Abstract
The relatively low frequencies of tumor Ag-specific T-cells in PBMC and metastases from cancer patients have long precluded the analysis of their direct ex vivo cytolytic capacity. Using a new composite technique that works well with low cell numbers, we aimed at determining the functional competence of melanoma-specific CD8+ T-cells. A multiparameter flow cytometry based technique was applied to assess the cytolytic function, degranulation and IFNγ production by tumor Ag-specific CD8+ T-cells from PBMC and tumor-infiltrated lymph nodes (TILN) of melanoma patients. We found strong cytotoxicity by T-cells not only when they were isolated from PBMC but also from TILN. Cytotoxicity was observed against peptide-pulsed target cells and melanoma cells presenting the naturally processed endogenous antigen. However, unlike their PBMC-derived counterparts, T-cells from TILN produced only minimal amounts of IFNγ, while exhibiting similar levels of degranulation, revealing a critical functional dichotomy in metastatic lesions. Our finding of partial functional impairment fits well with the current knowledge that T-cells from cancer metastases are so-called exhausted, a state of T-cell hyporesponsiveness also found in chronic viral infections. The identification of responsible mechanisms in the tumor microenvironment is important for improving cancer therapies.
Keywords: Degranulation, cytotoxicity, exhaustion, human tumour immunology, interferon gamma
Introduction
A central issue in tumor immunology is that tumor cells do not express foreign antigens and are therefore not readily fought against by the immune system. Additionally, cancer cells have proven to be experts in immune evasion, making use of a wide repertoire of strategies to elude its adversaries. Nevertheless, tumor Ag-specific T-cells can be readily detected in PBMC of cancer patients, and it has been shown that such T-cells can play a significant role in delaying tumor progression or even eliminate cancer cells in murine model systems,1,2 as well as in cancer patients.3
Ag-specific reactivity is typically demonstrated by IFNγ ELISPOT assays.4 PBMC-derived tumor Ag-specific T-cells have been shown to secrete IFNγ in an Ag-specific manner.5-7 Solid tumors of peripheral tissues are infiltrated with tumor Ag-specific T-cells, and in tumor-infiltrated lymph nodes (TILN; also referred to as metastases hereafter) the tumor cells are also surrounded by immune cells that could potentially attack them. However, it has previously been reported that tumor Ag-specific CD8+ T-cells from melanoma metastases show impaired IFNγ production directly ex vivo, indicating a functional defect or inhibition at the tumor site.5,7,8 Importantly, IFNγ production is not necessarily representative for other functions of CD8+ T-cells. While IFNγ production was strongly impaired, we found that Perforin production was only marginally reduced and Granzyme B content appeared normal in Ag-specific T-cells from melanoma metastases.5,9 Based on these findings, we were interested in the ex vivo cytolytic capacity of tumor-specific CD8+ T-cells from cancer patients, as the lysis of tumor cells is important for successful tumor defense.
Target cell lysis can be achieved through different mechanisms: (1) release of lytic granule contents (Granzymes, Perforin and Granulysin), (2) cell-cell contact (Fas/FasL) and (3) cross-linking of death-receptors (TNFα/TNFRα Type I).10 Since a large proportion of Melan-A (also known as MART-1) specific CD8+ T-cells from melanoma patients express Perforin and Granzyme B,11 we hypothesized that their lytic activity would be mainly granule-dependent. Upon granule exocytosis, the lysosomal-membrane associated glycoprotein CD107a (also known as LAMP-1) is transferred to the plasma membrane. Cell surface detection of CD107a therefore serves as a read-out for granule exocytosis, and it is closely,12,13 though not absolutely,14 linked to lytic activity.
Hence, to further investigate the ex vivo functionality of tumor-specific CD8+ T-cells as well as the apparent functional impairment of TILN-derived cells, we assessed the ex vivo lytic capacity, degranulation and IFNγ production of Melan-A-specific CD8+ T-cells from PBMC and TILN of melanoma patients. To this end, we made use of our multiparameter LiveCount Assay (LCA),15 which was slightly modified (mLCA) to allow the concomitant analysis of lytic activity and surface CD107a, as in the original protocol, as well as intracellular IFNγ. In addition to detecting IFNγ production on a per cell basis, the mLCA does not require pre-purification of Ag-specific cells, thus reducing procedure-related potential influences on their viability and/or functionality.
While circulating T-cells showed strong cytolytic capacity, degranulation and IFNγ production, the results indicate a partial inhibition of T-cell functions at the tumor site, underlining that T-cells sampled from the PBMC do not always reflect functionality at the site of disease. Interestingly, the T-cells from metastases showed considerable lytic activity.
Results
Direct ex vivo cytotoxicity by Melan-A-specific CD8+ T-cells from PBMC or TILN of vaccinated melanoma patients
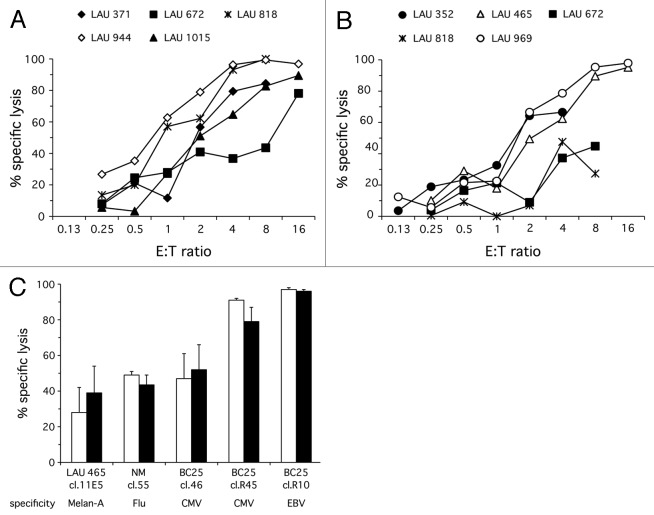
Melan-A-specific T-cells were isolated from five PBMC and five TILN samples and tested by ex vivo LCA in triplicates. These T-cells showed strong cytolytic function ex vivo. Though TILN-derived T-cells exhibited lower levels of cytolytic activity than those derived from PBMC (Fig. 1A and B), the difference was not statistically significant. Efficient cytotoxicity by TILN-derived T-cells was remarkable, given previous reports showing hypo-responsiveness of T-cells in metastases.5,7,8,16 In parallel to the assessment of primary T-cells, we also used a Melan-A-specific CTL clone (clone R11) in each experiment in order to assess inter-assay variability. The clone was consistently used 13 to 16 d after the periodic re-stimulation with PHA, such that the clone was always at a similarly high activation state. Indeed, results from clone R11 revealed favorable assay reproducibility (data not shown). In summary, these results show a surprisingly strong and consistent lysis of peptide-pulsed T2 cells by tumor Ag-specific T-cells isolated directly from the patients’ PBMC or TILN, comparable to the lytic activity of a CTL clone with strong cytolytic function.
Figure 1. Melan-A-specific T-cells from both PBMC and TILN of melanoma patients exert strong cytotoxicity directly ex vivo. Melan-A-specific CD8+ T-cells were FACS purified from PBMC [(A); n = 5] and TILN [(B); n = 5] of melanoma patients using pMHC multimers, and incubated for 4 h with an equal number of Melan-A-pulsed T2CMTMR-lo and HIV-pulsed T2CMTMR-hi at the indicated E:T ratios. All conditions were measured in triplicates. A semi-paired permutation test yielded no statistically significant difference between the cytolytic capacity of cells from PBMC and TILN (p = 0.2). (C) Pre-incubation with pMHC multimers does not significantly affect the lytic activity of CD8+ CTL clones. CTL clones specific for either Melan-A, Flu, CMV or EBV were left untreated (white bars) or incubated with relevant pMHC multimers (black bars) prior to incubating them for 4 h with an equal number of relevant-peptide-pulsed T2CMTMR-lo and irrelevant-peptide-pulsed T2CMTMR-hi. E:T = 4 was used for all clones except NM cl.55, which was assayed at E:T = 1. Mean cytolytic activity and SD of quadruplicates are shown for each clone. A paired, two-tailed t-test showed no difference between pMHC multimer treated or untreated cells (p = 0.94).
