Abstract
Musculoskeletal pain is a common reason for patients to seek care from healthcare providers. These conditions are predominantly nontraumatic injuries with a broad differential diagnosis and often without a specific diagnosis despite thorough history and examination. The management of these conditions is often discouraging for patients with continued chronic symptoms despite numerous diagnostic workups and treatment options. Effective communication with respect to the patient's goals is the key to a good outcome. The combination of an accurate diagnosis, an informed, motivated patient and a comprehensive review of the potential treatment options is beneficial for long-term success.
Keywords: differential diagnosis, lower back pain, mechanical low back pain, musculoskeletal diseases, patient care management, rehabilitation outcome, treatment effectiveness
Introduction
Musculoskeletal pain is a very common reason for patients to seek treatment from healthcare providers [Larsson et al. 2009; Walsh et al. 2008]. The musculoskeletal system depends on nerves, muscles and bones to provide function and structure for the body. The system also consists of cartilage, tendons, ligaments and bursa and all of these components can contribute to pain. While a comprehensive review of the evaluation and management of the entirety of conditions is not plausible, an outline of the fundamental management principles is valuable. Often the specific etiology of chronic musculoskeletal pain is unclear in the absence of obvious causes such as fracture, infection, tumor or significant arthritis. These conditions are predominantly nontraumatic with a broad differential diagnosis despite careful history and examination [Gaeta et al. 2008; Schoffl and Schoffl, 2007; O'Connor et al. 1997]. This is discouraging for patients who end up with chronic symptoms of uncertain etiology despite numerous diagnostic workups and conservative and/or interventional treatments [Lillrank, 2003]. These chronic symptoms result in significant utilization of healthcare resources often without meaningful improvement [Von Korff et al. 1988]. This not only affects patients' physical function but also their mental and emotional wellbeing, which contributes to their overall impairment [Foster et al. 2010].
When a person has pain they tend to avoid symptomatic activities but continue to function in order to complete routine necessary tasks such as activities of daily living, recreational and vocational pursuits. In order to accomplish these regular activities, symptomatic areas are protected by relative disuse and compensatory actions are utilized [Kibler, 1990]. This may lead to pain in new locations as well as resulting in some degree of disuse and continued symptoms at the initial injury site. This further complicates the diagnosis and may impede treatment. By the time symptoms are chronic, without a specific diagnosis and refractory to multiple treatment options, both patients and healthcare providers are frustrated. At the initial encounter effective communication with respect to the patient's goals is fundamental to a successful outcome [Matthias et al. 2010; Walsh et al. 2008]. While these goals may vary they tend to fall into two categories: ‘What is wrong?’ and ‘What can be done about it?’. If the patient leaves the encounter without at least meeting these objectives on some level they likely will remain discouraged [Walsh et al. 2008]. While painful musculoskeletal conditions such as tendinitis or bursitis can be thought of as relatively straightforward to evaluate, chronic low back pain provides a useful model for illustrating the management of chronic musculoskeletal pain. Low back pain is a common and expensive condition, estimated to cost US$85 billion in the United States in 1990, with direct medical costs accounting for approximately 20–33% of overall cost, and indirect costs of 67–80% [Cats-Baril, 1991 and Frymoyer, 1991]. This significant cost is for a condition that has a favorable natural history, with approximately 50% of people having resolution of back pain symptoms at 1 week [Carey et al. 1995; Coste et al. 1994], and 80–90% better by 6 weeks [Waddell, 1987]. Information and reassurance are the main reasons that patients consult physicians about back pain [Von Korff and Saunders, 1996; Bush et al. 1993]. Failure to receive an adequate explanation about the basis for spine symptoms is the most frequent reason why patients are dissatisfied with their medical care [Deyo, 1986 and Diehl, 1986].
Diagnosing musculoskeletal pain: Accuracy versus specificity
With chronic nonspecific low back pain, determining the cause of the symptoms (‘What is wrong?’) is the patient's as well as healthcare provider's first logical action in addressing the problem [Kuritzky, 2008]. The primary objective in evaluating a patient with back pain is to rule out concerning or ominous etiologies. A careful history and physical examination combined with an understanding of the relevant anatomy will often lead to the diagnosis [Deyo et al. 1992]. There are specific ‘red flags’ to be aware of that may predict more serious pathology. These include trauma, fever, unexpected weight loss, a history of cancer and neurologic deficits [Deyo et al. 1992]. Imaging or other ancillary studies may be required to further delineate the pathology. Unfortunately it is not uncommon in the presence of chronic pain that these diagnostic tools do not clearly identify the source of pain [Kuritzky, 2008]. Frequently treatment is delayed while a specific diagnosis is pursued. Patients may be relegated to chronic pain medications or the symptoms may be considered the manifestation of poor psychological coping skills [Katon et al. 1982]. It is important to inform patients that progress towards successfully addressing symptoms can be, made whether the evaluation process results in a precise diagnosis or simply rules out significant pathology. The diagnostic categories for chronic musculoskeletal pain can be thought of as serious, specific or nonspecific conditions and appropriate treatment pursued accordingly [Kuritzky, 2008; Walsh et al. 2008]. The pursuit of the diagnosis often starts with uncertainty where these diagnostic categories overlap. This is further clarified with the diagnostic process (Figure 1). To avoid grouping a serious or specific condition into the nonspecific category, continually enhancing knowledge with respect to anatomy, physiology and clinical conditions by re-evaluation is essential.
