data. 2011. [DOI] [PMC free article] [PubMed]
- 34.Jouvet P, Hutchison J, Pinto R, Menon K, Rodin R. Critical illness in children with influenza A/pH1N1 2009 infection in Canada. Pediatr Crit Care Med. 2010;11:609. doi: 10.1097/PCC.0b013e3181d9c80b. [DOI] [PubMed] [Google Scholar]
- 35.Louie J, Yang S. Hospitalizations with 2009 novel influenza A(H1N1) in California. Unpublished data. 2011.
- 36.Centers for Disease Control and Prevention (CDC) Hospitalized Patients with Novel Influenza A (H1N1) Virus Infection –- California, April–May, 2009. MMWR Morb Mortal Wkly Rep. 2009;58:541. [PubMed] [Google Scholar]
- 37.Lee EH, Wu C, Lee EU, Stoute A, Hanson H. Fatalities associated with the 2009 H1N1 influenza A virus in New York city. Clin Infect Dis. 2010;50:1504. doi: 10.1086/652446. [DOI] [PubMed] [Google Scholar]
- 38.Centers for Disease Control and Prevention (CDC) 2009 Pandemic Influenza A (H1N1) Virus Infections –- Chicago, Illinois, April–July 2009. MMWR Morb Mortal Wkly Rep. 2009;58:918. [PubMed] [Google Scholar]
- 39.Centers for Disease Control and Prevention (CDC) Patients hospitalized with 2009 pandemic influenza A (H1N1) - New York City, May 2009. MMWR Morb Mortal Wkly Rep. 2010;58:1440. [PubMed] [Google Scholar]
- 40.Kwan-Gett TS, Baer A, Duchin JS. Spring 2009 H1N1 influenza outbreak in King County, Washington. Disaster Med Public Health Prep. 2009;3:S116. doi: 10.1097/DMP.0b013e3181c6b818. [DOI] [PubMed] [Google Scholar]
- 41.Nguyen-Van-Tam JS, Openshaw P, Hashim A, Gadd EM, Lim WS. Risk factors for hospitalisation and poor outcome with pandemic A/H1N1 influenza: United Kingdom first wave (May-September 2009). Thorax. 2010;65:651. doi: 10.1136/thx.2010.135210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kumar S, Havens PL, Chusid MJ, Willoughby RE, Simpson P. Clinical and epidemiologic characteristics of children hospitalized with 2009 pandemic H1N1 influenza A infection. Pediatr Infect Dis J. 2010;29:594. doi: 10.1097/inf.0b013e3181d73e32. [DOI] [PubMed] [Google Scholar]
- 43.Harris PN, Dixit R, Francis F, Buettner PG, Leahy C. Pandemic influenza H1N1 2009 in north Queensland–risk factors for admission in a region with a large indigenous population. Commun Dis Intell. 2010;34:109. [PubMed] [Google Scholar]
- 44.Kelly H, Mercer G, Cheng A. Quantifying the risk of pandemic influenza in pregnancy and indigenous people in Australia in 2009. Euro Surveillance: Bulletin Europeen sur les Maladies Transmissibles = European Communicable Disease Bulletin 14. 2009. [PubMed]
- 45.Jain S, Kamimoto L, Bramley AM, Schmitz AM, Benoit SR. Hospitalized patients with 2009 H1N1 influenza in the United States, April-June 2009. N Engl J Med. 2009;361:1944. doi: 10.1056/NEJMoa0906695. [DOI] [PubMed] [Google Scholar]
- 46.Creanga AA, Johnson TF, Graitcer SB, Hartman LK, Al-Samarrai T. Severity of 2009 pandemic influenza A (H1N1) virus infection in pregnant women. Obstet Gynecol. 2010;115:726. doi: 10.1097/AOG.0b013e3181d57947. [DOI] [PubMed] [Google Scholar]
- 47.Bettinger JA, Sauve LJ, Scheifele DW, Moore D, Vaudry W. Pandemic influenza in Canadian children: a summary of hospitalized pediatric cases. Vaccine. 2010;28:3184. doi: 10.1016/j.vaccine.2010.02.044. [DOI] [PubMed] [Google Scholar]
- 48.Miller RR, Markewitz BA, Rolfs RT, Brown SM, Dascomb KK. Clinical findings and demographic factors associated with ICU admission in Utah due to novel 2009 influenza A(H1N1) infection. Chest. 2010;137:758. doi: 10.1378/chest.09-2517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Flint SM, Davis JS, Su JY, Oliver-Landry EP, Rogers BA. Disproportionate impact of pandemic (H1N1) 2009 influenza on Indigenous people in the Top End of Australia's Northern Territory. Med J Aust. 2010;192:622. doi: 10.5694/j.1326-5377.2010.tb03654.x. [DOI] [PubMed] [Google Scholar]
- 50.Flint SM, Su JY, Scott L, Krause V. The early experience of pandemic (H1N1) 2009 influenza in Northern Territory, Australia. The Northern Territory Disease Control Bulletin. 2009;16:8. [Google Scholar]
- 51.Cretikos M, Muscatello DJ, Patterson J, Conaty S, Churches T. Progression and impact of the first winter wave of the 2009 pandemic H1N1 influenza in New South Wales, Australia. Euro Surveill 14. 2009. [DOI] [PubMed]