The modified LiveCount Assay (mLCA) and original LCA provide comparable results
It could be argued that the vigorous cytotoxicity of patients’ T-cells was due to TCR triggering by peptide/MHC (pMHC) multimers used for their sorting by flow cytometry. To address this possibility, we tested CTL clones of different specificities and found similar levels of cytotoxicity, whether they were pre-incubated with pMHC multimers or not (Fig. 1C). Regardless, sorting by flow cytometry may alter cell viability and lytic performance in primary cells.15 Therefore, we optimised our assay to circumvent prior labeling and sorting of T-cells. This modified LiveCount Assay (mLCA) was validated with CTL clone R11 and produced similar titration curves in terms of specific lysis and CD107a upregulation as the original LCA (data not shown). Characteristics and differences of the two assays are listed in a table (Table S1, which demonstrates the differences between LCA and mLCA). The mLCA was then applied to assess the ex vivo cytotoxicity of Melan-A-specific T-cells from PBMC of three melanoma patients (Fig. 2A). Efficient cytotoxicity was detected, with E:T titration curves comparable to those obtained with the original LCA (Fig. 1A). Thus, considerable cytotoxicity was detected ex vivo, even without prior pMHC multimer based T-cell sorting.
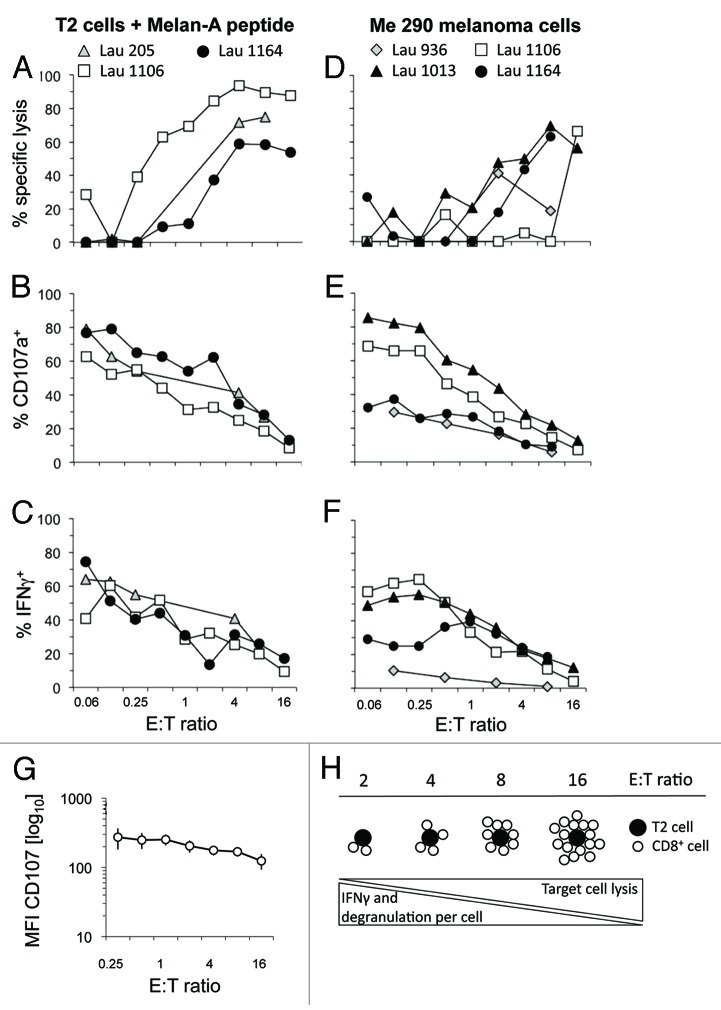
Figure 2. The modified LiveCount Assay (mLCA) allows to simultaneously determine cytotoxicity, degranulation and IFNγ production. CD8+ T-cells magnetically enriched from PBMC of melanoma patients were incubated with peptide-pulsed T2 target cells (A–C) or the endogenously Melan-A+ melanoma cell line Me 290 (D–F) at the indicated E:T ratios in the presence of fluorescently conjugated CD107a mAb. Brefeldin A was added after 1 h of co-incubation. After a further 3 h of co-incubation, cells were incubated with Melan-A/HLA-A2*0201 multimers, CD8 mAb, ViViD and, following fixation and permeabilisation, IFNγ mAb. (A and D) % specific lysis. (B and E) Degranulation as measured by CD107a upregulation on the cell surface. (C and F) IFNγ production. Results for peptide-loaded T2 and Me 290 melanoma target cells were compared using a semi-paired permutation test, yielding p values of 0.007 (lysis), 0.34 (CD107a upregulation) and 0.50 (IFNγ expression). (G) Mean fluorescence intensity (MFI) of cell surface CD107a staining at increasing E:T ratios with peptide-loaded T2 as target cells. The graph shows mean ± SEM of 5 PBMC and 5 TILN samples. (H) The scheme illustrates that CD107a and cytokine expression is reduced on a per cell basis in conditions of limited availability of specific target cells, while the overall specific lysis is increased.
Enhanced activation of Melan-A-specific CD8+ T-cells at low E:T ratios
In addition to the simultaneous assessment of cytotoxicity and degranulation, the mLCA allows to detect cytokine-producing cells (Fig. 2C and F), hence providing a more comprehensive evaluation of T-cell function. Although lysis was not detectable at low E:T ratios, the majority of Melan-A-specific T-cells degranulated under such conditions, with a mean of about 70% at E:T = 0.06 (Fig. 2B). With increasing E:T ratios, frequencies of CD107a+ cells decreased to values as low as 11% at E:T = 16. The proportion of IFNγ+ T-cells mirrored this observation. At E:T = 0.06, an average of 51% of Melan-A-specific T-cells were IFNγ+, but only a mean of 12% produced IFNγ at E:T = 16 (Fig. 2C). Similarly, the mean fluorescence intensity of cell surface CD107a detection, reflecting the average molecular density of this molecule per cell, decreased with increasing E:T ratios and increasing lysis (Fig. 2G). This suggests that at elevated E:T ratios, the cells that are participating in killing do not degranulate as much on a per-cell basis as seen at lower E:T ratios (Fig. 2H). Together, our data demonstrate that the majority of Melan-A-specific T-cells are potentially functional, and that different functions are revealed at different E:T ratios. Since cytotoxicity is measured as the result of a collective T-cell action and not on a per T-cell basis, degranulation and IFNγ production are more accurate measurements of activation of individual T-cells.
Successful recognition and killing of melanoma cells
To test the ability of Melan-A-specific T-cells to recognize melanoma cells based on their endogenous production and presentation of antigen, we compared the T-cell functions generated in response to Melan-A+ (Me 290) and Melan-A− (NA8-MEL) melanoma cell lines. Melan-A-specific T-cells directly isolated from PBMC of melanoma patients were able to lyse melanoma cells (Fig. 2D). Successful recognition of melanoma cells in the absence of synthetic peptide was also demonstrated by the T-cells’ ability to degranulate and produce IFNγ (Fig. 2E and F). However, lysis of unpulsed melanoma cells (Fig. 2D) was often less efficient than lysis of peptide-pulsed T2 cells (Fig. 2A), presumably due to lower levels of peptide being presented by tumor cells. This was not statistically significant (p = 0.08) if taking only mLCA data into account, probably due to low sample numbers, but did reach statistical significance when integrating the LCA data from Figure 1A (p = 0.007). Strikingly, stimulating with Me 290 revealed different response patterns generated by PBMC from different patients. While some delivered strong (LAU 1013) or weak (LAU 936) responses in all three parameters analyzed, others showed strong lysis with weak degranulation and IFNγ production (LAU 1164) or vice versa (LAU 1106).