Figure 1.
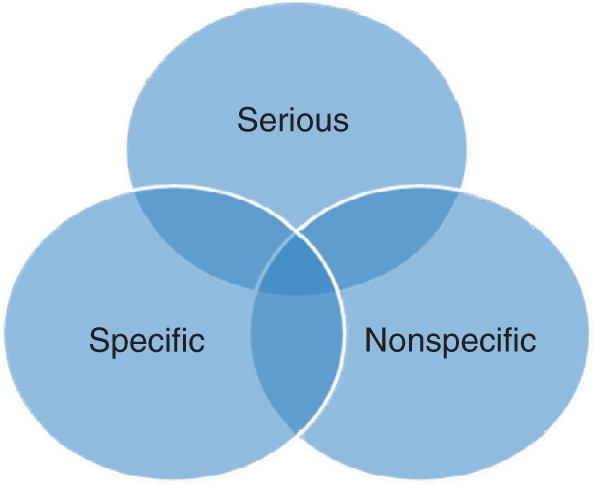
Accurate musculoskeletal diagnosis.
While establishing the diagnosis is the first step in managing persistent musculoskeletal pain, avoid overdiagnosing. An accurate diagnosis is better than an inaccurate, specific diagnosis as patients often focus on their diagnosis as the key to their treatment. While the exact pain generator can often be identified in many musculoskeletal conditions (e.g. lateral epicondylitis), in many other cases the exact pain generator is not identified, such as chronic nonspecific low back pain [Kuritzky, 2008]. In approximately 85% of patients, the exact cause of back pain cannot be identified [Deyo et al. 1992]. Diagnoses such as sacroiliac joint dysfunction, facet arthropathy, discogenic pain or segmental instability/misalignment are frequently employed. While these are potential sources of pain in the low back region, even with diagnostic injections and/or specific imaging modalities these diagnoses have a high degree of uncertainty. Once the patient has a specific diagnosis then treatment plans are focused on that region. Over the long term, this speculation regarding the source of pain may actually hinder recovery for the patient that is not improving as the accuracy of the diagnosis or the efficacy of the treatment will come into question. This is compounded with treatments that provide limited relief of chronic pain [Machado et al. 2009]. When a patient becomes dependent on passive modalities for short-term relief of symptoms this creates a dependency on providers and undermines self reliance. If a patient has been appropriately evaluated, and worrisome causes of back pain have been ruled out, a more accurate, less specific diagnosis such as chronic nonspecific low back pain can provide a platform to treat quantifiable functional deficits such as impaired strength and flexibility as well as reassure the patient.
The history is the first component of an accurate diagnosis. Details such as the relationship of symptoms to activity the frequency of symptoms and the location of symptoms help to focus the diagnosis. A useful and often overlooked tool in obtaining the history is to have the patient localize the area of pain by simply pointing to the symptomatic region. This is similar to having the patient fill out a pain diagram and is recommended at the beginning of the encounter. This technique is most useful when the symptomatic region is focal and is combined with a thorough knowledge of relevant differential diagnoses based on anatomic location of presenting symptoms.
The history should help focus the next component of the diagnosis, the physical examination. Because musculoskeletal symptoms can be the result of orthopedic, neurologic or rheumatologic processes, a comprehensive neuromuscular examination should incorporate a detailed neurologic as well as musculoskeletal examination. The neurologic examination of the extremities should include motor and sensory examination as well as reflexes. Patterns of abnormalities on the neurological examination will assist with the diagnosis. Weakness involving muscles from multiple nerves that all share the same myotome suggest a nerve root injury or radiculopathy, while weakness involving multiple nerve roots and a single nerve suggests a mononeuropathy. Sensory findings will help to confirm the diagnosis, although these patterns of abnormality may not always be reliable. Finally the muscle stretch reflexes and long-tract signs will further localize the lesion. Collateral information obtained with a comprehensive neuromuscular examination will focus the remainder of the exam and workup to other potential causes of chronic nonspecific low back pain (Figure 2). For example, hip osteoarthritis on examination may be characterized by groin and/or low back pain. During the comprehensive neuromuscular examination, if the patient has no neurologic deficits, no lumbar spine tenderness and painless lumbar range of motion this may suggest other etiologies such as hip joint pain and a specific diagnosis-focused examination of the hip is appropriate. A painful passive and active range of motion of the hip joint may suggest arthritis. Bursitis may be diagnosed by inspection, direct palpation, or provocative maneuvers. Combining the knowledge of the potential sources of pain at the primary location of the patient's symptoms with the presence or absence of neurologic findings then allows for focusing the remainder of the examination on specific maneuvers to further clarify the diagnosis.