- 52.Scriven J, Mcewen R, Mistry S, Green C, Osman H. Swine flu: a Birmingham experience. Clin Med. 2009;9:538. doi: 10.7861/clinmedicine.9-6-534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Webb SA, Pettila V, Seppelt I, Bellomo R, Bailey M. Critical care services and 2009 H1N1 influenza in Australia and New Zealand. N Engl J Med. 2009;361:1934. doi: 10.1056/NEJMoa0908481. [DOI] [PubMed] [Google Scholar]
- 54.Knight MP. Critical illness with AH1N1v influenza in pregnancy: a comparison of two population-based cohorts. BJOG. 2011;118:239. doi: 10.1111/j.1471-0528.2010.02736.x. [DOI] [PubMed] [Google Scholar]
- 55.Australian and New Zealand Intensive Care (ANZIC) Influenza Investigators. Critical illness due to 2009 A/H1N1 influenza in pregnant and postpartum women: population based cohort study. BMJ. 2010;340:c1279. doi: 10.1136/bmj.c1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Verrall A, Norton K, Rooker S, Dee S, Olsen L. Hospitalizations for pandemic (H1N1) 2009 among Maori and Pacific Islanders, New Zealand. Emerg Infect Dis. 2010;16:102. doi: 10.3201/eid1601.090994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dee S, Jayathissa S. Clinical and epidemiological characteristics of the hospitalised patients due to pandemic H1N1 2009 viral infection: experience at Hutt Hospital, New Zealand. N Z Med J. 2010;123:53. [PubMed] [Google Scholar]
- 58.Sachedina N, Donaldson LJ. Paediatric mortality related to pandemic influenza A H1N1 infection in England: an observational population-based study. Lancet. 2010;376:1852. doi: 10.1016/S0140-6736(10)61195-6. [DOI] [PubMed] [Google Scholar]
- 59.Kelly PM, Kotsimbos T, Reynolds A, Wood-Baker R, Hancox B. FluCAN 2009: initial results from sentinel surveillance for adult influenza and pneumonia in eight Australian hospitals. Med J Aust. 2011;194:174. doi: 10.5694/j.1326-5377.2011.tb03764.x. [DOI] [PubMed] [Google Scholar]
- 60.Chien YS, Su CP, Tsai HT, Huang AS, Lien CE. Predictors and outcomes of respiratory failure among hospitalized pneumonia patients with 2009 H1N1 influenza in Taiwan. J Infect. 2010;60:174. doi: 10.1016/j.jinf.2009.12.012. [DOI] [PubMed] [Google Scholar]
- 61.Subramony H, Lai FY, Ang LW, Cutter JL, Lim PL. An epidemiological study of 1348 cases of pandemic H1N1 influenza admitted to Singapore Hospitals from July to September 2009. Ann Acad Med Singapore. 2010;39:288. [PubMed] [Google Scholar]
- 62.Satterwhite L, Mehta A, Martin GS. Novel findings from the second wave of adult pH1N1 in the United States. Crit Care Med. 2010;38:2061. doi: 10.1097/CCM.0b013e3181eb96dc. [DOI] [PubMed] [Google Scholar]
- 63.Bandaranayake D, Jacobs M, Baker M, Hunt D, Wood T. The second wave of 2009 pandemic influenza A(H1N1) in New Zealand, January-October 2010. Euro Surveillance: Bulletin Europeen sur les Maladies Transmissibles = European Communicable Disease Bulletin 16. 2011. [PubMed]
- 64.Reyes L, Arvelo W, Estevez A, Gray J, Moir JC. Population-based surveillance for 2009 pandemic influenza A (H1N1) virus in Guatemala, 2009. Influenza Other Respi Viruses. 2010;4:140. doi: 10.1111/j.1750-2659.2010.00138.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Louriz M, Mahraoui C, Azzouzi A, El Fassy Fihri MT, Zeggwagh AA. Clinical features of the initial cases of 2009 pandemic influenza A (H1N1) virus infection in an university hospital of Morocco. Int Arch Med 3. 2010;26:7682–3–26. doi: 10.1186/1755-7682-3-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lahlou Amine I, Bajjou T, El Rhaffouli H, Laraqui A, Hilali F. Pandemic influenza A(H1N1)2009 in Morocco: experience of the Mohammed V Military Teaching Hospital, Rabat, 12 June to 24 December 2009. Euro Surveill 16. 2011. [PubMed]
- 67.Jagannatha RaoSR, Rao MJ, Swamy N, Umapathy BL. Profile of H1N1 infection in a tertiary care center. Indian J Pathol Microbiol. 2011;54:325. doi: 10.4103/0377-4929.81618. [DOI] [PubMed] [Google Scholar]