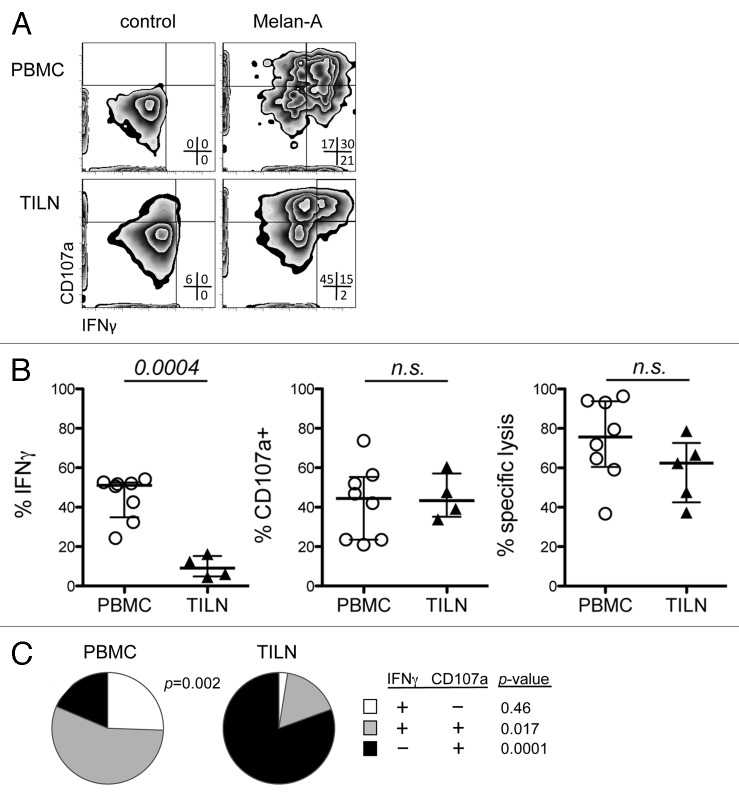
Low IFNγ production by Melan-A-specific CD8+ T-cells from TILN
We compiled the data obtained with T-cells from PBMC and TILN, as assessed with both the LCA and the mLCA. In concurrence with our previous studies,5,7,9 the percentage of IFNγ+ Melan-A-specific T-cells was consistently lower in TILN compared with PBMC (p = 0.0004; Figure 3A and B). In contrast, T-cells from TILN showed high ex vivo cytotoxicity and degranulation, similar to those displayed by the T-cells from PBMC (Fig. 3B). Comparison of lytic activity was performed at E:T = 4, while degranulation and IFNγ production were evaluated at E:T = 0.5. These E:T ratios were chosen as they yielded high, but not maximal, readings (Figs. 1 and 2), and the standard deviation due to experimental conditions was at a minimum (see Table S1, which shows Comparison of LCA with mLCA data). Moreover, the relative frequency of cells expressing either IFNγ, surface CD107a or both was significantly different between the two organs, with the bulk of TILN-derived cells producing either function being single-positive for CD107a, while PBMC-derived cells were largely double-positive (Fig. 3C). In conclusion, ex vivo assessment of T-cells from metastatic lesions consistently reveals deficient IFNγ responses.
Figure 3. TILN-derived melanoma-specific CD8+ T-cells exhibit decreased IFNγ production, but comparable degranulation to their PBMC-derived counterparts. (A) Representative dot plots for degranulation and IFNγ production by PBMC- (LAU 944) and TILN-derived (LAU 465) Melan-A-specific CD8+ T-cells. (B) Frequencies of Melan-A-specific T-cells positive for IFNγ, CD107a at E:T = 0.5. and % specific lysis at E:T = 4 is indicated. Data are means of triplicates. E:T Data for PBMC and TILN were compared using unpaired, two-tailed t-tests. (C) Pies show the relative proportion of Melan-A-specific CD8+ T-cells positive for either IFNγ and/or cell surface CD107a expressing either combination of these markers.
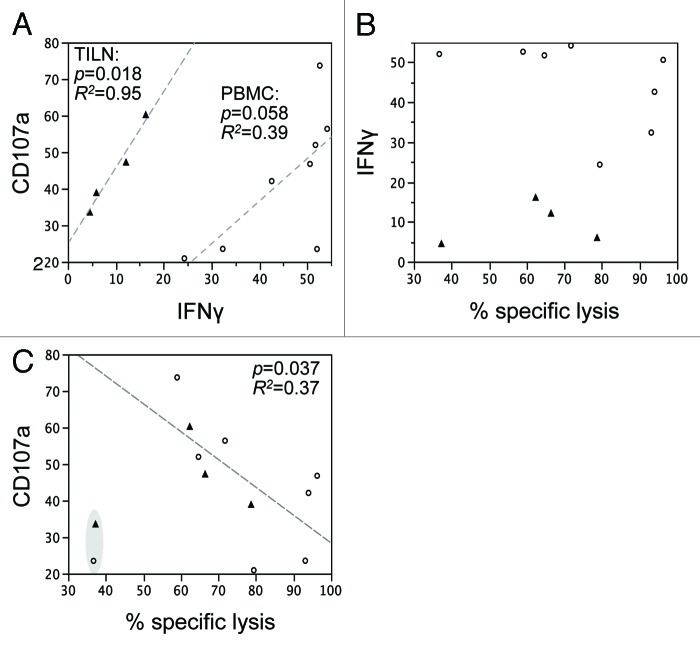
Apparent discrepancy between functional parameters
Even though Melan-A-specific CD8+ T-cells from TILN produced only low levels of IFNγ ex vivo, their IFNγ production correlated with degranulation (CD107a; Figure 4A). A similar trend was observed for PBMC. No correlation was observed between ex vivo IFNγ production and lytic capacity, underlining that IFNγ alone is not sufficient to determine a sample’s reactivity (functionality vs. exhaustion; Figure 4B). Interestingly, an inverse correlation was observed between degranulation and lytic activity (Fig. 4C). This indicates that samples with high ex vivo lytic activity might contain Melan-A-specific cells with high avidity. Thus, only a few (high avidity) cells of the total Melan-A-specific CD8+ T-cell population would be involved in target cell killing, resulting in low frequencies of CD107a+ cells. In contrast, more (lower avidity) cells are involved in Ag-specific lysis in samples with lower lytic activity, hence the elevated frequencies of CD107a+ cells.
Figure 4. Apparent discrepancy between functional parameters. Correlation analysis of functional parameters measured following Ag-specific stimulation of Melan-A-specific cells isolated from either PBMC (open circles) or TILN (closed triangles). (A) CD107a vs. IFNγ. (B) IFNγ vs. % specific lysis. (C) CD107a vs. % specific lysis. The outliers highlighted in gray have been excluded from the statistical analysis of CD107a vs. % specific lysis, as they had very low lytic capacity.