Figure 2.
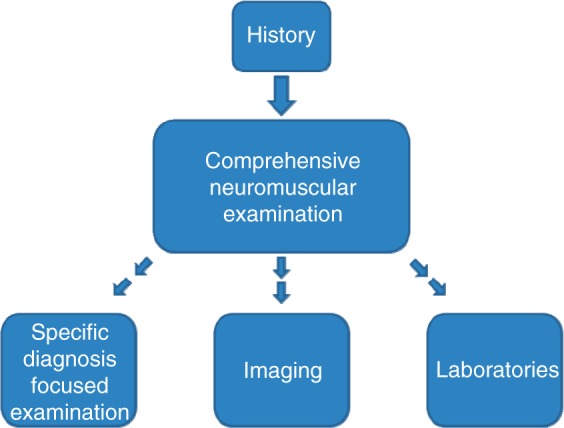
Diagnostic tools.
Further evaluation of persistent musculoskeletal pain with imaging is often necessary. Imaging studies of the lumbosacral spine are beneficial to rule out concerning pathology, but can be problematic in diagnosing the exact cause of pain. This is because in studies of asymptomatic people, normal ‘abnormalities’ are common. In a study of 98 asymptomatic subjects with lumbosacral magnetic resonance imaging (MRI) scans, only 36% had normal discs at all levels, with 52% having bulges, 27% having protrusions, and 1% having an extrusion. Thirty eight percent had abnormalities at more than one level [Jensen et al. 1994]. In a similar study of 67 asymptomatic subjects, lumbosacral MRI scans showed ‘abnormalities’ in 57% of patients older than 60 years of age, and in 35% of patients between 20 and 39 years [Boden et al. 1990]. This is not to say that degenerative spine conditions are not the cause of back pain, but that back pain is multi-factorial, and it is unclear as to whether these asymptomatic findings are predictive of future symptoms. In a study of 148 asymptomatic patients with MRI scans done at baseline and at 3 years, 83% were found to have some degree of disc degeneration at the start of the study. Sixty seven percent developed back and/or leg symptoms over the 3-year period, however annular ligament tears, disc bulges and disc protrusions did not predict future symptoms. Self-described depression was the most important predictor of future pain [Jarvik et al. 2001]. Conversely, not all people with symptoms will have abnormal MRI scans. In a study of 25 patients presenting with clinical findings of acute lumbar radiculopathy, 5 (20%) had normal MRI scans [Modic et al. 1995].
Treating musculoskeletal pain: Narrow the options
The possible treatment options (‘What can be done about it?’) for persistent musculoskeletal pain are finite, not infinite. It can be useful for patient education to classify these options. Treatment options may be grouped into four categories: therapies, medications, injections and surgery (Figure 3). Awareness of these broad concepts by both the patient and provider is useful in order to direct the course of treatment. The recognition that some patients may also have psychological factors associated with chronic pain that may impede recovery is also important [Foster et al. 2010]. While not all patients will require formal psychological evaluations, initiating intervention for those with psychological issues may be as valuable to the overall outcome as other customary treatment options. The patient that is aware of all of the possible management alternatives can then make an informed decision about treatment. It is important at this point that once significant pathology has been ruled out and potential management choices are discussed, the patient actively participates in the treatment decision [Larsson et al. 2009; Walsh et al. 2008]. These patients have typically had multiple treatment trials without success. Simply assigning more treatment is unlikely to result in different outcomes if the patient is not committed to the plan. If a patient is unsure about the course of care, it may be beneficial to have the patient follow up at a later date after considering their alternatives.
Figure 3.

Treatment options.