- 68.Chacko J, Gagan B, Ashok E, Radha M, Hemanth HV. Critically ill patients with 2009 H1N1 infection in an Indian ICU. Indian J Crit Care Med. 2010;14:82. doi: 10.4103/0972-5229.68220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Parakh A, Kumar A, Kumar V, Dutta AK, Khare S. Pediatric hospitalizations associated with 2009 pandemic influenza A (H1N1): an experience from a tertiary care center in north India. Indian J Pediatr. 2010;77:985. doi: 10.1007/s12098-010-0168-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ramakrishna K, Peter JV, Karthik G, Abraham AM, Surekha V. Influenza A (H1N1) 2009 pandemic: was there a difference in the two waves in patients requiring admission to the intensive-care unit? Clin Microbiol Infect. 2011;17:1358. doi: 10.1111/j.1469-0691.2011.03584.x. [DOI] [PubMed] [Google Scholar]
- 71.Pramanick A, Rathore S, Peter JV, Moorthy M, Lionel J. Pandemic (H1N1) 2009 virus infection during pregnancy in South India. Int J Gynaecol Obstet. 2011;113:35. doi: 10.1016/j.ijgo.2010.10.025. [DOI] [PubMed] [Google Scholar]
- 72.Puvanalingam A, Rajendiran C, Sivasubramanian K, Ragunanthanan S, Suresh S. Case series study of the clinical profile of H1N1 swine flu influenza. J Assoc Physicians India. 2011;59:16. [PubMed] [Google Scholar]
- 73.Sharma V, Verma PK, Gupta S, Sharma A. Mortality from Influenza A/H1N1 in a tertiary care teaching institution in North India. J Infect Dev Ctries. 2010;4:471. doi: 10.3855/jidc.1007. [DOI] [PubMed] [Google Scholar]
- 74.Chudasama RK, Patel UV, Verma PB, Amin CD, Savaria D. Clinico-epidemiological features of the hospitalized patients with 2009 pandemic influenza A (H1N1) virus infection in Saurashtra region, India (September, 2009 to February, 2010). Lung India. 2011;28:16. doi: 10.4103/0970-2113.76294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Chudasama RK, Patel UV, Verma PB, Fichadiya N, Svariya DR. Pediatric hospitalizations f0r 2009 influenza A (H1N1) in Saurashtra region, India. J Pediatr Sci. 2010;4:e27. [Google Scholar]
- 76.Chudasama RK, Patel UV, Verma PB. Hospitalizations associated with 2009 influenza A (H1N1) and seasonal influenza in Saurashtra region, India. J Infect Dev Ctries. 2010;4:841. doi: 10.3855/jidc.1049. [DOI] [PubMed] [Google Scholar]
- 77.Chudasama RK, Patel UV, Verma PB, Amin CD, Shah MH. Characteristics of Fatal Cases of Pandemic Influenza A (H1N1) from September 2009 to January 2010 in Saurashtra Region, India. Online J Health Allied Scs. 2010;9:9. [Google Scholar]
- 78.Chudasama RK, Verma PB, Amin CD, Gohel B, Savariya D. Correlates of severe disease in patients admitted with 2009 pandemic influenza A (H1N1) infection in Saurashtra region, India. Indian J Crit Care Med. 2010;14:120. doi: 10.4103/0972-5229.74169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Gupta BD, Purohit A. A clinical study of hospitalized H1N1 infected children in Western Rajasthan. J Trop Pediatr. 2011;57:90. doi: 10.1093/tropej/fmq048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Naseem A, Satti S, Khan MA, Saeed W. A clinical account of hospitalized 2009 pandemic influenza A (H1N1) cases. J Coll Physicians Surg Pak. 2011;21:102. [PubMed] [Google Scholar]
- 81.Van Kerkhove MD, Vandemaele KA, Shinde V, Jaramillo-Gutierrez G, Koukounari A. Risk factors for severe outcomes following 2009 influenza A (H1N1) infection: a global pooled analysis. PLoS Med. 2011;8:e1001053. doi: 10.1371/journal.pmed.1001053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Schanzer DL, Langley JM, Tam TW. Influenza-attributed hospitalization rates among pregnant women in Canada 1994–2000. J Obstet Gynaecol Can. 2007;29:629. doi: 10.1016/s1701-2163(16)32559-2. [DOI] [PubMed] [Google Scholar]
- 83.Hancock K, Veguilla V, Lu X, Zhong W, Butler EN. Cross-reactive antibody responses to the 2009 pandemic H1N1 influenza virus. N Engl J Med. 2009;361:1952. doi: 10.1056/NEJMoa0906453. [DOI] [PubMed] [Google Scholar]
- 84.Bhopal R. Glossary of terms relating to ethnicity and race: for reflection and debate. J Epidemiol Community Health. 2004;58:445. doi: 10.1136/jech.2003.013466. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Medline search strategy.
(DOCX)
Methodological quality.
(DOCX)
Confounding variables and meta-analysis results.
(DOCX)
(DOCX)
(DOCX)