Increased Ag-reactivity following peptide-vaccination
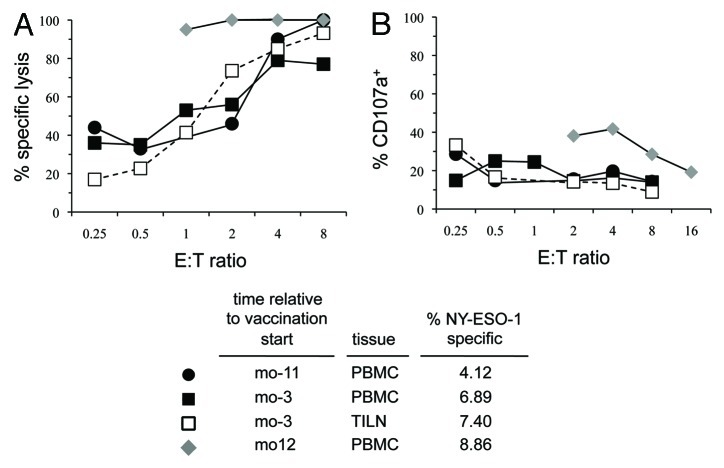
We were able to perform LCAs with longitudinal PBMC samples as well as one TILN from a melanoma patient positive for the cancer/testis Ag NY-ESO-1 (Fig. 5), before and after peptide vaccination.17 Samples obtained pre-vaccination revealed strong ex vivo cytolytic activity, but only very weak degranulation in response to NY-ESO-1-pulsed T2 cells. NY-ESO-1-specific CD8+ T-cells from a PBMC sample drawn after one year of monthly peptide vaccinations had even higher ex vivo cytolytic potential, and a significantly increased degranulation response.
Figure 5. Peptide-vaccination results in increased degranulation and cytolytic activity of tumor Ag-specific CD8+ T-cells. A longitudinal study was performed with NY-ESO-1-specific CD8+ T-cells from a melanoma patient. PBMC samples were collected 11 and 3 mo before, as well as 12 mo after commencing peptide vaccination. TILN were also obtained 3 mo pre-vaccination. (A) Cytolytic activity and (B) degranulation in response to incubation with NY-ESO-1 peptide-pulsed T2 cells were determined.
Discussion
In this study we simultaneously determined cytotoxicity, degranulation and cytokine production of human cancer-specific T-cells directly ex vivo, using the original and modified LiveCount Assays. Strong cytolytic activity was observed not only by circulating T-cells, but also by T-cells from melanoma metastases in lymph nodes, a remarkable result given previous reports of functional impairment of cancer-specific T-cells in metastases.5,7,8,16 T-cells readily killed peptide-pulsed target cells in an Ag-specific manner, to a similar extent as a representative and strongly cytolytic CD8+ CTL clone. We also found efficient recognition and killing of melanoma cells presenting naturally processed antigen. However, killing, degranulation and IFNγ production by T-cells differed considerably between patients, emphasizing the inter-individual differences in T-cell functionality, which possibly reflects, at least in part, differences in TCR avidities18 and cytotoxic mechanisms employed by individual T-cells.
Competent killing activity by T-cells from metastases is in agreement with the notion that cytolytic function often remains intact, despite defects in cytokine production, as observed in exhausted T-cells in chronic/protracted viral infections in mouse models (45) and in HIV and HCV patients.19,20 Recently, we and others have demonstrated that CD8+ T-cells from melanoma metastases are exhausted, as their gene expression profile overlapped significantly with the one of exhausted T-cells in chronic viral infections.7,21 T-cell exhaustion was originally described in mice infected with particular strains of lymphocytic choriomeningitis virus (LCMV) strains causing chronic infections. These mice generated LCMV-specific CD8 T-cells that are dysfunctional and cannot clear the virus.22,23 T-cell exhaustion is defined by the hierarchical loss of cytokine function of effector T-cells, first with the loss of IL-2, then TNFα and finally IFNγ 24. While some exhausted T-cells are driven into apoptosis, large numbers remain vital. The question whether exhausted T-cells are capable of cytolysis is still open.24,25 The immediate cytolytic function of T-cells observed in our experiments is in agreement with their differentiation profile, as the majority of T-cells had an effector memory phenotype (see Table S2 showing frequencies and phenotype of melan-A-specific CD8+ T-cells from PBMC and TILN). Indeed, both PBMC- and TILN-derived T-cells showed efficient Ag-specific cytotoxicity and degranulation directly ex vivo. In contrast, T-cells from TILN displayed impaired IFNγ production. This is in concert with our previous reports demonstrating that T-cells from melanoma metastases expressed abnormally low IFNγ levels.5,7 Such suppressed cytokine production proved to be reversible upon a 2 d in vitro culture in the presence of IL-2.5,7 Thus, T-cells appear to retain functional potential despite the hostility of the tumor environment, even though some of these functions might not be exerted locally due to effective suppressive mechanisms.
Numerous studies have analyzed T-cell function after prolonged in vitro culture, but such studies do not necessarily reflect in vivo function. In mice, where T-cell functions can be studied in vivo, CD8+ effector T-cells are highly cytolytic against target cells occurring as single loosely associated cells in the tissues.26 To some extent, CD8+ effector T-cells are also capable of attacking solid tumors, though in vivo imaging studies have shown that target cell lysis in solid tumors may be very slow27 and that T-cell function may be inhibited by environmental factors such as TGFβ.28,29 Indeed, several factors of the tumor microenvironment have been found to inhibit T-cells.8,30-34 The present data suggest that when CD8+ effector T-cells are separated from the tumor microenvironment, cytolytic function is immediate, whereas cytokine production requires a few days to recover.5
Partially deficient T-cell function has been described more than 20 y ago, in the context of murine thymic T-cell maturation.35 More recently, Ohlen et al. described tumor Ag-specific T-cells with normal effector function but deficient proliferation in a mouse model.36 Partial T-cell function may be due to deficient TCR signaling and/or co-stimulation, which must be strong for proliferation, intermediate for cytokine production and only weak for target cell lysis.37,38 Thus, our findings may be caused by partially deficient TCR and co-stimulatory signals, still sufficient for lysis but not for cytokine production. Furthermore, persistent Ag has been shown to result in impaired nuclear translocation of NFAT proteins, which in turn could negatively impact IFNγ production.25 In any case, the molecular mechanisms underlying the observed functional deficits of T-cells from metastases need to be addressed, and the responsible tumor-derived suppressive mechanism(s)8,30-34 identified. IFNγ is known to be essential for tumor defense,39 and so the lack of IFNγ in TILN is likely important. Tumor Ag-specific CD8+ T-cells are known to also exist in tumor-free lymph nodes.40 However, as frequencies of Ag-specific T-cells are very low in such patient samples, we were not able to test whether such cells behave like their counterparts found in TILN or PBMC.
Cytokine production and degranulation assays are complementary to cytotoxicity assays, with the former investigating intrinsic T-cell properties, and the latter their effects on target cells.14 Our data demonstrate the importance of E:T ratio titration when analyzing cytotoxicity vs. CD107a or IFNγ. Expression of CD107a and IFNγ reflect the proportion of Ag-specific T-cells productively interacting with target cells. The full functional potential of individual T-cells can only be revealed when stimulator/target cells outnumber Ag-specific T-cells. In contrast, cytolysis of target cells, a collective action of all T-cells present, is maximal with high E:T ratios (Fig. 2G). This is important for the design of functional assays.
Independent of E:T ratios, in a biological sample with mixed T-cell avidities and functionalities, a low frequency of Ag-specific cells with measureable cell surface expression of CD107a after 4h triggering might indicate the presence of high avidity cells. In this scenario, the high avidity fraction of the Ag-specific population is dominating the interactions with target cells, which results in a low frequency of degranulating cells but a high lytic activity. In the absence of cells with high functional avidity, many lower avidity cells combine their efforts to act against target cells, resulting in a higher fraction of degranulating cells but a lower lytic activity (Fig. 4).
High T-cell frequencies (i.e., > 0.3% of CD8+ T-cells) induced by endogenous tumors are often observed in metastases but rare in circulating blood cells of cancer patients. Novel T-cell vaccines may induce increased frequencies of tumor Ag-specific T-cells, as well as advanced T-cell differentiation that can be revealed by flow cytometry.41 However, since T-cell differentiation markers do not always correlate with functional characteristics, it is important to measure the T-cell functions directly whenever possible.