With nonspecific low back pain, once serious pathology is ruled out, treatment options can be discussed. Medications and injections tend to give short-term relief of symptoms [Roelofs et al. 2008]. These may help patients to progress towards active therapy programs but on their own are unlikely to ‘cure’ chronic pain with a limited course of treatment. Medications for back pain include nonsteroidal anti-inflammatory drugs, muscle relaxants, nonnarcotic analgesics (acetaminophen) and narcotics. Acetominophen and nonsteroidal anti-inflammatory drugs are often helpful for acute back pain. Muscle relaxants and narcotics can be of benefit, but should be prescribed for fixed periods. Medication treatment for chronic back pain is less clear and more controversial [Deyo, 1996]. Cyclooxygenase-2 inhibitors have fewer side effects compared with other nonsteroidal anti-inflammatory drugs, however there are concerns about increased cardiovascular risks. No specific nonsteroidal anti-inflammatory drug appears to be any more effective than another [Roelofs et al. 2008]. Spinal injections can be useful for both diagnostic and therapeutic purposes. However, unless they provide several months of pain relief, they may not be a feasible option for the long-term management of symptoms.
In some cases surgery for the appropriate diagnosis may be the optimum treatment. For the majority of chronic musculoskeletal conditions invasive procedures are the last resort when all other conservative treatments have failed. Indications for surgery are relative or absolute. Pain refractory to conservative or minimally invasive options is a relative indication for surgery, with the patient deciding that pain and/or quality of life issues necessitate surgical evaluation. Progressive neurologic deficits (strength or sensation deficits) or bowel or bladder dysfunction are urgent conditions and absolute indications for surgical evaluation. The most common mode of treatment for the majority of patients with low back pain is conservative treatment.
Therapies are the largest of the treatment choices and for the purpose of this discussion are used to describe all of the options that are not medications, injections or surgeries. Therapies can be thought of as passive or active. The experience of many patients is that the passive treatments such as ultrasound, ice, electrical stimulation, massage and bed rest provide short-term relief but do not alleviate chronic musculoskeletal symptoms over the long term [Hartigan et al. 1996].
Bedrest is a commonly prescribed conservative treatment for acute low back pain. However, with bedrest, patients get weaker, stiffer and deconditioned. Studies of bedrest have shown that shorter periods of bedrest (0 or 2 days compared with 4 or 7 days) are associated with fewer days of decreased activity, fewer lost workdays, and no difference in pain [Deyo et al. 1986; Gilbert et al. 1985]. Alternative treatments such as manipulation, massage and acupuncture can be useful for short-term pain relief, however these treatments usually do not result in long-term resolution of symptoms. Spinal manipulation has been shown to be helpful early in the course of acute back pain, usually within the first 2–4 weeks [MacDonald, 1990 and Bell, 1990; Hadler et al. 1987]. Passive modalities such as ultrasound and transcutaneous electrical nerve stimulation (TENS) have been shown to have no effect on pain or disability compared with usual care or placebo TENS [Herman et al. 1994; Faas et al. 1993].
Active therapy refers to exercise. Chronic musculoskeletal pain can lead to strength and flexibility limitations that result in further symptoms [Kibler et al. 1992]. No passive treatment will make a weak muscle strong. Restoring strength and flexibility to muscle groups can have limited success if the patient is deconditioned, so incorporating an aerobic exercise program is also valuable [Rainville et al. 1997; Hartigan et al. 1996]. Initially exercise focused on the region of chronic pain may increase the symptoms but will often lead to improved function [Ettinger et al. 1997; Rainville et al. 1992]. Realistic expectations are also necessary. If pain has been persistent for years and patients have altered their activities to accommodate their symptoms, restoring strength, flexibility and endurance will take months (not weeks) of daily (not weekly) active exercise.
Exercise is the mainstay of treatment for most benign, nonspecific back pain, because exercise addresses both the physiological as well as the psychosocial impacts of back pain. While it is beyond the scope of this paper to provide a comprehensive review of the literature with respect to the treatment options for nonspecific low back pain, there are multiple systematic reviews that support exercise as a reasonable approach for chronic spine pain [Choi et al. 2010; Dahm et al. 2010; Hayden et al. 2005]. Exercise can improve muscle strength, endurance and flexibility. Exercise also promotes appropriate health beliefs and active coping strategies, disrupts fear avoidance behaviors, enhances self efficacy, and reduces helplessness and social isolation. These psychosocial benefits of exercise can be as important as the physiological benefits [Hurley et al. 2003]. To understand the rationale for exercise as an optimal treatment option for back pain, it is important to understand the biomedical versus the biopsychosocial model of osteoarthritis because degenerative spine conditions are similar to osteoarthritis. The biomedical model of osteoarthritis states that there are pathological characteristics of osteoarthritis (loss of articular cartilage, osteophyte formation and synovitis) that impair normal anatomic function (restricted range of motion and muscle atrophy), leading to pain and disability, and further physiological impairments (decreased strength, endurance and joint stability) [Hurley et al. 2003]. The biopsychosocial model of osteoarthritis states that while there are pathological characteristics of osteoarthritis that may be perceived as pain, pain behavior and disability is a product of beliefs, understandings, experiences and emotions that may be modulated by the social environment. These psychosocial impacts of osteoarthritis are ill-health beliefs, helplessness, decreased self efficacy, passive coping strategies and inadequate social support [Hurley et al. 2003]. The biomedical model does not adequately explain why some people with severe radiographic evidence of spondylosis have minimal pain, and why some people with minimal radiographic evidence of spondylosis have severe pain. The biopsychosocial model better explains the weak association between joint damage, pain and disability, and why some people react differently to the same intervention [Hurley et al. 2003].
Exercise is supported as an intervention for acute, subacute and chronic low back pain. When considering studies of spine conditions, pain is often classified as acute (0–6 weeks' duration), subacute (6–12 weeks' duration) and chronic (greater than 12 weeks' duration). A randomized controlled trial of patients with acute low back pain compared bed rest with physical therapy programs and advice for the resumption of ordinary physical activity. The ordinary activity group had favorable pain, work and disability outcomes at 3 and 12 weeks [Malmivaara et al. 1995]. Another randomized controlled trial of patients with acute low back pain compared traditional passive physical therapy with a gradually progressive exercise program incorporating resistance training. The exercise group had increased strength and returned to work quicker compared with the traditional physical therapy group [Lindstrom et al. 1992].
A randomized controlled trial of patients with subacute low back pain compared passive, traditional physical therapy with advice to return to normal activities. Patients were advised to avoid illness behaviors, and not to be fearful about activities. The advice group had less work disability at 1 year [Indahl et al. 1995]. In an observation of cohorts, patients with subacute low back pain were given a 3–6-week intervention of intense, active exercise compared with passive, traditional therapy. The exercise group returned to work quicker resulting in a lower cost at 1 year than the traditional therapy group [Mitchell, 1990 and Carmen, 1990].
In a randomized controlled trial of chronic low back pain, patients were randomized to an exercise program versus a traditional back school. The exercise program involved progressive strengthening and stretching activities. The exercise group had decreased disability and pain compared with the traditional treatment group [Frost et al. 1995]. There have been a number of observational trials of progressive exercise programs in patients with chronic low back pain. Overall these demonstrate that aggressive exercise programs that identify and address impairments in lumbosacral strength and flexibility result in improved spinal function, improved activities of daily living, and decreased pain [Nelson et al. 1995; Rainville et al. 1992; Estlander et al. 1991; Manniche et al. 1991; Hazard et al. 1989; Mayer et al. 1987].
For patients with acute back pain, it may be enough to encourage them to resume daily activities as early as possible. Advice may be a powerful tool that the clinician can use to treat patients with low back pain. Most patients will understand that a strong, flexible back will feel better than a stiff, deconditioned back. Advice should focus on enabling the patient to resume normal activities. Concentrating on pain may have a deleterious effect. A prospective study comparing patients with ankle sprain and cervical strain assessed neurologic and musculoskeletal exams at 1 week, and at 3, 6 and 12 months. Both groups were asked to rate their upper body pain. Patients with ankle sprain had increased complaints of neck and back pain. The authors concluded that paying attention to a particular body region could have a pain-eliciting effect [Kasch et al. 2003]. Another study compared a control back pain pamphlet with an experimental pamphlet. The control pamphlet had traditional, disabling advice (the spine is easily damaged, often damage is permanent, avoid activity and be passive, focus on pain). The experimental pamphlet had enabling advice (the spine is strong and rarely damaged, back pain rarely represents serious disease, pain does not mean harm, activity is important to recovery, focus on function). Patients with acute or recurrent low back pain were randomized to receive the control or experimental pamphlet. Outcomes were assessed at 2 weeks, 3 months and 1 year. There were no change in pain scores, but the experimental pamphlet group had a positive shift in pain and activity beliefs, and had lower self-reported disability [Burton et al. 1999]. Cognitive behavioral therapy employing behavior and goal-oriented psychological treatment has also been shown to be effective for subacute and chronic low back pain [Lamb et al. 2010].
Conclusions
Persistent musculoskeletal pain syndromes can be a challenge to treat because the source of the symptoms may not be readily identifiable. Although many of the potential sources of musculoskeletal pain may not be identified with imaging studies, the lack of findings does not imply that the symptoms are not associated with a specific diagnosis. Alternatively, while examination and imaging may in fact pinpoint the diagnosis, it is important to educate the patient that the primary goal of these studies is often to evaluate and rule out other significant pathology [Walsh et al. 2008]. Appropriate care is best achieved with the combination of an accurate diagnosis and an informed, motivated patient [Stephens and Gross, 2007]. When the patient and the healthcare provider are reassured that there is not a serious, worrisome problem then the potential treatment options can be reviewed. These include conservative options (medications, physical therapy, exercise, etc.), minimally invasive options (spinal injections) and surgical options. Informing the patient of their alternatives and allowing the patient not only to take an active part in treatment decisions but also to be the principal director of their care is vital to long-term success.