Due to low numbers of available cells we were unable to determine whether peptide vaccination had a direct effect on the functionality of TILN-derived T-cells, or whether different vaccination protocols had disparate effects. Longitudinal studies including samples before and after immunotherapy would allow to determine whether a given (immuno-) therapy may indeed result in increased T-cell functionality, though such studies would be more practicable to be performed with PBMC samples. Our LCA analysis of four such samples (with pre- and post-vaccination time-points) from a single melanoma patient indicated an increase not only in the frequency, but also in the ex vivo detectable degranulation and lytic activity of the tumor Ag-specific T-cells.
Recognition of tumor cells presenting naturally processed tumor antigen is critical, but often not the case,42,43 presumably due to low amounts of naturally presented tumor antigen and low avidity of self-specific TCRs.11 The fact that T-cells were capable of killing melanoma cells in the absence of synthetic peptide suggests that TCR-affinities were relatively high, corresponding to our previous findings.11 However, tumor cell recognition varied between patients. In contrast to T-cells from patient LAU 1164, T-cells from patient LAU 1106 lysed Me 290 cells much less efficiently than peptide-pulsed T2 cells, suggesting that the former patient had better TCRs and consequently required lower amounts of antigen for efficient tumor recognition. In the future, comprehensive analyses of TCR repertoire and T-cell function will improve the characterization of T-cell responses. Recently, ex vivo assessment of cytokine production and cytotoxicity has become possible for groups of dominant T-cell clonotypes44 and even individual clonotypes, as we have demonstrated in a strong NY-ESO-1-specific T-cell response of a melanoma patient.17 As T-cell avidity and functionality are key for immune protection, such studies have the potential to reveal correlates of protection against disease,45 providing the rationale to improve T-cell based immunotherapies.
Patients and Methods
Patients and biological specimens
PBMC and TILN were obtained from 14 HLA-A2+ melanoma patients who gave informed consent for this study, approved by the ethical committee of the University of Lausanne and the Ludwig Institute for Cancer Research. PBMC from all patients except patient LAU 50 were analyzed after peptide vaccination with Melan-A peptide, CpG 7909 and IFA.41 Patients LAU 465 and LAU 969 had not received vaccination at the time of TILN isolation, while LAU 672 and LAU 818 had received Melan-A peptide in IFA46 and LAU 352 had received Melan-A peptide in AS02.47 Two PBMC draws and one TILN were obtained from patient LAU 50 before commencing administration of NY-ESO-1, Mage-A10 and Melan-A peptides in Montanide.48 One additional post-vaccination PBMC sample was also included in this study. Ex vivo mononuclear cells were purified and immediately frozen as described previously.40 Frequencies of Melan-A/HLA-A*0201 (see Table S2, which shows frequencies and phenotype of Melan-A-specific CD8+ T-Cells from PBMC and TILN) or NY-ESO-1/HLA-A*0201 multimer binding CD8+ T-cells were determined by flow cytometry.41
CD8+ CTL clones
The CD8+ CTL clones NM cl.55 (Influenza-specific), BC25 cl.R10 (EBV-specific), cl.R11 (Melan-A-specific), cl.R45 and cl.46 (both CMV-specific) were isolated from healthy donors, while LAU 465 cl.11E5 (Melan-A-specific) and LAU 50 cl.1 (NY-ESO-1-specific) were isolated from melanoma patients as follows: peptide/MHC multimer binding CD8+ T-cells were purified by FACS from PBMC, cloned by limiting dilution and periodically (every 3–4 weeks) expanded by stimulation with 1 μg PHA/ml (Sodiag), 5 × 105 irradiated allogeneic feeder cells/ml and 150IU hIL-2/ml (Glaxo Welcome). Cells were used 13–16 d after PHA-stimulation.
Target cell lines
The T2 cell line, a human TAP-deficient TxB cell hybrid expressing low levels of surface HLA-A*0201 and virtually no other surface class I MHC molecules49 was peptide-pulsed to serve as a target. The melanoma-derived cell lines Me 290 (Melan-A+ HLA-A*0201+)50 was used as a specific target, while NA8-MEL (Melan-A– HLA-A*0201+)51 served as an irrelevant melanoma target cell line. Me 290 was kindly provided by D. Rimoldi (Ludwig Institute for Cancer Research, Lausanne Branch, Switzerland), and their identity established by testing for the melanoma Ags Melan-A, Tyr, gp100 and HMW-MAA. NA8-MEL was a kind gift from F. Jotereau (INSERM); it expresses the common melanoma mutation in BRAF. All cell lines are routinely monitored for morphology, growth characteristics and the absence of mycoplasma. Since they are often used in cytolytic assays, potential alterations in their performance and hence their identity would be readily identified.
Media and buffers
Assays were performed in RPMI 1640 containing 100 IU penicillin/ml, 100 μg streptomycin/ml, 2 mM glutamine, 0.1mM non-essential amino acids, 1mM Na pyruvate (all from Gibco, Invitrogen), 5 × 10−5M β-ME (Sigma) and 8% human serum (HS; CTS) (subsequently referred to as RPMI 8% HS). The T-cell clones were maintained in RPMI 8% HS enriched with 150 IU hIL-2/ml (Roche Pharma). T2 cells and melanoma cell lines were cultured in RMPI 1640 with 0.24 mM l-asparagine, 0.55 mM l-arginine HCL (both from Sigma), 1.5 mM glutamine, 10 mM HEPES, 100IU penicillin/ml, 100 μg streptomycin/ml and 10% FCS (Gibco). Staining buffer was 50 mM EDTA (Fluka Chemie) and 0.2% BSA (Calbiochem) in PBS (CHUV) and used during CD8+ T-cell enrichment and immunofluorescent labeling procedures. For intracellular IFNγ detection, cells were fixed with 1% formaldehyde, 2% glucose and 5 mM sodium azide (both from Fluka Chemie) in PBS followed by intracellular labeling in staining buffer containing 0.1% saponin (Sigma).
Peptides and pMHC multimers
The following HLA-A*0201 restricted synthetic peptides were used in the assays: Melan-A26–35/A27L (ELAGIGILTV),52 HIV Polymerase468–476 (ILKEPVHGV),53 hCMV pp65495–503 (NLVPMVATV),54 EBV BMLF280–288 (GLCTLVAML),55 Influenza Matrix58–66 (GILGFVFTL)56 and NY-ESO-1157–165/C165A (SLLMWITQA).57 The peptides were produced by the Biochemistry Institute of the University of Lausanne. Fluorescent pMHC multimers (kindly provided by I. Luescher and P. Guillaume, Ludwig Institute for Cancer Research, Lausanne Branch, Switzerland) were constructed with recombinant HLA-A*0201 and the synthetic peptides indicated above, and were conjugated to APC or PE.
Antibodies and cellular dyes
The mAb CD8AmCyan, CD8APC-H7, IFNγPE-Cy7, anti-CD107aPE-Cy5 were purchased from BD Biosciences (Basel, Switzerland), CD8FITC from Beckman Coulter (Nyon, Switzerland) and CD8MicroBeads for magnetic-enrichment from Miltenyi Biotec (Bergisch Gladbach, Germany). Target cells were labeled with CellTracker® Orange CMTMR (5-(and-6)-((4-chloromethyl) benzoyl) amino) tetramethylrhodamine) or CFSE. The UV-excitable DNA stain DAPI (358ex 461em) or the Violet LIVE/DEAD® Fixable Dead Cell Stain (ViViD) (405ex 451em) were used to evaluate cellular viability (all dyes from Molecular Probes, Invitrogen, Leiden, Netherlands).
LiveCount Assay (LCA)
LCA were performed as described.15 Briefly, T2 cells were labeled with 0.1 μM or 2 μM CMTMR and pulsed with 1 μM of the appropriate peptide. Cells were then washed twice and re-suspended in RPMI 8% HS. A 1:1 mixture of specific and control target cells was prepared and the appropriate volume dispensed into a V-bottomed 96-well plate. CD8+ cells were enriched by magnetic cell sorting prior to isolating Melan-A- or NY-ESO-specific CD8+ T-cells by fluorescence activated cell sorting. Cells were dispensed into wells of a 96-well plate containing 125 or 250 cells of each target cell population to obtain the indicated E:T ratios. Control wells received only the target cell mixture in order to correct for eventual variations in target cell counts. All conditions were prepared in triplicates. Cells were incubated in 50 μl RPMI 8% HS containing CD107aPE-Cy5 mAb and after 3.5 h a fluorescently conjugated CD8 mAb was added. At the end of the 4h co-incubation period, cells were harvested, pelleted and re-suspended in 100 μl staining buffer containing 3 μg/ml DAPI. Samples were acquired on a FACS Vantage SE and analyzed with the instrument’s operating software (CellQuest®, BD Biosciences). Specific lysis was calculated as originally published.
Modified LiveCount Assay (mLCA)
T2 cells and/or melanoma cell lines were labeled with 0.125mM CFSE. T2 cells were pulsed with Melan-A peptide or left unpulsed. All targets were finally re-suspended in RPMI 8% HS. Upon thawing, PBMC and TILN were rested overnight in RPMI 8% HS and CD8+ cells enriched by magnetic cell sorting. These cells were then pelleted by centrifugation, taken up in RPMI 8% HS and dispensed into the wells of a U-bottomed 96-well plate containing specific or irrelevant target cells. Control wells contained only Ag-positive or Ag-negative targets in order to correct for eventual variations in target cell counts. All conditions were prepared in triplicates. Two series of experiments were performed. The first series was done at E:T = 0.5 with 0.12 × 106 to 1.42 × 106 CD8+ T-cells. The number of target cells was adjusted so as to achieve the desired E:T ratio according to the previously determined frequency of Melan-A-specific CD8+ T-cells (see Table S2, which shows frequencies and phenotype of Melan-A-specific CD8+ T-cells from PBMC and TILN). In the second series, the number of CD8+ T-cells was adjusted from patient to patient in order to contain a fixed number (3383) of Melan-A-specific cells per well. These were dispensed into wells containing target cells titrated to attain the indicated E:T ratios. Cells were incubated in 50 μl RMPI 8% HS containing CD107aPE-Cy5 mAb. After 1h, 15 μg/ml of the protein transport inhibitor Brefeldin A was added. At the end of the 4 h co-incubation period, the cells were transferred to tubes and incubated with Melan-A/HLA-A*0201 multimers. Samples were washed and re-suspended in 100 μl staining buffer containing ViViD prior to acquisition on a FACS Vantage SE.
Biostatistical analyses
For E:T titration curves the areas under the curves between E:T ratios 0.25 to 4 or 0.25 to 8 were calculated, and a semi-paired permutation test adapted. This test uses a traditional unpaired t-statistic, but compares it to a corrected permutation distribution in which pairing or the lack thereof is taken into account. To compare the lytic activity generated by pMHC multimer pre-treated vs. untreated CD8+ T-cell clones a paired, two-tailed t-test was applied. Pies were compared using the permutation analysis in Spice 5.1.58 Correlation analyses were performed in JMP 8.0 (SAS). All other comparisons were performed using an unpaired, two-tailed t-test.
Supplementary Material
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
Acknowledgments
We gratefully acknowledge the patients’ participation, as well as the hospital staff’s excellent collaboration. We thank A. Krieg, H. Bouzourene, J.-C. Cerottini, C. Gengler, J. Laurent, H.-A. Lehr, S. Leyvraz, O. Michielin, B. Niklaus, and V. Voelter for collaboration, I. Luescher and P. Guillaume for pMHC multimers, Seppic for Montanide ISA-51 (IFA), and Coley Pharmaceutical Group for CpG 7909. Special thanks go to M. Nason for biostatistical support. Excellent technical and secretarial help was received from C. Beauverd, C. Geldhof, and N. Montandon.
Y.M., E.D., P.R. and D.S. were involved in the conception and experimental design of the study, M.M. and D.S. performed clinical supervision and sampling of patients, P.B. and N.R. phenotyped the patient samples, Y.M., E.D. and P.B. performed the experimental work and together with D.S. analyzed the data. Y.M., E.D. and D.S. wrote the manuscript while all authors were involved in manuscript review and editing.
This work was supported in part by the Deutsche Forschungsgemeinschaft (DFG) grant MA2595/2–1 (Y.D.M.), the Lausanne Branch of the Ludwig Institute for Cancer Research (E.D. and P.B.), the University Hospital, Lausanne (M.M.), the Swiss National Science Foundation (SNF) and the National Center of Competence in Research (NCCR) (D.S. and N.R.), and grants from the Fondation Solidar-Immun (D.S.) and from the FP6 EU “Cancerimmunotherapy” (P.R.).
Footnotes
Previously published online: www.landesbioscience.com/journals/oncoimmunology/article/19856
References
- 1.Dunn GP, Koebel CM, Schreiber RD. Interferons, immunity and cancer immunoediting. Nat Rev Immunol. 2006;6:836–48. doi: 10.1038/nri1961. [DOI] [PubMed] [Google Scholar]
- 2.Stagg J, Johnstone RW, Smyth MJ. From cancer immunosurveillance to cancer immunotherapy. Immunol Rev. 2007;220:82–101. doi: 10.1111/j.1600-065X.2007.00566.x. [DOI] [PubMed] [Google Scholar]
- 3.Rosenberg SA, Yang JC, Sherry RM, Kammula US, Hughes MS, Phan GQ, et al. Durable complete responses in heavily pretreated patients with metastatic melanoma using T-cell transfer immunotherapy. Clin Cancer Res. 2011;17:4550–7. doi: 10.1158/1078-0432.CCR-11-0116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Speiser DE, Pittet MJ, Guillaume P, Lubenow N, Hoffman E, Cerottini JC, et al. Ex vivo analysis of human antigen-specific CD8+ T-cell responses: quality assessment of fluorescent HLA-A2 multimer and interferon-gamma ELISPOT assays for patient immune monitoring. J Immunother. 2004;27:298–308. doi: 10.1097/00002371-200407000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Zippelius A, Batard P, Rubio-Godoy V, Bioley G, Lie´nard D, Lejeune F, et al. Effector function of human tumor-specific CD8 T cells in melanoma lesions: a state of local functional tolerance. Cancer Res. 2004;64:2865–73. doi: 10.1158/0008-5472.CAN-03-3066. [DOI] [PubMed] [Google Scholar]
- 6.Rosenberg SA, Sherry RM, Morton KE, Scharfman WJ, Yang JC, Topalian SL, et al. Tumor progression can occur despite the induction of very high levels of self/tumor antigen-specific CD8+ T cells in patients with melanoma. J Immunol. 2005;175:6169–76. doi: 10.4049/jimmunol.175.9.6169. [DOI] [PubMed] [Google Scholar]