Footnotes
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
The authors declare that there is no conflict of interest.
References
- Boden S.D., Davis D.O., Dina T.S., Patronas N.J., Wiesel S.W. (1990) Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Amer 72: 403–408 [PubMed] [Google Scholar]
- Burton A.K., Waddell G., Tillotson K.M., Summerton N. (1999) Information and advice to patients with back pain can have a positive effect. A randomized controlled trial of a novel educational booklet in primary care. Spine 24: 2484–2491 [DOI] [PubMed] [Google Scholar]
- Bush T., Cherkin D., Barlow W. (1993) The impact of physician attitudes on patient satisfaction with care for low back pain. Arch Fam Med 2: 301–305 [DOI] [PubMed] [Google Scholar]
- Carey T.S., Garrett J., Jackman A., McLaughlin C., Fryer J., Smucker D.R. (1995) The outcomes and costs of care for acute low back pain among patients seen by primary care practitioners, chiropractors, and orthopedic surgeons. The North Carolina back pain project. New Eng J Med 333: 913–917 [DOI] [PubMed] [Google Scholar]
- Cats-Baril W.L., Frymoyer J.W. (1991) The economics of spinal disorders, In: Frymoyer J.W. (ed.). The Adult Spine: Principles and Practice, Raven Press: New York [Google Scholar]
- Choi B.K.L., Verbeek J.H., Tam W.W., Jiang J.Y. (2010) Exercises for prevention of recurrences of low-back pain. Cochrane Database Syst Rev 1, CD00655 DOI:10.1002/14651858.CD006555.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coste J., Delecoeuillerie G., de Lara A. Cohen, Le Parc J.M., Paolaggi J.B. (1994) Clinical course and prognostic factors in acute low back pain: An inception cohort study in primary care practice. BMJ 308: 577–580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahm K.T., Jamtvedt G., Hagen K.B. (2010) Advice to rest in bed versus advice to stay active for acute low-back pain and sciatica. Cochrane Database Syst Rev 6: CD007612. [DOI] [PubMed] [Google Scholar]
- Deyo R.A. (1996) Drug therapy for back pain Which drugs help which patients? Spine 21: 2840–2849 [DOI] [PubMed] [Google Scholar]
- Deyo R.A., Diehl A.K. (1986) Patient satisfaction with medical care for low-back pain. Spine 11: 28–30 [DOI] [PubMed] [Google Scholar]
- Deyo R.A., Diehl A.K., Rosenthal M. (1986) How many days of bed rest for acute low back pain? A randomized clinical trial. New Eng J Med 315: 1064–1070 [DOI] [PubMed] [Google Scholar]
- Deyo R.A., Rainville J., Kent D.L. (1992) What can the history and physical examination tell us about low back pain? JAMA 268: 760–765 [PubMed] [Google Scholar]
- Estlander A.M., Mellin G., Vanharanta H., Hupli M. (1991) Effects and follow-up of a multi-modal treatment program including intensive physical training for low back pain patients. Scand J Rehabil Med 23: 97–102 [PubMed] [Google Scholar]
- Ettinger W.H., Jr., Burns R., Messier S.P., Applegate W., Rejeski W.J., Morgan T., et al. (1997) A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis. The fitness arthritis and seniors trial (FAST). JAMA 277: 25–31 [PubMed] [Google Scholar]
- Faas A., Chavannes A.W., van Eijk J.T., Gubbels J.W. (1993) A randomized, placebo-controlled trial of exercise therapy in patients with acute low back pain. Spine 18: 1388–1395 [PubMed] [Google Scholar]
- Foster N.E., Thomas E., Bishop A., Dunn K.M., Main C.J. (2010) Distinctiveness of psychological obstacles to recovery in low back pain patients in primary care. Pain 148: 398–406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frost H., Klaber Moffett J.A., Moser J.S., Fairbank J.C. (1995) Randomised controlled trial for evaluation of fitness programme for patients with chronic low back pain. Br Med J 310: 151–154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaeta M., Minutoli F., Mazziotti S., Visalli C., Vinci S., Gaeta F., et al. (2008) Diagnostic imaging in athletes with chronic lower leg pain. Am J Roentgenol 191: 1412–1419 [DOI] [PubMed] [Google Scholar]
- Gilbert J.R., Taylor D.W., Hildebrand A., Evans C. (1985) Clinical trial of common treatments for low back pain in family practice. Br Med J (Clin Res Ed) 291: 791–794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadler N.M., Curtis P., Gillings D.B., Stinnett S. (1987) A benefit of spinal manipulation as adjunctive therapy for acute low-back pain: A stratified controlled trial. Spine 12: 702–706 [PubMed] [Google Scholar]
- Hartigan C., Miller L., Liewehr S.C. (1996) Rehabilitation of acute and subacute low back and neck pain in the work-injured patient. Orthop Clin North Am 27: 841–860 [PubMed] [Google Scholar]
- Hayden J., van Tulder M.W., Malmivaara A., Koes B.W. (2005) Exercise therapy for treatment of non-specific low back pain. Cochrane Database Syst Rev (3): CD000335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hazard R.G., Fenwick J.W., Kalisch S.M., Redmond J., Reeves V., Reid S., et al. (1989) Functional restoration with behavioral support. A one-year prospective study of patients with chronic low-back pain. Spine 14: 157–161 [PubMed] [Google Scholar]
- Herman E., Williams R., Stratford P., Fargas-Babjak A., Trott M. (1994) A randomized controlled trial of transcutaneous electrical nerve stimulation (CODETRON) to determine its benefits in a rehabilitation program for acute occupational low back pain. Spine 19: 561–568 [DOI] [PubMed] [Google Scholar]
- Hurley M.V., Mitchell H.L., Walsh N. (2003) In osteoarthritis, the psychosocial benefits of exercise are as important as physiological improvements. Exerc Sport Sci Rev 31: 138–143 [DOI] [PubMed] [Google Scholar]
- Indahl A., Velund L., Reikeraas O. (1995) Good prognosis for low back pain when left untampered. A randomized clinical trial. Spine 20: 473–477 [DOI] [PubMed] [Google Scholar]
- Jarvik J.J., Hollingworth W., Heagerty P., Haynor D.R., Deyo R.A. (2001) The longitudinal assessment of imaging and disability of the back (LAIDBack) study: Baseline data. Spine 26: 1158–1166 [DOI] [PubMed] [Google Scholar]
- Jensen M.C., Brant-Zawadzki M.N., Obuchowski N., Modic M.T., Malkasian D., Ross J.S. (1994) Magnetic resonance imaging of the lumbar spine in people without back pain. New Eng J Med 331: 69–73 [DOI] [PubMed] [Google Scholar]
- Kasch H., Bach F.W., Stengaard-Pedersen K., Jensen T.S. (2003) Development in pain and neurologic complaints after whiplash: A 1-year prospective study. Neurology 60: 743–749 [DOI] [PubMed] [Google Scholar]
- Katon W., Kleinman A., Rosen G. (1982) Depression and somatization: A review. Part I. Am J Med 72: 127–135 [DOI] [PubMed] [Google Scholar]
- Kibler W.B. (1990) Clinical aspects of muscle injury. Med Sci Sports Exerc 22: 450–452 [PubMed] [Google Scholar]
- Kibler W.B., Chandler T.J., Stracener E.S. (1992) Musculoskeletal adaptations and injuries due to overtraining. Exerc Sport Sci Rev 20: 99–126 [PubMed] [Google Scholar]
- Kuritzky L. (2008) Current management of acute musculoskeletal pain in the ambulatory care setting. Am J Ther 15: S7–S11 [DOI] [PubMed] [Google Scholar]
- Lamb S.E., Hansen Z., Lall R., Castelnuovo E., Withers E., Nichols V., et al. (2010) Group cognitive behavioral treatment for low-back pain in primary care: A randomized controlled trial and cost-effectiveness analysis. Lancet 375: 916–923 [DOI] [PubMed] [Google Scholar]
- Larsson M.E., Nordholm L.A., Ohrn I. (2009) Patients’ views on responsibility for the management of musculoskeletal disorders — a qualitative study. BMC Musculoskelet Disord 10: 103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lillrank A. (2003) Back pain and the resolution of diagnostic uncertainty in illness narratives. Soc Sci Med 57: 1045–1054 [DOI] [PubMed] [Google Scholar]
- Lindstrom I., Ohlund C., Eek C., Wallin L., Peterson L.E., Nachemson A. (1992) Mobility, strength, and fitness after a graded activity program for patients with subacute low back pain. A randomized prospective clinical study with a behavioral therapy approach. Spine 17: 641–652 [DOI] [PubMed] [Google Scholar]