- 7.Baitsch L, Baumgaertner P, Devêvre E, Raghav SK, Legat A, Barba L, et al. Exhaustion of tumor-specific CD8⁺ T cells in metastases from melanoma patients. J Clin Invest. 2011;121:2350–60. doi: 10.1172/JCI46102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hargadon KM, Brinkman CC, Sheasley-O’neill SL, Nichols LA, Bullock TN, Engelhard VH. Incomplete differentiation of antigen-specific CD8 T cells in tumor-draining lymph nodes. J Immunol. 2006;177:6081–90. doi: 10.4049/jimmunol.177.9.6081. [DOI] [PubMed] [Google Scholar]
- 9.Baitsch L, Fuertes-Marraco SA, Legat A, Meyer C, Speiser DE. The three main stumbling blocks for anticancer T cells. Trends Immunol. 2012;Epub ahead of press doi: 10.1016/j.it.2012.02.006. [DOI] [PubMed] [Google Scholar]
- 10.Ch´vez-Gal´n L, Arenas-Del Angel MC, Zenteno E, Ch´vez R, Lascurain R. Cell death mechanisms induced by cytotoxic lymphocytes. Cell Mol Immunol. 2009;6:15–25. doi: 10.1038/cmi.2009.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Speiser DE, Baumgaertner P, Voelter V, Devevre E, Barbey C, Rufer N, et al. Unmodified self antigen triggers human CD8 T cells with stronger tumor reactivity than altered antigen. Proc Natl Acad Sci U S A. 2008;105:3849–54. doi: 10.1073/pnas.0800080105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Betts MR, Brenchley JM, Price DA, De Rosa SC, Douek DC, Roederer M, et al. Sensitive and viable identification of antigen-specific CD8+ T cells by a flow cytometric assay for degranulation. J Immunol Methods. 2003;281:65–78. doi: 10.1016/S0022-1759(03)00265-5. [DOI] [PubMed] [Google Scholar]
- 13.Rubio V, Stuge TB, Singh N, Betts MR, Weber JS, Roederer M, et al. Ex vivo identification, isolation and analysis of tumor-cytolytic T cells. Nat Med. 2003;9:1377–82. doi: 10.1038/nm942. [DOI] [PubMed] [Google Scholar]
- 14.Wolint P, Betts MR, Koup RA, Oxenius A. Immediate cytotoxicity but not degranulation distinguishes effector and memory subsets of CD8+ T cells. J Exp Med. 2004;199:925–36. doi: 10.1084/jem.20031799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Devêvre E, Romero P, Mahnke YD. LiveCount Assay: concomitant measurement of cytolytic activity and phenotypic characterisation of CD8(+) T-cells by flow cytometry. J Immunol Methods. 2006;311:31–46. doi: 10.1016/j.jim.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 16.Pre´vost-Blondel A, Zimmermann C, Stemmer C, Kulmburg P, Rosenthal FM, Pircher H. Tumor-infiltrating lymphocytes exhibiting high ex vivo cytolytic activity fail to prevent murine melanoma tumor growth in vivo. J Immunol. 1998;161:2187–94. [PubMed] [Google Scholar]
- 17.Derre´ L, Bruyninx M, Baumgaertner P, Devevre E, Corthesy P, Touvrey C, et al. In Vivo Persistence of Codominant Human CD8+ T Cell Clonotypes Is Not Limited by Replicative Senescence or Functional Alteration. J Immunol. 2007;179:2368–79. doi: 10.4049/jimmunol.179.4.2368. [DOI] [PubMed] [Google Scholar]
- 18.Riquelme E, Carreño LJ, Gonz´lez PA, Kalergis AM. The duration of TCR/pMHC interactions regulates CTL effector function and tumor-killing capacity. Eur J Immunol. 2009;39:2259–69. doi: 10.1002/eji.200939341. [DOI] [PubMed] [Google Scholar]
- 19.Quigley M, Pereyra F, Nilsson B, Porichis F, Fonseca C, Eichbaum Q, et al. Transcriptional analysis of HIV-specific CD8+ T cells shows that PD-1 inhibits T cell function by upregulating BATF. Nat Med. 2010;16:1147–51. doi: 10.1038/nm.2232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nakamoto N, Cho H, Shaked A, Olthoff K, Valiga ME, Kaminski M, et al. Synergistic reversal of intrahepatic HCV-specific CD8 T cell exhaustion by combined PD-1/CTLA-4 blockade. PLoS Pathog. 2009;5:e1000313. doi: 10.1371/journal.ppat.1000313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wherry EJ, Ha SJ, Kaech SM, Haining WN, Sarkar S, Kalia V, et al. Molecular signature of CD8+ T cell exhaustion during chronic viral infection. Immunity. 2007;27:670–84. doi: 10.1016/j.immuni.2007.09.006. [DOI] [PubMed] [Google Scholar]
- 22.Moskophidis D, Lechner F, Pircher H, Zinkernagel RM. Virus persistence in acutely infected immunocompetent mice by exhaustion of antiviral cytotoxic effector T cells. Nature. 1993;362:758–61. doi: 10.1038/362758a0. [DOI] [PubMed] [Google Scholar]
- 23.Zajac AJ, Blattman JN, Murali-Krishna K, Sourdive DJ, Suresh M, Altman JD, et al. Viral immune evasion due to persistence of activated T cells without effector function. J Exp Med. 1998;188:2205–13. doi: 10.1084/jem.188.12.2205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wherry EJ, Blattman JN, Murali-Krishna K, van der Most R, Ahmed R. Viral persistence alters CD8 T-cell immunodominance and tissue distribution and results in distinct stages of functional impairment. J Virol. 2003;77:4911–27. doi: 10.1128/JVI.77.8.4911-4927.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Agnellini P, Wolint P, Rehr M, Cahenzli J, Karrer U, Oxenius A. Impaired NFAT nuclear translocation results in split exhaustion of virus-specific CD8+ T cell functions during chronic viral infection. Proc Natl Acad Sci U S A. 2007;104:4565–70. doi: 10.1073/pnas.0610335104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Oehen S, Brduscha-Riem K. Differentiation of naive CTL to effector and memory CTL: correlation of effector function with phenotype and cell division. J Immunol. 1998;161:5338–46. [PubMed] [Google Scholar]
- 27.Breart B, Lemaìtre F, Celli S, Bousso P. Two-photon imaging of intratumoral CD8+ T cell cytotoxic activity during adoptive T cell therapy in mice. J Clin Invest. 2008;118:1390–7. doi: 10.1172/JCI34388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pittet MJ, Grimm J, Berger CR, Tamura T, Wojtkiewicz G, Nahrendorf M, et al. In vivo imaging of T cell delivery to tumors after adoptive transfer therapy. Proc Natl Acad Sci U S A. 2007;104:12457–61. doi: 10.1073/pnas.0704460104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schoenborn JR, Wilson CB. Regulation of interferon-gamma during innate and adaptive immune responses. Adv Immunol. 2007;96:41–101. doi: 10.1016/S0065-2776(07)96002-2. [DOI] [PubMed] [Google Scholar]
- 30.Allavena P, Sica A, Garlanda C, Mantovani A. The Yin-Yang of tumor-associated macrophages in neoplastic progression and immune surveillance. Immunol Rev. 2008;222:155–61. doi: 10.1111/j.1600-065X.2008.00607.x. [DOI] [PubMed] [Google Scholar]
- 31.Gajewski TF, Meng Y, Harlin H. Immune suppression in the tumor microenvironment. J Immunother. 2006;29:233–40. doi: 10.1097/01.cji.0000199193.29048.56. [DOI] [PubMed] [Google Scholar]
- 32.Ochsenbein AF, Sierro S, Odermatt B, Pericin M, Karrer U, Hermans J, et al. Roles of tumour localization, second signals and cross priming in cytotoxic T-cell induction. Nature. 2001;411:1058–64. doi: 10.1038/35082583. [DOI] [PubMed] [Google Scholar]