- MacDonald R.S., Bell C.M. (1990) An open controlled assessment of osteopathic manipulation in nonspecific low-back pain. Spine 15: 364–370 [DOI] [PubMed] [Google Scholar]
- Machado L.A., Kamper S.J., Herbert R.D., Maher C.G., McAuley J.H. (2009) Analgesic effects of treatments for non-specific low back pain: A meta-analysis of placebo-controlled randomized trials. Rheumatology 48: 520–527 [DOI] [PubMed] [Google Scholar]
- Malmivaara A., Hakkinen U., Aro T., Heinrichs M.L., Koskenniemi L., Kuosma E., et al. (1995) The treatment of acute low back pain — bed rest, exercises, or ordinary activity? New Eng J Med 332: 351–355 [DOI] [PubMed] [Google Scholar]
- Manniche C., Lundberg E., Christensen I., Bentzen L., Hesselsoe G. (1991) Intensive dynamic back exercises for chronic low back pain: A clinical trial. Pain 47: 53–63 [DOI] [PubMed] [Google Scholar]
- Matthias M.S., Bair M.J., Nyland K.A., Huffman M.A., Stubbs D.L., Damush T.M., et al. (2010) Self-management support and communication from nurse care managers compared with primary care physicians: A focus group study of patients with chronic musculoskeletal pain. Pain Management Nursing 11: 26–34 [DOI] [PubMed] [Google Scholar]
- Mayer T.G., Gatchel R.J., Mayer H., Kishino N.D., Keeley J., Mooney V. (1987) A prospective two-year study of functional restoration in industrial low back injury. An objective assessment procedure. JAMA 258: 1763–1767 [PubMed] [Google Scholar]
- Mitchell R.I., Carmen G.M. (1990) Results of a multicenter trial using an intensive active exercise program for the treatment of acute soft tissue and back injuries. Spine 15: 514–521 [DOI] [PubMed] [Google Scholar]
- Modic M.T., Ross J.S., Obuchowski N.A., Browning K.H., Cianflocco A.J., Mazanec D.J. (1995) Contrast-enhanced MR imaging in acute lumbar radiculopathy: A pilot study of the natural history. Radiology 195: 429–435 [DOI] [PubMed] [Google Scholar]
- Nelson B.W., O'Reilly E., Miller M., Hogan M., Wegner J.A., Kelly C. (1995) The clinical effects of intensive, specific exercise on chronic low back pain: A controlled study of 895 consecutive patients with 1-year follow up. Orthopedics 18: 971–981 [DOI] [PubMed] [Google Scholar]
- O'Connor F.G., Howard T.M., Fieseler C.M., Nirschl R.P. (1997) Managing overuse injuries: A systematic approach. Phys Sports Med 25: 88–113 [DOI] [PubMed] [Google Scholar]
- Rainville J., Ahern D.K., Phalen L., Childs L.A., Sutherland R. (1992) The association of pain with physical activities in chronic low back pain. Spine 17: 1060–1064 [DOI] [PubMed] [Google Scholar]
- Rainville J., Sobel J., Hartigan C., Monlux G., Bean J. (1997) Decreasing disability in chronic back pain through aggressive spine rehabilitation. J Rehabil Res Dev 34: 383–393 [PubMed] [Google Scholar]
- Roelofs P.D., Deyo R.A., Koes B.W., Scholten R.J., van Tulder M.W. (2008) Nonsteroidal anti-inflammatory drugs for low back pain: An updated Cochrane review. Spine 33: 1766–1774 [DOI] [PubMed] [Google Scholar]
- Schoffl V.R., Schoffl I. (2007) Finger pain in rock climbers: Reaching the right differential diagnosis and therapy. J Sports Med Phys Fitness 47: 70–78 [PubMed] [Google Scholar]
- Stephens B., Gross D.P. (2007) The influence of a continuum of care model on the rehabilitation of compensation claimants with soft tissue disorders. Spine 32: 2898–2904 [DOI] [PubMed] [Google Scholar]
- Von Korff M., Dworkin S.F., Le Resche L., Kruger A. (1988) An epidemiologic comparison of pain complaints. Pain 32: 173–183 [DOI] [PubMed] [Google Scholar]
- Von Korff M., Saunders K. (1996) The course of back pain in primary care. Spine 21: 2833–2837 [DOI] [PubMed] [Google Scholar]
- Waddell G. (1987) 1987 Volvo award in clinical sciences. A new clinical model for the treatment of low-back pain. Spine 12: 632–644 [DOI] [PubMed] [Google Scholar]
- Walsh N.E., Brooks P., Hazes J.M., Walsh R.M., Dreinhofer K., Woolf A.D., et al. (2008) Standards of care for acute and chronic musculoskeletal pain: The bone and joint decade (2000–2010). Arch Phys Med Rehabil 89: 1830–1845 [DOI] [PubMed] [Google Scholar]