- 33.Speiser DE, Miranda R, Zakarian A, Bachmann MF, McKall-Faienza K, Odermatt B, et al. Self antigens expressed by solid tumors Do not efficiently stimulate naive or activated T cells: implications for immunotherapy. J Exp Med. 1997;186:645–53. doi: 10.1084/jem.186.5.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zou W. Immunosuppressive networks in the tumour environment and their therapeutic relevance. Nat Rev Cancer. 2005;5:263–74. doi: 10.1038/nrc1586. [DOI] [PubMed] [Google Scholar]
- 35.Shimonkevitz RP, Bevan MJ. Split tolerance induced by the intrathymic adoptive transfer of thymocyte stem cells. J Exp Med. 1988;168:143–56. doi: 10.1084/jem.168.1.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ohle´n C, Kalos M, Cheng LE, Shur AC, Hong DJ, Carson BD, et al. CD8(+) T cell tolerance to a tumor-associated antigen is maintained at the level of expansion rather than effector function. J Exp Med. 2002;195:1407–18. doi: 10.1084/jem.20011063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bachmann MF, Sebzda E, Kündig TM, Shahinian A, Speiser DE, Mak TW, et al. T cell responses are governed by avidity and co-stimulatory thresholds. Eur J Immunol. 1996;26:2017–22. doi: 10.1002/eji.1830260908. [DOI] [PubMed] [Google Scholar]
- 38.Faroudi M, Utzny C, Salio M, Cerundolo V, Guiraud M, Müller S, et al. Lytic versus stimulatory synapse in cytotoxic T lymphocyte/target cell interaction: manifestation of a dual activation threshold. Proc Natl Acad Sci U S A. 2003;100:14145–50. doi: 10.1073/pnas.2334336100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Blankenstein T. The role of tumor stroma in the interaction between tumor and immune system. Curr Opin Immunol. 2005;17:180–6. doi: 10.1016/j.coi.2005.01.008. [DOI] [PubMed] [Google Scholar]
- 40.Romero P, Dunbar PR, Valmori D, Pittet M, Ogg GS, Rimoldi D, et al. Ex vivo staining of metastatic lymph nodes by class I major histocompatibility complex tetramers reveals high numbers of antigen-experienced tumor-specific cytolytic T lymphocytes. J Exp Med. 1998;188:1641–50. doi: 10.1084/jem.188.9.1641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Speiser DE, Lie´nard D, Rufer N, Rubio-Godoy V, Rimoldi D, Lejeune F, et al. Rapid and strong human CD8+ T cell responses to vaccination with peptide, IFA, and CpG oligodeoxynucleotide 7909. J Clin Invest. 2005;115:739–46. doi: 10.1172/JCI23373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.So T, Hanagiri T, Chapiro J, Colau D, Brasseur F, Yasumoto K, et al. Lack of tumor recognition by cytolytic T lymphocyte clones recognizing peptide 195-203 encoded by gene MAGE-A3 and presented by HLA-A24 molecules. Cancer Immunol Immunother. 2007;56:259–69. doi: 10.1007/s00262-006-0186-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Speiser DE, Cerottini JC, Romero P. Can hTERT peptide (540-548) -specific CD8 T cells recognize and kill tumor cells? Cancer Immun. 2002;2:14. [PubMed] [Google Scholar]
- 44.Price DA, Brenchley JM, Ruff LE, Betts MR, Hill BJ, Roederer M, et al. Avidity for antigen shapes clonal dominance in CD8+ T cell populations specific for persistent DNA viruses. J Exp Med. 2005;202:1349–61. doi: 10.1084/jem.20051357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kalia V, Sarkar S, Gourley TS, Rouse BT, Ahmed R. Differentiation of memory B and T cells. Curr Opin Immunol. 2006;18:255–64. doi: 10.1016/j.coi.2006.03.020. [DOI] [PubMed] [Google Scholar]
- 46.Lie´nard D, Rimoldi D, Marchand M, Dietrich PY, van Baren N, Geldhof C, et al. Ex vivo detectable activation of Melan-A-specific T cells correlating with inflammatory skin reactions in melanoma patients vaccinated with peptides in IFA. Cancer Immun. 2004;4:4. [PubMed] [Google Scholar]
- 47.Ayyoub M, Zippelius A, Pittet MJ, Rimoldi D, Valmori D, Cerottini JC, et al. Activation of human melanoma reactive CD8+ T cells by vaccination with an immunogenic peptide analog derived from Melan-A/melanoma antigen recognized by T cells-1. Clin Cancer Res. 2003;9:669–77. [PubMed] [Google Scholar]
- 48.Baumgaertner P, Rufer N, Devevre E, Derre L, Rimoldi D, Geldhof C, et al. Ex vivo detectable human CD8 T-cell responses to cancer-testis antigens. Cancer Res. 2006;66:1912–6. doi: 10.1158/0008-5472.CAN-05-3793. [DOI] [PubMed] [Google Scholar]
- 49.Salter RD, Cresswell P. Impaired assembly and transport of HLA-A and -B antigens in a mutant TxB cell hybrid. EMBO J. 1986;5:943–9. doi: 10.1002/j.1460-2075.1986.tb04307.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Valmori D, Gervois N, Rimoldi D, Fonteneau JF, Bonelo A, Lie´nard D, et al. Diversity of the fine specificity displayed by HLA-A*0201-restricted CTL specific for the immunodominant Melan-A/MART-1 antigenic peptide. J Immunol. 1998;161:6956–62. [PubMed] [Google Scholar]
- 51.Guilloux Y, Lucas S, Brichard VG, Van Pel A, Viret C, De Plaen E, et al. A peptide recognized by human cytolytic T lymphocytes on HLA-A2 melanomas is encoded by an intron sequence of the N-acetylglucosaminyltransferase V gene. J Exp Med. 1996;183:1173–83. doi: 10.1084/jem.183.3.1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Valmori D, Fonteneau JF, Lizana CM, Gervois N, Lie´nard D, Rimoldi D, et al. Enhanced generation of specific tumor-reactive CTL in vitro by selected Melan-A/MART-1 immunodominant peptide analogues. J Immunol. 1998;160:1750–8. [PubMed] [Google Scholar]
- 53.Walker BD, Flexner C, Birch-Limberger K, Fisher L, Paradis TJ, Aldovini A, et al. Long-term culture and fine specificity of human cytotoxic T-lymphocyte clones reactive with human immunodeficiency virus type 1. Proc Natl Acad Sci U S A. 1989;86:9514–8. doi: 10.1073/pnas.86.23.9514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Solache A, Morgan CL, Dodi AI, Morte C, Scott I, Baboonian C, et al. Identification of three HLA-A*0201-restricted cytotoxic T cell epitopes in the cytomegalovirus protein pp65 that are conserved between eight strains of the virus. J Immunol. 1999;163:5512–8. [PubMed] [Google Scholar]
- 55.Steven NM, Annels NE, Kumar A, Leese AM, Kurilla MG, Rickinson AB. Immediate early and early lytic cycle proteins are frequent targets of the Epstein-Barr virus-induced cytotoxic T cell response. J Exp Med. 1997;185:1605–17. doi: 10.1084/jem.185.9.1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bednarek MA, Sauma SY, Gammon MC, Porter G, Tamhankar S, Williamson AR, et al. The minimum peptide epitope from the influenza virus matrix protein. Extra and intracellular loading of HLA-A2. J Immunol. 1991;147:4047–53. [PubMed] [Google Scholar]
- 57.Valmori D, Dutoit V, Lie´nard D, Rimoldi D, Pittet MJ, Champagne P, et al. Naturally occurring human lymphocyte antigen-A2 restricted CD8+ T-cell response to the cancer testis antigen NY-ESO-1 in melanoma patients. Cancer Res. 2000;60:4499–506. [PubMed] [Google Scholar]
- 58.Roederer M, Nozzi JL, Nason MC. SPICE: exploration and analysis of post-cytometric complex multivariate datasets. Cytometry A. 2011;79:167–74. doi: 10.1002/cyto.a.21015. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.